Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic precipitated fear of contagion and influenced many people to avoid the emergency department (ED). It is unknown if this avoidance effected overall health or disease mortality.
Objective
We aimed to quantify the decreased ED volume in the United States, determine whether it occurred simultaneously across the country, find which types of patients decreased, and measure resultant changes in patient outcomes.
Methods
We retrospectively accessed a multihospital, multistate electronic health records database managed by HCA Healthcare to obtain a case series of all patients presenting to an ED during the early COVID-19 pandemic (March 1–May 31, 2020) and the same dates in 2019 for comparison. We determined ED volume using weekly totals and grouped them by state. We also recorded final diagnoses codes and mortality data to describe patient types and outcomes.
Results
The weekly ED volume from 160 facilities dropped 44% from 141,408 patients (week 1, March 1–7, 2020) to a nadir of 79,618 patients (week 7, April 12–18, 2020), before rising back to 105,667 (week 13, May 24–30, 2020). Compared with 2019, this overall decline was statistically significant (p < 0.001). The decline was universal across disease categories except for infectious disease and respiratory illnesses, which increased. All-cause mortality increased during the pandemic, especially for those with infectious disease, circulatory, and respiratory illnesses.
Conclusions
The COVID-19 pandemic and an apparent fear of contagion caused a decrease in ED presentations across our hospital system. The decline in ED volume was associated with increased ED mortality, perhaps from delayed ED presentations.
Keywords: emergency department utilization, emergency department volume, novel coronavirus 2019, SARS-CoV-2
Introduction
In late December 2019, a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic began in the Wuhan province of China. Over the next several months, the viral disease called coronavirus disease 2019 (COVID-19) spread throughout China and began to spread internationally as well, first to Iran and Italy and then subsequently to the United States. The first “hotspots” in the United States occurred in February and March of 2020 on the west coast (in California, Oregon, and Washington), followed rapidly by the New York City tristate area. By April 2020, SARS-CoV-2 began spreading across the United States. Many emergency departments (EDs) had a dramatic drop in utilization, while at the same time treating patients with higher acuity and boarding the admitted patients in the ED. The total number of weekly ED visits in the United States reported by the National Syndromic Surveillance Program at the U.S. Centers for Disease Control and Prevention (CDC) for weeks 1 to 11 of 2020 ranged between 2.22 and 2.41 million per week and declined sharply to a low of 1.25 million per week at week 14 (March 29–April 4), when the CDC stopped reporting these data online (1). After April 4, 2020, the CDC reported that a high volume of telemedicine visits precluded them from gaining accurate data on ED visits for COVID-19–like illness or influenza-like illnesses. However, the sharp decline in ED patient volume had many unanticipated consequences, including decreased hours, furloughs, or terminations for many health care workers (physicians and others) (2,3).
In 2017, the most recent year complete data were available from the CDC, there were an estimated 139.0 million patient visits to EDs (4). Historically, the rate of growth for ED patient volume per year is 2.3 million. By extrapolation, 2019 had an estimated 143.6 million patient visits. In 2020, we hypothesize that ED visits were significantly reduced because of the COVID-19 pandemic, which would also increase case severity (1). Multiple factors may have influenced patients to stay away from the ED during the pandemic. One possible explanation is that patients did not want to be exposed to SARS-CoV-2 by coming to the ED (5, 6, 7). Another possibility is that a surge in telehealth and telemedicine decreased the need for urgent care visits (8). Lastly, there is the possibility that patients are simply going without the emergent care that they need (9, 10, 11, 12, 13). If either the first or third possibility are correct, one would expect worsening of mortality or other health outcome statistics (14).
HCA Healthcare maintains an electronic data warehouse (EDW) consisting of all patient care visits within their hospital system. In 2019, HCA Healthcare treated 9.2 million ED patients, or approximately 6.4% of all patients reporting to EDs in the country (based on the 143.6 million visits estimated by the CDC). The HCA Healthcare EDW provides an excellent resource to identify trends in ED utilization and may be especially useful to illuminate clinical outcomes during the COVID-19 pandemic. Using the data from the EDW we sought to quantify the types of ED patients who presented to the ED during the pandemic, based on chief complaint or final diagnosis. The data can also be broken down geographically by state, which will allow us to determine if the timeline for changes in ED volume occurred at the same or different times across the country. We will also be able to quantify the recovery of ED volumes in the database. Lastly, the EDW also contains some outcome data, which allow us to determine if delayed ED presentations were associated with worse patient outcomes. The primary purpose of this retrospective analysis of our hospital system was to see if there was a relationship with ED volume and patient outcomes. We hypothesized that as ED patient volume declined, the patient mortality rate would go up.
Methods
We retrospectively accessed a central database containing data from all HCA Healthcare hospitals in the United States. Volume level ED data were abstracted from March 1, 2019 through May 31, 2020 for all adult (age >18) patients seen in HCA Healthcare EDs. Safe Harbor deidentification techniques were used such that no protected health information was abstracted out of the central database for our analyses. The project received an institutional-level institutional review board exempt determination. We included all HCA Healthcare hospitals with EDs; and excluded any hospital located outside of the United States, any hospital without an ED, and any hospital or ED newly acquired by HCA Healthcare in 2020 that would not have comparison data from 2019. For each ED in our dataset, we identified its location (state) and number of licensed hospital inpatient beds as a proxy for hospital size. Precise ED size (bed count) was not available. Then we calculated ED volumes on a weekly basis for each hospital during the early phase of the COVID-19 pandemic (March 1-May 30, 2020) and for comparison the corresponding weeks in 2019. Final ED diagnosis codes were collected and collated by organ systems based on the first letter of the International Classification of Diseases, 10th revision (ICD-10) codes. Other data abstracted from the database included the disposition from the ED (admission, discharged, or expired), the highest level of inpatient floor required for admitted patients (floor or intensive care unit), the duration of hospitalization (days), and the final status (discharged home, to hospice, or died).
Statistical analysis was performed using SAS software (version 9.4; SAS Inc., Cary, NC) and graphs were created using Tableau or Excel (Microsoft, Redmond, WA). Descriptive statistics were used to categorize hospital by size and location. We compared ED volumes for all hospitals in the same weeks between 2019 and 2020 using the Wilcoxon signed rank test. We divided our data for subgroup analysis by location (state), organ system (final diagnosis codes), or outcomes by mortality rates (number of deaths/actual ED volume). An α level of p < 0.05 was accepted as the level of statistical significance for all comparisons. Lastly, we performed a generalized linear model analysis to compare the relationship of actual ED volume and mortality rate (number of deaths/actual ED volume). This was done with and without including the infectious disease category to account for any COVID-19–related deaths.
Results
HCA Healthcare owns 186 hospitals in its health care system. After we applied exclusion criteria, 160 hospital EDs were included in our analysis. These hospitals were located in 18 states across the continental United States; however, the majority were located in the southeast and southwestern areas of the country. Collectively, the hospitals contained 44,296 licensed inpatient beds and 1.32 million ED visits during the study period. Description of the hospitals, location (state), and their ED patient volumes are shown in Table 1, Table 2 . The overall ED volume in our study period during 2020 was significantly lower that the same time period in 2019 (p < 0.001).
Table 1.
Geographic Location and Sizes of all EDs With Weekly Encounters
| State | Hospitals Within State (n) | Total Licensed Inpatient Beds, n (% of Total) | ED Volume by Week Number (n) |
Max Decrease from Week 1 (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||||
| CA | 5 | 1858 (4.19) | 5873 | 5822 | 4895 | 3873 | 3560 | 3225∗ | 3255 | 3446 | 3574 | 3709 | 3689 | 4050 | 4281 | 45.1 |
| CO | 6 | 2311 (5.22) | 5837 | 5697 | 4730 | 4120 | 3641 | 3369 | 3180∗ | 3695 | 3720 | 3577 | 3667 | 4116 | 4164 | 45.5 |
| FL | 44 | 12,037 (27.17) | 45,364 | 45,223 | 39,578 | 31,653 | 26,654 | 25,361 | 25,081∗ | 25,678 | 26,690 | 28,291 | 28,750 | 31,682 | 32,608 | 44.7 |
| GA | 7 | 1744 (3.94) | 6897 | 7409 | 6128 | 4958 | 4295 | 3994∗ | 4012 | 4134 | 4351 | 4738 | 4906 | 5355 | 5547 | 42.1 |
| ID | 2 | 468 (1.06) | 1181 | 1179 | 1100 | 876 | 762 | 796 | 728∗ | 764 | 757 | 770 | 851 | 920 | 1008 | 38.4 |
| IN | 1 | 278 (0.63) | 364 | 386 | 314 | 289 | 222 | 221∗ | 224 | 255 | 266 | 238 | 266 | 268 | 277 | 39.3 |
| KS | 4 | 1374 (3.1) | 3309 | 3179 | 2599 | 2300 | 1972 | 1899 | 1757∗ | 1957 | 2051 | 2182 | 2229 | 2375 | 2573 | 46.9 |
| KY | 2 | 384 (0.87) | 1163 | 1145 | 971 | 812 | 650 | 636∗ | 663 | 672 | 766 | 810 | 784 | 869 | 929 | 45.3 |
| LA | 3 | 914 (2.06) | 2480 | 2488 | 1995 | 1536 | 1260 | 1158∗ | 1171 | 1314 | 1361 | 1472 | 1522 | 1729 | 1754 | 53.3 |
| MS | 1 | 130 (0.29) | 3329 | 3253 | 2739 | 2270 | 2120 | 1976∗ | 1981 | 2084 | 2131 | 2336 | 2328 | 2651 | 2661 | 40.6 |
| MO | 5 | 1058 (2.39) | 599 | 630 | 533 | 431 | 327 | 306∗ | 335 | 353 | 347 | 365 | 432 | 458 | 435 | 48.9 |
| NV | 3 | 1349 (3.05) | 1120 | 1066 | 971 | 753 | 620 | 642 | 676 | 682 | 724 | 742 | 762 | 824 | 869 | 44.6 |
| NH | 2 | 306 (0.69) | 4780 | 4860 | 4345 | 3558 | 3189 | 2968∗ | 2970 | 3069 | 3326 | 3293 | 3412 | 3511 | 3803 | 37.9 |
| SC | 3 | 941 (2.12) | 4740 | 4822 | 4117 | 3219 | 2874 | 2696 | 2692∗ | 2888 | 2940 | 3227 | 3352 | 3818 | 3961 | 43.2 |
| TN | 11 | 2251 (5.08) | 8216 | 8378 | 7225 | 6009 | 5234 | 5074 | 5050∗ | 5323 | 5423 | 5780 | 6000 | 6317 | 6730 | 38.5 |
| TX | 45 | 13,042 (29.44) | 35,269 | 35,678 | 30,887 | 24,832 | 20,891 | 19,936 | 19,767∗ | 21,310 | 22,408 | 23,185 | 23,141 | 25,707 | 25,906 | 44.0 |
| UT | 6 | 671 (1.51) | 1612 | 1544 | 1432 | 1331 | 1071∗ | 1128 | 1072 | 1203 | 1178 | 1212 | 1239 | 1391 | 1390 | 33.6 |
| VA | 10 | 3180 (7.18) | 9262 | 9240 | 7833 | 6308 | 5460 | 5047 | 4974∗ | 5321 | 5655 | 5792 | 5851 | 6487 | 6702 | 46.3 |
| All states | 160 | 44,296 | Median | 44.3 | ||||||||||||
| IQR | 39.6–45.5 | |||||||||||||||
ED = emergency department; IQR = interquartile range.
Week 1 began on March 1, 2020. Week 13 began on May 24, 2020.
Indicates the state's lowest volume between weeks 1 and 13.
Table 2.
Weekly ED Volumes During Study Period
| Week # | Dates | Volume in 2019 | Volume in 2020 | Difference |
|---|---|---|---|---|
| 1 | 03/01–03/07 | 134,663 | 141,408 | −6745 |
| 2 | 03/08–03/14 | 142,250 | 142,012 | 238 |
| 3 | 03/15–03/21 | 140,515 | 122,406 | 18,109 |
| 4 | 03/22–03/28 | 139,466 | 99,143 | 40,323 |
| 5 | 03/29–04/04 | 135,917 | 84,824 | 51,093 |
| 6 | 04/05–04/11 | 138,945 | 80,452 | 58,493 |
| 7 | 04/12–04/18 | 135,525 | 79,618 | 55,907 |
| 8 | 04/19–04/25 | 133,779 | 84,187 | 49,592 |
| 9 | 04/26–05/02 | 136,850 | 87,727 | 49,123 |
| 10 | 05/03–05/09 | 136,691 | 91,820 | 44,871 |
| 11 | 05/10–05/16 | 135,410 | 93,361 | 42,049 |
| 12 | 05/17–05/23 | 137,442 | 102,605 | 34,837 |
| 13 | 05/24–05/30 | 139,167 | 105,677 | 33,490 |
| Median monthly ED volume | 136,850 | 93,361 | 42,049 | |
| IQR | (135,525–139,167) | (84,824–105,677) | (33,490–49,592) | |
| Wilcoxon Signed Rank test | p < 0.001 |
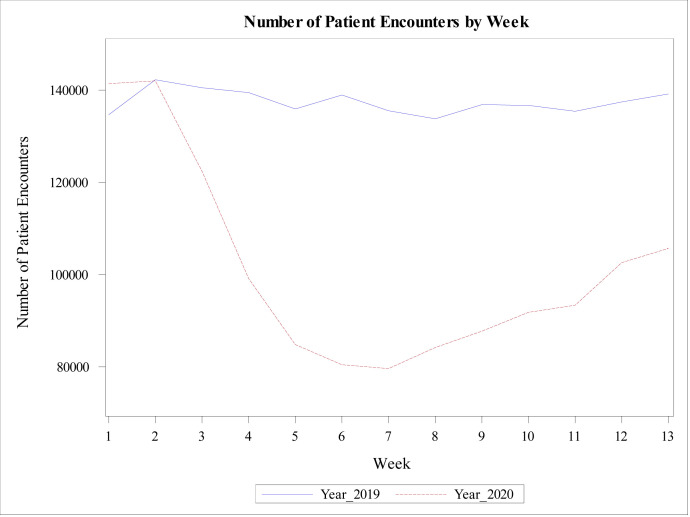
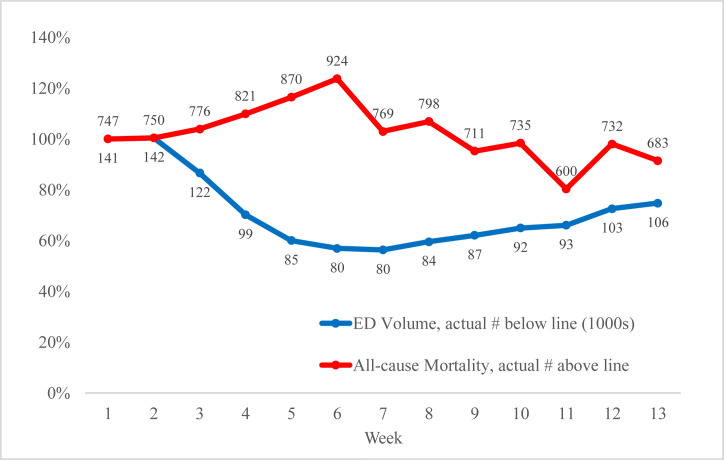
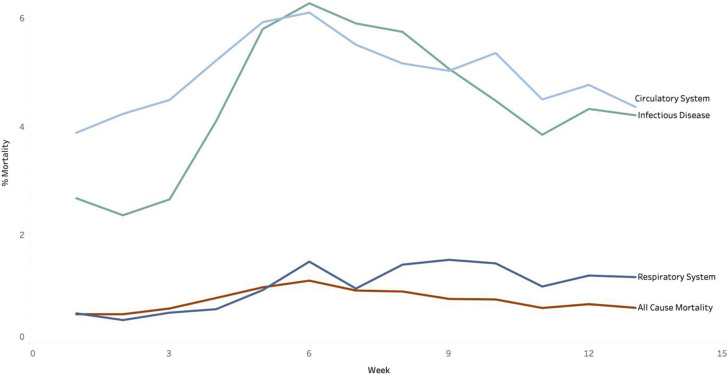
Using this large sample, we tracked the ED volume across the study timeframe between March and May 2020 (Figure 1 ). During the 2020 study period, we noted that the ED volumes decreased (−18,107 visits) beginning in week 3 (March 15–21, 2020). By week 6 (April 5–11, 2020), the volumes had dropped >43% (−58,493 visits) compared with the volumes during the same week of 2019. In other words, the ED volumes in week 6 were about 57% of expected volume, based on 2019 numbers. At the same time, the all-cause mortality count increased from 747 to a maximum of 924 deaths in a week (Figure 2 ). Analysis of the individual final diagnosis codes and their associated mortality percentages (top 3) are illustrated in Figure 3 . The 2 organ systems with the greatest increase in presentation to the ED were the infectious disease and respiratory categories. The 3 organ systems with the greatest increase in mortality rates were the infectious disease, circulatory, and respiratory categories.
Figure 1.
Number of patient encounters in the emergency department in 2019 and 2020. Week 1 began on March 1, 2020.
Figure 2.
Relative weekly emergency department (ED) volume and all-cause mortality compared with week 1 (March 1, 2020).
Figure 3.
Weekly mortality by disease category, top 3 categories. Week 1 began on March 1, 2020.
After the nadir of ED volume in weeks 6 and 7, ED volume started to recover slowly toward the expected volumes of 2019. For example, by week 10, the ED volume was at 64.9% of the corresponding 2019 volume. In addition, all-cause mortality was declining by week 10 but was still higher than the baseline value (week 1). This pattern continued until the end of the study period, but neither all-cause mortality nor ED volume reached their respective baseline values. By week 13 (May 24–30, 2020), the ED volume recovered to only 74.7% of the 2019 values, and the all-cause mortality remained higher than week 1's value in our dataset.
Generalized linear model analysis further supported the inverse relationship between ED volume and mortality percentage (actual mortality/actual ED volume) in each week. While controlling for all disease categories, lower weekly ED volumes were significantly related to a higher overall mortality percentage. For every 10,000 fewer weekly patient encounters, a 0.086 increased mortality percentage was expected (degrees of freedom = 17, R 2 = 0.932, p < 0.001). While controlling for all disease categories except infectious disease patients (which contain COVID-19 and other infectious disease patients), lower weekly ED volumes were still significantly related to a higher mortality percentage. For every 10,000 fewer weekly patient encounters, a 0.0597 increased mortality percentage was expected (degrees of freedom = 16, R 2 = 0.944, p < 0.001).
Discussion
Our results support the observations from the CDC that ED patient volume in the United States significantly decreased in March and April of 2020 (1). However, the CDC stopped reporting ED volume around week 14 of 2020 on their website, corresponding to the week ending April 4, 2020. Our data showed that ED volume continued to decline in the HCA Healthcare system for an additional 2 weeks, until the week ending April 18, 2020. ED volumes gradually increased after that but had not returned to baseline by the end of our study period (May 30, 2020). These findings are consistent with nationwide data reported from the CDC in their weekly morbidity and mortality report (15).
This study shows that the decreased ED patient volume during the early stages of the COVID-19 pandemic was associated with an increased number of deaths, and actual numbers can be seen in Figure 2. Figure 3 shows 3 disease categories in which mortality rose during the study period: infectious diseases, circulatory illness, and respiratory illnesses. Overall mortality also increased during the study period. It is important to note that these mortality increases occurred before these hospitals had more than minimal presence of SARS-CoV-2 in the community as reflected by publicly reported SARS-CoV-2 testing results (16,17). Major increases—“spikes” in cases—were not recorded in most southeastern or southwestern states until June 2020. As such, our observed increased mortality should not be attributed to complications of SARS-CoV-2 infection.
There have been multiple reports in the media during this time that the general population was afraid to go to their local hospitals because of the perceived risk of contracting SARS-CoV-2 infection (5, 6, 7). For example, a survey of 1000 telehealth patients in June 2020 revealed that only 12% of respondents felt an urgent care/ED was safe to enter compared with 42% finding a grocery store safe (5). We did not attempt to discern the cause of the decreased ED volumes in our study. We can only assert that the decreased ED volumes occurred several weeks after the calendar “start” of the COVID-19 pandemic. However, given that the local SARS-CoV-2 infection rates do not correlate with the decreased ED volumes, we can infer that public perception and fear of their local hospital may be responsible for some of the decreased volume (16,17).
Paradoxically, the public fear of contagion causing patients not to present to the ED for treatment may have been irrational and caused public harm by increasing their overall mortality from all illnesses. Symptoms of illness, such as chest pain, that would have normally compelled them to present for medical treatment may have been ignored for longer amounts of time. The SARS-CoV-2 virus had a low prevalence of disease and overall mortality numbers in the Southern United States during our study period (16). The COVID-19 hotspots (i.e., New York City), however, had an approximate 1.4% case fatality rate (confirmed cases/confirmed deaths) during April and May 2020 (18). Avoiding the ED from fear of contagion can have bad consequences. Our generalized linear model of mortality percentages showed that delaying ED treatment in nonhotspot locations during the early COVID-19 pandemic was associated with an increased mortality percentage.
Lastly, during past viral epidemics such as influenza A (H1N1) in 2009, EDs planned for and saw a surge of ED patient volume (19, 20, 21). We were unable to find any reported evidence that the 2009 H1N1-related increase of ED volume caused either a higher or lower all-cause mortality or ED performance during the surge (21). More focus at that time was paid on disaster preparedness and finding ways to upsize capacity to treat a surge of patients (22, 23, 24, 25). The worldwide COVID-19 pandemic was different; our analysis of the HCA Healthcare system showed that the fear of contagion unexpectedly decreased ED utilization and this was associated with increased all-cause mortality.
Limitations
Though the electronic database at HCA Healthcare was quite large, it has some clear limitations. First, the majority of HCA Healthcare hospitals (89/160) and ED patients resided in 2 states (Florida and Texas). Therefore, despite HCA Healthcare hospitals being represented in 18 states, the entirety of the database is not representative of the whole country. Rather, it is more representative of the southwestern and southeastern states. The absence of analysis in zones of higher COVID-19 activity in April and May (New York City) may have affected our results. Nevertheless, all 18 states with HCA Healthcare hospitals had a nadir of ED patient volumes between April 5 and April 18, 2020. These restrictions prevent us from generalizing our findings to geographic locations outside of our database. However, as COVID-19 was a nationwide pandemic and economic collapse, and our data are consistent with the nationwide data from the CDC, we assume a similar pattern of decreased ED patient volumes occurred in all other nonhotspot states (1).
Second, with this deidentified dataset we were only able to collect volume level data on a weekly basis. No patient-specific data—such as patient age, race, gender, or chief complaint—were collected, thus limiting our results and analysis. It would have been interesting to know which types of patients were less likely to present to the ED during this time period; this has been reported elsewhere by the CDC (15). We arbitrarily set an end date for our query of the database, knowing that this is a snapshot of the pandemic still occurring. However, fear and hysteria were greatest in this timeframe, and this would allow us to show the greatest change in resultant ED volumes. It would be interesting to investigate how ED volume recovered from June through the end of 2020 and beyond.
Lastly, we group patients into disease categories by using the first letter of the final ICD-10 code. This was the only way to determine which types of patients had presented for treatment. Although it was a crude measurement, it did provide some useful information. For ED patients that were discharged home, the primary final diagnosis code was used (no secondary diagnosis codes). Similarly, for any admitted patients, only the primary final discharge diagnosis code was used in this assessment. This system would introduce errors and missed diagnoses, such as if they were sequenced incorrectly. It also caused some misclassification for our analysis. For example, if a patient was diagnosed with “chest pain” (ICD-10 R07.9), it would fall under the category of “signs, symptoms, abnormal clinical/lab findings”; if a patient was diagnosed with “angina pectoris” (ICD-10 I20), it would fall under the “circulatory system.” Many different organ system complaints would fall under the abnormal clinical findings grouping, so the presenting complaint data from this grouping is nonspecific. In our analysis, about 18% fell into the abnormal clinical findings grouping. However, the remaining 82% of patients we believe were grouped into organ systems with reasonable fidelity. Averaged over >1 million patients, we feel it was still a reliable indicator of disease category for the entire cohort. Assuming the variance stayed consistent across the time period, the weekly data still showed visible differences.
Conclusions
In summary, ED volume within HCA Healthcare dropped ≤44% during the early stages of the COVID-19 pandemic. In addition, patient mortality for common conditions increased significantly during this time period, especially for infectious disease, circulatory, and respiratory illnesses. This occurred despite relatively low SARS-CoV-2 infection rates in our regions during the early stages of the pandemic. Our results suggest that avoiding the ED during a frightening pandemic may be ill advised and may increase the percentage of patient deaths. During future pandemics, public health efforts should be made to counteract the public's fear of contagion at hospitals. In truth, with all staff wearing personal protective equipment and treating patients in isolation, the ED may be one of the safer public places outside of one's home. ED providers should focus on maintaining current standard of care for all types of patients during an infectious pandemic, and being prepared to treat higher acuity patients who may have waited longer and became more ill before presenting to the ED.
Article Summary
1. Why is this topic important?
Emergency department (ED) patient volumes declined during the coronavirus disease 2019 pandemic, and it is unknown if that affected patient outcomes.
2. What does this study attempt to show?
This study shows that public fear of the ED during an infectious pandemic is ill advised and may lead to worse overall patient outcomes.
3. What are the key findings?
The coronavirus disease 2019 pandemic caused a >40% decrease in patient volume in the spring of 2020. Our study of 160 EDs showed that during this period, the all-cause mortality percentage more than doubled. Specifically, patients with circulatory, respiratory, and infectious disease illnesses had worse outcomes during this period.
4. How is patient care impacted?
Patient fear of the ED during a national pandemic caused worse outcomes for all medical conditions, possibly because of delayed presentations of all types of critical illnesses.
Acknowledgments
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Footnotes
Reprints are not available from the authors.
References
- 1.U.S. Centers for Disease Control and Prevention website. COVIDView: a weekly surveillance summary of U.S. COVID-19 activity. Emergency department visits percentage of visits for COVID-19-like illness (CLI) or influenza-like illness (ILI) September 29, 2019 - April 18, 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/09112020/covid-like-illness.html Available at:
- 2.Brooksbank T. Health care workers fear losing their jobs during coronavirus pandemic. https://abcnews.go.com/Health/health-care-workers-fear-losing-jobs-coronavirus-pandemic/story?id=70087102 Available at:
- 3.Anderson M. Amid pandemic, hospitals lay off 1.4M workers in April. https://www.npr.org/2020/05/10/853524764/amid-pandemic-hospitals-lay-off-1-4m-workers-in-april Available at:
- 4.Rui P., Kang K. National Hospital Ambulatory Medical Care Survey: 2017 emergency department summary tables. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf Available at:
- 5.COVID-19 impact: 43% of patients apprehensive about going back to see a healthcare provider in person until at least the fall, with anxiety lasting into 2021. https://www.businesswire.com/news/home/20200728005153/en/COVID-19-Impact-43-Patients-Apprehensive-Healthcare-Provider Available at:
- 6.McFarling L. ‘Where are all our patients?’: Covid phobia is keeping people with serious heart symptoms away from ERs. https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/ Available at:
- 7.Stone W., Yu E. COVID-19 fears may be causing people to ignore medical emergencies. https://www.npr.org/2020/05/06/851173949/covid-19-fears-may-be-causing-people-to-ignore-medical-emergencies Available at:
- 8.Bosworth A., Ruhter J., Samson L.W., et al. Medicare beneficiary use of telehealth visits: early data from the start of COVID-19 Pandemic. https://aspe.hhs.gov/system/files/pdf/263866/HP_IssueBrief_MedicareTelehealth_final7.29.20.pdf Available at:
- 9.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Filippo O., D’Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for acs during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Solomon M.D., McNulty E.J., Rana J.S., et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 12.Siripanthong B., Hanff T.C., Levin M.G., et al. Coronavirus disease 2019 is delaying the diagnosis and management of chest pain, acute coronary syndromes, myocarditis and heart failure. Future Cardiol. 2021;17:3–6. doi: 10.2217/fca-2020-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lange S.J., Ritchey M.D., Goodman A.B., et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teo K.-C., Leung W.C.Y., Wong Y.-K., et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johns Hopkins University of Medicine website. Coronavirus resource center. https://coronavirus.jhu.edu Available at:
- 17.U.S. Centers for Disease Control and Prevention website. Coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-nCoV/index.html Available at:
- 18.Coronavirus (COVID-19) Mortality Rate. https://www.worldometers.info/coronavirus/coronavirus-death-rate/ Available at:
- 19.Doshi S.S., Stauffer K.E., Fiebelkorn A.P., et al. The burden and severity of illness due to 2009 pandemic influenza A (H1N1) in a large US city during the late summer and early fall of 2009. Am J Epidemiol. 2012;176:519–526. doi: 10.1093/aje/kws137. [DOI] [PubMed] [Google Scholar]
- 20.Sugerman D., Nadeau K.H., Lafond K., et al. A survey of emergency department 2009 pandemic influenza A (H1N1) surge preparedness--Atlanta, Georgia, July-October 2009. Clin Infect Dis. 2011;52(suppl 1):S177–S182. doi: 10.1093/cid/ciq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schanzer D.L., Schwartz B. Impact of seasonal and pandemic influenza on emergency department visits, 2003-2010, Ontario, Canada. Acad Emerg Med. 2013;20:388–397. doi: 10.1111/acem.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin L.J., Dong H., Liu Q., Talbot J., Qiu W., Yasui Y. Predicting influenza-like illness-related emergency department visits by modelling spatio-temporal syndromic surveillance data. Epidemiol Infect. 2019;147:e312. doi: 10.1017/S0950268819001948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li C., Ren R.Q., Zhou L. A review on the preparedness plans on influenza pandemics, by WHO and China: the current status and development [in Chinese] Zhonghua Liu Xing Bing Xue Za Zhi. 2018;39:1032–1035. doi: 10.3760/cma.j.issn.0254-6450.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Filice C.E., Vaca F.E., Curry L., Platis S., Lurie N., Bogucki S. Pandemic planning and response in academic pediatric emergency departments during the 2009 H1N1 influenza pandemic. Acad Emerg Med. 2013;20:54–62. doi: 10.1111/acem.12061. [DOI] [PubMed] [Google Scholar]
- 25.Hall G.G., Perry A.G., VanDijk A., Moore K.M. Influenza assessment centres: a case study of pandemic preparedness to alleviate excess emergency department volume. CJEM. 2013;15:198–205. doi: 10.2310/8000.2012.120808. [DOI] [PubMed] [Google Scholar]