INTRODUCTION
Perioperative management of hip fractures is challenging because of multiple co-morbidities and poor physiological reserve in elderly patients. Pain is a major symptom and effective pain management utilising fascia iliaca compartment block (FICB) and femoral nerve (FN) block is popular among anaesthesiologists.[1] Recently, the pericapsular nerve group (PENG) block was described targeting the articular branches of FN, accessory obturator nerve (ON) and possibly ON in providing analgesia for hip fractures.[2] In our prospective cohort study, we wanted to evaluate the analgesic efficacy of PENG block in hip fracture patients for providing optimal sitting position for spinal anaesthesia (SA).
METHODS
After informed written consent, we selected a total of 20 consecutive patients for hip fracture surgery. The study was approved by the institutional ethics committee (HWH/Ethics Comm./Project/2018/27 dated November 15, 2018) and conducted between December 5, 2018, and February 15, 2019. All patients had visual analogue pain score (VAS) ≥5 (0-no pain, 10-worst imaginable pain) and received PENG block in pre-operative area. Patients with coagulopathy, allergy to planned drugs and those who refused SA were excluded from the study.
A curvilinear probe (2-5 MHz Vivid iq, GE Healthcare) was used, which was covered with Tegaderm to maintain sterility. Blocks were performed in supine position with adequate groin exposure. The probe was first placed at the anterior superior iliac spine in transverse plane, and then moved caudally to identify anterior inferior iliac spine (AIIS). The probe was then rotated to align the AIIS and iliopubic eminence (IPE) [Figure 1a]. This revealed the iliopsoas tendon and muscle together with femoral vessels superficially. A 21 G 100-mm echogenic needle (Ultraplex®360, B Braun Melsungen, Germany) was inserted in-plane from lateral to medial, and the tip was kept at the midpoint of AIIS and IPE deep to psoas tendon. After lifting of psoas tendon by hydrolocation, 20 ml of 0.25% bupivacaine with 4 mg dexamethasone was injected in 5 ml aliquots after negative aspiration [Figure 1b]. VAS at rest and passive movement (15° straight leg-raise) was measured 30 min following the block by another anaesthesiologist who was not performing the block. Subsequently, patients were taken to OT for SA. We measured the ease of sitting for the conduct of SA, which was performed by the same anaesthesiologist who measured the VAS in pre-operative area. This was graded as: 0-not satisfactory, 1-satisfactory, 2-good and 3-optimal. At 24 h following the block, we also asked the patients about their feedback on this block: 1-good, if necessary, will not hesitate for repeat block in future; 2-bad, will never opt for it.
Figure 1.
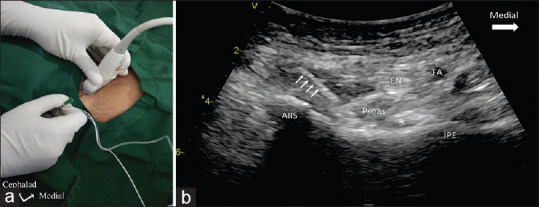
(a) Figure showing position of the hip, probe orientation and needle insertion. (b) Figure shows sonoanatomy of the block with needle (marked with white arrow) insertion from lateral to medial. Tip is below the psoas tendon (marked with asterix). FN- Femoral nerve, FA- Femoral artery, AIIS- Anterior inferior iliac spine, IPE- Iliopubic eminence
Continuous data were described as mean and standard deviation (SD) or median and interquartile range whichever appropriate. Discrete categorical data were presented as n(%). P < 0.05 was considered statistically significant.
RESULTS
The demographic data and VAS score at various points are shown in Table 1. Pre-block VAS pain score (expressed as mean ± SD) at rest and passive movement dropped from 7.45 ± 1.53 and 9.45 ± 0.75 to 1.1 ± 1.07 and 2.35 ± 1.34, respectively, 30 min following the block (P < 0.001). Thirty minutes following the block, 7 of 20 patients reported no pain (VAS 0) at rest, and remaining 13 patients reported mild pain (VAS ≤ 3). Furthermore, with passive movement of the hip, 80% of patients reported mild intensity of pain, whereas the rest 20% reported VAS of 4–5 (moderate intensity pain). The positioning of patients for SA was optimal, good and satisfactory in 75%, 15% and 10%, respectively. None of the positionings was considered unsatisfactory. Thirteen patients (65%) responded that they were happy with the block and would not hesitate to accept the same block in the future if the need arises. No side effects or complications were noted in any of the patients.
Table 1.
Demographic data and visual analogue scale pain score at various points
| Total number of patients | (n)---20 |
|---|---|
| Age (years): median (IQR) | 69.5 (65-76) |
| Gender (%) | |
| Female | 60 |
| Male | 40 |
| ASA physical status (n) | |
| II | 4 |
| III | 16 |
| Fracture type (%) | |
| NOF | 20 |
| IT | 10 |
| NOF with IT extension | 70 |
| Procedure type | |
| Hemiarthroplasty | 20 |
| Femur nailing | 80 |
| VAS score at various points | |
| Pre-procedure VAS at rest, mean±SD | 7.45±1.53 |
| Pre-procedure VAS at 15◦ passive SLR, mean±SD | 9.45±0.75 |
| Post-procedure VAS at rest (30 mins), mean±SD | 1.1±1.07 |
| Post-procedure VAS at 15° passive SLR (30 min), mean±SD | 2.35±1.34 |
| Ease of patient positioning for spinal (0-3), mean±SD | 2.65±0.67 |
NOF – Neck of Femur, IT – Intertrochanteric, VAS – Visual analogue score, SLR – Straight leg raise, SD – Standard deviation, ASA – American Society of Anesthesiologists
DISCUSSION
This prospective cohort study examined the analgesic efficacy of the PENG block in hip fractures and its effects on positioning for SA. PENG block provided excellent immediate (30 min after the block) analgesia both at rest and passive movement of the hip. Patients experienced a median drop of 6–7 points in VAS pain score 30 min following the block, both at rest and passive movements, which is similar to the initial description of PENG block.[2] We also evaluated the ease of positioning for SA following the block. The anaesthesiologist performing SA described the optimal and good sitting position in 75% and 15% of patients, respectively. In rest 10% of patients, support was needed for making them upright for the SA. Acharya et al. published a case series recently on PENG block and found that 9 of 10 patients did not need any support while making them upright for SA.[3]
Since the initial publication, the PENG block has created great interest among the regional anaesthesia community.[4,5,6,7] In addition to analgesic benefit, PENG block has been used in hip arthroscopy, hip dislocation and other indications.[8] Jadon et al. recently described landmark-based PENG block, which can further enhance its acceptability in places where anaesthesiologists have no access to ultrasound to perform this block. Jadon et al. also noticed the analgesic benefit and effect in making the patients sit comfortably for the conduct of SA.[8] What makes PENG block special from others is that it targets the articular branches innervating the anterior hip joint and does not lead to motor weakness if done properly.[2] Furthermore, the analgesic benefit is profound in terms of the median drop in pain score following the block.[2,9] Variable blockade of ON is known following FICB, which is not the case in PENG block, as shown in a recent dye study.[10,11] PENG block has its own disadvantages, including the deep nature of the block and difficulty in needle tip visualisation. The drug needs to be deposited deep to psoas tendon; otherwise, complications like quadriceps weakness may occur as reported in 2 cases.[12] In the first case, the block was done post-operatively and needle visualisation was challenging, whereas in the second case, needle tip was more medially placed, which could lead to diffusion of drug to block FN thus leading to quadriceps weakness.[12] Hence, it is advisable to perform the block in the pre-operative period as the sonoanatomy usually gets distorted following hip surgery post-operatively.
CONCLUSION
PENG block provides excellent analgesia in hip fractures and helps in upright positioning for the conduct of SA. PENG block can be an attractive and potential alternative option for regional anaesthesiologists in managing the elderly hip fracture patients. Randomised trials comparing PENG block with FICB with large sample size and a dose determining study could establish the efficacy of the PENG block.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors sincerely acknowledge the inputs provided by Dr Abhijit S Nair, Consultant Anesthesiologist, Basavatarakam Cancer Institute, Hyderabad in refining the manuscript and critical suggestions.
REFERENCES
- 1.Scurrah A, Shiner CT, Stevens JA, Faux SG. Regional nerve blockade for early analgesic management of elderly patients with hip fracture-a narrative review. Anaesthesia. 2018;73:769–83. doi: 10.1111/anae.14178. [DOI] [PubMed] [Google Scholar]
- 2.Girón-Arango L, Peng PW, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43:859–63. doi: 10.1097/AAP.0000000000000847. [DOI] [PubMed] [Google Scholar]
- 3.Acharya U, Lamsal R. Pericapsular nerve group block: An excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol. 2020;2020:1830136. doi: 10.1155/2020/1830136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ueshima H, Otake H. Clinical experiences of pericapsular nerve group (PENG) block for hip surgery. J Clin Anesth. 2018;51:60–1. doi: 10.1016/j.jclinane.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Ueshima H, Otake H. Pericapsular nerve group (PENG) block is effective for dislocation of the hip joint. J Clin Anesth. 2019;52:83. doi: 10.1016/j.jclinane.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Orozco S, Muñoz D, Jaramillo S, Herrera AM. Pericapsular nerve group (PENG) block for perioperative pain control in hip arthroscopy. J Clin Anesth. 2020;59:3–4. doi: 10.1016/j.jclinane.2019.04.037. [DOI] [PubMed] [Google Scholar]
- 7.Talawar P, Tandon S, Tripathy DK, Kaushal A. Combined pericapsular nerve group and lateral femoral cutaneous nerve blocks for surgical anaesthesia in hip arthroscopy. Indian J Anaesth. 2020;64:638–40. doi: 10.4103/ija.IJA_57_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jadon A, Sinha N, Chakraborty S, Singh B. Pericapsular nerve group (PENG) block: A feasibility study of landmark based technique. Indian J Anaesth. 2020;64:710–3. doi: 10.4103/ija.IJA_388_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guay J, Parker MJ, Griffiths R, Kopp S. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;5:CD001159. doi: 10.1002/14651858.CD001159.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Desmet M, Vermeylen K, Van Herreweghe I, Carlier L, Soetens F, Lambrecht S, et al. A Longitudinal Supra-Inguinal Fascia Iliaca Compartment Block Reduces Morphine Consumption After Total Hip Arthroplasty. Reg Anesth Pain Med. 2017;42:327–33. doi: 10.1097/AAP.0000000000000543. [DOI] [PubMed] [Google Scholar]
- 11.Tran J, Agur A, Peng P. Is pericapsular nerve group (PENG) block a true pericapsular block? Reg Anesth Pain Med. 2019 doi: 10.1136/rapm-2018-100278. rapm-2018-100278. doi: 10.1136/rapm-2018-100278. [DOI] [PubMed] [Google Scholar]
- 12.Yu HC, Moser JJ, Chu AY, Montgomery SH, Brown N, Endersby RV. Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg Anesth Pain Med. 2019;44:611–3. doi: 10.1136/rapm-2018-100354. [DOI] [PubMed] [Google Scholar]


