Abstract
Emergence of the COVID-19 crisis has catalyzed rapid paradigm shifts throughout medicine. Even after the initial wave of the virus subsides, a wholesale return to the prior status quo is not prudent. As a specialty that values the proper application of new technology, radiation oncology should strive to be at the forefront of harnessing telehealth as an important tool to further optimize patient care. We remain cognizant that telehealth cannot and should not be a comprehensive replacement for in-person patient visits because it is not a one for one replacement, dependent on the intention of the visit and patient preference. However, we envision the opportunity for the virtual patient “room” where multidisciplinary care may take place from every specialty. How we adapt is not an inevitability, but instead, an opportunity to shape the ideal image of our new normal through the choices that we make. We have made great strides toward genuine multidisciplinary patient-centered care, but the continued use of telehealth and virtual visits can bring us closer to optimally arranging the spokes of the provider team members around the central hub of the patient as we progress down the road through treatment.
Keywords: COVID-19, telehealth, multidisciplinary care, patient-centered care, healthcare access
The emergence of the COVID-19 crisis has catalyzed rapid paradigm shifts throughout medicine. However, various factors and unknowns prevent accurate predictions of how many of these changes are merely temporary versus how many will be a part of the “new normal.” Even after the initial wave of the virus subsides, a wholesale return to the prior status quo is not prudent. As a specialty that values the proper application of new technology, radiation oncology should strive to be at the forefront of harnessing telehealth as an important tool to further optimize patient care. We remain cognizant that telehealth cannot and should not be a comprehensive replacement for in-person patient visits because it is not a one for one replacement, dependent on the intention of the visit and patient preference. However, we envision the opportunity for the virtual patient “room” where multidisciplinary care may take place from every specialty.
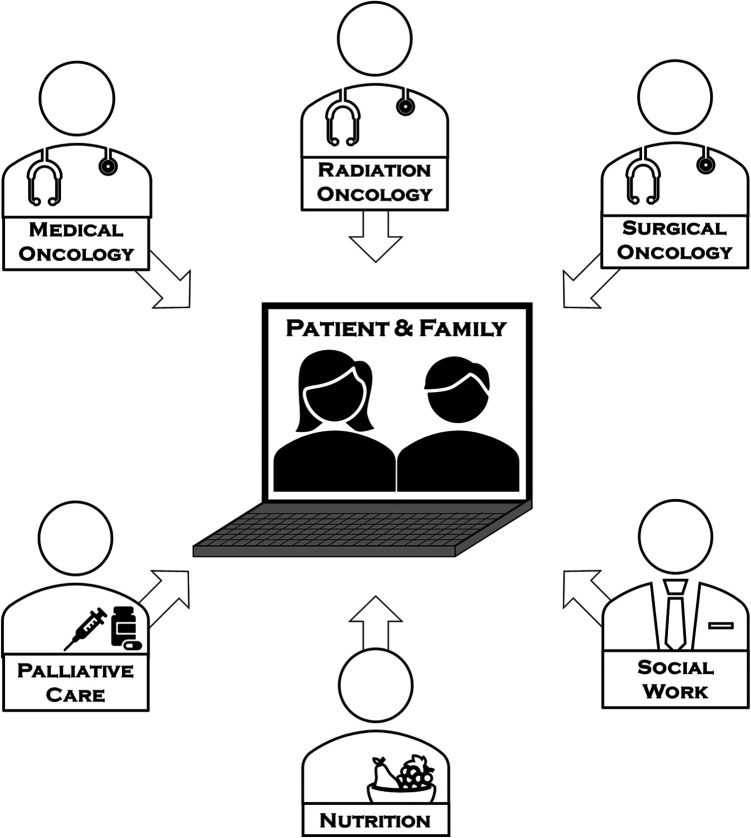
Team-based care through tumor boards and multidisciplinary clinics have become a pillar of oncologic management.1 Many of these clinics may not be optimally co-located, either spatially or temporally. In the past, when patients shared their anxieties and absorbed profoundly impactful clinical information, they were in a foreign environment of the outpatient clinic. However, with the rapid adoption of videoconferencing for telehealth visits, we are typically seeing patients in their own environments, whether at home or elsewhere, and with caregivers, family, and friends. The vast majority of videoconferencing software in routine clinical use allows for easy access of multiple professionals to conference into a single call at one time. This allows for a real-time meeting of multiple subspecialists. Allowing for providers to enter the patient’s space together and present the ideal consolidated recommendation provides a true idealization of the virtual patient room as the patient’s space (Figure 1). Truly in the service of the patient, this would provide a single nexus where providers come to the patient, rather than the other way around.
Figure 1.
Representation of a patient-centered digital space to which multidisciplinary providers come.
In fact, looking outside of the institutional team, incorporating the patient’s primary care physician and other members of the patient’s care team would also facilitate real-time communication without the need to rely only on treatment summaries and avoid associated logistical challenges. Even if a real-time visit is not possible, using videoconferencing software to record a short summary of the discussion, potentially highlighting pertinent imaging and laboratory findings for review, would be timelier and more comprehensive than notes received weeks after. As billing evolves, this may even present the opportunity for a single note, signed by multiple physicians, that is a consensus recommendation—decreasing the redundancy of multiple notes.
Telehealth visits have also been useful outside of an initial visit. When seeing add-on patients at our center, we frequently run into space limitations and patients needing to navigate to another, potentially unfamiliar clinic. Now, we can go to them without the need to scramble for an empty clinic room. For other visits, many patients at our center come from across the state, driving several hours and waiting several more hours to see a provider for a 30-minute appointment to go over a scan or labwork. This is particularly problematic in the multi-disciplinary environment where coordinating visits with multiple specialists is complex and may require repeat trips to the clinic for the patient. Instead, having providers go to the patient in their virtual space creates value for the patient by reducing transportation costs, opportunity costs of time and missing work, the ability of other, out of state family or friends to attend, and further increases patient choice. This also could save transit time for providers who are shuttling between different locations. For example, after stereotactic body radiation therapy to a lung lesion, or to the pancreas, surveillance imaging and labwork could easily be reviewed virtually, with many software programs allowing for screen sharing to review images. Many of these programs provide HIPAA compliance.2 In an era when PSA testing may be widely obtained, and digital exams not always necessary3 virtual prostate cancer follow-up visits are especially well-received. Some existing models have been successfully implemented paralleling traditional in-person workflows,4 which can easily be transposed on the oncology care model. Sirintrapun and Lopez.5 point to a number of successful pilot models which should be expanded and be more widely adopted. Various national and international organizations have also endorsed the rapid adoption of telehealth as a tool to maintain high standards of care with the competing risk of the current pandemic. The American Society of Clinical Oncology endorsed triaging visits appropriate for transition to the virtual space to create an integrated clinical model and expand service capacities through surges.6 The International Society of Geriatric Oncology has adopted similar guidelines to use telehealth to reduce exposure and maintain coordinated continuity of care.7
Despite all of the benefits of virtual visits, it is not a panacea to replace the in-person patient visit. Effectively using telehealth requires a delicate balance between depersonalization and commoditization versus expediency and ease, best achieved by keeping the interest of the patient as the central focus. Additionally, these visits are not replacements for the physical exam. “Laying of the hands” is a critical portion of establishing patient rapport and creating a bond of trust and empathy. This rapport may be more difficult to establish virtually at initial visits and more difficult to maintain through breaking bad news, such as a transition to hospice, and other emotional conversations without the potential comfort of physical presence.8 However, these deficits may be counterbalanced for the patient by being in a more familiar environment and easily joined by caregivers. The inability to perform a full physical exam raises the specter of increased medicolegal liability if major decisions are made without an in-person visit, requiring increased caution. Another challenge to relying solely on virtual visits is on the patient side: it assumes easy, on-demand access to high speed internet, audio/visual capabilities, and facility with technology that may not necessarily be available. Based on recent census data, more than 30% of US households headed by a person age 65 or older lack a desktop or laptop computer and more than half lack smartphones.9 Despite the reduction in rural access disparities though the proliferation of digital and mobile health,10 these infrastructure and digital literacy limitations are magnified even further outside of the United States in low- and middle-income countries, precluding uniform adoption of robust telehealth capabilities. If we expect virtual visits to become a staple in the continuum of oncologic care, we must ensure accessibility to both hardware and broadband through partnerships with both governmental and non-governmental organizations.11 This could potentially be mitigated by providing patients with the necessary technology.12
Although telehealth platforms are typically subject to stringent security and monitoring requirements to ensure privacy and prevention of data breaches under federal law, increased adoption may lead to increased opportunities for data breaches compromising patient privacy. In the current acute phase of the pandemic, these concerns are magnified by the temporary suspension of HIPAA-compliant platform requirements, requiring additional caution.13
Aside from the psychological implications, there are certain logistic hurdles related to standard approaches to care in radiation oncology. Many disease sites do not lend themselves as effectively to virtual visits. For examples, a flexible nasolaryngoscopic examination is a key prerequisite for head and neck cancers that is not substitutable with a virtual visit. On the other hand, for some gastrointestinal sub-sites and some thoracic malignancies, a physical exam potentially could be deferred to time of simulation for radiation treatment planning.
Although the technological capability of telehealth has been available, multiple barriers previously prevented widespread adoption. High fixed costs for secure technological infrastructure paired with minimal reimbursement for a restricted range of services have consistently been touted as the 2 highest barriers.14 Outside of reimbursement from Medicare, other payors are regulated at the state level.15 Coupled with a lack of interstate provider licensure, different rules on allowed providers, approved settings, technology requirements created a disparate patchwork of statutes and regulations. In the midst of this pandemic, the Centers for Medicare and Medicaid services have temporarily expanded coverage and payment for telehealth services under an 1135 waiver, including pay parity with in-person visits, relaxation of originating site requirements, and practice across state lines.13 Given the extensive regulatory framework, maintaining the current wholesale adoption of telehealth services seems unlikely to survive the acute phase of the pandemic. The retention of pay parity and increases in reimbursements in general for telehealth is critical for preserving its continued use.16
This crisis has pushed us to adopt and harness new technology out of necessity. As the initial phases of the pandemic subside, we should strive to preserve the best aspects of telehealth and apply it as a tool in the appropriate setting based on the patient’s needs. How we adapt is not an inevitability, but instead, an opportunity to shape the ideal image of our new normal through the choices that we make. We believe creating the virtual patient room will optimize multidisciplinary care by truly keeping the patient in the center of the care team. We have made great strides toward genuine multidisciplinary patient-centered care, but the continued use of telehealth and virtual visits can bring us closer to optimally arranging the spokes of the provider team members around the central hub of the patient as we progress down the road through treatment. The opportunity to enter the patient’s room as a multidisciplinary team provides new opportunity for improved care.
Footnotes
Authors’ Note: Our study did not require an ethical board approval because it did not contain human or animal trials.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Sarah E. Hoffe: Dr. Hoffe reports being a member of the editorial board for Cancer Control. Peter A. S. Johnstone: Dr. Johnstone reports other (Honorarium) from Huron Consulting, outside the submitted work. Louis B. Harrison: Dr. Harrison reports being a principal investigator on a research project with ViewRay, Inc, outside the submitted work. Stephen A. Rosenberg: Dr. Rosenberg reports personal fees from Novocure, outside the submitted work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Austin J. Sim, MD, JD  https://orcid.org/0000-0001-5523-4347
https://orcid.org/0000-0001-5523-4347
References
- 1. Kagan AR. The multidisciplinary clinic. Int J Radiat Oncol Biol Phys. 2005;61(4):967–968. [DOI] [PubMed] [Google Scholar]
- 2. Earon SA. Video in Healthcare Communications. Zoom; Accessed May 18, 2020 https://zoom.us/whitepaper?case=healthcare&zcid=1231 [Google Scholar]
- 3. Johnstone PA, McFarland JT, Riffenburgh RH, Amling CL. Efficacy of digital rectal examination after radiotherapy for prostate cancer. J Urol. 2001;166(5):1684–1687. [PubMed] [Google Scholar]
- 4. Feil F, Koenig K. A new multidisciplinary virtual care model at UT Health Austin. UT Health Austin Blog [Internet]. June 17, 2020. Accessed August 25, 2020 https://uthealthaustin.org/blog/new-multidisciplinary-virtual-care-model
- 5. Sirintrapun SJ, Lopez AM. Telemedicine in cancer care. Am Soc Clin Oncol Educ Book. 2018(38):540–545. [DOI] [PubMed] [Google Scholar]
- 6. American Society of Clinical Oncology. ASCO Special Report: A Guide to Cancer Care Delivery During the COVID-19 Pandemic. ASCO; May 19, 2020. Accessed August 25, 2020 https://www.asco.org/sites/new-www.asco.org/files/content-files/2020-ASCO-Guide-Cancer-COVID19.pdf [Google Scholar]
- 7. Battisti NML, Mislang AR, Cooper L, et al. Adapting care for older cancer patients during the COVID-19 pandemic: recommendations from the International Society of Geriatric Oncology (SIOG) COVID-19 Working Group [published online July 16, 2020]. J Geriatr Oncol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Holstead RG, Robinson AG. Discussing serious news remotely: navigating difficult conversations during a pandemic [published online May 18, 2020]. JCO Oncol Pract. 2020. doi: 10.1200/OP.20.00269. [DOI] [PubMed] [Google Scholar]
- 9. Velasquez D, Mehotra A. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. Health Affairs Blog. May 8, 2020. Accessed May 18, 2020 https://www.healthaffairs.org/do/10.1377/hblog20200505.591306/full/
- 10. Gonzalez BD. Promise of mobile health technology to reduce disparities in patients with cancer and survivors. JCO Clin Cancer Inform. 2018;2:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Källander K, Tibenderana JK, Akpogheneta OJ, et al. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: a review. J Med Internet Res. 2013;15(1):e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. [DOI] [PubMed] [Google Scholar]
- 13. Centers for Medicare & Medicaid Services. Medicare telemedicine health care provider fact sheet. CMS Newsroom. March 17, 2020. Accessed May 18, 2020 https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 14. Thomas L, Capistrant G. State telemedicine gaps analysis coverage & reimbursement. mTelehealth [Internet]. January 19, 2016. Accessed May 18, 2020 https://mtelehealth.com/state-telemedicine-gaps-analysis-coverage-reimbursement/
- 15. Lackman NM, Acosta JN, Levine SJ. 50-State Survey of Telehealth Commercial Payer States. Foley.com [Internet]. December 2019. Accessed May 18, 2020 https://www.foley.com/-/media/files/insights/health-care-law-today/19mc21486-50state-survey-of-telehealth-commercial.pdf
- 16. Huckman RS. What will U.S. health care look like after the pandemic? Harvard Business Review [Internet]. April 07, 2020. Accessed May 05, 2020 https://hbr.org/2020/04/what-will-u-s-health-care-look-like-after-the-pandemic