Abstract
Background
Helminthic infections, in particular those caused by gastrointestinal nematodes (GIN), are found worldwide and are among the most economically important diseases of goats. Anthelmintic resistance (AR) in GIN of goats is currently present worldwide, and single- or multidrug resistant species are widespread. The aim of this study was to determine the prevalence of AR to benzimidazoles (BZ), macrocyclic lactones (ML) and imidazothiazoles represented by levamisole (LEV) in the Polish goat herds by using an in vitro larval development test, which is useful especially in large-scale epidemiological surveys.
Results
This cross-sectional study was conducted from September 2018 to June 2019 and enrolled 42 dairy goat herds scattered over the entire country. The most commonly used anthelmintic class in goat herds in Poland were BZ (92%), followed by ML (85%) and LEV (13%). BZ-resistant GIN populations were found in 37 herds (88%, CI 95%: 75 to 95%), ML-resistant GIN populations in 40 herds (95%, CI 95, 84 to 99%), and LEV-resistant GIN populations in 5 herds (12%, CI 95%: 5 to 25%). Multidrug resistance involving all three anthelmintic classes was found in 5 herds (12%, CI 95, 5 to 25%). Based on the morphological features of stage 3 larvae the main resistant GIN turned out to be Haemonchus contortus and Trichostrongylus spp. The use of BZ and frequency of anthelmintic treatments were significantly related to the presence of AR to BZ in Polish goat herds.
Conclusions
This cross-sectional study demonstrates the existence of AR to BZ, ML and LEV on Polish goat farms. Resistance to BZ and ML is widespread, while AR to LEV is currently at a low level. A considerable proportion of herds harbours multidrug resistant GIN, which requires further consideration. An effective anthelmintic treatment strategy, reasonable preventive measures and better understanding of the resistance-related management practices by farmers and veterinarians may delay further development of AR.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12917-020-02721-9.
Keywords: Anthelmintic resistance; Gastrointestinal nematodes; Larval development test; Goats, benzimidazoles; Macrocyclic lactones; Levamisole
Background
Parasitic infections, especially those caused by gastrointestinal nematodes (GIN), are one of the main factors responsible for economic losses in goat farming around the world [1]. Their control is mainly based on the use of three chemical classes of anthelmintics: benzimidazoles (BZ), macrocyclic lactones (ML), and imidazothiazoles including levamisole (LEV). The widespread and uncontrolled use of anthelmintics has resulted in the emergence of anthelmintic resistance (AR). In some countries the proportion of resistant GIN strains is currently so high that precludes effective control of parasitic diseases [2].
Several factors are responsible for the development of AR in parasites, of which most important are a high treatment frequency [3], underdosing of the anthelmintics, and continuous use of the same anthelmintic class over several years [4]. These factors, together with certain types of farm management, can promote the development of AR, especially in goats which need higher doses to ensure anthelmintic efficacy since they metabolise and eliminate various medicines quicker than sheep and cattle [5, 6].
Several in vivo and in vitro tests have been developed for detection of AR. An in vivo fecal egg count reduction test (FECRT) is recommended by the World Association for the Advancement of Veterinary Parasitology (WAAVP). However, this test requires animals in a herd to be either tested twice which makes it expensive, time-consuming and laborious, or a randomly selected group of animals in a herd be left untreated which, in turn, is impractical and hardly acceptable to farmers. Moreover, high inter-animal variation in the pharmacokinetics of anthelmintics in goats may lower the quality of FECRT results [5, 6]. The use of some in vitro methods like egg hatch test (EHT) or molecular tests (RT-PCR or pyrosequencing) is currently limited to BZ [7]. Moreover, EHT can be performed only on fresh fecal samples containing only eggs in early stage of development, while molecular tests are expensive and require specialized equipment in the laboratory, which makes them unsuited for routine AR diagnostics. Therefore, the most efficient in vitro test is the larval development test (LDT) which currently exists in several modifications allowing detection of AR to all three anthelmintic classes [7–10]. The LDT offers an alternative to the laborious in vivo FECRT and allows investigation of AR to all anthelmintic classes in a single test regardless of the herd size [11]. Moreover, the LDT is the only in vitro AR diagnostic test that has been commercialized and registered on the market as DrenchRite® [12].
Thus far, a number of reports have been published on the occurrence of AR in goat herds in Europe, and the prevalence of AR especially to BZ appears to be very high in some European countries (Rose et al. 2015). In France studies have shown a prevalence of AR to BZ to vary between 70 to 100% [13, 14]. Very close are results of a recent Slovakian study [15]. Many studies have demonstrated the existence of AR to the main anthelmintic classes in goat herds outside of Europe, namely in the United States [11, 16], Cuba [17], Kenya [18], South Africa [19], Uganda [20], Ethiopia [21], Malaysia [22, 23], India [24–26], and Pakistan [27].
Data on the AR situation in Polish small ruminant population are only fragmentary. In the last two decades, sporadic cases of AR to BZ in sheep, cattle, horses, pigs and goats have been reported [28–31]. Recently, first cases of AR to ML and LEV, as well as multidrug resistance (MDR) in goat herds have been described [32, 33].
On the other hand, our long cooperation with a number of Polish goat farmers has shown not only that GIN infections constitute a considerable clinical problem but also that the factors predisposing to the development of AR are present in the vast majority of goat herds. Therefore, we hypothesized that those cases of AR reported so far were only the tip of the iceberg, and we decided to carry out a large-scale epidemiological observational study to determine the prevalence of AR to the three basic anthelmintic classes in Polish goat herds and identify the genus or species of resistant larvae.
Results
Goat herd characteristics
Forty-two dairy goat herds were enrolled in this cross-sectional study (49% of 85 herds invited). They were evenly scattered over the entire country (located in 13 of 16 provinces of Poland). They counted from 4 to 155 adult goats with the median (IQR) of 15 (10 to 23) goats. Only 5 herds (12%) consisted of more than 50 adult goats and only 2 of them counted more than 100 heads. In most of them two Polish local breeds, Polish White Improved and Polish Fawn Improved, were kept. Nine herds (21%) kept only Anglo-Nubian goats and three herds (7%) kept a traditional local goat breed – Carpathian. In the vast majority of herds (39 of 42; 93%) goats were grazed from April to October. In 10 herds (24%) goats were grazed together on the same pasture with sheep and in 8 herds (19%) with cattle. Only 13 herds (31%) relied solely on their own replacement, the remaining 29 herds (69%) purchased goats from other herds.
Only 3 herds (7%) did not practice routine deworming. In the remaining 39 herds (93%) at least one anthelmintic was routinely used. Most of the herds which practiced routine deworming (n = 26; 67%) dewormed twice a year, 7 herds (18%) once a year, and 6 herds (15%) three or four times a year. BZ (albendazole and fenbendazole) were used in 36 herds (92% of herds practicing routine deworming), ML (eprinomectin, rarely ivermectin) in 33 herds (85%) and LEV in only 5 herds (13%).
Prevalence of anthelmintic resistance
AR to each of the anthelmintic classes was detected using LDT in Polish goat herds. The most prevalent was AR to ML detected in 40 herds (95%, CI 95%: 84 to 99%) and to BZ detected in 37 herds (88%, CI 95%: 75 to 95%). AR to LEV was detected in 5 herds (12%, CI 95%: 5 to 25%) (Table 1).
Table 1.
Results of the larval development test (LDT) in 42 Polish goat herds
| Herd No. | No. of adult goats | Benzimidazoles | Macrocyclic lactones | Levamisole | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PDc (%) | cPD at the DC of 0.08 μg/ml (%) with CI 95% | EC50 (μg/ml) | EC99 (μg/ml) | AR | PDc (%) | cPD at the DC of 21.6 ng/ml (%) with CI 95% | EC50 (ng/ml) | EC99 (ng/ml) | AR | PDc (%) | cPD at the DC of 2.0 μg/ml (%) with CI 95% | EC50 (μg/ml) | EC99 (μg/ml) | AR | ||
| 1 | 10 | 98.0 | 0 | 0.009 | 0.011 | ND | 98.0 | 70.0 (61.2–77.6) | 36.6 | 546.2 | severe | 98.0 | 0 | 0.41 | 1.88 | ND |
| 2 | 14 | 98.0 | 99.0 (96.4–99.7) | 0.273 | 0.793 | severe | 97.4 | 97.7 (94.1–99.1) | 134.3 | 2374 | severe | 100 | 9.1 (4.6–17.3) | 0.50 | 3.12 | mild |
| 3 | 16 | 95.0 | 42.1 (34.5–50.1) | 0.082 | 1.054 | moderate | 95.0 | 41.0 (33.0–49.6) | 20.1 | 924.5 | moderate | 95.0 | 0 | 0.55 | 2.04 | ND |
| 4 | 26 | 98.4 | 77.5 (71.4–82.6) | 0.301 | 5.323 | severe | 98.4 | 70.1 (62.3–76.9) | 49.4 | 4891 | severe | 93.2 | 0 | 0.37 | 1.7 | ND |
| 5 | 5 | 97.8 | 31.7 (25.6–38.4) | 0.030 | 2.990 | moderate | 97.8 | 59.3 (52.4–65.9) | 33.1 | 1524 | severe | 97.8 | 1.0 (0.3–3.6) | 0.45 | 1.13 | ND |
| 6 | 8 | 98.4 | 53.9 (46.9–60.6) | 0.091 | 1.354 | severe | 98.4 | 100 (98.0–100) | 109.9 | 1094 | severe | 98.4 | 3.6 (1.7–7.1) | 0.45 | 2.82 | mild |
| 7 | 4 | 100 | 81 (73.7–86.6) | 0.165 | 1.645 | severe | 100.0 | 93.3 (87.7–96.4) | 148.4 | 6831 | severe | 100 | 0 | 0.03 | 0.06 | ND |
| 8 | 35 | 98.8 | 97.2 (90.6–99.2) | 0.333 | 0.924 | severe | 98.8 | 83.0 (76.2–88.1) | 81.5 | 2169 | severe | 98.8 | 0 | 0.22 | 0.48 | ND |
| 9 | 40 | 98.6 | 2.2 (0.7–7) | 0.007 | 0.042 | ND | 98.6 | 53.7 (40.3–66.7) | 12.2 | 560.7 | severe | 98.6 | 0 | 0.27 | 0.59 | ND |
| 10 | 7 | 98.7 | 14.0 (9.5–20.3) | 0.014 | 0.135 | moderate | 98.7 | 45.3 (38.4–52.4) | 27.1 | 722.1 | moderate | 98.7 | 34.8 (24.3–47.0) | 0.74 | 231.3 | moderate |
| 11 | 23 | 97.3 | 91.0 (85.2–94.7) | 0.223 | 0.829 | severe | 97.3 | 72.3 (65.1–78.5) | 121.5 | 257,438 | severe | 97.3 | 54.4 (40.9–67.3) | 2.72 | 269.1 | severe |
| 12 | 155 | 98.2 | 7.3 (3.4–14.9) | 0.030 | 0.300 | mild | 98.2 | 85.0 (78.6–89.7) | 33.1 | 329.5 | severe | 98.2 | 0 | 0.30 | 0.95 | ND |
| 13 | 123 | 98.6 | 85.0 (78.4–89.8) | 0.223 | 1.032 | severe | 98.6 | 82.8 (76.7–87.5) | 99.5 | 4579 | severe | 98.6 | 0 | 0.45 | 1.13 | ND |
| 14 | 13 | 93.2 | 31.8 (25.1–39.3) | 0.050 | 4.929 | moderate | 93.2 | 61.3 (54.1–68.1) | 33.1 | 3278 | severe | 92.9 | 0 | 0.06 | 0.38 | ND |
| 15 | 11 | 95.0 | 84.9 (78.7–89.5) | 0.247 | 1.991 | severe | 95.0 | 97.1 (93.5–98.7) | 134.3 | 1725 | severe | 95 | 0 | 0.45 | 1.89 | ND |
| 16 | 17 | 86.8 | 27.9 (20.6–36.5) | 0.050 | 1.065 | moderate | 86.8 | 52.4 (43.9–60.8) | 24.5 | 7661 | severe | 86.8 | 0 | 0.22 | 1.80 | ND |
| 17 | 13 | 86.8 | 10.7 (7.1–15.8) | 0.018 | 0.392 | moderate | 86.8 | 52.1 (44.9–59.3) | 27.1 | 1248 | severe | 86.8 | 0 | 0.15 | 1.49 | ND |
| 18 | 10 | 97.9 | 56.3 (47.7–64.6) | 0.081 | 3.778 | severe | 97.9 | 77.2 (69.7–83.3) | 73.7 | 1577 | severe | 97.9 | 0 | 0.18 | 0.85 | ND |
| 19 | 20 | 98.7 | 0 | 0.003 | 0.008 | ND | 98.7 | 65.3 (55.0–74.3) | 30.0 | 2966 | severe | 98.7 | 0 | 0.08 | 0.31 | ND |
| 20 | 5 | 96.2 | 92.2 (86.3–95.7) | 0.183 | 0.679 | severe | 96.2 | 79.5 (72.3–85.2) | 73.7 | 3392 | severe | 96.2 | 4.8 (2.3–9.8) | 0.30 | 6.45 | mild |
| 21 | 21 | 100 | 6.3 (3.2–11.9) | 0.014 | 0.290 | mild | 100 | 80.9 (72.3–87.3) | 66.7 | 11,000 | severe | 100 | 0 | 0.14 | 0.63 | ND |
| 22 | 72 | 92.4 | 0 | 0.003 | 0.014 | ND | 92.4 | 20.0 (14.8–26.4) | 9.0 | 240.4 | moderate | 92.4 | 0 | 0.10 | 0.63 | ND |
| 23 | 11 | 91.6 | 15.3 (11.0–20.9) | 0.025 | 0.529 | moderate | 91.6 | 37.7 (31.2–44.6) | 11.0 | 1091 | moderate | 91.6 | 1.1 (0.3–3.7) | 0.09 | 1.17 | ND |
| 24 | 14 | 97.0 | 84.5 (78.9–88.9) | 0.607 | 189.4 | severe | 97.0 | 63.9 (57.1–70.3) | 54.6 | 5405 | severe | 97.0 | 0 | 0.18 | 1.15 | ND |
| 25 | 26 | 94.0 | 18.6 (13.8–24.6) | 0.022 | 2.215 | moderate | 94.0 | 18.6 (13.8–24.6) | 4.5 | 1400 | moderate | 94.0 | 0 | 0.10 | 0.37 | ND |
| 26 | 10 | 94.0 | 42.6 (35.9–49.5) | 0.074 | 3.419 | moderate | 94.0 | 50.5 (43.7–57.4) | 24.5 | 244.1 | severe | 94.0 | 0 | 0.13 | 0.48 | ND |
| 27 | 8 | 90.8 | 22.0 (16.8–28.3) | 0.015 | 4.683 | moderate | 90.8 | 0 | 1.6 | 16.4 | ND | 90.8 | 0 | 0.09 | 0.42 | ND |
| 28 | 16 | 96.8 | 94.5 (90.5–96.9) | 0.905 | 9.003 | severe | 96.8 | 52.2 (45.3–59) | 22.2 | 285.1 | severe | 96.8 | 0 | 0.18 | 0.58 | ND |
| 29 | 10 | 93.2 | 91.2 (86.5–94.4) | 0.741 | 7.371 | severe | 93.2 | 92.8 (88.4–95.6) | 54.6 | 252.6 | severe | 93.2 | 0 | 0.25 | 0.62 | ND |
| 30 | 16 | 92.2 | 32.0 (25.9–38.7) | 0.041 | 0.872 | moderate | 92.2 | 94.9 (90.9–97.2) | 49.4 | 183.6 | severe | 92.6 | 0 | 0.20 | 0.51 | ND |
| 31 | 20 | 94.8 | 95.5 (91.6–97.6) | 0.497 | 6.378 | severe | 94.8 | 96 (92.3–98) | 90.0 | 283.9 | severe | 94.8 | 0 | 0.22 | 0.70 | ND |
| 32 | 9 | 98.8 | 31.8 (24.8–39.8) | 0.061 | 0.605 | moderate | 98.8 | 93.4 (87.5–96.7) | 73.7 | 463.1 | severe | 98.8 | 0 | 0.45 | 1.42 | ND |
| 33 | 76 | 97.9 | 0 | 0.001 | 0.001 | ND | 97.9 | 0 | 0.1 | 13.4 | ND | 97.9 | 0 | 0.06 | 0.38 | ND |
| 34 | 13 | 98.9 | 91.4 (86.0–94.8) | 0.497 | 155.1 | severe | 98.9 | 67.1 (59.8–73.7) | 54.6 | 5405 | severe | 98.9 | 0 | 0.18 | 0.74 | ND |
| 35 | 10 | 97.8 | 92.6 (86.0–96.2) | 0.368 | 7.873 | severe | 97.8 | 96.3 (91–98.5) | 73.7 | 595.1 | severe | 97.8 | 0 | 0.27 | 0.72 | ND |
| 36 | 27 | 90.6 | 81.7 (75.7–86.4) | 0.368 | 9.798 | severe | 90.6 | 79.4 (72.4–85) | 44.7 | 956.6 | severe | 90.6 | 0 | 0.20 | 0.93 | ND |
| 37 | 5 | 96.8 | 51.5 (44.4–58.5) | 0.082 | 13.54 | severe | 96.8 | 5.3 (2.5–11.0) | 3.7 | 47.1 | mild | 96.8 | 0 | 0.20 | 0.64 | ND |
| 38 | 6 | 97.0 | 90.7 (84.1–94.8) | 1.649 | 974.7 | severe | 97.0 | 83.5 (75.6–89.2) | 54.6 | 543.2 | severe | 97.0 | 0 | 0.27 | 0.86 | ND |
| 39 | 73 | 97.2 | 88.0 (81.0–92.6) | 0.301 | 5.232 | severe | 97.2 | 92.0 (85.9–95.6) | 109.9 | 2353 | severe | 97.2 | 0.9 (0.2–4.5) | 0.47 | 2.19 | ND |
| 40 | 22 | 88.9 | 57.9 (50.6–64.9) | 0.135 | 13.40 | severe | 88.9 | 7.9 (4.8–12.7) | 9.0 | 56.7 | mild | 88.9 | 0 | 0.17 | 0.41 | ND |
| 41 | 21 | 98.8 | 63.4 (54.8–71.2) | 0.165 | 16.37 | severe | 98.8 | 94.9 (90.4–97.4) | 121.5 | 562.1 | severe | 98.8 | 0 | 0.18 | 0.39 | ND |
| 42 | 18 | 93.2 | 63.3 (53.5–72.1) | 0.150 | 3.201 | severe | 93.2 | 29.0 (21.0–38.5) | 12.2 | 260.7 | moderate | 93.2 | 0 | 0.33 | 1.05 | ND |
AR anthelmintic resistance, DC discriminating concentration, PDc percentage of developing larvae in the control wells, cPD at the DC corrected percentage of larvae developing in tested wells at the discriminating concentration of a given anthelmintic agent, CI 95 95% confidence interval, EC50 median effective concentration, EC99 the 99th percentile effective concentration, ND not detected
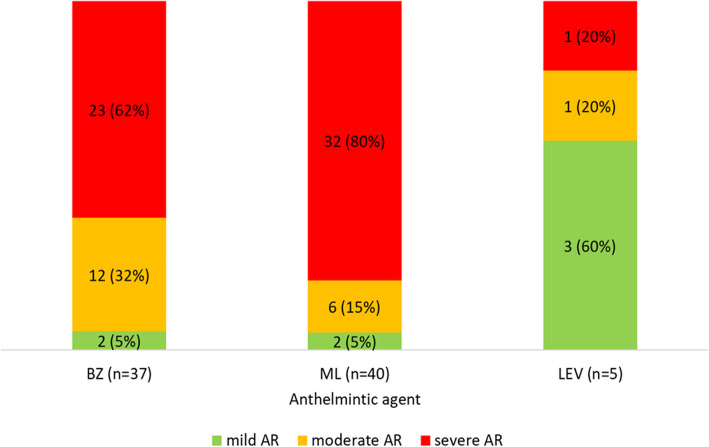
Only one herd was free from AR to any of anthelmintics. AR to one anthelmintic was found in 5 herds (AR to ML in 4 herds, and to BZ in one herd), AR to two anthelmintics in 31 herds (BZ and ML in all) and AR to all three anthelmintics (synonymous to MDR) in 5 herds, which yielded the prevalence of MDR to be 12% (CI 95%: 5 to 25%). In most of herds AR to BZ and ML was severe (> 50% of larvae developed at the discriminating concentration, DC), while AR to LEV was mostly mild (< 10% of larvae developed at the DC) (Fig. 1).
Fig. 1.
The number (percentage) of herds harbouring resistant GIN populations of various severity of anthelmintic resistance (AR) to benzimidazoles (BZ), macrocyclic lactones (ML) and levamisole (LEV) in Polish goat population classed as mild (< 10% of larvae developed at the discriminating concentration), moderate (10–50% of larvae developed), and severe (> 50% of larvae developed)
Corrected percentage of larvae developing in tested wells (cPD) at the DC was significantly positively correlated with EC50 for all three anthelmintic classes and this correlation was high for BZ (Rs = 0.94, p < 0.001) and ML (Rs = 0.90, p < 0.001), and moderate for LEV (Rs = 0.48, p = 0.001) (Fig. S1). EC50 and EC99 for susceptible and resistant GIN populations are summarized in Table 2.
Table 2.
Effective concentrations of anthelmintics inhibiting 50% (EC50) and 99% (EC99) of larvae in gastrointestinal nematode (GIN) populations from herds classified as susceptible and resistant, presented as the median, interquartile range (IQR), and range in parenthesis
| GIN population | No. of herds | EC50 | EC99 |
|---|---|---|---|
| Benzimidazoles – discriminating concentration (DC) = 0.08 μg/ml | |||
| susceptible | 5 | 0.003, 0.003–0.007 (0.001–0.009) | 0.011, 0.008–0.014 (0.001–0.042) |
| resistant | 37 | 0.150, 0.050–0.301 (0.014–1.649) | 2.990, 0.872–7.371 (0.135–974.682) |
| Macrocyclic lactones – DC = 21.6 ng/ml | |||
| susceptible | 2 | 0.892 (0.135–1.649) | 14.902 (13.398–16.400) |
| resistant | 40 | 49.402, 24.533–77.576 (3.669–148.413) | 1092.628, 396.322–3122.438 (47.127–257,437.7) |
| Levamisole – DC = 2.0 μg/ml | |||
| susceptible | 37 | 0.202, 0.135–0.301 (0.025–0.549) | 0.724, 0.480–1.148 (0.062–2.185a) |
| resistant | 5 | 0.497, 0.449–0.741 (0.301–2.718) | 6.446, 3.121–231.343 (2.824–269.110) |
a GIN populations from two herds (no. 5 and 23 in Table 1) were classified as susceptible despite ED99 > 2 μg/ml because the corrected percentage larval development at the DC was ≤1%
cPD at the DC in BZ-resistant populations ranged from 6 to 99% with the median (IQR) of 63% (32 to 91%), and was not significantly different from cPD at the DC in ML-resistant populations which ranged from 5 to 100% with the median (IQR) of 71% (52 to 92%) (p = 0.883). cPD at the DC in LEV-resistant populations ranged from 4 to 54% with the median of 9%, and was significantly lower than both the former (p = 0.047) and the latter GIN populations (p = 0.010).
Gastrointestinal nematode populations
H. contortus was present in 41 herds (98%, CI 95%: 88 to 100%), Trichostrongylus spp. in 37 herds (88%, CI 95%: 75 to 95%), Oesophagostomum spp. in 22 herds (52%, CI 95%: 38 to 67%), and Teladorsagia spp. in 14 herds (33%, CI 95%: 21 to 48%). Median fecal egg count (FEC) in the herds ranged from 75 to 2450 epg.
At the DC, no Oesophagostomum larvae developed irrespective of the herd’s AR status. In the case of BZ-resistance H. contortus larvae developed at the DC in 95% of the populations which initially harboured this GIN, Trichostrongylus larvae in 81% of the populations, and Teladorsagia larvae in 36% of the populations. In the case of ML-resistance Trichostrongylus larvae developed at the DC in 91% of the populations, Teladorsagia larvae in 79% of the populations and H. contortus larvae in 74% of the populations. In the case of LEV-resistance Trichostrongylus larvae developed at the DC in 100% of the populations, while H. contortus larvae in 20% of the populations, and Teladorsagia larvae in no population. Of 5 herds resistant to LEV, 3 had Trichostrongylus spp. as the only GIN left in wells with LEV at the DC, and 2 had Trichostrongylus spp. and H. contortus. These results indicated that H. contortus spp. and Trichostrongylus spp. were mainly responsible for AR to BZ, all three GIN were responsible for AR to ML, while Trichostrongylus spp. was the main GIN resistant to LEV (Fig. 2).
Fig. 2.
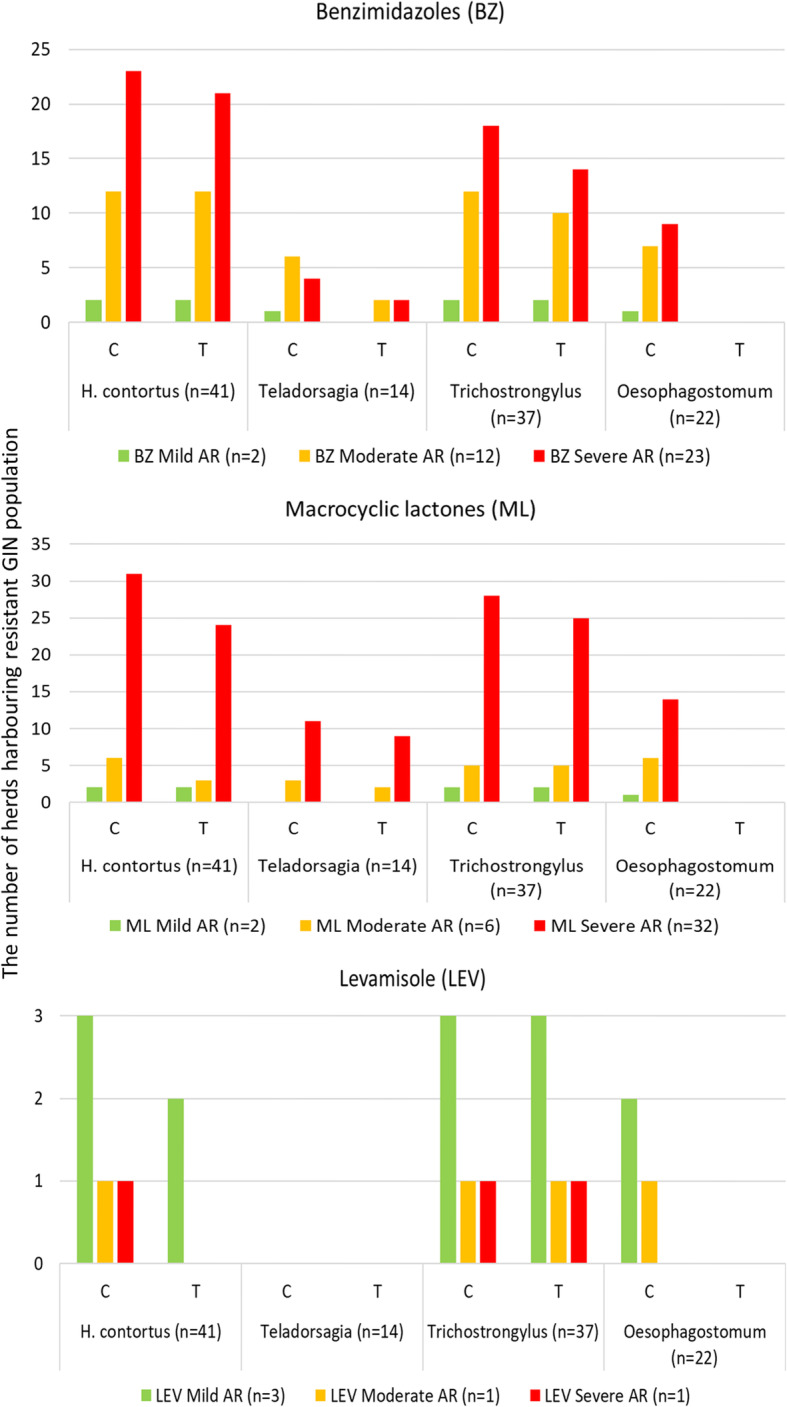
The number of herds harbouring GIN populations resistant to benzimidazoles (BZ), macrocyclic lactones (ML), and levamisole (LEV) in which larvae developed in control wells (C) and in tested wells (T) at the discriminating concentration (DC). Anthelmintic resistance was classed as mild (< 10% of larvae developed at the DC), moderate (10–50% of larvae), and severe (> 50% of larvae). Letter “n” stands for the number of herds infected with a relevant GIN
Factors linked to AR
Presence of AR to BZ and ML in virtually all investigated herds reduced the reliability of most statistical analyses. The number of times goats had been dewormed was significantly positively linked with the intensity of AR to BZ (p = 0.007), but not to ML (p = 0.643) or LEV (p = 0.849). The use of BZ was significantly related to the presence of AR to BZ (p = 0.002), however there was no significant relationship between the use of ML and LEV and the presence of relevant AR (p = 0.449 and p = 0.099, respectively). Interestingly, AR to LEV was observed in 3 herds whose owners declared not to have used LEV in previous 3 years. The same applied to 9 herds with AR to ML, and 3 herds with AR to BZ. None of the following: access to pasture, introducing goats from other herds, and grazing with sheep or cattle on common pasture was significantly linked with AR to any of the anthelmintics.
Discussion
Our cross-sectional study shows that AR to BZ and ML is widespread in Polish goat herds, whereas AR to LEV is uncommon. This is the first study systematically investigating the prevalence of AR to three basic classes of anthelmintics in small ruminants in Poland. Similar surveys based on in vitro tests have so far been conducted in Europe on sheep flocks in Lithuania [9, 34] and Ireland [35], and sheep and goat flocks in Slovakia [15, 36]. Moreover, the LDT is a commonly applied technique in the AR prevalence studies in the United States [11, 16, 37, 38], Philippines [39, 40], Canada [41] and the New Zealand [42, 43] in both goat and sheep flocks. The LDT allows to estimate efficacy of anthelmintics in nematode populations from small farms where performance of a FECRT for even one anthelmintic would be impractical [11, 40]. This is the case in Poland, where most of goat herds consist of only a few animals.
Anthelmintics most often used in goats in Poland are albendazole, fenbendazole and eprinomectin, while levamisole is used rarely and this fact appears to directly correspond to the prevalence of AR. BZ are relatively inexpensive and have short withdrawal periods, which matters a lot to Polish farmers as their herds mainly produce milk and cheese. Moreover, BZ are believed to eliminate tapeworms and liver flukes which are commonly considered by farmers widespread and dangerous for goats, even though our observations seem to contradict those statements [44]. Anyway, several decades of relying virtually solely on BZ must have led to the point at which we are now – the vast majority of herds harbour resistant GIN. Cold comfort is the fact that Polish situation does not seem to be much distinct from other European countries where prevalence of AR to BZ in goats is equally high [3, 15, 45].
Surprisingly, AR to ML is equally widespread in Poland, yet the first case was described only a year ago [32]. The prevalence of AR to ML in goats varies between European countries from 0% in Norway [46], 20% in Italy [47] to 100% in some regions of Switzerland [48]. Situation in Poland is closer to this in Switzerland and AR to ML in goats has already exceeded 90%. The most important cause seems to be the presence on the Polish veterinary market of eprinomectin in pour-on formulation for cattle with milk withdrawal period of 0 days (routinely extrapolated to goats). Pour-on formulation makes its use very simple and eprinomectin is also commonly used in Poland to control external parasite invasions without taking into account its simultaneous effect on GIN. These facts make it one of the most popular anthelmintic agents in Poland. However, eprinomectin is very likely to be commonly underdosed in Polish goat population since the appropriate dose of eprinomectin against GIN in goats is at least two times higher than that for cattle [49, 50], Unfortunately, our experience shows that this fact is unknown or routinely neglected by farmers and veterinarians, also for financial reasons. As all avermectins have the same mechanism of action the cross-resistance with ivermectin is complete [51]. Moreover, it has been suggested that ML may select single nucleotide polymorphism at BZ-resistance-associated codons of β-tubulin [52, 53]. As a consequence, AR to ML and BZ appear to be mutually related phenomena and frequent use of ML may stimulate the development of BZ resistance.
AR to LEV in Polish goat population is still uncommon and mild, which appears to result from its rare use. LEV is viewed by veterinarians as an old-fashioned drug with narrow margin of safety and low effectiveness so they prefer to avoid it. Data on the prevalence of AR to LEV in goats in Europe are limited, mainly case reports have been published in Denmark [54], France [13, 14], and the UK [55]. Recent, large-scale Dutch study did not reveal AR to LEV in sheep flocks [56].
Interestingly, AR to certain anthelmintic classes was observed on some farms where their owners declared not to have used this particular anthelmintic class at all. We suppose there are three possible explanations to this phenomenon, none of which excludes the others. First, the farmers may have not been fully aware of anthelmintics used since some of them are administered by veterinarians during consultation on the farm, especially in the case of injectable anthelmintics. Secondly, our questionnaire applied to quite a long period of time (3 years) and it is likely that farmers could have simply forgotten the facts of using of anthelmintics on their farms. And thirdly, there could be some goats purchased from other herds in Poland or abroad which had been dewormed with this particular anthelmintic and thus carried resistant GIN population. It is mainly the case in herds with AR to LEV and without previous use of this anthelmintic as in all these herds Anglo-Nubian goats were kept and goats of this breed are usually imported to Poland from abroad, mostly from Germany where AR to all three anthelmintic classes in small ruminants has so far been detected [57]. Moreover, owners of these three herds declared in the questionnaire to have purchased goats in the past.
Multidrug resistance of GIN in goats in Europe is not widespread [45], and only a few cases have so far been reported in Denmark [54], France [13], Switzerland [58], UK [59] and Poland [33]. Given that on most of farms BZ and ML are used, either separately, simultaneously or interchangeably, multidrug AR will most likely develop in those herds which, seeking the solution for dropping effectiveness of routine deworming, will switch to levamisole and use it intensively for some time. As AR to LEV seems to develop quite quickly [60] a year of routine LEV use suffices to produce AR.
In our study we decided to use the DC rather than the EC50 criterion for differentiation between resistant and susceptible GIN as an application of the EC50 may sometimes underestimate the resistance and thus some herds might have been incorrectly classed by this criterion as susceptible [61]. It has been suggested that using the EC99 values or the DC in the in vitro tests such as the LDT or EHT can substantially increase test sensitivity of the test and identify resistance when only a small proportion of the GIN population is resistant [8, 61, 62]. To maintain high accuracy of our classification we decided to use two criteria, one based on the corrected percentage of development at the DC and the another based on EC99, simultaneously.
AR to BZ and ML seems to be conveyed by three main GIN which we identified in our study – H. contortus, Trichostrongylus spp., and Teladorsagia spp. Only Oesophagostomum spp. showed no potential to become resistant to any anthelmintic which is at odds with some recent studies in which Oesophagostomum spp. was together with H. contortus and Trichostrongylus spp. resistant to BZ and ML [63, 64]. Moreover, our observation has to be treated with caution as the only DC which has been scientifically proven to indicate AR is the DC of IVM-AG for H. contortus. Initially, it had been set at 5.4 ng/ml, however then its elevation to 21.6 ng/ml was suggested [8], and as a consequence we decided to use the higher DC as a safer option. However, nothing is known about the DC indicating AR in Trichostrongylus spp. or Teladorsagia sp. so we cannot be sure that the development of these GIN at this DC corresponds to their resistance to ML. Even though it is very likely to be so, it undoubtedly warrants further investigation. Interestingly, it seems that Trichostrongylus spp., not H. contortus as we initially expected, is the main culprit responsible for the early stage of development of AR to LEV. We made this observation first in our recent study [33] and this survey appears to confirm it, however we do not know any studies regarding this topic in goats. Studies so far conducted in sheep and goats have indicated that both Trichostrongylus spp. and H. contortus are responsible for AR to LEV [11, 13, 14, 16, 25, 37, 38, 54, 57, 63–69].
Our work presents the results of an in vitro test (LDT) which may in some circumstances differ from those obtained in an in vivo method such as FECRT. Such discrepancies have multifactorial background and most of these factors remain beyond researcher’s control [15, 70, 71]. Nevertheless, LDT and FECRT have been proven to show moderate to good agreement, especially regarding BZ and LEV resistance detection [10, 15, 72, 73]. Therefore, our results are likely to present the true AR status of the examined goat herds.
The main drawback to our study is the fact that herds enrolled in the survey were not randomly selected. Their owners had sent fecal samples to our laboratory at least once before so they were probably somehow aware of the importance of parasite control in goats. Given that most of them used to deworm all their goats routinely, usually using the same drug for a long time, they were more likely to promote the development of AR on their farms. Therefore, it is possible that our results may to some extent overestimate AR prevalence in the country, and we hope they do so. Anyway, they allow to realize that this problem already exists in Poland and unless actions are undertaken to stop it, soon no anthelmintic will remain effective in some goat herds. The another drawback to our study is that when we performed LDT with LEV we wrongly used 1.3% DMSO in control wells while LEV was diluted in water (contrary to TBZ and IVM-AG which were diluted in 1.3% DMSO). As a result if 1.3% DMSO had a potential to reduce larval development, this mistake could have falsely increased the corrected percentage of developing larvae in tested wells at the DC. Our previous observations have not indicated that DMSO at such a low concentration impacts on larval development to any noteworthy extent (unpublished data). However, even if it did we hope that the double criterion we used for classification GIN populations as resistant would reduce the risk of falsely positive result to an acceptable minimum.
Conclusions
This study provides the first comprehensive data on the prevalence of AR in goat herds in Poland. AR to BZ and ML is widespread, while AR to LEV is currently at a low level. Therefore, an appropriate strategy of GIN control should be applied by farmers and veterinarians as soon as possible not to let the situation slip out of control.
Methods
Study design
This was a cross-sectional study and lasted virtually one year, from September 2018 to June 2019. During this time the owners of 85 private dairy goat herds who had cooperated with our laboratory in previous 4 years (2015–2018), were invited to voluntarily enrol in the study. Those who declared participation were asked to collect fecal samples after at least 8 weeks since the last deworming had passed, and detailed instructions on proper collection and preparation of anaerobically stored fecal samples were sent to them. In herds which consisted of less than 15 adult goats fecal samples were collected from all animals, otherwise samples were collected from 15 to 20 goats selected by the owners. The owners were asked to pick only these goats which had been present on their farm for at least 8 previous weeks to avoid including goats dewormed within this period of time by the former owner. Fecal samples were collected by the farmers (owners of the goats) directly from the rectum. Pooled fecal samples weighing 50–100 g were placed in plastic containers filled with tap water to ensure anaerobic conditions. Samples were delivered to the laboratory within 24 h at room temperature and processed within next 24 h so that the total time which had elapsed between sample collection and examination did not exceed 48 h.
In each herd the following information was collected using the questionnaire: the number of adult goats (> 6 month-old) and kids, access to the pasture, co-grazing or rotational grazing with sheep and cattle, purchase of goats from other herds, and the history of deworming including the number of times the herd had been dewormed in previous 3 years and drugs used.
According to Polish legal regulations (The Act of the Polish Parliament of 15 January 2015 on the Protection of Animals Used for Scientific or Educational Purposes, Journal of Laws 2015, item 266) no formal ethics consent was required for this study except for the informed consent of participants, which we obtained in written from each participating farmer.
Larval development test
Based on the technique defined by Hubert and Kerboeuf [74], the larval development test (LDT) was performed with the modifications of Várady et al. [75, 76]. Nematode eggs were collected by sequentially sieving the anaerobically stored fecal samples through stacked sieves with apertures of 250, 100 and 25 μm. The material collected on the 25 μm sieve was washed with tap water, sedimented, and then flotation method with saturated sodium chloride was applied in order to obtain the suspension of the nematodes eggs [7]. After extraction, eggs were inspected microscopically to ensure that embryonation had not yet begun and suspended in deionized water at a concentration of 70–100 eggs in 10 μl per well. The pure thiabendazole (Sigma-Aldrich, Merck, Germany; TBZ), ivermectin aglycone (Santa Cruz Biotechnology, USA; IVM-AG), and levamisole (Sigma-Aldrich, Merck, Germany; LEV) were firstly dissolved in ≥99.5% dimethyl sulfoxide (Sigma-Aldrich, Merck, Germany; DMSO) in case of TBZ and IVM-AG or deionized water in case of LEV and serially diluted 1:2 in DMSO (TBZ, IVM-AG) or in deionized water (LEV). The overall DMSO concentration in the pre-dilution plate was 20%. Then, diluted anthelmintics and DMSO (control) were moved to the test plate to yield final concentration of 1.3% in the tested wells. The 12 concentrations of TBZ, IVM-AG and LEV finally used in the LDT ranged from 0.0006 to 1.28 μg/ml, from 0.084 to 173.6 ng/ml, and from 0.020 to 32 μg/ml, respectively. Test was performed on 96-well cell culture plates (Sarsted, Germany) with culture medium (150 μl) which consisted of 10 μl of (all in one test plate) TBZ, IVM-AG, LEV or DMSO (1.3%; control wells) solution, 110 μl of deionised water, 20 μl of culture medium as described by Hubert and Kerboeuf [77] and 10 μl of a suspension (approximately 70–100 eggs) containing Amphotericin B (Sigma-Aldrich, Merck, Germany) at a concentration of 5 μg/ml. Each anthelmintic concentration was tested in duplicate. The LDT plates (sealed – to prevent drying) were incubated for 7 days at 25 °C (Cooled incubator, INCU-Line® Standard, VWR). After the incubation period, 10 μl of Lugol’s solution was added to each well to terminate development of larvae. The unhatched eggs and L1-L3 larvae were counted under an inverted microscope in each well (Olympus, CKX53, Poland) and the L3 larvae were classified at species/genus level in the tested and control wells following the procedure detailed elsewhere [78]. The arithmetic mean of the percentage of larvae developing in two tested wells at each anthelmintic concentration (percentage development in tested wells, PDT) was corrected by the percentage of developing larvae in the control wells (PDC) according to the following formula:
cPD = PDT / PDC,
where cPD stood for corrected percentage of larvae developing in tested wells.
The concentration of each anthelmintic inhibiting development of 50% (median effective concentration, EC50) and 99% (EC99) of larvae was estimated using the 4 parameter logistic curve [79].
The results of LDT were interpreted with respect to the discriminating concentration (DC) of anthelmintic agent which was defined as the concentration of anthelmintic at which the development of at least 99% of susceptible larvae (corrected by the larvae developing in control wells as mentioned above) would have been inhibited [7, 62]. The following DC were used in the study: 0.08 μg/ml for TBZ [15], 21.6 ng/ml [34, 36] for IVM-AG, and 2.0 μg/ml for LEV [80].
Two criteria had to be simultaneously fulfilled to classify a GIN population from a given goat herd as resistant to the particular anthelmintic: cPD at the DC significantly higher than 1% (meaning that the entire 95% confidence interval (CI 95%) was above 1%) and EC99 > DC.
AR was arbitrarily classed in terms of severity as follows: cPD at the DC from > 1 to 10% – mild AR, from > 10 to 50% – moderate AR, above 50% – severe AR. Multidrug AR (MDR) was defined as the presence of AR to all three different classes of anthelmintics.
Statistical analysis
Numerical variables were presented as the median, interquartile range (IQR) and range, and compared between groups using the Mann-Whitney U test (unpaired groups) or Wilcoxon signed rank test (paired groups). Categorical variables were given as count and percentage in a group, and compared between groups using the Pearson’s chi-square test or the Fisher exact test. The 95% confidence intervals (CI 95%) for percentages were calculated using the Wilson score method [81]. Correlations between cPD at the DC and EC50 were assessed using the Spearman’s rank correlation coefficient (Rs). The significance level (α) was set at 0.05 and the Bonferroni correction was applied in the case of multiple comparisons. Statistical analysis was performed in TIBCO Statistica 13.3.0 (TIBCO Software Inc., Palo Alto, CA).
Supplementary Information
Additional file 1: Fig. S1. Correlations (presented as the Spearman’s rank correlation coefficients, Rs) between the corrected percentage of larvae developing in tested wells (cPD) at the discriminating concentration (DC) of each anthelmintic agent and the median effective concentration (ED50) of each anthelmintic agent. Scatter plots presenting correlations between cPD at DC and ED50 for each of anthelmintic agents.
Acknowledgments
This article is based upon work from COST Action COMBAR CA16230, supported by COST (European Cooperation in Science and Technology).
Abbreviations
- α
Significance level
- AR
Anthelmintic resistance
- BZ
Benzimidazoles
- CI 95%
Confidence interval for the level of confidence of 95%
- cPD
Corrected percentage of developing larvae
- DC
Discriminating concentration
- DMSO
Dimethyl sulfoxide
- EC50
Median effective concentration
- EC99
The 99th percentile effective concentration
- EHT
Egg hatch test
- epg
Eggs per gram
- FEC
Fecal egg count
- FECRT
Fecal egg count reduction test
- GIN
Gastrointestinal nematodes
- IQR
Interquartile range
- IVM
Ivermectin
- IVM-AG
Ivermectin aglycone
- LDT
Larval development test
- LEV
Levamisole
- MDR
Multidrug resistance
- ML
Macrocyclic lactones
- PDC
Percentage development in control wells
- PDT
Percentage development in tested wells
- Rs
Spearman’s rank correlation coefficient
- TBZ
Thiabendazole
Authors’ contributions
MM, MC and JK designed the study. MM, AM, OS-J, AV-P, MV processed fecal samples and performed parasitological tests. MC performed statistical and epidemiological analysis. MM, MC, IM-D and JK interpreted the results and wrote the manuscript draft. MS, PG, MV reviewed the manuscript. All authors have read and approved the manuscript.
Funding
The study was partly financed by the grant from the Ministry of Science and Higher Education of the Republic of Poland, decision no. 9506/E-385/R/2018. The funding body provided financial support for modernizing and equipping the parasitological laboratory in which parasitological tests were performed. The funding body had no direct role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The data sets used and/or analyzed are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was carried out in accordance with the standards recommended by the EU Directive 2010/63/EU for animal experiments and Good Laboratory Practice and The Act of the Polish Parliament of 15 January 2015 on the Protection of Animals Used for Scientific or Educational Purposes (Journal of Laws 2015, item 266). According to Polish legal regulations (The Act of the Polish Parliament of 15 January 2015 on the Protection of Animals Used for Scientific or Educational Purposes, Journal of Laws 2015, item 266) no formal ethics consent was required for this study except for the informed consent of participants. Therefore, the written informed consent for participation in the study, including processing fecal samples and data collected in the questionnaire, was obtained by us from all farmers who decided to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoste H, Sotiraki S, de Jesús Torres-Acosta JF. Control of endoparasitic nematode infections in goats. Vet Clin North Am Food Anim Pract. 2011;27:163–173. doi: 10.1016/j.cvfa.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Várady M, Papadopoulos E, Dolinská M, Königová A. Anthelmintic resistance in parasites of small ruminants: sheep versus goats. Helmintologia. 2011;48:137–144. doi: 10.2478/s11687-011-0021-7. [DOI] [Google Scholar]
- 3.Chartier C, Pors I, Hubert J, Rocheteau D, Benoit C, Bernard N. Prevalence of anthelmintic resistant nematodes in sheep and goats in Western France. Small Rum Res. 1998;29:33–41. doi: 10.1016/S0921-4488(97)00116-8. [DOI] [Google Scholar]
- 4.Sargison ND, Jackson F, Bartley DJ, Wilson DJ, Stenhouse LJ, Penny CD. Observations on the emergence of multiple anthelmintic resistance in sheep flocks in the south-east of Scotland. Vet Parasitol. 2007;145:65–76. doi: 10.1016/j.vetpar.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 5.Aksit D, Yalinkilinc HS, Sekkin S, Boyacioğlu M, Cirak VY, Ayaz E, Gokbulut C. Comparative pharmacokinetics and bioavailability of albendazole sulfoxide in sheep and goats, and dose dependent plasma disposition in goats. BMC Vet Res. 2015;11:124. doi: 10.1186/s12917-015-0442-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.González Canga A, Sahagún Prieto AM, José Diez Liébana M, Martínez NF, Vega MS, Vieitez JJ. The pharmacokinetics and metabolism of ivermectin in domestic animal species. Vet J. 2009;179:25–37. doi: 10.1016/j.tvjl.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Coles GC, Jackson F, Pomroy WE, Prichard RK, von Samson-Himmelstjerna G, Silvestre A, Taylor MA, Vercruysse The detection of anthelmintic resistance in nematodes of veterinary importance. Vet Parasitol. 2006;136:167–185. doi: 10.1016/j.vetpar.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 8.Dolinská M, Königová A, Letková V, Molnár L, Várady M. Detection of ivermectin resistance by a larval development test – Back to the past or step forward? Vet Parasitol. 2013;198:154–158. doi: 10.1016/j.vetpar.2013.07.043. [DOI] [PubMed] [Google Scholar]
- 9.Kupčinskas T, Stadalienė I, Šarkūnas M, Petkevičius S. Anthelmintic resistance in sheep farms in Lithuania detected by in vitro micro-agar larval development test. Vet Med Zoot. 2015;72:21–23. [Google Scholar]
- 10.Ruffell A, Raza A, Elliott TP, Kotze AC. The use of the larval development assay for predicting the in vivo efficacy of levamisole against Haemonchus contortus and Trichostrongylus colubriformis. Vet Parasitol. 2018;30:6–11. doi: 10.1016/j.vetpar.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Crook EK, O'Brien DJ, Howell SB, Storey BE, Whitley NC, Burke JM, Kaplan RM. Prevalence of anthelmintic resistance on sheep and goat farms in the mid-Atlantic region and comparison of in vivo and in vitro detection methods. Small Rumin Res. 2016;143:89–96. doi: 10.1016/j.smallrumres.2016.09.006. [DOI] [Google Scholar]
- 12.Anonymous . Drenchrite®©, Larval Development Assay Standard Operating Procedures, Horizon Technology Pty Ltd, Roseville, NSW, Australia. 1996. [Google Scholar]
- 13.Chartier C, Soubirac F, Pors I, Silvestre A, Hubert J, Couquet C, Cabaret J. Prevalence of anthelmintic resistance in gastrointestinal nematodes of dairy goats under extensive management conditions in southwestern France. J Helminthol. 2001;75:325–330. doi: 10.1017/S0022149X01000506. [DOI] [PubMed] [Google Scholar]
- 14.Paraud C, Kulo A, Pors I, Chartier C. Resistance of goat nematodes to multiple anthelmintics on a farm in France. Vet Rec. 2009;164:563–564. doi: 10.1136/vr.164.18.563. [DOI] [PubMed] [Google Scholar]
- 15.Babják M, Konigöva A, Urda-Dolinská M, Vadlejch J, Varády M. Anthelmintic resistance in goat herds – in vivo versus in vitro detection methods. Vet Parasitol. 2018;254:10–14. doi: 10.1016/j.vetpar.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 16.Howell SB, Burke JM, Miller JE, Terrill TH, Valencia E, Williams MJ, Williamson LH, Zajac AM, Kaplan RM. Prevalence of anthelmintic resistance on sheep and goat farms in the south-eastern United States. J Am Vet Med Assoc. 2008;233:1913–1919. doi: 10.2460/javma.233.12.1913. [DOI] [PubMed] [Google Scholar]
- 17.Arece-García J, López-Leyva Y, Olmedo-Juárez A, Ramírez-Vargas G, Reyes-Guerrero D, López Arellano ME, De Gives PM, Várady M, Rojo-Rubio R, González-Garduño R. First report of multiple anthelmintic resistance in goat farm in Cuba. Helminthologia. 2017;54:358–362. doi: 10.1515/helm-2017-0037. [DOI] [Google Scholar]
- 18.Wanyangu SW, Bain RK, Rugutt MK, Nginyi JM, Mugambi JM. Anthelmintic resistance amongst sheep and goats in Kenya. Prev Vet Med. 1996;25:285–290. doi: 10.1016/0167-5877(95)00502-1. [DOI] [Google Scholar]
- 19.Bakunzi FR, Nkomo LK, Motsei LE, Ndou RV, Nyirenda M. A survey on anthelmintic resistance in nematode parasites of communally grazed sheep and goats in a rural area of north West Province, Republic of South Africa. Life Sci J. 2013;10:391–393. [Google Scholar]
- 20.Nabukenya I, Rubaire-Akiiki C, Olila D, Muhangi D, Höglund J. Anthelmintic resistance in gastrointestinal nematodes in goats and evaluation of FAMACHA diagnostic marker in Uganda. Vet Parasitol. 2014;205:666–675. doi: 10.1016/j.vetpar.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 21.Wakayo BU, Dewo TF. Anthelmintic resistance of gastrointestinal parasites in small ruminants: a review of the case of Ethiopia. J Vet Sci Technol. 2015;S10:001. [Google Scholar]
- 22.Dorny P, Claerebout E, Vercruysse J, Sani R, Jalila A. Anthelmintic resistance in goats in peninsular Malaysia. Vet Parasitol. 1994;55:327–342. doi: 10.1016/0304-4017(94)90073-6. [DOI] [PubMed] [Google Scholar]
- 23.Basripuzi HB, Sani RA, Ariff OM. Anthelmintic resistance in selected goat farms in Kelantan. Mal J Anim Sci. 2012;15:47–56. [Google Scholar]
- 24.Das M, Singh S. Anthelmintic resistance to nematodes in sheep and goat farms in Hisar. J Vet Parasitol. 2005;19:103–106. [Google Scholar]
- 25.Manikkavasagan I, Binosundar ST, Raman M. Survey on anthelmintic resistance to gastrointestinal nematodes in unorganized goat farms of Tamil Nadu. J Parasit Dis. 2015;39:258–261. doi: 10.1007/s12639-013-0335-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh R, Bal MS, Singla LD, Kaur P. Detection of anthelmintic resistance in sheep and goat against fenbendazole by faecal egg count reduction test. J Parasit Dis. 2016;41:463–466. doi: 10.1007/s12639-016-0828-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jabbar A, Iqbal Z, Saddiqi HA, Babar W, Saeed M. Prevalence of multiple anthelmintic resistant gastrointestinal nematodes in dairy goats in a desolated tract (Pakistan) Parasitol Res. 2008;103:29–35. doi: 10.1007/s00436-008-0923-6. [DOI] [PubMed] [Google Scholar]
- 28.Balicka-Ramisz A, Ramisz A, Malecki J, Supera K. Case of the resistance of the gastrointestinal nematodes to fenbendazole in sheep (in polish with summary in English) Magazyn Weterynaryjny. 1997;6:442–443. [Google Scholar]
- 29.Balicka-Ramisz AK, Ramisz AZ. Benzimidazoles resistance in nematode parasites in domesticated animals in north-west part of Poland. Electron J Pol Agric Univ. 1999;2:2. [Google Scholar]
- 30.Kowal J, Wyrobisz A, Nosal P, Kucharski M, Kaczor U, Skalska M, Sendor P. Benzimidazole resistance in the ovine Haemonchus contortus from southern Poland –coproscopical and molecular findings. Ann Parasitol. 2016;62:119–123. doi: 10.17420/ap6202.43. [DOI] [PubMed] [Google Scholar]
- 31.Mickiewicz M, Czopowicz M, Górski P, Kaba J. The first reported case of resistance of gastrointestinal nematodes to benzimidazole anthelmintic in goats in Poland. Ann Parasitol. 2017;63:317–322. doi: 10.17420/ap6304.118. [DOI] [PubMed] [Google Scholar]
- 32.Mickiewicz M, Czopowicz M, Moroz A, Szaluś-Joardanow O, Górski P, Várady M, Königová A, Spinu M, Lefkaditis M, Kaba J. Development of resistance to eprinomectin in gastrointestinal nematodes in a goat herd with pre-existing resistance to benzimidazoles. Pol J Vet Sci. 2019;22:753–760. doi: 10.24425/pjvs.2019.131404. [DOI] [PubMed] [Google Scholar]
- 33.Mickiewicz M, Czopowicz M, Kawecka-Grochocka E, Moroz A, Szaluś-Jordanow O, Várady M, Königová A, Spinu M, Górski P, Bagnicka E, Kaba J. The first report of multidrug resistance in gastrointestinal nematodes in goat population in Poland. BMC Vet Res. 2020;16:270. doi: 10.1186/s12917-020-02501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kupčinskas T, Stadalienė I, Šarkūnas M, Riškevičienė V, Várady M, Höglund J, Petkevičius S. Prevalence of anthelmintic resistance on Lithuanian sheep farms assessed by in vitro methods. Acta Vet Scand. 2015;57:88. doi: 10.1186/s13028-015-0179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Good B, Hanrahan JP, De Waal DT, Patten T, Kinsella A, Lynch CO. Anthelmintic-resistant nematodes in Irish commercial sheep flocks – the state of play. Ir Vet J. 2012;65:21. doi: 10.1186/2046-0481-65-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dolinská M, Ivanišinová O, Königová A, Várady M. Anthelmintic resistance in sheep gastrointestinal nematodes in Slovakia detected by in-vitro methods. BMC Vet Res. 2014;10:233. doi: 10.1186/s12917-014-0233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Terrill TH, Kaplan RM, Larsen M, Samples OM, Miller JE, Gelaye S. Anthelmintic resistance on goat farms in Georgia: efficacy of anthelmintics against gastrointestinal nematodes in two selected goat herds. Vet Parasitol. 2001;97:261–268. doi: 10.1016/S0304-4017(01)00417-4. [DOI] [PubMed] [Google Scholar]
- 38.Mortensen LL, Williamson LH, Terrill TH, Kircher RA, Larsen M, Kaplan RM. Evaluation of prevalence and clinical implications of anthelmintic resistance in gastrointestinal nematodes in goats. J Am Vet Med Assoc. 2003;223:495–500. doi: 10.2460/javma.2003.223.495. [DOI] [PubMed] [Google Scholar]
- 39.Venturina VM, Ancheta PB, Dobson RJ, Eduardo SL, Gray GD. Use of a larval development assayto estimate anthelmintic efficacy in goats in smallholder farming systems. Philippine Agricultural Scientist. 2003;86:134–139. [Google Scholar]
- 40.Ancheta PB, Dumilon RA, Venturina VM, Cerbito WA, Dobson RJ, LeJambre LF, Villar EC, Gray GD. Efficacy of benzimidazole anthelmintics in goats and sheep in the Philippines using a larval development assay. Vet Parasitol. 2004;120:107–121. doi: 10.1016/j.vetpar.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 41.Falzon LC, Menzies PI, Shakya KP, Jones-Bitton A, Vanleeuwen J, Avula J, Stewart H, Jansen JT, Taylor MA, Learmount J, Peregrine AS. Anthelmintic resistance in sheep flocks in Ontario, Canada. Vet Parasitol. 2013;193:150–62. [DOI] [PubMed]
- 42.Shyam S. A survey of anthelmintic resistance and parasite management practices on sheep farms in New Zealand: a dissertation presented in partial fulfilment of the requirements for the degree of Master of Veterinary Studies (Veterinary Parasitology) at Massey University. Palmerston North: Master of Veterinary Studies (M.V.S.); 2004. p. 37–54.
- 43.Kamaludeen J. Studies on the occurrence of anthelmintic resistance in goat parasites in New Zealand: a thesis presented in partial fulfilment of the requirements for the degree of Master of Veterinary Studies in Parasitology at Massey University, Palmerston North, New Zealand. Palmerston North: Master of Veterinary Studies (M.V.S.); 2010. p. 52–73.
- 44.Mickiewicz M, Czopowicz M, Moroz A, Witkowski L, Szaluś-Jordanow O, Nalbert T, Markowska-Daniel I, Górski P, Kaba J. Common endoparasitic infections in goats in Poland – diagnostics and treatment (in polish with summary in English) Życie weterynaryjne. 2017;92:665–668. [Google Scholar]
- 45.Rose H, Rinaldi L, Bosco A, Mavrot F, de Waal T, Skuce P, Charlier J, Torgerson PR, Hertzberg H, Hendrickx G, Vercruysse J, Morgan ER. Widespread anthelmintic resistance in European farmed ruminants: a systematic review. Vet Rec. 2015;176:546. doi: 10.1136/vr.102982. [DOI] [PubMed] [Google Scholar]
- 46.Domke AVM, Chartier C, Gjerde B, Höglund J, Leine N, Vatn S, Stuen S. Prevalence of anthelmintic resistance in gastrointestinal nematodes of sheep and goats in Norway. Parasitol Res. 2012;111:185–193. doi: 10.1007/s00436-012-2817-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zanzani S, Gazzonis A, Di Cerbo A, Várady M, Manfredi M. Gastrointestinal nematodes of dairy goats, anthelmintic resistance and practices of parasite control in northern Italy. BMC Vet Res. 2014;10:114. doi: 10.1186/1746-6148-10-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murri S, Knubben-Schweizer G, Torgerson P, Hertzberg H. Frequency of eprinomectin resistance in gastrointestinal nematodes of goats in canton Berne, Switzerland. Vet Parasitol. 2014;203:114–119. doi: 10.1016/j.vetpar.2014.02.052. [DOI] [PubMed] [Google Scholar]
- 49.Gawor J, Borecka A, Malczewski A. Use of eprinomectin (Eprinex pour-on) to control natural infection by gastro-intestinal nematodes in goats. Med Weter. 2000;56:398–400. [Google Scholar]
- 50.Rostang A, Devos J, Chartier C. Review of the Eprinomectin effective doses required for dairy goats: where do we go from here? Vet Parasitol. 2020;277:1089–1092. doi: 10.1016/j.vetpar.2019.108992. [DOI] [PubMed] [Google Scholar]
- 51.Lespine A, Ménez C, Bourguinat C, Prichard RK. P-glycoproteins and other multidrug resistance transporters in the pharmacology of anthelmintics: prospects for reversing transport- dependent anthelmintic resistance. Int J Parasitol Drugs Drug Resist. 2012;2:58–75. doi: 10.1016/j.ijpddr.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mottier ML, Prichard RK. Genetic analysis of a relationship between macrocyclic lactone and benzimidazole anthelmintic selection on Haemonchus contortus. Pharmacogen Genomics. 2008;18:129–140. doi: 10.1097/FPC.0b013e3282f4711d. [DOI] [PubMed] [Google Scholar]
- 53.Williamson SM, Storey B, Howell S, Harper KM, Kaplan RM, Wolstenholme AJ. Candidate anthelmintic resistance-associated gene expression and sequence polymorphisms in a triple-resistant field isolate of Haemonchus contortus. Mol Biochem Parasitol. 2011;180:99–105. doi: 10.1016/j.molbiopara.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 54.Maingi N, Bjørn H, Thamsborg SM, Bøgh HO, Nansen P. A survey of anthelmintic resistance in nematode parasites of goats in Denmark. Vet Parasitol. 1996;66:53–66. doi: 10.1016/S0304-4017(96)01006-0. [DOI] [PubMed] [Google Scholar]
- 55.Hong C, Hunt KR, Coles GC. Occurrence of anthelmintic resistant nematodes on sheep farms in England and goat farms in England and Wales. Vet Rec. 1996;139:83–86. doi: 10.1136/vr.139.4.83. [DOI] [PubMed] [Google Scholar]
- 56.Ploeger HW, Everts RR. Alarming levels of anthelmintic resistance against gastrointestinal nematodes in sheep in the Netherlands. Vet Parasitol. 2018;262:11–15. doi: 10.1016/j.vetpar.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 57.Voigt K, Scheuerle M, Hamel D, Pfister K. High perinatal mortality associated with triple anthelmintic resistance in a German sheep flock. Tierarztl Prax Ausg G Grosstiere Nutztiere. 2012;40:107–111. doi: 10.1055/s-0038-1623104. [DOI] [PubMed] [Google Scholar]
- 58.Schnyder M, Torgerson PR, Schönmann M, Kohler L, Hertzberg H. Multiple anthelmintic resistance in Haemonchus contortus isolated from south African Boer goats in Switzerland. Vet Parasitol. 2005;128:285–290. doi: 10.1016/j.vetpar.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 59.Jackson F, Jackson E, Coop RL. Evidence of multiple anthelmintic resistance in a strain of Teladorsagia circumcincta (Ostertagia circumcincta) isolated from goats in Scotland. Res Vet Sci. 1992;53:371–374. doi: 10.1016/0034-5288(92)90142-O. [DOI] [PubMed] [Google Scholar]
- 60.Zajac AM, Gipson TA. Multiple anthelmintic resistance in a goat herd. Vet Parasitol. 2000;87:163–172. doi: 10.1016/S0304-4017(99)00174-0. [DOI] [PubMed] [Google Scholar]
- 61.Várady M, Cudeková P, Corba J. In vitro detection of benzimidazole resistance in Haemonchus contortus: egg hatch test versus larval development test. Vet Parasitol. 2007;149:104–110. doi: 10.1016/j.vetpar.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 62.Čudeková P, Várady M, Dolinská M, Königová A. Phenotypic and genotypic characterisation of benzimidazole susceptible and resistant isolates of Haemonchus contortus. Vet Parasitol. 2010;172:155–159. doi: 10.1016/j.vetpar.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 63.Dey AR, Begum N, Anisuzzaman Alim MA, Alam MZ. Multiple anthelmintic resistance in gastrointestinal nematodes of small ruminants in Bangladesh. Parasitol Int. 2020;77:102–105. doi: 10.1016/j.parint.2020.102105. [DOI] [PubMed] [Google Scholar]
- 64.Herrera-Manzanilla FA, Ojeda-Robertos NF, González-Garduño R, Cámara-Sarmiento R, Torres-Acosta JFJ. Gastrointestinal nematode populations with multiple anthelmintic resistance in sheep farms from the hot humid tropics of Mexico. Vet Parasitol Reg Stud Reports. 2017;9:29–33. doi: 10.1016/j.vprsr.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 65.Chandrawathani P, Yusoff N, Wan LC, Ham A, Waller PJ. Total anthelmintic failure to control nematode parasites of small ruminants on government breeding farms in Sabah. East Malaysia Vet Res Commun. 2004;28:479–489. doi: 10.1023/B:VERC.0000040240.69004.dc. [DOI] [PubMed] [Google Scholar]
- 66.Waghorn T, Knight J, Leathwick D. The distribution and anthelmintic resistance status of Trichostrongylus colubriformis, T. vitrinus and T. axeiin lambs in New Zealand. N Z Vet J. 2014;62:152–159. doi: 10.1080/00480169.2013.871193. [DOI] [PubMed] [Google Scholar]
- 67.Chaparro JJ, Villar D, Zapata JD, López S, Howell SB, López A, Storey BE. Multi-drug resistant Haemonchus contortus in a sheep flock in Antioquia, Colombia. Vet Parasitol Reg Stud Reports. 2017;10:29–34. doi: 10.1016/j.vprsr.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 68.Hodgson B, Mulvaney CJ. Resistance to a triple-combination anthelmintic in Trichostrongylus spp. on a commercial sheep farm in New Zealand. N Z Vet J. 2017;65:1–5. doi: 10.1080/00480169.2017.1333468. [DOI] [PubMed] [Google Scholar]
- 69.Oliveira PAD, Riet-Correa B, Estima-Silva P, Coelho ACB, Santos BLD, Costa MAP, Ruas JL, Schild AL. Multiple anthelmintic resistance in southern Brazil sheep flocks. Rev Bras Parasitol Vet. 2017;26:427–432. doi: 10.1590/s1984-29612017058. [DOI] [PubMed] [Google Scholar]
- 70.Vidyaszankar AN, Kaplan RM, Chan S. Statistical approach to measure the efficacy of anthelmintic treatment on horse farms. Parasitology. 2007;134:2027–2039. doi: 10.1017/S003118200700340X. [DOI] [PubMed] [Google Scholar]
- 71.Vidyaszankar AN, Hanlon BM, Kaplan RM. Statistical and biological considerations in evaluating drug efficacy in equine strongyle parasites using fecal egg count data. Vet Parasitol. 2012;185:45–56. doi: 10.1016/j.vetpar.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 72.Taylor MA, Learmount J, Lunn E, Morgan C, Craig BH. Multiple resistance to anthelmintics in sheep nematodes and comparison of methods used for their detection. Small Rumin Res. 2009;86:67–70. doi: 10.1016/j.smallrumres.2009.09.020. [DOI] [Google Scholar]
- 73.Maingi N, Bjorn H, Dangolla A. The relationship between faecal egg count reduction and the lethal dose 50% in the egg hatch assay and larval development assay. Vet Parasitol. 1998;77:133–145. doi: 10.1016/S0304-4017(97)00222-7. [DOI] [PubMed] [Google Scholar]
- 74.Hubert J, Kerboeuf D. A micro-larval development assay for the detection of anthelmintic resistance in sheep nematodes. Vet Rec. 1992;130:442–446. doi: 10.1136/vr.130.20.442. [DOI] [PubMed] [Google Scholar]
- 75.Várady M, Bjørn H, Nansen P. In vitro characterization of anthelmintic susceptibility of field isolates of the pig nodular worm Oesophagostomum spp., susceptible or resistant to various anthelmintics. Int J Parasitol. 1996;26:733–740. doi: 10.1016/0020-7519(96)00051-3. [DOI] [PubMed] [Google Scholar]
- 76.Várady M, Corba J, Letková V, Kovác G. Comparison of two versions of larval development test to detect anthelmintic resistance in Haemonchus contortus. Vet Parasitol. 2009;160:267–271. doi: 10.1016/j.vetpar.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 77.Hubert J, Kerboeuf D. A new method for culture of larvae used in diagnosis of ruminant gastrointestinal strongylosis: comparison with fecal cultures. Can J Comp Med. 1984;48:63–71. [PMC free article] [PubMed] [Google Scholar]
- 78.van Wyk JA, Mayhew E. Morphological identification of parasitic nematode infective larvae of small ruminants and cattle: a practical lab guide. Onderstepoort J Vet Res. 2013;80:1–14. doi: 10.4102/ojvr.v80i1.539. [DOI] [PubMed] [Google Scholar]
- 79.Dobson RJ, Griffiths DA, Donald AD, Waller PJ. A genetic model describing the evolution of levamisole resistance in Trichostrongylus colubriformis, a nematode parasite of sheep. IMA J Math Appl Med Biol. 1987;4:279–293. doi: 10.1093/imammb/4.4.279. [DOI] [PubMed] [Google Scholar]
- 80.Taylor MA. A larval development test for the detection of anthelmintic resistance in nematodes of sheep. Res Vet Sci. 1990;49:198–202. doi: 10.1016/S0034-5288(18)31077-4. [DOI] [PubMed] [Google Scholar]
- 81.Altman D, Machin D, Bryant T, Gardner M. Statistics with Confidence: Confidence Intervals and Statistical Guidelines. 2nd ed. Bristol: BMJ Books; 2000.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig. S1. Correlations (presented as the Spearman’s rank correlation coefficients, Rs) between the corrected percentage of larvae developing in tested wells (cPD) at the discriminating concentration (DC) of each anthelmintic agent and the median effective concentration (ED50) of each anthelmintic agent. Scatter plots presenting correlations between cPD at DC and ED50 for each of anthelmintic agents.
Data Availability Statement
The data sets used and/or analyzed are available from the corresponding author on reasonable request.