Abstract
Background
Despite recent progress in the treatment of ST‐segment–elevation myocardial infarction, data on geographic disparities application of the evidence‐based therapy remain limited.
Methods and Results
The J‐PCI (Japanese Percutaneous Coronary Intervention) registry is a nationwide registry to assure the quality of delivered care. Between January 2014 and December 2018, 209 521 patients underwent percutaneous coronary intervention for ST‐segment–elevation myocardial infarction in 1126 institutions. The patients were divided into tertiles according to the population density (PD) of the percutaneous coronary intervention institution location (low: <951.7/km2, n = 69 797; medium: 951.7–4729.7/km2, n = 69 750; high: ≥4729.7/km2, n = 69 974). Patients treated in high PD administrative districts were younger and more likely to be male. No significant correlation was observed between PD and door‐to‐balloon time (regression coefficients: 0.036 per 1000 people/km2; 95% CI, −0.232 to 0.304; P = 0.79). Patients treated in low‐PD areas had higher crude in‐hospital mortality rates than those treated in high‐PD areas (low: 2.89%; medium: 2.60%; high: 2.38%; P < 0.001); PD and in‐hospital mortality had a significantly inverse association, before and after adjusting for baseline characteristics (crude odds ratio [OR], 0.983 per 1000/km2; 95% CI, 0.973–0.992; P < 0.001; adjusted OR, 0.980 per 1000/km2; 95% CI, 0.964–0.996; P = 0.01, respectively). Higher‐PD districts had more operators per institution (low: 6; interquartile range, 3–10; medium: 7; IQR, 3–13; high: 8; IQR, 5–13; P < 0.001), suggesting an inverse association with in‐hospital mortality (OR, 0.992; 95% CI, 0.986–0.999; P = 0.03).
Conclusions
Geographic inequality was observed in in‐hospital mortality of patients with ST‐segment–elevation myocardial infarction who underwent percutaneous coronary intervention. Variation in the number of operators per institution, rather than traditional quality indicators (eg, door‐to‐balloon time) might explain the difference in in‐hospital mortality.
Keywords: percutaneous coronary intervention, population studies, ST‐segment–elevation myocardial infarction
Nonstandard Abbreviations and Acronyms
- AMI
acute myocardial infarction
- IQR
interquartile range
- NCDR
National Cardiovascular Data Registry
- OR
odds ratio
- PCI
percutaneous coronary intervention
- PD
population density
- STEMI
ST‐segment–elevation myocardial infarction
Clinical Perspective.
What Is New?
In this nationwide prospective registry including 209 521 patients who underwent percutaneous coronary intervention for ST‐segment–elevation myocardial infarction in 1126 institutions, population density and in‐hospital mortality had a significantly inverse association, before and after adjusting for baseline characteristics.
Higher–population density districts had more operators per institution, which might explain the difference in in‐hospital mortality.
What Are the Clinical Implications?
Marked geographic inequality was observed in immediate case fatality; patients treated in population‐dense areas had a lower in‐hospital mortality than those treated in less dense areas.
Over the past decades, the outcome of patients with acute myocardial infarction (AMI) has improved considerably. 1 , 2 Post‐AMI outcome largely depends on the access to immediate and specialized medical interventions and implementation of evidence‐based clinical practice guideline recommendations. 3 , 4 , 5 Such accessibility and implementation are greatly influenced by the geographic location and the level of facilities available within the community and the hospital to which a patient initially presents.
Japan has a universal healthcare system that is operated by the federal government, 6 and ambulance services are administered by a government‐based system and include professional emergency care providers, with minimum fee applied to the insurers. 7 However, the access to and delivery of healthcare services still exhibit inequalities. This gap may have widened over the recent years, given that small‐sized hospitals are downgraded or closing in recent years. In the past decades, the population and industry in Japan have shifted to urban areas, paralleling with depopulation and aging of rural areas; consequently, access to medical services in less population‐dense areas has become limited. 8 , 9 , 10
In this study, we aimed to assess the discrepancy by population density (PD) on the quality and clinical outcomes of patients who underwent primary percutaneous coronary intervention (PCI) after experiencing ST‐segment–elevation MI (STEMI), using a nationwide procedural registry and a data set from complete population census data in Japan. Identifying the association between PD and the outcome of PCI may aid in improving the political and administrative strategy for AMI.
Methods
The J‐PCI (Japanese Percutaneous Coronary Intervention) registry is an ongoing prospective multicenter nationwide PCI registry maintained by the Japanese Association of Cardiovascular Intervention and Therapeutics. The J‐PCI registry aims to provide national, regional, and institutional information on the general view of the patient background, clinical presentation, angiographic and procedural details, and in‐hospital outcomes (full variable definitions are available at cvit.jp/registry/jpci_definition.pdf) as a foundation for further quality improvement. 11 , 12 In addition, the J‐PCI registry has been incorporated into the National Clinical Data system, a nationwide prospective web‐based registry linked to medical and surgical board certification since 2013. Cardiac catheterization procedures are carried out in both publicly and privately funded hospitals in Japan, but because registration in the J‐PCI database is mandatory for both systems, data completeness is high; approximately 85% to 90% of all PCI procedures in Japan were estimated to be registered in the J‐PCI registry, when compared with the annual reports from the insurance claims data. The J‐PCI study protocol conformed to the principles outlined in the Declaration of Helsinki and was approved by the Institutional Review Board of the Network for Promotion of Clinical Studies (a specialized nonprofit organization affiliated with Osaka University Graduate School of Medicine in Osaka, Japan). Written informed consent was waived because of the retrospective study design.
In the present analysis, we included 1 199 008 patients undergoing PCI in 1156 institutions between January 2014 and December 2018. STEMI was defined as AMI with ST‐segment elevation on ≥ 2 contiguous leads (≥0.2 mV in a precordial lead at the J point or ≥ 0.1 mV in a limb lead), new left bundle branch block, or posterior myocardial infarction on a 12‐lead ECG accompanied by elevated cardiac biomarkers. Elevated cardiac biomarkers were defined as elevated creatine kinase or creatine kinase myocardial band levels (2‐fold higher than the normal values) or elevated troponin levels (≥99th percentile). Cardiogenic shock was defined as an episode of systolic blood pressure < 80 mm Hg, cardiac index < 1.8 L/min/m2, or the requirement for parenteral inotropic or vasopressor agents or mechanical support to maintain blood pressure and cardiac indexes above those levels. Cardiopulmonary arrest was defined as cardiac arrest or respiratory arrest requiring cardiopulmonary resuscitation within 24 hours before the PCI procedure.
In accordance with the Transparency and Openness Promotion Guidelines, the data that support the findings of this study are available from the corresponding author upon reasonable request.
Geographic and Population Data
In Japan, a complete population census was conducted every 5 years to clarify the population status. Geographic and population data of the administrative county districts were collected from the complete population census in 2015 provided by the Statistics Bureau, Ministry of Internal Affairs and Communications. 13 In 2015, Japan was inhabited by approximately 127 million people per 378 000 km2 area. Within 3 levels of the administrative district (eg, national, prefectural, and municipal), we compared the PD municipally, comprising cities, towns, and villages. For the present analysis, the patients were divided into tertiles according to the PD at the location of PCI institution (low: <951.7/km2, n = 69 797; medium: 951.7–4729.7/km2, n = 69 750; high: ≥4729.7/km2, n = 69 974).
Outcomes
The primary outcome of this study was in‐hospital death (either until discharge, or within 30 days after PCI for patients with prolonged hospitalization). In each participating hospital, a data manager collects the in‐hospital outcome. The Japanese Association of Cardiovascular Intervention and Therapeutics holds an annual meeting of data managers and visits 30 to 40 randomly chosen participating institutions yearly to check the quality of submitted data, which revealed a high accuracy, with < 1% inconsistency from auditing visits.
We also examined the institutional and operator volume and door‐to‐balloon time to evaluate their disparity in different PD tertiles for data sets collected after January 2016 (76.7% of the studied patients; collection on door‐to‐balloon time was initiated after this time). Door‐to‐balloon time was defined as the time starting from the patient’s arrival at the institution to the first balloon inflation during PCI. Institutions and operators have unique identifiers, and institutional and operator volume were calculated as the mean annual number of patients with STEMI per institution or per operator.
Statistical Analysis
Figure 1 illustrates the study flowchart. Of the 1 199 008 patients that underwent PCI from 1126 institutions, 209 521 (17.4%) were diagnosed with STEMI. PDs of administrative districts in Japan are shown in Figure 2A. We classified the patients into tertiles according to the PD of the PCI institution location (low: <951.7/km2, n = 69 797; medium: 951.7–4729.7/km2, n = 69 750; high: ≥4729.7/km2, n = 69 974).
Figure 1. Study flowchart.
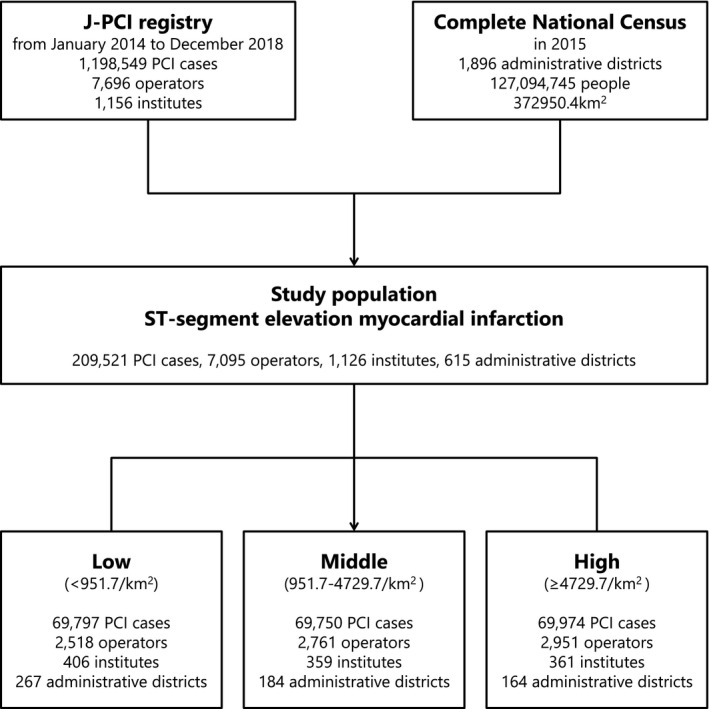
PCI indicates percutaneous coronary intervention.
Figure 2.
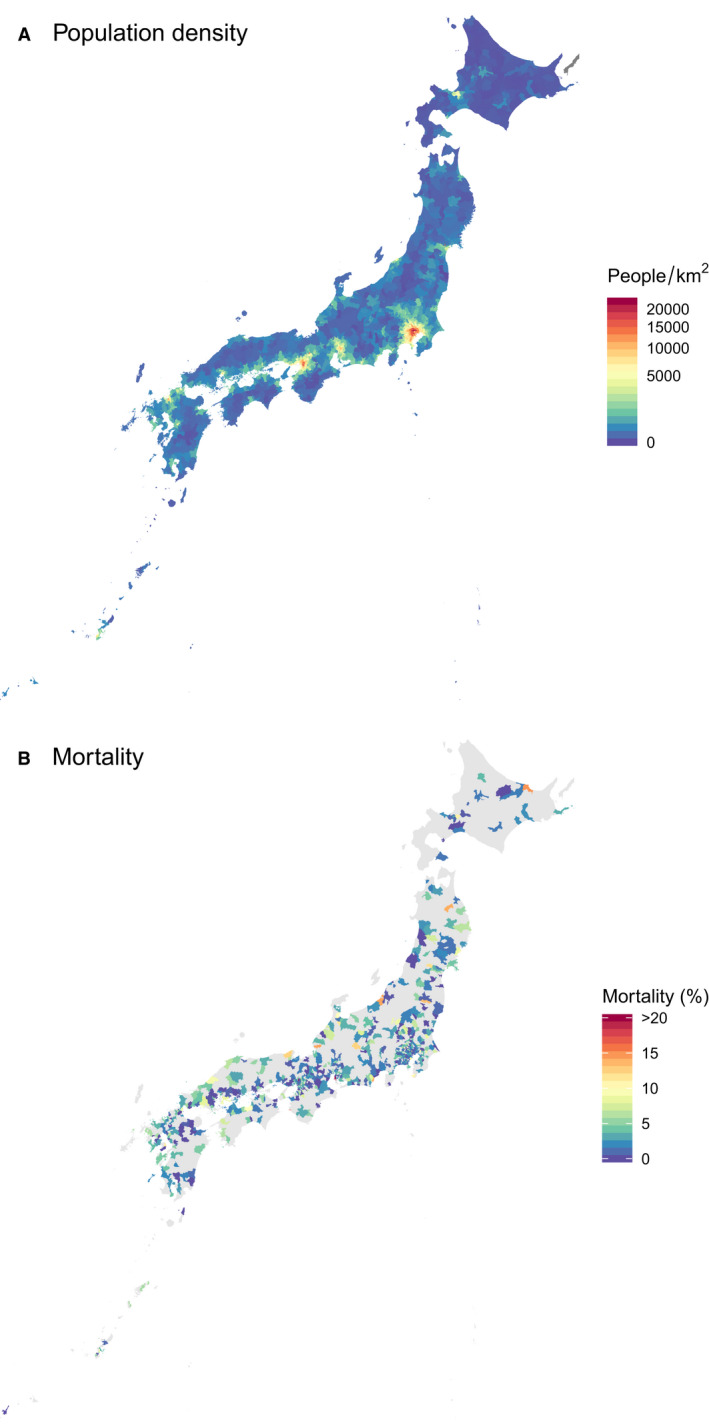
(A) Population density and (B) mean in‐hospital mortality according to the administrative districts.
Categorical variables, which were reported as numbers with relative percentage, were compared using the chi‐square test, whereas continuous variables, which were expressed as mean ± SD or median and interquartile range (IQR), were compared using 1‐way ANOVA or the Kruskal‐Wallis rank‐sum test. We constructed generalized linear mixed models or generalized additive mixed models to assess the effect of explanatory variables on in‐hospital mortality (binomial with logit link function) or door‐to‐balloon time (Gaussian with identity link function). In the multivariable models, the variables listed in Table 1 were also included as explanatory variables to adjust for baseline characteristics. To assess the interaction of PD and door‐to‐balloon time on in‐hospital mortality, the interaction variable was further added to the models. The PCI institutions were included as a random intercept. Odds ratios (ORs) or regression coefficients and their 95% CI were reported. Two‐sided P values of < 0.05 indicates significance. All data were analyzed using the R statistical software version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria) with glmmML and gamm4 packages.
Table 1.
Baseline Characteristics According to the Tertiles of Population Density
| Population Density | Overall |
Low <951.7 People/km2 |
Medium 951.7–4729.7 People/km2 |
High ≥4729.7 People/km2 |
P Value |
|---|---|---|---|---|---|
| Number of patients | 209 521 | 69 797 | 69 750 | 69 974 | |
| Age, y* | 68.6 ± 13.0 | 69.1 ± 12.9 | 68.7 ± 12.9 | 68.0 ± 13.1 | <0.001 |
| Male, n (%)* | 158 866 (76.1 | 52 462 (75.6) | 52 789 (76.0) | 53 615 (76.6) | <0.001 |
| Hypertension, n (%)* | 138 637 (71.2%) | 46 863 (72.2) | 46 085 (70.9) | 45 689 (70.4) | <0.001 |
| Hyperlipidemia, n (%)* | 117 332 (60.2) | 38 315 (59.0) | 39 150 (60.2) | 39 867 (61.4) | <0.001 |
| Diabetes mellitus, n (%)* | 72 587 (37.3) | 24 533 (37.8) | 24 288 (37.4) | 23 766 (36.6) | <0.001 |
| Smoker, n (%)* | 81 468 (41.8) | 26 702 (41.1) | 26 469 (40.7) | 28 297 (43.6) | <0.001 |
| Renal failure, n (%)* | 27 620 (14.2) | 8820 (13.6) | 9517 (14.6) | 9283 (14.3) | <0.001 |
| Dialysis, n (%)* | 4532 (2.33) | 1341 (2.07) | 1596 (2.45) | 1595 (2.46) | <0.001 |
| Prior percutaneous coronary intervention, n (%)* | 33 741 (16.2) | 11 055 (15.9) | 11 108 (16.0) | 11 578 (16.6) | <0.001 |
| Prior coronary artery bypass grafting, n (%)* | 2131 (1.02) | 612 (0.882) | 737 (1.06) | 782 (1.12) | <0.001 |
| Prior heart failure, n (%)* | 12 183 (5.92%) | 4100 (6.00) | 4436 (6.47) | 3647 (5.30) | <0.001 |
| Prior myocardial infarction, n (%)* | 25 624 (12.4) | 8452 (12.2) | 8368 (12.1) | 8804 (12.7) | 0.002 |
| Cardiopulmonary arrest, n (%)* | 12 704 (6.12) | 3661 (5.30) | 4172 (6.03) | 4871 (7.01) | <0.001 |
| Cardiogenic shock, n (%)* | 24 887 (12.0) | 7974 (11.6) | 8068 (11.7) | 8845 (12.7) | <0.001 |
| Access site, n (%) | |||||
| Femoral | 87 823 (41.9) | 29 476 (42.2) | 28 040 (40.2) | 30 307 (43.3) | <0.001 |
| Radial | 115 834 (55.3) | 38 230 (54.8) | 39 775 (57.0) | 37 829 (54.1) | |
| Others | 5863 (2.80) | 2091 (3.00) | 1935 (2.77) | 1837 (2.63) | |
| Target vessels, n (%) | |||||
| Single‐vessel disease | 122 850 (58.6) | 40 376 (57.8) | 41 209 (59.1) | 41 265 (59.0) | <0.001 |
| Double‐vessel disease | 52 126 (24.9) | 17 850 (25.6) | 16 969 (24.3) | 17 307 (24.7) | |
| Triple‐vessel disease | 26 833 (12.8) | 9184 (13.2) | 8790 (12.6) | 8859 (12.7) | |
| Left main disease | 7712 (3.68) | 2387 (3.42) | 2782 (3.99) | 2543 (3.63) | |
Included as explanatory variables in the multivariable models.
Results
Baseline Characteristics
Overall, majority of studied patients had hypertension (71.2%), followed by hyperlipidemia (60.2%), smoking (41.8%), and diabetes mellitus (37.3%). In addition, 14.2% had renal failure, 12.4% had previous myocardial infarction, 5.9% had heart failure, and 2.3% were on maintenance dialysis. PCI was previously performed in 16.2% and coronary bypass grafting in 1.0% of the patients.
The baseline characteristics of patients in each PD tertile are summarized in Table 1. Patients treated in high‐PD administrative districts were, in general, younger (low: 69.1 ± 12.9 years; medium: 68.7 ± 12.9 years; high: 68.0 ± 13.1 years) and likely to be men (low: 75.6%; medium: 76.0%; high: 76.6%). Patients in the higher PD group more often exhibited cardiopulmonary arrest (low: 5.3%; medium: 6.0%; high: 7.0%) and cardiogenic shock (low: 11.6%; medium: 11.7%; high: 12.7%).
Geographic and population data are summarized in Table 2. PCI institutions were located in 615 out of the 1896 administrative districts in Japan (32.4%), covering 94 240 396 people (74.1%) with 127 064.5 km2 (34.1%). Compared with the high‐PD area, the medium‐PD area had a total area of approximately 4.6 times larger, and the low‐PD area had 26 times larger. The low‐, medium‐, and high‐PD tertiles had a mean age of 47.0 ± 24.3, 45.0 ± 23.8, and 44.3 ± 23.0 years; a male proportion of 48.3%, 48.6%, and 49.0%; annual number of deaths of 315 477 (1.15%/y), 285 614 (0.92%/y), and 296 884 (0.83%/y), respectively.
Table 2.
Geographic and Population Data According to the Tertiles of Population Density
| Population Density | Overall |
Low <951.7 People/km2 |
Medium 951.7–4729.7 People/km2 |
High ≥4729.7 People/km2 |
|---|---|---|---|---|
| No. of administrative districts | 615 | 267 | 184 | 164 |
| Total area, km2 | 127 064.5 | 104 554.6 | 18 497.96 | 4011.99 |
| Total population | 94 240 396 | 27 468 751 | 31 141 796 | 35 629 849 |
| Age, y* | 45.3 ± 23.7 | 47.0 ± 24.3 | 45.0 ± 23.8 | 44.3 ± 23.0 |
| ≥70 y, n (%) | 16 862 402 (18.1) | 5 602 416 (20.6) | 5 486 370 (17.8) | 5 773 616 (16.5) |
| Male, n (%) | 45 885 435 (48.7) | 13 268 684 (48.3) | 15 150 304 (48.6) | 17 466 447 (49.0) |
| Annual number of deaths, n (%/y) | 897 975 (0.95/y) | 315 477 (1.15/y) | 285 614 (0.92/y) | 296 884 (0.83/y) |
| Cardiogenic † | 134 735 (0.14/y) | 48 596 (0.18/y) | 42 317 (0.14/y) | 43 822 (0.12/y) |
| Acute myocardial infarction † | 24 774 (0.026/y) | 9702 (0.035/y) | 7930 (0.025/y) | 7142 (0.020/y) |
People aged ≥ 100 years were excluded.
Cause of death of residents in each district was determined through the official death certificates.
In‐Hospital Mortality
Distribution of mean in‐hospital mortality according to the PD is illustrated in Figure 2B. Patients treated in the low‐PD administrative districts had higher in‐hospital mortality rates than those treated in the high‐PD administrative districts (low: 2.89%; medium: 2.60%; high: 2.38%; P < 0.001; Figure 3). In the multivariable logistic regression mixed model adjusting for baseline characteristics, the risk of in‐hospital mortality was significantly lower in the highest‐PD tertile than in the lowest‐PD tertile (low: reference; medium: OR, 0.879; 95% CI, 0.794–1.067; P = 0.19; high: OR, 0.747; 95% CI, 0.616–0.970; P = 0.003). According to the univariate and multivariable logistic regression mixed models including PD as a continuous variable, a significant inverse association was observed between PD and in‐hospital mortality, before and after adjusting for baseline characteristics (crude OR, 0.983 per 1000 people/km2; 95% CI, 0.973–0.992; P < 0001; adjusted OR, 0.980 per 1000 people/km2; 95% CI, 0.964–0.996; P = 0.01).
Figure 3. In‐hospital mortality according to population density.
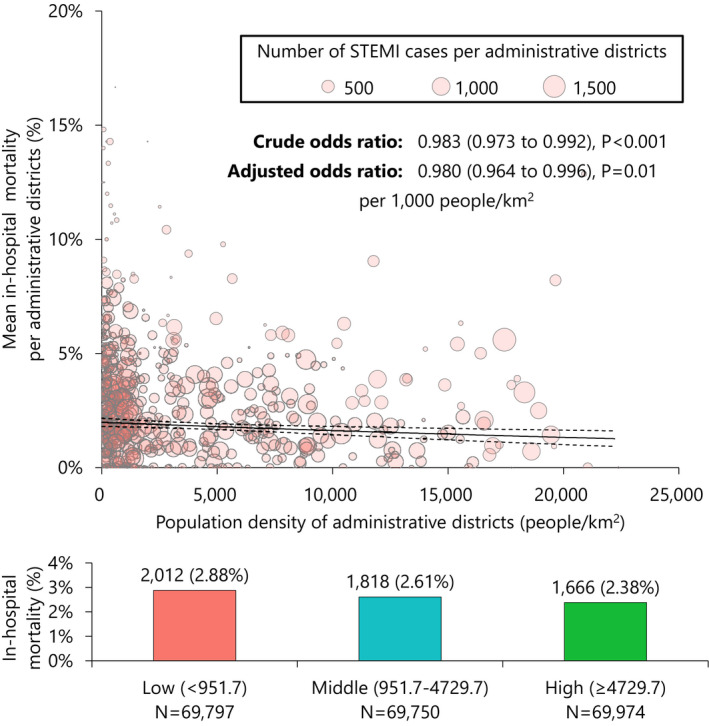
In the upper panel, odds ratios were assessed by the univariate or multivariable generalized linear mixed model including population density of administrative districts as the exploratory variable and in‐hospital mortality as the response variable. Circles represents mean in‐hospital mortality over population density at each administrative district, while their size indicates number of patients with STEMI per administrative district. In the lower panel, the bar graph demonstrates in‐hospital mortality according to the population density tertiles. STEMI indicates ST‐segment–elevation myocardial infarction.
Door‐to‐Balloon Time
Door‐to‐balloon time was < 60 minutes in 31.7%, 60 to 90 minutes in 40.9%, 91 to 120 minutes in 12.9%, and ≥ 120 minutes in 14.5%. The generalized additive mixed model demonstrated that in‐hospital mortality increased from a door‐to‐balloon time of 60 minutes up to 120 minutes (Figure 4A). A significant linear association was also found in the generalized linear mixed model (OR, 1.042 per 10 minutes; 95% CI, 1.037–1.048; P < 0.001). While median door‐to‐balloon time was minimally but significantly different among PD tertiles (low: 72; IQR, 55–93; medium: 70; IQR, 53–90; high: 72; IQR, 55–92; P < 0.001), PD and door‐to‐balloon time had no significant correlations (regression coefficients: 0.036 per 1000 people/km2; 95% CI, –0.232 to 0.304; P = 0.79). The inverse association between PD and in‐hospital mortality remained significant in the model adjusting for door‐to‐balloon time (adjusted OR, 0.981 per 1000 people/km2; 95% CI, 0.970–0.993; P = 0.001) and in the multivariable model adjusting for baseline characteristics and door‐to‐balloon time (adjusted OR, 0.979 per 1000 people/km2; 95% CI, 0.960–0.998; P = 0.03). No significant interactions were observed between PD and door‐to‐balloon time on in‐hospital mortality in the former model (P for interaction 0.23) and in the latter multivariable model (P for interaction 0.67).
Figure 4. In‐hospital mortality in patients with STEMI according to (A) door‐to‐balloon time, (B) number of patients per institution, (C) number of patients per operator, and (D) number of operators per institution.
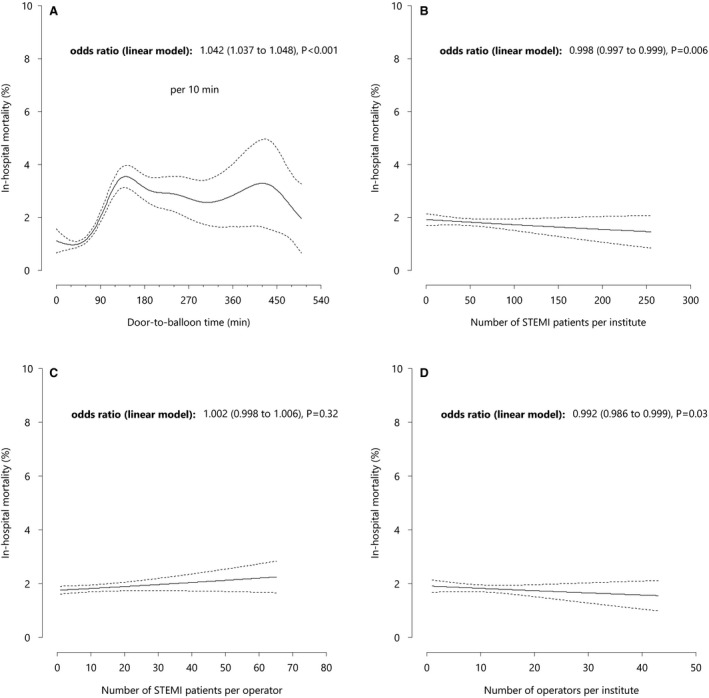
STEMI indicates ST‐segment–elevation myocardial infarction.
Institutional and Operator Volume
The annual number of patients with STEMI per institution was significantly associated with in‐hospital mortality in the overall population (OR, 0.998; 95% CI, 0.997–0.999; P = 0.006; Figure 4B), but no significant difference was observed within the individual PD groups (low: 27.6; IQR, 9.65–49.0; medium: 27.6; IQR, 7.90–55.5; high: 32.8; IQR, 12.2–58.6; P = 0.13; Table 3). 14 The annual number of patients with STEMI per operator was not associated with in‐hospital mortality in the overall population (OR, 1.002; 95% CI, 0.998–1.006; P = 0.32; Figure 4C).
Table 3.
Institution and Operator Volumes According to the Tertiles of Population Density
| Population Density | Overall |
Low <951.7 People/km2 |
Medium 951.7–4729.7 People/km2 |
High ≥4729.7 People/km2 |
P Value |
|---|---|---|---|---|---|
| No. of patients | 209 521 | 69 797 | 69 750 | 69 974 | |
| No. of institutions | 1126 | 406 | 359 | 361 | |
| Annual number of patients with STEMI per institution | 29.0 (9.60–53.2) | 27.6 (9.65–49.0) | 27.6 (7.90–55.5) | 32.8 (12.2–58.6) | 0.13 |
| Annual number (%) of patients with STEMI per institution> 36* | 478 (42.5) | 156 (38.4) | 157 (43.7) | 165 (45.7) | 0.11 |
| No. of operators per institution | 7 (4–12) | 6 (3–10) | 7 (3–13) | 8 (5–13) | <0.001 |
| No. of operators | 7095 | 2518 | 2761 | 2951 | |
| Annual number of patients with STEMI per operator | 3.4 (1.2–7.2) | 3.8 (1.4–8.0) | 3.4 (1.2–7.0) | 3.2 (1.2–6.6) | <0.001 |
| Annual number (%) of patients with STEMI per operators> 11* | 989 (12.0) | 353 (14.0) | 319 (11.5) | 317 (10.7) | <0.001 |
STEMI indicates ST‐segment–elevation myocardial infarction.
Specific cutoff values were chosen according to the ACCF/AHA/SCAI 2013 Update of the Clinical Competence Statement on Coronary Artery Interventional Procedures. 14
The number of patients with STEMI per operator was significantly higher in the lower‐PD area than in the higher‐ and medium‐PD areas (low: 3.8; IQR, 1.4–8.0; medium: 3.4; IQR, 1.2–7.0; high: 3.2; IQR, 1.2–6.6; P < 0.001). Of note, the number of operators per institution was greater in the higher‐PD administrative districts (low: 6; IQR, 3–10; medium: 7; IQR, 3–13; high: 8; IQR, 5–13; P < 0.001), and it was inversely associated with in‐hospital mortality overall (OR, 0.992; 95% CI; 0.986–0.999; P = 0.03, Figure 4D).
In the exploratory analyses, the annual number of patients with STEMI per institution (regression coefficients, −0.130; 95% CI, −0.169 to − 0.091; P < 0.001), the number of patients with STEMI per operator (regression coefficients, −0.083; 95% CI, −0.014 to − 0.026; P = 0.004), and the number of operators per institution (regression coefficients, −0.446; 95% CI, −0.657 to − 0.234; P < 0.001) were inversely associated with door‐to‐balloon time, respectively.
Discussion
In the present analysis of a nationwide database that comprised more than 200 000 patients with STEMI who underwent primary PCI, a marked geographic inequality was observed in in‐hospital mortality. Patients treated in a population‐dense area had a lower in‐hospital mortality than those treated in a less dense area. In‐hospital mortality and the number of operators per institution were inversely associated. Furthermore, PD and door‐to‐balloon time significantly correlated, and a difference was observed in the number of operators per institution rather than the traditional quality indicators.
The overall in‐hospital mortality of 2.62% after PCI for STEMI in our study was comparable with that in Western countries. In the NCDR (National Cardiovascular Data Registry) CathPCI registry, the in‐hospital mortality of patients with STEMI treated with primary PCI was 4.5% to 5.0% between 2005 and 2011, 1 whereas that in the European Society of Cardiology countries ranged from 2.2% to 6.1% in 2010 or 2011. 2 However, the mortality rate varied from 2.38% in the highest‐PD tertile to 2.88% in the lowest‐PD tertile, and an inverse association was also found between the PD and the in‐hospital mortality after PCI for STEMI in the patient‐level analysis. This finding is in line with the fact that a greater annual number of deaths in the lower‐PD tertile were registered in the population census data with regard to all‐cause deaths, cardiogenic deaths, and deaths from AMI. Meanwhile, patients with STEMI in the lower‐PD administrative districts had an older mean age than those in other districts. Furthermore, the proportion of cardiovascular risk factors was minimal but significantly different among the 3 groups. These differences in baseline characteristics might explain the observed inverse association between in‐hospital mortality and PD. Of note, the proportions of cardiopulmonary arrest and cardiogenic shock, which are well‐known predictors for in‐hospital mortality, were greater in patients treated in the higher PD than the other areas.
We also assessed the institutional and operator volume to clarify the hypothesis that imbalance in institutional or operator volume could be an underlying mechanism of urban‐rural difference in in‐hospital mortality. We confirmed that institutional volume and in‐hospital mortality had a volume‐outcome relationship, conforming to previous reports. 15 , 16 , 17 However, the institutional volume among the 3 groups had no significant differences, suggesting that institutional volume per se was not the main reason for the observed inverse association between PD and in‐hospital mortality. Moreover, the operator volume‐outcome relationship was unclear in the previous report from our registry 16 and in the British Cardiovascular Intervention Society registry, 18 but it was significant in the Nationwide Inpatient Sample database, 15 in NCDR, 19 and in a large‐scale meta‐analysis. 20 In the present analysis, the annual number of patients with STEMI per operator was not associated with in‐hospital mortality, and it was even lower in the high‐PD tertile. Taken together, institutional and operator volume was not the direct reason for the difference in in‐hospital mortality among PD tertiles. Meanwhile, the number of operators per institution was greater in higher‐PD tertiles than in other tertiles, and it was associated with a lower in‐hospital mortality. Although the correlation does not simply imply causation, rearrangement of operators between urban and rural areas may improve the outcomes in the lower‐PD administrative districts.
PD had no clear correlation with door‐to‐balloon time. However, patients with AMI in rural areas were reportedly associated with a longer onset‐to‐balloon time than those in urban areas, while time from emergency medical service contact‐to‐balloon time was comparable between urban and rural areas. 21 , 22 Considering that a short onset‐to‐balloon time was associated with a lower in‐hospital mortality, 1 , 23 a greater number of operators per institution in the greater‐PD administrative districts might help patients with STEMI undergo primary PCI in a timely manner, resulting in a lower risk of in‐hospital mortality. While current guidelines for the treatment of STEMI recommend a door‐to‐balloon time of ≤ 90 minutes for patients undergoing primary PCI, we observed a clear dose‐response relationship between shorter patient‐specific door‐to‐balloon time with lower in‐hospital mortality between 60 and 120 minutes, which was in line with the previous reports from the NCDR CathPCI registry. 1 , 24 Additional data collection is needed to test whether a more aggressive target of door‐to‐balloon time of ≤ 60 minutes reduce the in‐hospital mortality at the population level and to clarify the correlation between onset‐to‐balloon time and PD and its impact on clinical outcomes.
Limitations
The present study has several important limitations. First, given that we registered only PCI procedures in the J‐PCI registry, patients who manifested STEMI but did not undergo PCI were not evaluated. However, most patients with STEMI (97.2%) underwent primary PCI rather than coronary artery bypass grafting or medical therapy in Japan. 25 Second, we assessed the PD only in the administrative districts with PCI‐capable centers (n = 92 920 691; 73.1% of the entire Japanese population). Patients living in the administrative districts without PCI‐capable centers would be transferred to other administrative districts. However, we could assume that (1) patients with STEMI were transferred to the nearest PCI‐capable centers and (2) the PD of the nearest administrative districts was comparable with the patient’s administrative districts according to the geographic distribution of PD (Figure 2). Third, we did not adjust for common socioeconomic factors that could be associated with outcomes and represent important confounders. Fourth, door‐to‐balloon time was available only in 76.7% of the eligible patients. Fifth, the generalizability of our observation to other countries remains uncertain, especially for the analyses of annual number of patients with STEMI per operator and per institution. Finally, while number of operators per institution might explain the difference in in‐hospital mortality among PD tertiles, the underlying mechanisms for the observed difference were largely unknown.
Conclusions
Marked geographic inequality was observed in in‐hospital mortality of patients with STEMI who underwent PCI; patients treated in population‐dense areas had a lower in‐hospital mortality than those treated in less dense areas. Variation in the number of operators per institution, rather than traditional quality indicators (eg, door‐to‐balloon time) might explain the difference in in‐hospital mortality.
Sources of Funding
None.
Disclosures
Dr Yamaji reports investigator‐initiated grant funding from Abbott. Dr Kohsaka reports investigator‐initiated grant funding from Bayer and Daiichi Sankyo and personal fees from Bristol‐Myers Squibb. Dr Inohara has a research grant from Boston Scientific. Dr Ishii receives lecture fees from Astellas, AstraZeneca, Bayer, Bristol‐Myers Squibb, Chugai, Daiichi Sankyo, MSD, Otsuka, and Pfizer. Dr Amano receives lecture fees from Astellas Pharma, AstraZeneca, Bayer, Daiichi Sankyo, and Bristol‐Myers Squibb. Dr Ikari received research grant from Boston Scientific and Bayer. The remaining authors have no disclosures to report.
Acknowledgments
The authors are indebted to the participating patients and the members of Japanese Association of Cardiovascular Intervention and Therapeutics for collecting data.
(J Am Heart Assoc. 2020;9:e016952 DOI: 10.1161/JAHA.120.016952.)
For Sources of Funding and Disclosures, see page 10.
References
- 1. Nallamothu BK, Normand S‐LT, Wang Y, Hofer TP, Brush JE, Messenger JC, Bradley EH, Rumsfeld JS, Krumholz HM. Relation between door‐to‐balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;1114–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kristensen SD, Laut KG, Fajadet J, Kaifoszova Z, Kala P, Di Mario C, Wijns W, Clemmensen P, Agladze V, Antoniades L, et al. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: current status in 37 ESC countries. Eur Heart J. 2014;1957–1970. [DOI] [PubMed] [Google Scholar]
- 3. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli‐Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;119–177. [DOI] [PubMed] [Google Scholar]
- 4. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, et al. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;9:e362–e425. [DOI] [PubMed] [Google Scholar]
- 5. Ozaki Y, Katagiri Y, Onuma Y, Amano T, Muramatsu T, Kozuma K, Otsuji S, Ueno T, Shiode N, Kawai K, et al. CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) in 2018. Cardiovasc Interv Ther. 2018;178–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ikegami N, Yoo B‐K, Hashimoto H, Matsumoto M, Ogata H, Babazono A, Watanabe R, Shibuya K, Yang B‐M, Reich MR, et al. Japanese universal health coverage: evolution, achievements, and challenges. The Lancet. 2011;1106–1115. [DOI] [PubMed] [Google Scholar]
- 7. Takahashi M, Kohsaka S, Miyata H, Yoshikawa T, Takagi A, Harada K, Miyamoto T, Sakai T, Nagao K, Sato N, et al. Association between prehospital time interval and short‐term outcome in acute heart failure patients. J Card Fail. 2011;742–747. [DOI] [PubMed] [Google Scholar]
- 8. Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, Gupta R, Kelishadi R, Iqbal R, Avezum A, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high‐income, middle‐income, and low‐income countries (the PURE Study): a prospective epidemiological survey. The Lancet. 2011;1231–1243. [DOI] [PubMed] [Google Scholar]
- 9. Joynt KE, Orav EJ, Jha AK. Mortality rates for Medicare beneficiaries admitted to critical access and non‐critical access hospitals, 2002–2010. JAMA. 2013;1379–1387. [DOI] [PubMed] [Google Scholar]
- 10. Li X, Murugiah K, Li J, Masoudi FA, Chan PS, Hu S, Spertus JA, Wang Y, Downing NS, Krumholz HM, et al. Urban‐rural comparisons in hospital admission, treatments, and outcomes for ST‐segment‐elevation myocardial infarction in China from 2001 to 2011: a retrospective analysis from the China peace study (patient‐centered evaluative assessment of cardiac events). Circ Cardiovasc Qual Outcomes. 2017;9:e003905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sakakura K, Inohara T, Kohsaka S, Amano T, Uemura S, Ishii H, Kadota K, Nakamura M, Funayama H, Fujita H, et al. Incidence and determinants of complications in rotational atherectomy: insights from the national clinical data (J‐PCI Registry). Circ Cardiovasc Interv. 2016;9:e004278. [DOI] [PubMed] [Google Scholar]
- 12. Yamaji K, Kohsaka S, Morimoto T, Fujii K, Amano T, Uemura S, Akasaka T, Kadota K, Nakamura M, Kimura T. Relation of ST‐segment elevation myocardial infarction to daily ambient temperature and air pollutant levels in a Japanese nationwide percutaneous coronary intervention registry. Am J Cardiol. 2017;872–880. [DOI] [PubMed] [Google Scholar]
- 13. The 2015 population census of Japan . https://www.stat.go.jp/data/kokusei/2015/kekka.html. Accessed December 6, 2019.
- 14. Harold JG, Bass TA, Bashore TM, Brindis RG, Brush JE Jr, Burke JA, Dehmer GJ, Deychak YA, Jneid H, Jollis JG, et al. ACCF/AHA/SCAI 2013 update of the clinical competence statement on coronary artery interventional procedures: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training (writing committee to revise the 2007 clinical competence statement on cardiac interventional procedures). Circulation. 2013;436–472. [DOI] [PubMed] [Google Scholar]
- 15. Badheka AO, Patel NJ, Grover P, Singh V, Patel N, Arora S, Chothani A, Mehta K, Deshmukh A, Savani GT, et al. Impact of annual operator and institutional volume on percutaneous coronary intervention outcomes: a 5‐year United States experience (2005–2009). Circulation. 2014;1392–1406. [DOI] [PubMed] [Google Scholar]
- 16. Inohara T, Kohsaka S, Yamaji K, Amano T, Fujii K, Oda H, Uemura S, Kadota K, Miyata H, Nakamura M. Impact of institutional and operator volume on short‐term outcomes of percutaneous coronary intervention: a report from the Japanese nationwide registry. JACC Cardiovasc Interv. 2017;918–927. [DOI] [PubMed] [Google Scholar]
- 17. Post PN, Kuijpers M, Ebels T, Zijlstra F. The relation between volume and outcome of coronary interventions: a systematic review and meta‐analysis. Eur Heart J. 2010;1985–1992. [DOI] [PubMed] [Google Scholar]
- 18. Hulme W, Sperrin M, Curzen N, Kinnaird T, De Belder MA, Ludman P, Kwok CS, Gale CP, Cockburn J, Kontopantelis E, et al. Operator volume is not associated with mortality following percutaneous coronary intervention: insights from the British Cardiovascular Intervention Society registry. Eur Heart J. 2018;1623–1634. [DOI] [PubMed] [Google Scholar]
- 19. Fanaroff AC, Zakroysky P, Dai D, Wojdyla D, Sherwood MW, Roe MT, Wang TY, Peterson ED, Gurm HS, Cohen MG, et al. Outcomes of PCI in relation to procedural characteristics and operator volumes in the United States. J Am Coll Cardiol. 2017;2913–2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Strom JB, Wimmer NJ, Wasfy JH, Kennedy K, Yeh RW. Association between operator procedure volume and patient outcomes in percutaneous coronary intervention: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2014;560–566. [DOI] [PubMed] [Google Scholar]
- 21. Sorensen JT, Terkelsen CJ, Norgaard BL, Trautner S, Hansen TM, Botker HE, Lassen JF, Andersen HR. Urban and rural implementation of pre‐hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST‐elevation myocardial infarction. Eur Heart J. 2011;430–436. [DOI] [PubMed] [Google Scholar]
- 22. Masuda J, Kishi M, Kumagai N, Yamazaki T, Sakata K, Higuma T, Ogimoto A, Dohi K, Tanigawa T, Hanada H, et al. Rural‐urban disparity in emergency care for acute myocardial infarction in Japan. Circ J. 2018;1666–1674. [DOI] [PubMed] [Google Scholar]
- 23. Shiomi H, Nakagawa Y, Morimoto T, Furukawa Y, Nakano A, Shirai S, Taniguchi R, Yamaji K, Nagao K, Suyama T, et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;9:e3257. [DOI] [PubMed] [Google Scholar]
- 24. Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door‐to‐balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;901–909. [DOI] [PubMed] [Google Scholar]
- 25. Nakamura M, Yamagishi M, Ueno T, Hara K, Ishiwata S, Itoh T, Hamanaka I, Wakatsuki T, Sugano T, Kawai K, et al. Current treatment of ST elevation acute myocardial infarction in Japan: door‐to‐balloon time and total ischemic time from the J‐AMI registry. Cardiovasc Interv Ther. 2013;30–36. [DOI] [PubMed] [Google Scholar]


