Abstract
Atherosclerotic cardiovascular disease (ASCVD) has posed an increasing burden on Americans and the United States healthcare system for decades. In addition, ASCVD has had a substantial economic impact, with national expenditures for ASCVD projected to increase by over 2.5‐fold from 2015 to 2035. This rapid increase in costs associated with health care for ASCVD has consequences for payers, healthcare providers, and patients. The issues to patients are particularly relevant in recent years, with a growing trend of shifting costs of treatment expenses to patients in various forms, such as high deductibles, copays, and coinsurance. Therefore, the issue of “financial toxicity” of health care is gaining significant attention. The term encapsulates the deleterious impact of healthcare expenditures for patients. This includes the economic burden posed by healthcare costs, but also the unintended consequences it creates in form of barriers to necessary medical care, quality of life as well tradeoffs related to non‐health–related necessities. While the societal impact of rising costs related to ASCVD management have been actively studied and debated in policy circles, there is lack of a comprehensive assessment of the current literature on the financial impact of cost sharing for ASCVD patients and their families. In this review we systematically describe the scope and domains of financial toxicity, the instruments that measure various facets of healthcare‐related financial toxicity, and accentuating factors and consequences on patient health and well‐being. We further identify avenues and potential solutions for clinicians to apply in medical practice to mitigate the burden and consequences of out‐of‐pocket costs for ASCVD patients and their families.
Keywords: catastrophic expense, cost-of-care, financial distress, financial toxicity, medical bankruptcy, medical bills, out-of-pocket costs
Subject Categories: Quality and Outcomes, Ethics and Policy, Coronary Artery Disease, Peripheral Vascular Disease
For decades, atherosclerotic cardiovascular disease (ASCVD) has posed an increasing burden on Americans and the US healthcare system. In addition, ASCVD also has a substantial economic impact on our society, with national expenditures for ASCVD of $126 billion in 2015, which are projected to increase by over 2.5‐fold to $309 billion in 2035. In total, after accounting for indirect costs of lost productivity, these costs are expected to increase from $322 to $509 billion over this period. 1 This rapid increase in ASCVD‐related costs has significant consequences for payers, providers, and patients.
The issues of costs to patients are particularly relevant to patients in recent years, with a growing trend toward shifting costs of treatment expenses to patients in various forms, such as high deductibles, copays, and coinsurance. 2 , 3 , 4 , 5 Therefore, the issue of “financial toxicity” of health care is gaining significant attention. In general, financial toxicity encapsulates the scope of direct healthcare‐related expenditures at the patient level and the unintended indirect consequences that result in barriers to necessary medical care and better quality of life, as well tradeoffs related to non‐health–related necessities. Although the national impact of rising costs related to ASCVD management has been actively studied and a subject of policy interventions, 6 , 7 , 8 , 9 , 10 , 11 there is a lack of comprehensive assessment of the current literature on the financial impact of cost sharing for health care in ASCVD on patients and their families.
In this review we systematically describe the domains of financial toxicity, with the goal to identify avenues to mitigate the burden and consequences of costs for health care for patients with ASCVD and their families. The review is structured in sections that (1) define financial toxicity in the context of its broad domains of measurement; (2) identify sources and magnitude of expenditures for health care in patients with ASCVD relative to their financial means, particularly among patients at high risk because of a lack of adequate insurance or limited financial means; (3) address the subjective challenges posed by healthcare costs on patients, spanning their direct and indirect effects; (4) describe ongoing efforts to tackle financial toxicity from healthcare costs; and (5) highlight potential future directions to specifically address healthcare financial toxicity for vulnerable patients with ASCVD and their families.
Measurement of Financial Toxicity
Financial toxicity from healthcare costs is defined under objective and subjective domains. Objective financial toxicity measures healthcare spending relative to affordability. Some of these measures have been standardized internationally. The World Bank defines a catastrophic healthcare expense as a healthcare expense that exceeds 40% of a family's cumulative postsubsistence income, which is the income after accounting for spending on food‐related expenses. 12 Such catastrophic expenses are in turn associated with an elevated risk of bankruptcy and financial ruin. 13 , 14 The minimization of catastrophic healthcare expenditures is accepted as a global goal for healthcare systems to achieve, and is important given its correlation to an inability to sustain life's basic needs for a family. 12 However, spending on health care relative to income is a continuum; lower thresholds still likely pose a substantial burden on patients and their families. Some thresholds, such as expenses exceeding 20% of income, are identified as a high financial burden. 15 , 16
In subjective financial toxicity, financial information is reported by the patients themselves, who provide information beyond that of paid expenses. Notably, they share their difficulty paying medical bills. 17 , 18 This information allows for a more thorough assessment of how financial challenges modify care and potential care‐seeking behavior. However, it is acquired by interviews directly with patients, 19 which are only included in select national surveys that are linked to healthcare costs and spending. Furthermore, even a combination of objective and subjective measures is not likely to reflect the financial toxicity of healthcare costs in its entirety, as many may suffer loss of wealth, savings, and even bankruptcy based on their disease status. Moreover, there is financial loss from lost productivity in the form of absenteeism, lower wages based on their disease status, depleted savings, and other measures of financial restraint. 20 , 21
Prevalence of Financial Toxicity in Atherosclerotic Cardiovascular Disease
Economic Burden of Atherosclerotic Cardiovascular Disease: Objective Measures
Healthcare spending on ASCVD represents a substantial proportion of national healthcare spending. 1 The cost burden for patients and their families has only recently been recognized (Figure 1). Across the spectrum of cardiovascular disease, the presence of ASCVD was associated with an excess of $5500 dollars in annual costs, increased resource utilization, and lost productivity. 22 In our recent study, we investigated the healthcare costs incurred by patients with ASCVD and their family members. The overall healthcare costs were extensive and exceeded $20 000 annually for patients with ASCVD, with average annual out‐of‐pocket spending exceeding $2000. 15 Overall, for families with a member with ASCVD, nearly 16% of the household income is spent on out‐of‐pocket healthcare expenditures. 15 Moreover, nearly 1 in 8 (14%) or 2.7 million US families with a member with ASCVD reported financial hardship (out‐of‐pocket healthcare expense exceeding 20% of postsubsistence income) and 5% or 1 million families reported catastrophic health expenditures (out‐of‐pocket healthcare expense exceeding 40% of postsubsistence income). 15 Overall, insurance premiums and prescription medications were the main costs for families with a member with ASCVD (Figure 2A), representing 44% and 22% of out‐of‐pocket healthcare spending among middle‐income and high‐income groups, and 30% and 34% among low‐income groups, respectively. These percentages remained similar within low‐income families with objective financial hardship and catastrophic health expenditures (Figure 2B).
Figure 1. Financial toxicity among adults with atherosclerotic cardiovascular disease in the United States.
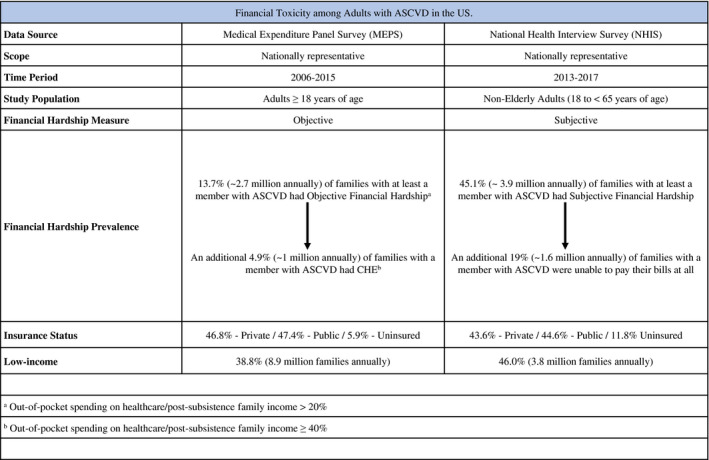
A, Out‐of‐pocket spending on healthcare/post‐subsistence family income >20%. B, Out‐of‐pocket spending on healthcare/postsubsistence family income ≥40%. Data from studies by Khera et al 15 and Valero‐Elizondo et al. 23
ASCVD indicates atherosclerotic cardiovascular disease; and CHE, catastrophic healthcare expenditures.
Figure 2. A, Mean annual out‐of‐pocket expenditures.
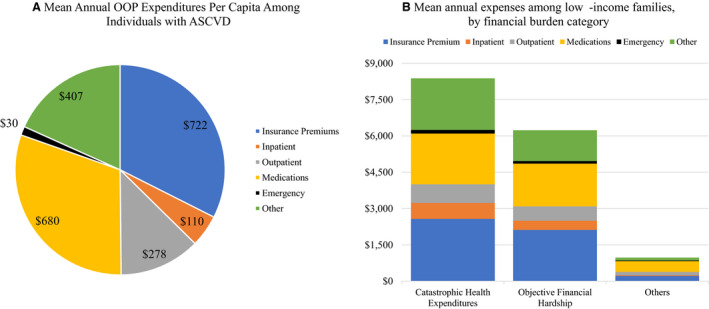
B, Overall annual expenses among low‐income families, stratified by financial burden category, by spending category among individuals with atherosclerotic cardiovascular disease. Data from studies by Khera et al 15 and Valero‐Elizondo et al. 23 ASCVD indicates atherosclerotic cardiovascular disease; CHE, catastrophic healthcare expenditures; and OOP, out‐of‐pocket.
Economic Burden of Atherosclerotic Cardiovascular Disease: Subjective Measures
Compared with more objective measures such as determination of total out‐of‐pocket spending relative to household income, subjective measures of financial toxicity reported by patients with ASCVD are substantially greater. At the national level, families of 3.9 million nonelderly adults (<65 years of age) with ASCVD—45% of families with a member with ASCVD—reported significant difficulty paying medical bills over a 12‐month period (Figure 1). Further, 1 in 5 adults with ASCVD, representing 1.6 million nonelderly adults, was unable to pay any medical bills. 23 These high rates of subjective measures of financial toxicity likely highlight that the objective burden of healthcare spending does not capture the extent of financial challenges encountered by families because of their healthcare costs. The excess subjective financial stress may highlight instances where essential care was deferred, but may also represent personal perception of monetary difficulties that are not captured in objective measures or other financial commitments. 24
Factors Associated With Financial Toxicity
Early insights into financial toxicity among patients with ASCVD and their families suggest that although financial toxicity is prevalent across patient groups, the risk is more pronounced among low‐income families, the uninsured, and the nonelderly who do not have universal healthcare coverage afforded by Medicare (Figure 3). 14 , 25 , 26 , 27 , 28 , 29 , 30
Figure 3. Factors associated with financial toxicity among individuals with atherosclerotic cardiovascular disease.
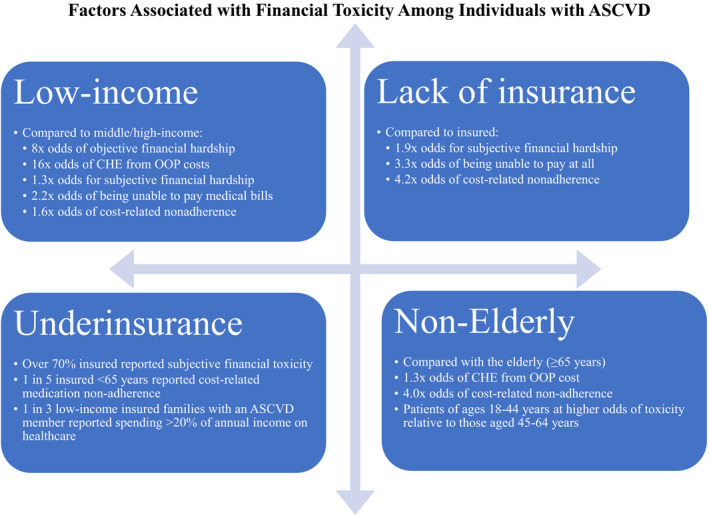
Data from studies by Khera et al, 15 Valero‐Elizondo et al, 23 and Khera et al. 31 ASCVD indicates atherosclerotic cardiovascular disease; CHE, catastrophic healthcare expenditures; CRN, cost‐related medication nonadherence; and OOP, out‐of‐pocket.
Family Income
Low family income is a major risk factor for financial toxicity from healthcare costs. Compared with middle‐income and high‐income families, low‐income families have nearly 4‐fold higher healthcare spending that exceeds 20% of their annual family income (7.0% versus 25.0%). 15 Further, low‐income families had nearly a 10‐fold higher prevalence of experiencing catastrophic health expenditures from out‐of‐pocket costs (1.1% versus 11.1%). After accounting for differences in the characteristics of patients and their families, low‐income families had 8‐fold higher odds of spending 20% or more on healthcare costs and 16‐fold higher odds of catastrophic health expenditures from healthcare expenses. 15 Total healthcare expenses were similar for low‐income families and middle‐income and high‐income families, even though low‐income families had incomes that were 5‐fold lower than those of middle‐income and high‐income families. In parallel, focusing on subjective measures, more than half of the low‐income families with a member with ASCVD reported challenges covering medical bills, with over 2‐fold higher odds of being unable to pay medical bills at all when compared with middle‐income and high‐income families (OR, 2.24; 95% CI, 1.79–2.80). 23
Uninsured and Underinsurance
The literature uniformly reports that similar to families from lower socioeconomic strata, those lacking health insurance more often have financial toxicity—and worse outcomes—when compared with those with insurance. 14 , 26 , 27 , 28 , 29 In a national study of hospitalized patients <65 years of age without health insurance, 85% of patients with acute myocardial infarction and 75% with stroke were expected to suffer catastrophic health expenses based on the costs of hospitalization and patient income. 32 In assessing subjective measures, uninsured patients with ASCVD were at a particularly high risk, with nearly 2‐fold higher odds (OR, 1.86; 95% CI, 1.46–2.36) of any financial hardship from medical bills within the last year, and over 3‐fold higher odds (OR, 3.27; 95% CI, 2.49–4.30) of being unable to pay at all compared with those with health insurance. 23 These findings underscore the ongoing attention needed by policymakers to expand health insurance access for ASCVD patients requiring continued medical care and treatment, especially for low‐income families and the uninsured.
Although the expansion of health insurance coverage in recent years—particularly under the Affordable Care Act—has facilitated increased access to health insurance for more US residents, for a large proportion of patients, insurance coverage provides inadequate financial protection. 29 , 33 This state of underinsurance has increased; now 1 in 4 Americans delays medical treatment because of cost, 34 despite access to insurance. Underinsurance manifests itself with imperfect financial coverage in the face of rising insurance premiums, deductibles, and coinsurance. Notably, the vast majority of patients with ASVCD who report problems paying bills are actually insured, 15 , 23 suggesting inadequate protection against out‐of‐pocket health expenses. Moreover, among nonelderly insured individuals with ASCVD, 1 in 3 from low‐income families faced catastrophic health expenditures from out‐of‐pocket health‐related expenses if they were covered with self‐purchased private insurance, compared with 1 in 5 of those with public insurance. 15 , 31 Such non‐employment–based private insurance had 1.5‐fold higher spending on insurance premiums compared with employment‐based/group‐based private insurance, and was 10‐fold higher compared with public insurance. 15 Insurance premiums represent a substantial proportion of out‐of‐pocket healthcare spending among those insured by these policies, despite otherwise similar healthcare spending. Under current insurance programs, patients are more likely to bear out‐of‐pocket costs for services that are usually subsidized by employers and have high insurance premiums, as well as high deductible expenses and coinsurance payments for most healthcare services.
Nonelderly Patients
Nonelderly adults, representing adults below the age‐based insurance protections offered by Medicare, have higher rates of financial toxicity. This group is particularly vulnerable because of the lack of universal healthcare coverage, healthcare issues caused by unexpected events, and ongoing work commitments, as well as financial responsibilities for dependents. They also have smaller financial reserves to allow them to offset unexpected healthcare expenditures. 20 , 25 , 35 , 36 , 37 Early evidence suggests that despite a higher comorbidity burden and medical‐risk profile, as well as limited active employment, the elderly are still less likely to be challenged by health care. Compared with the nonelderly, elderly patients with ASCVD from low‐income families had lower odds of catastrophic health expenditures from out‐of‐pocket costs (OR, 0.74; 95% CI, 0.58–0.93). 15 Younger patients, in general, reported higher rates of subjective hardship from medical bills overall. 23 , 37 , 38 Surveys of Medicare beneficiaries consistently show that they are less likely to have cost‐related health issues (including problems paying medical bills and high out‐of‐pocket costs), and are more satisfied with their insurance coverage. 39 Similar trends were found among patients with diabetes mellitus, where nonelderly patients were 2‐fold more likely to be unable to afford medical bills relative to the elderly (41.1% versus 20.7%, respectively). 40 Although there is a lower prevalence of ASCVD in patients under 40 years of age, younger adults (18–39 years of age) consistently have higher financial toxicity relative to middle‐aged adults (40–64 years of age), 20 , 23 , 31 , 37 , 40 highlighting some of the challenges of younger adults with limited insurance and scarce financial reserves to cover unexpected healthcare costs.
Consequences of Financial Toxicity
A series of health outcomes and patient behaviors is closely related to the occurrence of financial toxicity. These outcomes span medical and social domains, including suboptimal medical care and the ability to afford basic necessities, like food or housing, 14 especially among those with chronic conditions such as cardiovascular disease and cancer. 41 The interrelated, but distinct, effects of financial toxicity from healthcare costs include (1) direct patient distress, and (2) indirect challenges of healthcare costs, either medical or social. Distress spans financial and psychological domains and reflects in health‐related quality of life. Some examples of financial challenges include cost‐related medication nonadherence, delaying or foregoing medical care, and insecurity about food (Figure 4).
Figure 4. Schematic overview of financial toxicity in atherosclerotic cardiovascular disease.
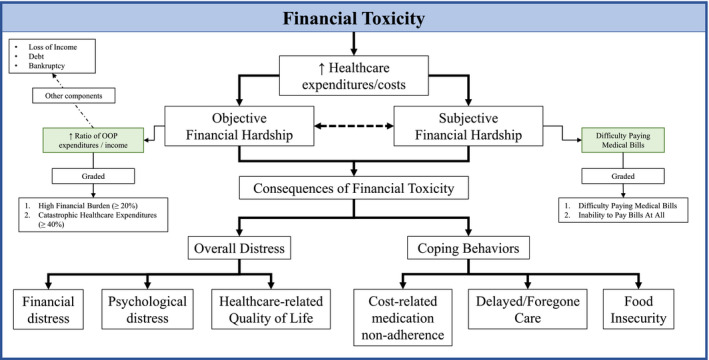
OOP indicates out‐of‐pocket.
Financial Distress and Quality of Life
Financial toxicity is associated with increased worry, anxiety, and even depression. Individuals who reported an inability to pay medical bills had more than 3‐fold higher odds (OR, 3.60; 95% CI, 2.68–4.82) of subjective distress from healthcare finances. 23 These health‐related stressors can often damage other aspects of a patient's life, such as self‐perception of health, mental health, and health‐related quality of life. Overall, psychological distress has been linked to mental health problems, including depression and anxiety, 42 as well as higher expenditures and utilization when compared with those individuals without psychological distress. 43 , 44 , 45 Individuals with ASCVD experiencing catastrophic health expenditures had worse self‐perceived poor health status (OR, 1.86; 95% CI, 1.65–2.10), psychological distress (OR, 1.73; 95% CI, 1.43–2.10), and even clinical depression (OR, 1.55; 95% CI, 1.35–1.79). 46 In a nationally representative sample of US adults ≥40 years of age with ASCVD, reported financial toxicity was associated with higher odds of poor mental (OR, 1.26; 95% CI, 1.08–1.48) and poor physical (OR, 1.44; 95% CI, 1.26–1.85) health‐related quality of life. 46 Other understudied direct consequences of financial toxicity, which include loss of work/income, depletion of assets, medical debt, and bankruptcy, are poorly understood. 47 Whether financial catastrophe is associated with reduced life expectancy and premature mortality among patients with ASCVD has not yet been studied. 48
Cost‐Related Medication Nonadherence
One of the most prominent consequences of health‐related costs is cost‐related medication nonadherence. This includes taking less medication, skipping doses, and/or delaying filling a prescription because of cost. These have been well‐documented across a spectrum of healthcare conditions, 49 , 50 including ASCVD, 31 as well as diabetes mellitus 51 , 52 and cancer. 53 In a report of hospitalized individuals with acute coronary syndrome or decompensated heart failure, Osborn et al found that individuals with subjective financial toxicity were significantly less likely to adhere to their medications and had worse self‐rated health. 54 Recently, we found that nationally almost 13% of adults with ASCVD in the United States (2.2 million annually) reported cost‐related nonadherence, particularly among patients under 65 years of age, where 1 in 4 reported cost‐related nonadherence to medications. 31 Furthermore, these patients had nearly 9‐fold higher odds of resorting to alternative therapies (OR, 8.9; 95% CI, 6.6–12.1). 31 Other groups of patients, including those lacking adequate health insurance and those from low‐income families, were also susceptible to medication nonadherence based on cost.
Delaying or Foregoing Medical Care
Another potential consequence of financial toxicity from healthcare costs is delaying and/or foregoing care because of cost. Although insurance is designed to be protective, among nonelderly individuals, those reporting difficulty paying their medical bills delay or forego care based on cost at a rate of 2 to 3 times that of those who have no difficulty paying medical bills, regardless of insurance status. 36 , 38 This was recently redemonstrated in patients with cardiovascular disease, where subjectively measured, rather than objectively measured, financial toxicity was associated with care delayed or avoided because of cost. 14
Food Insecurity
Financial burden from healthcare costs also affects social well‐being. Food insecurity—not being able to afford food or have enough to eat—is likely a late‐onset consequence of financial toxicity, and often involves entire families. Food insecurity has been associated with a higher 10‐year risk for cardiovascular disease, 55 inversely associated with traditional cardiovascular risk factors and achieving ideal cardiovascular health, 55 , 56 and correlated with overall worse self‐reported health. 41 In the context of financial toxicity, we previously reported that individuals with ASCVD that were unable to pay their medical bills at all had nearly 3‐fold higher odds (OR, 2.89; 95% CI, 2.1–3.9) of suffering from food insecurity, when compared with those without any difficulty paying medical bills. 23 Other aspects of social insecurity caused by medical costs are housing instability and homelessness, which have not been evaluated in any dedicated studies.
Future Directions
Our understanding of financial toxicity and the policy, socioeconomic, and sociocultural drivers, specifically related to ASCVD patients and their families, remains poor. Multilevel interventions are necessary to better isolate the nature of toxicity from healthcare costs, along with standardization of their measurement, while prospectively evaluating potential solutions. For example, there are gaps in our knowledge of whether cardiologists or physicians caring for patients with ASCVD address the issue of cost in their medical decision‐making or in conversations with their patients. Professional societies such as the American College of Cardiology and the American Heart Association do not offer guidance on these challenges, and clinical practice guidelines do not incorporate cost considerations into a clinical care framework and patient‐centered decision‐making. 57 An example from another clinical specialty further highlights the challenges. One in 3 oncologists reports feeling uncomfortable or unable (or unprepared) to discuss costs with their patients. 58 This is despite over 2 decades of recognition of financial toxicity in oncology practices and the recognition of cost as an important component of patient care. 57 , 59 This further emphasizes the need for more training and education of our healthcare providers.
Patients' perceptions of cost discussions are also unclear, especially whether they would be a welcome relief or perceived as a barrier to high quality care. Discussions about costs can be embarrassing for patients, 60 who could feel subjected to social bias or stigma. 61 Hanmer and colleagues reported that a single question about difficulty paying monthly bills is more informative about health utility and costs than more complex questions exploring assets and income. 62 Bodenmann et al similarly found that a question on problems paying bills may help identify patients at risk of foregoing future care. 61 A systematic approach that incorporates costs of care assessments and considerations about financial toxicity in the clinical workflow aids in the identification of all who are vulnerable 63 , 64 , 65 Implementing this in clinical practice questionnaires or intake forms may be a practical first step. A more detailed evaluation may be targeted to those screened with this question of subjective financial toxicity from health care. 66 Moreover, studies, which have systematically evaluated costs and have monitored patient's perceptions, have found a positive influence on the patient–provider relationship, 67 , 68 , 69 , 70 , 71 , 72 in contrast to theoretical considerations regarding the negative effects of rapport. 73
A strategy has been implemented in oncology practices whereby the financial considerations of care are managed by the patient in consultation with a patient navigator distinct from the care team. 74 , 75 , 76 , 77 This model allows patients to address financial challenges with care with a member of the care team distinct from those team members making treatment decisions. Such a navigator can play a role in creating a framework of care with the healthcare team that minimizes the risk of financial toxicity from healthcare choices, especially where efficacious but lower cost alternatives exist, and for helping patients navigate these care decisions that align with their health as well as financial goals. 76
At a broader healthcare system level, the solution to financial toxicity likely would require policy reform, as the major goal would be to limit out‐of‐pocket expenditures, which should be scaled to the income of each patient. 26 Notably, since the passage of the Affordable Care Act, out‐of‐pocket health expenditures have improved. 78 However, given the substantial burden of expenses from maintaining insurance coverage, further interventions would need to be directed at improving the quality of insurance coverage. Although the majority of Americans are dealing with the realities of stagnant wage growth and limited savings/assets to cover these unexpected expenses, 79 , 80 the current trends toward greater cost‐sharing by payers in the form of higher deductibles and coinsurance will likely further exacerbate financial toxicity, especially for low‐income patients with ASCVD and their families.
Overall, a focus on costs may have positive implications for the health of our patients. Patients would likely benefit from discussions about unmet needs and financial matters in their clinical encounters, 81 as it may ensure wider compliance with evidence‐based medical therapies. Berkowitz et al demonstrated that focusing on patients' basic needs together with referral to a social program to help those who needed it, improved blood pressure and cholesterol levels among adults attending primary care clinics in Boston, Massachussets. 82 Similarly, the prevention of shock through early engagements in healthcare‐related financial considerations may avert morbidity and mortality from financially devastating events. 48 Further, a focus on prevention that only targets ASCVD and its risk factors will be ineffective as a population strategy unless it is paired with a focus on the prevention of financial toxicity from healthcare needs for this chronic condition, particularly among socioeconomically disadvantaged groups. 81 These issues are of particular relevance today as strategies focusing on the management of cardiovascular risk factors will continue to widen the financial and health divide between the vulnerable and the privileged, as the physical and mental health of the vulnerable is inextricably tied to their financial health. 46 , 83
In summary, financial toxicity among individuals with ASCVD and their families is an underrecognized, but highly prevalent condition, affecting millions of patients and their families. Despite improved health insurance coverage, patients continue to be inadequately protected from financial risk posed by healthcare costs. A substantial number of our patients are vulnerable. Multifaceted interventions are needed across the healthcare service spectrum with the goal to recognize these challenges early and pursue patient‐specific interventions that may help to alleviate this burden. Finally, health policy reform that ensures the protection of patients from healthcare costs is essential to ensure an equitable healthy future.
Sources of Funding
Dr Khera is supported by the National Center for Advancing Translational Sciences (grant UL1TR001105) of the National Institutes of Health. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosures
Dr Nasir is supported by the Jerold B. Katz Academy of Translational Research, and serves on the Advisory board for Amgen, Novartis and Esperion. The remaining authors have no disclosures to report.
(J Am Heart Assoc. 2020;9:e017793 DOI: 10.1161/JAHA.120.017793.)
For Sources of Funding and Disclosures, see page 8.
References
- 1. Khavjou OA, Phelps D, Leib A. Projections of cardiovascular disease prevalence and costs: 2015–2035. Available at: http://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_491513.pdf. Accessed August 2, 2018.
- 2. Abdus S, Selden TM, Keenan P. The financial burdens of high‐deductible plans. Health Aff (Millwood). 2016;35:2297–2301. [DOI] [PubMed] [Google Scholar]
- 3. Mazurenko O, Buntin MJB, Menachemi N. High‐deductible health plans and prevention. Annu Rev Public Health. 2019;40:411–421. [DOI] [PubMed] [Google Scholar]
- 4. Press VG, Gerald JK. High‐deductible health plans make the chronically ill pay more for less. Ann Am Thorac Soc. 2020;17:30–31. [DOI] [PubMed] [Google Scholar]
- 5. Miller GE, Vistnes JP, Rohde F, Keenan PS. High‐deductible health plan enrollment increased from 2006 to 2016, employer‐funded accounts grew in largest firms. Health Aff (Millwood). 2018;37:1231–1237. [DOI] [PubMed] [Google Scholar]
- 6. Khera R, Dharmarajan K, Wang Y, Lin Z, Bernheim SM, Wang Y, Normand ST, Krumholz HM. Association of the hospital readmissions reduction program with mortality during and after hospitalization for acute myocardial infarction, heart failure, and pneumonia. JAMA Netw Open. 2018;1:e182777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Khera R, Krumholz HM. Effects of the hospital readmissions reduction program. Circ Cardiovasc Qual Outcomes. 2018;11:e005083 DOI: 10.1161/CIRCOUTCOMES.118.005083. [DOI] [PubMed] [Google Scholar]
- 8. Khera R, Wang Y, Bernheim SM, Lin Z, Krumholz HM. Post‐discharge acute care and outcomes following readmission reduction initiatives: national retrospective cohort study of Medicare beneficiaries in the United States. BMJ. 2020;368:l6831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khera R, Wang Y, Nasir K, Lin Z, Krumholz HM. Evaluation of 30-day hospital readmission and mortality rates using regression‐discontinuity framework. J Am Coll Cardiol. 2019;74:219–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wadhera RK, Bhatt DL. Toward precision policy—the case of cardiovascular care. N Engl J Med. 2018;379:2193–2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320:2542–2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–117. [DOI] [PubMed] [Google Scholar]
- 13. Bernard DM, Johansson P, Fang Z. Out‐of‐pocket healthcare expenditure burdens among nonelderly adults with hypertension. Am J Manag Care. 2014;20:406–413. [PubMed] [Google Scholar]
- 14. Bernard D, Fang Z. Financial burdens and barriers to care among nonelderly adults with heart disease: 2010–2015. J Am Heart Assoc. 2019;8:e008831 DOI: 10.1161/JAHA.118.008831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khera R, Valero‐Elizondo J, Okunrintemi V, Saxena A, Das SR, de Lemos JA, Krumholz HM, Nasir K. Association of out‐of‐pocket annual health expenditures with financial hardship in low‐income adults with atherosclerotic cardiovascular disease in the United States. JAMA Cardiol. 2018;3:729–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shrime MG, Dare A, Alkire BC, Meara JG. A global country‐level comparison of the financial burden of surgery. Br J Surg. 2016;103:1453–1461. [DOI] [PubMed] [Google Scholar]
- 17. Altice CK, Banegas MP, Tucker‐Seeley RD, Yabroff KR. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109:djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cohen RA, Kirzinger WK. Financial burden of medical care: a family perspective. NCHS Data Brief. 2014;142:1–8. [PubMed] [Google Scholar]
- 19. Azzani M, Roslani AC, Su TT. The perceived cancer‐related financial hardship among patients and their families: a systematic review. Support Care Cancer. 2015;23:889–898. [DOI] [PubMed] [Google Scholar]
- 20. Gordon LG, Merollini KMD, Lowe A, Chan RJ. A systematic review of financial toxicity among cancer survivors: we can't pay the co‐pay. Patient. 2017;10:295–309. [DOI] [PubMed] [Google Scholar]
- 21. Jones SMW, Walker R, Fujii M, Nekhlyudov L, Rabin BA, Chubak J. Financial difficulty, worry about affording care, and benefit finding in long‐term survivors of cancer. Psychooncology. 2018;27:1320–1326. [DOI] [PubMed] [Google Scholar]
- 22. Valero‐Elizondo J, Salami JA, Ogunmoroti O, Osondu CU, Aneni EC, Malik R, Spatz ES, Rana JS, Virani SS, Blankstein R, et al. Favorable cardiovascular risk profile is associated with lower healthcare costs and resource utilization: the 2012 Medical Expenditure Panel Survey. Circ Cardiovasc Qual Outcomes. 2016;9:143–153. [DOI] [PubMed] [Google Scholar]
- 23. Valero‐Elizondo J, Khera R, Saxena A, Grandhi GR, Virani SS, Butler J, Samad Z, Desai NR, Krumholz HM, Nasir K. Financial hardship from medical bills among nonelderly U.S. adults with atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2019;73:727–732. [DOI] [PubMed] [Google Scholar]
- 24. Chen JE, Lou VW, Jian H, Zhou Z, Yan M, Zhu J, Li G, He Y. Objective and subjective financial burden and its associations with health‐related quality of life among lung cancer patients. Support Care Cancer. 2018;26:1265–1272. [DOI] [PubMed] [Google Scholar]
- 25. Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29:308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Miller GE, Sarpong EM, Hill SC. Does increased adherence to medications change health care financial burdens for adults with diabetes? J Diabetes. 2015;7:872–880. [DOI] [PubMed] [Google Scholar]
- 27. Cohen RA, Zammitti EP. Problems paying medical bills among persons under age 65: Early release of estimates from the National Health Interview Survey, 2011–June 2017. National Center for Health Statistics. 2017. Available from: https://www.cdc.gov/nchs/nhis/releases.htm. Accessed August 31, 2020.
- 28. Baird KE. Recent trends in the probability of high out‐of‐pocket medical expenses in the United States. SAGE Open Med. 2016;4:2050312116660329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kielb ES, Rhyan CN, Lee JA. Comparing health care financial burden with an alternative measure of unaffordability. Inquiry. 2017;54:46958017732960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mszar R, Grandhi GR, Valero‐Elizondo J, Caraballo C, Khera R, Desai N, Virani SS, Blankstein R, Blaha MJ, Nasir K. Cumulative burden of financial hardship from medical bills across the spectrum of diabetes mellitus and atherosclerotic cardiovascular disease among non‐elderly adults in the United States. J Am Heart Assoc. 2020;9:e015523 DOI: 10.1161/JAHA.119.015523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Khera R, Valero‐Elizondo J, Das SR, Virani SS, Kash BA, de Lemos JA, Krumholz HM, Nasir K. Cost‐related medication nonadherence in adults with atherosclerotic cardiovascular disease in the United States, 2013 to 2017. Circulation. 2019;140:2067–2075. [DOI] [PubMed] [Google Scholar]
- 32. Khera R, Hong JC, Saxena A, Arrieta A, Virani SS, Blankstein R, de Lemos JA, Krumholz HM, Nasir K. Burden of catastrophic health expenditures for acute myocardial infarction and stroke among uninsured in the United States. Circulation. 2018;137:408–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Collins SR, Bhupal HK, Doty MM.Health insurance coverage eight years after the ACA: fewer uninsured Americans and shorter coverage gaps, but more underinsured.
- 34. Saad L. More Americans Delaying Medical Treatment Due to Cost. 2019. Available at: https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx?utm_source=alert&utm_medium=email&utm_content=morelink&utm_campaign=syndication Accessed January 3, 2018.
- 35. Ramsey S, Blough D, Kirchhoff A, Kreizenbeck K, Fedorenko C, Snell K, Newcomb P, Hollingworth W, Overstreet K. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood). 2013;32:1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kent EE, Forsythe LP, Yabroff KR, Weaver KE, de Moor JS, Rodriguez JL, Rowland JH. Are survivors who report cancer‐related financial problems more likely to forgo or delay medical care? Cancer. 2013;119:3710–3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yabroff KR, Dowling EC, Guy GP Jr, Banegas MP, Davidoff A, Han X, Virgo KS, McNeel TS, Chawla N, Blanch‐Hartigan D, et al. Financial hardship associated with cancer in the United States: findings from a population‐based sample of adult cancer survivors. J Clin Oncol. 2016;34:259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hamel L, Norton M, Pollitz K, Levitt L, Claxton G, Brodie M. The burden of medical debt: results from the Kaiser Family Foundation/New York Times Medical Bills Survey. Henry J Kaiser Family Foundation; 2016. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2016/01/8806-the‐burden-of-medical-debt-results-from-the-kaiser-family-foundation-new-york-times-medical-bills-survey.pdf. Accessed July 15, 2018. [Google Scholar]
- 39. Davis K, Stremikis K, Doty MM, Zezza MA. Medicare beneficiaries less likely to experience cost- and access‐related problems than adults with private coverage. Health Aff (Millwood). 2012;31:1866–1875. [DOI] [PubMed] [Google Scholar]
- 40. Caraballo C, Valero‐Elizondo J, Khera R, Mahajan S, Grandhi GR, Virani SS, Mszar R, Krumholz HM, Nasir K. Burden and consequences of financial hardship from medical bills among nonelderly adults with diabetes mellitus in the United States. Circ Cardiovasc Qual Outcomes. 2020;13:e006139 DOI: 10.1161/CIRCOUTCOMES.119.006139 [DOI] [PubMed] [Google Scholar]
- 41. Charkhchi P, Fazeli Dehkordy S, Carlos RC. Housing and food insecurity, care access, and health status among the chronically ill: an analysis of the behavioral risk factor surveillance system. J Gen Intern Med. 2018;33:644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Knowles SR, Castle DJ, Biscan SM, Salzberg M, O'Flaherty EB, Langham R. Relationships between illness perceptions, coping and psychological morbidity in kidney transplants patients. Am J Med Sci. 2016;351:233–238. [DOI] [PubMed] [Google Scholar]
- 43. Han X, Lin CC, Li C, de Moor JS, Rodriguez JL, Kent EE, Forsythe LP. Association between serious psychological distress and health care use and expenditures by cancer history. Cancer. 2015;121:614–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Okunrintemi V, Valero‐Elizondo J, Michos ED, Salami JA, Ogunmoroti O, Osondu C, Tibuakuu M, Benson EM, Pawlik TM, Blaha MJ, et al. Association of depression risk with patient experience, healthcare expenditure, and health resource utilization among adults with atherosclerotic cardiovascular disease. J Gen Intern Med. 2019;34:2427–2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Xiang X, Larrison CR, Tabb KM. Trends in health care utilization among adults with serious psychological distress: 2003–2014. Psychiatr Serv. 2016;67:743–748. [DOI] [PubMed] [Google Scholar]
- 46. Annapureddy A, Valero‐Elizondo J, Khera R, Grandhi GR, Spatz ES, Dreyer RP, Desai NR, Krumholz HM, Nasir K. Association between financial burden, quality of life, and mental health among those with atherosclerotic cardiovascular disease in the United States. Circ Cardiovasc Qual Outcomes. 2018;11:e005180 DOI: 10.1161/CIRCOUTCOMES.118.005180 [DOI] [PubMed] [Google Scholar]
- 47. Lentz R, Benson AB III, Kircher S. Financial toxicity in cancer care: prevalence, causes, consequences, and reduction strategies. J Surg Oncol. 2019;120:85–92. [DOI] [PubMed] [Google Scholar]
- 48. Pool LR, Burgard SA, Needham BL, Elliott MR, Langa KM, Mendes de Leon CF. Association of a negative wealth shock with all‐cause mortality in middle‐aged and older adults in the United States. JAMA. 2018;319:1341–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McElfish PA, Long CR, Payakachat N, Felix H, Bursac Z, Rowland B, Hudson JS, Narcisse MR. Cost‐related nonadherence to medication treatment plans: Native Hawaiian and Pacific Islander National Health Interview Survey, 2014. Med Care. 2018;56:341–349. [DOI] [PubMed] [Google Scholar]
- 50. Marcum ZA, Zheng Y, Perera S, Strotmeyer E, Newman AB, Simonsick EM, Shorr RI, Bauer DC, Donohue JM, Hanlon JT. Prevalence and correlates of self‐reported medication non‐adherence among older adults with coronary heart disease, diabetes mellitus, and/or hypertension. Res Social Adm Pharm. 2013;9:817–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kang H, Lobo JM, Kim S, Sohn MW. Cost‐related medication non‐adherence among U.S. adults with diabetes. Diabetes Res Clin Pract. 2018;143:24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Patel MR, Piette JD, Resnicow K, Kowalski‐Dobson T, Heisler M. Social determinants of health, cost‐related nonadherence, and cost‐reducing behaviors among adults with diabetes: findings from the National Health Interview Survey. Med Care. 2016;54:796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kaul S, Avila JC, Mehta HB, Rodriguez AM, Kuo YF, Kirchhoff AC. Cost‐related medication nonadherence among adolescent and young adult cancer survivors. Cancer. 2017;123:2726–2734. [DOI] [PubMed] [Google Scholar]
- 54. Osborn CY, Kripalani S, Goggins KM, Wallston KA. Financial strain is associated with medication nonadherence and worse self‐rated health among cardiovascular patients. J Health Care Poor Underserved. 2017;28:499–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ford ES. Food security and cardiovascular disease risk among adults in the United States: findings from the National Health and Nutrition Examination Survey, 2003–2008. Prev Chronic Dis. 2013;10:E202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Leung C, Tester J, Laraia B. Household food insecurity and ideal cardiovascular health factors in US adults. JAMA Intern Med. 2017;177:730–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping‐up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68:153–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Schrag D, Hanger M. Medical oncologists' views on communicating with patients about chemotherapy costs: a pilot survey. J Clin Oncol. 2007;25:233–237. [DOI] [PubMed] [Google Scholar]
- 59. Cagle JG, Carr DC, Hong S, Zimmerman S. Financial burden among US households affected by cancer at the end of life. Psychooncology. 2016;25:919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zafar SY, Newcomer LN, McCarthy J, Fuld Nasso S, Saltz LB. How should we intervene on the financial toxicity of cancer care? One shot, four perspectives. Am Soc Clin Oncol Educ Book. 2017;37:35–39. [DOI] [PubMed] [Google Scholar]
- 61. Bodenmann P, Favrat B, Wolff H, Guessous I, Panese F, Herzig L, Bischoff T, Casillas A, Golano T, Vaucher P. Screening primary‐care patients forgoing health care for economic reasons. PLoS One. 2014;9:e94006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hanmer J, Cherepanov D. A single question about a respondent's perceived financial ability to pay monthly bills explains more variance in health utility scores than absolute income and assets questions. Qual Life Res. 2016;25:2233–2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Henrikson NB, Banegas MP, Tuzzio L, Lim C, Schneider JL, Walsh‐Bailey C, Scrol A, Hodge SM. Workflow requirements for cost‐of‐care conversations in outpatient settings providing oncology or primary care: a qualitative, human‐centered design study. Ann Intern Med. 2019;170:S70–S78. [DOI] [PubMed] [Google Scholar]
- 64. Henrikson NB, Banegas MP, Tuzzio L, Lim C, Schneider JL, Walsh‐Bailey C, Scrol A, Hodge SM. Clinical workflows to support cost‐of‐care conversations: multisite design study. J Clin Oncol. 2018;36:168–168.29220292 [Google Scholar]
- 65. Sloan CE, Ubel PA. The 7 habits of highly effective cost‐of‐care conversations. Ann Intern Med. 2019;170:S33–S35. [DOI] [PubMed] [Google Scholar]
- 66. Dine CJ, Masi D, Smith CD. Tools to help overcome barriers to cost‐of‐care conversations. Ann Intern Med. 2019;170:S36–S38. [DOI] [PubMed] [Google Scholar]
- 67. Irwin B, Kimmick G, Altomare I, Marcom PK, Houck K, Zafar SY, Peppercorn J. Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist. 2014;19:1135–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Henrikson NB, Chang E, Ulrich K, King D, Anderson ML. Communication with physicians about health care costs: survey of an insured population. Perm J. 2017;21:16–070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Hardee JT, Platt FW, Kasper IK. Discussing health care costs with patients: an opportunity for empathic communication. J Gen Intern Med. 2005;20:666–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Meisenberg BR, Varner A, Ellis E, Ebner S, Moxley J, Siegrist E, Weng D. Patient attitudes regarding the cost of illness in cancer care. Oncologist. 2015;20:1199–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bradham DD, Garcia D, Galvan A, Erb C. Cost‐of‐care conversations during clinical visits in federally qualified health centers: an observational study. Ann Intern Med. 2019;170:S87–S92. [DOI] [PubMed] [Google Scholar]
- 72. Perez SL, Weissman A, Read S, Smith CD, Colello L, Peter D, Nickel WUS. Internists' perspectives on discussing cost of care with patients: structured interviews and a survey. Ann Intern Med. 2019;170:S39–S45. [DOI] [PubMed] [Google Scholar]
- 73. McGraw AP, Tetlock PE. Taboo trade‐offs, relational framing, and the acceptability of exchanges. J Consum Psychol. 2005;15:2–15. [Google Scholar]
- 74. Spencer JC, Samuel CA, Rosenstein DL, Reeder‐Hayes KE, Manning ML, Sellers JB, Wheeler SB. Oncology navigators' perceptions of cancer‐related financial burden and financial assistance resources. Support Care Cancer. 2018;26:1315–1321. [DOI] [PubMed] [Google Scholar]
- 75. Yezefski T, Steelquist J, Watabayashi K, Sherman D, Shankaran V. Impact of trained oncology financial navigators on patient out‐of‐pocket spending. Am J Manag Care. 2018;24:S74–S79. [PubMed] [Google Scholar]
- 76. Shankaran V, Leahy T, Steelquist J, Watabayashi K, Linden H, Ramsey S, Schwartz N, Kreizenbeck K, Nelson J, Balch A, et al. Pilot feasibility study of an oncology financial navigation program. J Oncol Pract. 2018;14:e122–e129. [DOI] [PubMed] [Google Scholar]
- 77. Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, Abernethy AP. The financial toxicity of cancer treatment: a pilot study assessing out‐of‐pocket expenses and the insured cancer patient's experience. Oncologist. 2013;18:381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Goldman AL, Woolhandler S, Himmelstein DU, Bor DH, McCormick D. Out‐of‐pocket spending and premium contributions after implementation of the affordable care act. JAMA Intern Med. 2018;178:347–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Minarik J.Healthcare costs, wage growth, and inequality. Available at: https://www.ced.org/blog/entry/healthcare-costs-wage‐growth‐and‐inequality. Accessed February 24, 2020.
- 80. Rae M, Copeland R, Cox C. Tracking the rise in premium contributions and cost‐sharing for families with large employer coverage. 2019. Available at: https://www.healthsystemtracker.org/brief/tracking‐the‐rise‐in‐premium‐contributions‐and‐cost‐sharing‐for‐families‐with‐large-employer‐coverage/. Accessed February 24, 2020.
- 81. Woolf SH, Purnell JQ. The good life: working together to promote opportunity and improve population health and well‐being. JAMA. 2016;315:1706–1708. [DOI] [PubMed] [Google Scholar]
- 82. Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Agarwal S, Sud K, Thakkar B, Menon V, Jaber WA, Kapadia SR. Changing trends of atherosclerotic risk factors among patients with acute myocardial infarction and acute ischemic stroke. Am J Cardiol. 2017;119:1532–1541. [DOI] [PubMed] [Google Scholar]


