Abstract
Contrast-enhanced computed tomography (CECT) is commonly used for staging and diagnosing recurrent gastric cancer. Recently, 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET)/CT gained popularity as a diagnostic tool owing to advantages including dual functional and anatomical imaging, which may facilitate early diagnosis. The diagnostic performance of 18F-FDG PET/CT and CECT has been assessed in several studies but with variable results. Therefore, the present meta-analysis aimed to evaluate the accuracy of 18F-FDG PET/CT and CECT for primary TNM staging and the diagnosis of recurrent gastric cancers. A systematic search of the PubMed Central, Medline, Scopus, Cochrane and Embase databases from inception until January 2020 was performed. The Quality Assessment of Diagnostic Accuracy Study-2 tool was used to determine the quality of the selected studies. Pooled estimates of sensitivity and specificity were calculated. A total of 58 studies comprising 9,997 patients were included. Most studies had a low risk of bias. The sensitivity and specificity for nodal staging of gastric cancer were 49% (95% CI, 37-61%) and 92% (95% CI, 86-96%) for 18F-FDG PET/CT, respectively, and 67% (95% CI, 57-76%) and 86% (95% CI, 81-89%) for CECT, respectively. For metastasis staging, the sensitivity and specificity were 56% (95% CI, 40-71%) and 97% (95% CI, 87-99%) for 18F-FDG PET/CT, respectively, and 59% (95% CI, 41-75%) and 96% (95% CI, 83-99%) for CECT, respectively. For diagnosing cancer recurrence, the pooled sensitivity and specificity were 81% (95% CI, 72-88%) and 83% (95% CI, 74-89%) for 18F-FDG PET/CT, respectively, and 59% (95% CI, 41-75%) and 96% (95% CI, 83-99%) for CECT, respectively. Both 18F-FDG PET/CT and CECT were deemed highly useful for diagnosing recurrent gastric cancer due to their high sensitivities and specificities. However, these techniques cannot be used to exclude or confirm the presence of lymph node metastases or recurrent gastric cancer tumors, but can be used for the confirmation of distal metastasis.
Keywords: gastric cancer, meta-analysis, metastasis, TNM staging, validation studies
Introduction
The global burden of gastric cancer has drastically decreased over the last few decades (1). However, the disease remains a leading cause of cancer-associated mortality with an overall poor prognosis (2,3). One of the major factors increasing the mortality of gastric cancer is late diagnosis. It is estimated that ~80% of cases are diagnosed in the late stages of malignancy (1,3). Thus, early and accurate diagnosis along with appropriate TNM staging of all the gastric cancers is essential (4-7). Early detection enables the clinician to appropriately select the treatment strategy and correctly predict overall prognosis (8).
Several imaging modalities, including endoscopic ultrasound (EUS), contrast-enhanced computed tomography (CECT), magnetic resonance imaging (MRI) and 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET)/CT may be used for the diagnosis and TNM staging of gastric cancers (9). However, no specific guidelines exist regarding the most appropriate diagnostic modality for the staging of gastric cancer (10). In addition, there are limitations to each diagnostic tool for assessing gastric cancer. EUS cannot be used to evaluate the greater curvature wall, the fundus or the lymphatic spread (11,12) and it is highly dependent on the body habitus of the patient (13). CECT scans have limitations detecting flat lesions and feature poor contrast resolution for soft tissues (14,15). This may result in inaccurate assessments of lymph nodes, as CECT cannot detect microscopic nodal invasion and cannot exclude malignancy from normal large reactive nodes (14). MRI also has limitations including respiratory motion artifacts, high costs, long examination times and lack of standard gastric cancer protocols (16,17). Furthermore, nodal assessments via MRI are also limited by size criteria and the body coverage of a single examination is not suitable for metastasis staging (18). 18F-FDG PET/CT is a semi-quantitative method that assesses the FDG uptake in gastric tumors (19). However, standardized uptake values depend on numerous factors, including the time interval post-FDG injection, tumor size, technical parameters and normoglycemia (20,21). In addition, uptake values vary with pathological cancer types and mucinous cancers may provide false-negative results (22).
Such limitations associated with each imaging modality preclude the accurate preoperative staging of gastric cancer. Furthermore, ~50% of patients with advanced gastric cancers develop recurrences after treatment (23,24). Early detection of recurrence is also essential to reduce mortality associated with the disease. Out of the several imaging modalities, CECT and 18F-FDG PET/CT have been commonly used for the diagnosis and staging of gastric cancer. Studies have assessed the accuracy of each imaging tool in different settings with variable results. There is a requirement for high-quality evidence to determine the accuracy of these imaging modalities to guide clinical practice. Hence, the present systematic review and meta-analysis was performed to assess the accuracy of the diagnostic performance of 18F-FDG PET/CT and CECT for TNM staging of primary tumors and diagnosis of recurrences in patients with gastric cancer.
Materials and methods
Inclusion criteria
All types of studies examining the accuracy of CECT or 18F-FDG PET/CT for diagnosing and staging primary and recurrent gastric cancer were included. Studies were to compare the diagnostic accuracy of 18F-FDG PET/CT or CECT (screening tests) with the histopathological examination result, which was considered the ‘reference standard’. Full-text articles that reported on the sensitivity and specificity or provided information to calculate these values were included. Studies with sample sizes of <10 patients were excluded.
Search strategy
A systematic electronic search was performed in the databases PubMed Central, Medline, Scopus, Cochrane Library and Embase. The following medical subject headings and free-text terms were used for the search: ‘Validation studies’, ‘gastric carcinoma’, ‘staging’, ‘prognosis’, ‘gastric cancer’, ‘recurrence’, ‘sensitivity’, ‘specificity’, ‘diagnosis’, ‘computed tomography’, ‘positron emission tomography’, ‘fluorodeoxyglucose’ and ‘diagnostic accuracy studies’. The search included entries from the inception of the databases up to 1st January 2020 without any language restrictions. The reference lists of primary trials were also examined to further identify any relevant articles for inclusion in the present review.
Selection of studies
A total of two authors (ZZ and BZ) independently performed the primary screening of titles, key words and abstracts. Full texts of relevant studies were then retrieved. Secondary screening of the retrieved articles was then performed to select studies meeting the inclusion criteria. All disagreements were resolved in discussion with a third investigator (WC).
Data extraction and management
The primary investigators (ZZ and BZ) extracted the relevant data from the studies, which included the following: Study setting, design, inclusion and exclusion criteria, sample size, comorbidities, the mean age of participants, index test, and sensitivity and specificity values of the imaging modality. The data extracted were double-checked during the review and the study reports to ensure correctness. The study outcomes were as follows: Sensitivity, specificity, diagnostic odds ratio (DOR), positive likelihood ratio (LR+), negative likelihood ratio (LR-).
Risk of bias assessment
The Quality Assessment of Diagnostic Accuracy Studies-2 tool was used to assess the risk of bias for each study (25). The tool comprises the following domains: Patient selection bias, conduct and interpretation of index tests and reference standards, as well as time interval of outcome assessments. The studies in each domain were graded as having unclear, high or low risk of bias.
Statistical analysis
The present meta-analysis was performed using the STATA 14.2 software (StataCorp). The pooled values for sensitivity, specificity, LR-, LR+ and DOR for each the 18F-FDG PET/CT and the CECT imaging techniques were obtained using the bivariate meta-analysis method. A summary receiver operating characteristic (SROC) curve was generated and the area under the curve (AUC) was obtained. An AUC value closer to 1 indicated better diagnostic accuracy. Study-specific and pooled values of sensitivity and specificity were graphically represented using forest plots. The clinical values for both 18F-FDG PET/CT and CECT were determined by generating LR scattergrams. In addition, the probability that a patient with gastric cancer had nodal or distant metastases or recurrences was tested using Fagan plots. Bivariate boxplots were generated and heterogeneity was tested using the χ2 and I2 statistics (I2<25%, mild; I2=25-75%, moderate; and I2>75%, substantial heterogeneity). Publication bias was assessed graphically by funnel plots and also by Deek's test. The ‘Midas’ command package in STATA 14.2 software (StataCorp, LP) was used for all analyses.
Results
Selection of studies
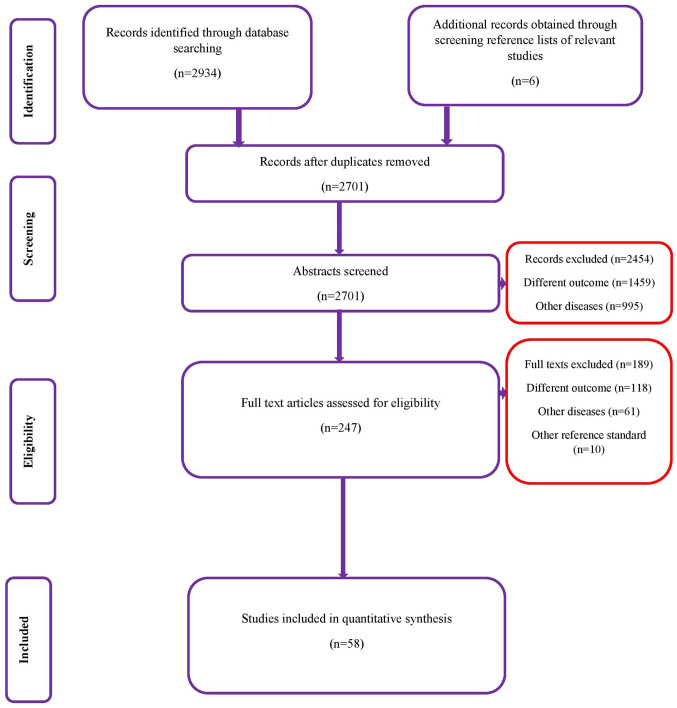
In the database search, a total of 2,934 records were identified, of which, 1,388 studies were from Medline, 880 from Scopus, 557 from Embase and 109 from the Cochrane library. After the first stage of screening, 247 studies were retrieved based on relevance. The full texts of these articles were extracted and it was assessed whether they fulfilled the inclusion criteria. Finally, a total of 58 studies met the inclusion criteria and were included in the review (Fig. 1).
Figure 1.
Search strategy.
Characteristics of the included studies
Table I lists the characteristics of the included studies (14,23,26-81). The majority of them (37/58) were retrospective in nature. Data from a total of 9,997 participants were analyzed in the included studies. The sample sizes of individual studies varied from 18 to 1,964 patients. All of the included studies used histopathology as the reference standard. Among the studies using 18F-FDG PET/CT as the index test, 11 reported data on lymph node metastases and 8 reported on distant metastases, while 16 reported on the accuracy of the imaging modality for detecting recurrent gastric cancer tumors. Among the studies using CECT as the index test, 37 studies reported data on lymph node metastases, 7 on distant metastasis and 4 on recurrent gastric cancer tumors.
Table I.
Characteristics of the included studies (n=58).
| Study number | First author and year | Country | Study design | Sample size | Type of diagnostic modality | Gold standard comparator | Outcomes reported | Sensitivity and specificity | (Refs) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Ahn et al, 2009 | South Korea | Retrospective | 434 | CECT | Histopathology | Lymph node metastasis | Sensitivity=17.0% Specificity=91.6% | (26) |
| 2 | Bilici et al, 2011 | Turkey | Retrospective | 34 | 18F-FDG PET/CT and CECT | Histopathology | Recurrent gastric cancer | Sensitivity (FDG-PET)=95.8% Specificity (FDG-PET)=100.0% Sensitivity (CECT)=62.5% Specificity (CECT)=100.0% | (27) |
| 3 | Blackshaw et al, 2003 | United Kingdom | Prospective | 100 | CECT | Histopathology | Distant metastasis | Sensitivity (CECT)=46.2% Specificity (CECT)=100.0% | (28) |
| 4 | Bosch et al, 2020 | United Kingdom | Retrospective | 105 | CECT | Histopathology | Distant metastasis | Sensitivity (CECT)=40.0% Specificity (CECT)=73.3% | (29) |
| 5 | Cayvarlı et al, 2014 | Turkey | Retrospective | 130 | 18F-FDG PET/CT and CECT | Histopathology | Recurrent gastric cancer | Sensitivity=91.2% Specificity=61.5% | (30) |
| 6 | Chen et al, 2005 | South Korea | Prospective | 68 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node and distant metastasis | FDG PET (LN): Sensitivity=56.0% Specificity=92.0% FDG PET (Distant): Sensitivity=30.0% Specificity=98.0% CECT (Distant): Sensitivity=80.0% Specificity=91.0% CECT (LN): Sensitivity=78.0% Specificity=61.0% | (31) |
| 7 | Chen et al, 2007 | Taiwan | Retrospective | 64 | CECT | Histopathology | Lymph node metastasis | Sensitivity=88.0% Specificity=80.0% | (32) |
| 8 | Chen et al, 2006 | Taiwan | Prospective study | 55 | CECT | Histopathology | Lymph node metastasis | Sensitivity=86.0% Specificity=77.0% | (14) |
| 9 | De Potter et al, 2002 | Belgium | Retrospective study | 33 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=70.0% Specificity=69.0% | (33) |
| 10 | D'Elia F et al, 2000 | Italy | Prospective | 107 | CECT | Histopathology | Lymph node metastasis | Sensitivity=97.0% Specificity=65.0% | (34) |
| 11 | Feng et al, 2013 | China | Prospective | 610 | CECT | Histopathology | Lymph node metastasis | Sensitivity=84.9% Specificity=61.0% | (35) |
| 12 | Filik et al, 2015 | Turkey | Retrospective | 25 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node metastasis | FDG PET: Sensitivity=82.0% Specificity=75.0% CECT: Sensitivity=64.0% Specificity=100.0% | (36) |
| 13 | Fujikawa et al, 2014 | Japan | Prospective | 525 | CECT | Histopathology | Lymph node metastasis | Sensitivity=4.0% Specificity=98.0% | (37) |
| 14 | Giganti et al, 2016 | Italy | Prospective | 55 | CECT | Histopathology | Lymph node metastasis | Sensitivity=90.0% Specificity=91.0% | (38) |
| 15 | Graziosi et al, 2011 | Italy | Retrospective | 50 | 18F-FDG PET/CT and CECT | Histopathology | Recurrent gastric cancer | Sensitivity=89.0% Specificity=85.0% | (39) |
| 16 | Ha et al, 2011 | South Korea | Retrospective | 78 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node metastasis | FDG PET: Sensitivity=89.0% Specificity=85.0% CECT: Sensitivity=69.0% Specificity=86.0% | (40) |
| 17 | Hasegawa et al, 2013 | Japan | Prospective | 315 | CECT | Histopathology | Lymph node metastasis | Sensitivity=46.4% Specificity=96.0% | (41) |
| 18 | Hwang et al, 2010 Korea | South | Prospective | 247 | CECT | Histopathology | Lymph node metastasis | Sensitivity=44.5% Specificity=85.3% | (42) |
| 19 | Jadvar et al, 2003 | United States of America | Retrospective | 18 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=77.7% Specificity=77.7% | (43) |
| 20 | Joo et al, 2015 | South Korea | Prospective | 47 | CECT | Histopathology | Lymph node metastasis | Sensitivity=43.3% Specificity=100.0% | (44) |
| 21 | Karakoyun et al, 2014 | Turkey | Prospective | 55 | CECT | Histopathology | Lymph node metastasis | Sensitivity=97.5% Specificity=73.3% | (45) |
| 22 | Kawanaka et al, 2016 | Japan | Retrospective study | 101 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node and distant metastasis | FDG PET (LN): Sensitivity=80.0% Specificity=70.0% CECT (Distant): Sensitivity=75.0% Specificity=97.0% FDG PET (Distant): Sensitivity=81.0% Specificity=100.0% CECT (LN): Sensitivity=84.0% Specificity=70.0% | (46) |
| 23 | Kim et al, 2005 | South Korea | Prospective | 106 | CECT | Histopathology | Lymph node metastasis | Sensitivity=71.7% Specificity=63.3% | (47) |
| 24 | Kim et al, 2009 | South Korea | Retrospective | 102 | CECT | Histopathology | Lymph node metastasis | Sensitivity=50.0% Specificity=91.0% | (48) |
| 25 | Kim et al, 2011 | South Korea | Retrospective | 71 | 18F-FDG PET/CT | Histopathology | Lymph node metastasis and recurrent gastric cancer | Lymph node metastasis: Sensitivity=40.0% Specificity=100.0% Recurrent gastric cancer: Sensitivity=51.0% Specificity=84.0% | (49) |
| 26 | Kim et al, 2013 | South Korea | Retrospective | 171 | CECT | Histopathology | Lymph node metastasis | Sensitivity=60.0% Specificity=89.0% | (50) |
| 27 | Kim et al, 2017 | South Korea | Retrospective | 600 | CECT | Histopathology | Recurrent gastric cancer | Sensitivity=75.9% Specificity=98.4% | (51) |
| 28 | Kudou et al, 2018 | Japan | Retrospective | 117 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node and distant metastasis | FDG PET (LN): Sensitivity=22.6% Specificity=90.0% CECT (Distant): Sensitivity=60.8% Specificity=67.6% FDG PET (Distant): Sensitivity=80.0% Specificity=64.0% CECT (LN): Sensitivity=52.0% Specificity=71.0% | (52) |
| 29 | Lee et al, 2010 | South Korea | Retrospective | 148 | CECT | Histopathology | Lymph node metastasis | Sensitivity=26.3% Specificity=98.8% | (53) |
| 30 | Lee et al, 2011 | South Korea | Retrospective | 93 | 18F-FDG PET/CT and CECT | Histopathology | Recurrent gastric cancer | FDG PET: Sensitivity=42.0% Specificity=57.0% CECT: Sensitivity=85.0% Specificity=87.0% | (54) |
| 31 | Lee et al, 2014 | South Korea | Retrospective | 46 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=100.0% Specificity=88.0% | (55) |
| 32 | Lim et al, 2006 | South Korea | Retrospective | 112 | CECT | Histopathology | Lymph node and distant metastasis | Sensitivity=35.0% Specificity=98.9% | (56) |
| 33 | Marrelli et al, 2011 | Italy | Prospective | 92 | CECT | Histopathology | Lymph node metastasis | Sensitivity=84.6% Specificity=95% | (57) |
| 34 | Mochiki et al, 2004 | Japan | Prospective | 85 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node metastasis | FDG PET: Sensitivity=35.0% Specificity=100.0% CECT: Sensitivity=65.0% Specificity=77.0% | (23) |
| 35 | Nakamoto et al, 2009 | Japan | Retrospective | 92 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=77.2% Specificity=91.7% | (58) |
| 36 | Namikawa et al, 2014 | Japan | Retrospective | 90 | 18F-FDG PET/CT | Histopathology | Lymph node metastasis | Sensitivity=64.0% Specificity=85.0% | (59) |
| 37 | Pan et al, 2013 | China | Prospective | 96 | CECT | Histopathology | Lymph node metastasis | Sensitivity=91.0% Specificity=60.0% | (60) |
| 38 | Park et al, 2009 | South Korea | Retrospective | 105 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=74.0% Specificity=76.0% | (61) |
| 39 | Park et al, 2010 | South Korea | Retrospective | 1964 | CECT | Histopathology | Lymph node metastasis | Sensitivity=57.0% Specificity=80.0% | (62) |
| 40 | Park et al, 2014 | South Korea | Retrospective | 74 | CECT | Histopathology | Lymph node metastasis | Sensitivity=51.0% Specificity=81.0% | (63) |
| 41 | Perlaza et al, 2018 | Spain | Prospective | 50 | 18F-FDG PET/CT and CECT | Histopathology | Distant metastasis | FDG PET: Sensitivity=63.0% Specificity=92.0% CECT: Sensitivity=65.0% Specificity=100.0% | (64) |
| 42 | Ren et al, 2007 | China | Retrospective | 77 | CECT | Histopathology | Lymph node metastasis | Sensitivity=83.0% Specificity=75.0% | (65) |
| 43 | Saito et al, 2015 | Japan | Retrospective | 90 | CECT | Histopathology | Lymph node metastasis | Sensitivity=55.0% Specificity=86.0% | (66) |
| 44 | Sharma et al, 2012 | India | Retrospective | 93 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=95.0% Specificity=79.0% | (67) |
| 45 | Shinohara et al, 2005 | Japan | Prospective | 451 | CECT | Histopathology | Lymph node metastasis | Sensitivity=67.0% Specificity=90.0% | (68) |
| 46 | Sim et al, 2009 | South | Retrospective Korea | 52 | 18F-FDG PET/CT | Histopathology and CECT | Recurrent gastric cancer | FDG PET: Sensitivity=68.0% Specificity=71.0% CECT: Sensitivity=89.0% Specificity=64.0% | (69) |
| 47 | Smyth et al, 2012 | United States of America | Prospective | 113 | 18F-FDG PET/CT | Histopathology | Distant metastasis | Sensitivity=35.0% Specificity=98.7% | (70) |
| 48 | Stell et al, 1996 | United Kingdom | Prospective | 65 | CECT | Histopathology | Lymph node and distant metastasis | LN: Sensitivity=26.0% Specificity=100.0% Distant: Sensitivity=7.6% Specificity=100.0% | (71) |
| 49 | Sun et al, 2008 | China | Retrospective | 23 | 18F-FDG PET/CT | Histopathology | Distant metastasis | Sensitivity=85.0% Specificity=77.7% | (72) |
| 50 | Tsujimoto et al, 2010 | Japan | Prospective | 205 | 18F-FDG PET/CT | Histopathology | LN metastasis | Sensitivity=21.0% Specificity=89.0% | (73) |
| 51 | Turlakow A et al, 2003 | United States of America | Retrospective | 37 | 18F-FDG PET/CT | Histopathology | Distant metastasis | Sensitivity=56.0% Specificity=93.0% | (74) |
| 52 | Yan et al, 2009 | China | Prospective | 670 | CECT | Histopathology | Lymph node metastasis | Sensitivity=86.0% Specificity=76.0% | (75) |
| 53 | Yan et al, 2010 | China | Prospective | 61 | CECT | Histopathology | Lymph node metastasis | Sensitivity=77.0% Specificity=73.0% | (76) |
| 54 | Yang et al, 2008 | Japan | Retrospective | 44 | CECT | Histopathology | Lymph node metastasis | Sensitivity=84.0% Specificity=84.0% | (77) |
| 55 | Yoon et al, 2012 | South Korea | Retrospective | 372 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node metastasis | FDG PET: Sensitivity=59.0% Specificity=88.0% CECT: Sensitivity=70.0% Specificity=82.0% | (78) |
| 56 | Yun et al, 2005 | South Korea | Retrospective | 30 | 18F-FDG PET/CT | Histopathology | Recurrent gastric cancer | Sensitivity=94.0% Specificity=69.0% | (79) |
| 57 | Yun et al, 2005 | South Korea | Retrospective | 81 | 18F-FDG PET/CT and CECT | Histopathology | Lymph node metastasis | FDG PET: Sensitivity=50.0% Specificity=98.0% CECT: Sensitivity=50.0% Specificity=98.0% | (80) |
| 58 | Zhong et al, 2012 | China | Retrospective | 115 | CECT | Histopathology | Lymph node metastasis | Sensitivity=87.0% Specificity=75.0% | (81) |
CECT, contrast-enhanced computed tomography; 18F-FDG PET, 18F-fluorodeoxyglucose positron emission tomography.
Methodological quality
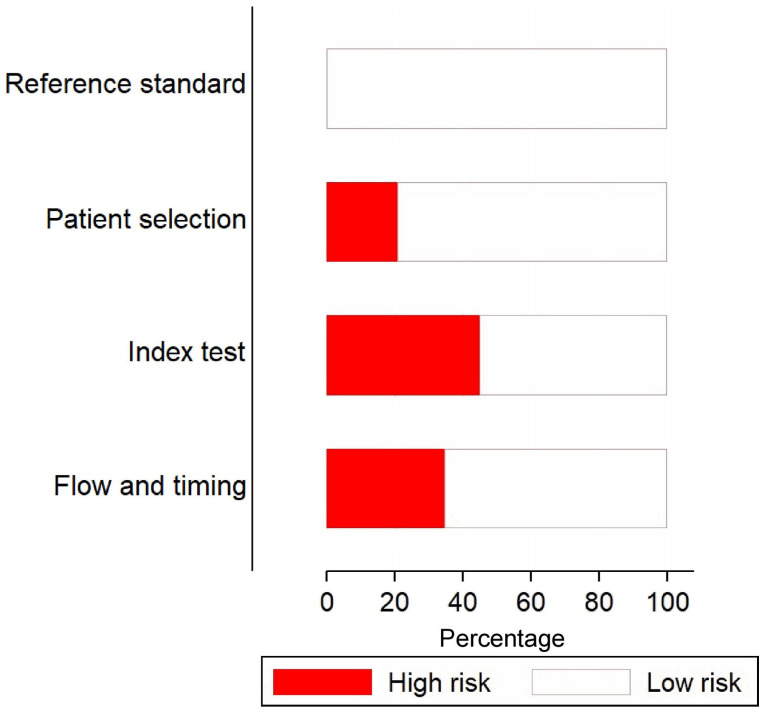
Fig. 2 depicts the risk of bias assessments for the included studies. A high risk of patient selection bias was present in almost 20% of the studies. Furthermore, >40% of the studies had a high risk of bias for conduct and interpretation of the index test. All of the studies had a low risk of bias for conduct and interpretation of reference standards. In addition, ~70% of the studies had low risks of bias for patient flow and interval between index tests and reference standards.
Figure 2.
Quality assessment for the included studies (n=59) using the Quality Assessment of Diagnostic Accuracy Study-2 tool.
Diagnostic performance of 18F-FDG PET/CT Lymph node metastasis
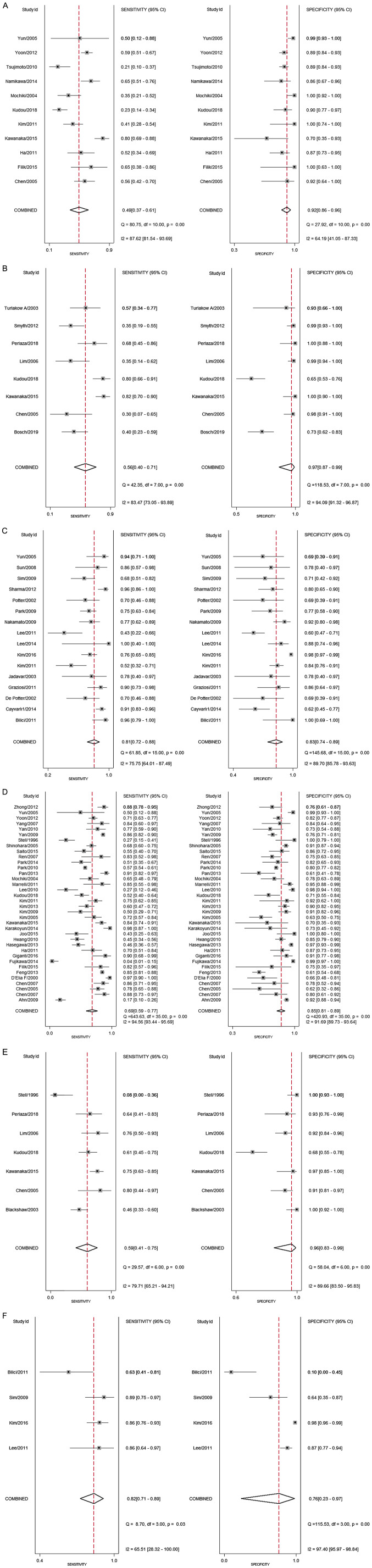
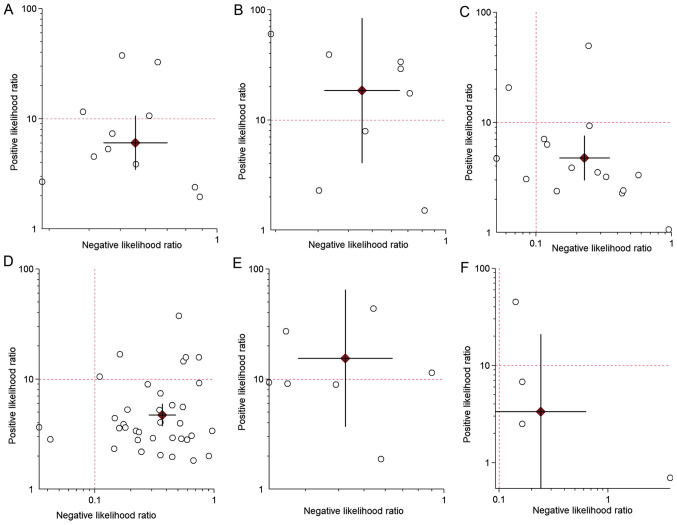
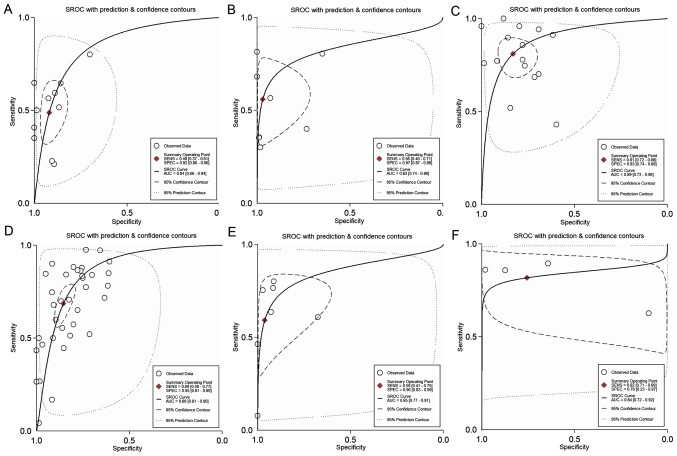
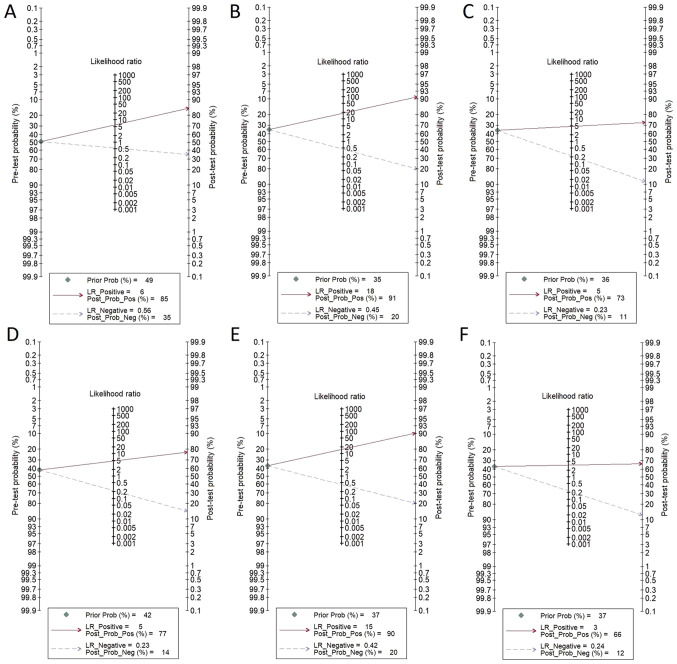
Overall, 11 studies evaluated the accuracy of 18F-FDG PET/CT for diagnosing lymph node metastases (N staging) among patients with gastric cancer. The pooled sensitivity and specificity were 49% (95% CI, 37-61%) and 92% (95% CI, 86-96%), respectively (Fig. 3). The DOR was 11 (95% CI, 6-21). The LR+ was 6.1 (95% CI, 3.5-10.6) and the LR- was 0.56 (0.44-0.70). The LR+ and LR- values were in the right lower quadrant of the LR scattergram, indicating that the 18F-FDG PET/CT cannot be used for confirmation or exclusion (Fig. 4). Fig. 5 presents the SROC curve for diagnosing nodal metastases using 18F-FDG PET/CT. The AUC was 0.84 (95% CI, 0.66-0.94), indicating a high diagnostic performance for 18F-FDG PET/CT. Fagan's nomogram indicated an average clinical utility of 18F-FDG PET/CT for diagnosing nodal metastasis, as the post-test probability (positive, 85%; negative, 35%) differed slightly from the pre-test probability (49%; Fig. 6).
Figure 3.
Pooled sensitivities and specificities of different imaging techniques for malignancy detection in patients with gastric cancer. Forest plot indicating the pooled sensitivity and specificity of (A) FDG PET for lymph node metastasis; (B) FDG PET for distant metastasis; (C) FDG PET for recurrent gastric cancer; (D) CECT for lymph node metastasis; (E) CECT for distant metastasis; and (F) CECT for recurrent gastric cancer. CECT, contrast-enhanced computed tomography; FDG PET, fluorodeoxyglucose positron emission tomography; df, degrees of freedom.
Figure 4.
Likelihood scattergrams. Scatter plots of (A) FDG PET for lymph node metastasis; (B) FDG PET for distant metastasis; (C) FDG PET for recurrent gastric cancer; (D) CECT for lymph node metastasis; (E) for CECT on distant metastasis; and (F) CECT for recurrent gastric cancer. Upper left quadrant: Exclusion and confirmation; LR+ >10, LR- <0.1. Upper right quadrant: Confirmation only; LR+ >10, LR- >0.1. Lower left quadrant: Exclusion or confirmation; LR+ <10, LR- <0.1. Lower right quadrant: No exclusion or confirmation; LR+ <10, LR- >0.1. Summary LR+ and LR- for index test with 95% confidence intervals. LR+/-, positive/negative likelihood ratio; CECT, contrast-enhanced computed tomography; FDG PET, fluorodeoxyglucose positron emission tomography.
Figure 5.
SROC curves. (A) FDG PET for lymph node metastasis; (B) FDG PET for distant metastasis; (C) FDG PET for recurrent gastric cancer; (D) CECT for lymph node metastasis; (E) CECT for distant metastasis; and (F) CECT for recurrent gastric cancer. CECT, contrast-enhanced computed tomography; FDG PET, fluorodeoxyglucose positron emission tomography; SROC, summary receiver operating characteristic; SENS, sensitivity; SPEC, specificity; AUC, area under the curve.
Figure 6.
Fagan nomogram evaluating the overall value of (A) FDG PET for lymph node metastasis; (B) FDG PET for distant metastasis; (C) FDG PET for recurrent gastric cancer; (D) CECT for lymph node metastasis; (E) CECT for distant metastasis; and (F) CECT for recurrent gastric cancer. CECT, contrast-enhanced computed tomography; FDG PET, fluorodeoxyglucose positron emission tomography; LR, likelihood ratio; Pos, positive; Neg, negative; Prob, probability.
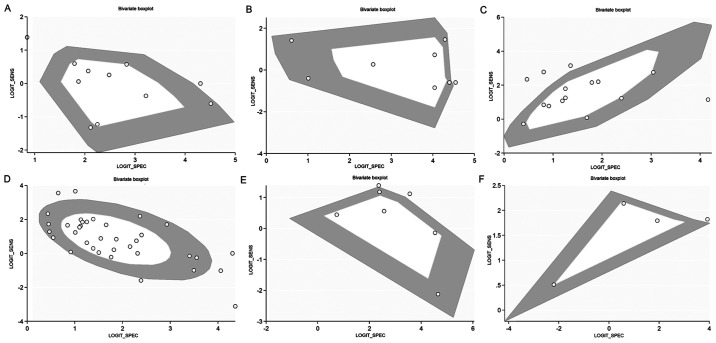
Considerable heterogeneity with a significant χ2 test (P<0.001) and an I2 value of 87.6% for pooling the sensitivity and 64.2% for specificity was determined, indicating substantial heterogeneity (Fig. 3). Of note, two studies were outside the circle of the bivariate box plot, indicating the possibility of between-study heterogeneity (Fig. 7). The funnel plot was symmetrical, indicating the absence of publication bias (Fig. S1), which was confirmed with a non-significant Deek's test (P=0.44).
Figure 7.
Bivariate boxplot of the sensitivities and specificities in the included studies. (A) FDG PET for lymph node metastasis; (B) FDG PET for distant metastasis; (C) FDG PET for recurrent gastric cancer; (D) CECT for lymph node metastasis; (E) CECT for distant metastasis; and (F) CECT for recurrent gastric cancer. SENS, sensitivity; SPEC, specificity.
Distant metastasis
In total, 8 studies evaluated the accuracy of 18F-FDG PET/CT for diagnosing distant metastases (M staging) among patients with gastric cancer. The pooled sensitivity and specificity were 56% (95% CI, 40-71%) and 97% (95% CI, 87-99%), respectively (Fig. 3). The DOR was 41 (95% CI, 8-206). The LR+ was 18.5 (95% CI, 4.1-83.6) and the LR- was 0.45 (0.32-0.65). LR+ and LR- values were in the right upper quadrant of the LR scattergram, indicating that the 18F-FDG PET/CT may be used for confirmation only (Fig. 4). Fig. 5 presents the SROC curve for diagnosing distant metastases using 18F-FDG PET/CT. The AUC of 0.83 (95% CI, 0.74-0.89) suggested a high diagnostic performance of 18F-FDG PET/CT. Fagan's nomogram indicated a good clinical utility for 18F-FDG PET/CT for diagnosing distant metastasis, as the post-test probability (positive, 91%; negative, 20%) was significantly different from the pre-test probability (35%) (Fig. 6).
Considerable heterogeneity with a significant Chi-square test (P<0.001) and an I2 value of 83.5% for pooling the sensitivity and 94.1% for specificity was determined, indicating substantial heterogeneity (Fig. 3). Of note, 1 study was outside of the bivariate box plot circle, indicating the possibility of between-study heterogeneity (Fig. 7). Publication bias was not assessed, as <10 studies reported on this outcome.
Recurrent gastric cancer
In total, 16 studies evaluated the accuracy of 18F-FDG PET/CT for diagnosing recurrent gastric cancer. The pooled sensitivity and specificity were 81% (95% CI, 72-88%) and 83% (95% CI, 74-89%), respectively (Fig. 3). The DOR was 21 (95% CI, 10-45). The LR+ was 4.8 (95% CI, 3-7.5) and the LR- was 0.23 (0.15-0.35). The LR+ and LR- values were in the right lower quadrant of the LR scattergram, indicating that the 18F-FDG PET/CT should not be used for confirmation or exclusion (Fig. 4). Fig. 5 presents the SROC curve for diagnosing recurrent gastric cancer tumors using 18F-FDG PET/CT. The AUC was 0.89 (95% CI, 0.73-0.96), indicating a high diagnostic performance of 18F-FDG PET/CT. Fagan's nomogram suggested a good clinical utility of 18F-FDG PET/CT for recurrent gastric cancer diagnosis, as the post-test probability (positive, 73%; negative, 11%) differed from the pre-test probability (36%; Fig. 6).
Considerable heterogeneity was determined with a significant Chi-square test (P<0.001) and an I2 value of 75.7% for pooling the sensitivity and 89.7% for specificity, indicating substantial heterogeneity (Fig. 3). A total of 4 studies were outside of the bivariate box plot circle, implying the possibility of between-study heterogeneity (Fig. 7). The funnel plot was symmetrical, indicating the absence of publication bias (Fig. S2). This was confirmed with a non-significant Deek's test (P=0.10).
Diagnostic performance of CECT. Lymph node metastasis
In total, 37 studies evaluated the accuracy of CECT for diagnosing lymph node metastases (N staging) among patients with gastric cancer. The pooled sensitivity and specificity were 69% (95% CI, 59-77%) and 85% (95% CI, 81-89%), respectively (Fig. 3). The DOR was 12 (95% CI, 9-17). The LR+ was 4.7 (95% CI, 3.8-5.8) and the LR- was 0.38 (0.30-0.50). The LR+ and LR- values were in the right lower quadrant of the LR scattergram, indicating that the CECT cannot be used for confirmation or exclusion (Fig. 4). Fig. 5 presents the SROC curve for diagnosing nodal metastases using CECT. The AUC was 0.86 (95% CI, 0.81-0.90), indicating a high diagnostic performance for CECT. Fagan's nomogram suggested an average clinical utility of CECT for nodal metastasis diagnosis, as the post-test probability (positive, 77%; negative, 14%) differed slightly from the pre-test probability (42%; Fig. 6).
Considerable heterogeneity with a significant Chi-square test (P<0.001) and an I2 value of 94.6% for pooling the sensitivity and 91.7% for specificity was determined, indicating substantial heterogeneity (Fig. 3). A total of six studies were outside the bivariate box plot circle, implying the possibility of between-study heterogeneity (Fig. 7). The funnel plot was found to be asymmetrical according to Deeks' test (P=0.02), indicating the presence of publication bias (Fig. S3).
Distant metastasis
A total of 7 studies evaluated the accuracy of CECT for diagnosing distant metastasis (M staging) among patients with gastric cancer. The pooled sensitivity and specificity were 59% (95% CI, 41-75%) and 96% (95% CI, 83-99%), respectively (Fig. 3). The DOR was 36 (95% CI, 9-147). The LR+ was 15.4 (95% CI, 3.7-64.3) and the LR- was 0.42 (0.28-0.64). The LR+ and LR- values were in the right upper quadrant of the LR scattergram, indicating that the CECT may be used for confirmation only (Fig. 4). Fig. 5 presents the SROC curve for diagnosing distant metastases using CECT. The AUC was 0.85 (95% CI, 0.77-0.91), indicating a high diagnostic performance of CECT. Fagan's nomogram suggested a good clinical utility of CECT for distant metastasis diagnosis, as the post-test probability (positive, 90%; negative, 20%) differed significantly from the pre-test probability (37%) (Fig. 6).
Considerable heterogeneity with a significant Chi-square test (P<0.001) and an I2 value of 79.7% for pooling the sensitivity and 89.7% for specificity was determined, indicating substantial heterogeneity (Fig. 3). A total of 2 studies were outside the bivariate box plot circle, suggesting between-study heterogeneity (Fig. 7). Publication bias was not assessed, as <10 studies reported on this outcome.
Recurrent gastric cancer
In total, 4 studies evaluated the accuracy of CECT for diagnosing patients with recurrent gastric cancer. The pooled sensitivity and specificity were 82% (95% CI, 71-89%) and 76% (95% CI, 23-97%), respectively (Fig. 3). The DOR was 14 (95% CI, 0.89-217). The LR+ was 3.4 (95% CI, 0.54-21) and the LR- was 0.24 (0.09-0.63). The LR+ and LR- values were in the right lower quadrant of the LR scattergram, indicating that the CECT cannot be used for confirmation or exclusion (Fig. 4). Fig. 5 presents the SROC curve for diagnosing recurrent gastric cancer using CECT. The AUC was 0.84 (95% CI, 0.72-0.92), indicating a high diagnostic performance of CECT. Fagan's nomogram suggested a good clinical utility of CECT for diagnosing recurrent gastric cancer, as the post-test probability (positive, 66%; negative, 12%) differed from the pre-test probability (37%) (Fig. 6).
Considerable heterogeneity was determined with a significant Chi-square test (P<0.001) and an I2 value of 65.5% for pooling the sensitivity and 95.4% for specificity, indicating substantial heterogeneity (Fig. 3). Of note, one study was outside the bivariate box plot circle, indicating the possibility of between-study heterogeneity (Fig. 7). Publication bias was not assessed, as <10 studies reported on this outcome.
Discussion
Various imaging modalities are available for the staging of primary gastric cancers and diagnosing recurrent lesions. For several years, CECT scans have been routinely used for preoperative staging of gastric cancer around the world. However, 18F-FDG PET/CT is a relatively new technique that is being incorporated for the pre-operative staging of several malignant lesions (19,20). An important advantage offered by 18F-FDG PET/CT is that it combines functional images from PET and anatomical details of the CT scan, thereby overcoming the limitations of the individual imaging modalities (21). Both PET and CT are acquired in the same session for 18F-FDG PET/CT and the modality allows for the accurate anatomical localization of malignant lesions. Evidence suggests that 18F-FDG PET/CT may also facilitate early diagnosis, particularly for recurrent lesions with negative findings on conventional imaging (19-21). In order to present high-level evidence to guide clinical practice, the current literature was reviewed to analyze the diagnostic accuracies of both 18F-FDG PET/CT and CECT for patients with primary and recurrent gastric cancers.
The present study provided a pooled analysis of data from a large number of studies comprising a total of 9,997 participants. Initially, the diagnostic accuracy of both imaging modalities for lymph node metastases was assessed and it was revealed that 18F-FDG PET/CT had a pooled sensitivity of 49% and specificity of 92% with a high diagnostic performance (AUC=0.84). On the other hand, CECT had a better pooled sensitivity (69%) but lower specificity (85%) and higher diagnostic accuracy (AUC=0.86) for the same. For distant metastasis, the diagnostic accuracies of both techniques (sensitivity and specificity) were similar. Furthermore, for recurrent gastric cancer, the pooled sensitivities were similar for both techniques, but the pooled specificity was higher for 18F-FDG PET/CT than for CECT. The results of the present study concur with previous reviews conducted by Zhong et al (81) in 2012 and Li et al (82) in 2016, which demonstrated that 18F-FDG PET/CT had a higher diagnostic performance than CECT for recurrent gastric cancer but CECT is better for preoperative staging of nodal metastasis. These studies also suggested that both techniques are equally accurate in detecting distant metastases among patients with gastric cancer.
The LR scattergrams of both techniques had the LR+ and LR- in the right lower quadrant, indicating that these techniques cannot be used to exclude or confirm the presence of lymph node metastases or recurrent gastric cancer tumors. However, both 18F-FDG PET/CT and CECT had LR scattergrams occupying the right upper quadrant for distant metastases, indicating that both techniques may be used for confirming the M staging of gastric cancer. The clinical values of both 18F-FDG PET/CT and CECT for all the outcomes were high, as Fagan's nomogram exhibited a significant increase in the post-test probabilities compared to the pre-test probabilities. However, while inferring these results, the quality and methodology differences between the included studies should be considered, as these may potentially influence the conclusions. There was significant inter-study heterogeneity among the included studies as indicated by a significant Chi-square test and I2 statistic results. Furthermore, Deek's test and the funnel plots indicated the possibility of publication bias among the studies reporting on the diagnostic accuracy of CECT for lymph node metastasis. Publication bias for other outcomes for CECT was not assessed due to an insufficient number of studies in the analysis. However, there was no evidence of publication bias among the studies reporting on the outcomes for 18F-FDG PET/CT.
The present study has the following strengths: As compared with previous reviews on the subject (81,82), the present study provided comprehensive and updated evidence on the accuracy of 18F-FDG PET/CT and CECT for primary gastric cancer TNM staging and detection of recurrence. The lack of publication bias for the 18F-FDG PET/CT analysis in the present review adds credibility to the overall results. However, the present study also has certain limitations. First, there was a high risk of bias in certain studies assessing the accuracy of CECT, which may have influenced the final estimates. In addition, significant inter-study heterogeneity was identified between the studies included in the present review. This may have influenced the accuracy of the pooled results. Finally, no meta-regression was performed to explore the sources of heterogeneity among the included studies.
Despite these limitations, the present study provided valuable insight regarding the diagnostic performance of two important non-invasive imaging modalities for screening patients with gastric cancer for preoperative TNM staging and postoperative recurrence. 18F-FDG PET/CT has a sensitivity well below the acceptable threshold for N staging for gastric cancer, indicating that it cannot be used for diagnosing nodal metastasis in patients with gastric cancer. Although CECT had a satisfactory sensitivity and specificity for all the outcomes, it did not meet the SnNout triage test criteria for sensitivity and the SpPin criteria for the specificity of a diagnostic test for N staging of gastric cancer and recurrent gastric cancer (83). This means that CECT cannot be used to confirm or rule out nodal metastases or recurrent gastric cancer tumors in patients. However, both 18F-FDG PET/CT and CECT meet the SpPin criteria for the specificity of a diagnostic test for gastric cancer M staging, which indicates that both techniques may be used to confirm distant metastasis with a high level of confidence in patients with gastric cancer. The present results may prompt a change in clinical practices for the diagnosis and staging of gastric cancer. Both 18F-FDG PET/CT and CECT may be used as first-line imaging modalities for M staging of the disease. However, further studies from different geographical regions of the world are also required, as current evidence from low- and middle-income regions is limited. With more generalizable data, new global guidelines and practices may be generated for patients with gastric cancer irrespective of the setting. Affordability of the tests should also be considered by cost-effectiveness analyses to choose the best and the most cost-effective technique for gastric cancer diagnosis and staging.
In conclusion, the present study indicated that both FDG PET/CT and CECT are highly useful imaging modalities for diagnosing recurrent gastric cancer due to their high sensitivities and specificities. These techniques cannot be used to exclude or confirm the presence of lymph node metastases or recurrent gastric cancer tumors, but can be used for the confirmation of distal metastasis.
Supplementary Material
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
ZZ, BZ and CJ designed the project; WC and HX were involved in data collection and data analysis. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Balakrishnan M, George R, Sharma A, Graham DY. Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep. 2017;19(36) doi: 10.1007/s11894-017-0575-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 3.de Martel C, Forman D, Plummer M. Gastric cancer: Epidemiology and risk factors. Gastroenterol Clin North Am. 2013;42:219–240. doi: 10.1016/j.gtc.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Japanese gastric cancer treatment guidelines 2014 (ver. 4) Gastric Cancer. 2017;20:1–19. doi: 10.1007/s10120-016-0622-4. Japanese Gastric Cancer Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ono H, Yao K, Fujishiro M, Oda I, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Ichinose M, Matsui T. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer. Dig Endosc. 2016;28:3–15. doi: 10.1111/den.12518. [DOI] [PubMed] [Google Scholar]
- 6.Eom BW, Yu JS, Ryu KW, Kook MC, Kim YI, Cho SJ, Lee JY, Kim CG, Choi IJ, Yoon HM, Kim YW. Optimal submucosal invasion of early gastric cancer for endoscopic resection. Ann Surg Oncol. 2015;22:1806–1812. doi: 10.1245/s10434-014-4308-z. [DOI] [PubMed] [Google Scholar]
- 7.Ajani JA, Bentrem DJ, Besh S, D'Amico TA, Das P, Denlinger C, Fakih MG, Fuchs CS, Gerdes H, Glasgow RE, et al. Gastric cancer, version 2.2013: Featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2013;11:531–546. doi: 10.6004/jnccn.2013.0070. [DOI] [PubMed] [Google Scholar]
- 8.de Steur WO, Hartgrink HH, Dikken JL, Putter H, van de Velde CJ. Quality control of lymph node dissection in the Dutch gastric cancer trial. Br J Surg. 2015;102:1388–1393. doi: 10.1002/bjs.9891. [DOI] [PubMed] [Google Scholar]
- 9.Hwang SW, Lee DH. Is endoscopic ultrasonography still the modality of choice in preoperative staging of gastric cancer? World J Gastroenterol. 2014;20:13775–13782. doi: 10.3748/wjg.v20.i38.13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. doi: 10.6004/jnccn.2010.0012. National Comprehensive Cancer Network: NCCN clinical practice guidelines in oncology. Gastric Cancer, V.2.2010, 2010. [DOI] [PubMed] [Google Scholar]
- 11.Lim JH, Ko YT, Lee DH. Transabdominal US staging of gastric cancer. Abdom Imaging. 1994;19:527–531. doi: 10.1007/BF00198255. [DOI] [PubMed] [Google Scholar]
- 12.Suk KT, Lim DW, Kim MY, Park DH, Kim KH, Kim JM, Kim JW, Kim HS, Kwon SO, Baik SK, Park SJ. Thickening of the gastric wall on transabdominal sonography: A sign of gastric cancer. J Clin Ultrasound. 2008;36:462–466. doi: 10.1002/jcu.20450. [DOI] [PubMed] [Google Scholar]
- 13.Solbiati L, Tonolini M, Cova L, Goldberg SN. The role of contrast-enhanced ultrasound in the detection of focal liver leasions. Eur Radiol. 2001;11 (Suppl 3):E15–E26. doi: 10.1007/pl00014125. [DOI] [PubMed] [Google Scholar]
- 14.Chen CY, Wu DC, Kang WY, Hsu JS. Staging of gastric cancer with 16-channel MDCT. Abdom Imaging. 2006;31:514–520. doi: 10.1007/s00261-005-0218-7. [DOI] [PubMed] [Google Scholar]
- 15.Kim AY, Kim HJ, Ha HK. Gastric cancer by multidetector row CT: Preoperative staging. Abdom Imaging. 2005;30:465–472. doi: 10.1007/s00261-004-0273-5. [DOI] [PubMed] [Google Scholar]
- 16.Tunaci M. Carcinoma of stomach and duodenum: Radiologic diagnosis and staging. Eur J Radiol. 2002;42:181–192. doi: 10.1016/s0720-048x(02)00035-9. [DOI] [PubMed] [Google Scholar]
- 17.Kwee RM, Kwee TC. Imaging in local staging of gastric cancer: A systematic review. J Clin Oncol. 2007;25:2107–2116. doi: 10.1200/JCO.2006.09.5224. [DOI] [PubMed] [Google Scholar]
- 18.Koh DM, Collins DJ. Diffusion-weighted MRI in the body: Applications and challenges in oncology. AJR Am J Roentgenol. 2007;188:1622–1635. doi: 10.2214/AJR.06.1403. [DOI] [PubMed] [Google Scholar]
- 19.Dassen AE, Lips DJ, Hoekstra CJ, Pruijt JF, Bosscha K. FDG-PET has no definite role in preoperative imaging in gastric cancer. Eur J Surg Oncol. 2009;35:449–455. doi: 10.1016/j.ejso.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Thie JA. Understanding the standardized uptake value, its methods, and implications for usage. J Nucl Med. 2004;45:1431–1434. [PubMed] [Google Scholar]
- 21.Boellaard R, Krak NC, Hoekstra OS, Lammertsma AA. Effects of noise, image resolution, and ROI definition on the accuracy of standard uptake values: A simulation study. J Nucl Med. 2004;45:1519–1527. [PubMed] [Google Scholar]
- 22.Long NM, Smith CS. Causes and imaging features of false positives and false negatives on F-PET/CT in oncologic imaging. Insights Imaging. 2011;2:679–698. doi: 10.1007/s13244-010-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mochiki E, Kuwano H, Katoh H, Asao T, Oriuchi N, Endo K. Evaluation of 18F-2-deoxy-2-fluoro-D-glucose positron emission tomography for gastric cancer. World J Surg. 2004;28:247–253. doi: 10.1007/s00268-003-7191-5. [DOI] [PubMed] [Google Scholar]
- 24.Yoo CH, Noh SH, Shin DW, Choi SH, Min JS. Recurrence following curative resection for gastric carcinoma. Br J Surg. 2000;87:236–242. doi: 10.1046/j.1365-2168.2000.01360.x. [DOI] [PubMed] [Google Scholar]
- 25.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann Internal Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. QUADAS-2 Group. [DOI] [PubMed] [Google Scholar]
- 26.Ahn HS, Lee HJ, Yoo MW, Kim SG, Im JP, Kim SH, Kim WH, Lee KU, Yang HK. Diagnostic accuracy of T and N stages with endoscopy, stomach protocol CT, and endoscopic ultrasonography in early gastric cancer. J Surg Oncol. 2009;99:20–27. doi: 10.1002/jso.21170. [DOI] [PubMed] [Google Scholar]
- 27.Bilici A, Ustaalioglu BB, Seker M, Kefeli U, Canpolat N, Tekinsoy B, Ozugur S, Gumus M. The role of 18F-FDG PET/CT in the assessment of suspected recurrent gastric cancer after initial surgical resection: Can the results of FDG PET/CT influence patients' treatment decision making? Eur J Nucl Med Mol Imaging. 2011;38:64–73. doi: 10.1007/s00259-010-1611-1. [DOI] [PubMed] [Google Scholar]
- 28.Blackshaw GR, Barry JD, Edwards P, Allison MC, Thomas GV, Lewis WG. Laparoscopy significantly improves the perceived preoperative stage of gastric cancer. Gastric Cancer. 2003;6:225–229. doi: 10.1007/s10120-003-0257-0. [DOI] [PubMed] [Google Scholar]
- 29.Bosch KD, Chicklore S, Cook GJ, Davies AR, Kelly M, Gossage JA, Baker CR. Staging FDG PET-CT changes management in patients with gastric adenocarcinoma who are eligible for radical treatment. Eur J Nucl Med Mol Imaging. 2020;47:759–767. doi: 10.1007/s00259-019-04429-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cayvarlı H, Bekiş R, Akman T, Altun D. The role of 18F-FDG PET/CT in the evaluation of gastric cancer recurrence. Mol Imaging Radionucl Ther. 2014;23:76–83. doi: 10.4274/mirt.83803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen J, Cheong JH, Yun MJ, Kim J, Lim JS, Hyung WJ, Noh SH. Improvement in preoperative staging of gastric adenocarcinoma with positron emission tomography. Cancer. 2005;103:2383–2390. doi: 10.1002/cncr.21074. [DOI] [PubMed] [Google Scholar]
- 32.Chen BB, Liang PC, Liu KL, Hsiao JK, Huang JC, Wong JM, Lee PH, Shun CT, Ming-Tsang Y. Preoperative diagnosis of gastric tumors by three-dimensional multidetector row ct and double contrast barium meal study: Correlation with surgical and histologic results. J Formos Med Assoc. 2007;106:943–952. doi: 10.1016/S0929-6646(08)60065-0. [DOI] [PubMed] [Google Scholar]
- 33.De Potter T, Flamen P, Van Cutsem E, Penninckx F, Filez L, Bormans G, Maes A, Mortelmans L. Whole-body PET with FDG for the diagnosis of recurrent gastric cancer. Eur J Nucl Med Mol Imaging. 2002;29:525–529. doi: 10.1007/s00259-001-0743-8. [DOI] [PubMed] [Google Scholar]
- 34.D'Elia F, Zingarelli A, Palli D, Grani M. Hydro-dynamic CT preoperative staging of gastric cancer: Correlation with pathological findings. A prospective study of 107 cases. Eur Radiol. 2000;10:1877–1885. doi: 10.1007/s003300000537. [DOI] [PubMed] [Google Scholar]
- 35.Feng XY, Wang W, Luo GY, Wu J, Zhou ZW, Li W, Sun XW, Li YF, Xu DZ, Guan YX, et al. Comparison of endoscopic ultrasonography and multislice spiral computed tomography for the preoperative staging of gastric cancer-results of a single institution study of 610 Chinese patients. PLoS One. 2013;8(e78846) doi: 10.1371/journal.pone.0078846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Filik M, Kir KM, Aksel B, Soyda Ç, Özkan E, Küçük ÖN, İbiş E, Akgül H. The role of 18F-FDG PET/CT in the primary staging of gastric cancer. Mol Imaging Radionucl Ther. 2015;24:15–20. doi: 10.4274/mirt.26349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fujikawa H, Yoshikawa T, Hasegawa S, Hayashi T, Aoyama T, Ogata T, Cho H, Oshima T, Rino Y, Morita S, Masuda M. Diagnostic value of computed tomography for staging of clinical T1 gastric cancer. Ann Surg Oncol. 2014;21:3002–3007. doi: 10.1245/s10434-014-3667-9. [DOI] [PubMed] [Google Scholar]
- 38.Giganti F, Orsenigo E, Arcidiacono PG, Nicoletti R, Albarello L, Ambrosi A, Salerno A, Esposito A, Petrone MC, Chiari D, et al. Preoperative locoregional staging of gastric cancer: Is there a place for magnetic resonance imaging? Prospective comparison with EUS and multidetector computed tomography. Gastric Cancer. 2016;19:216–225. doi: 10.1007/s10120-015-0468-1. [DOI] [PubMed] [Google Scholar]
- 39.Graziosi L, Bugiantella W, Cavazzoni E, Cantarella F, Porcari M, Baffa N, Donini A. Role of FDG-PET/CT in follow-up of patients treated with resective gastric surgery for tumour. Ann Ital Chir. 2011;82:125–129. [PubMed] [Google Scholar]
- 40.Ha TK, Choi YY, Song SY, Kwon SJ. F18-fluorodeoxyglucose-positron emission tomography and computed tomography is not accurate in preoperative staging of gastric cancer. J Korean Surg Soc. 2011;81:104–110. doi: 10.4174/jkss.2011.81.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasegawa S, Yoshikawa T, Shirai J, Fujikawa H, Cho H, Doiuchi T, Yoshida T, Sato T, Oshima T, Yukawa N, et al. A prospective validation study to diagnose serosal invasion and nodal metastases of gastric cancer by multidetector-row CT. Ann Surg Oncol. 2013;20:2016–2022. doi: 10.1245/s10434-012-2817-1. [DOI] [PubMed] [Google Scholar]
- 42.Hwang SW, Lee DH, Lee SH, Park YS, Hwang JH, Kim JW, Jung SH, Kim NY, Kim YH, Lee KH, et al. Preoperative staging of gastric cancer by endoscopic ultrasonography and multidetector-row computed tomography. J Gastroenterol Hepatol. 2010;25:512–518. doi: 10.1111/j.1440-1746.2009.06106.x. [DOI] [PubMed] [Google Scholar]
- 43.Jadvar H, Tatlidil R, Garcia AA, Conti PS. Evaluation of recurrent gastric malignancy with [F-18]-FDG positron emission tomography. Clin Radiol. 2003;58:215–221. doi: 10.1016/s0009-9260(02)00477-4. [DOI] [PubMed] [Google Scholar]
- 44.Joo I, Lee JM, Kim JH, Shin CI, Han JK, Choi BI. Prospective comparison of 3T MRI with diffusion-weighted imaging and MDCT for the preoperative TNM staging of gastric cancer. J Magn Reson Imaging. 2015;41:814–821. doi: 10.1002/jmri.24586. [DOI] [PubMed] [Google Scholar]
- 45.Karakoyun R, Demirci E, Karakoyun M, Karakaş B, Gündüz U, Sener Z, Gülenay S, Erol B, Sağtaş E. Reliability of MDCT, with MPR and hydro-CT technique, in resectability and lymphnode staging of gastric cancer. Minerva Chir. 2014;69:129–140. [PubMed] [Google Scholar]
- 46.Kawanaka Y, Kitajima K, Fukushima K, Mouri M, Doi H, Oshima T, Niwa H, Kaibe N, Sasako M, Tomita T, et al. Added value of pretreatment (18)F-FDG PET/CT for staging of advanced gastric cancer: Comparison with contrast-enhanced MDCT. Eur J Radiol. 2016;85:989–995. doi: 10.1016/j.ejrad.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 47.Kim HJ, Kim AY, Oh ST, Kim JS, Kim KW, Kim PN, Lee MG, Ha HK. Gastric cancer staging at multi-detector row CT gastrography: Comparison of transverse and volumetric CT scanning. Radiology. 2005;236:879–885. doi: 10.1148/radiol.2363041101. [DOI] [PubMed] [Google Scholar]
- 48.Kim DS, Hong SH, Choi JY, Paeng JC, Kim NR, Jun WS, Kang HS. Magnetic resonance imaging diagnoses of bone scan abnormalities in breast cancer patients. Nucl Med Commun. 2009;30:736–741. doi: 10.1097/MNM.0b013e32832ed375. [DOI] [PubMed] [Google Scholar]
- 49.Kim EY, Lee WJ, Choi D, Lee SJ, Choi JY, Kim BT, Kim HS. The value of PET/CT for preoperative staging of advanced gastric cancer: Comparison with contrast-enhanced CT. Eur J Radiol. 2011;79:183–188. doi: 10.1016/j.ejrad.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 50.Kim SH, Kim JJ, Lee JS, Kim SH, Kim BS, Maeng YH, Hyun CL, Kim MJ, Jeong IH. Preoperative N staging of gastric cancer by stomach protocol computed tomography. J Gastric Cancer. 2013;13:149–156. doi: 10.5230/jgc.2013.13.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim JH, Heo SH, Kim JW, Shin SS, Min JJ, Kwon SY, Jeong YY, Kang HK. Evaluation of recurrence in gastric carcinoma: Comparison of contrast-enhanced computed tomography and positron emission tomography/computed tomography. World J Gastroenterol. 2017;23:6448–6456. doi: 10.3748/wjg.v23.i35.6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kudou M, Kosuga T, Kubota T, Okamoto K, Komatsu S, Shoda K, Konishi H, Shiozaki A, Fujiwara H, Arita T, et al. Value of preoperative PET-CT in the prediction of pathological stage of gastric cancer. Ann Surg Oncol. 2018;25:1633–1639. doi: 10.1245/s10434-018-6455-0. [DOI] [PubMed] [Google Scholar]
- 53.Lee IJ, Lee JM, Kim SH, Shin CI, Lee JY, Kim SH, Han JK, Choi BI. Diagnostic performance of 64-channel multidetector CT in the evaluation of gastric cancer: Differentiation of mucosal cancer (T1a) from submucosal involvement (T1b and T2) Radiology. 2010;255:805–814. doi: 10.1148/radiol.10091313. [DOI] [PubMed] [Google Scholar]
- 54.Lee MR, Unger JG, Rohrich RJ. Management of the nasal dorsum in rhinoplasty: A systematic review of the literature regarding technique, outcomes, and complications. Plast Reconstr Surg. 2011;128:538e–550e. doi: 10.1097/PRS.0b013e31822b6a82. [DOI] [PubMed] [Google Scholar]
- 55.Lee DY, Lee CH, Seo MJ, Lee SH, Ryu JS, Lee JJ. Performance of (18)F-FDG PET/CT as a postoperative surveillance imaging modality for asymptomatic advanced gastric cancer patients. Ann Nucl Med. 2014;28:789–795. doi: 10.1007/s12149-014-0871-4. [DOI] [PubMed] [Google Scholar]
- 56.Lim JS, Kim MJ, Yun MJ, Oh YT, Kim JH, Hwang HS, Park MS, Cha SW, Lee JD, Noh SH, et al. Comparison of CT and 18F-FDG pet for detecting peritoneal metastasis on the preoperative evaluation for gastric carcinoma. Korean J Radiol. 2006;7:249–256. doi: 10.3348/kjr.2006.7.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marrelli D, Mazzei MA, Pedrazzani C, Di Martino M, Vindigni C, Corso G, Morelli E, Volterrani L, Roviello F. High accuracy of multislices computed tomography (MSCT) for para-aortic lymph node metastases from gastric cancer: A prospective single-center study. Ann Surg Oncol. 2011;18:2265–2272. doi: 10.1245/s10434-010-1541-y. [DOI] [PubMed] [Google Scholar]
- 58.Nakamoto Y, Togashi K, Kaneta T, Fukuda H, Nakajima K, Kitajima K, Murakami K, Fujii H, Satake M, Tateishi U, et al. Clinical value of whole-body FDG-PET for recurrent gastric cancer: A multicenter study. Jpn J Clin Oncol. 2009;39:297–302. doi: 10.1093/jjco/hyp010. [DOI] [PubMed] [Google Scholar]
- 59.Namikawa T, Okabayshi T, Nogami M, Ogawa Y, Kobayashi M, Hanazaki K. Assessment of (18)F-fluorodeoxyglucose positron emission tomography combined with computed tomography in the preoperative management of patients with gastric cancer. Int J Clin Oncol. 2014;19:649–655. doi: 10.1007/s10147-013-0598-6. [DOI] [PubMed] [Google Scholar]
- 60.Pan Z, Pang L, Ding B, Yan C, Zhang H, Du L, Wang B, Song Q, Chen K, Yan F. Gastric cancer staging with dual energy spectral CT imaging. PLoS One. 2013;8(e53651) doi: 10.1371/journal.pone.0053651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Park MJ, Lee WJ, Lim HK, Park KW, Choi JY, Kim BT. Detecting recurrence of gastric cancer: The value of FDG PET/CT. Abdom Imaging. 2009;34:441–447. doi: 10.1007/s00261-008-9424-4. [DOI] [PubMed] [Google Scholar]
- 62.Park SR, Kim MJ, Ryu KW, Lee JH, Lee JS, Nam BH, Choi IJ, Kim YW. Prognostic value of preoperative clinical staging assessed by computed tomography in resectable gastric cancer patients: A viewpoint in the era of preoperative treatment. Ann Surg. 2010;251:428–435. doi: 10.1097/SLA.0b013e3181ca69a7. [DOI] [PubMed] [Google Scholar]
- 63.Park K, Jang G, Baek S, Song H. Usefulness of combined PET/CT to assess regional lymph node involvement in gastric cancer. Tumori. 2014;100:201–206. doi: 10.1700/1491.16415. [DOI] [PubMed] [Google Scholar]
- 64.Perlaza P, Ortín J, Pagès M, Buxó E, Fernández-Esparrach G, Colletti PM, Rubello D, Mayoral M, Sánchez N, Ruiz C, et al. Should 18F-FDG PET/CT be routinely performed in the clinical staging of locally advanced gastric adenocarcinoma? Clin Nucl Med. 2018;43:402–410. doi: 10.1097/RLU.0000000000002028. [DOI] [PubMed] [Google Scholar]
- 65.Ren G, Cai R, Chen KM. Clinical value of multidetector computed tomography in detecting lymph node metastasis of early gastric cancer. Zhonghua Zhong Liu Za Zhi. 2007;29:852–855. (In Chinese) [PubMed] [Google Scholar]
- 66.Saito T, Kurokawa Y, Takiguchi S, Miyazaki Y, Takahashi T, Yamasaki M, Miyata H, Nakajima K, Mori M, Doki Y. Accuracy of multidetector-row CT in diagnosing lymph node metastasis in patients with gastric cancer. Eur Radiol. 2015;25:368–374. doi: 10.1007/s00330-014-3373-9. [DOI] [PubMed] [Google Scholar]
- 67.Sharma P, Singh H, Suman SK, Sharma A, Reddy RM, Thulkar S, Bal C, Malhotra A, Kumar R. 18F-FDG PET-CT for detecting recurrent gastric adenocarcinoma: Results from a non-oriental Asian population. Nucl Med Commun. 2012;33:960–966. doi: 10.1097/MNM.0b013e328355b694. [DOI] [PubMed] [Google Scholar]
- 68.Shinohara T, Ohyama S, Yamaguchi T, Muto T, Kohno A, Ogura T, Kato Y, Urashima M. Preoperative TNM staging of advanced gastric cancer with multi-detector row computed tomography. JMAJ. 2005;48:175–182. [Google Scholar]
- 69.Sim SH, Kim YJ, Oh DY, Lee SH, Kim DW, Kang WJ, Im SA, Kim TY, Kim WH, Heo DS, Bang YJ. The role of PET/CT in detection of gastric cancer recurrence. BMC Cancer. 2009;9(73) doi: 10.1186/1471-2407-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smyth E, Schöder H, Strong VE, Capanu M, Kelsen DP, Coit DG, Shah MA. A prospective evaluation of the utility of 2-deoxy-2-[(18) F]fluoro-D-glucose positron emission tomography and computed tomography in staging locally advanced gastric cancer. Cancer. 2012;118:5481–5488. doi: 10.1002/cncr.27550. [DOI] [PubMed] [Google Scholar]
- 71.Stell DA, Carter CR, Stewart I, Anderson JR. Prospective comparison of laparoscopy, ultrasonography and computed tomography in the staging of gastric cancer. Br J Surg. 1996;83:1260–1262. [PubMed] [Google Scholar]
- 72.Sun L, Su XH, Guan YS, Pan WM, Luo ZM, Wei JH, Wu H. Clinical role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in post-operative follow up of gastric cancer: Initial results. World J Gastroenterol. 2008;14:4627–4632. doi: 10.3748/wjg.14.4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tsujimoto H, Sugasawa H, Ono S, Ichikura T, Yamamoto J, Hase K. Has the accuracy of preoperative diagnosis improved in cases of early-stage gastric cancer? World J Surg. 2010;34:1840–1846. doi: 10.1007/s00268-010-0587-0. [DOI] [PubMed] [Google Scholar]
- 74.Turlakow A, Yeung HW, Salmon AS, Macapinlac HA, Larson SM. Peritoneal carcinomatosis: Role of (18)F-FDG PET. J Nucl Med. 2003;44:1407–1412. [PubMed] [Google Scholar]
- 75.Yan C, Zhu ZG, Yan M, Zhang H, Pan ZL, Chen J, Xiang M, Chen MM, Liu BY, Yin HR, Lin YZ. Value of multidetector-row computed tomography in the preoperative T and N staging of gastric carcinoma: A large-scale Chinese study. J Surg Oncol. 2009;100:205–214. doi: 10.1002/jso.21316. [DOI] [PubMed] [Google Scholar]
- 76.Yan C, Zhu ZG, Yan M, Zhang H, Pan ZL, Chen J, Xiang M, Chen MM, Liu BY, Yin HR, Lin YZ. Size of the largest lymph node visualized on multi-detector-row computed tomography (MDCT) is useful in predicting metastatic lymph node status of gastric cancer. J Int Med Res. 2010;38:22–33. doi: 10.1177/147323001003800103. [DOI] [PubMed] [Google Scholar]
- 77.Yang QM, Kawamura T, Itoh H, Bando E, Nemoto M, Akamoto S, Furukawa H, Yonemura Y. Is PET-CT suitable for predicting lymph node status for gastric cancer? Hepatogastroenterology. 2008;55:782–785. [PubMed] [Google Scholar]
- 78.Yoon NR, Park JM, Jung HS, Cho YK, Lee IS, Choi MG, Chung IS, Song KY, Park CH. Usefulness of 18F-fluoro-2-deoxyglucose positron emission tomography in evaluation of gastric cancer stage. Korean J Gastroenterol. 2012;59:347–353. doi: 10.4166/kjg.2012.59.5.347. [DOI] [PubMed] [Google Scholar]
- 79.Yun M, Choi HS, Yoo E, Bong JK, Ryu YH, Lee JD. The role of gastric distention in differentiating recurrent tumor from physiologic uptake in the remnant stomach on 18F-FDG PET. J Nucl Med. 2005;46:953–957. [PubMed] [Google Scholar]
- 80.Yun M, Lim JS, Noh SH, Hyung WJ, Cheong JH, Bong JK, Cho A, Lee JD. Lymph node staging of gastric cancer using (18)F-FDG PET: A comparison study with CT. J Nucl Med. 2005;46:1582–1588. [PubMed] [Google Scholar]
- 81.Zhong BY, Liu YX, Huang WF, Liu QQ, Liu SQ, Liu Y. Clinical value of 64-slice spiral 3-phase CT enhanced scanning for preoperative TNM staging assessment of gastric carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15:706–709. (In Chinese) [PubMed] [Google Scholar]
- 82.Li P, Liu Q, Wang C, Wang T, Liu J, Huang G, Song S. Fluorine-18-fluorodeoxyglucose positron emission tomography to evaluate recurrent gastric cancer after surgical resection: A systematic review and meta-analysis. Ann Nucl Med. 2016;30:179–187. doi: 10.1007/s12149-016-1058-y. [DOI] [PubMed] [Google Scholar]
- 83.Seevaratnam R, Cardoso R, McGregor C, Lourenco L, Mahar A, Sutradhar R, Law C, Paszat L, Coburn N. How useful is preoperative imaging for tumor, node, metastasis (TNM) staging of gastric cancer? A meta-analysis. Gastric Cancer. 2012;15 (Suppl 1):S3–S18. doi: 10.1007/s10120-011-0069-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.