Abstract
Governments worldwide have taken unprecedented social distancing and community lockdown measures to halt the COVID-19 epidemic, leaving millions of people restrained in locked-down communities and their mental well-being at risk. This study examines Chinese rural residents' mental health risk under emergency lockdown during the COVID-19 pandemic. It investigates how the environmental, socioeconomic, and behavioral dimensions of community support affect mental health in this emergency context. We also explore whether community support's effectiveness depends on the strictness of lockdown measures implemented and the level of individual perceived COVID-19 infection risk. We collect self-reported mental health risk, community support, and demographics information through a cross-sectional survey of 3892 Chinese rural residents living in small towns and villages. Ordinary least square regressions are employed to estimate the psychological effects of community support. The results suggest that the COVID-19 epidemic and lockdown policies negatively affect psychological well-being, especially for rural females. The capacity for community production has the largest impact on reducing mental health risks, followed by the stability of basic medical services, community cohesion, housing condition, the stability of communications and transportation supply, and the eco-environment. The effectiveness of different community support dimensions depends on the level of lockdown policy implemented and the levels of one's perceived risk of COVID-19 infection. Our study stresses the psychological significance of a healthy living environment, resilient infrastructure and public service system, and community production capacity during the lockdown in rural towns and villages.
Keywords: COVID-19 pandemic, Lockdown, Living environment, Community support, Mental health, Psychological well-being
1. Introduction
The outbreak of COVID-19 has caused 7,805,148 confirmed cases and 431,192 reported deaths globally as of June 15, 2020 (WHO, 2020a). In addition to pharmaceutical measures, many governments have taken unprecedented social distancing and quarantine measures to halt the transmission of COVID-19 and prevent potential massive outbreaks (Heymann and Shindo, 2020). For the first time, thousands of cities, towns, and villages are locked down, and billions of people are encouraged or forced to stay at home (Wilder-Smith et al., 2020). Such public health measures induce enormous social and economic costs (Xiao and Torok, 2020). Still, both existing studies and the WHO guidelines suggest that these measures effectively slow the pandemic's spread when vaccines and specific medicines are not yet available (Heymann and Shindo, 2020; Kiesha et al., 2020). This study explores how community support mitigates the effects of social isolation on mental health when lockdown policies are strictly implemented.
COVID-19 has changed the world tremendously, with nearly 20% of patients experiencing mental health problems (Taquet et al., 2020). When staying in lockdown situations, rural people in developing countries typically have more difficulties, such as disrupting public services and lack of medical attention (Ranscombe, 2020; Summers-Gabr, 2020). Chinese governments have imposed social distancing and lockdown measures on rural communities, and these measures are expected to last for months or even longer. The labor shortage and traffic disruption caused by lockdown policies had led to obstruction of agricultural production and transportation in rural communities; also, the quarantine had exposed the inadequacy of rural public service and community management. Therefore, people living in rural communities can be quite vulnerable to mental health problems (Guo et al., 2020; Hamadani et al., 2020). A recent study has shown that COVID-19 has significant mental health and community implications in rural social relations (Brooks et al., 2020). How to deal with mental health problems and community trauma for people in rural areas has become a critical concern.
Unlike normal daily circumstances, quarantine or lockdown situations would expose people to more complicated and wide-ranging stressors (Brooks et al., 2020). Individuals living in lockdown communities can suffer from loneliness and stress, which in turn can have significant impacts on their mental health and subjective well-being (Brooks et al., 2020; Wang G et al., 2020). Infection risk within the community and inadequate distribution of necessities can further worsen mental health (Pfefferbaum and North, 2020). Previous studies have shown that acute stress disorders are more likely to be observed among the general public who have had quarantine experience, especially among vulnerable groups, such as older adults and people living in remote areas (Yang et al., 2020 ; Li et al., 2020). The symptoms of quarantine-induced mental disorders include insomnia, fatigue, loss of concentration, depression, bipolar disorder, and in extreme cases, suicidal tendencies (Rajkumar, 2020; Rubin and Wessely, 2020), and these adverse effects did not fade quickly over time (Wang et al., 2020a,b). Therefore, understanding mental disorders' stressors under social isolation has practical implications in the current situation (Xiang et al., 2020; Arden and Chilcot, 2020).
Mental health has become one of the significant health challenges faced by the global population. Existing theories mainly focused on environmental determinants and social determinants. On one side, they highlighted the importance of the physical living environment. Specifically, some studies find that clean air and natural neighborhood environment are crucial determinants of population health (The Lancet Public Health, 2017). A higher level of neighborhood greenness, nature availability, and better green space quality (i.e., well-maintained, clean, large, and open) have significant positive effects on mental health during COVID-19 (Geng et al., 2020; Slater et al., 2020; Bratman et al., 2019), especially by increasing the frequency and duration of individual physical activity (Akpinar, 2016; Lu, 2019). Studies have shown that better housing and living conditions contributed to people's physical and mental health during the COVID-19(Tsai and Wilson, 2020; Jones and Grigsby-Toussaint, 2020). Housing with adequate space, a clean and safe environment, proper heating, sanitation, and lighting facilities play a significant role in increasing life satisfaction and well-being (Florian et al., 2011; Friesinger et al., 2019). A pleasant private outdoor green space (e.g., private garden, yard, open roof) is also conducive to psychological benefits (Lin et al., 2017).
On the other side, scholars also find that social factors such as individual education level, childhood experiences, and social life also affect people's mental health, sometimes through interacting with the physical environment (Mullins et al., 2016; Amin et al., 2019). Neighborhood assistance, community-based collaboration, and social support can significantly improve community social environments and increase individual mental well-being (Herrero and Gracia, 2007; Liu et al., 2017). Besides, social services (Sophie et al., 2020) and public infrastructure systems (The Lancet Public Health, 2017) also have critical influences on population health. Improved and accessible health services, social care, and other basic infrastructure, including safe drinking water, adequate food supply, sanitation, electricity, and transportation, are critical factors in promoting mental health (Bergmans et al., 2019; Phillipson et al., 2020). Telemedicine can make up for the lack of health services in rural areas, but poor internet access will affect information exchange and further exacerbate loneliness (Nagata, 2020).
Compared with cities, rural communities may have some advantages, such as lower population density, higher green coverage, tighter social networks, and more robust self-sufficiency in the food supply. Simultaneously, the disadvantages are also obvious, especially in remote and underdeveloped rural areas, such as fragile infrastructure and fewer public services, especially in terms of essential health and medical services. Moreover, in China, rural households hold fewer economic resources to defend againt adverse shocks and make a living in social isolation (Su et al., 2020). The COVID-19 pandemic has brought more attention to the modernization of rural governance capacity.
The scale, rapid development, and impact of massive community containment under the COVID-19 pandemic are unprecedented in history. The changes in the rural population's physical, psychological, and social conditions under isolation are also unprecedented, even extreme. It is a consensus that material and spiritual support at the community level significantly influence individuals' quality of life and subjective well-being, especially concerning daily life during quarantine (Zhu et al., 2020). Several studies have investigated how to mitigate quarantine experience's psychological impacts (Brooks et al., 2020). our study is the first to comprehensively assess the role of community support systems in protecting rural residents' mental health and psychological well-being during this unprecedented community lockdown. This particular case study will enhance our understanding and provide guiding significance for the living environment, social environment, and governance capabilities in rural areas during large-scale public health incidents. It will also contribute to the theoretical understanding of the association between environment and mental health.
In this study, we introduce a systematic framework incorporating socioeconomic factors (i.e., community production, social cohesion, social service, individual demographic characteristics), environmental factors (eco-environment, housing, basic infrastructure), and behavioral factors (i.e., physical activities) of community support into the analysis of the mental health and subjective well-being of individuals living in locked-down rural communities during the COVID-19 pandemic. We first examine the mental health risk of Chinese rural residents under the emergency lockdown during the pandemic and investigate how the different community-support factors affect mental health in this emergency context. To gain more comprehensive insights under different social conditions, we further explore whether community support's performance differs by the strictness of lockdown measures implemented (Wilder-Smith et al., 2020) and the level of individual perceived COVID-19 infection risk (Khosravi, 2020).
2. Material and methods
2.1. Sample and data collection
The study population comprises 3892 rural residents who have been living in small rural towns and villages for at least five days during the COVID-19 lockdown from all 34 provincial administrative regions in China. To collect the data, we randomly or semi-targeted distribute online questionnaires from February 16 to March 10, 2020. We gathered self-reported information about mental health risk, perceived and objective community support, demographic and socioeconomic characteristics in the survey. This work was reviewed and approved by the Village and Town Planning Branch of the Architectural Society of China.
2.2. Measure of self-reported mental health risk
We use the MADRS Montgomery Depression Rating Scale (Montgomery et al., 1979), the General Health-12 Scale (Montazeri et al., 2003), the World Health Organization Well-Being Index (Topp et al., 2015), and the Generalized Anxiety Self-rating Scale (Spitzer et al., 2006) for reference. The mental health risk of rural residents living in locked-down communities is measured by the average score of the four most common items indicating psychological distress: feelings of panic, anxiety, boredom and frustration, and loss of confidence (see Table 1 ). More specifically, we designed the following four questions to capture respondent's feeling of distress in the lockdown (Akpinar, 2016): Do you feel panic because of the pandemic spread during the COVID-19 (Akter and Basher, 2014); Are you bored and frustrated by doing nothing (Amin et al., 2019); Are you anxious about potential financial loss or abnormal production and lives (Kansiimeet al., 2020); Do you feel unconfident about overcoming the pandemic and restoring normal daily production and lives. Measurements are made through the five-point Likert scale, ranging from 1 (not distressed) to 5(highly distressed).
Table 1.
Indicator system of mental health risk and community support.
| Self-reported mental health status (Dependent variable) | Mental health risk | Panic |
|---|---|---|
| Boredom and frustration | ||
| Anxiety | ||
| Loss of confidence | ||
| Community Support (Independent variable) | Eco-environment | Natural environmental conditions |
| Air quality | ||
| Housing | Sufficient number of rooms | |
| Housing conditions | ||
| The landscape around the house | ||
| Community cohesion | Social order | |
| Neighborhood assistance | ||
| Physical activities | Frequency of outdoor activities in the exterior of the property and roofs | |
| Frequency of activities to open spaces (i.e. fields, forests, waterfronts etc.) outside the village | ||
| Community production | Self-produced food supply | |
| Self-produced vegetables supply | ||
| Self-produced meat and eggs supply | ||
| Impact on production and income | ||
| Infrastructure and public services | Water, electricity, energy and sanitation supply | |
| Communications and transportation supply | ||
| Basic supplies (i.e., supermarkets, commissaries, etc.) | ||
| Basic medical services |
2.3. Measure of community support
The level of community support is measured through six dimensions: eco-environment, housing condition, infrastructure and public services, community cohesion, community production, and physical activities, see Table 1. The eco-environment dimension includes two items of a village's natural environment (i.e., forests, fields, and watersides) and air quality. The housing-condition dimension consists of three items: the number and size of rooms, living conditions (i.e., heating, sanitation, and lighting facilities), and the exterior of the property and surrounding landscape. The measurements of community infrastructure and public services include basic infrastructure (i.e., water, electricity, energy, and sanitation supply), communications and transportation systems, distribution of basic supplies (i.e., groceries), and basic medical services. The community cohesion dimension includes social order and neighborhood assistance. The dimension of community production includes food self-sufficiency and the pandemic's overall impact on the household's production and income. The physical activity dimension focuses on the frequency of outdoor activities. Due to social distancing principles, we only examine the physical activities in outdoor space in private houses (i.e., the exterior of the property and roofs) or green open spaces outside villages (i.e., fields, forests, watersides). The four indicators constituting the fragility of community infrastructure and public service dimensions are binary variables characterized by whether the infrastructure services have been ever disrupted (0 is for being never disrupted, and is1 for being disrupted at least once). All the other indicators are made through the five-point Likert scale, ranging from 1 (strongly disagree, very poor, or very rare) to 5 (strongly agree, very good, or very frequent).
2.4. Socioeconomic conditions
We control for individual demographic and socioeconomic conditions in the study. The control variables include sex (male or female), age (<45 years, 45–60 years, and >60 years), educational attainment (elementary education, secondary education, and higher education), annual household income per capita (<¥3750, ¥3750–10000, ¥10000-30000, or >¥30000), and the major source of income (agriculture, non-agricultural and local, non-agricultural and non-local, and others).
2.5. The level of community lockdown and individual perceived risk of COVID-19 infection
We define low-level lockdown measures as taking daily management measures, local pandemic information reporting, conducting community cleaning and sanitization; intermediate-level measures as advocating for residents to stay at home, shutting down some or all shops and public centers, closing town/village borders to restrict access by non-residents; and high-level measures as closing town/village borders to restrict any population movement, enforcing stay at home orders for residents.
Individual perceived risk of COVID-19 infection is also measured at three different levels according to the physical distance from the nearest confirmed or suspected cases. We define low risk as perceived nearest confirmed or suspected cases occur in municipality or provincial level; medium risk as perceived nearest confirmed or suspected cases occur in county-level; high risk as perceived nearest confirmed or suspected cases occur in town, village or family level.
2.6. Statistical analysis
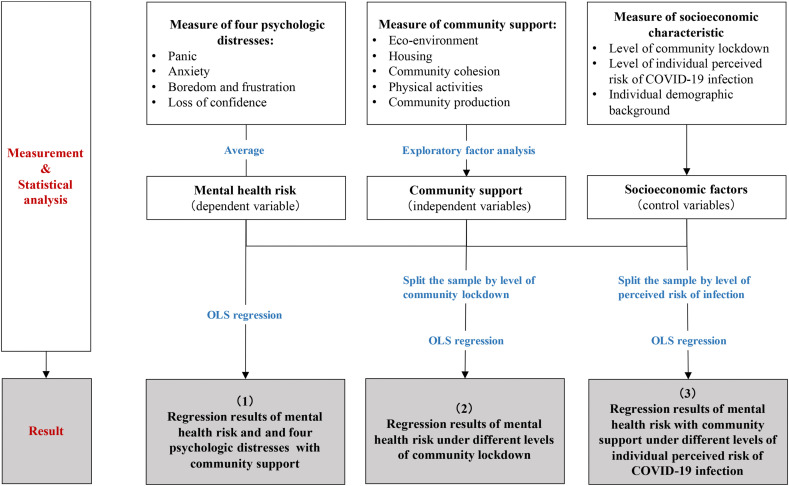
We first use exploratory factor analysis to extract the metric to obtain more valid contributing factors. Then, we apply ordinary least squares (OLS) regression to estimate the effect of community support on mental health risk and the four psychological distress indicators, controlling for socio-demographic characteristics. Further, we split the sample into three groups according to community lockdown level and use ordinary least square regressions separately to compare the effects of community support under different lockdown levels. All the statistical analyses above were performed with IBM SPSS Statistics 23 (Fig. 1 ).
Fig. 1.
Research flow analysis diagram.
3. Results
3.1. Descriptive statistics
Table 2 reports the descriptive statics of the 3892 respondents collected in this study. In terms of community support, all six dimensions show high scores. The average scores of natural environmental and housing variables are all higher than 3.6. The average score of social order reaches 4.17, which suggests that most rural communities in China are running well amid the outbreak. All items in community production score more than 3 points. Most of the respondents live in communities with middle-level lockdown (60.8%, N = 2364), while 27% (N = 1062) of the respondents are in communities with the high-level lockdown.
Table 2.
Characteristics of study participants (n = 3892).
| Mean |
Standard error |
|
| Self-reported mental health status (range 1–5) | ||
| Panic | 2.63 | 0.018 |
| Boredom and frustration | 2.65 | 0.020 |
| Anxiety | 3.07 | 0.020 |
| Loss of confidence | 1.49 | 0.011 |
| Mental health risk | 2.46 | 0.012 |
| Community Support (range 1–5) | ||
| Eco-environment | ||
| Natural environmental conditions (i.e., forests, fields, watersides etc.) | 3.82 | 0.014 |
| Air quality | 4.15 | 0.013 |
| Housing | ||
| Sufficient number of rooms | 3.64 | 0.015 |
| Housing conditions (i.e., heating, ventilation, lighting, etc.) | 3.85 | 0.014 |
| The landscape around the house | 3.60 | 0.014 |
| Community cohesion | ||
| Social order | 4.17 | 0.012 |
| Neighborhood assistance | 3.92 | 0.014 |
| Physical activities | ||
| Frequency of outdoor activities in the exterior of the property and roofs | 2.88 | 0.021 |
| Frequency of activities to open spaces (i.e. fields, forests, waterfronts etc.) outside the village | 2.08 | 0.019 |
| Community production | ||
| Self-produced food supply | 3.53 | 0.019 |
| Self-produced vegetable supply | 3.39 | 0.019 |
| Self-produced meat and eggs supply | 3.22 | 0.019 |
| Impact on production and income | 3.19 | 0.019 |
|
Number |
Percent |
|
| Infrastructure and public services | ||
| Water, electricity, energy, and sanitation supply | ||
| Once or more off of function | 928 | 23.8% |
| Never off of function | 2964 | 76.2% |
| Communications and transportation supply | ||
| Once or more off of function | 1709 | 43.9% |
| Never off of function | 2183 | 56.1% |
| Basic supplies (i.e., supermarkets, commissaries, etc.) | ||
| Once or more off of function | 848 | 21.8% |
| Never off of function | 3044 | 78.2% |
| Basic medical services | ||
| Once or more off of function | 1111 | 28.5% |
| Never off of function | 2781 | 71.5% |
| Socioeconomic characteristics | ||
| Level of community lockdown | ||
| Low level | ||
| Taking daily management measures | 252 | 6.5% |
| Reporting local pandemic situation, conducting community cleaning and sanitization | 214 | 5.5% |
| Medium level | ||
| Advocating residents to stay at home, shutting down some or all shops and public centers | 617 | 15.9% |
| Closing town/village borders to restrict access of non-residents | 1747 | 44.9% |
| High level | ||
| Closing town/village borders to restrict all population movements | 562 | 14.4% |
| Enforcing residents to stay at home | 500 | 12.8% |
| Sex | ||
| Male | 2341 | 60.1% |
| Female | 1551 | 39.9% |
| Age | ||
| <45 years | 2633 | 67.7% |
| 45–59 years | 1143 | 29.4% |
| >60 years | 116 | 3.0% |
| Education | ||
| Elementary education | 1296 | 33.3% |
| Secondary education | 936 | 24.0% |
| Higher education | 1660 | 42.7% |
| Annual household income | ||
| < ¥3750 | 1153 | 29.6% |
| ¥3750–10000 | 1731 | 44.5% |
| ¥10000-30000 | 720 | 18.5% |
| >¥30000 | 288 | 7.4% |
| Major source of income | ||
| Local agriculture, forestry, stockbreeding and fishery industry | 647 | 16.6% |
| Local non-agriculture, forestry, stockbreeding and fishery industry | 1464 | 37.6% |
| Non-local work | 1132 | 29.1% |
| Other sources | 649 | 16.7% |
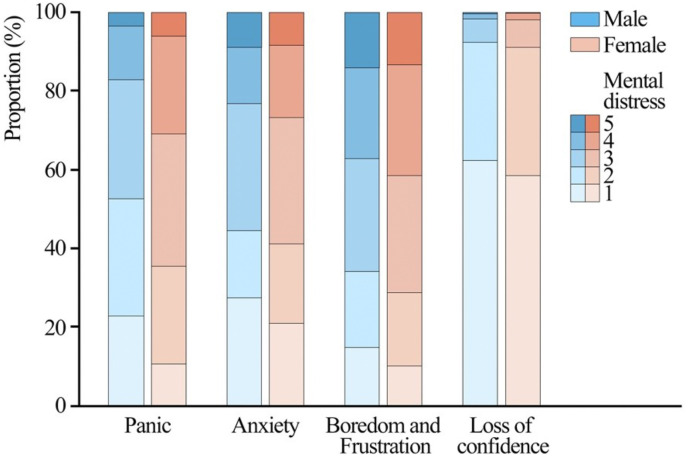
The average score for mental health risk of all respondents is 2.46. We notice the average score of anxiety is relatively high among the four categories of distress. The mental health risk is higher for female respondents (2.58) than for males (2.38). Fig. 2 shows the distribution of the reported level of each mental distress for male and female respondents separately. In general, female respondents are more vulnerable to panic, anxiety, boredom and frustration, and confidence loss. The gender difference is especially significant in the feeling of panic.
Fig. 2.
The ratio of male and female respondents reporting different level of mental distress, ranging from 1 (not distressed at all) to 5(highly distressed).
3.2. Factor analysis and regression results of mental health risk and community support
In the factor analysis of community support, we exclude all items related to infrastructure and public services because they were dummy variables. The other 13 items of community support were grouped and distinguished into five different factors, with a cumulative variance contribution rate of 71.530% (KMO = 0.801, p < 0,001). The factors describing community production consist of four items that are initially grouped into this category. Housing condition consists of two initial items, while this item (i.e. “14. What do you think of the landscape in and around your courtyard?”) was reallocated to the eco-environment scale instead. Community cohesion and physical activity consist of two items that were initially grouped into each category ( Table 3).
Table 3.
Factor analysis of the community support (including eco-environment, housing, sense of community, community production, physical activities).
| Factor loading | Accumulated Variance contribution rate% | |
|---|---|---|
| Community production | 20.200% | |
| After the COVID-19 outbreak, are you confident in being self-sufficient in vegetables? | 0.888 | |
| After the COVID-19 outbreak, are you confident in being self-sufficient on farmed meat and eggs? | 0.866 | |
| After the COVID-19 outbreak, are you confident in being self-sufficient on grains? | 0.843 | |
| Has the COVID-19 outbreak affected your family's production and income? | −0.508 | |
| Eco-environment | 35.856% | |
| What do you think of the air quality in your village/town? | 0.843 | |
| What do you think of the surrounding natural environment (forest, grassland, waterbody, etc.) in your village/town? | 0.827 | |
| What do you think of the landscape of the exterior of your property and surroundings? | 0.605 | |
| Housing | 48.475% | |
| Is there enough room and space in your house? | 0.869 | |
| What do you think about the living conditions of your house (i.e., heating, ventilation, lighting, etc.)? | 0.737 | |
| Community cohesion | 60.676% | |
| What is the current situation of community-based cooperation in your village/town after the COVID-19 outbreak? | 0.114 | |
| What is the current situation of social order in your village/town after the COVID-19 outbreak? | 0.126 | |
| Physical activity | 71.530% | |
| After the COVID-19 outbreak, how often do you go to your house's outdoor space (i.e., the exterior of your property and roof) for exercise? | 0.843 | |
| After the COVID-19 outbreak, how often do you go to the open space around your village/town (i.e., the field, waterfront, and forests) for exercise? | 0.806 |
Note: Requirements for factor analysis were assured with the KMO statistic (0.801) and Bartlett's test (p < 0.001). Items with low factor loadings (≤0.5) were excluded from a factor.
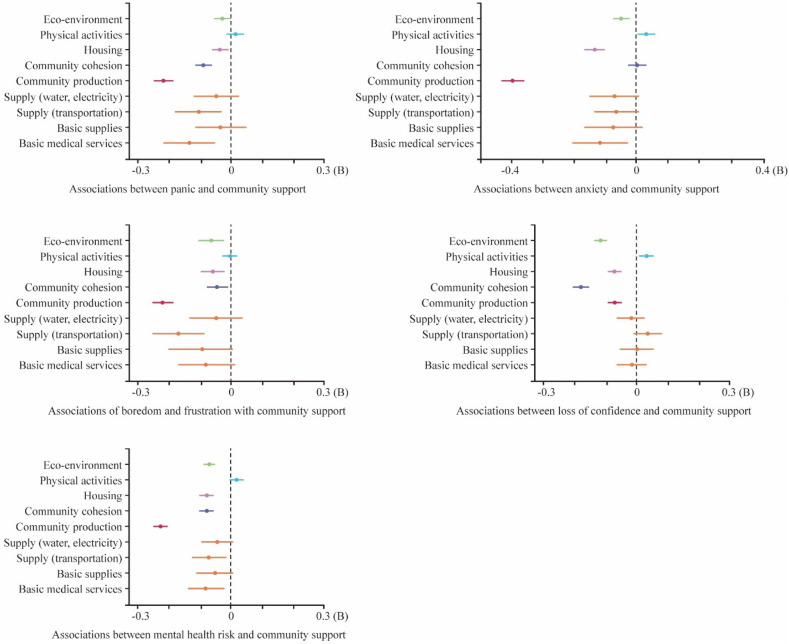
Table 4 shows the regressions on mental health risk and all four types of psychological distress, controlling individual socio-demographic characteristics. The dependent variable in the first column is a mental health risk. The capacity of community production (−0.227, 95% CI -0.249 to 0.206), basic medical services (−0.089, 95% CI -0.141 to −0.037), community cohesion (−0.084, 95% CI -0.105, −0.063), housing condition (−0.083, 95% CI -0.104, −0.062), external communications and transportation supply (−0.077, 95% CI -0.124 to-0.030), and eco-environment (−0.072, 95% CI -0.092 to −0.051) are all significantly related to reducing level of mental health risk. However, we don't find significant evidence showing that basic grocery supplies, water, electricity, energy and sanitation supply, or physical activity frequency are associated with mental health risk. According to Column 2–5, community support factors show relatively different effects on different dimensions of psychological distress. In infrastructure and public services, external communications and transportation maintenance relate to a lower sense of frustration and boredom, panic. The maintenance of basic medical services is associated with a lower sense of panic and anxiety. The higher capacity of community production and better housing conditions are related to lower levels of all four psychological symptoms. However, contrary to presupposition and previous research, physical activities' frequency is slightly and positively correlated with anxiety and confidence loss. Fig. 3 shows the different impacts of community support on mental health risk and four types of psychological distress. As for socio-demographic factors, we discovered rural females tend to have higher mental health risks and are much more vulnerable to panic. Older respondents, respondents with secondary or higher education, respondents who stayed in the community for more than 9 months, and respondents whose major incomes are from non-agricultural sectors tend to have a lower mental health risk level. They are also less likely to feel panicked, anxious, bored and frustrated.
Table 4.
Associations of mental health risk and four psychologic distresses with community support.
| Dependent Variable | Mental health risk | Panic | Anxiety | Boredom and frustration | Loss of confidence | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | 95%CI | B | 95%CI | B | 95%CI | B | 95%CI | B | 95%CI | |
| Community support | ||||||||||
| Eco-environment | −0.072*** | (-0.092, −0.051) | −0.033 | (-0.067, 0.000) | −0.058** | (-0.093, −0.023) | −0.074*** | (-0.112, −0.037) | −0.121*** | (-0.142, −0.100) |
| Physical activities | 0.019 | (-0.002, 0.040) | 0.006 | (-0.027, 0.040) | 0.037* | (0.002, 0.072) | −0.001 | (-0.039, 0.036) | 0.034** | (0.013, 0.055) |
| Housing | −0.083*** | (-0.104, −0.062) | −0.041* | (-0.074, −0.007) | −0.152*** | (-0.187, −0.116) | −0.066** | (-0.104, −0.029) | −0.074*** | (-0.095, −0.053) |
| Community cohesion | −0.084*** | (-0.105, −0.063) | −0.097*** | (-0.131, −.063) | 0.001 | (-0.035, 0.037) | −0.048* | (-0.086, −0.010) | −0.192*** | (-0.214, −0.170) |
| Community production | −0.227*** | (-0.249, −0.206) | −0.215*** | (-0.249, −0.180) | −0.399*** | (-0.435, −0.363) | −0.221*** | (-0.259, −0.182) | −0.074*** | (-0.096, −0.052) |
| Infrastructure and public services | ||||||||||
| Water, electricity, energy and sanitation supply (uninterrupted) | −0.049 | (-0.100, 0.002) | −0.052 | (-0.134, 0.030) | −0.068 | (-0.155, 0.018) | −0.048 | (-0.140, 0.044) | −0.027 | (-0.079,0.025) |
| Communication and transportation supply (uninterrupted) | −0.077** | (-0.124, −0.030) | −0.111** | (-0.186, −0.035) | −0.060 | (-0.139, 0.019) | −0.175*** | (-0.259, −0.091) | 0.037 | (-0.010, 0.085) |
| Basic supplies (uninterrupted) | −0.053 | (-0.110, 0.003) | −0.034 | (-0.125, 0.056) | −0.075 | (-0.170, 0.020) | −0.099 | (-0.201, 0.002) | −0.005 | (-0.062, 0.053) |
| Basic medical services (uninterrupted) | −0.089** | (-0.141, −0.037) | −0.140** | (-0.224, −0.056) | −0.115* | (-0.203, −0.027) | −0.082 | (-0.175, 0.012) | −0.019 | (-0.072, 0.034) |
| Socioeconomic characteristics | ||||||||||
| Sex (reference group: Male) | 0.116*** | (0.073, 0.160) | 0.365*** | (0.295, 0.434) | 0.054 | (-0.020, 0.127) | 0.025 | (-0.053, 0.103) | 0.022 | (-0.022, 0.066) |
| Age (reference group: < 45 years) | ||||||||||
| 45–59 years | −0.112*** | (-0.160, −0.064) | −0.157*** | (-0.234, −0.080) | −0.197*** | (-0.278, −0.115) | −0.127** | (-.213, −.040) | 0.031 | (-0.018, 0.080) |
| >60 years | −0.194** | (-0.316, −0.071) | −0.219* | (-0.416, −0.022) | −0.431*** | (-.639, −.224) | -.220 | (-.441, .000) | 0.096 | (-0.029, 0.221) |
| Education (reference group: elementary education) | ||||||||||
| Secondary education | −0.122*** | (-0.177, −0.066) | −0.127** | (-0.216, −0.038) | −0.084 | (-0.178, 0.010) | −0.256*** | (-0.356, −0.155) | −0.019 | (-0.076, 0.037) |
| Higher education | −0.206*** | (-0.258, −0.153) | −0.103* | (-.0187, −0.018) | −0.296*** | (-0.385, −0.207) | −0.418*** | (-0.513, −0.324) | −0.006 | (-0.060, 0.047) |
| Major source of income (reference group: Local agriculture related industry) | ||||||||||
| Local non-agriculture related industry | −0.048 | (-0.100, 0.004) | 0.032 | (-0.051, .115) | −0.168*** | (-0.256, −0.081) | −0.105* | (-0.198, −0.011) | 0.048 | (-0.005, 0.101) |
| Non-local work | 0.064 | (-0.001, 0.128) | 0.028 | (-0.075, 0.130) | 0.058 | (-0.050, 0.167) | 0.141* | (0.026, 0.256) | 0.027 | (-0.038, 0.093) |
| Other sources | 0.057 | (-0.018, 0.131) | −0.040 | (-0.158, 0.079) | 0.168** | (0.043, 0.294) | 0.041 | (-0.092, 0.175) | 0.056 | (-0.019, 0.131) |
| Annual household income (reference group: < ¥3750) | ||||||||||
| ¥3750-10000 | −0.006 | (-0.055, 0.044) | 0.000 | (-0.079, 0.080) | −0.033 | (-0.116, 0.051) | −0.009 | (-0.098, 0.080) | 0.018 | (-0.033, 0.068) |
| ¥10000-30000 | −0.026 | (-0.089, 0.037) | 0.017 | (-0.083, 0.118) | −0.108* | (-0.215, −0.002) | −0.052 | (-0.165, 0.061) | 0.040 | (-0.024, 0.104) |
| >¥30000 | −0.033 | (-0.121, 0.055) | 0.053 | (-0.088, 0.194) | −0.077 | (-0.226, 0.072) | −0.072 | (-0.230, 0.087) | −0.038 | (-0.128, 0.051) |
| Annual residency duration (reference group: < 3 months) | ||||||||||
| 3–6 months | −0.085* | (-0.167, −0.002) | −0.047 | (-0.180, 0.086) | −0.070 | (-0.210, 0.070) | −0.170* | (-0.319, −0.021) | −0.051 | (-0.135, 0.033) |
| 6–9 months | 0.011 | (-0.106, 0.127) | 0.039 | (-0.147, 0.225) | −0.074 | (-0.270, 0.123) | 0.106 | (-0.103, 0.315) | −0.029 | (-0.147, 0.090) |
| >9 months | −0.194*** | (-0.247, −0.141) | −0.084 | (-0.169, 0.001) | −0.213*** | (-0.303, −0.123) | −0.411*** | (-0.506, −0.315) | −0.068* | (-0.122, −0.014) |
| Adjusted R2 | 0.249 | 0.124 | 0.206 | 0.135 | 0.131 | |||||
| Data (N) | 3892 | 3892 | 3892 | 3892 | 3892 | |||||
Note: *p < 0.05, **p < 0.01, ***p < 0.00.
Fig. 3.
Associations of mental health risk and four psychologic distresses with community support.
3.3. Regressions results under different level of community lockdown
Table 5 shows the association between residents' mental health risk and community support under different community lockdown levels. The results show the effectiveness of different community support dimensions is dependent on the level of lockdown policy implemented. We discover that community production is always a critical factor of rural community support in the pandemic lockdown. Community cohesion ranks higher for respondents under low and medium-level community control, while infrastructure and public service are more effective for respondents under high-level community control. For the socio-demographic variables, the results are consistent with the results of the full sample regression model. Based on the regression coefficients, we listed the four most effective types of community support in each group in order. For respondents in communities of low-level lockdown these are: basic groceries supply (−0.215, −0.396 to −0.034, p < 0.05), community production (−0.209, −0.271 to −0.146, p < 0.001), water, electricity, energy, and sanitation supply (−0.154, −0.307–0.001, p < 0.05), community cohesion (−0.106, −0.167–0.046, p < 0.01). For respondents living in medium-level lockdown communities, these are community production, housing condition, community cohesion, external communications, and transportation system. For respondents living in high-level lockdown communities, these are community production, basic medical services, external communications and transportation systems, and eco-environment.
Table 5.
Association of mental health risk under different levels of community lockdown.
| Sub-groups | Low epidemic prevention level | Medium epidemic prevention level | High epidemic prevention level | |||
|---|---|---|---|---|---|---|
| B | 95%CI | B | 95%CI | B | 95%CI | |
| Community support | ||||||
| Eco-environment | −0.101** | (-0.163, −0.039) | −0.062*** | (-0.089, −0.034) | −0.076*** | (-0.115, −0.037) |
| Physical activities | 0.044 | (-0.017, 0.105) | 0.016 | (-.010, 0.042) | 0.016 | (-0.027, 0.060) |
| Housing | −0.062* | (-0.121, −0.004) | −0.103*** | (-0.130, −0.076) | −0.056** | (-0.097, −0.016) |
| Community cohesion | −0.106** | (-0.167, −0.046) | −0.093*** | (-0.120, −0.065) | −0.050* | (-0.092, −0.007) |
| Community production | −0.209*** | (-0.271, −0.146) | −0.230*** | (-0.258, −0.201) | −0.230*** | (-0.270, −0.190) |
| Infrastructure and public services | ||||||
| Water, electricity, energy and sanitation supply (uninterrupted) | −0.154* | (-0.307, −0.001) | −0.017 | (-0.081, 0.047) | −0.069 | (-0.174, 0.035) |
| Communications and transportation supply (uninterrupted) | 0.068 | (-0.075, 0.210) | -.086** | (-0.145, −0.027) | −0.126* | (-0.220, −0.031) |
| Basic supplies (uninterrupted) | −0.215* | (-0.396, −0.034) | −0.017 | (-0.088, 0.054) | −0.084 | (-0.194, 0.026) |
| Basic medical services (uninterrupted) | −0.002 | (-0.160, 0.157) | −0.073* | (-0.138, −0.008) | −0.166** | (-0.271, −0.061) |
| Socioeconomic characteristics | ||||||
| Sex (reference group: Male) | 0.238*** | (0.106, 0.370) | 0.083** | (0.029, 0.138) | 0.161*** | (0.074, 0.247) |
| Age (reference group: < 45 years) | ||||||
| 45–59 years | −0.011 | (-0.158, 0.135) | −0.164*** | (-0.223, −0.104) | −0.010 | (-0.112, 0.091) |
| >60 years | −0.212 | (-0.539, 0.115) | −0.146 | (-0.311, 0.019) | −0.247* | (-0.476, −0.018) |
| Education (reference group: elementary education) | ||||||
| Secondary education | −0.297** | (-0.467, −0.128) | −0.110** | (-0.181, −0.039) | −0.045 | (-0.154, 0.064) |
| Higher education | −0.415*** | (-0.568, −0.261) | −0.162*** | (-0.228, −0.096) | −0.197*** | (-0.304, −0.090) |
| Major source of income (reference group: Local agriculture related industry) | ||||||
| Local non- agriculture related industry | 0.034 | (-0.122, 0.191) | −0.037 | (-0.102, 0.027) | −0.114* | (-0.222, −0.007) |
| Non-local work | 0.065 | (-0.127, 0.257) | 0.070 | (-0.010, 0.151) | 0.010 | (-0.119, 0.138) |
| Other sources | −0.012 | (-0.254, 0.229) | 0.086 | (-0.005, 0.176) | 0.012 | (-0.140, 0.165) |
| Annual household income (reference group: < ¥3750) | ||||||
| ¥3750-10000 | 0.001 | (-0.145, 0.148) | 0.001 | (-0.062, 0.064) | −0.018 | (-0.114, 0.078) |
| ¥10000-30000 | −0.031 | (-0.224, 0.162) | −0.046 | (-0.125, 0.033) | 0.031 | (-0.094, 0.157) |
| >¥30000 | 0.174 | (-0.081, 0.430) | −0.037 | (-0.148, 0.074) | −0.121 | (-0.297, 0.056) |
| Annual residency duration (reference group: < 3 months) | ||||||
| 3–6 months | −0.172 | (-0.425, 0.082) | −0.124* | (-0.227, −0.021) | 0.017 | (-0.151, 0.185) |
| 6–9 months | −0.199 | (-0.580, 0.183) | 0.098 | (-0.048, 0.244) | −0.088 | (-0.313, 0.137) |
| >9 months | −0.326*** | (-0.492, −0.160) | −0.213*** | (-0.280, −0.147) | −0.103 | (-0.207, 0.000) |
| Adjusted R2 | 0.258 | 0.247 | 0.259 | |||
| Data (N) | 466 | 2364 | 1062 | |||
Note: *p < 0.05, **p < 0.01, ***p < 0.001.
3.4. Regressions results under different level of the individual perceived risk of COVID-19 infection
Table 6 shows the associations between mental health risk and community support under low, medium, and high levels of the individual perceived risk of COVID-19 infection. The performance of community cohesion and housing condition on mitigating residents' mental health risk are dependent on the level of the perceived risk of infection: the higher the perceived infection risk, the more influential the community cohesion and housing condition are. However, inconsistent with previous regression models' results, we find no significant effects of communication, transportation, and basic medical service supplies in respondents with the subsample of a high level of the perceived risk of infection. Also, a higher frequency of physical activities shows a significant positive association with mental health risk in respondents with a medium to a high level of the perceived risk of infection. Same as previous results, community production always ranks first in rural community support in the pandemic lockdown, regardless of the level of the individual perceived risk of infection. For the socio-demographic variables, the results are consistent with the regression results with the full sample. Based on the regression coefficients, we listed the four most effective types of community support in each group in order. For respondents with the low perceived risk of infection, these are community production, basic medical services, communication and transportation supply, eco-environment. For respondents with the medium perceived risk of infection, these are community production, communication and transportation supply, housing condition, community cohesion. For respondents with a low perceived risk of infection, these are community production, community cohesion, and housing condition.
Table 6.
Association of mental health risk with community support under different levels of individual perceived risk of COVID-19 infection.
| Sub-groups | Low infection risk perception | Medium infection risk perception | High infection risk perception | |||
|---|---|---|---|---|---|---|
| B | 95%CI | B | 95%CI | B | 95%CI | |
| Community support | ||||||
| Eco-environment | −0.073*** | (-0.106, −0.041) | −0.085*** | (-0.117, −0.053) | −0.056 | (-0.119, 0.007) |
| Physical activities | −0.009 | (-0.043, 0.024) | 0.033* | (0.002, 0.064) | 0.087** | (0.022, 0.152) |
| Housing | −0.056** | (-0.090, −0.022) | −0.094*** | (-0.125, −0.062) | −0.106** | (-0.171, −0.041) |
| Community cohesion | −0.067*** | (-0.101, −0.033) | −0.090*** | (-0.122, −0.057) | −0.113*** | (-0.175, −0.052) |
| Community production | −0.243*** | (-0.277, −0.209) | −0.214*** | (-0.247, −0.181) | −0.222*** | (-0.288, −0.155) |
| Infrastructure and public services | ||||||
| Water, electricity, energy and sanitation supply (uninterrupted) | −0.037 | (-0.118, 0.044) | −0.072 | (-0.148, 0.004) | −0.055 | (-0.213, 0.103) |
| Communications and transportation supply (uninterrupted) | −0.081* | (-0.153, −0.009) | −0.112** | (-0.184, −0.040) | −0.017 | (-0.170, 0.137) |
| Basic supplies (uninterrupted) | −0.032 | (-0.119, 0.055) | −0.059 | (-0.146, 0.028) | −0.079 | (-0.251, 0.093) |
| Basic medical services (uninterrupted) | −0.107** | (-0.187, −0.026) | −0.086* | (-0.166, −0.005) | −0.035 | (-0.194, 0.124) |
| Socioeconomic characteristics | ||||||
| Sex (reference group: Male) | 0.096** | (0.029, 0.164) | 0.116** | (0.050, 0.183) | 0.198** | (0.064, 0.332) |
| Age (reference group: < 45 years) | ||||||
| 45–59 years | −0.110** | (-0.188, −0.032) | −0.117** | (-0.187, −0.048) | −0.142 | (-0.296, 0.011) |
| >60 years | −0.266* | (-0.483, −0.049) | −0.117 | (-0.287, 0.053) | −0.265 | (-0.653, 0.123) |
| Education (reference group: elementary education) | ||||||
| Secondary education | −0.067 | (-0.154, 0.019) | −0.118** | (-0.204, −0.032) | −0.208* | (-0.406, −0.010) |
| Higher education | −0.168*** | (-0.253, −0.084) | −0.178*** | (-0.261, −0.095) | −0.351*** | (-0.519, −0.183) |
| Major source of income (reference group: Local agriculture related industry) | ||||||
| Local non- agriculture related industry | −0.070 | (-0.160, 0.020) | −0.075* | (-0.149, −0.001) | 0.104 | (-0.040, 0.249) |
| Non-local work | 0.071 | (-0.027, 0.169) | 0.035 | (-0.068, 0.137) | 0.086 | (-0.101, 0.273) |
| Other sources | 0.071 | (-0.048, 0.190) | 0.084 | (-0.026, .195) | −0.084 | (-0.309, 0.140) |
| Annual household income (reference group: < ¥3750) | ||||||
| ¥3750-10000 | −0.038 | (-0.115, 0.039) | 0.040 | (-0.036, 0.116) | −0.024 | (-0.180, 0.133) |
| ¥10000-30000 | −0.069 | (-0.170, 0.031) | 0.013 | (-0.081, 0.107) | 0.083 | (-0.113, 0.279) |
| >¥30000 | −0.120 | (-0.254, 0.014) | 0.026 | (-0.109, 0.161) | .030 | (-0.240, 0.299) |
| Annual residency duration (reference group: < 3 months) | ||||||
| 3–6 months | −0.085 | (-0.206, 0.035) | −0.114 | (-0.244, 0.016) | −0.136 | (-0.415, 0.142) |
| 6–9 months | 0.048 | (-0.128, 0.224) | 0.061 | (-0.121, 0.243) | −0.239 | (-0.591, 0.114) |
| >9 months | −0.209*** | (-0.293, −0.125) | −0.199*** | (-0.279, −0.118) | −0.123 | (-0.286, 0.039) |
| Adjusted R2 | 0.253 | 0.247 | 0.234 | |||
| Data (N) | 1535 | 1742 | 427 | |||
Note: *p < 0.05, **p < 0.01, ***p < 0.001.
4. Discussion
Many Chinese rural residents living in lockdown communities are at risk of mental disorders during the COVID-19 pandemic. About 20%–40% of the respondents report extraordinarily high or high levels of panic, anxiety, boredom, and frustration, and 15% of the respondents report a complete loss of confidence to combat COVID-19. Our findings suggest that lockdown policies' potential psychological consequences during the COVID-19 pandemic deserve more attention (Brooks et al., 2020). The psychological stressors work in different aspects, such as fear for disease spread, anxiety for potential economic loss, and boredom caused by isolation.
Understanding the gender difference in the impacts of the COVID-19 outbreak is a fundamental step to create equitable interventions, but it has long been neglected in practice (Wenham et al., 2020). Previous studies have found that females are likely to carry heavier social and economic burdens and suffer more from psychological disorders (Hall Kelli et al., 2020; Qiu et al., 2017). We further show that rural female respondents have higher mental health risks during the pandemic and also are more vulnerable to panic, anxiety, boredom, and frustration. Therefore, we urge on a policy framework of higher gender equity in the COVID-19 response.
Many studies have confirmed the positive role of community support (e.g., adequate information and basic supplies, communication, and social collaboration) in mitigating psychological distress (Manuell and Cukor, 2011). This study provides consistent findings in the context of the COVID-19 pandemic. We also introduced a systematic analytical framework, which incorporates socioeconomic, environmental, and behavioral factors of community support, to analyze residents' well-being in lockdown communities. We find that community production capacity has the largest impact on reducing mental health risks, followed by the stability of basic medical services, community cohesion, housing condition, the stability of communications and transportation supply, and the eco-environment. It is also worth noting that we conducted this study in the context of national community containment with huge scale and influence unprecedented in history, not even during the SARS or Ebola pandemic. Global policies and experiences in the past year have shown that large-scale social distancing and community containment are the most effective methods in response to the COVID-19 pandemic until effective and safe vaccines appear. Therefore, our study is meaningful to understanding how to secure material and mental support at the community level facing the pandemic not yet over and for future public health emergencies.
Specifically, we discuss the importance of a healthy living environment, resilient community infrastructure and public service system, and community production capacity for residents' mental health during catastrophic events. Comfortable eco-environment and housing conditions are significantly associated with lower mental health risks, as we predicted. We also find that mental health disorders are higher if basic medical services and external transportation and communication systems are fragile. Getting basic medical service and health care is important to those confirmed or potential COVID-19 infected residents and others with basic diseases or higher health risks (e.g., older adults and children) (Benedict, 2008; Zhang and Liu, 2007). The wise use of communication systems and social media during lockdown can improve voluntary compliance (Wilder-Smith et al., 2020). The rise of online businesses and education platforms has largely normalized daily work and schooling routines, contributing to maintaining psychological health (Wang et al., 2020). It is worth noting that community production is the most influential factor in mitigating mental health disorders in most scenarios. The food consumption pattern in Chinese rural areas is different from that in cities, as rural residents largely rely on semi-subsistence farming (Gale, 2005). The interruption of agricultural production and semi-subsistence could lead rural households to face food crises and economic loss, which in turn impair their mental health (Akter and Basher, 2014; Berry et al., 2015).
Further, we find that a harmonious social environment is more positively associated with better mental health when the lockdown measures are modest, and when the individual perceived risk of COVID-19 infection are higher. WHO guidelines have listed community-based collaboration and communication as a major necessity in pandemic control (WHO, 2020b). Our findings further indicate that when governments apply relatively modest lockdown policies or when individuals are under a higher burden for potential infection, rural residents attach greater importance to community cohesion (i.e., social order, community-based collaboration, and neighborhood assistance). In many rural communities, existing family and social networks provide the basis for creating an intimate and supportive social environment, which can protect residents' psychological well-being in the context of isolation. In communities that adopted stricter lockdown measures, the disruption of basic medical services, and the disruption of external transportation or communication systems become more effective predictors of mental health risks. The importance of housing conditions increases when rural residents perceive a higher risk of infection. The housing condition, medical services, transportation, and communication systems tend to be more unsatisfactory and fragile in rural communities. The government should take these disadvantages into account when designing lockdown policies for public health issues.
The emergency lockdown has had a huge impact on rural production and household income, and exposed the inability and deficiency of basic infrastructure, medical service, social care and rural governance ability. Agricultural production is the determinant of rural livelihood and national food security (Monica et al., 2020). The COVID-19 negatively influenced the food supply chain, and many countries have adopted food export control measures (Yuan et al., 2020). In the post-epidemic period, the government needs to improve the production and supply chain by building a modern and intelligent agricultural system that integrates the planting, processing, storage, and distribution of agricultural products to ensure national food security and rural household productivity. Rural living environment and public service must make more livable, resilient, and healthier rural communities. First, it is necessary to strengthen the construction of fragile infrastructures such as water, power, and internet supply by building more resilient infrastructure system in the face of emergencies. Second, it is necessary to design a green space system that connects the natural environment, community public space, and individual residents to provide space for public and private activities. Besides, based on promoting rural medical and health services, it is necessary to strengthen the construction of a social security system for left-behind children, women, and the elderly in rural areas to ensure health equity and overall harmony in rural communities. It is also necessary to create a civic culture by stabilizing the rural community bonds and enhancing the power of ritual and moral rules. A governance structure that combines the rule of government law and morality is likely to improve rural community's ability to quickly and effectively respond in public emergencies.
This study has numerous limitations. First, the cross-sectional design of the study limits evidence of causality that might support future policymaking. A second limitation is that no data on prior history of mental health outcomes are available before the COVID-19 outbreak, so it cannot be entirely sure whether some disorders were already existed predated this pandemic. Finally, the study accepts randomly sampled and semi-targeted voluntary participants across the country, potentially introducing selection bias into the results. Nevertheless, the associations between reported community support and mental health distresses are consistent with other existing similar studies. We hope to conduct follow-up surveys of the rural residents' mental health and community improvement in further research. We also plan to conduct comparative research on returning migrant workers and urban residents.
5. Conclusion
This study examines Chinese rural residents' mental health risk under emergency lockdown during the COVID-19 pandemic. It investigates how the environmental, socioeconomic, and behavioral factors of community support affect mental health and psychological distress in this context. We also compare the effectiveness of community support under modest and strict lockdown policies and different levels of the individual perceived risk of COVID-19 infection. The results suggest that the COVID-19 pandemic and lockdown policies have negative psychological consequences, especially for rural females. The capacity for community production has the largest impact on reducing mental health risks, followed by the stability of basic medical services, community cohesion, housing condition, the stability of communications and transportation supply, and the eco-environment. Community cohesion is more positively associated with respondents' mental health under modest lockdown and higher perceived infection risk. At the same time, the basic medical service, communication, and transportation system are more helpful for respondents under strict lockdown and lower perceived infection risk.
Finally, we propose that more attention should be addressed to the psychological well-being of the rural residents with lockdown experience during and after the pandemic. We also discuss the necessity of building rural communities with a healthy living environment, resilient infrastructure systems, and stronger socioeconomic capacities. This study has implications for lockdown policies in the COVID-19 pandemic and has implications for rural planning in the future.
Author statement
Ziyu Jia: Investigation, Formal analysis, Writing – original draft, Shijia Xu: Investigation, Formal analysis, Writing – original draft, Zican Zhang: Investigation, Formal analysis, Data curation, Writing – original draft, Zhengyu Cheng, Haoqing Han, Haoxiang Xu, Mingtian Wang, Hong Zhang: Investigation, Zhengxu Zhou: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision, Funding acquisition, Yi Zhou: Methodology, Formal analysis, Writing – review & editing, Supervision
Funding
This work was supported by the National Natural Science Foundation of China (51508298), Humanity and Social Science Foundation of Ministry of Education of China (19YJC840064).
Declaration of competing interest
We declare no competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jrurstud.2021.01.015.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Akpinar A. How is quality of urban green spaces associated with physical activity and health? Urban For. Urban Green. 2016;16:76–83. [Google Scholar]
- Akter S., Basher S.A. The impacts of food price and income shocks on household food security and economic well-being: evidence from rural Bangladesh. Global Environ. Change. 2014;25:150–162. [Google Scholar]
- Amin V., Fletcher J., Behrman J., et al. IZA Discussion Papers; 2019. Mental health, schooling attainment and polygenic scores: are there significant gene-environment associations?[J] p. 12452. [DOI] [Google Scholar]
- Arden M.A., Chilcot J. Health psychology and the coronavirus (COVID‐19) global pandemic: a call for research. Br. J. Health Psychol. 2020;25(2):231–232. doi: 10.1111/bjhp.12414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedict R.E. Quality medical homes: meeting children's needs for therapeutic and supportive services. Pediatrics. 2008;121:e127–e134. doi: 10.1542/peds.2007-0066. [DOI] [PubMed] [Google Scholar]
- Bergmans R.S., Sadler R.C., Wolfson J.A., et al. Moderation of the association between individual food security and poor mental health by the local food environment among adult residents of flint, Michigan[J] Health equity. 2019;3(1):264–274. doi: 10.1089/heq.2018.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry E.M., Sandro D., Barbara B., Alexandre M., Piero C. Food security and sustainability: can one exist without the other? Publ. Health Nutr. 2015;18:2293–2302. doi: 10.1017/S136898001500021X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bratman G.N., Anderson C.B., Berman M.G., et al. Nature and mental health: an ecosystem service perspective[J] Science advances. 2019;5(7) doi: 10.1126/sciadv.aax0903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence[J] Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florian L., Peter K., Leila H., Fabian S., Heike T., Philipp S., Stefan W., C P.J., Marcella R., Michael D., Andreas M. City living and urban upbringing affect neural social stress processing in humans. Nature. 2011;474:498–501. doi: 10.1038/nature10190. [DOI] [PubMed] [Google Scholar]
- Friesinger J.G., Topor A., Bøe T.D., et al. Vol. 57. Health & place; 2019. Studies regarding supported housing and the built environment for people with mental health problems: a mixed-methods literature review[J] pp. 44–53. [DOI] [PubMed] [Google Scholar]
- Gale H.F. Vol. 2005. USDA-ERS Economic Research Report; 2005. Commercialization of food consumption in rural China[J] 8. [DOI] [Google Scholar]
- Geng D., Innes J., Wu W., Wang G. Impacts of COVID-19 pandemic on urban park visitation: a global analysis. J. For. Res. 2020:1–15. doi: 10.1007/s11676-020-01249-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Fu M., Liu D., et al. Child abuse & neglect; 2020. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents[J] p. 104667. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall Kelli Stidham, Samari Goleen, Garbers Samantha, et al. Centring sexual and reproductive health and justice in the global COVID-19 response. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamadani J.D., Hasan M.I., Baldi A.J., et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series[J] The Lancet Global Health. 2020;8(11):e1380–e1389. doi: 10.1016/S2214-109X(20)30366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrero J., Gracia E. Measuring perceived community support: factorial structure, longitudinal invariance, and predictive validity of the PCSQ (perceived community support questionnaire) J. Community Psychol. 2007;35:197–217. [Google Scholar]
- Heymann D.L., Shindo N. COVID-19: what is next for public health?[J] Lancet. 2020;395(10224):542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A., Grigsby-Toussaint D.S. Cities & Health; 2020. Housing stability and the residential context of the COVID-19 pandemic[J] pp. 1–3. [DOI] [Google Scholar]
- Kansiime A Monica K., et al. Vol. 137. World Development; 2020. COVID-19 implications on household income and food security in Kenya and Uganda: findings from a rapid assessment. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khosravi M. Perceived risk of COVID-19 pandemic: the role of public worry and trust. Electron J Gen Med. 2020;17(4) [Google Scholar]
- Kiesha P., Yang L., Tim R., Adam J.K., Rosalind M.E., Nicholas D. The effect of control strategies that reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China. Lancet Public Health. 2020;5(5):e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control[J] Brain Behav. Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin B.B., Gaston K.J., Fuller R.A., Wu D., Shanahan D.F. How green is your garden?: urban form and socio-demographic factors influence yard vegetation, visitation, and ecosystem service benefits. Landsc. Urban Plann. 2017;157:239–246. [Google Scholar]
- Liu Y., Zhang F., Wu F., Liu Y., Li Z. The subjective well-being of migrants in Guangzhou, China: the impacts of the social and physical environment. Cities. 2017;60(PT.A):333–342. [Google Scholar]
- Lu Y. Using Google Street View to investigate the association between street greenery and physical activity[J] Landsc. Urban Plann. 2019;191:103435. [Google Scholar]
- Manuell M.E., Cukor J. Mother Nature versus human nature: public compliance with evacuation and quarantine. Disasters. 2011;35:417–442. doi: 10.1111/j.1467-7717.2010.01219.x. [DOI] [PubMed] [Google Scholar]
- Montazeri A., Harirchi A.M., Shariati M., Garmaroudi G., Ebadi M., Fateh A. The 12-item General Health Questionnaire (GHQ-12): translation and validation study of the Iranian version. Health Qual. Life Outcome. 2003;1:66. doi: 10.1186/1477-7525-1-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery S.A., Åsberg M., Montgomery S.A., Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry the Journal of Mental Science. 1979;134:382. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Mullins N., Power R.A., Fisher H.L., et al. Polygenic interactions with environmental adversity in the aetiology of major depressive disorder[J] Psychol. Med. 2016;46(4):759–770. doi: 10.1017/S0033291715002172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata J.M. Rapid scale-up of telehealth during the COVID-19 pandemic and implications for subspecialty care in rural areas[J] J. Rural Health. 2020 doi: 10.1111/jrh.12433. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic[J] N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Phillipson J., Gorton M., Turner R., et al. The COVID-19 pandemic and its implications for rural economies[J] Sustainability. 2020;12(10):3973. [Google Scholar]
- Qiu P., Eric D., Caine Fengsu, Hou Catherine, Cerulli Marsha. Depression as seen through the eyes of rural Chinese women: implications for help-seeking and the future of mental health care in China. J. Affect. Disord. 2017;227:38–47. doi: 10.1016/j.jad.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature[J] Asian journal of psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranscombe P. Rural areas at risk during COVID-19 pandemic[J] Lancet Infect. Dis. 2020;20(5):545. doi: 10.1016/S1473-3099(20)30301-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin G.J., Wessely S. The psychological effects of quarantining a city. Rmd Open. 2020;368 doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- Slater S.J., Christiana R.W., Gustat J. Peer Reviewed: recommendations for keeping parks and green space accessible for mental and physical health during COVID-19 and other pandemics[J] Prev. Chronic Dis. 2020;17:200204. doi: 10.5888/pcd17.200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sophie W., Lee B., Tanith R., Margaret W., David T., Ben B. Effects on mental health of a UK welfare reform, Universal Credit: a longitudinal controlled study., the Lancet. Publ. Health. 2020;5(3):e157–e164. doi: 10.1016/S2468-2667(20)30026-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Summers-Gabr N.M. Rural–urban mental health disparities in the United States during COVID-19. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S222–S224. doi: 10.1037/tra0000871. [DOI] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., et al. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA[J] The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet Public Health The environment we live in. Lancet Public Health. 2017;2:e483. doi: 10.1016/S2468-2667(17)30199-8. [DOI] [PubMed] [Google Scholar]
- Topp C.W., Østergaard S.D., Søndergaard S., Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother. Psychosom. 2015;84:167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- Tsai J., Wilson M. COVID-19: a potential public health problem for homeless populations[J] The Lancet Public Health. 2020;5(4):e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China[J] Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., et al. Mitigate the effects of home confinement on children during the COVID-19 outbreak[J] Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . Homepage World Health Organization; 2020. WHO Health Emergency Dashboard WHO (COVID-19) [Google Scholar]
- WHO . 2020. COVID-19 strategic preparedness and response plan: operational planning guidelines to support country preparedness and response. [Google Scholar]
- Wilder-Smith A., Freedman D.O., Xiang Y.T., Yang Y., Li W., et al. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak[J] J. Trav. Med. 2020;27(2) doi: 10.1093/jtm/taaa020. taaa020. 2020 Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed[J]. The Lancet Psychiatry, 7(3): 228-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y., Torok M.E. Taking the right measures to control COVID-19[J] Lancet Infect. Dis. 2020;20(5):523–524. doi: 10.1016/S1473-3099(20)30152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Li W., Zhang Q., et al. Mental health services for older adults in China during the COVID-19 outbreak[J] The Lancet Psychiatry. 2020;7(4):e19. doi: 10.1016/S2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan F., Yang P., Feng X.U., et al. Impact of COVID-19 epidemic on the international food supply chain and countermeasures of shandong province[J] Asian Agricultural Research. 2020;2020(8) [Google Scholar]
- Zhang W., Liu G. Childlessness, psychological well-being, and life satisfaction among the elderly in China. J. Cross-Cult. Gerontol. 2007;22:185–203. doi: 10.1007/s10823-007-9037-3. [DOI] [PubMed] [Google Scholar]
- Zhu S., Wu Y., Zhu C., et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements[J] Brain Behav. Immun. 2020;87:56–58. doi: 10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.