Introduction
Gender refers to gender identity and/or sociocultural roles, whereas sex refers to attributes that characterize biologic sex. Gender and sex each play a role in the development and progression of CKD, yet these two terms are often inappropriately used interchangeably in scientific and medical literature. In many studies, common gender identity category terms (woman and man) and sex category terms (female and male) are erroneously treated as synonymous. As such, we generally cannot empirically distinguish between the effects of gender and sex when interpreting results in most clinical studies. However, it is likely that important gender-related differences exist in nephrology in terms of access to medical care, dietary intake, medication adherence, or choice of ESKD treatment. Marked sex-related differences in kidney pathophysiology, immunology, and response to therapy may also interact with gendered variables to influence health outcomes.
Gender is increasingly being recognized as a fluid concept, as is evident through increased gender research, knowledge, and dialogue. Traditionally, gender has been viewed as a binary concept with woman/girl or man/boy being cisgender individuals whose gender identity aligns with their sex assigned at birth. However, for some individuals, their gender identity does not fit neatly into these two categories. Examples include transgender (gender identity and/or gender expression not aligning with sex assigned at birth), gender nonconforming or nonbinary (gender identity and/or expression not aligning with society’s perception of how one should look or act on the basis of sex assigned at birth), and Two-Spirit (individuals believed to be born with both male and female spirits) individuals. Furthermore, femininity and masculinity scales have been shown to better reflect the range of gender diversity than standard categorical gender measures and have been linked to important health outcomes.
How Does Gender Affect Care for Patients with CKD?
Using the limited binary definition, significant gender disparities exist in the prevalence of kidney disease. Despite the important sex- and gender-related divergence in disease course and outcomes, Kidney Diseases Improving Global Outcomes guidelines for the management of CKD and its complications remain sex- and gender-blind. Examples where sex and gendered factors play important roles in kidney care include anemia targets, fracture risk, kidney transplant outcomes, KRT initiation and maintenance, and mortality.
The challenges of including race as a variable in the Chronic Kidney Disease Epidemiology Collaboration equation have recently been outlined (1). Similarly, we highlight that different challenges exist with the inclusion of sex/gender in the calculation of eGFR (2) and risk of kidney failure (3). It is unclear if sex or gender should be considered in this calculation because the studies included in the derivation and validation of the equation did not specify how sex and/or gender were collected or used. As such, estimation of kidney function and risk of kidney failure in gender-diverse populations is unclear with important implications. Specifically, this is pertinent for drug dosing, referral to nephrology, transplant eligibility, and initiation and prescription of dialysis, as highlighted in a patient report of a transgender man with CKD being evaluated for kidney transplant (4).
CKD Care and the Transgender Community: Knowledge Gaps
Globally, the medical literature estimates that 0.3%–0.5% of the population identify as transgender, but studies suggest that 30%–50% of transgender individuals do not disclose their gender identity to health care providers; therefore, the prevalence may actually be higher (5). As per the National Transgender Discrimination Survey Report on Health and Health Care, ≥80% of transgender individuals have either used gender-affirming hormone therapy or plan to use it. Although limited data suggest adverse cardiovascular effects of gender-affirming hormone therapy, no literature exists examining the effects of exogenous sex hormone therapy or gonadectomy on kidney function in the transgender population, a growing and medically underserved group worldwide. These data suggest that laboratory reference intervals need to be established for transgender patients being treated with gender-affirming hormone therapy as these may vary depending on patients’ biochemical sex hormone configuration (6). Recent studies have examined the association between initiation of gender-affirming hormone therapy and laboratory parameters in both transgender women (having estrogen and antiandrogen therapy, such as spironolactone) and transgender men (having testosterone therapy). In general, we know that gender-affirming hormone therapy can alter body composition in terms of body fat and lean body mass and that creatinine values are proportional to muscle mass; furthermore, spironolactone is recommended for treatment of resistant hypertension and is associated with reduced BP, eGFR, and proteinuria. To date, studies suggest a decrease or no effect of estrogen or antiandrogen therapy on serum creatinine in transgender women and that testosterone therapy in transgender men is associated with an increase in creatinine, but the true effect of sex hormone therapy on kidney function remains unclear.
Furthermore, the formulation and route of administration of gender-affirming hormone therapy may also play a role in kidney function. Feminizing hormone therapy can include oral, transdermal, or injectable estradiol therapy, and masculinizing hormone therapy can include either transdermal or injectable testosterone therapy. Each formulation has its own pharmacokinetic properties to consider, such as whether the exogenous sex hormone is absorbed from the gastrointestinal tract or the skin integument, is subject to first-pass hepatic metabolism, and is characterized by steady systemic levels or by levels with peak and trough variation, as well as the role of kidney excretion. There is a need to better understand the effects of the differing gender-affirming hormone therapies not only on kidney function but also on their safety and potential risks, including venous thromboembolic, cardiovascular, mental health, and cancer outcomes. To our knowledge, there is no published literature evaluating CKD prevalence and outcomes in the transgender population, with the available information being limited to small numbers of patient reports. We and others have shown that sex hormones in the form of contraception (7), postmenopausal hormone therapy (8,9), and testosterone replacement therapy (10) are implicated in the development and progression of CKD, but the effects of gender-affirming hormone therapy or gonadectomy on kidney function are unclear. The National Institutes of Health has recently highlighted the urgent need to delineate the relationship between sex hormones and kidney disease development and progression (11).
The Future of Gender and CKD: A Road Map to Gender-Inclusive Kidney Care and Research
Transgender and gender-diverse individuals experience significant health disparities and often report negative experiences while accessing health care resources, leading to decreased interaction with the health care system due to fears of discrimination. Health care providers are caring for an increasing number of gender-diverse individuals with or at risk of CKD, and facing uncertainty in how gender-affirming hormone therapy or gonadectomy or a person’s gender identity may affect kidney and other health outcomes. In this context, they may be tempted to attribute acute or chronic illness to these treatments, although in the absence of research, these clinical quandaries remain unanswered.
The theme of World Kidney Day 2020 is “Kidney Health for Everyone Everywhere—from Prevention to Detection and Equitable Access to Care.” A first step in reaching this laudable goal lies in acknowledging the urgent need to understand how sex and gendered factors affect kidney function and care, with the aim to prevent and treat CKD. We propose a “road map” to sex- and gender-inclusive clinical kidney research and care (Figure 1). New foundational knowledge and research capacity are necessary for developing sex- and gender-inclusive approaches for the prevention, diagnosis, and treatment of kidney disease moving forward.
Figure 1.
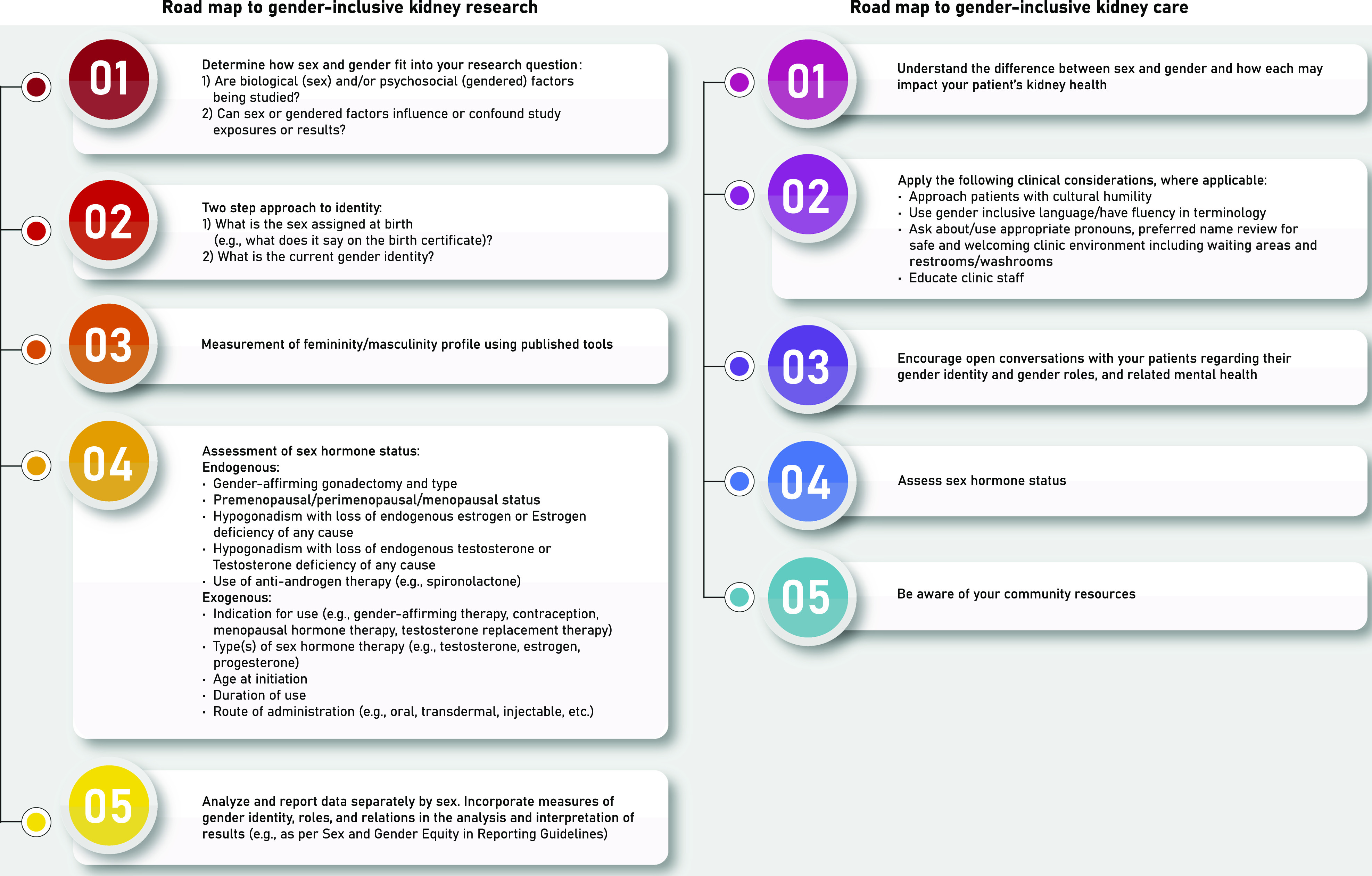
Road map to gender-inclusive clinical kidney research and care.
Disclosures
All authors have nothing to disclose.
Funding
None.
Acknowledgments
We thank Alexa Desjarlais for graphic design.
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or CJASN. Responsibility for the information and views expressed herein lies entirely with the author(s).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Eneanya ND, Yang W, Reese PP: Reconsidering the consequences of using race to estimate kidney function. JAMA 322: 113–114, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate [published correction appears in Ann Intern Med 155: 408, 2011]. Ann Intern Med 150: 604–612, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tangri N, Grams ME, Levey AS, Coresh J, Appel LJ, Astor BC, Chodick G, Collins AJ, Djurdjev O, Elley CR, Evans M, Garg AX, Hallan SI, Inker LA, Ito S, Jee SH, Kovesdy CP, Kronenberg F, Heerspink HJ, Marks A, Nadkarni GN, Navaneethan SD, Nelson RG, Titze S, Sarnak MJ, Stengel B, Woodward M, Iseki K; CKD Prognosis Consortium: Multinational assessment of accuracy of equations for predicting risk of kidney failure: A meta-analysis [published correction appears in JAMA 315: 822, 2016]. JAMA 315: 164–174, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitley CT, Greene DN: Transgender man being evaluated for a kidney transplant. Clin Chem 63: 1680–1683, 2017. [DOI] [PubMed] [Google Scholar]
- 5.Sequeira GM, Ray KN, Miller E, Coulter RWS: Transgender youth’s disclosure of gender identity to providers outside of specialized gender centers. J Adolesc Health 66: 691–698, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldstein Z, Corneil TA, Greene DN: When gender identity doesn’t equal sex recorded at birth: The role of the laboratory in providing effective healthcare to the transgender community. Clin Chem 63: 1342–1352, 2017. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed SB, Hovind P, Parving HH, Rossing P, Price DA, Laffel LM, Lansang MC, Stevanovic R, Fisher ND, Hollenberg NK: Oral contraceptives, angiotensin-dependent renal vasoconstriction, and risk of diabetic nephropathy. Diabetes Care 28: 1988–1994, 2005. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed SB, Culleton BF, Tonelli M, Klarenbach SW, Macrae JM, Zhang J, Hemmelgarn BR; Alberta Kidney Disease Network : Oral estrogen therapy in postmenopausal women is associated with loss of kidney function. Kidney Int 74: 370–376, 2008. [DOI] [PubMed] [Google Scholar]
- 9.Monster TB, Janssen WM, de Jong PE, de Jong-van den Berg LT; Prevention of Renal and Vascular End Stage Disease Study Group : Oral contraceptive use and hormone replacement therapy are associated with microalbuminuria. Arch Intern Med 161: 2000–2005, 2001. [DOI] [PubMed] [Google Scholar]
- 10.Filler G, Ramsaroop A, Stein R, Grant C, Marants R, So A, McIntyre C: Is testosterone detrimental to renal function? Kidney Int Rep 1: 306–310, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bairey Merz CN, Dember LM, Ingelfinger JR, Vinson A, Neugarten J, Sandberg KL, Sullivan JC, Maric-Bilkan C, Rankin TL, Kimmel PL, Star RA; Participants of the National Institute of Diabetes and Digestive and Kidney Diseases Workshop on “Sex and the Kidneys” : Sex and the kidneys: Current understanding and research opportunities. Nat Rev Nephrol 15: 776–783, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]


