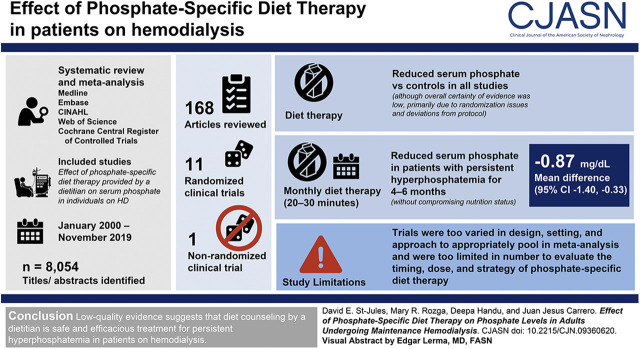
Visual Abstract
Keywords: hyperphosphatemia, nutrition, chronic kidney disease, ESRD, hemodialysis, phosphorus
Abstract
Background and objectives
Hyperphosphatemia is a persistent problem in individuals undergoing maintenance hemodialysis, which may contribute to vascular and bone complications. In some dialysis centers, dietitians work with patients to help them manage serum phosphate. Given the regularity of hyperphosphatemia in this population and constraints on kidney dietitian time, the authors aimed to evaluate the evidence for this practice.
Design, setting, participants, & measurements
There was a systematic review and meta-analysis of clinical trials. MEDLINE, Embase, CINAHL, Web of Science, Cochrane Central Register of Controlled Trials, and other databases were searched for controlled trials published from January 2000 until November 2019 in the English language. Included studies were required to examine the effect of phosphate-specific diet therapy provided by a dietitian on serum phosphate in individuals on hemodialysis. Risk of bias and certainty of evidence were assessed using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) method.
Results
Of the 8054 titles/abstracts identified, 168 articles were reviewed, and 12 clinical trials (11 randomized, one nonrandomized) were included. Diet therapy reduced serum phosphate compared with controls in all studies, reaching statistical significance in eight studies, although overall certainty of evidence was low, primarily due to randomization issues and deviations from protocol. Monthly diet therapy (20–30 minutes) significantly lowered serum phosphate in patients with persistent hyperphosphatemia for 4–6 months, without compromising nutrition status (mean difference, −0.87 mg/dl; 95% confidence interval, −1.40 to −0.33 mg/dl), but appeared unlikely to maintain these effects if discontinued. Unfortunately, trials were too varied in design, setting, and approach to appropriately pool in meta-analysis, and were too limited in number to evaluate the timing, dose, and strategy of phosphate-specific diet therapy.
Conclusions
There is low-quality evidence that monthly diet therapy by a dietitian appears to be a safe and efficacious treatment for persistent hyperphosphatemia in patients on HD.
Introduction
Excess dietary phosphate intake likely contributes to cardiovascular and bone diseases in individuals with CKD (1). CKD–mineral and bone disorder (CKD-MBD) describes the unique presentation of cardiovascular and bone conditions in individuals with CKD, and the underlining metabolic derangements of calcium and phosphate metabolism that contribute to these outcomes (2). The 2020 Kidney Disease Outcomes Quality Initiative (KDOQI) Clinical Practice Guidelines for Nutrition in CKD recommend that patients with stages 3a–5D CKD adjust their dietary phosphate intake to maintain serum phosphate in the normal range (Grading of Recommendations, Assessment, Development, and Evaluations [GRADE] evidence 1B) (3).
To address hyperphosphatemia while managing other diet-related disease complications, dietitians develop dietary interventions tailored to a patient’s specific needs, interests, and abilities (4). Dietary phosphate restrictions are a central component of the diet prescribed for people with kidney disease and one of the main focuses of counseling by kidney dietitians (5). However, even in hemodialysis (HD) clinics with access to kidney dietitians, patients have knowledge deficits and report difficulties tracking nutrients such as phosphate (6,7), and approximately half of patients on HD have predialysis hyperphosphatemia (serum phosphate levels >5.5 mg/dl) (8,9). Given the constraints on dietitian time (10) and regularity of hyperphosphatemia, the efficacy of phosphate-specific diet therapy and its potential to further improve phosphate management in this population should be examined.
As a complement to the 2020 National Kidney Foundation and Academy of Nutrition and Dietetics KDOQI Clinical Practice Guidelines for Nutrition in CKD (3), a systematic review and meta-analysis of controlled trials was conducted to examine the following research question: In adults with CKD, what is the effect of phosphate-specific diet therapy delivered by a dietitian (or international equivalent) on serum phosphate levels?
Materials and Methods
The protocol for this systematic review adhered to PRISMA guidelines (Supplemental Appendix 1) (11) and was registered at Open Science Framework (osf.io/eaqk7) (12).
Eligibility Criteria and Search Plan
Eligibility criteria were determined a priori (Table 1): studies were eligible if they examined adults with CKD (population) who received phosphate-focused interventions provided by a dietitian or international equivalent (intervention), compared with individuals who received standard care, which may include different or less-intensive care from a dietitian (comparison), and reported primary outcomes that were nutrition related (outcomes). Health and adverse outcomes were explored as secondary outcomes. Only clinical trials published in the English language from 2000 until November 23, 2019 were included.
Table 1.
Eligibility criteria for a systematic review and meta-analysis examining the effect of phosphate-specific diet therapy by a dietitian on phosphate levels
| Criteria | Include | Exclude |
|---|---|---|
| Population | Adults ≥18 yr of age | Population includes individuals <18 yr of age |
| Human | ||
| With CKD | At risk for CKD, cancer, or other terminal/serious conditions | |
| Stages 2–5 | ||
| Pre- and postdialysis | ||
| With or without diabetes | ||
| Pre- and post-transplant | ||
| Intervention | Diet therapy provided by a dietitian or international equivalent | Dietary interventions not delivered by a dietitian or international equivalent |
| Diet therapy focused on reducing phosphate levels | Interventions comparing types of oral nutrition supplements or intradialytic parenteral nutrition, but no other differences in dietitian care between groups | |
| Comparison | Must have a comparison group that is either | Has no comparison group |
| Not receiving an intervention from a dietitian | Receives same intervention from a dietitian as the intervention group (e.g., a different aspect of CKD care is altered, but not care from a diet therapy) | |
| Is receiving a different intervention from a dietitian (e.g., education/counseling for low protein diet from and dietitian versus standard care from a dietitian) | Supplement study in which the supplement changes but counseling from a dietitian is not different between groups | |
| Study design | Randomized controlled trials, nonrandomized controlled trials, quasi-experimental trials; systematic reviews and guidelines will be reviewed for relevant references | Observational studies, retrospective studies, noncontrolled trials, case reports, narrative reviews |
| Outcomes | Primary outcomes of interest/goals of diet therapy | Outcomes that are not primary outcomes of interest or goals of diet therapy |
| Setting | Clinical or outpatient | No limits |
| Size of study group | ≥6 participants in each arm | <6 participants in each arm |
| Study drop-out rate | No limits | No limits |
| Yr range | January 1, 2000 to search date of November 23, 2019 | Before 2000 or after the search date of November 23, 2019 |
| Language | English | Not in English |
Peer-reviewed literature was searched by an information specialist using MEDLINE (Ovid), Embase (Ovid), CINAHL (Ebsco), Web of Science, Cochrane Central Register of Controlled Trials (Ovid), Cochrane Database of Systematic Reviews (Ovid), Health Technology Assessment Database (Ovid), and Database of Abstracts of Reviews of Effects (Ovid) databases (Supplemental Appendix 2). Because only one trial was conducted in a non-HD population, authors narrowed the scope of the analyses a posteriori to the HD population (13).
Study Selection
Results from the database searches were uploaded and screened using Rayyan software (14). Potentially included titles/abstracts were screened independently by two reviewers (M.R. and D.H.), and discrepancies were discussed until consensus was reached. All included titles/abstracts progressed to full-text review, which was conducted independently by two reviewers (M.R. and D.H.). Studies not reporting group sample size, mean change, and variance (or prepost values) in the primary outcome for each group were excluded in the meta-analysis, but were included in narrative synthesis. When eligibility was uncertain or data were incomplete, authors attempted to contact the studies’ corresponding authors to clarify details and provide additional data.
Data Extraction
A data extraction template was developed in Microsoft Excel, reviewed by study authors, tested, and used for data extraction for each study. Data extracted included bibliographic information, sample characteristics (age, sex, dialysis type and vintage, baseline phosphate status, dietary phosphate intake), intervention description (duration and follow-up duration, frequency, session duration, and content of diet therapy), comparator description, and quantitative data (mean [variance] when possible) for continuous outcomes and risk ratio (95% confidence interval [95% CI]) for categoric outcomes) for categorical outcomes for the primary outcome of phosphate levels.
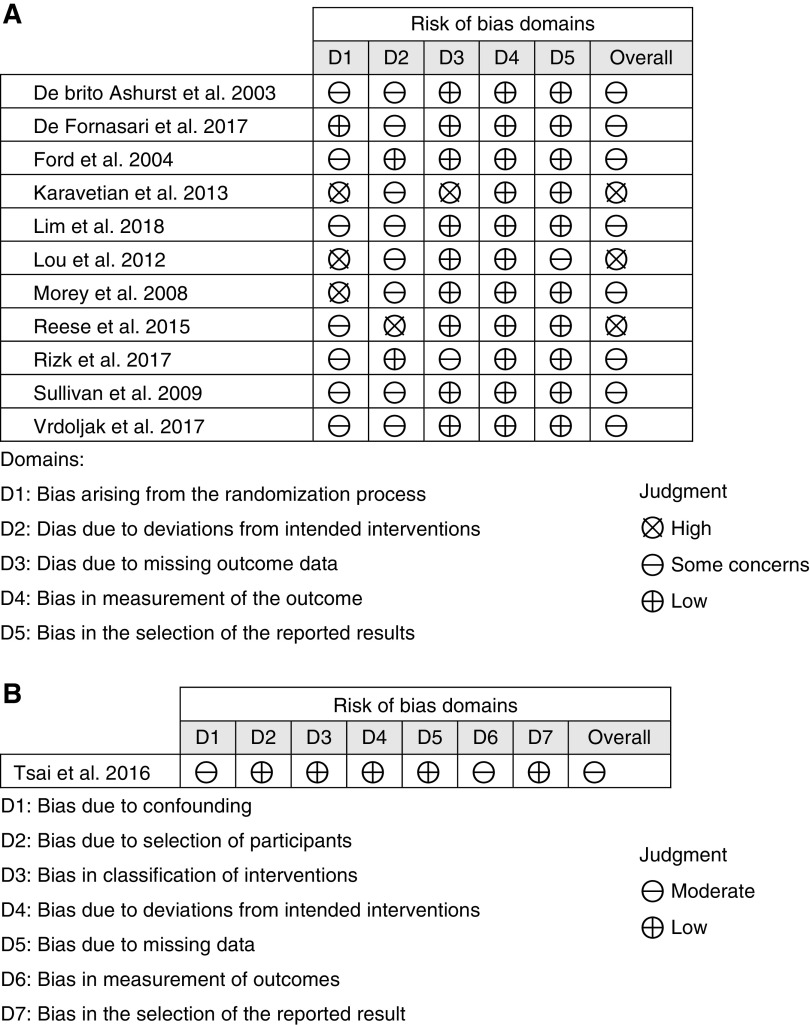
Risk of Bias of Individual Studies and across Studies
Randomized controlled trials (RCTs) were assessed for risk of bias from the randomization process, deviations from intended outcomes, missing outcome data, and measurement or reporting of the outcome using the ROB 2.0 tool (15). Non-RCTs were additionally assessed for risk of bias of confounding, participant selection, and classification of interventions using the ROBINS-I tool (16). Risk of bias was assessed independently by two reviewers (M.R. and D.H.), and discrepancies were determined by consensus.
The GRADE method (17) and GRADEpro (18) were used to determine certainty of evidence for each outcome for RCTs and non-RCTs separately. Certainty of evidence was determined on the basis of the risk of bias across studies, inconsistency in findings between studies, indirectness, imprecision of findings, and other factors. For non-RCTs, the certainty of evidence began at “high” because study limitations were considered in assessment with the ROBINS-I tool (16).
Synthesis of Results and Meta-Analyses
Extracted data were reported in a study characteristics table. An overview of included studies was synthesized narratively according to primary outcome. When possible, quantitative results were pooled in meta-analysis using a random effects model in OpenMetaAnalyst (19). Forest and funnel plots were created using RStudio (20). Heterogeneity was measured with I2 values, and publication bias was assessed using funnel plots. Subgroup analyses were conducted to compare intervention content and dose. Sensitivity analyses were conducted using leave-one-out analysis and by examining if effect size changed according to intervention duration (<6 months) and baseline phosphate status. Associations between serum phosphate enrollment criteria, baseline and changes in serum phosphate in the reference group, and intervention effect size were assessed using a scatterplot with linear-regression analysis in Microsoft Excel.
Quantitative data were included in meta-analyses when possible, and results are presented in forest plots. A GRADE summary of findings table was used to present overall effects, sample sizes, study designs, certainty of evidence, and overall conclusions (21). GRADE’s robvis tool was used to present the risk of bias assessment for each included study (22).
Results
Serum Phosphate Levels
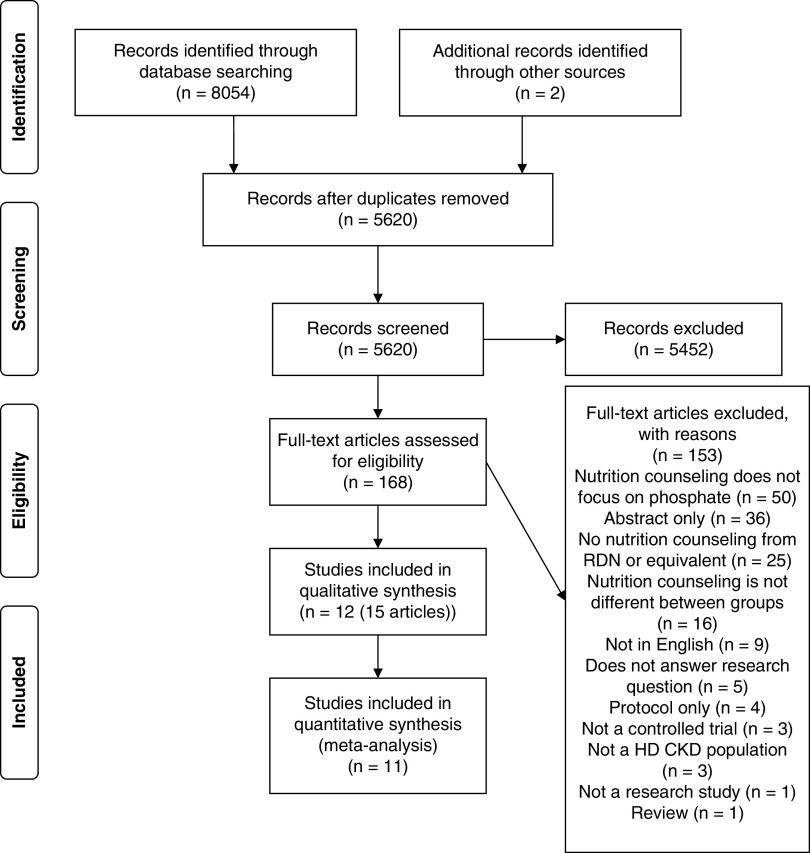
The database search identified 8054 titles/abstracts, full texts of 168 articles were reviewed, and 15 articles representing 12 studies were included (11 RCTs [23–33], one non-RCT [34]) (Figure 1, Table 2).
Figure 1.
PRISMA flow diagram for systematic review examining the effect of providing phosphate-specific diet therapy by a dietitian in individuals with CKD. HD, hemodialysis; RDN, registered dietician. Reprinted from ref. 11, which is available under the terms of the Creative Commons Attribution License.
Table 2.
Study characteristics of controlled trials examining the effect of phosphate-specific diet therapy delivered by a dietitian on primary outcomes in individuals with CKD on dialysis
| Study | Population | Intervention | Control |
|---|---|---|---|
| Multicomponent, low-dose interventions | |||
| Ashurst et al. (32); United Kingdom; RCT (single-center, random by patient) |
Sample size: 56/58 Vintage: >1 yr (not required) Age (mean [range], yr): 54 (22–88) Sex (female): 40% PO4: ≥1 recent (3 mo) ≥5.3 mg/dl |
Components Diet therapy (BL for 40 min) Diet ax: diet history Focus: LPD (NR) and binder adherence Behavior: NR Materials/handouts Tool for monitoring medicationsa Booklet and magnets on LPD, binder, and dialysis Follow-up: monthly for 3 mo (graph and 3 mo mean) Maintenance: no additional |
Components Usual care Diet therapy by renal dietitian Materials/handouts Tool for monitoring medicationsa |
| Lim et al. (24); Korea; RCT (single-center, 2:1 ratio intervention-to-control, random by patient)b |
Sample size: 70/70 Vintage: ≥3 mo Age (mean [SD], yr): 59 (16) Sex (female): 47% PO4: no requirement |
Components Diet therapy (BL for 30 min) Diet ax: NR Focus: LPD (NR, additives) Behavior: lessons Pharmacist consult (BL for 30 min) Follow-up: 1 mo Maintenance: 2 mo |
Components Usual care (NR) |
| Multicomponent, medium-dose interventions | |||
| Ford et al. (33); United States; RCT (multicenter [3], random by patient) |
Sample size: 63/70 Vintage: NR Age: 74% >50 yr Sex (female): 62% PO4: 3-mo mean ≥6.0 mg/dlb |
Components Diet therapy (1×/mo for 20–30 min) Diet ax: NR Focus: LPD (NR, protein foods, dairy products, additives), and binder and dialysis adherence Behavior: NR Materials/handouts Posters, handouts, and puzzles (NR); tool for monitoring serum phosphate Follow-up: 6 mo Maintenance: no additional |
Components Usual care Diet therapy by renal dietitian |
| Morey et al. (26); United Kingdom; RCT (multicenter [NR], random by patient) |
Sample size: (60–67)/67 (last obs.) Vintage: >6 mo Age (mean [SD], yr): intervention, 60 (16); control, 55 (16) Sex (female): 63% PO4: 3-mo mean ≥5.6 mg/dlc |
Components Diet therapy (1×/mo, time NR) Diet ax: diet history Focus: LPD (NR) and binder adherence Behavior: individualized Follow-up: 6 mo Maintenance: 6 mo |
Components Usual care Diet therapy by renal dietitian |
| Lou et al. (25); Spain; RCT (multicenter [5], random by center [4], and shift [1]) |
Sample size: 80/91 Vintage: >6 mo Age (mean [SD], yr): intervention, 61 (15); control, 63 (16) Sex (female): 48% PO4: 3-mo mean >5.5 mg/dlc |
Components Diet therapy (1×/mo for 30 min) Diet ax: NR Focus: Mediterranean diet–based LPD (PBPF, dairy products, whole grains, additives, demineralization) Behavior: NR Materials/handouts Diet plans for LPD Follow-up: 6 mo Maintenance: no additional |
Components Usual care (NR) |
| Multicomponent, high-dose interventions | |||
| Karavetian et al. (28); Lebanon; three-arm RCT (single-center, random by dialysis shift) |
Sample size: 87/122 Vintage: ≥3 mo Age: 36% ≥65 yr Sex (female): 52% PO4: no requirement |
Components Diet therapy (2×/wk for 20 min, and 1×/mo for 10 min) Diet ax: NR Focus: LPD (NR, protein foods, dairy products, whole grains, additives) Behavior: self-management counseling Materials/handouts Interactive games (graded)a Booklet on LPD and binders Follow-up: 8 wk Maintenance: no additional |
Components control 1 (primary) Usual care Diet therapy with hospital dietitian (referral <1×/6 mo) Components control 2 Usual care Diet therapy with hospital dietitian (referral <1×/6 mo) Materials/handouts Interactive games (not graded)a |
| Reese et al. (30); United States; three-arm RCT (multicenter [3], random by patients) |
Sample size: 24/24 (diet-therapy and usual-care arms only) Vintage: NR Age (median [IQR], yr): intervention, 52 (47–58); control, 53 (50–55) Sex (female): 22% PO4: 3-mo median >5.5 mg/dlc with no hypophosphatemia (<3.5 mg/dl) |
Components Diet therapy (BL for 45–60 min + ≥3×/wk [≥1×in-person or by telephone, time NR]) Diet ax: NR Focus: LPD (NR, protein foods, dairy products, whole grains, food preparation; not additives) and binder adherence Behavior: motivational interviewing and precaution adoption process model Follow-up: 10 wk Maintenance: no additional |
Components Usual care Diet therapy with renal dietitian |
| Tsai et al. (34); Taiwan; nonrandomized study (single-center, allocated by patient [method NR]) |
Sample size: 61/68 Vintage: ≥6 mo Age (mean [SD], yr): intervention, 58 (11); control, 57 (12) Sex (female): 38% PO4: 3-mo mean and most recent >5.5 mg/dlc |
Components Diet therapy (1×/2 wk for 30-min) Diet ax: 24-h recall Focus: LPD (NR, additives) and binder adherence Behavior: lessons with quizzes Materials/handouts Booklet (42 pages, HD diet, LPD, binders, dialysis, diet plan for LPD) Follow-up: 4 mo Maintenance: 4 mo |
Components Usual care Education by dialysis nurses and physicians Materials/handouts Sheets on LPD |
| Rizk et al. (29) (NEMO trial); Lebanon; three-arm RCT (multicenter [12], 1:1 ratio intervention 1–to-control random by shift, 2:1 ratio intervention 2–to-control random by center)d |
Sample size: 545/570 Vintage: ≥3 mo Age (mean [SD], yr): interventions 1 and 2, 58 (15) and 61 (15) Control: 60 (15) Sex (female): 41% PO4: no requirement |
Components intervention 1 (primary) Trained study dietitians (32 h) Diet therapy (2×/wk for 15 min) Diet ax: NR Focus: LPD (NR, protein foods, dairy products, whole grains, additives), and binder and dialysis adherence Behavior: lessons, transtheoretic model, adherence contest Materials/handouts Recipe book, booklet on LPD, clinic poster on LPDa Components intervention 2 Trained hospital dietitians (32 h) Follow-up: 6 mo Maintenance: 6 mo |
Components Usual care Diet therapy by hospital dietitian (referral <1×/6 mo) Materials/handouts Clinic poster on LPDa |
| Targeted interventions, phosphate additives | |||
|
Sullivan et al. (27); United States; RCT (multicenter [14], random by shift) |
Sample size: 279/279 (multiple imputation) Vintage: ≥6 mo Age (mean [SD] yr): intervention, 54 (13); control, 52 (12) Sex (female): 39% PO4: 3-mo mean and most recent >5.5 mg/dlc |
Components Diet therapy (BL for 30-min + telephone in mo 2, time NR) Diet ax: NR Focus: Additives Behavior: NR Materials/handouts Case (additives list, magnifying glass), handout (fast food) Follow-up: 3 mo Maintenance: no additional |
Components Usual care Diet therapy with renal dietitian |
|
de Fornasari et al. (31); Brazil; RCT (single-center, random by patient) |
Sample size: 131/140 Vintage: ≥6 mo Age (mean [SD] yr): intervention, 56 (13); control, 56 (15) Sex (female): 39% (n=134) PO4: ≥3 recent (3 mo) ≥5.5 mg/dlc |
Components Diet therapy (1× between d 10–30 and 1× at d 45: time NR) Diet ax: dietary recalls (1), food records (3) at BL Focus: additives Behavior: NR Education by clinic dietitian (BL)a Renal diet and LPD (NR, protein foods, dairy products, whole grains) Materials/handoutsa Booklet on LPD (NR) Follow-up: d 45 and 3 mo Maintenance: no additional |
Components Usual care Diet therapy by renal dietitian Education by clinical dietitian (BL)a Renal diet and LPD (NR, protein foods, dairy products, whole grains) Materials/handouts (BL)a Booklet on LPD (NR) |
| Targeted interventions, meal preparation | |||
|
Vrdoljak et al. (23); Croatia; RCT (single-center, random by patient) |
Sample size: 47/50 Vintage: NR Age (median [IQR] yr): intervention, 73 (62–77); control, 68 (60–73) Sex: NR PO4: >4.4 mg/dlc or ↑ Ca+2 or↑ PTH |
Components Diet therapy (1×/wk for 2 mo, 15–20 mins)a Diet ax: NR Focus: demineralization Behavior: NR Meals (two meals per dialysis, demineralized) Diet therapy (BL ×3 d+1×/week for 2 mo, 15 min) Diet ax: NR Focus: HD diet, LPD (NR, plant-rich, additives) Behavior: lessons Materials/handoutsa Handouts (HD diet, LPD, menus) Follow-up: monthly up to 12 mo (graph only, NR) Maintenance: no additional |
Components Usual care NR Meals (two meals per dialysis, prepared normally) Diet therapy (BL ×3 d+1×/wk for 2 mo, 15 min)a Diet ax: NR Focus: HD diet, LPD (NR, plant rich, additives) Behavior: lessons Materials/handoutsa Handouts (HD diet, LPD, menus) |
RCT, randomized controlled trial; PO4, phosphate; BL, baseline; ax, assessment; LPD, low-protein diet; NR, not reported; obs., observation; PBPF, plant-based protein foods; IQR, interquartile range; HD, hemodialysis; Ca2+, calcium ion; PTH, parathyroid hormone.
Interventions that span two or more groups (also indicated in italics).
The primary outcome in Lim, et al. (24) was calcium-phosphate product. However, use of this outcome is discouraged by Kidney Disease Improving Global Outcomes (1) and, therefore, this study reported the secondary outcome of phosphate levels.
Conversion factors for units: serum phosphate levels in mg/dl to mmol/L ×3.096.
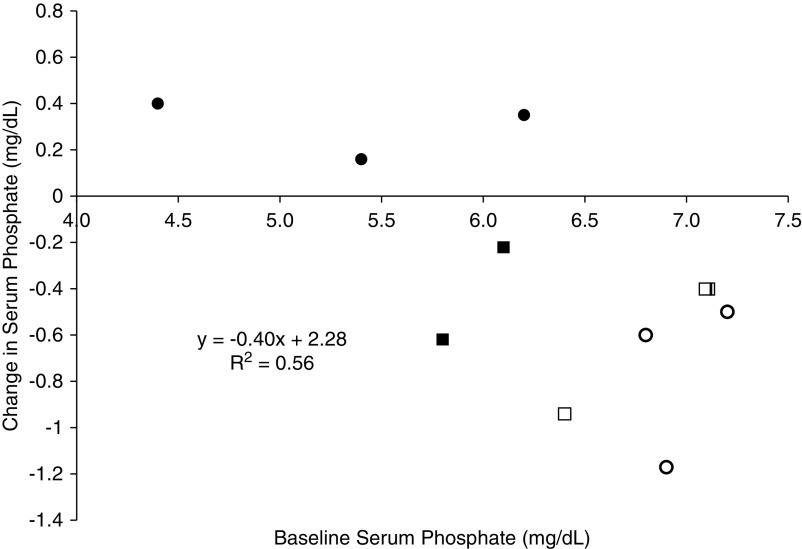
Sample sizes ranged from 24 to 545 participants, and study durations ranged from one session to 1 year. Randomization was mostly allocated at the patient level (22,23,25,29–33), although some studies randomized by shift (26,27), or center and shift (24,28). Serum phosphate enrollment criteria ranged from not requiring hyperphosphatemia (23,24,28,29) to requiring persistent and recent hyperphosphatemia (27,34). Enrollment criteria for serum phosphate were important determinants of baseline serum phosphate concentrations, and corresponding changes in serum phosphate (Figure 2). Among studies reporting mean baseline serum phosphate (n=9; serum phosphate range, 4.4–7.2 mg/dl), a serum phosphate difference of +1.0 mg/dl was associated with a 0.4 mg/dl greater decrease in serum phosphate in the control groups (r=−0.75; P=0.02). Serum phosphate levels were relatively normal at baseline in several of the trials that enrolled patients without hyperphosphatemia (23,24,28).
Figure 2.
Serum phosphate enrollment criteria at baseline affects changes in serum phosphate levels in reference groups of included studies in a systematic review. Black circles represent studies with no baseline requirement for participants’ serum phosphate levels; black squares represent studies in which participants were required to have recent hyperphosphatemia; white circles represent studies in which participants were required to have persistent hyperphosphatemia at baseline; white squares represent studies in which participants were required to have persistent hyperphosphatemia and hyperphosphatemia on most recent monthly blood test.
Studies were also conducted in diverse settings, including Brazil (31), Croatia (23), Lebanon (28,29), Spain (25), South Korea (24), Taiwan (34), the United Kingdom (26,32), and the United States (27,30,33). Differences in settings were associated with differences in usual care practices. Indeed, routine diet therapy provided by kidney dietitians was reported in the UK- and US-based studies (26,27,30,32,33), but was unavailable in the Lebanese and Taiwanese studies (28,29,34). In the HD clinic in Croatia (23), patients were provided two meals during each dialysis session, affording a partial controlled-feeding component to the intervention. Specifically, meals provided to the intervention-group participants were prepared using demineralization methods to lower phosphate content.
Intervention approaches were substantially different across studies (Table 2). Components of the low-phosphate diet included restrictions on whole grains, dairy products, plant- and/or animal-based protein foods, phosphate additives, and/or meal preparation methods, but were often not clearly defined. Many interventions also included nondietary strategies, specifically a focus on improving adherence to phosphate binders (26,28–30,32–34) and/or dialysis (29,33,34), and included a baseline pharmacist consultation in one study (24). Moreover, despite all studies using dietitian interventionists, dietary assessment was rarely reported and, when included, methods varied (diet history [26,32], diet recall [34], and records [31]). Most studies provided some form of patient materials and/or tools (23,25,27–29,31–34), which were also provided to the comparison groups in five studies (23,29,31,32,34).
Despite the differences in study design, setting, and approach, authors concluded that studies could reasonably be categorized on the basis of the focus of their interventions (e.g., multicomponent, phosphate additives, meal preparation) and, for multicomponent studies, their dose: low (one session total), moderate (one session or 1.0–1.5 months), or high (>1 session/mo) (Table 2).
Multicomponent Interventions
Two RCTs examined the short-term effect of a single session of multicomponent diet therapy (30–40 minutes) on serum phosphate (24,32). Both interventions resulted in a nonsignificant decrease in serum phosphate levels (mean difference, −0.45 mg/dl; 95% CI, −1.22 to 0.32 mg/dl; I2=26%; Figure 3). Three RCTs examined the effect of monthly, multicomponent diet therapy for 6 months on serum phosphate levels in patients with persistent hyperphosphatemia (25,26,33). Two out of three studies found a significant effect of diet therapy on serum phosphate (mean difference, −0.87 mg/dl; 95% CI, −1.40 to 0.33 mg/dl; I2=0%; Figure 3) (25,33). Four clinical trials, including three RCTs and one non-RCT, examined the effect of greater-than-monthly multicomponent diet therapy on serum phosphate levels (28–30,34). One RCT was excluded from the meta-analysis because authors were unable to obtain the necessary data (30). This study was an underpowered pilot trial that found a nonsignificant greater decrease in median change in serum phosphate in the diet therapy group at 10 weeks (−0.80 [interquartile range, −1.15 to 0.2] mg/dl versus −0.45 [interquartile range, −1.2 to 0.50] mg/dl; P value not reported). Among the remaining three studies, one RCT (28) and the non-RCT (34) reported a significant effect of diet therapy on serum phosphate levels (mean difference, −0.78 mg/dl; 95% CI, −1.27 to −0.29 mg/dl; I2=25%; Figure 3).
Figure 3.
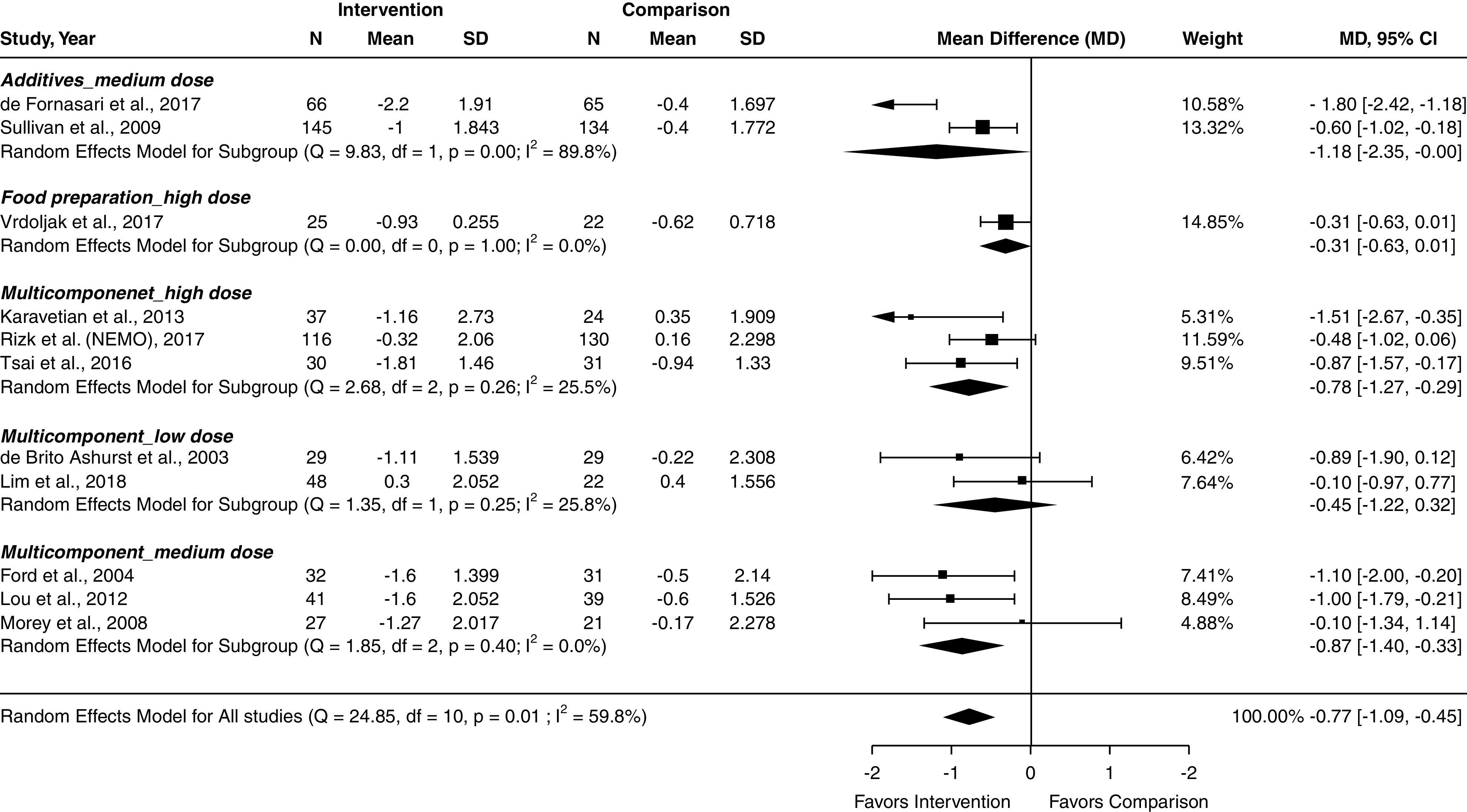
Forest plot of included studies demonstrates that the intervention of providing phosphate-specific diet therapy by a dietitian reduces serum phosphate levels in individuals with CKD on hemodialysis. Conversion factors for units: serum phosphate levels in mg/dl to mmol/L ×3.096. 95% CI, 95% confidence interval.
Targeted Interventions
Three studies examined the effect of phosphate-specific diet therapy that was focused on aspects of food processing or preparation (phosphate additives [27,31], meal preparation [23]) on serum phosphate. The two trials focused on avoiding phosphate additives found that diet therapy was efficacious for lowering serum phosphate (mean difference, −1.18 mg/dl; 95% CI, −2.35 to 0.00 mg/dl; I2=90%; Figure 3), but the trial focused on meal preparation found no significant effect (mean difference, −0.31 mg/dl; 95% CI, −0.61 to 0.01 mg/dl; Figure 3).
Pooled analysis of 11 studies indicated phosphate-specific diet therapy significantly decreased serum phosphate levels compared with control groups, with moderate heterogeneity in effect size (mean difference, −0.77 mg/dl; 95% CI, −1.09 to −0.45 mg/dl; I2=60%; Figure 3) (23–29,31–34). Publication bias was NS (Supplemental Figure 1). In sensitivity analyses, the magnitude of effect was slightly higher when limited to studies that included required baseline serum phosphate ≥5.5 mg/dl (mean difference, −0.86 mg/dl; 95% CI, −1.30 to −0.42 mg/dl) (24–27,31,33,34), and slightly lower when limited to studies without a high/serious risk of bias (mean difference, −0.70 mg/dl; 95% CI, −1.06 to −0.35 mg/dl) (Supplemental Figure 2). In leave-one-out analysis, results were not markedly changed by removing any single study. All studies demonstrated a high risk of bias or some concerns in risk of bias (Figure 4). Risk of bias and heterogeneity/imprecision resulted in “low” certainty evidence, suggesting phosphate-focused diet therapy reduces serum phosphate levels (Table 3).
Figure 4.
Randomized controlled trials (RCTs) and non-RCTs included in a systematic review examining the effect of phosphate-specific diet therapy provided by a dietitian on serum phosphate levels demonstrate high or some/moderate concerns in risk of bias. Risk of bias demonstrated in individual (A) randomized controlled trials (RCTs) and (B) non-RCTs included in a systematic review examining the effect of phosphate-specific diet therapy provided by a dietitian on serum phosphate levels.
Table 3.
Summary of findings describing the effect of phosphate-specific medical nutrition therapy provided by a dietitian on serum phosphate levels
| Outcomes | Anticipated Absolute Effectsa (95% CI) | No. of Participants (studies) | Certainty of the Evidence (GRADE) | Comments | ||
|---|---|---|---|---|---|---|
| Risk with Usual Care | Risk with Phosphate-Focused Diet Therapy | |||||
| QALY; follow-up: 6 mo | Reference | — | 545 (one RCT) | ⊕⊕◯◯ lowb,c | Phosphate-focused diet therapy from a dietitian may result in little or no difference in QALY. | |
| Serum phosphate levels; follow-up: range, 2.5–12 mo | Reference | MD 0.76 mg/dld lower (1.12 lower to 0.41 lower) | Total: 1168 (12 RCTs) In meta-analysis: 1144 (11 RCTs) |
⊕⊕◯◯ lowe,f | The evidence suggests phosphate-focused diet therapy from a dietitian reduces serum phosphate levels. | |
| Serum phosphate levels; follow-up: 10 wk | Reference | MD 0.87 mg/dld lower (1.57 lower to 0.17 lower) | 61 (one nonrandomized study)g | ⊕⊕◯◯ lowh,i | The evidence suggests phosphate-focused diet therapy from a dietitian results in a reduction in serum phosphate levels. | |
| Adverse events; follow-up: 3 mo | Not estimable | Not estimable | 279 (one RCT) | ⊕⊕◯◯ lowc,g | Phosphate-focused diet therapy from a dietitian may result in little or no difference in adverse events. | |
GRADE Working Group grades of evidence: high certainty, we are very confident the true effect lies close to that of the estimate of the effect; moderate certainty, we are moderately confident in the effect estimate, the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different; low certainty, our confidence in the effect estimate is limited, the true effect may be substantially different from the estimate of the effect; very low certainty, we have very little confidence in the effect estimate, the true effect is likely to be substantially different from the estimate of the effect. ⊕⊕◯◯ indicates “low” certainty of evidence. 95% CI, 95% confidence interval; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; QALY, quality-adjusted life-years; RCT, randomized controlled trial; MD, mean difference.
The risk in the intervention group (and its 95% CI) is determined on the basis of the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
Risk of bias from randomization and missing outcomes data.
One study only.
Conversion factors for units: serum phosphate levels in mg/dl to mmol/L ×3.096.
Of the 11 included studies, three had high risk of bias and eight had some concerns in risk of bias using the ROB 2.0 tool.
Heterogeneity of results was moderate I2=63.2%; wide 95% CI.
Risk of bias from randomization and deviations of intended intervention.
Some concerns in ROB as assessed by the ROBINS-I tool.
Small sample size and/or wide 95% CI.
Mortality, Quality of Life, and Adverse Events
The NEMO trial examined the effect of greater-than-monthly (high-dose), multicomponent medical nutrition therapy on the secondary, patient-centered outcomes of mortality and quality of life, reported as the composite measure of quality-adjusted life-years (29). Low-certainty evidence demonstrated phosphate-focused diet therapy from a dietitian may result in little or no difference in quality-adjusted life-years (Table 3).
One included study reported adverse events from the intervention focusing on phosphate additives for 3 months (27). Low certainty of evidence demonstrated phosphate-focused diet therapy from a dietitian may result in little or no difference in adverse events (Table 3).
Discussion
This systematic review and meta-analyses examined the effect of phosphate-specific diet therapy on serum phosphate in patients undergoing HD. Diet therapy was found to be efficacious in reducing phosphate levels. Despite heterogeneity among the included studies, the findings from this review and meta-analyses show consistency and provide useful insights on the practice and research of diet therapy for managing hyperphosphatemia in adults on HD.
The majority of studies found a significant effect of diet therapy on serum phosphate levels (25,27,28,31,33,34), and the studies that found no effect were either not powered to assess this outcome (30), had serum phosphate levels at baseline that were low relative to normal (23,24,29), and/or were low relative to the control group (23,26). In weighing these limitations, the trials in this review, although limited in number and found to be at high risk of bias, suggest:
a single session of diet therapy can lower serum phosphate in adults with hyperphosphatemia for up to 3 months (one RCT [32]);
monthly diet-therapy sessions of approximately 20–30 minutes can significantly lower serum phosphate in adults on HD with hyperphosphatemia over a 6-month period (two RCTs [25,33]);
in settings without kidney dietitians, frequent diet therapy (two or more times totaling ≥1 h/mo) can significantly lower serum phosphate in adults on HD in the short term (2–4 months) (one RCT [28], one non-RCT [34]); and
two diet-therapy sessions focused on avoiding phosphate additives can significantly lower serum phosphate in adults on HD over a 3-month period (two RCTs [27,31]).
The effects of diet therapy on serum phosphate appeared to be due to reduced dietary phosphate load. Although nutrition assessment of dietary phosphate load is problematic, participants receiving phosphate-specific diet therapy reported greater adherence to specific dietary strategies, such as avoiding phosphate additives and limiting phosphate-rich foods (27,28,34). In contrast, no differences were noted in phosphate-binder adherence (24,26,30), and phosphate-binder dose and pill burden either stayed the same (24–26) or decreased (23,25,34). In addition, the only multicomponent intervention that focused on diet alone was one of the two trials that showed benefit of monthly diet therapy over 6 months (25).
Only four studies examined the maintenance effects of phosphate-specific diet therapy on serum phosphate. The findings from Ashurst et al. (32) indicate a single session of phosphate-specific diet therapy may have effects lasting up to 3 months. However, the longer-term evaluations of maintenance effects at 4 (34) and 6 months (26,29) reported a decline in efficacy after the intervention phase. These findings support the notion that diet therapy is a treatment, not a cure, for diet-related complications, and suggests phosphate-specific diet therapy monitoring and evaluation plans should include long-term phosphate management strategies. The findings on safety were relatively varied and sparse, but most studies mentioned concerns that strategies to reduced dietary phosphate load might compromise protein status because many phosphate-rich foods are also sources of protein (23–26,29,32,34,35). Overall, no negative effects of phosphate-specific diet therapy on protein status were found, including visceral protein status (23,25,31,34), objective markers of protein intake (23,31,34), measures of body composition and physical function, and indices of malnutrition and health-related quality of life (36).
The 2020 KDOQI Clinical Practice Guidelines for Nutrition in CKD work group “emphasizes to individualize recommendations after appropriate evaluation of the patient’s daily intake” (3). Nutrition assessment is a key feature of the tailored diet-therapy approach that is generally used by dietitians in clinical practice. Indeed, the KDOQI guidelines further note that diet therapy “requires expertise (preferably consultation with a kidney dietitian)” (3) and the US-based National Institutes of Diabetes and Digestive and Kidney Diseases states “it is vital to engage and refer to a registered dietitian… knowledgeable in CKD diet and nutrition to assess and conduct individualized….Medical nutrition therapy for patients with CKD” (37). Despite this, most diet-therapy interventions appeared to use a one-size-fits-all approach, which fails to leverage the unique education and training of dietitians. In fact, only four studies reported a dietary assessment component to the intervention (26,31,32,34).
Although guidelines advocate strong support for kidney dietitians, a 2005–2007 Centers for Medicare and Medicaid Services Medical Evidence Report of incident HD patients in the United States (n=192,307) found most patients saw a kidney dietitian for the first time in the year leading up to dialysis (9%) or after starting HD (88%) (38). Unfortunately, no studies in the nondialyzed population met the inclusion criteria in our analysis, despite calls to prioritize research “to evaluate the clinical benefits associated with the use of dietary interventions in patients with CKD stages 3–5D” in the 2009 (39) and 2017 (2) Kidney Disease Improving Global Outcomes clinical practice guidelines for CKD-MBD (39); the call for research was echoed in the 2020 KDOQI nutrition guidelines (3).
In terms of dose, it appears that approximately 30 min/mo of phosphate-specific diet therapy was sufficient to lower serum phosphate in patients on HD with persistent hyperphosphatemia, at least as long as it is maintained, for up to 6 months. This dose of diet therapy exceeds the total amount of time available by almost 50% (approximately 21 min/mo), according to a recent time and motion pilot study of US kidney dietitians (10), indicating the moderate dose of diet therapy in this study was, in practice, very high. The importance of patient contact is supported by the findings from the second treatment arm of the trial by Rizk et al. (29) (Table 2). In this arm, the hospital dietitians who provide care by referral (less than one time per 6 months) received 32 hours of specialist training in nutrition but had no additional contact with participants beyond usual care referrals. Mean serum phosphate levels were unchanged in this group.
Several factors affected the results and potential effect of this systematic review. For one, we excluded clinical trials that did not meet our inclusion criteria, such as trials that lacked a control group (40) or those that used strategies other than diet therapy delivered by a dietitian (41–43). This review was also limited by the availability of RCTs (e.g., only in patients on dialysis) and details reported in the publications, especially related to the dietary approaches and strategies used (Table 2). Although behavioral approaches are key to diet-therapy efficacy, the differences in approach were too varied to come to firm conclusions and may be better demonstrated through comparative efficacy trials than usual-care trials because the usual care and clinical efficacy of the dietary and nondietary strategies may differ across study settings.
More broadly, other limitations and aspects of phosphate control in HD affected our findings, including crosscontamination between study arms among patients sharing their experiences among themselves and staff (44), inability to assess changes in dietary phosphate load stemming from differences in phosphate bioavailability by food source (45), and the effects of food processing (46) and preparation (47). Finally, because serum phosphate has high intraindividual variability and, likely related, varying adherence and responsiveness to dietary phosphate and important confounders such as phosphate binders and dialysis (48), enrollment criteria for serum phosphate had to balance regression to the mean with loss of potential effect size (Figure 2).
Phosphate-specific diet therapy is efficacious and safe for treating persistent hyperphosphatemia in patients on HD. Monthly diet-therapy sessions of 30 minutes appeared sufficient to lower serum phosphate without compromising nutrition status for up to 6 months, although lower doses were unavailable for comparison, and this effect appeared to fade when the intervention stopped. The limited number of RCTs and diversity of approaches used represents a key challenge in establishing evidence-based dietetic practice guidelines. Overall, these findings highlight relevant opportunities for challenging, but influential, research on dietary management of CKD-MBD and signal the potential to improve serum phosphate levels in individuals on HD through additional dietetic services.
Disclosures
J.J. Carrero reports receiving speaker fees from Abbott, AstraZeneca, Nutricia, and ViforPharma; grant funding from Astellas, AstraZeneca, ViforPharma, and Swedish Research Council (grant 2019-01059); and being a consultant for AstraZeneca and Baxter. D. Handu, M.R. Rozga, and D.E. St-Jules have memberships to the Academy of Nutrition and Dietetics and are registered dietitians through the Commission of Dietetic Regulation. D. Handu and M.R. Rozga are employed by the Academy of Nutrition and Dietetics. J.J. Carrero, D. Handu, and M.R. Rozga participated in the evidence search and drafting of the 2020 KDOQI Clinical Practice Guidelines for Nutrition in CKD.
Funding
Funding for this systematic review was provided by the Academy of Nutrition and Dietetics.
Supplementary Material
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Dietary Therapy for Managing Hyperphosphatemia,” on pages 9–11.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.09360620/-/DCSupplemental.
Supplemental Appendix 1. Adapted PRISMA checklist for systematic reviews.
Supplemental Appendix 2. Database search to identify articles addressing the PICO question: In individuals with CKD, what is the effect of medical nutrition therapy provided by a registered dietitian nutritionist or international equivalent on nutrition outcomes?
Supplemental Figure 1. Funnel plots demonstrating publication bias for the outcomes (A) serum phosphate levels and (B) hyperphosphatemia.
Supplemental Figure 2. Sensitivity analysis for meta-analysis demonstrating the effect of phosphate-focused MNT delivered by a dietitian on serum phosphate levels according to (A) baseline serum phosphate levels ≥5.5 mg/dl and (B) study risk of bias.
References
- 1.Ritter CS, Slatopolsky E: Phosphate toxicity in CKD: The killer among us. Clin J Am Soc Nephrol 11: 1088–1100, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kidney Disease Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group : KDIGO 2017. Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Available at https://kdigo.org/wp-content/uploads/2017/02/2017-KDIGO-CKD-MBD-GL-Update.pdf. Accessed October 21, 2020 [DOI] [PMC free article] [PubMed]
- 3.Ikizler TA, Burrowes JD, Byham-Gray LD, Campbell KL, Carrero J-J, Chan W, Fouque D, Friedman AN, Ghaddar S, Goldstein-Fuchs DJ, Kaysen GA, Kopple JD, Teta D, Wang AY, Cuppari L: KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis 76: S1–S107, 2020 [DOI] [PubMed] [Google Scholar]
- 4.Writing Group of the Nutrition Care Process/Standardized Language Committee: Nutrition care process and model part I: The 2008 update. J Am Diet Assoc 108: 1113–1117, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Hand RK, Burrowes JD: Renal dietitians’ perceptions of roles and responsibilities in outpatient dialysis facilities. J Ren Nutr 25: 404–411, 2015 [DOI] [PubMed] [Google Scholar]
- 6.Durose CL, Holdsworth M, Watson V, Przygrodzka F: Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. J Am Diet Assoc 104: 35–41, 2004 [DOI] [PubMed] [Google Scholar]
- 7.St-Jules DE, Woolf K, Pompeii ML, Sevick MA: Exploring problems in following the hemodialysis diet and their relation to energy and nutrient intakes: The BalanceWise study. J Ren Nutr 26: 118–124, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Isakova T, Wahl P, Vargas GS, Gutiérrez OM, Scialla J, Xie H, Appleby D, Nessel L, Bellovich K, Chen J, Hamm L, Gadegbeku C, Horwitz E, Townsend RR, Anderson CAM, Lash JP, Hsu CY, Leonard MB, Wolf M: Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int 79: 1370–1378, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Block GA, Kilpatrick RD, Lowe KA, Wang W, Danese MD: CKD-mineral and bone disorder and risk of death and cardiovascular hospitalization in patients on hemodialysis. Clin J Am Soc Nephrol 8: 2132–2140, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hand RK, Albert JM, Sehgal AR: Quantifying the time used for renal dietitian’s responsibilities: A pilot study. J Ren Nutr 29: 416–427, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group: Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol 62: 1006–1012, 2009 [DOI] [PubMed] [Google Scholar]
- 12.Rozga M: Effect of medical nutrition therapy by a dietitian to manage phosphorus levels in adults with chronic kidney disease on dialysis: A systematic review and meta-analysis. Open Science Framework, 2020. Available at: osf.io/eaqk7. Accessed May 19, 2020 [Google Scholar]
- 13.Jiang N, Fang W, Gu AP, Yuan JZ, Yang XX, Lin AW, Ni ZH, Qian JQ: Improving diet recipe and cooking methods attenuates hyperphosphatemia in patients undergoing peritoneal dialysis. Nutr Metab Cardiovasc Dis 25: 846–852, 2015 [DOI] [PubMed] [Google Scholar]
- 14.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A: Rayyan-A web and mobile app for systematic reviews. Syst Rev 5: 210, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT: RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366: l4898, 2019 [DOI] [PubMed] [Google Scholar]
- 16.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP: ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355: i4919, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guyatt G, Oxman AD, Sultan S, Brozek J, Glasziou P, Alonso-Coello P, Atkins D, Kunz R, Montori V, Jaeschke R, Rind D, Dahm P, Akl EA, Meerpohl J, Vist G, Berliner E, Norris S, Falck-Ytter Y, Schünemann HJ: GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol 66: 151–157, 2013 [DOI] [PubMed] [Google Scholar]
- 18.GRADEpro GDT: GRADEpro guideline development tool, Hamilton, Canada, McMaster University, 2020. Available at: https://gradepro.org/. Accessed May 29, 2020 [Google Scholar]
- 19.Byron CW, Issa JD, Thomas AT, Joseph L, Paul T, Christopher HS: Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw 49: 1–15, 2012 [Google Scholar]
- 20.R Core Team: R: A language and environment for statistical computing. Vienna, Austria, R Foundation for Statistical Computing, 2010. Available at: https://www.R-project.org. Accessed October 16, 2020 [Google Scholar]
- 21.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ: GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64: 383–394, 2011 [DOI] [PubMed] [Google Scholar]
- 22.McGuinness LA, Higgins JPT: Risk-of-bias VISualization (robvis): An R package and shiny web app for visualising risk-of-bias assessments [published online ahead of print April 26, 2020]. Res Synth Methods 10.1002/jrsm.1411 [DOI] [PubMed] [Google Scholar]
- 23.Vrdoljak I, Panjkota Krbavčić I, Bituh M, Leko N, Pavlović D, Vrdoljak Margeta T: The impact of education and cooking methods on serum phosphate levels in patients on hemodialysis: 1-year study. Hemodial Int 21: 256–264, 2017 [DOI] [PubMed] [Google Scholar]
- 24.Lim E, Hyun S, Lee JM, Kim S, Lee MJ, Lee SM, Oh YS, Park I, Shin GT, Kim H, Morisky DE, Jeong JC: Effects of education on low-phosphate diet and phosphate binder intake to control serum phosphate among maintenance hemodialysis patients: A randomized controlled trial. Kidney Res Clin Pract 37: 69–76, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lou LM, Caverni A, Gimeno JA, Moreno R, Pérez J, Alvarez R, Campos B, García M, Gutiérrez A, Bielsa S, Castilla J, Sanz A, Martin F; Aragon CKD Research Group: Dietary intervention focused on phosphate intake in hemodialysis patients with hyperphosphoremia. Clin Nephrol 77: 476–483, 2012 [PubMed] [Google Scholar]
- 26.Morey B, Walker R, Davenport A: More dietetic time, better outcome? A randomized prospective study investigating the effect of more dietetic time on phosphate control in end-stage kidney failure haemodialysis patients. Nephron Clin Pract 109: c173–c180, 2008 [DOI] [PubMed] [Google Scholar]
- 27.Sullivan C, Sayre SS, Leon JB, Machekano R, Love TE, Porter D, Marbury M, Sehgal AR: Effect of food additives on hyperphosphatemia among patients with end-stage renal disease: A randomized controlled trial. JAMA 301: 629–635, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Karavetian M, Ghaddar S: Nutritional education for the management of osteodystrophy (nemo) in patients on haemodialysis: A randomised controlled trial. J Ren Care 39: 19–30, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Rizk R, Hiligsmann M, Karavetian M, Evers SMAA: Cost-effectiveness of dedicated dietitians for hyperphosphatemia management among hemodialysis patients in Lebanon: Results from the Nutrition Education for Management of Osteodystrophy trial. J Med Econ 20: 1024–1038, 2017 [DOI] [PubMed] [Google Scholar]
- 30.Reese PP, Mgbako O, Mussell A, Potluri V, Yekta Z, Levsky S, Bellamy S, Parikh CR, Shults J, Glanz K, Feldman HI, Volpp K: A pilot randomized trial of financial incentives or coaching to lower serum phosphorus in dialysis patients. J Ren Nutr 25: 510–517, 2015 [DOI] [PubMed] [Google Scholar]
- 31.de Fornasari MLL, Sens YADS: Replacing phosphorus-containing food additives with foods without additives reduces phosphatemia in end-stage renal disease patients: A randomized clinical trial. J Ren Nutr 27: 97–105, 2017 [DOI] [PubMed] [Google Scholar]
- 32.Ashurst IB, Dobbie H: A randomized controlled trial of an educational intervention to improve phosphate levels in hemodialysis patients. J Ren Nutr 13: 267–274, 2003 [DOI] [PubMed] [Google Scholar]
- 33.Ford JC, Pope JF, Hunt AE, Gerald B: The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J Ren Nutr 14: 36–44, 2004 [DOI] [PubMed] [Google Scholar]
- 34.Tsai WC, Yang JY, Luan CC, Wang YJ, Lai YC, Liu LC, Peng YS: Additional benefit of dietitian involvement in dialysis staffs-led diet education on uncontrolled hyperphosphatemia in hemodialysis patients. Clin Exp Nephrol 20: 815–821, 2016 [DOI] [PubMed] [Google Scholar]
- 35.St-Jules DE, Woolf K, Pompeii ML, Kalantar-Zadeh K, Sevick MA: Reexamining the phosphorus-protein dilemma: Does phosphorus restriction compromise protein status? J Ren Nutr 26: 136–140, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karavetian M, Elzein H, Rizk R, Jibai R, de Vries N: Nutritional education for management of osteodystrophy: Impact on serum phosphorus, quality of life, and malnutrition. Hemodial Int 20: 432–440, 2016 [DOI] [PubMed] [Google Scholar]
- 37.National Institute of Diabetes and Digestive and Kidney Diseases: Collaborate with a registered dietitian, 2020. Available at: https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/kidney-disease/identify-manage-patients/manage-ckd/collaborate-registered-dietitian. Accessed April 30, 2020
- 38.Slinin Y, Guo H, Gilbertson DT, Mau LW, Ensrud K, Collins AJ, Ishani A: Prehemodialysis care by dietitians and first-year mortality after initiation of hemodialysis. Am J Kidney Dis 58: 583–590, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kidney Disease Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group : KDIGO 2009. Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Available at https://kdigo.org/wp-content/uploads/2017/02/KDIGO-2009-CKD-MBD-Guideline-English.pdf. Accessed October 21, 2020 [DOI] [PMC free article] [PubMed]
- 40.Cupisti A, D’Alessandro C, Baldi R, Barsotti G: Dietary habits and counseling focused on phosphate intake in hemodialysis patients with hyperphosphatemia. J Ren Nutr 14: 220–225, 2004 [PubMed] [Google Scholar]
- 41.Caldeira D, Amaral T, David C, Sampaio C: Educational strategies to reduce serum phosphorus in hyperphosphatemic patients with chronic kidney disease: Systematic review with meta-analysis. J Ren Nutr 21: 285–294, 2011 [DOI] [PubMed] [Google Scholar]
- 42.Milazi M, Bonner A, Douglas C: Effectiveness of educational or behavioral interventions on adherence to phosphate control in adults receiving hemodialysis: A systematic review. JBI Database Syst Rev Implement Reports 15: 971–1010, 2017 [DOI] [PubMed] [Google Scholar]
- 43.Taylor LM, Kalantar-Zadeh K, Markewich T, Colman S, Benner D, Sim JJ, Kovesdy CP: Dietary egg whites for phosphorus control in maintenance haemodialysis patients: A pilot study. J Ren Care 37: 16–24, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karavetian M, de Vries N, Rizk R, Elzein H: Dietary educational interventions for management of hyperphosphatemia in hemodialysis patients: A systematic review and meta-analysis. Nutr Rev 72: 471–482, 2014 [DOI] [PubMed] [Google Scholar]
- 45.Moe SM, Zidehsarai MP, Chambers MA, Jackman LA, Radcliffe JS, Trevino LL, Donahue SE, Asplin JR: Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease. Clin J Am Soc Nephrol 6: 257–264, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Calvo MS, Uribarri J: Contributions to total phosphorus intake: All sources considered. Semin Dial 26: 54–61, 2013 [DOI] [PubMed] [Google Scholar]
- 47.Jones WL: Demineralization of a wide variety of foods for the renal patient. J Ren Nutr 11: 90–96, 2001 [DOI] [PubMed] [Google Scholar]
- 48.Sherman RA: Hyperphosphatemia in dialysis patients: Beyond nonadherence to diet and binders. Am J Kidney Dis 67: 182–186, 2016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.