Abstract
Background:
Diabetes mellitus is one of the major health problems in the world. Stress and mental illnesses adversely affect glycemic control. In most patients, a multidisciplinary approach including physical activity, healthy diet, and stress management is required for glycemic control. Mindfulness-based stress reduction (MBSR) is a structured group program that reduces emotional distress through self-awareness and assuming the responsibility for individual choices, and results in increased effective health behaviors. Here, we aimed to evaluate the effects of mindfulness meditation on glycemic control and mental health in patients with type 2 diabetes.
Materials and Methods:
This randomized clinical trial study was performed in 2018 in Isfahan city. A total number of 108 patients with diabetes mellitus type 2 were selected and allocated randomly to two groups, intervention (12 weeks MBSR program) and control (routine care). Depression, anxiety, and stress scores regarding to depression, anxiety, and stress Scale - 21 questionnaire and also amounts of fasting blood sugar (FBS) and hemoglobin A1C (HbA1C) were assessed and analyzed using independent t-test, paired t-test, Mann–Whitney U-test, and Chi-square, before and 13 weeks after educational programs.
Results:
The means of HbA1C, FBS, and depression, anxiety, and stress scores improved significantly after intervention in the MBSR group. Except FBS levels, all outcome variable scores' mean change was significant between the two groups.
Conclusions:
In general, this study revealed that mindfulness meditation could be helpful in improving the quality of mental health and lowering glycemic control indices in patients with type 2 diabetes mellitus.
Keywords: Blood glucose, diabetes mellitus, type 2, mental health, meditation a mindfulness
Introduction
Diabetes mellitus is one of the major health problems in the world.[1] The modern lifestyle (reduced physical activity, poor diet, and elevated stress) is among the factors that resulted in an increase in the prevalence of this disease in recent years. As diabetes mellitus is a chronic disease, it places great stress on the patient, and studies showed that some psychological disorders, such as depression and anxiety, are more prevalent among these patients. Stress and mental illnesses also adversely affect glycemic control.[2] Medication alone is not enough for glycemic control in most patients; therefore, a multidisciplinary approach including physical activity, healthy diet, and stress management is required. In so doing, psychological interventions are simultaneously undertaken along with medical ones to control this disease and its associated complications.[3,4] Mindfulness-based stress reduction (MBSR) which refers to a type of meditation that emphasizes the awareness of the present moment in a nonjudgmental way is one of these interventions.[5]
The interest in the therapeutic use of mindfulness has recently increased so that many studies have been conducted in various fields using mindfulness techniques.[6,7,8] MBSR is a structured group program that aims to reduce stress to promote mental health and reduce pain and suffering. These trainings aim to increase the patients' awareness and acceptance of their internal and external experiences so that they can think and react constructively, rather than passively, to the stressors. Over time, this method reduces emotional distress through self-awareness and assuming the responsibility for individual choices, and results in increased effective health behaviors.[9,10]
A review study conducted by Merkes revealed the positive therapeutic effects of mindfulness for disorders such as chronic pain, rheumatoid arthritis, type 2 diabetes mellitus, chronic fatigue syndrome, and cardiovascular disease, without having any side effects and negative consequences.[11] Another review study on stress management techniques showed that mindfulness can significantly influence the patients' coping with their disease and better disease management in various diseases such as cancer, cardiovascular diseases, diabetes mellitus, and chronic pain.[5] Therefore, it might be concluded that stress reduction by MBSR has a considerable therapeutic value in reducing emotional distress (depression and anxiety) in a variety of chronic diseases.[12]
Conflicting results were obtained from the studies conducted to evaluate the effect of stress control on diabetes management concerning glycemic control and improving mental health.[9,13,14] Therefore, the need to conduct further studies to investigate the effect of mindfulness interventions on diabetes is highly felt.[4] Given the importance and prevalence of diabetes and the impact of its control on the related complications, as well as the fact that few studies have been conducted on the impact of mindfulness on diabetes and its control in Iran, and the lack of definitive results in previous studies, the present study aimed to investigate the effect of mindfulness on controlling glycemic indexes and mental health in patients with type 2 diabetes.
Materials and Methods
This randomized controlled clinical trial study was conducted in 108 diabetic patients referred to Imam Ali Comprehensive Urban Health Center in Isfahan, a central city in Iran, in 2019.
For sample size calculation, we assumed an attrition rate of 10%, effect size of 20% with at least 80% power and statistical significance level at 0.05. Following enrollment, the dropout exclusion rate at the stage of analysis was 6.48%, yielding a final sample of 101 patients. The inclusion criteria were: adult women (age ranged 30–59 years) with type 2 diabetes mellitus diagnosed by a doctor, the history of diabetes for at least 6 months, having a health record at the health center, and hemoglobin A1C (HbA1c) between 7% and 9%. Patients with acute mental diseases, chronic diseases such as cancer or any other serious medical condition, pregnancy and lactation, alcohol and substance abuse, serious complications caused by diabetes, undergoing psychological treatments in the past year were excluded from this research. Diabetic men were not included because of fewer refer to the health center. Imam Ali Comprehensive Urban Health Center has 5 population blocks based on geographical area. In order to prevent contamination, using random number table, blocks 1 and 5 were randomly allocated to the intervention and control groups, respectively. Then, based on the electronic health records, the diabetic patients were randomly selected and were replaced with the next record if they did not meet the inclusion criteria. The final sample was invited to a briefing session, where written informed consent was obtained from all participants before conducting the intervention, which was conducted under protocols approved by Isfahan University of Medical Sciences Ethics Committee (IR.MUI.MED.REC.1397.165). The trial was registered in the Iranian Clinical Trials Registry, with registration number IRCT2019090813044527N1.
Afterward, demographic information, including age, level of education, employment and marital status, were obtained from them. Anxiety, depression, and stress scores were measured by the depression, anxiety and stress scale-21 (DASS-21) questionnaire.[15] The questionnaire comprises 21 statements related to negative symptoms (depression, anxiety, and stress). The validity and reliability of this questionnaire were confirmed in the Iranian population.[16] Each participant is required to rate the statements, regarding the feelings experienced over the past week, in terms of intensity/frequency using a three-point Likert scale ranging from 0 to 3. Each of the three measures of depression, anxiety, and stress included seven items, and the total score of each of them is obtained by summing up its seven items and multiplying by 2. Therefore, the range of scores in each area is 0–42, and the higher the score, the more severe the disorder. A venous fasting blood sample was collected from the participants to measure fasting blood sugar (FBS) and HbA1c.
Throughout the study, the control group was routinely cared for by the health-care system according to national guidelines for diabetes care. In addition to routine care, the intervention group received eight sessions (2 h each) of group mindfulness training once a week by a certified instructor and then practiced at home for 4 weeks and weekly self-reports were presented on the home practices.
The following topics were discussed in the eight training sessions: explanations about mindfulness, doing yoga exercises, meditation, receiving feedback, and answering questions, breathing exercises, and sleep hygiene training. In the 13th week (1 week after the end of the intervention), FBS and HbA1c were re-measured and the DASS-21 questionnaire was completed.
The data were analyzed using the Statistical Package for Social Sciences SPSS for Windows version 16 (SPSS Inc., Chicago IL.). For group comparisons, independent sample t-test, and the Mann–Whitney U-test were used, according to normality (assessed by the Kolmogorov–Smirnov test) for continuous variables and the Chi-squared test for qualitative variables. Paired-sample t-test was used for before-after comparisons. The significance level for the analyses was set as 5%. For ethical considerations, the control group received two sessions of mindfulness training along with printed content after the end of the project.
Results
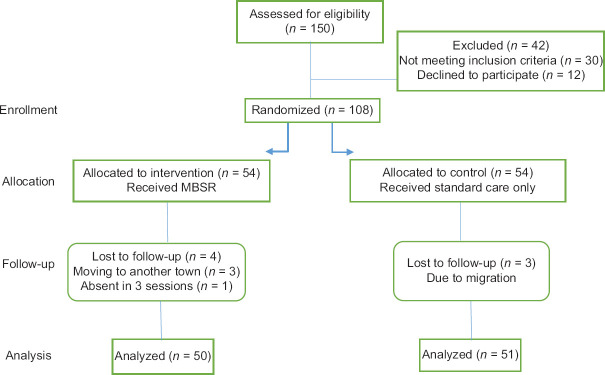
One hundred and eight patients participated in this study; three patients from the control group and four patients from the intervention group left the study. Finally, 50 and 51 patients were analyzed in the intervention and control group, respectively. The patients' follow-up chart is illustrated in Figure 1.
Figure 1.
Flowchart of participants
As shown in Table 1, there was no significant difference between the two groups in terms of demographic and baseline characteristics.
Table 1.
Demographic and Baseline characteristics (n=101)
| Characteristics | MBSR (n=50) | Control (n=51) | P |
|---|---|---|---|
| Age, mean±SD | 56.4±4.57 | 57.7±5.65 | 0.2 |
| Marital status, n (%) | |||
| Single | 1 (1.9) | 1 (1.9) | 0.82 |
| Married | 46 (86.8) | 43 (82.7) | |
| Widow/divorced | 6 (11.3) | 8 (15.4) | |
| Education level, n (%) | |||
| Elementary school | 17 (32.1) | 11 (20.4) | 0.14 |
| Guidance school | 31 (58.5) | 39 (72.2) | |
| High school | 5 (9.4) | 2 (3.7) | |
| Academic | 0 | 2 (3.7) | |
| Job, n (%) | |||
| Housewife | 43 (84.3) | 40 (75.5) | 0.15 |
| Government’s employee | 2 (3.9) | 8 (15.1) | |
| Self-employment | 6 (11.8) | 5 (9.4) | |
| HBA1C, mean±SD | 8.2±0.72 | 8.1±0.61 | 0.72 |
| FBS, mean±SD | 175.3±34.76 | 176.4±25.21 | 0.85 |
| Depression score, mean±SD | 17.1±6.94 | 15.0±6.30 | 0.09 |
| Anxiety score, mean±SD | 17.1±7.33 | 15.0±8.78 | 0.17 |
| Stress score, mean±SD | 21.1±8.23 | 19.2±7.98 | 0.24 |
MBSR: Mindfulness-based stress reduction group, SD: Standard deviation, FBS: Fasting blood sugar, HbA1c: Hemoglobin A1c
The means of HbA1C and FBS, and depression, anxiety, and stress scores before and after intervention in the two groups are presented in Table 2. As shown in Table 2, all mental health and glycemic control indices improved significantly after intervention in the intervention group.
Table 2.
Pre- and post-test values (n=101)
| Outcome, mean±SD | MBSR (n=50) | Control (n=51) | P |
|---|---|---|---|
| HBA1C | |||
| Before | 8.2±0.72 | 8.15±0.61 | 0.72 |
| After | 7.09±0.65 | 7.46±0.74 | 0.008* |
| P | <0.001* | <0.001* | |
| FBS | |||
| Before | 175.35±34.76 | 176.44±25.21 | 0.85 |
| After | 146.32±22.34 | 152.68±24.44 | 0.16 |
| P | <0.001* | <0.001* | |
| Depression score | |||
| Before | 17.15±6.94 | 15.0±6.30 | 0.09 |
| After | 13.69±8.07 | 14.55±8.06 | 0.58 |
| P | <0.001* | 0.41 | |
| Anxiety score | |||
| Before | 17.15±7.33 | 15.0±8.78 | 0.17 |
| After | 13.09±7.67 | 15.05±8.51 | 0.21 |
| P | <0.001* | 0.92 | |
| Stress score | |||
| Before | 21.11±8.23 | 19.72±7.98 | 0.24 |
| After | 17.36±8.51 | 18.73±7.86 | 0.39 |
| P | <0.001* | 0.37 |
*Significant at 0.05. MBSR: Mindfulness-based stress reduction group, FBS: Fasting blood sugar, HbA1c: Hemoglobin A1c, SD: Standard deviation
Mean changes of outcome variables after intervention were compared between the groups. Based on findings shown in Table 3, except FBS levels, all outcome variable scores' mean change was significant between the two groups. Although HbA1C levels were decreased in both groups after intervention, the difference was statistically significant.
Table 3.
Mean changes of outcome variables by study groups after intervention
| Outcome, mean±SEM | MBSR (n=50) | Control (n=51) | P |
|---|---|---|---|
| HBA1C | 1.1±0.08 | 0.68±0.1 | 0.007* |
| FBS | 29.03±4.6 | 23.75±3.67 | 0.11 |
| Depression score | 3.45±0.53 | 0.44±0.54 | <0.001* |
| Anxiety score | 3.98±0.65 | 0.05±0.56 | <0.001* |
| Stress score | 3.75±0.57 | 0.39±0.44 | <0.001* |
*Significant at 0.05. MBSR: Mindfulness-based stress reduction group, FBS: Fasting blood sugar, HbA1c: Hemoglobin A1c, SEM: Standard error of mean
Discussion
This study revealed an improvement in the glycemic and mental health indices in patients with type 2 diabetes following mindfulness training. Concerning the effect of different stress control methods on diabetes mellitus, several studies confirmed the role of stress control on diabetes improvement.[17,18,19,20,21] Boehm et al. also showed that good mental health status might positively influence diabetes and its control and reduce its complications.[22] The focus of the study conducted by Goyal et al., in 2014 was on the effect of mindfulness sessions on mental health. They investigated 3515 patients in 47 studies and concluded that this training can reduce patients' stress and anxiety and regulate their negative behaviors.[23] The study by Cash and Whittingham also highlighted the importance of mindfulness in reducing stress, anxiety, and depression, as well as improving patients' psychological quality.[24]
The findings of all these studies are consistent with those of our study. The awareness of the important role of psychological interventions in preventing lifestyle-related disorders and health promotion is increasingly encouraged. Among these psychological interventions, mindfulness, as a behavioral therapy technique, aims to reduce stress in patients and increase acceptance.[25] However, studies conducted by Hartmann et al. and van Son et al. revealed that although mindfulness training reduces anxiety and stress and improves patients' quality of life, it has no significant effect on blood sugar indices, including HbA1C.[10,26] A systematic review conducted by Noordali et al. revealed conflicting results about the effect of MBSR on HbA1c but more confident results in terms of mental health improvement.[27]
FBS and HbA1c were also decreased in the control group; however, the amount of reduction was significantly higher in the intervention group. This suggests that factors other than mental health also play a role in glycemic control. It can be said that routine care for diabetics in health care centers is well done.
It can be acknowledged that mindfulness-based therapy through stress management, improving mental health status and lifestyle, and encouraging patients to make better use of their medications might positively influence diabetes mellitus control.
Limitations of the study
Many other factors, including lifestyle, affect blood sugar, but we were not able to control some of the lifestyle components such as nutrition and physical activity in this study. Furthermore, although the researcher was present when participants were completing the questionnaires and provided explanations in case of any ambiguities in items, due to the self-report nature of the questionnaire on the one hand and the literacy level of the participants, on the other hand, the responses were not expected to be accurate enough.
Conclusions
In general, this study revealed that mindfulness training improved the quality of mental health and lowered glycemic control indices in patients with type 2 diabetes mellitus; therefore, health care centers are recommended to include this training in their routine care for these patients.
Financial support and sponsorship
This study was granted by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors of this paper highly appreciate the research and health deputies of Isfahan University of Medical Sciences for the financial and executive support of the project.
References
- 1.Animaw W, Seyoum Y. Increasing prevalence of diabetes mellitus in a developing country and its related factors. PLoS One. 2017;12:e0187670. doi: 10.1371/journal.pone.0187670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitebird RR, Kreitzer MJ, Vazquez-Benitez G, Enstad CJ. Reducing diabetes distress and improving self-management with mindfulness. Soc Work Health Care. 2018;57:48–65. doi: 10.1080/00981389.2017.1388898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thind H, Fava JL, Guthrie KM, Stroud L, Gopalakrishnan G, Sillice M, et al. Yoga as a complementary therapy for adults with type 2 diabetes: Design and rationale of the healthy, active, and in control (HA1C) study. Int J Yoga Therap. 2018;28:123–32. doi: 10.17761/2018-00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medina WL, Wilson D, de Salvo V, Vannucchi B, de Souza ÉL, Lucena L, et al. Effects of mindfulness on diabetes mellitus: Rationale and overview. Curr Diabetes Rev. 2017;13:141–7. doi: 10.2174/1573399812666160607074817. [DOI] [PubMed] [Google Scholar]
- 5.Varvogli L, Darviri C. Stress management techniques: Evidence-based procedures that reduce stress and promote health. Health Sci J. 2011;5:74. [Google Scholar]
- 6.Jung HY, Lee H, Park J. Comparison of the effects of Korean mindfulness-based stress reduction, walking, and patient education in diabetes mellitus. Nurs Health Sci. 2015;17:516–25. doi: 10.1111/nhs.12229. [DOI] [PubMed] [Google Scholar]
- 7.Youngwanichsetha S, Phumdoung S, Ingkathawornwong T. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res. 2014;27:227–30. doi: 10.1016/j.apnr.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Rosenzweig S, Reibel DK, Greeson JM, Edman JS, Jasser SA, McMearty KD, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: A pilot study. Altern Ther Health Med. 2007;13:36–8. [PubMed] [Google Scholar]
- 9.Carpenter R, DiChiacchio T, Barker K. Interventions for self-management of type 2 diabetes: An integrative review. Int J Nurs Sci. 2019;6:70–91. doi: 10.1016/j.ijnss.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartmann M, Kopf S, Kircher C, Faude-Lang V, Djuric Z, Augstein F, et al. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: Design and first results of a randomized controlled trial (the Heidelberger diabetes and stress-study) Diabetes Care. 2012;35:945–7. doi: 10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merkes M. Mindfulness-based stress reduction for people with chronic diseases. Aust J Prim Health. 2010;16:200–10. doi: 10.1071/PY09063. [DOI] [PubMed] [Google Scholar]
- 12.Fanning J, Osborn CY, Lagotte AE, Mayberry LS. Relationships between dispositional mindfulness, health behaviors, and hemoglobin A1c among adults with type 2 diabetes. J Behav Med. 2018;41:798–805. doi: 10.1007/s10865-018-9938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koloverou E, Tentolouris N, Bakoula C, Darviri C, Chrousos G. Implementation of a stress management program in outpatients with type 2 diabetes mellitus: A randomized controlled trial. Hormones (Athens) 2014;13:509–18. doi: 10.14310/horm.2002.1492. [DOI] [PubMed] [Google Scholar]
- 14.Keyworth C, Knopp J, Roughley K, Dickens C, Bold S, Coventry P. A mixed-methods pilot study of the acceptability and effectiveness of a brief meditation and mindfulness intervention for people with diabetes and coronary heart disease. Behav Med. 2014;40:53–64. doi: 10.1080/08964289.2013.834865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 16.Sahebi A, Asghari MJ, Salari R. Validation of depression anxiety and stress scale (DASS-21) for Iranian population. Iranian Psychology. 2005;1(4):50–60. [Google Scholar]
- 17.Bay R, Bay F. Combined therapy using acupressure therapy, hypnotherapy, and transcendental meditation versus placebo in type 2 diabetes. J Acupunct Meridian Stud. 2011;4:183–6. doi: 10.1016/j.jams.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Khatri D, Mathur KC, Gahlot S, Jain S, Agrawal RP. Effects of yoga and meditation on clinical and biochemical parameters of metabolic syndrome. Diabetes Res Clin Pract. 2007;78:e9–10. doi: 10.1016/j.diabres.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Priya G, Kalra S. Mind-body interactions and mindfulness meditation in diabetes. Eur Endocrinol. 2018;14:35–41. doi: 10.17925/EE.2018.14.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar V, Jagannathan A, Philip M, Thulasi A, Angadi P, Raghuram N. Role of yoga for patients with type II diabetes mellitus: A systematic review and meta-analysis. Complement Ther Med. 2016;25:104–12. doi: 10.1016/j.ctim.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Armani Kian A, Vahdani B, Noorbala AA, Nejatisafa A, Arbabi M, Zenoozian S, et al. The impact of Mindfulness-based stress reduction on emotional wellbeing and glycemic Control of patients with type 2 diabetes mellitus. J Diabetes Res eCollection. 2018 doi: 10.1155/2018/1986820. Article ID 1986820, 6 pages. https://doiorg/101155/2018/1986820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boehm JK, Trudel-Fitzgerald C, Kivimaki M, Kubzansky LD. The prospective association between positive psychological well-being and diabetes. Health Psychol. 2015;34:1013–21. doi: 10.1037/hea0000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med. 2014;174:357–68. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cash M, Whittingham K. What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness. 2010;1:177–82. [Google Scholar]
- 25.Sudhir PM. Advances in psychological interventions for lifestyle disorders: Overview of interventions in cardiovascular disorder and type 2 diabetes mellitus. Curr Opin Psychiatry. 2017;30:346–51. doi: 10.1097/YCO.0000000000000348. [DOI] [PubMed] [Google Scholar]
- 26.van Son J, Nyklícek I, Pop VJ, Blonk MC, Erdtsieck RJ, Spooren PF, et al. The effects of a mindfulness-based intervention on emotional distress, quality of life, and HbA (1c) in outpatients with diabetes (DiaMind): A randomized controlled trial. Diabetes Care. 2013;36:823–30. doi: 10.2337/dc12-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noordali F, Cumming J, Thompson JL. Effectiveness of mindfulness-based interventions on physiological and psychological complications in adults with diabetes: A systematic review. J Health Psychol. 2017;22:965–83. doi: 10.1177/1359105315620293. [DOI] [PubMed] [Google Scholar]