Abstract
Objective:
To assess whether frequency of marijuana and alcohol use are cross-sectionally associated with indicators of social and emotional well-being including loneliness, psychological distress, and flourishing across important life domains among young adults.
Method:
The study sample included 562 participants ages 22–29 who were originally recruited from an urban Pacific Northwest region in the US as part of a longitudinal study of social role transitions and alcohol use. At one assessment, participants completed an online survey that included a 3-item measure of loneliness, a 4-item measure of depression and anxiety symptoms, and a 12-item measure of flourishing as well as measures of marijuana and alcohol use frequency. Linear and generalized linear models were used to estimate associations of marijuana and alcohol use frequency with indicators of well-being.
Results:
Greater frequency of marijuana use was associated with higher levels of loneliness, higher levels of psychological distress, and lower levels of flourishing, with the greatest difference observed for daily marijuana users compared to non-users. However, these indicators of well-being did not significantly differ by levels of alcohol use frequency.
Conclusion:
Study findings suggest that frequent users of marijuana, but not alcohol, may experience more loneliness, more psychological distress, and less flourishing. Intervention approaches for frequent marijuana users may be warranted to reduce impacts of loneliness and psychological distress and improve overall well-being.
Keywords: marijuana, alcohol, loneliness, young adulthood, flourishing, psychological distress
1. Introduction
There is increasing concern about the social and emotional well-being of young adults (typically defined as ages 18 to 29). Within this age group, the prevalence of major depression and anxiety has been increasing (Weinberger et al., 2018; Goodwin et al., 2020). Loneliness is also common. One recent survey showed that 23% of Generation Z respondents reported often or always feeling lonely (Ballard, 2019), and a survey of college students found that nearly two-thirds reported feeling “very lonely” in the past year (American College Health Association, 2018). Loneliness has been linked to poor mental health outcomes (Cacioppo et al., 2006; Van Orden et al., 2010) as well as poor health more broadly (Holt-Lundstad & Smith, 2015; Leigh-Hunt et al., 2017). There are also concerns about increases in loneliness and their downstream effects during the ongoing Covid-19 pandemic (Killgore et al., 2020; Lee et al., 2020).
Substance use during young adulthood is also of public health importance as the prevalence of substance use and disordered use are highest during this developmental period (Compton et al, 2016; Patrick et al., 2016). As social attitudes and laws regarding marijuana use have become more relaxed in the US, there is particular concern about increasing prevalence of marijuana use and daily use among young adults (Center for Behavioral Health Statistics and Quality, 2020). Numerous studies have shown associations of marijuana and alcohol use with mental health problems including depression and anxiety (Dierker et al., 2018; Gobbi et al., 2019; Grant & Hartford, 1995; Lev-Ran et al., 2014, Moore et al., 2007). Further, there is some evidence that marijuana and alcohol use may be associated with loneliness (McKay et al., 2017; Osgood et al., 2014; Pandva et al., 2017).
It will also be important to understand how substance use relates to overall flourishing, not merely negative health outcomes. Flourishing is becoming a goal of public mental health beyond the absence of mental illness (Herman et al., 2005). Distinct from mental illness, flourishing has been conceptualized as exhibiting positive psychological well-being, psychosocial functioning, and positive emotions (Keyes, 2007), with other conceptualizations including domains of happiness and life satisfaction, mental and physical health, meaning and purpose, character and virtue, and close social relationships (VanderWeele al., 2017). Of the little research available, there is some evidence that flourishing is negatively related to substance use (Keyes et al., 2005; McGaffin et al., 2015), but other studies have shown no association (Low, 2011; Schotanus-Dijkstra et al., 2017). Thus, further examination of the association between substance use and flourishing is warranted.
To our knowledge, few studies have directly examined the relative strength of associations of marijuana and alcohol use with multiple, but conceptually and empirically distinct, indicators of emotional and social well-being among young adults, including both risk (e.g., loneliness) and protective (e.g., flourishing) psychosocial indicators of functioning. Understanding the potential differential associations of marijuana and alcohol could bring more clarity into the etiology of these outcomes in an era of more relaxed attitudes and laws related to marijuana use. Using cross-sectional survey data from young adults aged 22 to 29 originally recruited from the Greater Seattle area, this study examined whether frequency of marijuana and alcohol use were associated with loneliness, psychological distress, and flourishing.
2. Materials and Methods
2.1. Participants and Design
Study participants were originally recruited Pbetween2015–2016 in the greater Seattle, Washington, area as part of a longitudinal study on social role transitions and alcohol use. They were recruited through social media, community outreach, newspaper and online advertisements and other methods (for detailed study methods see Patrick et al., 2018). Eligibility criteria included being 18 to 23 years-old at screening, drinking any alcohol in the past year, living within 60 miles of study offices, and willingness to attend an in-person session for identification verification, consent, and training. Study procedures included a baseline assessment, 24 months of consecutive monthly surveys, and a 30-month post baseline follow-up. This longitudinal study included 778 young adults. Participants were compensated $40 in Amazon gift cards for the baseline and 30-month assessment and between $20 and $45 for monthly surveys depending on survey length.
In January 2020, all eligible participants who did not discontinue study participation during the original longitudinal study (N=767) were invited to complete an additional supplemental online assessment to obtain updated contact information and current social role status, mental health and substance use. Participants received email and text message invitations to this new survey with a link to an information statement followed by an online survey which was open for three weeks. Of those invited, 580 (75.6%) completed the assessment. More frequent marijuana users at baseline were less likely to complete the survey (χ2 (4) = 18.72; p-value <0.001). There was no statistically significant difference in survey completion by alcohol use frequency (p-value = .136). Participants were compensated with a $15 Amazon.com eGiftcard for completion of the survey. All activities were approved by the local institutional review board and no adverse consequences were reported. This final January 2020 assessment was used for the current study due to the inclusion of loneliness and flourishing measures, which were not included in any of the prior assessments.
2.2. Measures
Marijuana use frequency.
Participants indicated the number of days in the past month that they used marijuana. To group individuals according to different levels of use, we created a categorical variable based on this item: None, 1–9, 10–19, 20–29, and 30 days in the past month.
Alcohol use frequency.
Using an item from the Quantity Frequency questionnaire (Marlatt et al, 1995), participants reported their past month frequency of drinking, with response options ranging from "I did not drink at all" (0) to "Every day" (10). To approximate the categories of marijuana frequency above, this variable was collapsed into four categories for analyses: did not drink at all, once a month to once a week, two times a week to three times a week, and four times a week or more. Daily use was infrequent (1.0%) and, thus, not included as a separate category.
Loneliness.
The Three-Item Loneliness Scale (Hughes et al., 2004), which was based on the Revised UCLA Loneliness Scale (Russell et al., 1980), asked participants to report from 0 (hardly ever) to 2 (often) how often they felt “that you lack companionship”, “left out”, and “isolated from others”. Items scores were summed to yield an overall score (α = .80).
Depression and Anxiety.
Depression and anxiety symptoms were measured with the Patient Health Questionnaire-4 (Kroenke et al., 2009). Two items assessed how often they were bothered by depressive symptoms (“Little interest or pleasure in doing things”, “Feeling down, depressed, or hopeless”) and two assessed anxiety symptoms (“Feeling nervous, anxious, or on edge”, “Not being able to stop or control worrying”). Response options ranged from 0 (“not at all”) to 3 (“nearly every day”). The four items were summed to yield a measure of psychological distress (α = .89). The total PHQ-4 score has been used previously in various studies (e.g., Holingue et al., 2020; Pitcho-Prelorentzos et al., 2018) and shows strong correlations with other mental health and functioning scales (Kroenke et al, 2009).
Flourishing.
The 12-item flourishing measure asked participants to rate their status on six domains (two items each) considered to be universally desired: happiness and life satisfaction, mental and physical health, meaning and purpose, character and virtue, close social relationships, and financial and material stability (Vanderweele, 2017). Each item was scored from 0 to 10 with 10 indicating the greatest frequency or level of that item, and then summed for a total score (α = .91).
Demographic characteristics including age, sex (0: female; 1: male), race (dummy coded as White [reference], Asian, Other), Hispanic ethnicity (0: no; 1: yes), sexual orientation (0: heterosexual, 1: non-heterosexual), and parents’ highest level of education were used as covariates in analyses.
2.3. Data Analytic Plan
Regression models were used for our primary analytic approach. When examining frequency of use as the covariate of interest, we entered dummy variables with the reference category being no use in the past month. In additional models, we entered the marijuana and alcohol use variables as ordinal variables to test for a linear trend. We treated loneliness and flourishing as Gaussian distributed outcomes in linear models. Because of its positive skew and evidence of over-dispersion, PHQ-4 score was modeled using negative binomial regression to estimate count ratios, which describe the proportional increase in the count (i.e., total score) associated with a 1-unit increase in the covariate of interest. All models adjusted for demographic characteristics.
As sensitivity analyses, we explored different characterizations of alcohol use including past month typical number of drinks per week and number of binge drinking episodes. Results showed a similar pattern of associations to those of frequency of any drinking and, thus, were not reported here. Further, to account for potential differences in survey inclusion, additional sensitivity analyses adjusted for baseline marijuana use categories. Results were essentially unchanged and not reported here.
Analyses were conducted using R Statistical Software, version 3.6.2 (R Core Team, 2019).
3. Results
Analyses included 562 (96.9%) participants without missing covariate or outcome data at the study visit. Table 1 shows distributions of study variables. Outcomes were moderately correlated with one another (Loneliness-Flourishing Spearman’s ρ = −0.52; Flourishing-Psychological Distress ρ = −0.58; Loneliness-Psychological Distress ρ = 0.48). Prior to categorization, marijuana and alcohol use frequency showed a correlation of ρ = 0.12.
Table 1.
Distribution of participant characteristics.
| Variable | Mean (SD) or % | Range |
|---|---|---|
| Completed Bachelor’s degree | 70.9 | |
| Parent completed Bachelor’s degree | 66.9 | |
| Male sex | 39.2 | |
| Race/ethnicity | ||
| White, non-Hispanic | 54.2 | |
| Asian-American, non-Hispanic | 18.8 | |
| Other, non-Hispanic | 18.2 | |
| Hispanic ethnicity, any race | 8.8 | |
| Non-heterosexual orientation | 30.0 | |
| Age, years a | 25.1 (1.8) | 22, 29 |
| Number of marijuana use days, past month | ||
| 0 | 59.3 | |
| 1–9 | 21.9 | |
| 10–19 | 5.4 | |
| 20–29 | 7.7 | |
| 30 | 5.6 | |
| Frequency of past month alcohol use | ||
| None | 14.8 | |
| Once a month to weekly | 49.6 | |
| 2–3 times per week | 24.6 | |
| 4 times/week to daily | 11.0 | |
| Loneliness b | 2.3 (1.8) | 0, 6 |
| Flourishing c | 77.4 (20.4) | 17, 120 |
| PHQ-4 d | 3.8 (3.1) | 0, 12 |
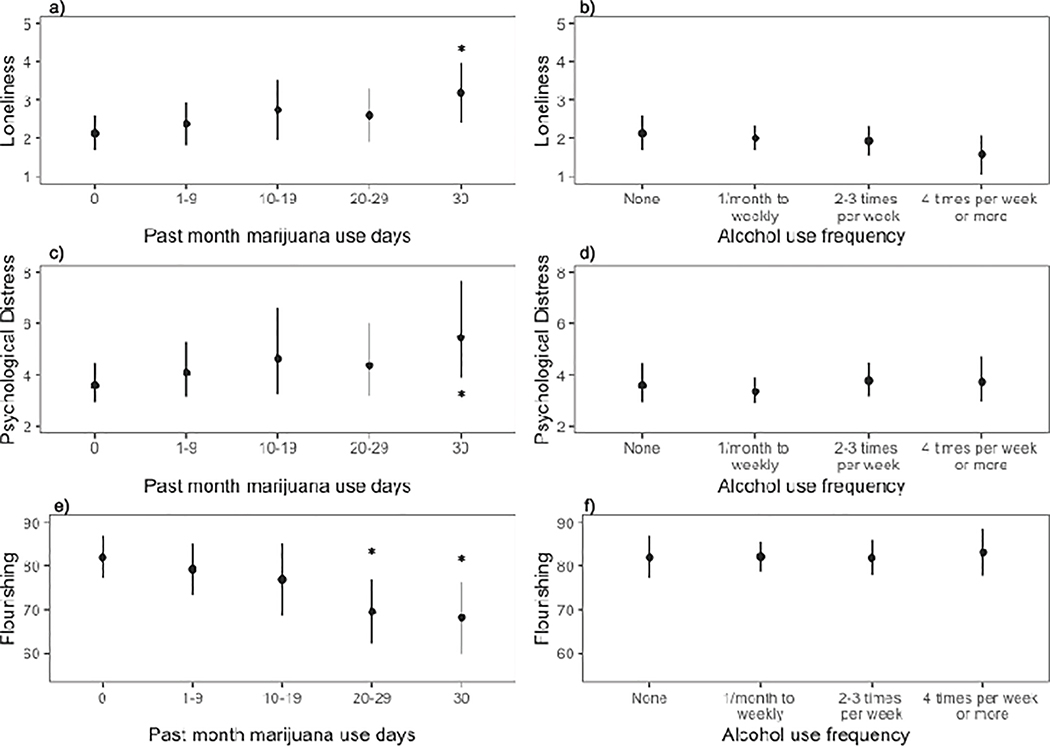
Figure 1 shows model-predicted levels of loneliness, psychological distress, and flourishing by categories of marijuana and alcohol use. There appeared to be a general dose-response association where more frequent marijuana users showed greater loneliness, more psychological distress, and less flourishing (p for linear trend <.001). However, statistically significant differences relative to non-users were only observed for daily users for loneliness and distress, and for daily users and those using 20–29 days for flourishing (see full model results in the online Supplemental Table). In contrast, for alcohol use, more frequent users did not show statistically significant differences in the outcomes relative to non-users.
Figure 1.
Model-predicted levels and 95% confidence intervals of loneliness (a and b), psychological distress (c and d), and flourishing (e and f) according to marijuana and alcohol use categories.
4. Discussion
In this study of young adults, those using marijuana more frequently over the past month showed worse social and emotional well-being compared to non-users. There appeared to be a general dose-response association where the difference compared to non-users tended to be stronger with greater frequency of marijuana use, with daily users showing the greatest difference. In contrast, there was no statistically significant association between frequency of alcohol use and any of the outcomes.
The lack of association between alcohol use frequency and indicators of emotional well-being may be consistent with other studies of young adult samples (e.g., Cranford et al., 2009; Kenney et al., 2013). Results may also reflect trends showing a decoupling of the association between heavy alcohol use and depression (Keyes et al., 2020). Young adults report multiple motivations for alcohol use, which can include facilitation of social goals (e.g., making new friends, finding dating partners; Schulenberg and Maggs, 2002). Thus, frequent alcohol use, to a degree, may be more socially normative and not necessarily indicative of psychological distress. However, given that young adults who engage in solitary drinking are at risk for increased depressive symptoms (Fleming et al., in press; Keough et al., 2015) and loneliness (Gonzalez & Skewes, 2013), we encourage future work to examine how contexts of alcohol and marijuana use (e.g., solitary versus social use) as well as their co-use and simultaneous use may impact psychosocial indicators of well-being.
Although it is becoming more socially accepted and available especially in states where recreational use is legal, marijuana use is not as normative as alcohol use. Frequent marijuana use may, then, reflect a pattern of substance use that is less common for social purposes and more common for self-medication purposes to cope with negative affect (Patrick et al., 2019; Skalisky et al., 2019), especially among those with mood and anxiety disorders (Sarvet et al., 2018). Some studies have found that marijuana users have shown higher levels of emotion dysregulation (Bonn-Miller et al., 2008), which could account for increased levels of distress.
Results indicating that frequent marijuana users show lower levels of flourishing may be consistent with studies indicating that adolescent marijuana users have worse social role adaptation and functioning as well as lower life satisfaction in young adulthood (Brook et al., 2002; Fergusson et al., 2015; Schulenberg et al., 2005). This is concerning given that young adulthood is a formative developmental period when social roles are formalized and thus could portend lingering effects into later adulthood.
This study had some notable limitations. This sample was recruited from one metropolitan region in the Northwest US via social media and other sources. Thus, results may not generalize to the broader population of young adults in the US; especially notable since a large percentage reported non-heterosexual orientation, most of the sample completed 4-year college, and a majority still lived in WA, a legal marijuana state in January 2020. Also, this study used cross-sectional data and could not assess temporality of the associations.
Findings suggest that young adult marijuana users, especially frequent users, may show poor emotional and social well-being, including more loneliness, more psychological distress, and less flourishing. This group may benefit from interventions that provide strategies for reducing high-risk use, addressing motivations for use, and adaptive strategies for managing mood and loneliness. Interventions for loneliness have aimed to increase social interactions, enhance social support, and improve social skills (Cacioppo et al., 2015), but future work could specifically examine these components among frequent marijuana users.
Supplementary Material
HIGHLIGHTS.
Young adult substance use and social and emotional health indicators were assessed.
Marijuana use was associated with loneliness and distress and less flourishing.
Alcohol use frequency was not associated with any of the indicators of well-being.
Frequent marijuana users may show low levels of social and emotional well-being.
Acknowledgements.
The authors are grateful to Devon Alisa Abdallah for her assistance with data management and documentation of study procedures.
Role of Funding Source. This study was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (R01AA027496, R01AA022087, PI: Christine Lee). The funders did not play any role in the design, data collection, analyses, interpretation of results, or manuscript preparation for this study. The content of this paper is solely the responsibility of the authors and does not necessarily reflect the official views of the funding agencies.
Footnotes
Conflict of Interest. No conflict declared.
Declarations of Interests: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American College Health Association, 2018. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2018. Silver Spring, MD: American College Health Association. [Google Scholar]
- Ballard J, 2019. Millenials are the loneliest generation. Retrieved from https://today.yougov.com/topics/lifestyle/articles-reports/2019/07/30/loneliness-friendship-new-friends-poll-survey.
- Bonn-Miller MO, Vujanovic AA, & Zvolensky MJ, 2008. Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Subst. Use Misuse, 43, 1653–1665. [DOI] [PubMed] [Google Scholar]
- Brook JS, Adams RE, Balka EB, & Johnson E, 2002. Early adolescent marijuana use: Risks for the transition to young adulthood. Psychol. Med, 32, 79. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA, 2006. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol. Aging, 21, 140. [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT, 2015. Loneliness: Clinical import and interventions. Perspect. Psychol. Sci, 10, 238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2020. Results from the 2019 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Admiinistration, Rockville, MD: Retrieved from https://datafiles.samhsa.gov/ [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, & Hughes A, 2016. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiat, 3, 954–964. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Eisenberg D, & Serras AM, 2009. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addict. Behav, 34, 134–145. [DOI] [PubMed] [Google Scholar]
- Dierker L, Selya A, Lanza S, Li R, & Rose J, 2018. Depression and marijuana use disorder symptoms among current marijuana users. Addict. Behav, 76, 161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ, 2015. Psychosocial sequelae of cannabis use and implications for policy: findings from the Christchurch Health and Development Study. Soc. Psychiatry Psychiatr. Epidemiol, 50, 1317–1326. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Stevens AL, Jaffe AE, Cadigan JM, Rhew IC, & Lee CM, in press Antecedents, correlates, and potential consequences of young adult solitary alcohol use. Psychol. Addict. Behav. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, Ware M, Marmorstein N, Cipriani A, Dendukuri N, & Mayo N, 2019. Association of cannabis use in adolescence and risk of depression, anxiety, Pre-proofandsuicidalityinyoungadulthood:a systematic review and meta-analysis. JAMA Psychiatry, 76, 426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, & Skewes MC, 2013. Solitary heavy drinking, social relationships, and negative mood regulation in college drinkers. Addict. Res. Theory, 21, 285–294. [Google Scholar]
- Goodwin RD, Weinberger AH, Kim JH, Wu M, & Galea S, 2020. Trends in anxiety among adults in the United States, 2008–2018: Rapid increases among young adults. J. Psychiatr. Res, 130, 441–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, & Harford TC, 1995. Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey. Drug Alcohol Depend, 39, 197–206. [DOI] [PubMed] [Google Scholar]
- Herrman H, Saxena S, & Moodie R, 2005. Promoting mental health: concepts, emerging evidence, practice: a report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. World Health Organization, Geneva, Switzerland. [Google Scholar]
- Holingue C, Kalb LG, Riehm KE, Bennett D, Kapteyn A, Veldhuis CB, Johnson RM, Fallin MD, Kreuter F, Stuart EA, & Thrul J, 2020. Mental Distress in the United States at the Beginning of the COVID-19 Pandemic. Am. J. Public Health, 110, 1628–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D, 2015. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci, 10, 227–237. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT, 2004. A Short Scale for Measuring Loneliness in Large Surveys: Results from two population-based studies. Res. Aging, 26, 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeste DV, Lee EE, & Cacioppo S, 2020. Battling the modern behavioral epidemic of loneliness: Suggestions for research and interventions. JAMA Psychiatry, 77, 553–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keough MT, O'Connor RM, Sherry SB, & Stewart SH, 2015. Context counts: Solitary drinking explains the association between depressive symptoms and alcohol-related problems in undergraduates. Addict. Behav, 42, 216–221. [DOI] [PubMed] [Google Scholar]
- Kenney SR, Lac A, Labrie JW, Hummer JF, & Pham A, 2013. Mental health, sleep quality, drinking motives, and alcohol-related consequences: a path-analytic model. J. Stud. Alcohol Drugs, 74, 841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CL, 2005. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consul. Clin. Psychol, 73, 539. [DOI] [PubMed] [Google Scholar]
- Keyes CLM, 2007. Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. Am. Psychol, 62, 95–108. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hamilton A, Patrick ME, & Schulenberg J, 2020. Diverging Trends in the Relationship Between Binge Drinking and Depressive Symptoms Among Adolescents in the U.S. From 1991 Through 2018. J. Adolesc. Health, 66, 529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WD, Cloonen SA, Taylor EC, & Dailey NS, 2020. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res, 290, 113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, & Löwe B, 2009. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics,50, 613–621. [DOI] [PubMed] [Google Scholar]
- Lee CM, Cadigan JM, & Rhew IC, 2020. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health, 67, 714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, & Caan W, 2017. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. [DOI] [PubMed] [Google Scholar]
- Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, & Rehm J, 2014. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol. Med, 44, 797. [DOI] [PubMed] [Google Scholar]
- Low KG, 2011. Flourishing, Substance Use, and Engagement in Students Entering College: A Preliminary Study. J. Am. Coll. Health, 59, 555–561. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, & Larimer, M., 1995. Preventing alcohol abuse in college students: A harm-reduction approach. In Boyd GM, Howard J, Zucker RA (Eds.), Alcohol problems among adolescents: Current directions in prevention research (pp. 147–172). Hillside, NJ, England: Lawrence [Google Scholar]
- McGaffin BJ, Deane FP, Kelly PJ, & Ciarrochi J, 2015. Flourishing, languishing and moderate mental health: Prevalence and change in mental health during recovery from drug and alcohol problems. Addict. Res. Theory, 23, 351–360. [Google Scholar]
- McKay MT, Konowalczyk S, Andretta JR, & Cole JC, 2017. The direct and indirect effect of loneliness on the development of adolescent alcohol use in the United Kingdom. Addict. Behav. Rep, 6, 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, & Lewis G, 2007. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet, 370, 319–328. [DOI] [PubMed] [Google Scholar]
- Osgood DW, Feinberg ME, Wallace LN, & Moody J, 2014. Friendship group position and substance use. Addict. Behav, 39, 923–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandya I, 2017. Adjustment, anxiety and loneliness in cannabis users and controls. Indian Journal of Health & Wellbeing, 8, 864–866. [Google Scholar]
- Patrick ME, Terry McElrath YM, Kloska DD, & Schulenberg JE, 2016. High-intensity drinking among young adults in the United States: Prevalence, frequency, and developmental change. Alcohol Clin. Exp. Res, 40, 1905–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Rhew IC, Lewis MA, Abdallah DA, Larimer ME, Schulenberg JE, & Lee CM, 2018. Alcohol motivations and behaviors during months young adults experience social role transitions: Microtransitions in early adulthood. Psychol. Addict. Behav, 32, 895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Fairlie AM, Cadigan JM, Abdallah DA, Larimer ME, & Lee CM, 2019. Daily Motives for Alcohol and Marijuana Use as Predictors of Simultaneous Use Among Young Adults. J. Stud. Alcohol Drugs, 80, 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitcho-Prelorentzos S, Kaniasty K, Hamama-Raz Y, Goodwin R, Ring L, Ben-Ezra M, & Mahat-Shamir M, 2018. Factors associated with post-election psychological distress: The case of the 2016 US presidential election. Psychiatry Res, 266, 1–4. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2019. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- Russell D, Peplau LA, & Cutrona CE, 1980. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J. Pers. Soc. Psychol, 39, 472. [DOI] [PubMed] [Google Scholar]
- Sarvet AL, Wall MM, Keyes KM, Olfson M, Cerdá M, & Hasin DS, 2018. Self-medication of mood and anxiety disorders with marijuana: Higher in states with medical marijuana laws. Drug Alcohol Depend, 186, 10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schotanus-Dijkstra M, Ten Have M, Lamers SM, de Graaf R, Bohlmeijer ET, 2017. The longitudinal relationship between flourishing mental health and incident mood, anxiety and substance use disorders. Eur. J. Public Health, 27, 563–568. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, & Maggs JL, 2002. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J. Stud. Alcohol, Suppl, 54–70. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Merline AC, Johnston LD, O'Malley PM, Bachman JG, & Laetz VB, 2005. Trajectories of marijuana use during the transition to adulthood: The big picture based on national panel data. J. Drug Issues, 35, 255–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalisky J, Wielgus MD, Aldrich JT, & Mezulis AH, 2019. Motives for and impairment associated with alcohol and marijuana use among college students. Addict. Behav, 88, 137–143. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr, 2010. The interpersonal theory of suicide. Psychol. Rev, 117, 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, 2017. On the promotion of human flourishing. Proc. Natl. Acad. Sci. U.S.A, 114, 8148–8156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, & Weiss SR, 2014. Adverse health effects of marijuana use. N. Engl. J. Med, 370, 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, & Goodwin RD (2018). Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychological medicine, 48(8), 1308–1315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.