Abstract
Background
The access site for endovascular therapy (EVT) is often limited because of multi-vascular diseases. Prior lower limb bypass can potentially limit the availability of common femoral artery access when EVT is required.
Case summary
An 88-year-old woman who presented with non-healing ulceration in the dorsalis pedis of the left foot despite treatment for several months was admitted to our hospital. She had undergone axillo-bilateral femoral bypass surgery for right critical limb ischaemia 3 years previously. Ultrasound and contrast computed tomography demonstrated bypass graft occlusion, left superficial femoral artery (SFA)-popliteal artery long chronic total occlusion from the origin with severe calcification and severe stenosis in the bilateral common femoral artery close to the anastomotic site. EVT for the left SFA occlusion was necessary to save the left foot, but access sites for EVT were limited. We decided to puncture an occluded axillo-femoral prosthetic bypass graft. It is difficult to cross the wire with only an antegrade approach. Therefore, it was necessary to use a bi-directional approach with dorsalis pedis artery puncture and the Rendez-vous technique. Finally, angiogram demonstrated improved blood flow to the wound site, and haemostasis at the puncture site could be achieved by manual compression. The ulceration healed within a month.
Discussion
Direct puncture of a prosthetic bypass graft and additional techniques resulted in complete revascularization. Thus, direct puncture of a bypass graft could be a useful EVT strategy for patients with complex and extremely long chronic total occlusion.
Keywords: Case report, Peripheral artery disease, Endovascular treatment, Superficial femoral artery, Chronic total occlusion, Direct graft puncture
Learning points
The access site for endovascular therapy is often limited because these patients have multi-vascular diseases and have previously undergone lower limb bypass surgery.
Direct puncture of a bypass graft could also be a useful endovascular therapy strategy for patients with complex peripheral artery disease.
The Rendez-vous technique, distal puncture and other techniques have been recognized as being useful for long chronic total occlusion lesions.
Introduction
Peripheral artery disease is becoming more common because of the aging population, the growing prevalence of diabetes, and the spread of renal insufficiency. These systematic comorbidities contribute to lesion complexity.1 Clinical guidelines recommend revascularization as one of the first steps in the treatment of chronic limb-threatening ischaemia (CLTI).2 The access site for endovascular therapy (EVT) in these patients is often limited because of the presence of multi-vascular diseases. Prior lower limb bypass can potentially limit the availability of common femoral artery access when EVT is required.
Timeline
| Time | Events |
|---|---|
| 4 years previously | Axillo-bilateral femoral bypass for right chronic limb-threatening ischaemia, bilateral common iliac artery stenosis, bilateral superficial artery total occlusion |
| 2 years previously | Right below-knee amputation due to diabetic foot ulcer |
| One month prior to admission | Non-healing ulceration in the dorsalis pedis of the left foot despite treatment for several months |
| Month 0 in- hospital management | Endovascular therapy using direct puncture of a prosthetic bypass graft, Rendez-vous technique and distal puncture |
| Month 1 | The ulceration healed |
Case presentation
An 88-year-old woman who presented with non-healing ulceration in the dorsalis pedis of the left foot despite treatment for several months was admitted to our hospital (Figure 1). She had undergone axillo-bilateral femoral bypass surgery for right critical limb ischaemia (CLI) 3 years previously with bilateral common iliac artery (CIA) stenosis with severe calcification and vessel tortuosity and bilateral superficial femoral artery (SFA)-popliteal artery (Pop. A) chronic total occlusion (CTO). Unfortunately, a year later, she required right below-knee amputation due to diabetic gangrene. On admission, the ankle-brachial pressure index (ABI) of the left side was 0.5 and skin perfusion pressure (SPP) was markedly low: 19 mmHg for the dorsal artery and 21 mmHg for the plantar artery. Ultrasound and contrast computed tomography demonstrated bypass graft occlusion, left SFA-Pop. A long CTO from the origin with severe calcification and severe stenosis in the bilateral common femoral artery was close to the anastomotic site (Figure 2). We considered that the cause of CLTI was the left SFA occlusion. Endovascular therapy for the left SFA occlusion was necessary to save the left foot, but access sites for EVT were limited.
Figure 1.
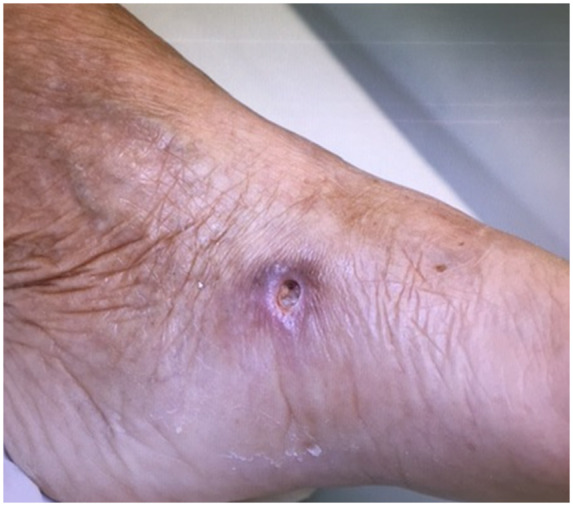
Non-healing ulceration in the dorsalis pedis of the left foot despite treatment for several months.
Figure 2.
Ultrasound (A) and contrast computed tomography (B, C) demonstrated bypass graft occlusion, left superficial femoral artery (SFA)-popliteal artery (Pop. A) long chronic total occlusion (CTO) from the origin with severe calcification and severe stenosis in the bilateral common femoral artery is close to the anastomotic site. DFA, deep femoral artery.
The contralateral femoral artery was a difficult option because the right CIA had stenosis with a calcified lesion and blood vessel meandering. The ipsilateral femoral artery showed stenosis by the anastomosis of the bypass graft, and the left SFA was occluded from the origin. We decided to puncture the occluded axillo-femoral prosthetic bypass graft. First, ultrasonography was performed, and the border of the thrombus in the graft lumen was confirmed. We punctured the occluded side of the border on rib bone in consideration of haemostasis (Figure 3). A 6 Fr 45 cm sheath (TERUMO, Japan) was inserted in an antegrade manner, and 5000 units of unfractionated heparin were administered intravenously. Control angiogram demonstrated left SFA occlusion from the origin to the popliteal artery with severe calcification and short occlusion of the anterior-tibial artery. A 0.014-inch wire (Command, Century, Japan) could not pass through the SFA-CTO lesion with an antegrade approach. Only a penetration wire (Astato9-12, ASAHI INTECC, Japan) could be slightly advanced into the CTO lesion. Next, distal puncture from the dorsalis pedis artery was performed; a 0.014-inch soft-tip wire (Cruise, ASAHI INTECC, Japan) was passed retrogradely to the popliteal artery through the anterior-tibial artery CTO lesion. Subsequently, a 0.035-inch wire (Radifocus 1.5 J stiff, TERUMO, Japan) could be advanced to the popliteal artery antegradely using the knuckle wire technique. The antegrade and retrograde wires could meet by using the Rendez-vous technique in the popliteal artery in the CTO site (Figure 4). After repeated pre-dilatation with a non-compliance balloon, self-expandable bare-nitinol stents (LIFE stent; Medicon, Japan, Innova; Boston Scientific, USA) were deployed from the proximal SFA to the popliteal artery. Finally, angiogram demonstrated complete revascularization, although the intravascular ultrasound revealed an incomplete expansion of stent only in the part of calcification (Figure 5). Hemostasis of the puncture site was safely achieved with only 5 min of manual compression. After treatment, the ABI improved to 0.9 and the level of SPP improved to 56 mmHg for the dorsal artery and 52 mmHg for the plantar artery. The ulceration epithelized within a month.
Figure 3.
The yellow arrow indicates the puncture site in this procedure. The puncture site of the prosthetic bypass graft is on the 12th rib.
Figure 4.
(A) Control angiogram demonstrated left superficial femoral artery occlusion from the origin to the popliteal artery with severe calcification and short occlusion of the anterior-tibial artery (ATA). (B) Distal puncture, Knuckle wire technique and Rendez-vous technique is useful techniques for complex long chronic total occlusion lesion.
Figure 5.
Final angiogram demonstrated significant improvement of blood flow in superficial femoral artery-popliteal artery (A) and also below the knee lesion (B and C), although the intravascular ultrasound revealed an incomplete expansion of stent in the part of calcification (A). The ulceration could be epithelized quickly (D).
Discussion
While bypass surgery has been the standard method of revascularization, it is not feasible in every patient because of associated comorbidities such as cardiovascular disease and heart failure. In these cases, EVT can be applied in CLI patients due to the development of new devices and improved techniques.3 However, the access sites for EVT are often limited because these patients have multi-vascular diseases and have previously undergone lower limb bypass surgery. To our knowledge, this is the first report of successful EVT for long SFA-CTO with the direct puncture of a prosthetic bypass graft.
In our case, puncture of the common femoral artery (CFA) was a general access site, whereas the abdominal aorta and iliac artery had severe tortuosity and the CFA showed a graft anastomosis. Thus, it was difficult to approach from the bilateral CFA, and it was also impossible to advance a catheter from the brachial artery to the descending aorta due to severe aorta meandering. Finally, we had to choose direct puncture of the axillo-femoral bypass graft. Although direct puncture of prosthetic bypass grafts has been shown to carry no greater risk for catheter angiography than puncture of native vessels, there were some concerns about complications related to the direct puncture of a prosthetic bypass graft.4,5 Previous reports have demonstrated that the frequency of complications was about 10–20%. The major causes of complications are bleeding and infection.4–10
In this case, different methods were considered to avoid bleeding. First, the border of the occlusion site was detected by ultrasonography and the sheath was advanced from the occluded site. With this method, the puncture was made in an occluded site, which made it easy to achieve haemostasis. A previous report recommended the use of ultrasound guidance to avoid complications.11
Ultrasound guidance should be considered for any patient at high risk for a difficult access or complications. Moreover, ultrasound provides information about the tissue characteristics around the bypass graft. These tissue characteristics can help to achieve haemostasis and avoid expansion bleeding into free space. Fortunately, we achieved haemostasis rather easily due to the adhesion of the bypass graft after the operation. On the contrary, we should not perform direct graft puncture immediately after bypass surgery to prevent bleeding and infectious complications. Second, the puncture site was just above the 12th rib. Effective manual compression could be achieved because the 12th rib was present under the puncture site. Thus, we could safely and easily achieve haemostasis in a short time after the removal of the sheath.8 If we had not been able to achieve complete haemostasis, surgical cut-down and suturing were planned as the next strategy.
Since the SFA and popliteal artery had long CTO with severe calcification, it was difficult to cross the wire using only an antegrade approach. Thus, we had to use a bi-directional approach involving dorsalis pedis artery puncture and the Rendez-vous technique. Bi-directional wiring is useful for improving the success rate of recanalization for CTO in the field of peripheral intervention. Externalization of the wire can enable a strong back-up force for the deployment of devices in severe calcification lesions. Regarding the incomplete stent expansion in the part of severe calcification, we expected short-term patency until healing ulcer because activity of daily living (ADL) of this patient was in the stage of severe frailty, although we were concerned about the increased risk of in-stent restenosis. Thus, direct puncture of a prosthetic bypass graft along with other techniques resulted in complete revascularization despite the presence of an extremely long chronic total occlusion with a severely calcified lesion.
Conclusion
We experienced a complex case of EVT that was treated from an occluded axillo-femoral bypass graft. We were able to recanalize and safely achieve hemostasis using various techniques. The Rendez-vous technique, distal puncture, and other methods are useful for the treatment of long CTO lesions. Thus, direct puncture of a bypass graft could also be a useful EVT strategy for patients with complex peripheral artery disease.
Lead author biography

Makoto Sugihara graduated from Fukuoka University School of Medicine in 2001. From 2004 to 2008, he underwent training to be an interventional cardiologist at Fukuoka Tokusyukai Hospital and Kyusyu Medical Center, Fukuoka, Japan. He now works in the Department of Cardiology at Fukuoka University Hospital, Fukuoka, Japan. He has a special interest in interventional cardiology and endovascular treatment.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidelines.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Iida O, Nakamura M, Yamauchi Y, Kawasaki D, Yokoi Y, Yokoi H. et al. Endovascular treatment for infrainguinal vessels in patients with critical limb ischemia: OLIVE registry, a prospective, multicenter study in Japan with 12-month follow-up. Circ Cardiovasc Interv 2013;6:68–76. [DOI] [PubMed] [Google Scholar]
- 2. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg 2007;33:S1–75. [DOI] [PubMed] [Google Scholar]
- 3. Iida O, Soga Y, Yamauchi Y, Hirano K, Kawasaki D, Yamaoka T. et al. Clinical efficacy of endovascular therapy for patients with critical limb ischemia attributable to pure isolated infrapopliteal lesions. J Vasc Surg 2013;57:974–981. [DOI] [PubMed] [Google Scholar]
- 4. Eisenberg RL, Mani RL, McDonald EJ.. The complication rate of catheter angiography by direct puncture through aorto-femoral bypass grafts. Am J Roentgenol 1976;126:814–816. [DOI] [PubMed] [Google Scholar]
- 5. AbuRahma AF, Robinson PA, Boland JP.. Safety of arteriography by direct puncture of a vascular prosthesis. Am J Surg 1992;164:233–236. [DOI] [PubMed] [Google Scholar]
- 6. Cowling MG, Belli AM, Buckenham TM.. Evaluation and complications of direct graft puncture in thrombolysis and other interventional techniques. Cardiovasc Intervent Radiol 1996;19:82–84. [DOI] [PubMed] [Google Scholar]
- 7. Gallagher MJ, Dixon SR, Safian RD, Madala M, Abraham R, Rimar SD. et al. Safety of percutaneous transfemoral coronary and peripheral procedures via aortofemoral synthetic vascular grafts. Am J Cardiol 2005;96:382–385. [DOI] [PubMed] [Google Scholar]
- 8. Katoh H, Nozue T, Michishita I.. Direct puncture of the prosthetic bypass graft in the treatment of critical limb ischemia patient undergoing prior axillo-femoral bypass. Cardiovasc Interv and Ther 2013;28:123–127. [DOI] [PubMed] [Google Scholar]
- 9. Lee DE, Waldman DL, Sumida RK, Green RM.. Direct graft puncture with use of a crossed catheter technique for thrombolysis of peripheral bypass grafts. J Vasc Interv Radiol 2000;11:445–452. [DOI] [PubMed] [Google Scholar]
- 10. Page JE, Buckenham TM, Taylor RS.. Accelerated thrombolysis facilitated by direct puncture of occluded prosthetic femoral grafts. Australas Radiol 1992;36:230–233. [DOI] [PubMed] [Google Scholar]
- 11. Seto AH, Abu-Fadel MS, Sparling JM, Zacharias SJ, Daly TS, Harrison AT, Suh WM. et al. Real-time ultrasound guidance facilitates femoral arterial access and reduces vascular complications: FAUST (Femoral Arterial Access With Ultrasound Trial). JACC Cardiovasc Interv 2010;3:751–758. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.






