Abstract
Background:
Non-pharmacological intervention methods such as rehabilitation training or psychological treatment are mostly used in the treatment of depression owing to the limitation of adverse reactions such as drug treatment. However, the best non-pharmacological treatment strategy for depression in college students is unclear. Therefore, it is significant to discover non-drug intervention methods that can improve the depression symptoms of college students.
Method:
Electronic databases as of Sep 15, 2019, were searched, and reference lists and pharmaceutical dossiers were reviewed to detect published and unpublished studies from the date of their inception to Sep 15, 2019. With document quality evaluations and data extraction, Meta-Analysis was performed using a random effect model to evaluate the intervention effect of the aerobic exercise, traditional Chinese exercises, and meditation.
Results:
A total of 44 original studies were included. The random effect model was used to combine the effect values with Standard Mean Difference (SMD), and the results were: aerobic exercise [SMD = –0.53, 95% CI (–0.77, –0.30), I2 = 80%, P < .001], traditional Chinese exercises [SMD = –0.42, 95% CI (–0.74, –0.10), I2 = 90%, P = .01], meditation [SMD = –0.51, 95% CI (–0.90, –0.12), I2 = 79%, P = .01]. There was greater heterogeneity among the included studies: aerobic exercise (I2 = 80%, P < .001), traditional Chinese medicine methods (I2 = 90%, P < .001), and meditation (I2 = 79%, P < .001).
Conclusions:
This study revealed that the depression symptoms of college students can be effectively improved by aerobic exercise, traditional Chinese exercises, and meditation. Aerobic exercise would have a better effect on anxiety and stress while traditional Chinese exercise would have a better effect on stress. Further research (such as high-quality randomized controlled trials and long-term follow-up) is required to evaluate the effects of aerobic exercise, traditional Chinese exercise, and meditation on the depressive symptoms of college students to further apply complementary and alternative therapies.
Ethics and dissemination:
The results of the effects of aerobic exercise, traditional Chinese exercises, and meditation on depressive symptoms for a college student will be reported in a peer-reviewed publication. Hopefully, our findings from this meta-analysis can provide the most up-to-date evidence for the contribution to preventing the occurrence of depressive symptoms in college students.
Keywords: college students, depressive symptoms, exercise, meditation, traditional Chinese exercises
1. Introduction
The depressive symptom is a relatively common and harmful mental health disease in colleges and universities, affecting 17.3 to 34.5% of European and American college students, making it difficult for them to achieve self-worth in personal education, social communication, and career development.[1–4] It is worth noting that depression emotion can make these students feel desperate[5] and unwilling to seek outside help;[6] resulting in easily delaying the disease treatment and even suicidal behavior.[7] Therefore, it is of extreme importance to find acceptive and effective interventions that can improve mental health problems such as depression in college students.
Although antidepressant medication is classified as a first-level recommendation, there are still many problems such as drug resistance and side effects.[8] More and more researchers focus on non-drug treatments. The exercise was classified as first-level in the 2016 edition of the Canadian Clinical Guidelines for Emotional and Anxiety Therapy. Meditation and traditional Chinese exercises were classified as secondary-level.[9–12]
Aerobic exercise, traditional Chinese exercises, and meditation have been applied to the treatment of depression. Aerobic exercise is the physical movement of the skeletal muscles, which causes energy expenditure to exceed resting levels and is related to physical health, life satisfaction, and mental health.[13,14] Traditional Chinese exercises are part of low to moderate-intensity aerobic exercises, such as tai chi, Baduanjin, qigong, and other mind-body therapy.[15–17] It guides movements through ideas and cooperates with abdominal breathing; since its exercise intensity is low and medium, the heart rate does not rise suddenly during exercise. Meditation is considered to emphasize mindfulness,[18] concentration, and self-transcendence, focusing more on the improvement of the spiritual realm instead of just the improvement of the body.[19] However, whether exercise, meditation, and traditional Chinese exercises can improve the physical and psychological health of college students with depressive symptoms remains unknown.
Although many studies of Randomized Controlled Trials evaluated the effects of aerobic exercise, traditional Chinese exercises, and meditation, there were no randomized controlled trials comparing aerobic exercise, traditional Chinese exercises, and meditation. The way to overcome this limitation is to compare the effects of different interventions using a meta-analysis method to provide evidence-based evidence. Therefore, meta-analysis is used in this study to compare 3 intervention methods of aerobic exercise, traditional Chinese exercise, and meditation, as well as their respective intervention effects on college students’ depressive symptoms.
2. Methods
A meta-analysis and systematic review were conducted following the general principles outlined in the Centre for Reviews and Dissemination Guidance and the PRISMA statement. A meta-analysis and systematic review conducted in 2018 are reported in this paper, which is available on the PROSPERO website by CRD42018087104.
2.1. Literature search
A range of resources was searched for published and unpublished studies, grey literature, and on-going research. We did a meta-analysis and systematic review. We searched the PubMed, EMBASE, MEDLINE, Web of Science (science and social science citation index), The Cochrane Library (Cochrane Database of Systematic Reviews), Cochrane Central Register of Controlled Trials (CENTRAL), China Biology Medicine disc, and CINAHL (EBSCO) from the date of their inception to Sep 15, 2019, with English and Chinese. We used a combination of relevant free-text terms, synonyms, and Medical Subject Headings to search: Students, Depression, Aerobic Exercise, Traditional Chinese exercises, and meditation. Bibliographies of relevant reviews, materials, and guidelines were also checked, and Internet information searches were made of websites relating to depression. It is worth noting that in the search process, Aerobic Exercise, Traditional Chinese exercises, and meditation are used as the search direction.
2.2. Included criteria
This study only included clinical randomized controlled trials; the subjects were college students with depressive symptoms or diagnosed with depression; interventions included at least one of the following treatments: aerobic exercise, traditional Chinese exercise, and meditation (or other treatments Combination); research outcome assessment should include depression (or anxiety, stress, and other psychological related indicators).
Two reviewers independently screened all abstracts and full papers, with disagreements resolved by discussion, or a third reviewer. Eligible treatments include Aerobic Exercise, Traditional Chinese exercises, and meditation. We selected control conditions, such as pharmacological interventions, treatment as usual, and no intervention were considered, as well as active comparators, in which 2 different interventions have been compared within the same studies. Students (including college students or undergraduate students or graduate students) with depressive symptom were assessed by depression scale (such as Beck Depression Inventory , Profile of Mood States Profile of Mood States, and Center for Epidemiologic Studies Depression Scale, etc.).
2.3. Exclusion criteria
The exclusion criteria are provided as follows: Non-randomized trials, case reports, case series, reviews, qualitative studies, observational studies, meta-analyses, ecological studies, conference proceedings, letters, comments, and policy papers. Results for different doses/regimens of the same type of treatment within a study were pooled. Only were the final values used in an initial analysis. However, more studies were included by calculating final values for trials reporting change from baseline data, and trial baseline data with variance estimates were also reported (Table 1).
Table 1.
Research characteristics table.
| Author/Years | Study design | Number analysed at end of treatment (N) | Population characters | Country | Duration | Classification | Main Outcome(s) | Sceond Outcome(s) |
| Carole L. Bandy, et al 2019 | Pilot study | 67 (33/34) | PTSD in South African University Students (DSM-IV for diagnosis) experimental group age 20.6 ± 2.75 yrs comparison group age 21.1 ± 1.55 yrs | USA | 105 d (15 wk) | Transcendental Meditation Practice | Beck Depression Inventory | none |
| Yu Chen, et al 2013 | RCT | 60 (30/30) | Chinese nursing students age 19.5 ± 0.87 years | China | 7 d (1 wk) | Brief mindfulness meditation | SDS | The Chinese version of the Self-Rating Anxiety Scale (SAS) |
| Yune Sik Kang, et al 2009 | RCT | 41 (21/20) | Juniors and seniors Nursing students Experimental group age 22.69 ± 1.49 yrs Control group age 22.25 ± 0.86 years | Korea | 8 wk | Stress coping program based on mindfulness meditation | Beck Depression Inventory | The state trait anxiety inventory (STAI) |
| R. GINA SILVERSTEIN, et al 2011 | RCT | 28 (12/16) | Undergraduates age 20 ± 1.0 yrs | USA | 12 wk | Meditation | Brief Symptom Inventor (BSI) | none |
| Ke-Ping Yang et al 2009 | Pilot study | 242 (119/123) | College Students All participants were female and 19 to 20 yrs of age | China, Taiwan | 18 wk | Meditation | Life Adaptation Scale (LAS) | none |
| Sanford I. Nidich et al 2009 | RCT | 207(93/114) | College Students TM age 25.4 ± 9.2 yrs Control age 26.2 ± 9.9 years | USA | 3 mo (12 wk) | Transcendental Meditation | Profile of Mood States | none |
2.4. Observation indicators
Symptoms of depression (as a primary or secondary outcome) in university/college students were assessed as the main observation indicators in our study. Besides, the secondary observation indicators (specific indicators directly related to depression symptoms) included in the literature (such as anxiety and stress) were analyzed.
2.5. Assessment of trial quality and data extraction
We assessed the studies’ risk of bias in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (For the Cochrane Handbook for Systematic Reviews of Interventions, please refer to the website of http://handbook-5-1.cochrane.org/). Additionally, 2 investigators (ZL and JS) independently selected the studies, reviewed the main reports and supplementary materials, extracted the relevant information from the included trials, and assessed the risk of bias. Data extraction and quality assessments were performed by one reviewer and independently checked by a second. Disagreements were resolved by discussion or a third reviewer.
2.6. Synthesis and analysis
Meta-analysis was performed using RevMan 5.3 software. A Chi-squared test is used to determine whether there is statistical heterogeneity between the results of the study. If P ≥ .1, I2 < 50%, it can be considered that multiple similar studies are homogenous, and a fixed-effect model is used for meta-analysis; if P < .1, I2 ≥ 50%, but with clinical homogeneity, the random-effects model was selected. For continuous data, different measurement tools are used for the same variable, the statistic is analyzed using standardized mean difference (SMD).
Meta-regression and Publication bias of standards-compliant data using Stata15 software to find heterogeneity.
2.7. Subgroup analysis and meta-regression
Subgroup analysis and meta-regression were performed according to the following variables (training duration, control group, depression scales, published nation, published years, and sample sizes).
3. Results
A total of 11520 articles were retrieved on database search. Through reviewing the abstract and the full text, 7273 of them were eliminated for various reasons. Afterward, 368 articles were excluded and 44 articles were included through the full-text review of the remaining 412 articles (Fig. 1).
Figure 1.
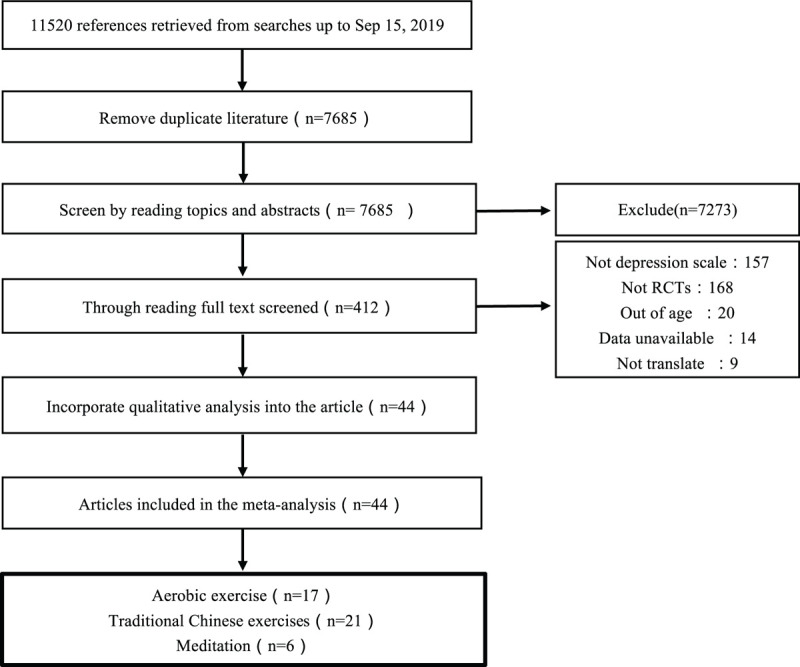
PRISMA flow chart. This is a PRISMA flow chart of this study, which details the selection of articles in this study. In the end, 44 articles were included.
3.1. Quality assessment and quality of the evidence
To evaluate the risk levels included in this study, among them, 28 trials were found to have a high or ambiguous bias risk in generating random sequences, 7 trials were found to have concealed treatment allocation, 9 trials were found to have blinded participants, 7 trials investigators were found to have been blinded, 7 trials participants and investigators were found to have been blinded, and the completeness of the results of the 3 trials. Except for depression scale score change, no evidence of small study effects based on funnel plot asymmetry was observed, even though the number of studies recruited in each comparison was relatively small (Appendix. 1). According to the grading of recommendations, assessment, developmental, and evaluations (GRADE) performed on the articles, the quality of the 38 studies is classified as poor quality, the remaining 4 research is classified as general quality in the meta-analysis, and only 2 research is considered to have a low risk of bias, limiting the effectiveness of the randomization and leads to the baseline imbalance; besides, differences in interventions hinder the presentation of complete research quality assessment results, and the quality of evidence is stronger in some areas than in other areas (Appendix. 2).
3.2. Effects of aerobic exercise, traditional Chinese exercises, and meditation on university students with depressive symptoms
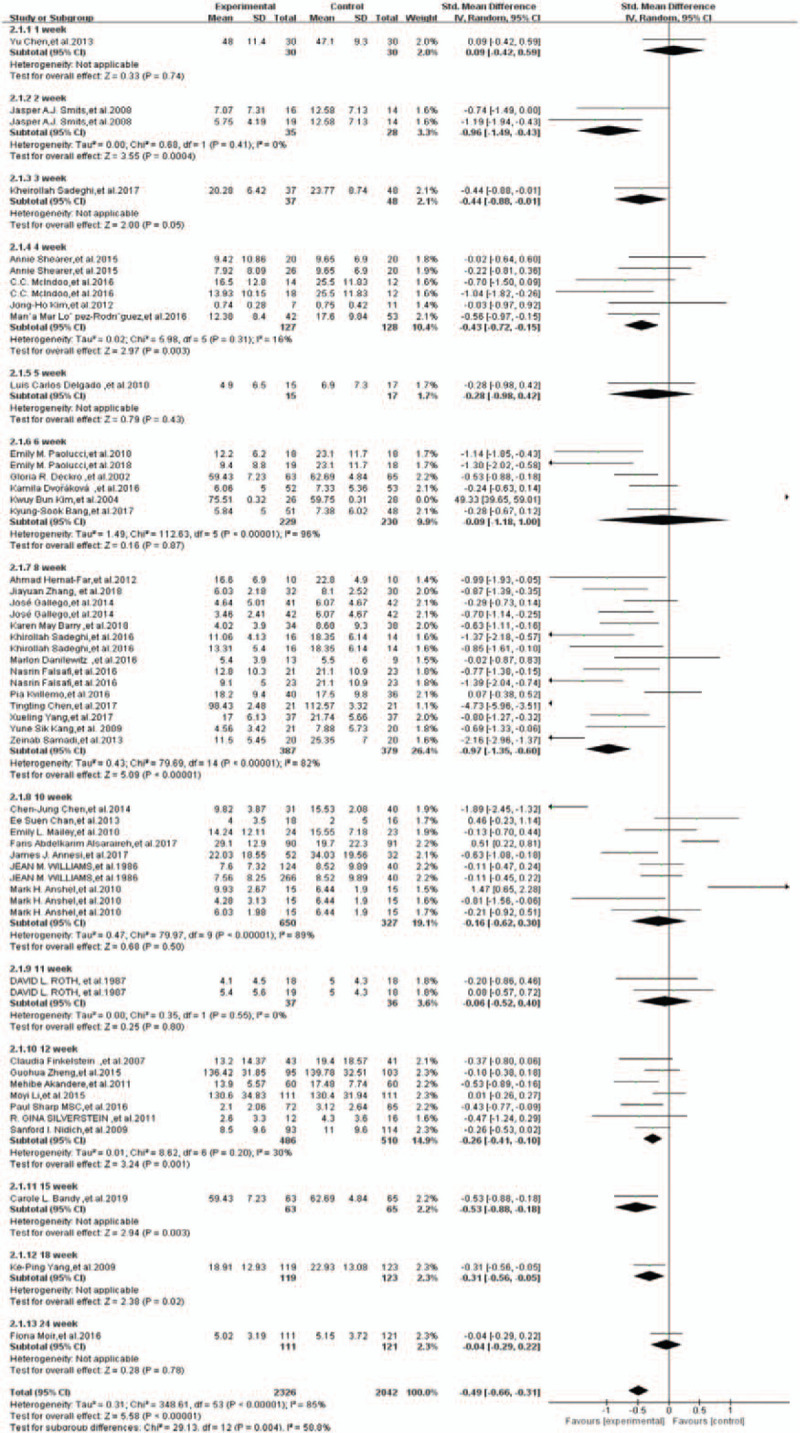
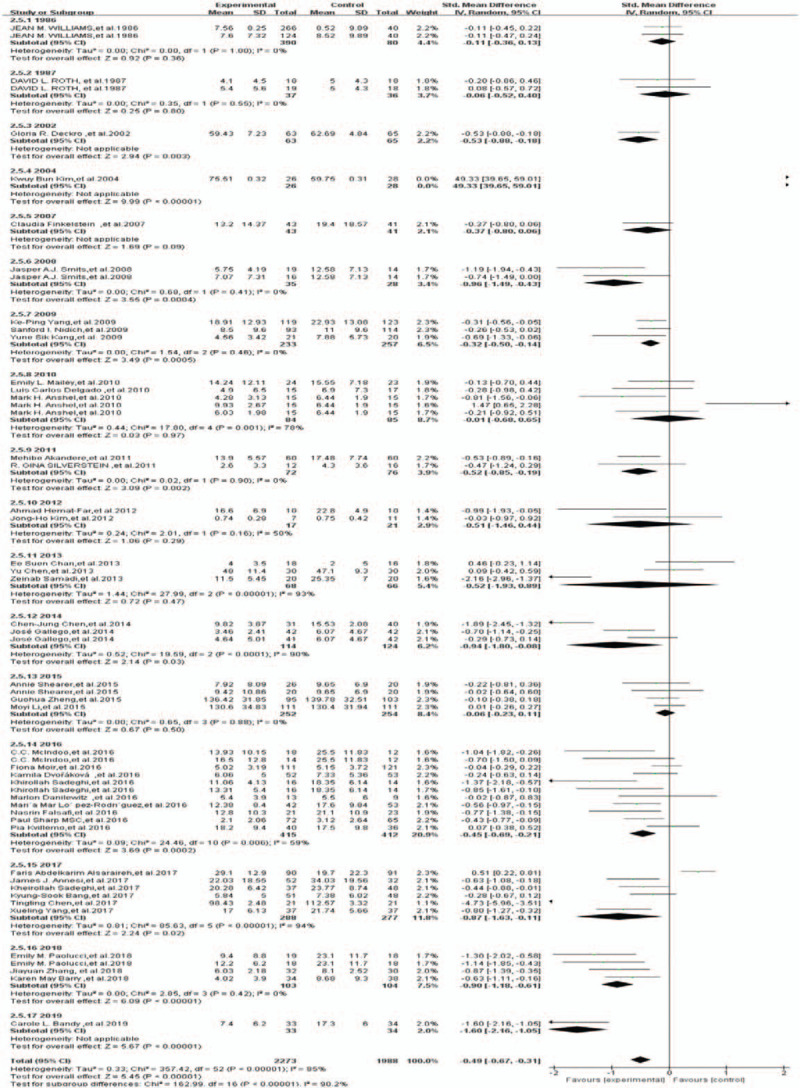
In this study, 17 researches reported aerobic exercise, 21 traditional Chinese exercises, and 6 meditation. Considering outcomes for depressive symptoms, the mean effect size for aerobic exercise SMD was: -0.53, 95%CI[-0.77,-0.30], I2 = 80%; P < .001; the mean effect size for traditional Chinese exercises SMD was:-0.42, 95%CI[-0.74,-0.10], I2 = 90%, P < .01; the mean effect size for meditation SMD was:-0.51, 95%CI[-0.90,-0.12], I2 = 79%, P < .01. The forest plot for intervention effects on depressive symptoms is provided in Fig. 2.
Figure 2.
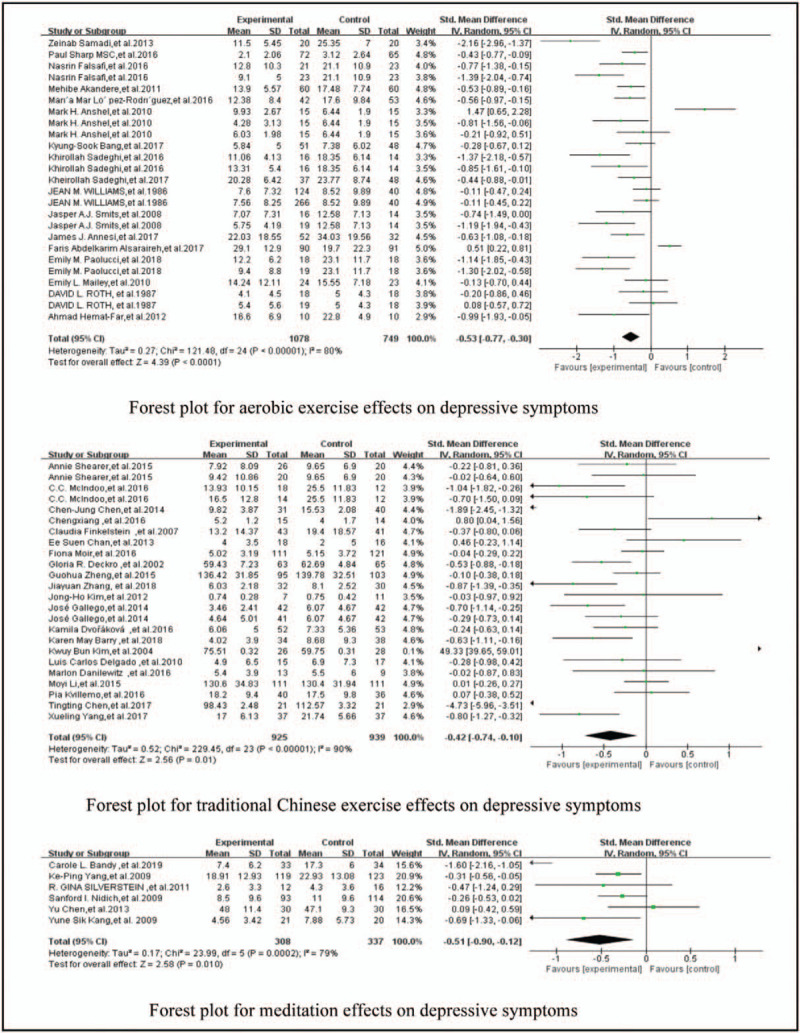
Forest plot for intervention effects on depressive symptoms. In this study, 17 researches reported aerobic exercise, 21 traditional Chinese exercises, and 6 meditation. Considering outcomes for depressive symptoms, the test overall effect for aerobic exercise: SMD:−0.53, 95%CI[−0.77,−0.30], P < .001, I2 = 80%; Traditional Chinese exercises: SMD:−0.42, 95%CI[−0.74,−0.10], P = .01, I2 = 90%; and meditation: SMD:−0.51, 95%CI[−0.90,−0.12],P = .01), I2 = 79%.
3.3. Effects of aerobic exercise, traditional Chinese exercises, and meditation on university students with anxiety and stress
It can be revealed through the analysis of random effect model that the effect of aerobic exercise on anxiety is: [SMD = –0.50, 95% CI (–0.77, –0.23), I2 = 36%, P = .0003]; the effect of traditional Chinese exercise on anxiety is: [SMD = –0.03, 95% CI (–0.57, 0.51), I2 = 90%, P = .92]: the effect of meditation on anxiety is: [SMD = –0.15, 95% CI (–0.71, 0.41), I2 = 41%, P = .60]: the effect of aerobic exercise on stress is: [SMD = –5.38, 95% CI (–8.04, –2.73), I2 = 0%, P < .0001]; and the effect of traditional Chinese exercise on stress is: [SMD = – 0.78, 95% CI (–1.52, –0.04), I2 = 62%, P = .04]; besides, there are no secondary outcomes of stress involved in the included meditation studies. The forest plot for intervention effects on anxiety and the forest plot for intervention effects on stress are presented in Fig. 3 and Fig. 4, respectively.
Figure 3.
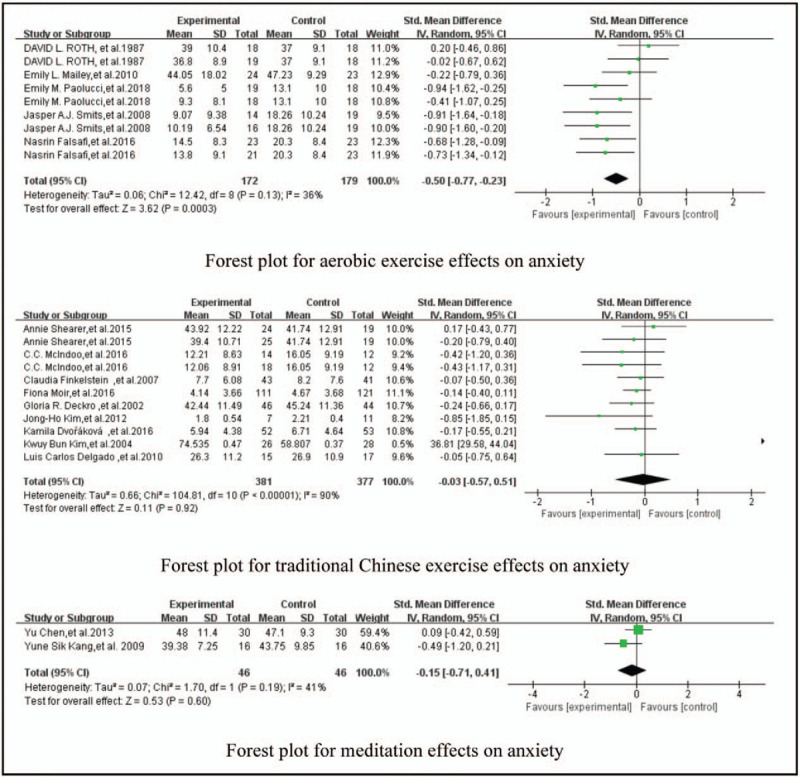
Forest plot for intervention effects on anxiety. Through the analysis of random effect model, it is found that the effect of aerobic exercise on anxiety [SMD:−0.50, 95%CI (−0.77,−0.23), P = .0003, I2 = 36%], the effect of traditional Chinese exercise on anxiety [SMD:−0.03, 95%CI(−0.57,0.51), P = .92, I2 = 90%], the effect of meditation on anxiety [SMD:−0.15, 95%CI(−0.71,0.41), P = .60, I2 = 41%].
Figure 4.
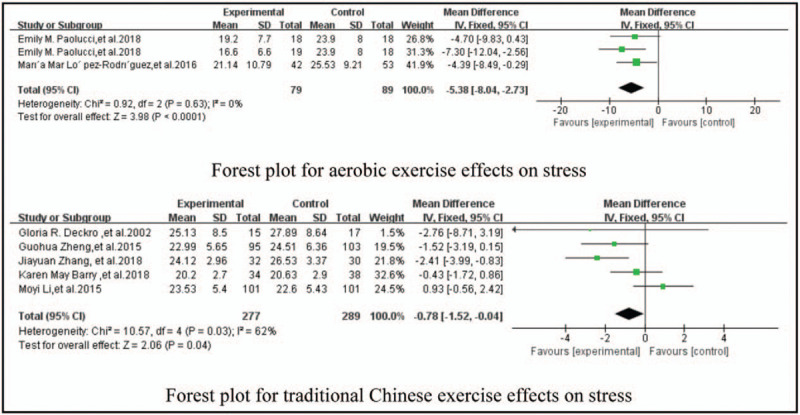
Forest plot for intervention effects on stress. Through the analysis of random effect model, it is found that the effect of aerobic exercise on stress [SMD:−5.38, 95%CI(−8.04,−2.73), P < .0001, I2 = 0%], the effect of traditional Chinese exercise on stress [SMD:−0.78, 95%CI(−1.52,−0.04), P = .04, I2 = 62%], and there are no secondary outcomes of stress involved in the included meditation studies.
3.4. Subgroup analysis
Subgroup: intervention duration
It can be observed that 2 , 4 , 8 , 12 , 15 , and 18 weeks were statistically significant through the subgroup analysis of the training duration. It was indicated after combining the effect values [SMD = –0.49, 95%CI (–0.66, –0.31), I2 = 58.8%, P < .001] that the intervention duration is one of the factors of heterogeneity in this study. There was no statistical difference in the subgroup difference test (I2 = 74.4%, P = .004) (Fig. 5).
Figure 5.
Forest plot for subgroup analysis of training time. By subgroup analysis of the training duration, 2 weeks [Z = 3.55, P = .0004], 4 weeks [Z = 2.97, P = .003], 8 weeks [Z = 5.09, P<.001], 12 weeks [Z = 3.24, P = .001], 15 weeks [Z = 2.94, P = .003], 18 weeks [Z = 2.38, P = .02] were statistically significant. After combining the effect values [SMD = –0.49, 95%CI(–0.66, –0.31), P = .004, I2 = 85%], indicating that the intervention duration is one of the factors of heterogeneity in this study.
Subgroup: control group
As demonstrated from the results acquired using the control group as a control variable for the subgroup analysis, the routine activity group, the waiting list group, and the positive control group were all significant. It was indicated after combining the effect values [SMD = 9.86, 95%CI (9.72,9.99), I2 = 100%, P < .001] that the control group is one of the factors of heterogeneity in this study. There was no statistical difference in the subgroup difference test (I2 = 100%, P<.001) (Fig. 6).
Figure 6.
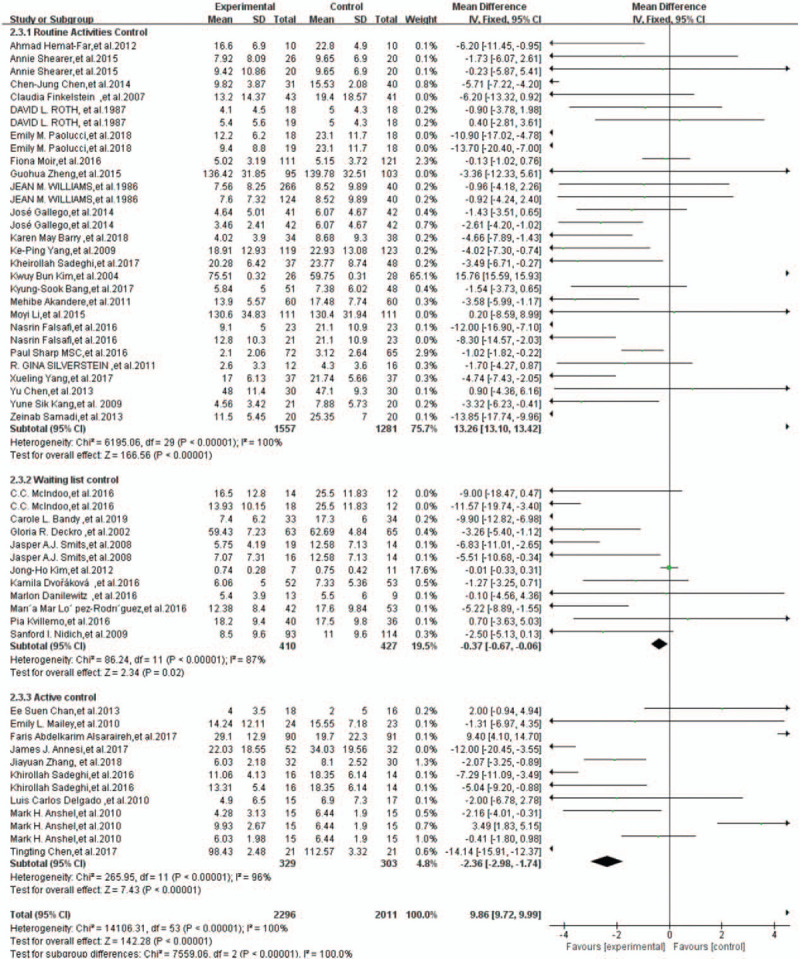
Forest plot for subgroup analysis of control group. Using the control group as a control variable for the subgroup analysis, it was found that the routine activity group [Z = 166.56, P<.001], the waiting list group [Z = 2.34, P = .02], and the positive control group [Z = 7.43, P<.001] were all significant. After combining the effect values [SMD = 9.86, 95%CI(9.72,9.99), P < .001, I2 = 100%], indicating that the control group is one of the factors of heterogeneity in this study.
Subgroup: depression scale
As illustrated from the results obtained using different depression scales as control variables for subgroup analysis, Beck Depression Inventory, 28-item General Health Questionnaire, 12-item General Health Questionnaire, Depression Status Inventory, Life Adaptation Scale, and Depression Mood Self-Report Inventory for Adolescence were all significant. It was indicated after combining the effect values [SMD = -0.49, 95%CI (-0.67, -0.32), I2 = 85%, P<.001] that the depression scale is one of the factors of heterogeneity in this study. There was no statistical difference in the subgroup difference test (I2 = 92.7%, P<.001) (Fig. 7).
Figure 7.
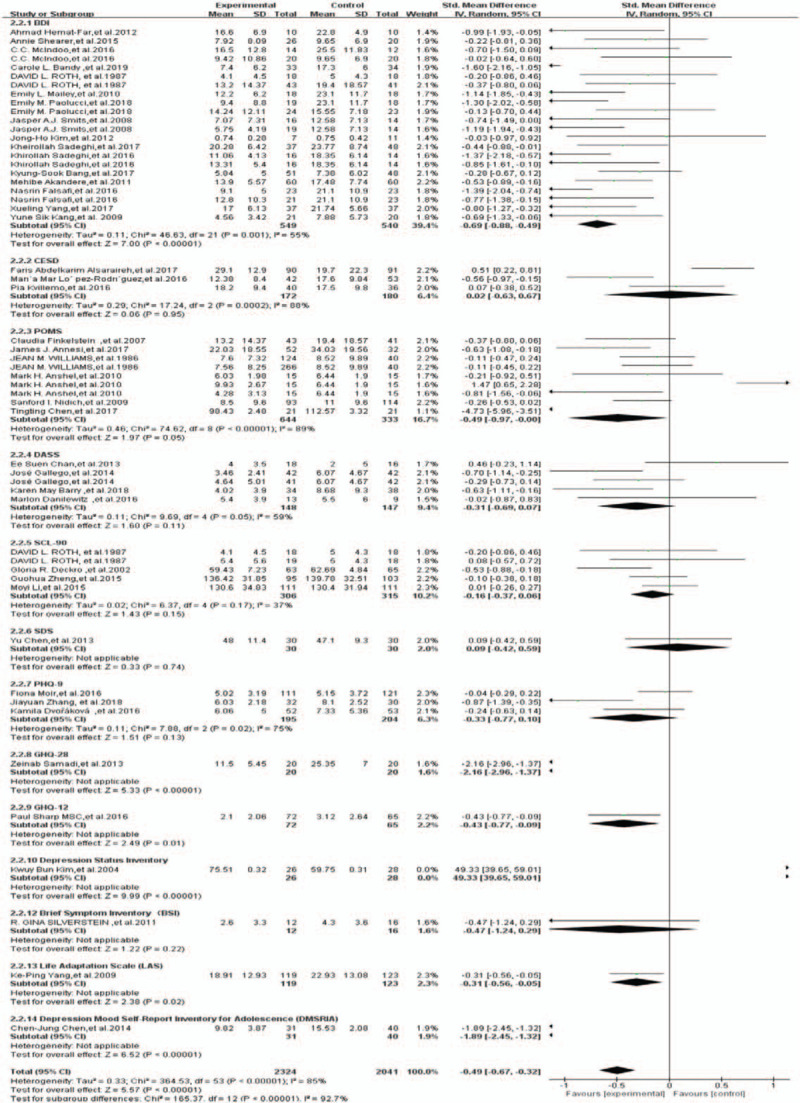
Forest plot for subgroup analysis of depression scale. Using different depression scales as control variables for subgroup analysis, the results showed that BDI [Z = 7.00, P<.001], GHQ-28 [Z = 5.33, P < .001], GHQ-12 [Z = 2.49, P = .02], DSI [Z = 9.99, P < .001], LAS [Z = 2.38, P = .02], DMSRIA [Z = 6.52, P<.001] were significant. After combining the effect values [SMD = −0.49, 95%CI (−0.67, −0.32), P<.001, I2 = 85%], indicating that the depression scale is one of the factors of heterogeneity in this study.
Subgroup: published nation
The results obtained using the different published nations as control variables for subgroup analysis demonstrated that the USA, China, Canada, Spain, Iran, Jordan, Turkey, and Korea were significant. It was indicated after combining the effect values [SMD = -0.51, 95%CI (-0.68, -0.33), I2 = 86%, P < .001] that the published nation is one of the factors of heterogeneity in this study. There was no statistical difference in the subgroup difference test (I2 = 83.7%, P<.001) (Fig. 8).
Figure 8.
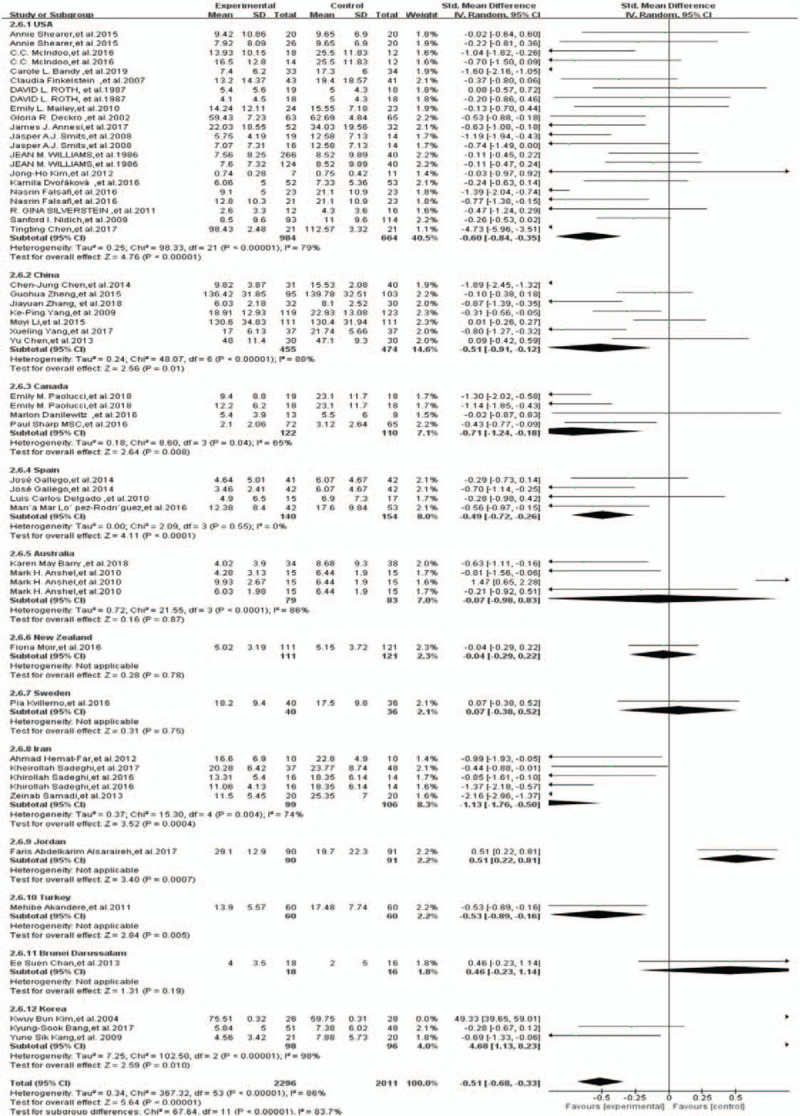
Forest plot for subgroup analysis of country. Using different published nation as control variables for subgroup analysis, the results showed that USA [Z = 4.76, P<.001], China [Z = 2.56, P = .01], Canada [Z = 2.64, P = .008], Spain [Z = 4.11, P<.001], Iran [Z = 3.52, P = .0004], Jordan [Z = 3.40, P = .0007], Turkey [Z = 2.84, P = .005], Korea [Z = 2.59, P = .01] were significant. After combining the effect values [SMD = −0.51, 95%CI (−0.68, −0.33), P < .001, I2 = 86%], indicating that the Published nation is one of the factors of heterogeneity in this study.
Subgroup: published years
The results acquired using different published years as control variables for subgroup analysis suggested that 2002, 2004, 2008, 2009, 2011, 2014, 2016, 2017, 2018, and 2019 were significant. It was indicated after combining the effect values [SMD = -0.49, 95%CI (-0.67, -0.31), I2 = 85%, P<.001] that the published years is one of the factors of heterogeneity in this study. There was no statistical difference in the subgroup difference test (I2 = 90.2%, P<.001) (Fig. 9).
Figure 9.
Forest plot for subgroup analysis of published years. Using different published years as control variables for subgroup analysis, the results showed that 2002 [Z = 2.94, P = .003], 2004 [Z = 9.99, P<<.001], 2008 [Z = 3.55, P = .0004)], 2009 [Z = 3.49, P = .0005], 2011 [Z = 3.09, P = .002], 2014 [Z = 2.14, P = .03], 2016 [Z = 3.69, P = .0002], 2017 [Z = 2.24, P = .02], 2018 [Z = 6.09, P<.0001], 2019 [Z = 5.67, P<.0001] were significant. After combining the effect values [SMD = −0.49, 95%CI (−0.67, −0.31), P<.001, I2 = 85%], indicating that the published years is one of the factors of heterogeneity in this study.
Subgroup: sample sizes
The results obtained using different sample sizes as control variables for subgroup analysis demonstrated that >30, >50, and >100 were significant. It was indicated after combining the effect values [SMD = -0.49, 95%CI (-0.67, -0.31), I2 = 86%, P = .03] that the sample sizes is one of the factors of heterogeneity in this study. There was no statistical difference in the subgroup difference test (I2 = 65.9%, P = .03) (Fig. 10).
Figure 10.
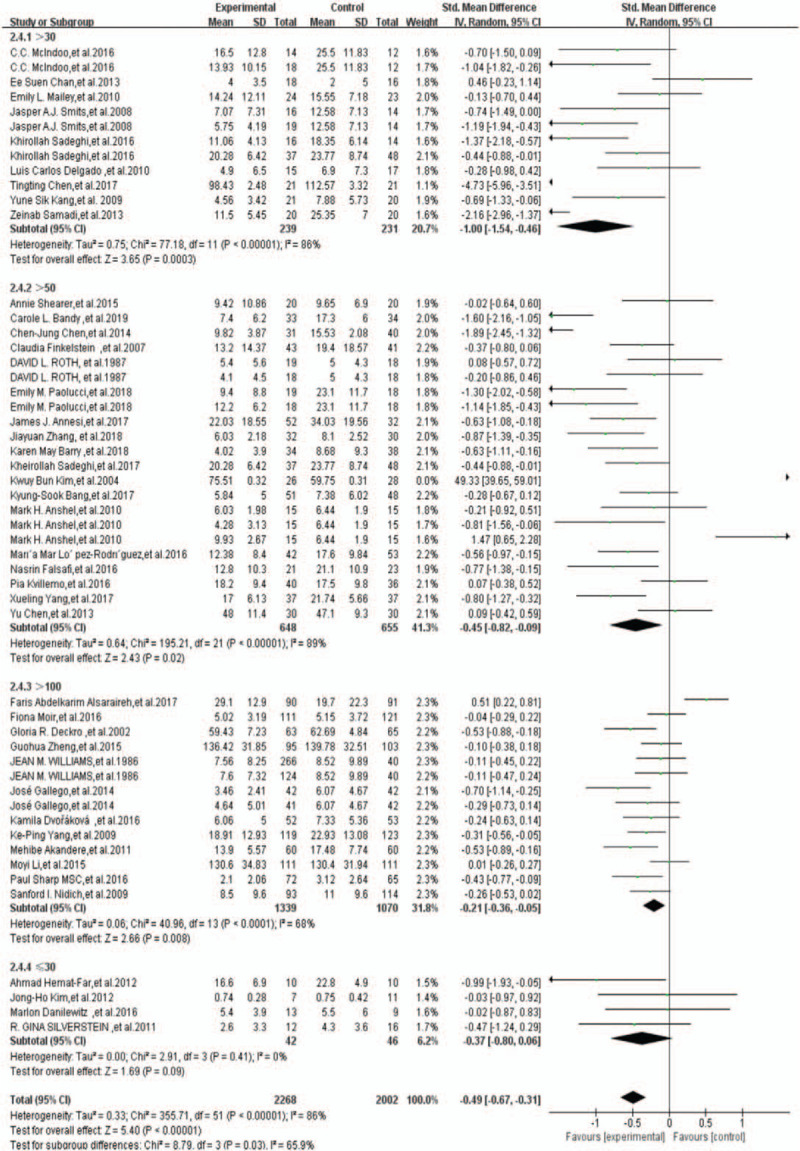
Forest plot for subgroup analysis of sample sizes. Using different sample sizes as control variables for subgroup analysis, the results showed that >30 [Z = 3.65, P = .0003], >50 [Z = 2.43, P = .02], >100 [Z = 2.66, P = .008], were significant. After combining the effect values [SMD = −0.49, 95%CI (−0.67, −0.31), P = .03, I2 = 86%], indicating that the sample sizes is one of the factors of heterogeneity in this study.
3.5. Meta-regression analyses
Meta-regression analysis of covariates was performed using the depression scale, training duration, country, years, control group, and sample size as covariates. The meta-regression results reveal that the regression values of the depression scale, training duration, and control group can explain 11.11% heterogeneity of the study, the publication country, and sample size can explain 8.33% heterogeneity, and the publication years can explain 5.55% heterogeneity (Table 2).
Table 2.
Meta regression data.
| Covariates | Tau2 | 95%CI | P |
| depression scale | 0.40 | (−1.118, −0.154) | .469 |
| publication country | 0.39 | (−0.474,0.164) | .273 |
| training duration | 0.40 | (−0.063,0.101) | .647 |
| publication years | 0.38 | (−0.125,0.025) | .185 |
| control group | 0.40 | (−0.606,0.260) | .427 |
| sample size | 0.33 | (−0.089, 0.665) | .132 |
3.6. Publication bias
The publication bias of this study used the Stata 15 software for data processing, and the data in the literature was represented by SMD; the intervention group SMD, the control group SMD and the intervention group number, and the control group number were input. Besides, the Begg method was used for analysis; continuous correction z = 0.73; continuous correction P = .468 > .05; thus, the publication bias is not statistically significant (Fig. 11).
Figure 11.
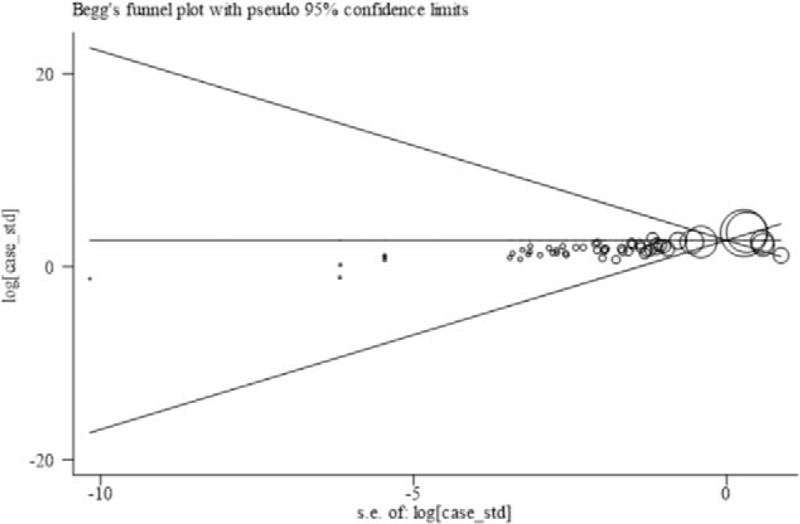
Funnel plot of publishing bias. The publication bias of this study used the Stata 15 software for data processing, the data in the literature was represented by SMD, the intervention group SMD, the control group SMD and the intervention group number, the control group number were input, and the Begg method was used for analysis, continuous correction z = 0.73, continuous correction P = .468 > 0.05, indicating that the publication bias is not statistically significant.
4. Discussion
The combined effect value of SMD indicates that aerobic exercise, traditional Chinese exercise, and meditation can all improve the depression symptoms of college students. From early intervention to early prevention, early exercise decompression, meditation, and mutual communication can be used to prevent college students from developing depression, contributing to the incidence of depression. However, the effectiveness of individual studies has been limited by factors such as the quality of the literature and the difficulty of achieving double-blind design through sports intervention.
Recent studies have demonstrated that aerobic exercise can be used as a psychological intervention to improve mental health. Besides, regular aerobic exercise is helpful for mental health. It is mainly manifested in the ability to reduce negative reactions (such as anxiety and depression) and increase positive reactions (such as improving self-esteem, and energy) to achieve mood improvement.[20] Aerobic exercise is an effective treatment for depression and may also be a treatment assisting antidepressants.[13] Moderate-intensity aerobic exercise is more effective in major depressive disorder. Exercise has a significant effect on improving the situation of patients with depression.[21]
Traditional Chinese exercises focus on the interaction between body and mind. Traditional Chinese exercises such as Tai Chi and Baduanjin use the mind to affect body functions and can directly improve human health, belonging to the category of mind-body therapy.[22] Traditional Chinese exercises are very popular in complementary and alternative therapies, including various philosophical concepts (such as Buddhism, Confucianism, and Taoism)[23] that combine physical, emotional, spiritual, and behavioral elements through gentle movements and breathing. They are considered to be a diverse and complex means of mind-body intervention.[24–26] When trainers practice, they can relax, increase their concentration and self-awareness, improve self-efficacy, and ultimately improve the symptoms of depression. Moreover, traditional Chinese exercises can reduce the negative emotions of depression, resulting in a reduction in pain and negative emotions, with a significant effect on alleviating depression. This suggests that traditional Chinese exercises can be considered to be another option for treating depression. According to the research by Breedvelt et al, effective and reasonable early intervention may reduce the incidence of depression in young people, and traditional Chinese exercise, such as Tai Chi, can be the first choice for college students.[27,28] The results of Marko et al verify that Tai Chi can alleviate the stress response in subjects.[16] This could be the achieved effects of Tai Chi in promoting physical and mental health and also applicable for stress and emotional management in college students.
Meditation originated from Eastern Buddhist meditation and has become an important method of psychotherapy. Meditation training tries to help patients accept the environment and the facts that are happening (including the state of the disease and the environment) in a peaceful manner and get rid of their anxiety and depression by encouraging them to focus on the present and not making subjective judgments on the status quo.[29,30] Meditation focuses on breathing. During the training process, individuals adjust internal and external stress, improve the patient's stress state, enhance the patient's self-control, and enter a relaxed state to improve the effect of depression.[31] Meditation affects the central nervous system and mental state and can effectively reduce stress and promote physical and mental health.[32–34] Meditation can promote relief of multiple negative psychological emotions and stress,[18] reduce depression, anxiety, and stress, and improve participants’ quality of life.[35]
Another finding of this study, a meta-analysis of secondary outcome indicators, found that aerobic exercise had better effects on anxiety and stress while traditional Chinese exercise therapy had better effects on stress. Aerobic exercise has been used as a first-line treatment for mild to moderate depression, with a better effect compared to antidepressants; besides, exercise as an adjunct to medicine has also been verified to improve depression symptoms.[36] Among them, the effect of aerobic exercise on anxiety or stress management has been demonstrated in studies, and exercise can effectively improve anxiety or stress-related anxiety symptoms.[37] Compared with normal healthy participants, exercise is more beneficial to patients. Especially for the effect of exercise on anxiety, exercise has a positive effect on mental illnesses such as anxiety and depression.[38] Additionally, psychological stress promotes the production of corticotropin-releasing hormone and catecholamines in the human body, resulting in interfering with the microbiome. During stress, changes in gut microbes could affect the regulation of neurotransmitters mediated by microbes and gut function;[39] meanwhile, traditional Chinese exercise uses the interaction between thought, body, behavior, and environment to correct the body and mental dysfunction, contributing to better physical and mental health.[40] Another finding of this study may provide a scientific idea, and different intervention methods focus on different emotional problems. This conclusion may be controversial due to the limitations of the articles included in this study (such as the quality of the included articles) while this may also provide a new idea for future research.
College students are in the transition period from high school to university. Due to changes in learning pressure,[41] social communication,[42] and living environment,[43] college students must quickly adapt to the pressure and burden brought by academic competition and social life, leading to psychological stress among college students and even depression.[44,45] If psychological counseling for college students is not conducted in time, it might result in slight anxiety, insomnia, low grades, or severe cases of drug abuse, violence, or even suicidal tendency.[4] Moreover, long-term depression symptoms turn into a depressed state of mind, causing a decline in subjective well-being and poor interpersonal relationships and work efficiency.[46] Aerobic exercise or traditional Chinese exercise such as jogging and Tai Chi, as a daily exercise for college students, are easy to be popularized and applied in colleges and can be used as an effective intervention to prevent depression in college students. Therefore, the active promotion of traditional Chinese exercise, aerobic exercise or meditation, and other related courses and regular practice in colleges can play a positive role in promoting and improving mental health in depressed college students and target early interventions for college students with high stress to avoid depression.
There are a few limitations to this study. First, the participants in all the included studies are college students. Thus, the application of these findings to other people in the same age group would be limited, such as young people with high stress and young women of childbearing age. Second, the follow-up duration of all the literature cited in this study is deficient. Therefore, the long-term effects of various intervention methods could not be determined. Long-term observation and follow-up of subjects should be conducted in further research. Finally, many depression scales serving as outcomes may lead to a certain degree of selection bias due to the relatively low quality of the included randomized controlled trials, the relatively simple of the choice of interventions, and the comparability of the scale data before and after the intervention. Consequently, the quality control standard of clinical trials should be based on evidence-based medical standards in the future.
5. Conclusion
Aerobic exercise, traditional Chinese exercises, and meditation are effective interventions to improve depressive symptoms in college students and are easy to be promoted and applied in universities. Specifically, aerobic exercise may have a better effect on anxiety and stress while traditional Chinese exercise may have a better effect on stress. However, the quality of most research evidence in this area of research is relatively low. Therefore, high-quality randomized controlled clinical studies will be conducted on the effects of aerobic exercise, traditional Chinese exercises, and meditation on college students’ depressive symptoms in the future.
Author contributions
JSW, JT conceived of the idea, designed the study protocol. JS, ZZL drafted the manuscript. JS, ZZL, JT participated in the revision of the manuscript of the study.
Conceptualization: Jing-song Wu, Jing Tao.
Data curation: Jian Song, Jia Huang.
Formal analysis: Zhi-zhen Liu.
Funding acquisition: Jing-song Wu.
Methodology: Jing Tao.
Software: Zhi-zhen Liu.
Supervision: Jing Tao.
Writing – original draft: Jian Song, Zhi-zhen Liu.
Writing – review & editing: Zhi-zhen Liu, Jia Huang, Jing-song Wu, Jing Tao.
Supplementary Material
Footnotes
Abbreviation: SMD = Standard Mean Difference.
How to cite this article: Song J, Liu Zz, Huang J, Wu Js, Tao J. Effects of aerobic exercise, traditional Chinese exercises, and meditation on depressive symptoms of college student: a meta-analysis of randomized controlled trials. Medicine. 2021;100:1(e23819).
JS is the first author.
This trial was funded by the National Natural Science Foundation of China (Number 81804164).
The funder played no role in the design of the reviews, data collection, meta-analysis and in writing of the manuscript.
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Supplemental digital content is available for this article.
This is the research characteristics table of this study, which records the research characteristics of this research included in this study in detail.
Table description: Meta-regression analysis of covariates was performed using the depression scale, training duration, country, years, control group and sample size as covariates. The meta-regression results show that the regression values of the depression scale, training duration and control group can explain 11.11% heterogeneity of the study, the publication country and sample size can explain 8.33% heterogeneity, and the publication years can explain 5.55% Heterogeneity.
References
- [1].Boehm MA, Lei QM, Lloyd RM, et al. Depression, anxiety, and tobacco use: overlapping impediments to sleep in a national sample of college students. J Am Coll Health 2016;64:565–74. [DOI] [PubMed] [Google Scholar]
- [2].Macaskill A. The mental health of university students in the United Kingdom. Brit J Guid Couns 2013;41:426–41. [Google Scholar]
- [3].Zivin K, Eisenberg D, Gollust SE, et al. Persistence of mental health problems and needs in a college student population. J Affect Disord 2009;117:180–5. [DOI] [PubMed] [Google Scholar]
- [4].Acharya L, Jin L, Collins W. College life is stressful today – Emerging stressors and depressive symptoms in college students[J]. Journal of American college health 2018;66:655–64. [DOI] [PubMed] [Google Scholar]
- [5].Garlow SJ, Rosenberg J, Moore JD, et al. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress Anxiety 2008;25:482–8. [DOI] [PubMed] [Google Scholar]
- [6].Sidana S, Kishore J, Ghosh V, et al. Prevalence of depression in students of a medical college in New Delhi: a cross-sectional study. Australas Med J 2012;5:247–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chang EC, Chang OD, Lucas AG, et al. Depression, loneliness, and suicide risk among latino college students: A test of a psychosocial interaction model. Soc Work (New York) 2019;64:51–60. [DOI] [PubMed] [Google Scholar]
- [8].Celentano DD, Aramrattana A, Sutcliffe CG, et al. Associations of substance abuse and sexual risks with self-reported depressive symptoms in young adults in northern Thailand. J Addict Med 2008;2:66–73. [DOI] [PubMed] [Google Scholar]
- [9].Ravindran AV, Balneaves LG, Faulkner G, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 5. Compl Alt Med Treat 2016;61:576–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Parikh SV, Quilty LC, Ravitz P, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 2. Psychological treatments. Can J Psychiatry 2016;61:524–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kvam S, Kleppe CL, Nordhus IH, et al. Exercise as a treatment for depression: A meta-analysis. Journal of affective disorders 2016;202:67–86. [DOI] [PubMed] [Google Scholar]
- [12].Solomon D, Adams J. The use of complementary and alternative medicine in adults with depressive disorders. A critical integrative review. J Affect Disord 2015;179:101–13. [DOI] [PubMed] [Google Scholar]
- [13].Kvam S, Kleppe CL, Nordhus IH, et al. Exercise as a treatment for depression: a meta-analysis. J Affect Disord 2016;202:67–86. [DOI] [PubMed] [Google Scholar]
- [14].Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med 2011;41:15–28. [DOI] [PubMed] [Google Scholar]
- [15].Bo A, Mao W, Lindsey MA. Effects of mind-body interventions on depressive symptoms among older Chinese adults: a systematic review and meta-analysis. Int J Geriatr Psychiatry 2017;32:509–21. [DOI] [PubMed] [Google Scholar]
- [16].Nedeljkovic M, Ausfeld-Hafter B, Streitberger K, et al. Taiji practice attenuates psychobiological stress reactivity - a randomized controlled trial in healthy subjects. Psychoneuroendocrino 2012;37:1171–80. [DOI] [PubMed] [Google Scholar]
- [17].Wang C, Chan CHY, Ho RTH, et al. Managing stress and anxiety through qigong exercise in healthy adults: A systematic review and meta-analysis of randomized controlled trials. BMC Complement Altern Med 2014;14:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med 2014;174:357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Breedvelt JJF, Amanvermez Y, Harrer M, et al. The effects of meditation, yoga, and mindfulness on depression, anxiety, and stress in tertiary education students: a Meta-Analysis. Front Psychiatry 2019;10:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Mikkelsen K, Stojanovska L, Polenakovic M, et al. Exercise and mental health. Maturitas 2017;106:48–56. [DOI] [PubMed] [Google Scholar]
- [21].Schuch FB, Vancampfort D, Richards J, et al. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res 2016;77:42–51. [DOI] [PubMed] [Google Scholar]
- [22].Huston P, McFarlane B. Health benefits of tai chi: what is the evidence? Can Fam Physician 2016;62:881–90. [PMC free article] [PubMed] [Google Scholar]
- [23].Alperson SY. Tai Chi philosophy and nursing epistemology. ANS Adv Nurs Sci 2008;31:E1–5. [DOI] [PubMed] [Google Scholar]
- [24].Wang X, Huang L, Liu Y, et al. Effects of tai chi program on neuromuscular function for patients with knee osteoarthritis: study protocol for a randomized controlled trial. Trials 2013;14:375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Zheng G, Huang M, Liu F, et al. Tai chi chuan for the primary prevention of stroke in middle-aged and elderly adults: a systematic review. Evid Based Complement Alternat Med 2015;2015:742118–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hempel S, Taylor SL, Solloway MR, et al. Evidence map of tai chi. Washington (DC): Department of Veterans Affairs (US); 2014. [PubMed] [Google Scholar]
- [27].Breedvelt J, Kandola A, Kousoulis AA, et al. What are the effects of preventative interventions on major depressive disorder (MDD) in young adults? A systematic review and meta-analysis of randomized controlled trials. J Affect Disord 2018;239:18–29. [DOI] [PubMed] [Google Scholar]
- [28].Cramer H, Anheyer D, Lauche R, et al. A systematic review of yoga for major depressive disorder. J Affect Disord 2017;213:70–7. [DOI] [PubMed] [Google Scholar]
- [29].Brewer JA, Garrison KA. The posterior cingulate cortex as a plausible mechanistic target of meditation: findings from neuroimaging. Ann N Y Acad Sci 2014;1307:19–27. [DOI] [PubMed] [Google Scholar]
- [30].Boccia M, Piccardi L, Guariglia P, et al. The meditative mind: A comprehensive Meta-Analysis of MRI studies. Biomed Res Int 2015;2015:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Tang YY, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci 2015;16:213–25. [DOI] [PubMed] [Google Scholar]
- [32].Robins CJ, Keng SL, Ekblad AG, et al. Effects of mindfulness-based stress reduction on emotional experience and expression: a randomized controlled trial. J Clin Psychol 2012;68:117–31. [DOI] [PubMed] [Google Scholar]
- [33].Ding X, Tang Y, Tang R, et al. Improving creativity performance by short-term meditation. Behav Brain Funct 2014;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Tang YY, Ma Y, Wang J, et al. Short-term meditation training improves attention and self-regulation. Proc Natl Acad Sci U S A 2007;104:17152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Khoury B, Knauper B, Schlosser M, et al. Effectiveness of traditional meditation retreats: a systematic review and meta-analysis. J Psychosom Res 2017;92:16–25. [DOI] [PubMed] [Google Scholar]
- [36].Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiat Med 2011;41:15–28. [DOI] [PubMed] [Google Scholar]
- [37].Stubbs B, Vancampfort D, Rosenbaum S, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: a meta-analysis. Psychiat Res 2017;249:102–8. [DOI] [PubMed] [Google Scholar]
- [38].Wegner M, Helmich I, Machado S, et al. Effects of exercise on anxiety and depression disorders: review of meta- analyses and neurobiological mechanisms[J]. CNS Neurol Disord-Dr 2014;13:1002–14. [DOI] [PubMed] [Google Scholar]
- [39].Househam AM, Peterson CT, Chopra D. The effects of stress and meditation on the immune system, human microbiota, and epigenetics. Advances in mind-body medicine 2017;31:10–25. [PubMed] [Google Scholar]
- [40].Esch T, Kream RM, Stefano GB. Chromosomal processes in Mind-Body medicine: chronic stress, cell aging, and telomere length[J]. Med Sci Monitor 2018;24:134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Beiter R, Nash R, McCrady M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disorders 2015;173:90–6. [DOI] [PubMed] [Google Scholar]
- [42].van den Brink RHS, Schutter N, Hanssen DJC, et al. Prognostic significance of social network, social support and loneliness for course of major depressive disorder in adulthood and old age. Epidemiol Psych Sci 2018;27:266–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Rautio N, Filatova S, Lehtiniemi H, et al. Living environment and its relationship to depressive mood: a systematic review. Int J Soc Psychiatry 2017;64:92–103. [DOI] [PubMed] [Google Scholar]
- [44].Yang L, Zhao Y, Wang Y, et al. The Effects of Psychological Stress on Depression[J]. Curr Neuropharmacol 2015;13:494–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiat Res 2017;255:186–94. [DOI] [PubMed] [Google Scholar]
- [46].Ibrahim AK, Kelly SJ, Adams CE, et al. A systematic review of studies of depression prevalence in university students. J Psychiatr Res 2013;47:391–400. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


