Abstract
Introduction
The American Board of Internal Medicine (ABIM) requires that trainees receive procedural training for certification; however, Internal Medicine (IM) residents perform a variable number of procedures throughout residency training. This results in differences in confidence levels as well as procedural competence. For active-duty military trainees, this is especially problematic, as these procedural skills are often required during deployment soon after residency graduation. This deficit can be improved through standardized simulation-based training.
Methods
All internal medicine residents at our institution were invited to participate in a standardized simulation-based training program for core internal medicine procedures (lumbar puncture, arterial line, central line, thoracentesis, paracentesis, and arthrocentesis). Residents were asked to qualitatively rate their perceived procedural confidence using a Likert scale ranging from 1 (not at all confident) to 5 (extremely confident) in their ability to independently perform core internal medicine procedures prior to the simulation exercise. Experienced senior residents and internal medicine faculty instructed and supervised each resident as they performed the procedures. Following the simulation exercise, the residents repeated the survey and were asked to report whether or not they found the exercise useful.
Results
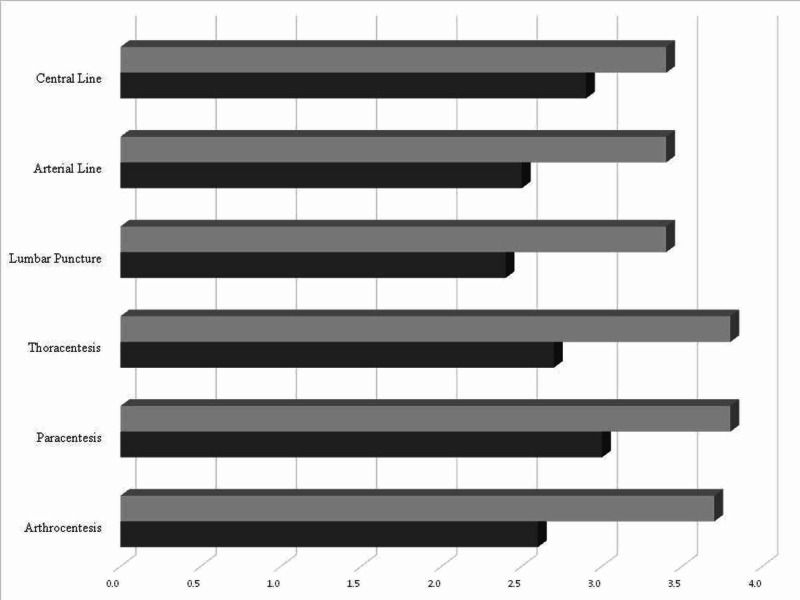
Of the 96 residents invited to participate, 49 completed the pre-simulation questionnaire and 36 completed the post-simulation questionnaire. The cumulative mean Likert scale confidence rating for all procedures showed a statistically significant improvement post-simulation as compared to pre-simulation, including lumbar puncture (2.45±1.1 vs. 3.42±0.87, p<0.05), arterial line (2.48±1.06 vs. 3.39±1.04, p < 0.05), central line (2.86±1.08 vs. 3.5±1.02, p < 0.05), thoracentesis (2.67±1.10 vs. 3.64±0.83, p < 0.05), paracentesis (3.1±1.08 vs. 3.82±0.74, p < 0.05), and arthrocentesis (2.56±1.07 vs. 3.67±0.80, p < 0.05). All (36/36) trainees reported that they perceived the simulation exercise as valuable.
Conclusion
Internal medicine residents across all post-graduate year (PGY) levels at our institution lacked confidence to independently perform core internal medicine procedures. Utilizing simulation-based medical education as an adjunct to clinical training is well accepted by internal medicine trainees, and resulted in significantly improved procedural confidence. This intervention was well received by trainees and could feasibly be replicated at other active-duty military internal medicine residency programs to assist with readiness. Research is currently in progress to correlate in-situ competency and evaluate clinical outcomes of this improved confidence.
Keywords: simulation education, military medicine, procedural competency
Introduction
The American Board of Internal Medicine (ABIM) requires that Internal Medicine (IM) residents receive procedural training; however, residents are not mandated to perform all procedures, and only general competence is required [1]. This has led to significant heterogeneity in the procedural skills training that IM residents receive with a consistent emphasis on experiential learning, particularly the “see one, do one, teach one” model [2-4]. However, reported clinical procedural experience has been demonstrated to be an unreliable proxy for procedural skill [5]. Additionally, due to this variability in clinical experience and in the training received during residency, levels of confidence and competence in performing common bedside procedures differ greatly among trainees [6].
This lack of standardized training experience directly impacts patient outcomes due to the invasive nature of these procedures and the associated risk for complications [7-9]. Additionally, for active-duty military IM residents, the lack of procedural confidence is of particular concern because IM specialists and subspecialists often deploy as intensivists with the expectation to maintain procedural competence for deployment readiness per the Air Force’s Comprehensive Medical Readiness Program (CMRP) as well as the Army’s Individual Critical Task List (ICTL).
In order to address these deficits, high-fidelity simulation-based mastery learning (SBML) has been identified as a way to standardize procedural experience and produce measurable quality outcomes [10,11]. SBML has been utilized to improve outcomes in multiple facets of medical training, including communication skills and ultrasound techniques [12,13]. Furthermore, SBML has been used to improve training in advanced cardiac life support (ACLS) due to perceived trainee discomfort and reported deficits [14,15]. Given the success with high-fidelity SBML in these areas of medical training, this teaching technique has been incorporated into procedural training to address these deficits. Significant improvements have been demonstrated in procedural competence and confidence among trainees by using SBML to learn multiple procedures, including central line placement, lumbar puncture, paracentesis, thoracentesis, and arthrocentesis in the civilian sector [16-20]. Given the requirement for procedural competence placed upon active-duty internists, and the emphasis on the use of simulation to augment clinical skills, we explored the utility of simulation in improving perceived procedural confidence in active-duty IM residents.
Due to the demonstrated benefits of high-fidelity simulation and deliberate practice in teaching procedural skill, efforts have been made to use SBML to instruct trainees in core internal medicine procedures [21,22]. However, there remains no standardized, simulation-based curriculum utilized across Internal Medicine residency training programs within the military healthcare system. We report the results of the adoption of a simulation-based medical education curriculum for core IM invasive bedside procedures and its implementation at a single IM residency program for active-duty military resident physicians.
Materials and methods
All IM residents in post-graduate year (PGY) 1-3 at Brooke Army Medical Center in San Antonio, Texas, were invited to participate in the simulated training course. The course included multiple two-hour sessions that were conducted over two separate days with each session including three of six procedural skills: lumbar puncture, arterial line, central line, thoracentesis, paracentesis and arthrocentesis. Participants were divided into small groups comprised of two or three residents that rotated through each skill station. Experienced senior residents and IM faculty instructed and supervised each resident as they performed the procedures. Skills education and training were performed on a combination of high-fidelity SimMan3G mannequins (Laerdal), CentraLineMan system (Simulab), and Ultrasound ArteriaLine Trainer (Simulab).
Prior to the simulation sessions, the participants completed a questionnaire with non-identifiable demographic information, consent, and perceived procedural confidence level using a Likert scale with 1 correlating with (not at all confident), 2 (not so confident), 3 (somewhat confident), 4 (very confident), 5 (extremely confident) in their ability to independently perform core internal medicine procedures. Following the simulation session, the participants repeated the same questionnaire with an additional question about the overall perceived utility of the skills course. Data from the pre- and post-test survey were compared using Kruskal-Wallis tests with statistical significance set at p < 0.05.
Results
Of the 96 residents invited to participate, 49 completed the pre-simulation questionnaire and 36 completed the post-simulation questionnaire. The group was comprised of 26%, 33% and 41% of residents from the PGY1, PGY2 and PGY3 classes, respectively. All procedures showed a statistically significant improvement post-simulation as compared to pre-simulation, including lumbar puncture (2.45±1.1 vs. 3.42±0.87, p < 0.05), arterial line (2.48±1.06 vs. 3.39±1.04, p < 0.05), central line (2.86±1.08 vs. 3.5±1.02, p < 0.05), thoracentesis (2.67±1.10 vs. 3.64±0.83, p < 0.05), paracentesis (3.1±1.08 vs. 3.82±0.74, p < 0.05), and arthrocentesis (2.56±1.07 vs. 3.67±0.80, p < 0.05). All (36/36) trainees reported that they perceived the simulation exercise as valuable on the post-simulation questionnaire (Table 1; Figure 1).
Table 1. Comparison of self-reported confidence by Likert scale among residents, by PGY year for each individual core invasive procedure.
PGY, post-graduate year; SD, standard deviation
| Pre-Simulation | Post-Simulation | |||||||||||||
| 1 | 2 | 3 | 4 | 5 | Average±SD | 1 | 2 | 3 | 4 | 5 | Average±SD | p-value | ||
| Central Line | 5 | 14 | 16 | 11 | 3 | 2.86 ± 1.08 | 1 | 5 | 15 | 9 | 6 | 3.5 ± 1.02 | 0.030 | |
| PGY1 | 5 | 5 | 1 | 2 | 0 | 1.62 ± 1.08 | 1 | 5 | 2 | 3 | 1 | 3.17 ± 1.19 | ||
| PGY2 | 0 | 4 | 10 | 1 | 1 | 2.94 ± 0.19 | 0 | 0 | 7 | 2 | 1 | 3.4 ± 0.7 | ||
| PGY3 | 0 | 5 | 5 | 8 | 2 | 3.35 ± 0.99 | 0 | 0 | 6 | 4 | 4 | 3.86 ± 0.86 | ||
| Arterial Line | 9 | 17 | 15 | 6 | 2 | 2.48 ± 1.06 | 1 | 5 | 16 | 7 | 7 | 3.39 ± 1.04 | <0.001 | |
| PGY1 | 5 | 7 | 1 | 0 | 0 | 1.69 ± 0.63 | 1 | 3 | 4 | 2 | 2 | 2.64 ± 1.24 | ||
| PGY2 | 2 | 7 | 5 | 1 | 1 | 2.5 ± 1.03 | 0 | 0 | 7 | 2 | 1 | 3.4 ± 0.69 | ||
| PGY3 | 2 | 3 | 9 | 5 | 1 | 3 ± 1.03 | 0 | 2 | 5 | 3 | 4 | 3.64 ± 1.08 | ||
| Lumbar Puncture | 13 | 9 | 21 | 4 | 2 | 2.45 ± 1.1 | 0 | 4 | 18 | 9 | 5 | 3.42 ± 0.87 | <0.001 | |
| PGY1 | 6 | 1 | 6 | 0 | 0 | 2 ± 1 | 0 | 3 | 3 | 5 | 1 | 3.33 ± 0.98 | ||
| PGY2 | 4 | 3 | 8 | 0 | 1 | 2.44 ± 1.09 | 0 | 1 | 6 | 2 | 1 | 3.3 ± 0.82 | ||
| PGY3 | 3 | 5 | 7 | 4 | 1 | 2.75 ± 1.12 | 0 | 0 | 9 | 2 | 3 | 3.57 ± 0.85 | ||
| Thoracentesis | 7 | 17 | 17 | 8 | 3 | 2.67 ± 1.1 | 0 | 1 | 20 | 18 | 6 | 3.64 ± 0.83 | 0.002 | |
| PGY1 | 4 | 10 | 5 | 0 | 0 | 2.05 ± 1.17 | 0 | 1 | 9 | 4 | 1 | 3.33 ± 0.91 | ||
| PGY2 | 2 | 1 | 9 | 2 | 0 | 2.79 ± 0.91 | 0 | 0 | 5 | 9 | 1 | 3.73 ± 0.74 | ||
| PGY3 | 1 | 6 | 3 | 6 | 3 | 3.21 ± 0.9 | 0 | 0 | 6 | 5 | 4 | 3.87 ± 0.85 | ||
| Paracentesis | 4 | 12 | 15 | 17 | 4 | 3.1 ± 1.08 | 0 | 1 | 17 | 16 | 11 | 3.82 ± 0.74 | <0.001 | |
| PGY1 | 4 | 6 | 5 | 3 | 1 | 2.53 ± 0.71 | 0 | 1 | 7 | 4 | 3 | 3.6 ± 0.72 | ||
| PGY2 | 0 | 3 | 5 | 5 | 1 | 3.29 ± 0.89 | 0 | 0 | 5 | 7 | 3 | 3.87 ± 0.59 | ||
| PGY3 | 0 | 3 | 5 | 9 | 2 | 3.53 ± 1.23 | 0 | 0 | 5 | 5 | 5 | 4 ± 0.83 | ||
| Arthrocentesis | 9 | 15 | 17 | 7 | 2 | 2.56 ± 1.07 | 0 | 2 | 18 | 18 | 7 | 3.67 ± 0.8 | <0.001 | |
| PGY1 | 7 | 7 | 4 | 0 | 1 | 2 ± 1.05 | 0 | 2 | 6 | 4 | 3 | 3.53 ± 0.99 | ||
| PGY2 | 2 | 3 | 7 | 2 | 0 | 2.64 ± 0.93 | 0 | 0 | 6 | 9 | 0 | 3.6 ± 0.51 | ||
| PGY3 | 0 | 5 | 6 | 5 | 1 | 3.18 ± 0.93 | 0 | 0 | 6 | 5 | 4 | 3.87 ± 0.83 | ||
Figure 1. Mean self-reported confidence among residents for each individual core procedure.
Darker color represents the mean confidence rating prior to the simulation, with the lighter color representing after the simulation
Discussion
Despite evidence that high-fidelity simulation is an effective, well-received tool for procedural training as well as skills maintenance, a standardized simulation curriculum does not currently exist for training active duty IM residents in core procedures [23,24]. Our study adds to the growing body of evidence that supports the use of high-fidelity simulation and deliberate practice in a structured learning environment to improve trainee procedural confidence. Use of this model has previously been used most commonly to instruct trainees in individual procedures; however, our study demonstrates the feasibility of developing and implementing a curriculum for all core IM procedures. The course has subsequently become a sustainable adjunct to the curriculum at our institution and is held on an annual basis.
An important finding of our study was that significant improvement in procedural confidence was demonstrated consistently for each PGY level, including residents that had completed most of their training. This supports findings of previous studies demonstrating that deliberate practice in a controlled environment is a useful adjunct to procedural learning regardless of experience in the clinical setting [14]. Utilizing simulation-based procedural training as part of a standardized curriculum is of particular importance for military IM residents, as these procedures are often necessary during deployment soon after completion of residency. Consistent implementation of a curriculum such as ours could be useful in mitigating self-identified lack of procedural confidence among trainees [4-6].
Though our simulation curriculum demonstrates a practical model that could be replicated at other training programs, one potential limitation is the resources required. In order to implement this study, we used high-fidelity simulation mannequins from the simulation center at our institution, which may not be available at other institutions. The curriculum also involved supervision by IM faculty, which required approximately two hours of time volunteered for each session. The small-group training model with a high instructor-to-learner ratio was well-received by our residents; however, coordination of these resources may be an obstacle to course implementation at other institutions. This study was additionally limited by the relatively small sample size at a single institution and did not include a validation process for each procedural skill; however, this is a current goal for further study.
These limitations do not lessen the effect of the standardized curriculum on perceived confidence with bedside procedural skills; however, self-assessment does not always directly result in improved clinical performance [25,26]. Further research is needed to determine whether performance of all simulated core IM procedures translates to the clinical environment, including safety outcomes such as procedural complications and associated infections. Prior studies have demonstrated reduced rates of procedure-related complications through deliberate practice in a simulated environment [27-29]. However, these outcomes have primarily been studied in central venous catheter insertion and further outcomes research is needed for many of the other core IM procedures. Lastly, additional studies are needed to determine if deliberate practice during residency improves procedural confidence and competence among active-duty staff IM physicians in the pre-deployment setting.
Conclusions
Internal medicine residents across all post-graduate year levels at our institution lacked confidence to independently perform core internal medicine procedures. Utilizing simulation-based medical education as an adjunct to clinical training is well accepted by internal medicine trainees, and resulted in significantly improved procedural confidence across all post-graduate levels. This intervention was well received by trainees and could feasibly be replicated at other active-duty military internal medicine residency programs to assist with readiness. Research is currently in progress to correlate in-situ competency and evaluate clinical outcomes of this improved confidence.
Acknowledgments
The views expressed are solely those of the authors and do not reflect the official policy or position of the U.S. Army, U.S. Air Force, the Department of Defense or the U.S. Government.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.American Board of Internal Medicine. Internal medicine policies. [Sep;2020 ];https://www.abim.org/~/media/ABIM%20Public/Files/pdf/publications/certification-guides/policies-and-procedures.pdf 2020
- 2.Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Acad Med. 2011;86:706–711. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beyond “see one, do one, teach one”: toward a different training paradigm. Rodriguez-Paz JM, Kennedy M, Salas E, Wu AW, Sexton JB, Hunt EA, Pronovost PJ. BMJ Qual Saf. 2009;18:63–68. doi: 10.1136/qshc.2007.023903. [DOI] [PubMed] [Google Scholar]
- 4.Core competencies or a competent core? A scoping review and realist synthesis of invasive bedside procedural skills training in internal medicine. Brydges R, Stroud L, Wong BM, Holmboe ES, Imrie K, Hatala R. Acad Med. 2017;92:1632–1643. doi: 10.1097/ACM.0000000000001726. [DOI] [PubMed] [Google Scholar]
- 5.Residents' procedural experience does not ensure competence: a research synthesis. Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. J Grad Med Educ. 2017;9:201–208. doi: 10.4300/JGME-D-16-00426.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beyond the comfort zone: residents assess their comfort performing inpatient medical procedures. Huang GC, Smith CC, Gordon CE, Feller-Kopman DJ, Davis RB, Phillips RS, Weingart SN. Am J Med. 2006;119:71. doi: 10.1016/j.amjmed.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Central line proficiency test outcomes after simulation training versus traditional training to competence. Alsaad AA, Bhide VY, Moss JL Jr, Silvers SM, Johnson MM, Maniaci MJ. Ann Am Thorac Soc. 2017;14:550–554. doi: 10.1513/AnnalsATS.201612-987OC. [DOI] [PubMed] [Google Scholar]
- 8.Training using simulation in internal medicine residencies: an educational perspective. Flannery MT, Villarreal KF. Am J Med Sci. 2015;349:276–278. doi: 10.1097/MAJ.0000000000000406. [DOI] [PubMed] [Google Scholar]
- 9.Reliability and validity of a simulation-based acute care skills assessment for medical students and residents. Boulet JR, Murray D, Kras J, Woodhouse J, McAllister J, Ziv A. Anesthesiology. 2003;99:1270–1280. doi: 10.1097/00000542-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Clinical simulation: importance to the internal medicine educational mission. Ogden PE, Cobbs LS, Howell MR, Sibbitt SJ, DiPette DJ. Am J Med. 2007;120:820–824. doi: 10.1016/j.amjmed.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Impact of a simulation-based communication workshop on resident preparedness for end-of-life communication in the intensive care unit. Markin A, Cabrera-Fernandez DF, Bajoka RM, et al. Crit Care Res Pract. 2015;2015:534879. doi: 10.1155/2015/534879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teaching medical error disclosure to residents using patient-centered simulation training. Sukalich S, Elliott JO, Ruffner G. Acad Med. 2014;89:136–143. doi: 10.1097/ACM.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 13.Not Just Hocus POCUS: Implementation of a Point of Care Ultrasound Curriculum for Internal Medicine Trainees at a Large Residency Program. Mellor TE, Junga Z, Ordway S, et al. Mil Med. 2019;184:901–906. doi: 10.1093/milmed/usz124. [DOI] [PubMed] [Google Scholar]
- 14.Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Chest. 2008;133:56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- 15.Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Hayes CW, Rhee A, Detsky ME, Leblanc VR, Wax RS. Crit Care Med. 2007;35:1668–1672. doi: 10.1097/01.CCM.0000268059.42429.39. [DOI] [PubMed] [Google Scholar]
- 16.Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Barsuk JH, McGaghie WC, Cohen ER, O'Leary KJ, Wayne DB. Crit Care Med. 2009;37:2697–2701. [PubMed] [Google Scholar]
- 17.Simulation-based education with mastery learning improves residents' lumbar puncture skills. Barsuk JH, Cohen ER, Caprio T, McGaghie WC, Simuni T, Wayne DB. Neurology. 2012;79:132–137. doi: 10.1212/WNL.0b013e31825dd39d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simulation-based education with mastery learning improves paracentesis skills. Barsuk JH, Cohen ER, Vozenilek JA, O'Connor LM, McGaghie WC, Wayne DB. J Grad Med Educ. 2012;4:23–27. doi: 10.4300/JGME-D-11-00161.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mastery learning of thoracentesis skills by internal medicine residents using simulation technology and deliberate practice. Wayne DB, Barsuk JH, O'Leary KJ, Fudala MJ, McGaghie WC. J Hosp Med. 2008;3:48–54. doi: 10.1002/jhm.268. [DOI] [PubMed] [Google Scholar]
- 20.Hybrid simulation for knee arthrocentesis: improving fidelity in procedures training. Stroud L, Cavalcanti RB. J Gen Intern Med. 2013;28:723–727. doi: 10.1007/s11606-012-2314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.How we implemented a resident-led medical simulation curriculum in a large internal medicine residency program. Mathai SK, Miloslavsky EM, Contreras-Valdes FM, Milosh-Zinkus T, Hayden EM, Gordon JA, Currier PF. Med Teach. 2014;36:279–283. doi: 10.3109/0142159X.2013.875619. [DOI] [PubMed] [Google Scholar]
- 22.A 5-day intensive curriculum for interns utilizing simulation and active-learning techniques: addressing domains important across internal medicine practice. Dversdal RK, Gold JA, Richards MH, et al. BMC Res Notes. 2018;11:916. doi: 10.1186/s13104-018-4011-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Use of simulator-based medical procedural curriculum: the learner's perspectives. Shanks D, Wong RY, Roberts JM, Nair P, Ma IW. BMC Med Educ. 2010;10:77. doi: 10.1186/1472-6920-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. McGaghie WC, Siddall VJ, Mazmanian PE, Myers J. Chest. 2009;135:62–68. doi: 10.1378/chest.08-2521. [DOI] [PubMed] [Google Scholar]
- 25.The use of simulation in emergency medicine: a research agenda. Bond WF, Lammers RL, Spillane LL, et al. Acad Emerg Med. 2007;14:353–363. doi: 10.1197/j.aem.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 26.Graduating internal medicine residents’ self-assessment and performance of advanced cardiac life support skills. Wayne DB, Butter J, Siddall VJ, et al. Med Teach. 2006;28:365–369. doi: 10.1080/01421590600627821. [DOI] [PubMed] [Google Scholar]
- 27.Simulation-based education enhances patient safety behaviors during central venous catheter placement [ahead of print] Jagneaux T, Caffery TS, Musso MW, et al. J Patient Saf. 2020 doi: 10.1097/PTS.0000000000000425. [DOI] [PubMed] [Google Scholar]
- 28.Simulation training and its effect on long-term resident performance in central venous catheterization. Smith CC, Huang GC, Newman LR, et al. Simul Healthc. 2010;5:146–151. doi: 10.1097/SIH.0b013e3181dd9672. [DOI] [PubMed] [Google Scholar]
- 29.Short-term and long-term impact of the central line workshop on resident clinical performance during simulated central line placement. Laack TA, Dong Y, Goyal DG, Sadosty AT, Suri HS, Dunn WF. Simul Healthcare. 2014;9:228–233. doi: 10.1097/SIH.0000000000000015. [DOI] [PubMed] [Google Scholar]