Abstract
Background
Frailty was shown to be associated with psychosocial risk factors, but there are few longitudinal data.
Methods
We used data from waves 5 and 6 of the Survey of Health Aging Retirement in Europe (SHARE) to study the contribution of loneliness and social isolation to transitions towards frailty defined according to Fried criteria in a sample of 27,468 individuals aged ≥60.
Results
At baseline, there were 13,069 (47.6%) robust individuals, 11,430 (41.6%) pre-frail and 2,969 (10.8%) frail. After 2 years, among robust subjects at baseline, 8,706 (61.8%) were still robust, 4,033 (30.8%) were pre-frail and 330 (2.6%) were frail. Among those who were pre-frail, 1,504 (13.2%) progressed to frail and 3,557 (31.1%) became robust. Among frail people, 182 (6.1%) reversed to robust and 1,271 (42.8%) to pre-frail. Average and high levels of loneliness and social isolation were significantly associated with the risk of robust people becoming frail and pre-frail (except robust with high loneliness to become frail), and of pre-frail people to become frail (except with average loneliness). Reversion to robustness was inversely associated with high levels of loneliness.
Conclusion
Average levels of loneliness and social isolation should not be considered acceptable and should be actively addressed even in the absence of any health conditions through an available evidence-based intervention.
Keywords: frailty, loneliness, social isolation, older people, retirement
Key points
33.4% of European robust older individuals became pre-frail or frail after 2 years.
Average levels of loneliness or social isolation were reported by a quarter and two thirds of the population, respectively.
Average and high levels of loneliness and social isolation were associated with an increased risk of worsening frailty status.
High levels of loneliness prevented reversion in those who might otherwise improve their status.
Average loneliness and isolation should be tackled, although considered acceptable by professionals and even patients themselves.
Introduction
Frailty is a state of high vulnerability to the risk of adverse events when exposed to a stressor [1]. The frailty process occurs with the progression from robustness to functional decline [2] in a dynamic and relatively reversible process.
As for health conditions in general [3], social and psychological conditions, such as loneliness—the feeling of being alone—and social isolation—the number of social contacts and activities—have been found to be associated with frailty [4–7]. Such associations were investigated longitudinally using the Survey of Health, Ageing and Retirement in Europe (SHARE) database [8], but the roles of loneliness and social isolation per se were not investigated. We test the hypothesis that being socially isolated and feeling lonely are associated with an increased risk of becoming frail or pre-frail, and, vice versa, with a decreased probability of reversing the frailty status after 2 years in the European population.
Methods
The SHARE database comprises more than 120,000 individuals aged ≥50, accounting for more than 297,000 interviews across 27 European countries and Israel. Since 2004, data collections have taken place at 2–3 year intervals, accounting for seven survey waves. We use data from the fifth (2013) and sixth (2015) waves, as these were the most recent waves providing the information necessary for this analysis when we started the study. We retained people aged ≥60 years in the countries present in both surveys [9, 10], i.e. Sweden, Denmark, Austria, Germany, France, Switzerland, Belgium, Luxembourg, Czech Republic, Slovenia, Spain, Italy and Israel.
Frailty and pre-frailty were defined according to the five criteria of the Fried phenotype [11] (Supplementary Appendix 1 available in Age and Ageing online). However, the operationalization of these dimensions had to be adapted to the SHARE dataset [12, 13] as in other studies based on SHARE [13–15] (Supplementary Appendix 2 available in Age and Ageing online).
Participants completed the three-item version of the Revised UCLA Loneliness Scale [16]. Scores range from 3 to 9, with higher values indicating greater loneliness. We categorized subjects as 0–2, according to whether the original score was low (3), average (4 or 5) or high (≥6).
We created a score for social isolation from other yes/no variables: (i) being unmarried or not cohabiting; (ii) less than monthly contact with at least one child; and (iii) not doing voluntary or charity work or being a member of organizations, attending evening classes, social groups, clubs, political or community-related associations. We gave one point for each criterion satisfied, leading to scores ranging from 0 to 3. Higher values indicate greater social isolation. We categorized participants as 0–2, according to whether the original score was low (0) average (1) or high (≥2). The characteristics included in the indicator correspond to those used in a previous longitudinal study [17] considering the information available in the SHARE waves we have used (no information was available about contacts with friends and family members other than children), and in other studies based on SHARE [8], trying to use all the relevant information available.
In total, 39,475 cohort members aged ≥60 participated in wave 5, and 30,324 (78.4%) were re-interviewed at wave 6. In total, 30,267 had information about frailty status; of these, 27,468 had valid values in all the variables of interest, therefore representing our sample.
We considered the probability either to progress towards frailty or to reverse frailty. We computed separate relative risk ratios (RRRs) and 95% confidence intervals (CIs) for changing status from wave 5 to wave 6 for: robust individuals to become frail or pre-frail; pre-frail individuals to become frail or robust; and frail individuals to become pre-frail or robust. Using a longitudinal approach, in each subsample we used a multinomial logistic regression to compute RRRs for changing frailty status, according to social isolation and loneliness at wave 5. Each model contained terms for age (five years), sex, area of residence (large city, suburb of a large city, large town, small town, rural area), occupation (employed/self-employed, unemployed, retired, sick/disabled, homemaker/other), education (1–6 of the International Standard Classification of Education 1997), chronic illness (none, 1, ≥2), depression (0–12 on the EURO-D scale) [18] and sadness (‘In the last month have you been sad or depressed?’, yes/no).
The analysis was conducted using the statistical software package Stata, version 15 (College Station, TX, USA: StataCorp LP) and RStudio (Boston, MA, USA: RStudio Inc., Boston).
Results
At baseline, there were 13,069 (47.6%) robust, 11,430 (41.6%) pre-frail and 2,969 (10.8%) frail individuals. In the overall sample, the majority of people reported a low level of loneliness and an average level of social isolation. Although high social isolation was reported by 12% and high loneliness by 11% of the population, average social isolation was reported by almost two-thirds and average loneliness by a quarter. Average loneliness was more prevalent in pre-frail and frail individuals, and high levels were more prevalent in frail individuals. Average and high levels of social isolation were more frequent in pre-frail and frail people (Table 1).
Table 1.
Baseline characteristics of the participants (n = 27,468)
| Mean (SD), median (IQR) or n (%) | ||||
|---|---|---|---|---|
| Robust (n 13,069) | Pre-frail (n 11,430) | Frail (n 2,969) | Total (27,468) | |
| Age (years), mean (SD) | 68.6 (6.4) | 71.4 (7.7) | 76.0 (8.3) | 70.5 (7.6) |
| Female, n (%) | 6,380 (48.8) | 6,616 (57.9) | 1,989 (67.0) | 14,985 (54.6) |
| Loneliness, n (%) | ||||
| low | 9,521 (72.9) | 6,528 (57.1) | 1,268 (42.7) | 17,317 (63.0) |
| average | 2,902 (22.2) | 3,375 (29.5) | 858 (28.9) | 7,135 (26.0) |
| high | 646 (4.9) | 1,527 (13.4) | 843 (28.4) | 3,016 (11.0) |
| Social isolation, n (%) | ||||
| low | 4,049 (31.0) | 2,158 (18.9) | 213 (7.2) | 6,420 (23.4) |
| average | 7,743 (59.3) | 7,708 (67.4) | 2,201 (74.1) | 17,652 (64.3) |
| high | 1,277 (9.8) | 1,564 (13.7) | 555 (18.7) | 3,396 (12.4) |
| Area of residence, n (%) | ||||
| Large city | 1,737 (13.3) | 1,550 (13.6) | 404 (13.6) | 3,691 (13.4) |
| Suburbs of large city | 1,618 (12.4) | 1,318 (11.5) | 320 (10.8) | 3,256 (11.9) |
| Large town | 2,067 (15.8) | 1,861 (16.3) | 531 (17.9) | 4,459 (16.2) |
| Small town | 3,390 (25.9) | 3,159 (27.6) | 812 (27.4) | 7,361 (26.8) |
| Rural area/village | 4,257 (32.6) | 3,542 (31.0) | 902 (30.4) | 8,701 (31.7) |
| Occupation, n (%) | ||||
| Retired | 10,137 (77.6) | 8,960 (78.4) | 2,209 (74.4) | 21,306 (77.6) |
| Employed, self-employed or unemployed | 1,778 (13.6) | 897 (7.9) | 54 (1.8) | 2,729 (9.9) |
| Permanently disabled or sick | 157 (1.2) | 143 (1.3) | 13 (0.4) | 313 (1.1) |
| Homemaker, other | 89 (0.7) | 258 (2.3) | 146 (4.9) | 493 (1.8) |
| Education, n (%) | 908 (6.9) | 1,172 (10.3) | 547 (18.5) | 2,627 (9.6) |
| No qualification | 391 (3.0) | 741 (6.5) | 435 (14.7) | 1,567 (5.7) |
| Primary education | 2,050 (15.7) | 2,711 (23.7) | 1,027 (34.6) | 5,788 (21.1) |
| Secondary education | 7,084 (54.2) | 5,801 (50.8) | 1,216 (41.0) | 14,101 (51.3) |
| Tertiary education | 3,512 (26.9) | 2,130 (18.6) | 277 (9.3) | 5,919 (21.5) |
| Other | 32 (0.2) | 47 (0.4) | 14 (0.5) | 93 (0.3) |
| Depression, n (%) | ||||
| Probable | 789 (6.0) | 3,921 (34.3) | 2,028 (68.3) | 6,738 (24.5) |
| Sadness, n (%) | 3,235 (24.8) | 5,147 (45.0) | 1,903 (64.1) | 10,285 (37.4) |
| Chronic disease, n (%) ≥1 chronic disease | 9,822 (75.2) | 10,003 (87.5) | 2,894 (97.5) | 22,719 (82.7) |
When loneliness and social isolation were combined, the majority of people fell into the category low loneliness/average social isolation (11,127 individuals), whereas the least represented category was high loneliness/low social isolation (327).
After 2 years, progression towards pre-frailty or frailty was observed in 21% and reversion in 18% of the individuals. Among robust subjects at baseline, 8,706 (61.8%) were still robust, 4,033 (30.8%) were pre-frail and 330 (2.6%) were frail. Among those who were pre-frail, 1,504 (13.2%) progressed to frail and 3,557 (31.1%) became robust. Among frail people, 182 (6.1%) reversed to robust and 1,271 (42.8%) to pre-frail. Most people who reversed from pre-frail to robustness moved from having one condition of frailty to none (Supplementary Appendix 3 available in Age and Ageing online).
In the multivariate model, loneliness and social isolation were associated with the risk of robust people becoming frail and pre-frail (except for robust people with a high level of loneliness to become frail) (Figure 1A), and in the pre-frail to become frail (except with average loneliness) (Figure 1B). Risk of reversion from pre-frailty to robustness was significantly lower in people with a high level of loneliness (Figure 1B), and from frailty to robustness with both levels of loneliness (Figure 1C).
Figure 1.
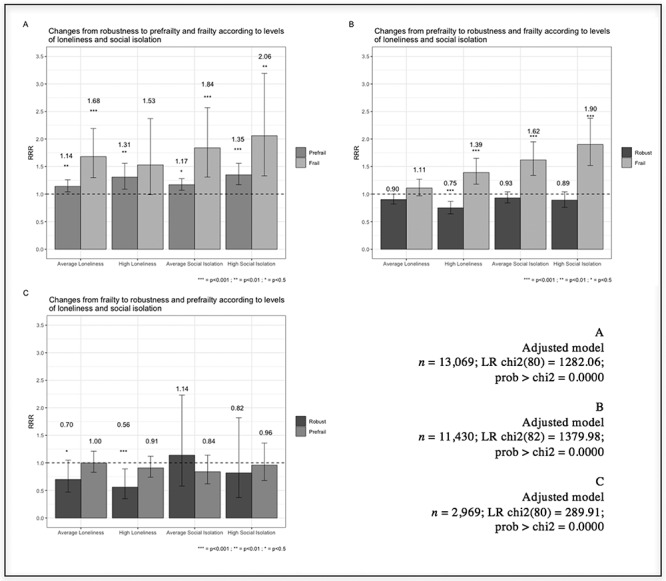
RRR and 95% CIs of changing status in robust (A), pre-frail (B) and frail (C) people according to levels of loneliness and social isolation.
Discussion
The findings from this large sample are in agreement with previous studies [11, 17, 19, 20] and confirm that social isolation and loneliness are an issue in the older population, although high levels of loneliness or high social isolation are uncommon, consistent with previous studies [21, 22].
About a fifth of the sample improved their frailty status, mainly moving from one condition of frailty to none, indicating that improvement is easier at the beginning of the process. Since there was a tendency for both levels of loneliness and social isolation to prevent reversion from pre-frailty to robustness, mitigation of these conditions can be a key factor in stopping progression. Alternatively, or in addition, a pre-frail status with only one condition can represent a temporary or acute worsening of the person’s health.
The magnitude of the associations of frailty with social isolation and loneliness was comparable. The ELSA study [17] found no association of social isolation with frailty after adjusting for several factors, corresponding mostly to the variables introduced in our models, suggesting that the significant effect of social isolation in our analysis is not due to insufficient adjustment. Prevalence of social isolation in the two studies was comparable, with median values corresponding to average social isolation in the overall sample in both studies. The association of frailty and social isolation in the ELSA study disappeared after adjustment for several factors, with RRRs still remaining non-significantly above 1. Since our sample was much larger, we may have had the possibility to show an association that could not be detected in the smaller ELSA sample. However, the two samples represented different, non-overlapping populations, which can create intrinsic differences in the mitigation of the health consequences of social isolation. For instance, one possible explanation is that, since social isolation may be directly associated with frailty through lack of opportunities for physical activity, in the SHARE sample social isolation hampered physical activities more than in the ELSA sample.
Our findings indicate that tackling social aspects of the life of frail and pre-frail people can reverse their condition, and that being less lonely and less socially isolated can help people maintain a robust or pre-frail status. It seems reasonable to act in a preventive fashion, rather than waiting for the process of frailty to start and progress.
Strengths of our study include the large sample size and the fact that SHARE was designed to be representative of the European older population. Our findings are consistent with those from other studies, thus reassuring us regarding their validity. However, the study has limitations. We used an adaptation of the Fried index of frailty that relies more on self-reported information. Our social isolation index was not validated. The short time between the two waves may have limited the number of changes and therefore affected the possibility to find significant associations. The possibilities offered by SHARE were not fully exploited as we did not address differences across countries.
Psychological and social factors should be considered inherent to frailty and ill-health. Attention should also be paid to average levels of loneliness and social isolation, which professionals and patients themselves often consider normal or acceptable, and should be actively addressed even in the absence of other health conditions through the available evidence-based interventions.
Supplementary Material
Contributor Information
Carlotta Micaela Jarach, Laboratory of Quality Assessment of Geriatric Therapies and Services, Istituto Services di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy; Department of Health Systems Management, Ben-Gurion University of the Negev, Israel.
Mauro Tettamanti, Laboratory of Geriatric Neuropsychiatry, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy.
Alessandro Nobili, Laboratory of Quality Assessment of Geriatric Therapies and Services, Istituto Services di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy.
Barbara D'avanzo, Laboratory of Quality Assessment of Geriatric Therapies and Services, Istituto Services di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy.
Supplementary data:
Supplementary data mentioned in the text are available to subscribers in Age and Ageing online.
Funding:
This paper uses data from SHARE waves 5 and 6 (DOIs: 10.6103/SHARE.w5.611, 10.6103/SHARE.w6.611); see Börsch-Supan et al. [23] for methodological details. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N°211,909, SHARE-LEAP: N°227,822, SHARE M4: N°261,982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06–11, OGHA_04–064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Conflict of interest:
None.
References
- 1. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381: 752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lang PO, Michel JP, Zekry D. Frailty syndrome: a transitional state in a dynamic process. Gerontology 2009; 55: 539–49. [DOI] [PubMed] [Google Scholar]
- 3. Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health 2013; 103: 2056–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Perissinotto CM, Stijacic Cenzer I, Covinosky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med 2012; 172: 1078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Herrera-Badilla A, Navarrete-Reyes AP, Amieva H, Avila-Funes JA. Loneliness is associated with frailty in community-dwelling elderly adults. J Am Geriatr Soc 2015; 63: 607–9. [DOI] [PubMed] [Google Scholar]
- 6. Mulasso A, Roppolo M, Giannotta F, Rabaglietti E. Associations of frailty and psychosocial factors with autonomy in daily activities: a cross-sectional study in Italian community-dwelling older adults. Clin Interv Aging 2016; 11: 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bessa B, Ribeiro O, Coelho T. Assessing the social dimension of frailty in old age: a systematic review. Arch Gerontol Geriatr 2018; 78: 101–13. [DOI] [PubMed] [Google Scholar]
- 8. Stolz E, Mayerl A, Waxxeneger A, Freidl W. Explaining the impact of poverty on old-age Europe: material, psychosicial and behaviour. Eur J Public Health 2017; 27: 1003–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Börsch-Supan A. Survey of health, ageing and retirement in Europe (SHARE) wave 5. Release version: 6.1.1. SHARE-ERIC. Data set. 2018a. doi: 10.6103/SHARE.w5.611. [DOI] [Google Scholar]
- 10. Börsch-Supan A. Survey of health, ageing and retirement in Europe (SHARE) wave 6. Release version: 6.1.1. SHARE-ERIC. Data set. 2018b. doi: 10.6103/SHARE.w6.611. [DOI] [Google Scholar]
- 11. Fried LP, Tangen CM, Walston J et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Bio Sci Med Sci 2001; 56: M146–56. [DOI] [PubMed] [Google Scholar]
- 12. Santos-Eggimann B, Cuénoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Bio Sci Med Sci 2009; 64: 675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Romero-Ortuno R, Walsh CD, Lawlor BA, Kenny RA. A frailty instrument for primary care: findings from the survey of health, ageing and retirement in Europe (SHARE). BMC Geriatr 2010; 10: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ilinca S, Calciolari S. The patterns of health care utilization by elderly Europeans: frailty and its implications for health systems. Health Serv Res 2015; 50: 305–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jarach CM, Cesari M. Frailty beyond the clinical dimension: discussion about the underlying aspect of the social capital. Minerva Med 2018; 109: 472–8. [DOI] [PubMed] [Google Scholar]
- 16. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging 2004; 26: 655–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English longitudinal study of ageing. Age Ageing 2018; 47: 392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Prince MJ, Reischies F, Beekman AT et al. Development of the EURO-D scale—a European Union initiative to compare symptoms of depression in 14 European centres. Br J Psychiatry 1999; 174: 330–8. [DOI] [PubMed] [Google Scholar]
- 19. Trevisan C, Veronese MS, Baggio G et al. Factors influencing transitions beteween frailty states in elderly adults: the Progetto Veneto Anziani longitudinal study. J Am Geriatr Soc 2017; 65: 169–84. [DOI] [PubMed] [Google Scholar]
- 20. Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med 2006; 166: 418–23. [DOI] [PubMed] [Google Scholar]
- 21. Sundström G, Fransson E, Malmberg B, Davey A. (2009). Loneliness among older Europeans. Eur J Ageing 2009; 6: 267–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Domenech-Abella J, Lara E, Rubio-Valera M et al. Loneliness and depression in the elderly: the role of social network. Soc Psychiatry Psychiatr Epidemiol 2017; 52: 381–90. [DOI] [PubMed] [Google Scholar]
- 23. Börsch-Supan AM, Brandt C, Hunkler T et al. Data resource profile: the survey of health, ageing and retirement in Europe (SHARE). Int J Epidemiol 2013; 42: 992–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


