Abstract
The study investigated whether lifetime stress exposure is associated with greater impulsivity and addictive behavior. We also examined whether stress and impulsivity interactively predicted food addiction and alcohol-related behavior. Greater lifetime stress exposure was related to more impulsivity and food addictive behaviors, but not alcohol-related consequences. There were no interactions between lifetime stress exposure and impulsivity in predicting addictive behaviors. Exploratory analyses revealed that early and adulthood stress exposure predicted food addiction, whereas only adulthood stress predicted alcohol-related consequences. Therefore, lifetime stress exposure is related to impulsivity and addiction, but these effects differ by addiction outcome and specific timing of stress exposure.
Keywords: addiction, impulsivity, open data, preregistered analysis, stress
Introduction
Addiction to food and alcohol is a key public health issue, with higher levels of substance use in younger adults than in other age groups (Center for Behavioral Health Statistics and Quality, 2016). In addition, food and alcohol addiction poses a substantial burden on young individuals, their families, and society as a whole (Center for Behavioral Health Statistics and Quality, 2016). Stress is a known risk factor for the development of appetitive behavior disorders, such as obesity and addiction (for a review, see Sinha and Jastreboff, 2013). Another risk factor for such behavior is impulsivity, or a predisposition toward quick reactions to stimuli without consideration of consequences (Moeller et al., 2001). Despite both of these factors being important risk factors for addictive disorders, their concurrent relation to addictive behavior has only rarely been assessed. The goal of the present study was to examine the relations among stress, impulsivity, and addiction, as well as the extent to which lifetime stress exposure interacts with trait impulsivity to predict addictive behavior related to food and alcohol.
Stress is thought to play a role in the development, maintenance, and relapse of addiction by increasing craving and motivation toward addictive behavior (Amlung and MacKillop, 2014; Clay et al., 2018). The relation between stress and addiction may be bidirectional, such that addictive behaviors may serve as a means to escape stress and blunted stress physiology, in turn, may confer increased risk for engaging in addictive behaviors (Buchanan et al., 2020a, 2020b; Carroll et al., 2017; Lovallo, 2013). A blunted stress response may drive an individual to seek out stimulation using drugs of abuse, and the subsequent activation of stress physiology via the hypothalamic-pituitary-adrenal (HPA) axis may contribute to the development of both tolerance to and withdrawal from the abused drugs (Wemm & Sinha, 2019).
Relatedly, stress may contribute to the development of eating disorders, such as food addiction, via alterations in HPA axis functioning and glucocorticoid gene expression (Imperatori et al., 2016; Sinha, 2018). In particular, psychological and sexual trauma during childhood are related to food addiction (Nunes-Neto et al., 2018). However, less is known about the differential impacts of stress based on the type of addictive behavior (i.e. behavioral addiction versus substance use). Therefore, additional research is needed to assess the impacts of life stress and its timing on various addictive behaviors that individuals exhibit.
Greater cumulative lifetime stress exposure has been related to more self-reported impulsivity (Hamilton et al., 2014), with early life stress being particularly strongly linked to impulsivity in past research (Espeleta et al., 2018; Hallowell et al., 2019). In addition, heightened impulsivity is a characteristic of many addictive disorders, such as alcohol addiction (Coskunpinar et al., 2013) and food addiction (Hardy et al., 2018; Sinha, 2018; Sinha and Jastreboff, 2013). Hence, measures of impulsivity are often associated with indices of stress and addiction (Kim, et al., 2018; Shin et al., 2015; Wardell et al., 2016; Zhu et al., 2016). Specifically, both alcohol and food addiction have been related to greater negative urgency, which highlights the role that negative emotion plays in addictive behavior (i.e. acting impulsively under distress; Pivarunas and Conner, 2015).
Impulsivity is a risk factor for behavior disorders such as criminality, overeating, and substance use more generally (Lejuez et al., 2010; Verdejo-Garcia et al., 2007). However, the specific aspects of how stress may relate to impulsivity, and how the stress-impulsivity relationship in turn influences addictive behavior, is not well understood. Several studies have examined associations among stress, impulsivity, and addiction (for reviews, see Lejuez et al., 2010; Lovallo, 2013). However, these studies have not generally assessed the specific timing or type of stress exposure over the lifespan (see Slavich and Shields, 2018). More comprehensive measurement of which stress-related factors (e.g. timing, type of stressor, developmental timing of exposure) most strongly impact impulsivity and addiction is necessary to help inform the development of comprehensive models of stress and health, and to design more focused interventions for preventing and treating addictive behavior and related health problems (Slavich, 2016, 2019).
The present study
To better understand the relations among life stress, impulsivity, and addiction, we recruited 200 healthy college students and assessed their lifetime stress exposure and self-reported impulsivity and addictive behaviors. We specifically chose this sample because college students report high levels of binge drinking, negative consequences of alcohol (Hingson, 2010), and high incidence of eating disorders and food addiction (Allen et al., 2013; Merikangas et al., 2010; Schulte and Gearhardt, 2017). We comprehensively measured participants’ cumulative lifetime stress exposure, which included assessing each experienced stressor’s severity, frequency, timing, duration, and primary social-psychological characteristic (Slavich and Shields, 2018). We also quantified impulsivity, food addiction, and negative consequences of alcohol using validated self-report measures of these constructs. The study, hypotheses, and intentions for exploratory analyses were all preregistered.
Based on the literatures reviewed above, we hypothesized that greater cumulative lifetime stress exposure would be related to greater impulsivity and greater reports of addictive behavior (e.g. food, alcohol), and that cumulative lifetime stress exposure would interact with impulsivity to predict addictive behavior. Stress may lead to impulsivity, which in turn may lead to addictive behavior. However, much of the existing research is based on cross-sectional mediation, which cannot confirm the causality of such relations. Therefore, it is more appropriate to use hierarchical or moderated regression models in cross-sectional studies that do not imply causality until such relations are tested in longitudinal study designs.
In addition, in exploratory analyses, we examined the predictive value of four different life stress models to determine which model best fit reports of food and alcohol addiction. First, we tested the cumulative lifetime stress model, also known as the allostatic load model, which posits that stress experienced across the entire lifespan results in additive effects on physiology, behavior, and cognition (for review, see Young et al., 2019). Second, we tested the early life stress, or biological embedding model, which contends that stress experienced early in life, or even prenatally, influences the development of the HPA axis in a way that has physical and mental health consequences across the lifespan (Lupien et al., 2009; Shonkoff et al., 2009). Third, we tested the sensitization model, which hypothesizes that early life experiences and recent life stress exposure both impact HPA axis function and stress-related outcomes in adulthood (Daskalakis et al., 2013; Young et al., 2019). Finally, we tested the mismatch hypothesis, which suggests an interactive effect of mismatching levels of early life stress and recent life stress on health outcomes (Nederhof and Schmidt, 2012; Paquola et al., 2017). To test these models (i.e. cumulative, early life, sensitization, and mismatch), we explored whether the timing of stress exposure was related to participants’ reports of food and alcohol addiction.
Method
Participants
Participants were 200 healthy young adults (133 females, 64 males, 3 did not indicate a gender) between the ages of 18 and 25 years old who were recruited from undergraduate courses. To increase the generalizability of the results, participants were not excluded based on physical health problems, or psychiatric or neurological disorders. Sample size was determined using the software program R (R Core Team, 2019) and the package ‘pwr’ (Champely, 2018). Our goal was to obtain 0.80 power to detect a small effect size of f2 = 0.05 at 0.05 alpha error probability for regression models with two predictors as well as one-tailed correlations of r = 0.20. This analysis specifically assessed the potential to detect the relations among stress, impulsivity, and addiction, as well as the interactive effects of life stress and impulsivity on measures of addiction. Upon completion of the study, participants received course credit for their time. All procedures were approved by the Institutional Review Board.
Measures
Lifetime stress exposure.
Lifetime stress exposure was assessed using the Stress and Adversity Inventory for Adults (STRAIN; Slavich and Shields, 2018). The STRAIN assesses stressful life experiences across 55 different acute and chronic stressors, and uses extensive branching logic to ask about stressors and includes follow-up questions when a stressor is endorsed (see https://www.strainsetup.com). The STRAIN has excellent concurrent, discriminate, and incremental validity, and has been shown to predict a wide variety of cognitive, biological, and health outcomes (e.g. Cazassa et al., 2020; Lam et al., 2019; Mayer et al., 2019; Olvera Alvarez et al., 2019; Pegg et al., 2019; Sturmbauer et al., 2019).
To test the preregistered hypotheses, we used the STRAIN’s main index of cumulative lifetime stress exposure, which indicates the total number of stressful life events and chronic difficulties that a participant experienced over their entire lifespan. Scores for cumulative lifetime stress exposure count in this sample ranged from 0 to 51.
Impulsivity.
The short form of the Urgency, Premeditation, Perseverance, Sensation Seeking, Positive Urgency, Impulsive Behavior Scale (UPPS) was used to measure self-reported impulsive behavior based on 5 different dimensions across 20 questions on a 4-point Likert-type scale (Cyders et al., 2014). There are a number of ways to conceptualize impulsivity (Evenden, 1999); we chose the urgency model, assessed via the UPPS, because it focuses on more emotion-based impulsivity, which is commonly associated with both stress and addiction (Cyders et al., 2014). Four questions each were used to assess the five dimensions: negative urgency (i.e. acting rashly under negative emotions; “When I am upset I often act without thinking.”), positive urgency (i.e. acting rashly under positive emotions), lack of premeditation (e.g. acting without thinking), lack of perseverance (e.g. not focusing on a task), and sensation seeking (e.g. seeking out extreme experiences). Participants rated the extent to which they agreed their behavior aligned with each question (i.e. agree strongly, agree some, disagree some, disagree strongly). The sum of each scale was used in the analyses reported below. Internal consistency of the UPPS subscales in the present study ranged from good to very good, Cronbach’s αs = 0.75 to 0.85.
Food addiction.
The modified Yale Food Addiction Scale Version 2.0 (mYFAS 2.0) was used in this study to assess addictive-like eating behavior focusing on processed foods, dependence, loss of control, and unsuccessful attempts to quit (Schulte and Gearhardt, 2017). The measure asks 13 questions (e.g. “My overeating got in the way of me taking care of my family or doing household chores.”) and participants respond on an 8-point scale based on frequency of the behavior they endorsed (e.g. never, less than monthly, 2 to 3 times a week). The sum for each participant was used for analyses and clinical cutoffs were calculated for descriptive purposes. Internal consistency of the mYFAS 2.0 in the present study was very good, Cronbach’s α = 0.86.
Alcohol-related behavior.
The Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler et al., 2005) was used to measure harmful drinking experiences over the past month across multiple domains: social, academic, riskiness, poor control, impaired self-care, lacking self-perception, blackout drinking, and dependence. Participants answered either “yes” or “no” to each question based on whether they have had the described experience (e.g. “I have become very rude, obnoxious or insulting after drinking”). The sum of all 24 questions were used to create a total YAACQ score. Internal consistency of the BYAACQ in the present study was very good, Cronbach’s α = 0.89.
Procedure
Participants came to the lab for a one-hour session. Upon arrival, participants were separated into different offices, each with a private computer. They then provided written informed consent before reporting their demographic information (e.g. age, race, income) and completing the questionnaires described above. The order of the questionnaires was counterbalanced across all participants. After completing the questionnaires, participant height and weight were measured using a stadiometer and scale by a trained research assistant in a private office.
Data management and analysis
Data, preregistered hypotheses, and code for preregistered analyses are posted on the Open Science Framework (Center for Open Science, Charlottesville, VA, USA) under the Stress, Addictive Behavior, & Impulsivity project: https://osf.io/uamd8/. We describe the hypotheses and statistical tests used to test them in the results section below. The preregistration indicated that we would investigate gambling behavior; however, 87% of participants did not endorse any gambling behavior, so these analyses were not conducted nor are they reported below. The natural logarithm transformation was applied when variables showed a significant positive skew (e.g. mYFAS 2.0, YAACQ, STRAIN lifetime stressor count). The variables presented in the figures represent the raw values. All data analyses were conducted using R (R Core Team, 2019), and all data and code for the analyses are available on the preregistration page. Upon review of the data, which indicated gender differences in reports of food addiction-related behavior, we used gender as a covariate in our food addiction models. Three participants’ STRAIN data were missing due to computer error and were excluded.
Results
The descriptive and clinical characteristics of the sample are presented in Table 1. Due to gender differences previously reported among the key variables (Cyders, 2013; Hodes and Epperson, 2019; Yu et al., 2018), independent t-tests were conducted to determine whether gender differences existed in this sample (see Table 1). Correlation analyses among the key variables (i.e. life stress, impulsivity, addiction) are described in Table 2.
Table 1.
Demographic characteristics for the full sample and by gender.
| Variable | Entire sample (n = 200) | Female (n = 133) | Male (n = 64) | Test for gender differences Statistic (df), p-value |
|---|---|---|---|---|
| Race | χ2(3) = 2.36, p = 0.50 | |||
| Caucasian | 151 (75.5%) | 102 (76.8%) | 47 (73.4%) | |
| African American | 10 (5%) | 5 (3.7%) | 5 (7.8%) | |
| Asian | 29 (14.5%) | 21 (15.8%) | 8 (12.5%) | |
| Other | 10 (5%) | 5 (3.7%) | 4 (6.3%) | |
| Ethnicity | χ2(1) = 2.11, p = 0.147 | |||
| Hispanic | 16 (8%) | 7 (5.2%) | 7 (10.9%) | |
| Non-Hispanic | 184 (92%) | 126 (94.8%) | 57 (89.1%) | |
| M (SD) | M (SD) | M (SD) | ||
| Age (years) | 18.9 (0.98) | 18.8 (.93) | 19.1 (1.05) | t(195) = −2.32, p = 0.022 |
| Body mass index | 24.2 (4.60) | 24.2 (4.68) | 24.1 (4.18) | t(176) = 0.126, p = 0.900 |
| STRAIN | ||||
| Lifetime stressor count* | 14.0 (9.29) | 14.7 (9.88) | 12.0 (7.51) | t(192) = 1.88, p = 0.062 |
| Lifetime stressor severity* | 32.1 (21.6) | 34.5 (22.9) | 26.0 (17.0) | t(192) = 2.62, p = 0.022 |
| Yale food addiction* | 7.83 (7.02) | 8.83 (7.43) | 5.61 (5.49) | t(195) = 3.09, p = 0.002 |
| Met clinical cutoff | 79 (39.5) | 60 (45.1%) | 19 (29.6%) | |
| Young adult alcohol consequences | 5.72 (5.10) | 5.77 (4.95) | 5.69 (5.50) | t(195) = 0.102, p = 0.919 |
| UPPS | Sum (SD) | Sum (SD) | Sum (SD) | |
| Negative urgency | 9.39 (2.45) | 9.36 (2.50) | 9.45 (2.39) | t(195) = −0.246, p = 0.806 |
| Positive urgency | 7.71 (2.65) | 7.37 (2.71) | 8.28 (2.37) | t(195) = −2.30, p = 0.022 |
| Sensation seeking | 11.4 (2.46) | 10.9 (2.56) | 12.2 (2.02) | t(195) = −3.32, p = 0.001 |
| Lacking premeditation | 6.54 (1.86) | 6.62 (1.75) | 6.31 (2.01) | t(195) = 1.09, p = 0.279 |
| Lacking perseverance | 6.67 (1.78) | 6.69 (1.82) | 6.63 (1.69) | t(195) = 0.246, p = 0.806 |
M = Mean; SD = Standard Deviation.
UPPS = Urgency, Premeditation, Perseverance, Sensation Seeking, Positive Urgency, Impulsive Behavior Scale.
Indicates Levene’s test is significant (p < 0.05).
Three participants identified as a non-binary gender.
Table 2.
Correlations among the main study variables.
| Measure | STRAIN | Addiction indices | UPPS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Lifetime stressor count | Lifetime stressor severity | Yale food addiction | Young adult alcohol consequences | Negative urgency | Positive urgency | Sensation seeking | Lacking premeditation | Lacking perseverance | |
| Lifetime stressor count | – | 0.923** | 0.305** | 0.117 | 0.173** | 0.101 | 0.062 | 0.087 | −0.032 |
| Lifetime stressor severity | – | 0.202** | 0.176** | 0.165** | 0.073 | 0.052 | 0.076 | −0.063 | |
| Yale food addiction | – | 0.193** | 0.348** | 0.196** | −0.081 | 0.188** | 0.181** | ||
| Young adult alcohol consequences | – | 0.316** | 0.297** | 0.219** | 0.318** | 0.062 | |||
| Negative urgency | – | 0.460** | −0.035 | 0.291** | 0.134 | ||||
| Positive urgency | – | 0.309** | 0.286** | 0.270** | |||||
| Sensation seeking | – | 0.105 | 0.055 | ||||||
| Lacking premeditation | – | 0.493** | |||||||
UPPS = Urgency, Premeditation, Perseverance, Sensation Seeking, Positive Urgency, Impulsive Behavior Scale. All correlations are two-tailed except those with directional hypotheses indicated in text. n = 200 for all analyses, except n = 197 for STRAIN analyses due to missing data.
p < 0.01.
Clinical characteristics
Using the scoring criteria for the mYFAS, 40.5% (n = 81) of the sample met the clinical significance criteria (i.e. endorsed ⩾2 symptoms) for food addiction, with scores ranging from 0 to 9.
Food addiction and impulsivity
As hypothesized, food addiction was associated with all the subscales of the UPPS except sensation seeking: negative urgency, r = 0.348, p < 0.001, 95% CI [.464–0.220]; positive urgency, r = 0.196, p = 0.005, 95% CI [0.326–0.059]; lack of premeditation, r = 0.188, p = 0.008, 95% CI [0.319–0.051]; and lack of perseverance, r = 0.181, p = 0.010, 95% CI [0.312–0.044] (see Table 2).
Alcohol consequences and impulsivity
As hypothesized, alcohol consequences reported on the BYAACQ were significantly related to all the subscales of the UPPS: negative urgency, r = 0.316, p < 0.001, 95% CI [0.436–0.185]; positive urgency, r = 0.297, p < 0.001, 95% CI [.419–0.165]; lack of premeditation, r = 0.318, p < 0.001, 95% CI [0.437–0.188]; and sensation seeking, r = 0.219, p = 0.002, 95% CI [0.347–0.083] (see Table 2).
Primary analyses
The first hypothesis was that greater lifetime stress exposure would be related to greater self-reported impulsivity. Results of one-tailed Pearson’s correlation analyses between lifetime stressor count and each subscale of the UPPS indicated that greater lifetime stress exposure was significantly related to negative urgency, r = 0.173, p = 0.008, 95% CI [0.056–1.00], but not to positive urgency (r = 0.101, p = 0.079), lacking premeditation (r = 0.087, p = 0.112), lacking perseverance (r = −0.032, p = 0.671), or sensation seeking (r = 0.062, p = 0.193) (see Table 2).
As hypothesized, there was a significant positive relationship between lifetime stressor count and food addictive behavior (the sum score of the mYFAS 2.0; r = 0.305, p < 0.001, 95% CI [0.193–1.00], one-tailed) (see Figure 1 and Table 2).
Figure 1.
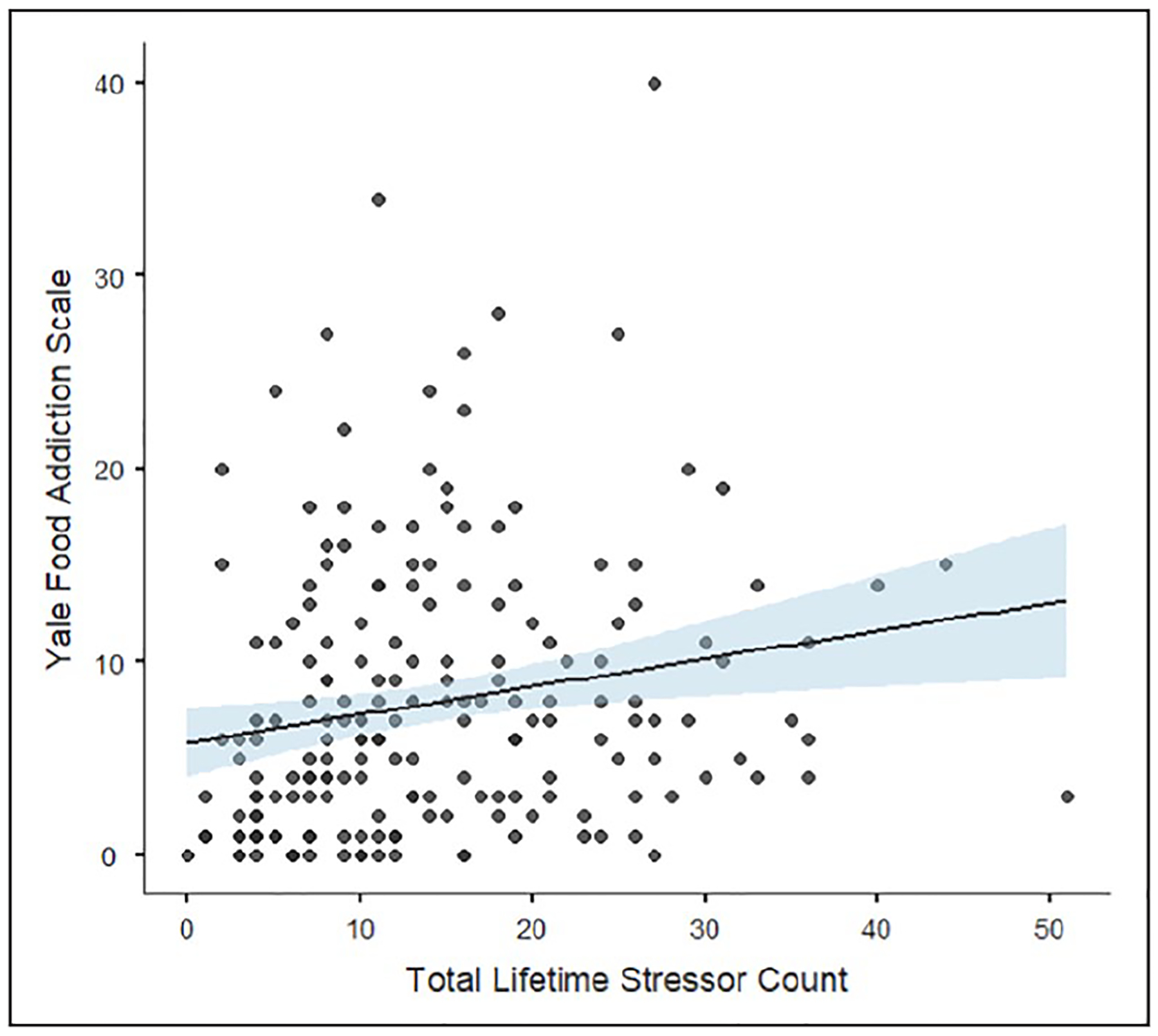
Relation between total lifetime stressor count and food addiction. Greater total lifetime stress exposure was related to more food addictive behavior.
We hypothesized that greater lifetime stress exposure would be related to more alcohol-related consequences. There was a positive relationship between number of stressors experienced over the life course and alcohol-related consequences, but this relationship was relatively weak and not statistically reliable, r = 0.117, p = 0.0504, 95% CI [0.000–1.00], one-tailed).
We hypothesized that lifetime stress exposure would interact with impulsivity to explain negative consequences of drinking alcohol. Contrary to this hypothesis, however, cumulative lifetime stressor count did not significantly interact with any facet of impulsivity to predict alcohol-related consequences (see Table 3).
Table 3.
Moderation estimates for alcohol-related consequences.
| Estimate | SE | t | p | |
|---|---|---|---|---|
| Lifetime stressor count | 0.0646 | 0.0673 | 1.68 | 0.346 |
| Negative urgency | 0.2815 | 0.0683 | 0.94 | <0.001 |
| Lifetime stressor count × Negative urgency | −0.0036 | 0.0675 | −2.16 | 0.956 |
| R2 = 0.096; F(3, 193) = 6.816, p < 0.001 | ||||
| Lifetime stressor count | 0.0874 | 0.0675 | 1.295 | 0.196 |
| Positive urgency | 0.2514 | 0.0682 | 3.684 | <0.001 |
| Lifetime stressor count × Positive urgency | −0.0494 | 0.0681 | −0.726 | 0.468 |
| R2 = 0.079; F(3, 193) = 5.543, p = 0.001 | ||||
| Lifetime stressor count | 0.1049 | 0.0672 | 1.561 | 0.120 |
| Sensation seeking | 0.2196 | 0.0674 | 3.256 | 0.001 |
| Lifetime stressor count × Sensation seeking | −0.1069 | 0.0672 | −1.590 | 0.113 |
| R2 = 0.081; F(3, 193) = 5.696, p < 0.001 | ||||
| Lifetime stressor count | 0.0900 | 0.0668 | 1.347 | 0.179 |
| Lacking premeditation | 0.2760 | 0.0666 | 4.144 | <0.001 |
| Lifetime stressor count × Lacking premeditation | −0.0262 | 0.0724 | −0.362 | 0.718 |
| R2 = 0.094; F(3, 193) = 6.702, p < 0.001 | ||||
| Lifetime stressor count | 0.1207 | 0.0701 | 1.722 | 0.086 |
| Lacking perseverance | 0.0469 | 0.0693 | 0.677 | 0.499 |
| Lifetime stressor count × Lacking perseverance | 0.0348 | 0.0696 | 0.501 | 0.617 |
| R2 = 0.018; F(3, 193) = 1.168, p = 0.323 | ||||
SE: standard error.
Finally, we hypothesized that lifetime stress exposure would interact with impulsivity to predict increased reports of food addiction. Contrary to hypotheses, though, lifetime stressor count did not interact with any facet of impulsivity to predict food addiction behavior (see Table 4).
Table 4.
Moderation estimates for food addiction (controlling for gender).
| Estimate | SE | t | p | |
|---|---|---|---|---|
| Lifetime stressor count | 0.2090 | 0.0616 | 3.394 | <0.001 |
| Negative urgency | 0.2482 | 0.0599 | 4.143 | <0.001 |
| Lifetime stressor count × Negative urgency | −0.0233 | 0.0587 | −0.398 | 0.691 |
| R2 = 0.208; F(4, 189) = 12.38, p < 0.001 | ||||
| Lifetime stressor count | 0.2450 | 0.0619 | 3.957 | <0.001 |
| Positive urgency | 0.1401 | 0.0630 | 2.222 | 0.027 |
| Lifetime stressor count × Positive urgency | 0.0372 | 0.0626 | 0.5950 | 0.552 |
| R2 = 0.160; F(4, 189) = 9.008, p < 0.001 | ||||
| Lifetime stressor count | 0.2596 | 0.0624 | 4.156 | <0.001 |
| Sensation seeking | −0.0466 | 0.0637 | −0.730 | 0.466 |
| Lifetime stressor count × Sensation seeking | 0.0125 | 0.0621 | 0.203 | 0.839 |
| R2 = 0.139; F(4, 189) = 7.598, p < 0.001 | ||||
| Lifetime stressor count | 0.2528 | 0.0618 | 4.086 | <0.001 |
| Lacking premeditation | 0.0651 | 0.0619 | 1.051 | 0.294 |
| Lifetime stressor count × Lacking premeditation | 0.1107 | 0.0674 | 1.643 | 0.102 |
| R2 = 0.153; F(4, 189) = 8.561, p < 0.001 | ||||
| Lifetime stressor count | 0.2669 | 0.0624 | 4.273 | <0.001 |
| Lacking perseverance | 0.1056 | 0.0613 | 1.722 | 0.087 |
| Lifetime stressor count × Lacking perseverance | 0.0440 | 0.0614 | 0.718 | 0.474 |
| R2 = 0.153; F(4, 189) = 8.516, p < 0.001 | ||||
SE: standard error.
Exploratory analyses: Stress exposure timing
Exploratory analyses were conducted to examine which lifetime stress model was most strongly related to addictive behaviors as a function of timing of stress exposure. We examined two specific time periods – namely, early-to-middle childhood (up to 12 years old) and adulthood life stress (after age 18). These age cut-offs are commonly used in life stress research (Del Giudice et al., 2011; Lupien et al., 2009). Results of these analyses revealed that food addiction was positively correlated with both early life stressor count, r = 0.291, p < 0.001, 95% CI [0.157–0.414] (Figure 2a), and adulthood life stressor count, r = 0.288, p < 0.001, 95% CI [0.155–0.411] (Figure 2b). In contrast, alcohol-related consequences were positively correlated with adulthood life stressor count, r = 0.241, p < 0.001, 95% CI [0.105–368], but not early life stressor count, r = −0.032, p = 0.655, 95% CI [–0.171–0.108].
Figure 2.
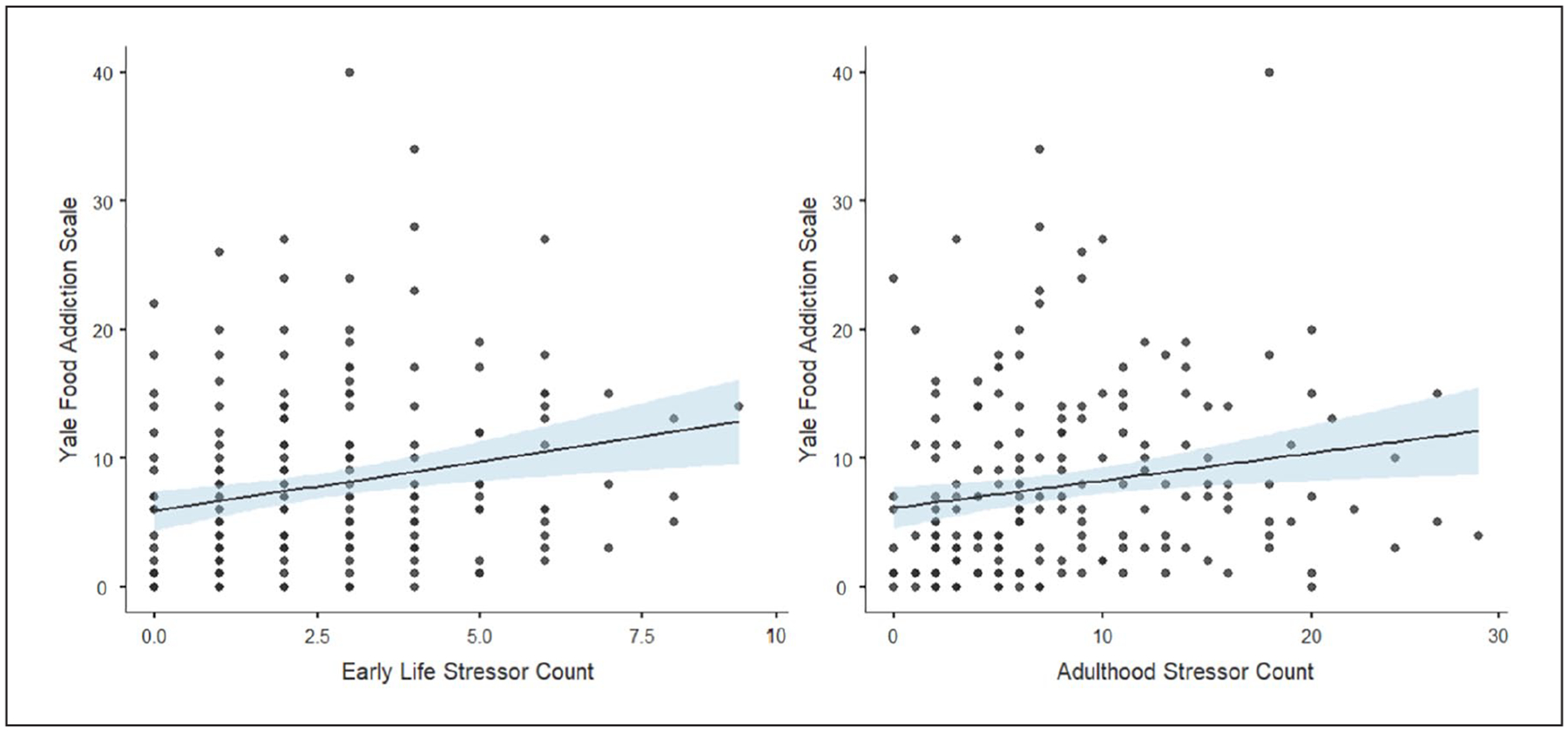
Relation between stress exposure timing and food addiction. Greater (a) early life stress exposure and (b) adulthood stress exposure were both related to more food addictive behavior.
In addition, research has suggested that early life stress may relate to or interact with recent life stress exposure (e.g. sensitization model, mismatch hypothesis) to predict health outcomes (see Young et al., 2019). To examine this possibility, we tested whether early and adulthood life stress exposure were interactively associated with food addiction and alcohol-related consequences. We found that early and adulthood life stress exposure were interactively associated with increased reports of food addiction (for estimates and simple slope estimates, see Table 5 and Figure 3), but not alcohol-related consequences. Consistent with the mismatch hypothesis, simple slopes analyses indicated that participants reporting higher early life stress exposure and lower adulthood life stress exposure reported the highest levels of food addiction. Importantly, the pattern is similar when the data are presented as adulthood simple slope estimates across varying levels of early life stress exposure (see Table 5).
Table 5.
Moderation and simple slope estimates for food addiction (controlling for gender).
| Estimate | SE | t | p | |
|---|---|---|---|---|
| Early life stressor count | 0.2106 | 0.0728 | 2.893 | 0.004 |
| Adulthood stressor count | 0.1567 | 0.0693 | 1.259 | 0.025 |
| Early life stressor count × Adulthood stressor count | −0.1498 | 0.0548 | −2.731 | 0.007 |
| R2 = 0.163; F (4, 189) = 9.171, p < 0.001 | ||||
| Adulthood simple slope estimates | ||||
| Average early life stress | 0.1584 | 0.0694 | 2.281 | 0.023 |
| Low (−ISD) Early life stress | 0.3082 | 0.0932 | 3.307 | 0.001 |
| High (+ISD) Early life stress | 0.0087 | 0.0835 | 0.1040 | 0.917 |
| Early life simple slope estimates | ||||
| Average adulthood stress | 0.2121 | 0.0730 | 2.906 | 0.004 |
| Low (−ISD) adulthood stress | 0.3623 | 0.1042 | 3.477 | <0.001 |
| High (+ISD) adulthood stress | 0.0620 | 0.0764 | 0.8113 | 0.418 |
SE: standard error.
Figure 3.
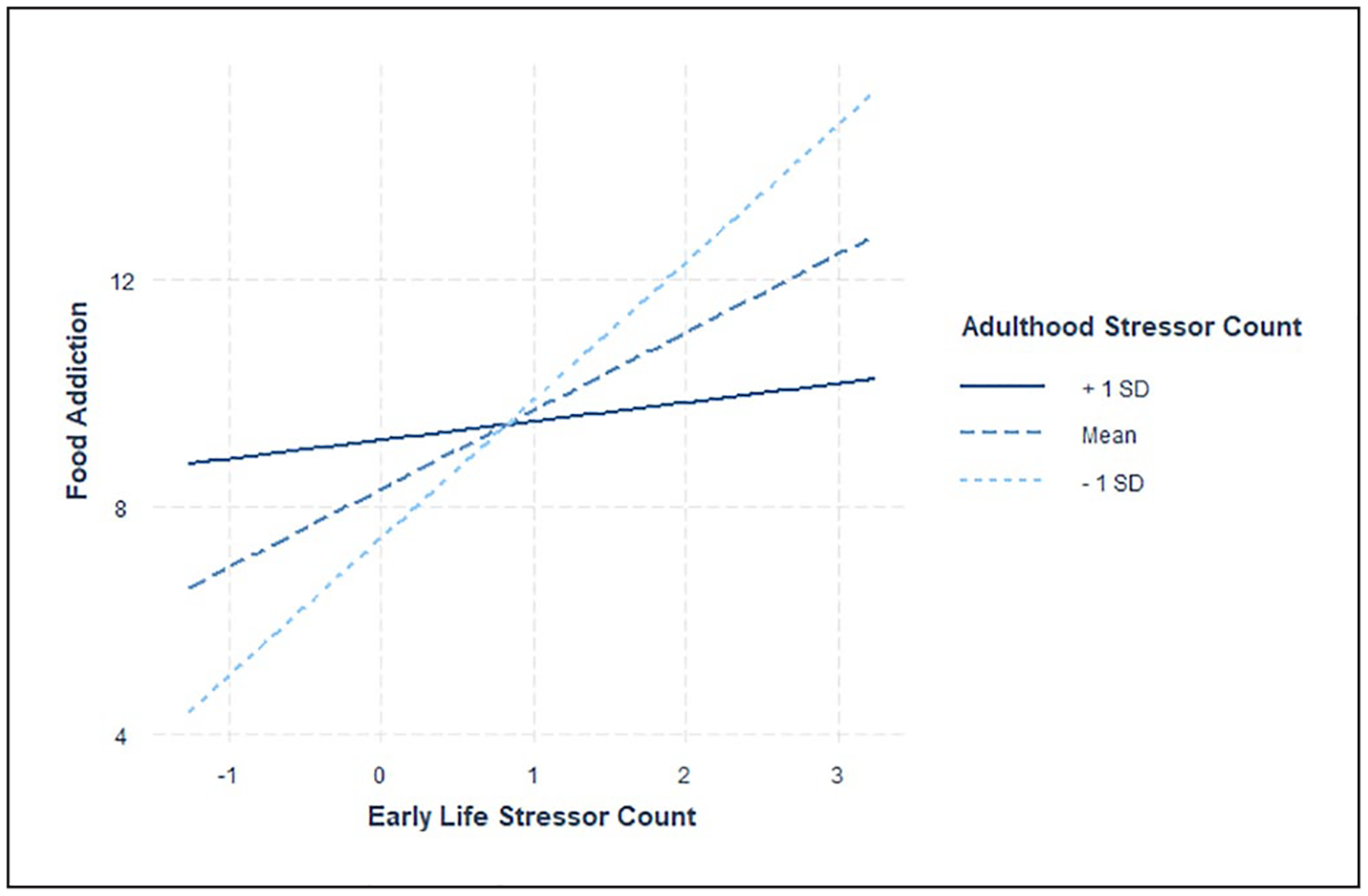
Early life and adulthood stressor simple slopes for food addiction. Simple slopes results indicate the steepest slopes for those with lower (−1 SD; dotted line) and mean levels (dashed line) of adulthood life stress exposure, as compared to those with higher adulthood life stress exposure (+1 SD; solid line). Individuals with lower adulthood life stress exposure and greater early life stress exposure reported the most food addictive behavior, whereas those reporting lower adulthood stress and lower early life stress exposure reported the least food addictive behavior. Individuals with greater adulthood life stress exposure did not report differences in food addictive behavior based on early life stress exposure. Mean centered values are presented on the x-axis. SD: Standard deviation.
Discussion
Life stress and trait impulsivity are often considered important contributors to the development of addictive behaviors (Lovallo, 2013). However, the concurrent and interactive influence of stress and impulsivity on addictive behaviors is not well understood. We addressed this issue in the present study by using well-validated measures to assess relations among life stress exposure, impulsivity, and addictive behavior toward food and alcohol. Three main findings emerged. First, consistent with preregistered predictions, we found that greater lifetime stress exposure was related to greater negative urgency, or the tendency to make impulsive decisions under negative emotionality. Second, greater lifetime stress exposure was related to greater food addiction, but not alcohol-related behavior. Furthermore, analyses indicated positive associations between impulsivity and addiction, which replicates prior research (Miller et al., 2017; Murphy et al., 2014). Contrary to hypotheses, we found no evidence that stress and impulsivity interacted to predict addictive behaviors. Lastly, in exploratory analyses, we found that mismatching levels of stress between childhood and recent life were related to greater reports of food addiction in young adulthood.
In exploratory analyses, we investigated whether the timing of life stress exposure was associated with addictive behaviors. We found that food addiction was related to both early and adulthood life stress exposure, whereas alcohol-related behavior was specifically associated with adulthood life stress exposure. Note that the age range of our participants was 18 to 25 years and so for many of them, adulthood stress may also be characterized as recent stress.
At least four prominent conceptual models have been proposed to explain the impact of stress timing on health and behavior – namely, the cumulative, biological-embedding, stress sensitization, and mismatch hypothesis life stress models (Del Giudice et al., 2010; Hostinar et al., 2015; Lovallo, 2013; Young et al., 2019). These models make different predictions based on the timing of stress exposure across the lifespan and the impact that stress has on health. Our results with alcohol-related behavior as the outcome are most consistent with the mismatch hypothesis. In particular, the highest food addiction scores were reported among those with mismatching levels of childhood versus recent life stress. Although bivariate associations may have been taken to support the sensitization model – which suggests that greater early life stress and greater recent life stress exposure are related to more negative health outcomes – the full results more strongly support the mismatch hypothesis (Nederhof and Schmidt, 2012; Paquola et al., 2017), which posits that mismatching levels of stress during childhood compared to recent life stress result in more negative outcomes.
Differences in early life programming, coupled with a mismatch between early life and recent stress exposure may lead to different patterns of stress-related health outcomes in adulthood (Nederhof and Schmidt, 2012). Such early life programming may account for trait differences in eating behavior that are subsequently impacted by exposure to stress at different points in life. These trait and state effects may result in the specific mismatching pattern that we observed with eating behavior (higher early life stress and higher later life stress associated with lower reports of food addiction). Furthermore, increases or decreases in food intake are often reported in response to stress or mood disorders (Konttinen et al, 2019; Sinha, 2018). Such deviations from ‘normal’ food intake represents an aberrant pattern regardless of whether it is an increase or decrease in eating behavior. Future research should specifically focus on relations among food addiction, trait factors such as personality, and state factors such as stress exposure to better understand the impact of these factors on eating behaviors.
Results of this study suggest important nuances in how stress exposure relates to addictive behaviors. In contrast to predictions from several theoretical models (i.e. the early life stress, cumulative, and sensitization models), only adulthood life stress exposure was significantly associated with alcohol-related consequences in young adults. Furthermore, there was support for the early life stress model (i.e. biological-embedding), the cumulative life stress model (i.e. allostatic load), and the mismatch hypothesis in predicting food addiction, but not for the sensitization model. Overall, differential patterns between stress and addiction were observed when comparing food and alcohol addiction.
What might explain this differential pattern of associations between stress and these outcomes? First, alcohol-related behavior may be driven less by stress and more by peer contexts (i.e. college) and the availability of alcohol on college campuses for younger, college-aged adults (Smith et al, 2019). Food addictive behavior, by contrast, may be more sensitive to stress due to accessibility of food at all ages – and in more situations than alcohol. This may allow food to become a coping mechanism that helps individuals regulate their emotions at a younger age (Wenzel et al., 2020). Similarly, the positive relation between impulsivity and alcohol behavior, but not eating behavior, may reflect the relatively lower social desirability of and greater difficulty in concealing alcohol behavior than eating behavior. Those who are more impulsive may be less likely to be influenced by such social norms as compared to those with lower impulsivity (Pérez-Fuentes et al., 2020). This relationship may be especially salient in our sample of younger adults as compared to older adults.
Given these results, we believe that future models of life stress should take stressor exposure timing into account when conceptualizing the different ways in which life stress impacts behavior. Likewise, it will be important to assess different aspects of life stress exposure in studies of stress and health to better understand how different stressors and periods of life stress exposure predict health and behavior. In addition, open access to data will assist researchers wanting to test other stress-related contingencies (e.g. stress type, stress duration) as well as different age cut points for stress models than those already published.
This study has several strengths. First, the study, its analyses, and hypotheses were preregistered and made available on the Open Science Framework website prior to data collection. Second, the study was well-powered to detect small-to-moderate effect sizes based on prior research using the STRAIN. Third, well-validated and reliable measures were used to assess life stress, impulsivity, and addictive behavior. Finally, inclusion and exclusion criteria were purposefully liberal in order to improve the generalizability of the findings.
Several limitations should also be noted. First, we sampled college students who were limited diversity in terms of age, gender, race, and ethnicity. This population reports high levels of both eating disorders (Merikangas et al., 2010) and negative consequences of alcohol (Arria et al., 2016), and so is therefore a critical population to study in its own right. Nevertheless, additional research is needed to examine the generalizability of the present results to other populations. Second, although self-report measures may be more reliable than some behavioral measures for assessing trait impulsivity (Enkavi et al., 2019), self-report measures of food and drinking behavior, and also of life stress exposure, are retrospective and can be subject to self-report biases. Future research employing other behavioral assessments of impulsivity and risk-taking behavior, and investigator-based assessments of life stress exposure, would thus be valuable. Third, because this was a cross-sectional study, additional longitudinal research is needed to examine the temporal ordering of the relations described here, and to address issues of causation and help elucidate the psychological and biological mechanisms underlying the effects observed.
Notwithstanding these limitations, the present data demonstrate for the first time that there are specific associations between lifetime stress exposure, impulsivity, and addictive behavior in emerging young adults. These results may thus help inform the development of more nuanced models of life stress and addictive behavior that take timing of stress exposure into account. In addition, these data may help to identify young adults who are at the greatest risk for engaging in addictive or risky behaviors. Looking forward, additional research is needed to replicate these effects in other samples and populations, to confirm the temporal ordering of effects described here, and to elucidate the multi-level mechanisms underlying these effects.
Public Health Significance Statement.
This study revealed that the timing of life stress exposure (e.g. early life versus recent stress exposure) is associated with different patterns of addictive behavior – namely, food addiction and alcohol use – in young adulthood.
Acknowledgements
The authors would like to thank the many research assistants who helped collect these data and presented preliminary results at conferences.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: GMS was supported by a Society in Science - Branco Weiss Fellowship, NARSAD Young Investigator (Grant No. #23958) from the Brain & Behavior Research Foundation, and National Institutes of Health (Grant No. K08 MH103443) to GMS. These organizations were in no way involved with design or conduct of the study, or the decision to write this article or submit it for publication.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data Accessibility
Data, preregistered hypotheses, and code for preregistered analyses are posted on the Open Science Framework under the Stress, Addictive Behavior, & Impulsivity project: https://osf.io/uamd8/
References
- Allen KL, Byrne SM, Oddy WH, et al. (2013) Early onset binge eating and purging eating disorders: Course and outcome in a population-based study of adolescents. Journal of Abnormal Child Psychology 41(7): 1083–1096. [DOI] [PubMed] [Google Scholar]
- Amlung M and MacKillop J (2014) Understanding the effects of stress and alcohol cues on motivation for alcohol via behavioral economics. Alcoholism: Clinical and Experimental Research 38(6): 1780–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, Allen HK, et al. (2016) Drinking like an adult? Trajectories of alcohol use patterns before and after college graduation. Alcoholism: Clinical and Experimental Research 40(3): 583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan TW, McMullin SD, Baxley C, et al. (2020a) Stress and gambling. Current Opinion in Behavioral Sciences 31: 8–12. [Google Scholar]
- Buchanan TW, McMullin SD, Mulhauser K, et al. (2020b) Diurnal cortisol and decision making under risk in problem gambling. Psychology of Addictive Behaviors 34(1): 218–229. [DOI] [PubMed] [Google Scholar]
- Carroll D, Ginty AT, Whittaker AC, et al. (2017) The behavioural, cognitive, and neural corollaries of blunted cardiovascular and cortisol reactions to acute psychological stress. Neuroscience & Biobehavioral Reviews 77: 74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cazassa MJ, Oliveira MdS, Spahr CM, et al. (2020) The stress and adversity inventory for adults (Adult STRAIN) in Brazilian Portuguese: Initial validation and links with executive function, sleep, and mental and physical health. Frontiers in Psychology 10: 3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (2016) Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51) Available at: https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf
- Champely S (2018) Package ‘pwr’: Basic Functions for Power Analysis. R package version 1.2. Available at: https://cran.r-project.org/web/packages/pwr/pwr.pdf
- Clay JM, Adams C, Archer P, et al. (2018) Psychosocial stress increases craving for alcohol in social drinkers: Effects of risk-taking. Drug and Alcohol Dependence 185: 192–197. [DOI] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL and Cyders MA (2013) Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research 37(9): 1441–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA (2013) Impulsivity and the sexes: Measurement and structural invariance of the UPPS-P Impulsive Behavior Scale. Assessment 20(1): 86–97. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, et al. (2014) Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors 39(9): 1372–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daskalakis NP, Bagot RC, Parker KJ, et al. (2013) The three-hit concept of vulnerability and resilience: Toward understanding adaptation to early-life adversity outcome. Psychoneuroendocrinology 38(9): 1858–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Giudice M, Ellis BJ and Shirtcliff EA (2011) The adaptive calibration model of stress responsivity. Neuroscience and Biobehavioral Reviews 35(7): 1562–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enkavi AZ, Eisenberg IW, Bissett PG, et al. (2019) Large-scale analysis of test–retest reliabilities of self-regulation measures. Proceedings of the National Academy of Sciences of the United States of America 116(12): 5472–5477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espeleta HC, Brett EI, Ridings LE, et al. (2018) Childhood adversity and adult health-risk behaviors: Examining the roles of emotion dysregulation and urgency. Child Abuse & Neglect 82: 92–101. [DOI] [PubMed] [Google Scholar]
- Evenden JL (1999) Varieties of impulsivity. Psychopharmacology 146(4): 348–361. [DOI] [PubMed] [Google Scholar]
- Hallowell ES, Oshri A, Liebel SW, et al. (2019) The mediating role of neural activity on the relationship between childhood maltreatment and impulsivity. Child Maltreatment 24(4): 389–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KR, Sinha R and Potenza MN (2014) Self-reported impulsivity, but not behavioral approach or inhibition, mediates the relationship between stress and self-control. Addictive Behaviors 39(11): 1557–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy R, Fani N, Jovanovic T, et al. (2018) Food addiction and substance addiction in women: Common clinical characteristics. Appetite 120: 367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW (2010) Magnitude and prevention of college drinking and related problems. Alcohol Research & Health 33(1–2): 45–54. [PMC free article] [PubMed] [Google Scholar]
- Hodes GE and Epperson CN (2019) Sex differences in vulnerability and resilience to stress across the lifespan. Biological Psychiatry 86(6): 421–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Lachman ME, Mroczek DK, et al. (2015) Additive contributions of childhood adversity and recent stressors to inflammation at midlife: Findings from the MIDUS study. Developmental Psychology 51(11): 1630–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imperatori C, Innamorati M, Lamis DA, et al. (2016) Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse & Neglect 58: 180–190. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Strong DR and Read JP (2005) Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief young adult alcohol consequences questionnaire. Alcoholism: Clinical and Experimental Research 29(7): 1180–1189. [DOI] [PubMed] [Google Scholar]
- Kim ST, Hwang SS, Kim HW, et al. (2018) Multidimensional impulsivity as a mediator of early life stress and alcohol dependence. Scientific Reports 8(1): 4104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konttinen H, van Strien T, Männistö S, et al. (2019) Depression, emotional eating and long-term weight changes: A population-based prospective study. The International Journal of Behavioral Nutrition and Physical Activity 16(1): 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam JCW, Shields GS, Trainor BC, et al. (2019) Greater lifetime stress exposure predicts blunted cortisol but heightened DHEA responses to acute stress. Stress and Health 35(1): 15–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez C, Magidson JF, Mitchell SH, et al. (2010) Behavioral and biological indicators of impulsivity in the development of alcohol use, problems, and disorders. Alcoholism: Clinical and Experimental Research 34(8): 1334–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR (2013) Early life adversity reduces stress reactivity and enhances impulsive behavior: Implications for health behaviors. International Journal of Psychophysiology 90(1): 8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, et al. (2009) Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience 10(6): 434–445. [DOI] [PubMed] [Google Scholar]
- Mayer SE, Prather AA, Puterman E, et al. (2019) Cumulative lifetime stress exposure and leukocyte telomere length attrition: The unique role of stressor duration and exposure timing. Psychoneuroendocrinology 104: 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, et al. (2010) Lifetime prevalence of mental disorders in U.S. Adolescents: Results from the national comorbidity survey replication–adolescent supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry 49(10): 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, DiBello AM, Lust SA, et al. (2017) Impulsive personality traits and alcohol use: Does sleeping help with thinking? Psychology of Addictive Behaviors 31(1): 46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, et al. (2001) Psychiatric aspects of impulsivity. American Journal of Psychiatry 158(11): 1783–1793. [DOI] [PubMed] [Google Scholar]
- Murphy CM, Stojek MK and MacKillop J (2014) Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite 73: 45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nederhof E and Schmidt MV (2012) Mismatch or cumulative stress: Toward an integrated hypothesis of programming effects. Physiology & Behavior 106(5): 691–700. [DOI] [PubMed] [Google Scholar]
- Nunes-Neto PR, Köhler CA, Schuch FB, et al. (2018) Food addiction: Prevalence, psychopathological correlates and associations with quality of life in a large sample. Journal of Psychiatric Research 96: 145–152. [DOI] [PubMed] [Google Scholar]
- Olvera Alvarez HA, Provencio-Vasquez E, Slavich GM, et al. (2019) Stress and health in nursing students: The nurse engagement and wellness study. Nursing Research 68(6): 453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquola C, Bennett MR, Hatton SN, et al. (2017) Utility of the cumulative stress and mismatch hypotheses in understanding the neurobiological impacts of childhood abuse and recent stress in youth with emerging mental disorder. Human Brain Mapping 38(5): 2709–2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pegg S, Ethridge P, Shields GS, et al. (2019) Blunted social reward responsiveness moderates the effect of lifetime social stress exposure on depressive symptoms. Frontiers in Behavioral Neuroscience 13: 178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Fuentes MDC, Molero Jurado MDM, Gázquez Linares JJ, et al. (2020) Individual variables involved in perceived pressure for adolescent drinking. International Journal of Environmental Research and Public Health 17(6): 2012–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivarunas B and Conner BT (2015) Impulsivity and emotion dysregulation as predictors of food addiction. Eating Behaviors 19: 9–14. [DOI] [PubMed] [Google Scholar]
- R Core Team (2019) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. Available at: https://www.R-project.org/ [Google Scholar]
- Schulte EM and Gearhardt AN (2017) Development of the modified Yale food addiction scale version 2.0. European Eating Disorders Review 25(4): 302–308. [DOI] [PubMed] [Google Scholar]
- Shin SH, Lee S, Jeon SM, et al. (2015) Childhood emotional abuse, negative emotion-driven impulsivity, and alcohol use in young adulthood. Child Abuse & Neglect 50: 94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT and McEwen BS (2009) Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. Journal of the American Medical Association 301(21): 2252–2259. [DOI] [PubMed] [Google Scholar]
- Sinha R (2018) Role of addiction and stress neuro-biology on food intake and obesity. Biological Psychology 131: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R and Jastreboff AM (2013) Stress as a common risk factor for obesity and addiction. Biological Psychiatry 73(9): 827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM (2016) Life stress and health: A review of conceptual issues and recent findings. Teaching of Psychology 43(4): 346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM (2019) Stressnology: The primitive (and problematic) study of life stress exposure and pressing need for better measurement. Brain, Behavior, and Immunity 75: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM and Shields GS (2018) Assessing lifetime stress exposure using the Stress and Adversity Inventory for Adults (Adult STRAIN): An overview and initial validation. Psychosomatic Medicine 80(1): 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RL, Salvatore JE, Aliev F, et al. (2019) Genes, roommates, and residence halls: A multidimensional study of the role of peer drinking on college students’ alcohol use. Alcoholism: Clinical and Experimental Research 43(6): 1254–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturmbauer SC, Shields GS, Hetzel EL, et al. (2019) The Stress and Adversity Inventory for Adults (Adult STRAIN) in German: An overview and initial validation. PLoS One 14(5): e0216419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Bechara A, Recknor EC, et al. (2007) Negative emotion-driven impulsivity predicts substance dependence problems. Drug and Alcohol Dependence 91(2–3): 213–219. [DOI] [PubMed] [Google Scholar]
- Wardell JD, Strang NM and Hendershot CS (2016) Negative urgency mediates the relationship between childhood maltreatment and problems with alcohol and cannabis in late adolescence. Addictive Behaviors 56: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wemm SE and Sinha R (2019) Drug-induced stress responses and addiction risk and relapse. Neurobiology of Stress 10: 100148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel KR, Weinstock J and McGrath AB (2020) The clinical significance of food addiction. Journal of Addiction Medicine. Epub ahead of print 31 January 2020. DOI: 10.1097/ADM.0000000000000626. [DOI] [PubMed] [Google Scholar]
- Young ES, Farrell AK, Carlson EA, et al. (2019) The dual impact of early and concurrent life stress on adults’ diurnal cortisol patterns: A prospective study. Psychological Science 30(5): 739–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Z, Indelicato NA, Fuglestad P, et al. (2018) Sex differences in disordered eating and food addiction among college students. Appetite 129: 12–18. [DOI] [PubMed] [Google Scholar]
- Zhu H, Luo X, Cai T, et al. (2016) Life event stress and binge eating among adolescents: The roles of early maladaptive schemas and impulsivity. Stress and Health 32(4): 395–401. [DOI] [PubMed] [Google Scholar]


