Abstract
Background: Most maternal deaths in the world occur during the postpartum period, especially within the first two days following delivery. This makes postnatal care (PNC) critical to improving the chances of maternal and child survival. Over the past 20 years, the proportion of women receiving antenatal care (ANC) in Ethiopia has increased while the proportion of those receiving PNC has remained low. This study aimed to understand the trends, determinants and urban–rural variations of PNC service utilisation. Methods: This study draws on the Ethiopian Demographic and Health Survey (EDHS) data for the years 2000 (n = 4552), 2005 (n = 4467), 2011 (n = 4445) and 2016 (n = 4275) to estimate the trends and determinants of PNC service utilisation. Multivariate logistic regression models with adjustment for clustering and sampling weights were used to investigate the association between the independent factors, the study factors and PNC service utilisation. Results: Over the twenty-year period of the EDHS, the proportion of Ethiopian women who received PNC services increased from 5.6% (95% CI: 4.6–6.9%) in 2000 to 18.5% (95% CI: 16.4–20.7%) in 2016. Similarly, women who received PNC services in urban areas increased from 15.2% (95% CI: 23.6–30.7%) in 2000 to 47% (95% CI: 60.4–67.3%) in 2016. Women who were in the wealthy quintile, had ANC visits, delivered in a health facility, and delivered by caesarean section were most likely to have PNC. The present study also showed that whilst birth spacing was a significant factor among urban women, wealth index, ANC visits, and perception of health facility distance were significant factors among rural women. Conclusions: The study suggests low levels of utilisation of PNC among Ethiopian women from rural districts. Geographically targeted interventions with a focus on low-socioeconomic rural women, and those with no previous contacts with the health system during pregnancy, are needed to improve PNC in Ethiopia.
Keywords: postnasal care, urban–rural variation, Ethiopia, Demographic and Health Survey
1. Introduction
Ethiopia is the second most populous country in Africa and has one of the highest rates of maternal mortality (401 deaths/100,000 live births in 2017) in the world [1,2,3]. Past research shows that most maternal deaths occur in the postpartum period as a result of haemorrhage, hypertensive disorders of pregnancy, abortion and sepsis [1]. Maternal mortality is a preventable global tragedy and proven and cost-effective interventions such as antenatal care (ANC), skilled delivery and postnatal care (PNC) have been reported to reduce morbidity and mortalities related to pregnancy and childbirth [4]. For instance, Bhutta and colleagues suggest that the provision of quality and effective care for women delivering in facilities could prevent an estimated 113,000 maternal deaths [5].
According to World Health Organization (WHO), a majority of maternal deaths in the world occur during the postpartum period, especially within the first two days after delivery, that makes the postnatal period critical to improving maternal and child survival [6]. The postpartum period is the period beginning 1 h after the delivery of the placenta and continuing until 6 weeks (42 days) after delivery [7]. Early PNC provides a window of opportunity for the identification and management of complications that may occur at the time of labour, delivery or immediately after delivery [7]. Health care providers will also counsel the mother about maternal nutrition, breastfeeding, immunisation and other childcare services. Furthermore, stress relieving psychological and emotional supports can also be provided [7,8].
Over the past 25 years, several programs have been developed and implemented to improve maternal health service utilisation in Ethiopia. Even though the proportion of women receiving ANC in Ethiopia is high [9], the proportion of women delivering by the assistance of a skilled attendant and having PNC remained low [10,11]. Research indicates that factors across individual through to health system levels contribute to this disparity between ANC and PNC. For instance, the 2011 Ethiopian Demographic and Health Survey (EDHS) revealed that fewer mothers living in rural areas received PNC compared to those living in urban areas (3% vs. 32%) [12]. According to Koblinsky and colleagues [13], the traditional home confinement of women after childbirth in Ethiopia contributes to the low use of PNC services. Others also reported significant regional variations in the use of ANC in Ethiopia with low levels reported in Somali, Oromia, Gambella and Southern Nations, Nationalities, and People’s Region (SNNPR) [14]. These findings imply the need for national and regional level interventions that target individual women, their families and surrounding communities as well as health care professionals and the wider health care system to improve the utilisation of maternity care services in Ethiopia.
There have been some studies that examined why PNC service utilisation remains low in Ethiopia. Some of these studies had a small sample size [15,16] and others covered a very small geographical area [17,18] that may put the representativeness of the studies and generalisability of the findings into question. Although there have been four rounds of the EDHS, studies that used these data have concentrated on the 2016 survey [19,20]. This makes investigating the determinants of PNC use in Ethiopia using the four nationally representative and relatively large sample surveys critical to identifying possible interventions. Results of this analysis can inform interventions that aim to improve the implementation and utilisation of maternal health services in Ethiopia and achieve the sustainable development goal 3 (SDG goal 3) of reducing the global maternal mortality ratio to less than 70 per 100,000 live births by 2030 [21]. According to WHO, this goal can be achieved by improving access to quality reproductive and maternal health services, ensuring universal health coverage for comprehensive reproductive and maternal health care, and addressing all causes of maternal morbidity and mortality [4]. Therefore, this study aimed to (1) examine the trends of PNC utilisation; (2) identify factors associated with the use of PNC, and (3) compare urban–rural variations of PNC use.
2. Materials and Methods
2.1. Data
The 2000–2016 EDHS data were used. EDHS is designed to estimate key national level population, health and nutrition indicators for program planning, monitoring and evaluation. Main advantages of EDHS data include high sample size and response rate, coverage of all regions and city administrations, and high standard data collection tools [22]. In the present study, a total of 17,740 (4552 in 2000, 4467 in 2005, 4445 in 2011 and 4275 in 2016) responses were analysed. All analysis was weighted to ensure actual representativeness of the data and to allow us draw nationally generalisable conclusions. Weighting was needed because some areas were oversampled to produce estimates for all the nine regions and two city administrations.
2.2. Study Setting
The Federal Democratic Republic of Ethiopia has nine regional states, two city administrations, 611 weredas (districts) and 15,000 kebeles. Regions are divided into zones, and zones, into administrative units called weredas. Each wereda is further subdivided into the lowest administrative unit called kebele (Population Census Commission, 2008). Ethiopia is the second most populous nation in Africa, with nearly 115 million people based on the 2019 United Nations estimate, after Nigeria with over 180 million people [23]. Males represent 50.5% of the population and females 49.5, with 21% being of reproductive age (15–49 years). Although health service coverage reaches 92% of the population, the utilisation of maternal healthcare services is low. The 2016 EDHS indicated that 62% of pregnant women received ANC, 26% of pregnant women delivered in a health facility, and 17% received PNC [24]. About 25% and 35% of all reproductive age women and married women use contraception, respectively.
2.3. Outcome Variable
The utilisation of postnatal care is the outcome variable in this study. PNC attendance (utilisation) was defined in this study as having at least one visit within the first 42 days (six weeks) of birth [25]. In the survey, this question was asked: After you gave birth, did anyone check on your health?” Response options included: “Yes” and “No”, to determine if the mother had attended any PNC visitor check-ups [24]. From the response, we used Yes = 1, and No = 0 for our analysis.
2.4. Independent Variables
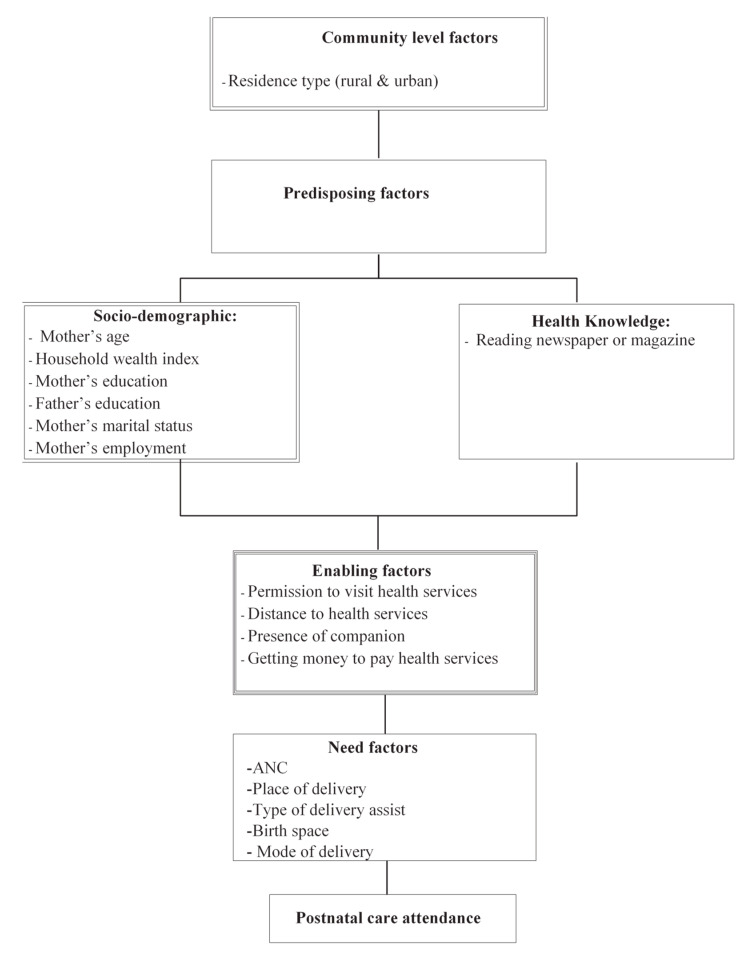
Independent variables in this study were chosen based on previous research on the topic [26]. Anderson’s behavioural framework [27] (see Figure 1) was used to organise the determinants of PNC utilisation. The factors assumed to influence the use of PNC were categorised into four main factors: community level, predisposing, enabling and need factors. Community level factors include geopolitical zone and residence type. Predisposing (socio-demographic and health knowledge factors) include maternal age, household wealth index, maternal and paternal education, marital and employment statuses and reading magazine or newspaper. Need factors include contraceptive use and future plan to have a child. Variables such as permission to visit health services, distance from health services, presence of companion and getting money to pay for health services are categorised as enabling factors.
Figure 1.
Conceptual framework.
2.5. Statistical Analysis
The analysis started with the calculation of simple frequencies and percentages for study variables for the total population, urban and rural residence location groups. A series of frequencies and cross tabulations were conducted to estimate the prevalence of PNC service by the study factors for the three locations. Univariate logistic regression analysis was conducted to examine factors associated with PNC service in Ethiopia and rural–urban differences. Variables with p value < 0.05 in univariate models were entered into multivariate models. Crude and adjusted odds ratios (ORs) and their 95% confidence intervals were reported in the present study for location groups. All analyses were performed using the “svy” command for calculation of counts and percentages in Stata 15.0 (Stata Corporation, College Station, TX, USA) to adjust for sampling weight, clustering and stratification.
2.6. Ethics
This study used secondary data made publicly available by ICF International and the EDHS. The authorisation for using the data in the current study was granted from the DHS program upon presenting the aims of the study and the research plan. Detailed information on the data collection procedures employed by EDHS has been published as a full report elsewhere [12,24].
3. Results
3.1. Background Characteristics of the Study Population
The study included a total weighted sample of 17,740 reproductive age women representing the nine regions and two city administrations of Ethiopia. The majority (72%) had no formal education and low (60.2%) wealth status. Nearly half (48%) of the participants were between 25 and 34 years. During their last pregnancy 30.9% of the women had ANC visits and the majority (85%) gave birth at home. Over two-thirds of the women (69.9%) reported that distance from a health facility is a big problem to access services (Table 1).
Table 1.
Prevalence of postnatal care by study factors in Ethiopia (Ethiopian Demographic and Health Survey (EDHS)) 2000–2016.
| Total Population | Urban | Rural | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | N | Prevalence (95%CI) | p Value | N | Prevalence (95%CI) | p Value | N | Prevalence (95%CI) | p Value |
| PNC Yes |
1744 | 9.82(9.03–10.6) | p < 0.001 | 636 | 9.8(9.03–10.6) | p < 0.001 | 1107 | 6.24(5.6–6.90) | p < 0.001 |
| No | 15,997 | 90.17(89.3–90.9) | p < 0.001 | 1132 | 90.17(89.3–90.9) | p < 0.001 | 14,864 | 90.17(89.3–90.9) | p < 0.00 |
| Predisposing factors | |||||||||
| Maternal education | |||||||||
| No education | 12,799 | 72 (72.5–73.6) | p < 0.001 | 575 | 32.5(28.5–36.8) | p < 0.001 | 12,223 | 76.5(75–78) | p < 0.001 |
| Primary | 4029 | 22.7(21.4–24.3) | 609 | 34.4(31–37.9) | 3421 | 21.4(20–23) | |||
| Secondary | 912 | 5.1(4.5–5.8) | 584 | 33(29.5–36.6) | 328 | 2(1.7–2.4) | |||
| Maternal working status | |||||||||
| Not working | 9753 | 57.8(55.9–59.6) | p < 0.001 | 902 | 51.2(46.8–55.5) | p = 0.142 | 8851 | 58.5(56.5–60.6) | p < 0.01 |
| Professional | 2146 | 12.7(11.6–13.8) | 604 | 34.2(30–38.7) | 1543 | 10(9.1–11.3) | |||
| Agricultural | 4968 | 29.4(27.6–31.3) | 256 | 14.5(11.2–18.6) | 4713 | 31(29.2–33.2) | |||
| Partner education | |||||||||
| No education | 9615 | 54.5(52.8–56.2) | p < 0.001 | 391 | 22.2(19.4–25.3) | p < 0.001 | 9224 | 58(56.3–59.8) | p < 0.001 |
| Primary | 6116 | 34.6(33.1–36.2) | 559 | 31.8(28.4–35.5) | 5557 | 35(33.3–36.6) | |||
| Secondary | 1906 | 10.8(9.9–11.7) | 805 | 45.8(41.9–49.8) | 1100 | 7(6.2–7.6) | |||
| Partner working status | |||||||||
| Not working | 567 | 3.25(2.7–3.8) | p < 0.001 | 91 | 5.3(3.7–7.5) | p = 0.052 | 477 | 3(2.4–3.6) | p < 0.001 |
| Professional | 1856 | 10.6(9.7–11.6) | 841 | 49.6(45.9–53.3) | 1015 | 6.4(5.8–7.1) | |||
| Agricultural | 14,990 | 86(84.9–87.1) | 762 | 45(41–48.9) | 14,227 | 90.5(89–91) | |||
| Household wealth index | |||||||||
| Poor | 10,289 | 60.2(58–62) | p < 0.001 | 110 | 6.5(4.6–9.19) | p < 0.001 | 10,179 | 66(63.9–68) | p < 0.001 |
| Middle | 4584 | 26.8(25.2–28.5) | 224 | 13.4(10.3–17.1) | 4360 | 28.2(26.5–30) | |||
| Rich | 2210 | 12.9(11.6–14.3) | 1338 | 80(76–83.5) | 871 | 5.6(4.8–6.5) | |||
| Mother’s age | |||||||||
| 15–24 | 5595 | 31.5(30.4–32.6) | p = 0.014 | 523 | 29.5(26–33.2) | p = 0.017 | 5072 | 31.7(30–32) | p = 0.189 |
| 25–34 | 8521 | 48(46.8–49.2) | 978 | 55.3(51.9–58.6) | 7543 | 47.2(46–48) | |||
| 35–49 | 3624 | 20.4(19.5–21.3) | 267 | 15(13.2–17.2) | 3356 | 21(20–22) | |||
| Marital status | |||||||||
| Never married | 109 | 0.61(0.46–0.81) | p = 0.003 | 33 | 1.86([1.2–2.8) | p = 0.209 | 76 | 0.47(0.33–0.67) | p = 0.040 |
| Currently married | 16,720 | 94.2(93.6–94.8) | 1579 | 89.3(86.6–91.5) | 15,140 | 94(94–95) | |||
| Formerly married | 911 | 5.13(4.6–5.7) | 156 | 8.8(6.7–11.3) | 755 | 4.7(4.2–5.3) | |||
| Reading magazine | |||||||||
| Yes | 358 | 7.79(7.12–8.51) | p < 0.001 | 261 | 14.9(12.4–17.8) | p < 0.001 | 94 | 0.59(0.44–0.79) | p < 0.001 |
| No | 1382 | 2.02(1.70–2.38) | 371 | 21(17.8–24.4) | 1011 | 6.33(5.71–7.01) | |||
| Need factors | |||||||||
| ANC visit | |||||||||
| None | 10,796 | 61(59.1–62.8) | p < 0.001 | 459 | 26.1(21.6–31.1) | p < 0.001 | 10,337 | 64.8(62.9–66.6) | p < 0.001 |
| 1–3 | 3901 | 22(20.9–23.2) | 436 | 24.8(21.4–28.5) | 3465 | 21.7(20.5–22.9) | |||
| Four or more | 3001 | 16.9(15.7–18.2) | 862 | 49(44.1–53.9) | 2140 | 13.4(12.2–14.6) | |||
| Place of delivery | |||||||||
| Home | 15,354 | 86.5(85–87.8) | p < 0.001 | 797 | 45(39.1–51) | p < 0.001 | 14,558 | 91(89.8–92.3) | p < 0.001 |
| Health facility | 2385 | 13.4(12.1–14.9) | 971 | 54.9(48.9–60.8) | 1414 | 8.8(7.7–10.1) | |||
| Type of delivery assist | |||||||||
| Health professional | 2468 | 13.9(12.5–15.3) | p < 0.001 | 1008 | 57(50.9–62.8) | p < 0.001 | 1461 | 9.1(7.9–10.4) | p < 0.001 |
| Traditional birth attendant (TBA) | 5493 | 30.9(29–32.8) | 362 | 20.4(16.4–25.2) | 5131 | 32(30.2–34) | |||
| Other non-health professional | 9779 | 55.1(53–57.1) | 398 | 22.5(18.6–26.9) | 9380 | 58(56–60) | |||
| Birth interval | |||||||||
| No previous birth | 3273 | 18.4(17.6–19.3) | p < 0.001 | 531 | 30.1(26.6–33.9) | p = 0.005 | 2741 | 17.1(16.3–18.03) | p < 0.001 |
| <24months | 2378 | 13.4(12.5–14.3) | 181 | 10.2(8.4–12.3) | 2197 | 13.7(12.8–14.7) | |||
| ≥24 months | 12,074 | 68(67–69) | 1050 | 59.5(55.5–63.5) | 11,024 | 69.0(67.9–70.1) | |||
| Enabling factors | |||||||||
| Accompany for medical help | |||||||||
| Big problem | 7798 | 59.1(57.2–61) | p < 0.001 | 483 | 33.1(29.1–37.3) | p = 0.138 | 7315 | 62.3(60.3–64.3) | p < 0.001 |
| Not a big problem | 5388 | 40.8(38.9–42.7) | 976 | 66.8(62.6–70.8) | 4412 | 37.6(35.6–39.6) | |||
| Distance from the health facility | |||||||||
| Big problem | 9226 | 69.9(67.9–71.8) | p < 0.001 | 402 | 27.6(23.9–31.6) | p = 0.013 | 8823 | 75.2([73.3–77.06) | p < 0.001 |
| Not a big problem | 3959 | 30(28.1–32) | 1054 | 72.3(68.4–76.03) | 2905 | 24.7(22.9–26.6) | |||
| Permission for medical help | |||||||||
| Big problem | 4790 | 36.3(34.4–38.3) | p < 0.001 | 260 | 17.8(14.4–21.7) | p = 0.234 | 4530 | 38.6([36.5–40.7) | p = 0.003 |
| Not a big problem | 8394 | 63.6(61.7–65.5) | 1195 | 82.16(78.2–85.5) | 7199 | 61.3(59.2–63.4) | |||
3.2. Utilisation of PNC Services in Ethiopia
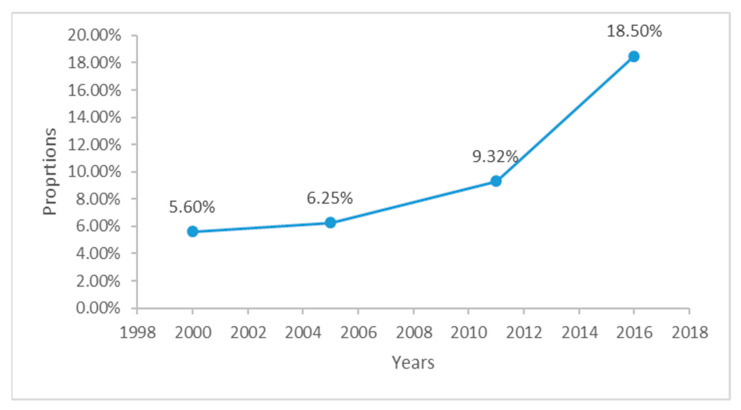
The analysis revealed that the use of PNC services increased from 5.6% to 18.5% over the 20-year period of the EDHS (Figure 2).
Figure 2.
Trends of postnatal care (PNC) utilisation in Ethiopia (EDHS) 2000–2016.
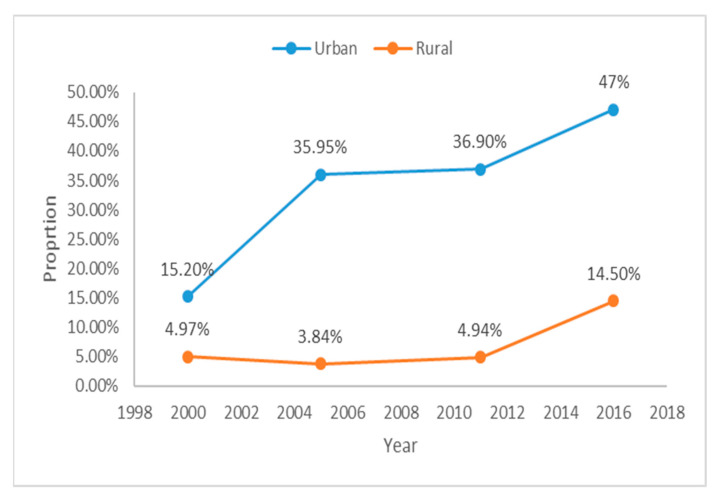
A significant variation in the use of PNC services between urban and rural areas was also identified. Whilst PNC use increased from 15.2% to 47% in Urban areas (Figure 3), the increase in rural areas was observed mainly during the 2016 survey.
Figure 3.
Trends of PNC in urban and rural women of Ethiopia (EDHS) 2000–2016.
3.3. Determinants of PNC in Ethiopia
Multivariate analysis revealed several factors that influence the use of PNC in Ethiopia (Table 2). From 2000 to 2016, mothers who had ANC visits during pregnancy were more likely to utilise PNC services as well. This association is positive for those women who had 1–3 (OR = 1.9, 95% CI [1.36–2.66] Table 3) and 4+ ANC visits (OR = 3.01, 95% CI [2.15–4.21]). The likelihood of having PNC was higher among urban women (OR = 2.99, 95% CI [1.43–3.45]) and those who delivered their babies by a caesarean section (OR = 4.3, 95% CI [2.39–7.71]). Health facility delivery was the other factor that significantly influenced the chance of women receiving PNC care with those women who delivered their babies in health facilities were about 2.5 times more likely to have PNC care (OR = 2.5, 95% CI [1.04–6.25]) compared to women who delivered at home. Over the 20-year period, mothers in the high-wealth quintile had higher odds of receiving PNC care compared with those who were from low socioeconomic households (OR = 1.57; 95% CI [1.12, 2.20]). Furthermore, mothers whose husbands had professional or semi–professional jobs were highly likely to utilise PNC services after the delivery of their babies (OR = 1.52; 95% CI [1.00, 2.34]). Finally, women who perceived that “distance from a health facility is not a big problem” were significantly likely to have engaged with PNC services (OR = 1.29; 95% CI [1.02, 1.62]).
Table 2.
Determinants of PNC use in Ethiopia (EDHS) 2000–2016 (n = 17,740).
| Variables | Unadjusted OR | 95%CI | p Value | Adjusted OR | 95%CI | p Value |
|---|---|---|---|---|---|---|
| Predisposing Factors | ||||||
| Maternal education | ||||||
| No education | 1.00 | |||||
| Primary | 2.57 | 2.16–3.05 | p < 0.001 | 0.95 | 0.72–1.26 | p = 0.75 |
| Secondary | 11.8 | 9.50–14.7 | p < 0.001 | 1.19 | 0.80–1.77 | p = 0.388 |
| Maternal Working status | ||||||
| Not working | 1.00 | |||||
| Professional | 2.33 | 1.92–2.84 | p < 0.001 | 1.02 | 0.77–1.35 | p = 0.869 |
| Agricultural | 0.78 | 0.64–0.94 | p = 0.013 | 1.13 | 0.87–1.48 | p = 0.335 |
| Residence | ||||||
| Rural | 1.00 | |||||
| Urban | 6.77 | 4.22–9.65 | p < 0.001 | 2.99 | 1.43–3.45 | p = 0.003 |
| Father’s education | ||||||
| No education | 1.00 | |||||
| Primary | 1.53 | 1.28–1.83 | p < 0.001 | 0.96 | 0.74–1.25 | p = 0.781 |
| Secondary | 5.27 | 4.36–6.37 | p < 0.001 | 0.86 | 0.62–1.20 | p = 0.399 |
| Father’s working status | ||||||
| Not working | 1.00 | |||||
| Professional | 1.57 | 1.07–2.31 | p = 0.020 | 1.52 | 1.000094–2.34 | p = 0.050 |
| Agricultural | 0.37 | 0.26–0.53 | p < 0.001 | 1.32 | 0.904–1.943 | p = 0.149 |
| Household wealth index | ||||||
| Poor | 1.00 | |||||
| Middle | 1.92 | 1.58–2.33 | p < 0.001 | 1.25 | 0.970–1.628 | p = 0.083 |
| Rich | 7.71 | 6.34–9.38 | p < 0.001 | 1.57 | 1.12–2.20 | p = 0.008 |
| Mother’s age | ||||||
| 15–24 | 1.00 | |||||
| 25–34 | 1.07 | 0.91–1.26 | p = 0.349 | 1.042 | 0.784–1.385 | p = 0.774 |
| 35–49 | 0.80 | 0.65– 0.99) | p = 0.046 | 0.832 | 0.573–1.220 | p = 0.338 |
| Need factors | ||||||
| ANC visit | ||||||
| None | 1.00 | |||||
| 1–3 | 4.22 | 3.40–5.25 | p < 0.001 | 1.911 | 1.36–2.66 | p < 0.001 |
| Four or more | 12.1 | 9.92–14.9 | p < 0.001 | 1.10 | 2.15–4.21 | p < 0.001 |
| Place of delivery | ||||||
| Home | 1.00 | |||||
| Health facility | 22.8 | 18.8–27.6 | p < 0.001 | 2.56 | 1.048–6.25 | p = 0.039 |
| Type of delivery assist | ||||||
| Health professional | 1.00 | |||||
| TBA | 0.06 | 0.05–0.08 | p < 0.001 | 0.218 | 0.085–0.559 | p = 0.002 |
| Other non-health professional | 0.02 | 0.02– 0.03 | p < 0.001 | 0.149 | 0.058–0.383 | p < 0.001 |
| Birth interval | ||||||
| No previous birth | 1.00 | |||||
| <24months | 0.34 | 0.26–0.44 | p < 0.001 | 0.75 | 0.477–1.194 | p = 0.230 |
| ≥24 months | 0.56 | 0.48–0.66 | p < 0.001 | 1.28 | 0.919–1.795 | p = 0.141 |
| Enabling factors | ||||||
| Accompany for medical help | ||||||
| Big problem | 1.00 | |||||
| Not a big problem | 2.29 | 1.93–2.72 | p < 0.001 | 0.99 | 0.786–1.268 | p = 0.991 |
| Distance from the health facility | ||||||
| Big problem | 1.00 | |||||
| Not a big problem | 3.68 | 3.14–4.32 | p < 0.001 | 1.29 | 1.02–1.61 | p = 0.028 |
| Permission for medical help | ||||||
| Big problem | 1.00 | |||||
| Not a big problem | 1.79 | 1.48–2.17 | p < 0.001 | 0.92 | 0.705–1.208 | p = 0.563 |
Table 3.
Determinants of PNC use in urban and rural Ethiopia (EDHS) 2000–2016 (n = 17,740).
| Urban Residence | Rural Residence | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Unadjusted OR | 95%CI | p Value | Adjusted OR | 95%CI | p Value | Unadjusted OR | 95%CI | p value | Adjusted OR | 95%CI | p Value |
| Predisposing factor | ||||||||||||
| Maternal education | ||||||||||||
| No education | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Primary | 1.80 | 1.20–2.69 | p = 0.004 | 0.63 | 0.35–1.13 | p = 0.125 | 2.16 | 1.7–2.6 | p < 0.001 | 1.06 | 0.77–1.4 | p = 0.72 |
| Secondary | 4.00 | 2.73–5.85 | p < 0.001 | 0.89 | 0.50–1.59 | p = 0.711 | 6.47 | 4.3–9.5 | p < 0.001 | 1.29 | 0.6–2.4 | p = 0.44 |
| Maternal Working status | ||||||||||||
| Not working | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Professional | 1.27 | 0.91–1.79 | p = 0.156 | 1.08 | 0.69–1.70 | p = 0.714 | 1.73 | 1.32–2.26 | p < 0.001 | 0.97 | 0.69–1.37 | p = 0.90 |
| Agricultural | 0.74 | 0.41–1.31 | p = 0.305 | 1.16 | 0.57–2.35 | p = 0.680 | 0.93 | 0.75–1.15 | p = 0.524 | 1.12 | 0.84–1.49 | p = 0.423 |
| Father’s education | ||||||||||||
| No education | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Primary | 1.64 | 1.07–2.51 | p = 0.023 | 1.17 | 0.63–2.16 | p = 0.610 | 1.29 | 1.05–1.57 | p = 0.012 | 0.92 | 0.68–1.23 | p = 0.581 |
| Secondary | 2.92 | 2.07–4.11 | p < 0.001 | 1.37 | 0.76–2.46 | p = 0.291 | 2.45 | 1.83–3.28 | p < 0.001 | 0.72 | 0.47–1.10 | p = 0.132 |
| Father’s working status | ||||||||||||
| Not working | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Professional | 0.56 | 0.29 1.08 | p =0.085 | 1.00 | 0.46–2.15 | p = 0.998 | 1.43 | 0.90–2.26 | p = 0.12 | 1.95 | 1.12–3.38 | p = 0.017 |
| Agricultural | 0.47 | 0.24–0.90 | p = 0.025 | 1.03 | 0.49–2.17 | p = 0.934 | 0.512 | 0.33–0.77 | p = 0.001 | 1.55 | 0.97–2.48 | p = 0.066 |
| Marital status | ||||||||||||
| Never married | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Formerly married | 0.69 | 0.24–1.97 | p = 0.493 | 1.05 | 0.50–2.19 | p = 0.333 | 0.416 | 0.15–1.09 | p = 0.075 | 1.40 | 0.73–2.70 | p = 0.305 |
| Currently married | 1.08 | 0.45–2.59 | p = 0.857 | 0.36 | 0.14–0.91 | p = 0.032 | ||||||
| Household wealth index | ||||||||||||
| Poor | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Middle | 2.51 | 1.00–6.29 | p < 0.001 | 1.32 | 0.411–4.25 | p = 0.083 | 1.75 | 1.43–2.14 | p < 0.001 | 1.19 | 0.90–1.57 | p = 0.201 |
| Rich | 4.25 | 1.83–9.84 | p < 0.001 | 1.43 | 0.51–3.96 | p = 0.008 | 3.62 | 2.76–4.76 | p < 0.001 | 1.85 | 1.23–2.79 | p = 0.003 |
| Mother’s age | ||||||||||||
| 15–24 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 25–34 | 1.50 | 1.06–2.11 | p = 0.020 | 1.17 | 0.70–1.95 | p = 0.774 | 0.86 | 0.70–1.05 | p = 0.150 | 1.03 | 0.71–1.49 | p = 0.873 |
| 35–49 | 0.98 | 0.62–1.55 | p = 0.961 | 0.57 | 0.25–1.29 | p = 0.338 | 0.81 | 0.63–1.03 | p = 0.096 | 0.96 | 0.62–1.49 | p = 0.888 |
| Need factors | ||||||||||||
| ANC visit | ||||||||||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 1–3 | 3.09 | 1.79–5.34 | p < 0.001 | 0.77 | 0.39–1.50 | p < 0.001 | 3.88 | 3.04–4.97 | p < 0.001 | 2.27 | 1.55–3.32 | p < 0.001 |
| Four or more | 7.73 | 4.71–12.6 | p < 0.001 | 1.78 | 0.92–3.41 | p < 0.001 | 8.58 | 6.66–11.0 | p < 0.001 | 3.27 | 2.21–4.83 | p < 0.001 |
| Place of delivery | ||||||||||||
| Home | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Health facility | 9.89 | 6.56–14.9 | p < 0.001 | 2.11 | 0.63–7.01 | p = 0.039 | 20.5 | 16.2–25.8 | p < 0.001 | 2.68 | 0.81–8.86 | p = 0.105 |
| Type of delivery assist | ||||||||||||
| Health professional | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| TBA | 0.086 | 0.05–0.14 | p < 0.001 | 0.185 | 0.053–0.648 | p = 0.008 | 0.078 | 0.06–0.10 | p < 0.001 | 0.22 | 0.06–0.76 | p = 0.017 |
| Other non-health professional | 0.084 | 0.04–0.015 | p < 0.001 | 0.181 | 0.046–0.706 | p = 0.014 | 0.031 | 0.02–0.04 | p < 0.001 | 0.14 | 0.04–0.51 | p = 0.002 |
| Birth interval | ||||||||||||
| No previous birth | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| <24months | 0.43 | 0.26–0.70 | p = 0.001 | 0.953 | 0.45–2.01 | p = 0.901 | 0.407 | 0.29–0.56 | p < 0.001 | 0.67 | 0.37–1.20 | p = 0.186 |
| ≥24 months | 0.75 | 0.54–1.03 | p = 0.079 | 1.78 | 1.08–2.95 | p = 0.023 | 0.64 | 0.52–0.79 | p < 0.001 | 1.11 | 0.71–1.72 | p = 0.634 |
| Accompany for medical help | ||||||||||||
| Big problem | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Not a big problem | 1.27 | 0.92–1.76 | p = 0.139 | 0.89 | 0.59–1.35 | p = 0.605 | 1.87 | 1.51–2.32 | p < 0.001 | 1.02 | 0.75–1.38 | p = 0.883 |
| Distance from the health facility | ||||||||||||
| Big problem | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Not a big problem | 1.53 | 1.09–2.14 | p = 0.014 | 1.18 | 0.75–1.88 | p = 0.459 | 2.60 | 2.12–3.17 | p < 0.001 | 1.35 | 1.03–1.76 | p = 0.029 |
| Permission for medical help | ||||||||||||
| Big problem | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Not a big problem | 1.32 | 0.83–2.09 | p = 0.234 | 0.66 | 0.343–1.27 | p = 0.213 | 1.39 | 1.11–1.74 | p = 0.004 | 0.97 | 0.72–1.31 | p = 0.893 |
3.4. Determinants of PNC Service Utilisation in Urban–Rural Ethiopia
Comparative multivariate analysis of the data revealed critical urban rural differences in factors that influence the use of PNC services (Table 3). Among the rural population, higher wealth increased the odds of having PNC services (AOR: 1.85, 95% CI: 1.23–2.79; p < 0.001 for wealthy category). Both rural and urban women who delivered their babies by caesarean section were more likely to have engaged with PNC services (AOR: 7.4, 95% CI: 2.51–21.68, p = 0.00 for rural and AOR: 3.5, 95% CI: 1.93–6.68, p = 0.00 for urban). Rural mothers with husbands who had a professional or semi–professional job were significantly likely to utilise PNC compared to those who had no employment (AOR: 1.96, 95% CI: 1.13–3.39, p = 0.00). The association between birth spacing of greater than 24 months and PNC service utilisation was significant for urban mothers (AOR: 1.78, 95% CI: 1.08–2.96; p < 0.001). Compared to rural women who had no ANC visits during pregnancy, those who had received ANC were significantly likely to also have PNC as well (AOR 2.28, 95% CI: 1.58–3.33, p = 0.00 for 1–3 ANC visits, and AOR 2.28, 95% CI: 1.58–3.33, p = 0.00 for 4+ visits). Distance from a health facility was another factor that showed significant association with PNC service utilisation among rural women. Those who had a perception that “distance is not a big problem” were more likely to have PNC (AOR 1.35, 95% CI: 1.03–1.77, p = 0.02).
4. Discussion
This analysis revealed that the use of PNC care has increased over the 20-year period of the EDHS although the proportion remains low. Findings also identified a substantial urban–rural difference among Ethiopian women’s engagement with PNC care. In addition, this study identified that PNC service utilisation was significantly influenced by predisposing and need factors of Anderson’s model of health behaviour. Accordingly, the likelihood of women to receive PNC service was higher among those who were from the rich wealth quintile, had ANC visits, delivered in a health facility, and delivery by caesarean section. Furthermore, the present study also showed that whilst birth spacing was a significant factor among urban women wealth index, ANC visits, and perception of a health facility’s distance were significant among rural women. The identification of these factors is critical for improving PNC service utilisation in Ethiopia and other developing countries.
An interesting finding of this study is the effects of need factors such as ANC attendance and delivery in a health facility on PNC service utilisation. The analysis found that mothers who had 1–3 ANC visits, and four or more visits as recommended by the WHO [28], were more likely to have PNC visits. Consistent with findings from Nigeria, Nepal and Ethiopia [29], our analysis also revealed that women who delivered in a health facility and by a caesarean section were significantly likely to use PNC services as well. The finding suggests that women are more likely to receive PNC service if they had interventions that improve access to and utilisation of ANC and skilled delivery care—this finding is consistent with studies from around the world [30]. The finding that urban women with over 24 months of birth spacing were more likely to use PNC implies the importance of family planning and maternal health service integration [31].
In this study, we showed that women who perceived that distance to the health facility was not a big problem were significantly less likely to use PNC care, suggesting that distance to the health facility and the associated transportation cost could be a barrier for some women to access PNC. This finding was in line with those of other studies in Ethiopia [32] and elsewhere [33], and suggests that physical proximity to health facilities and geographical distance have a significant role in the utilisation of PNC services. Consistent with other studies [33] rural women in the higher wealth index were significantly likely to use PNC services than those who were from poor categories. In Ethiopia, although maternal health services are free of charge [34,35], the cost of travel and/or medicines is out-of-pocket, which has been showed to act as barriers to full access to maternal health services in the country. These findings imply interventions that aim to improve women’s engagement with PNC care should focus on low socioeconomic rural women living far from health facilities.
This study has some strengths and limitations that should be considered when interpreting the findings. This study involved a nationally representative and relatively larger sample size compared to other cross-sectional studies in Ethiopia which implies that generalisation of the findings could be possible. Most of the study findings also support the conclusions from smaller studies which again demonstrates the national representativeness of the data. However, the cross-sectional nature of the data means that temporal association between the study variables and PNC cannot be established. In addition, self-reporting was the method employed during EDHS data collection which suggests that recall bias is a possibility which may lead to under- or over-estimation of proportions and associations between exposure and outcome variables. Furthermore, as this study relied on secondary analysis of EDHS data we could not see if variables not measured by the EDHS such as partner support, cultural practices, health status of women, transportation, health professional attitude and skills would influence the women’s engagement with PNC care, and this warrants the need of additional primary studies. Qualitative studies examining the women’s experiences of receiving PNC may also shed light on how these factors operate to influence the women’s access to care after childbirth.
5. Conclusions
Overall, the present study indicated the low level of utilisation of PNC among Ethiopian women with significant urban–rural variations. The study also demonstrated that ANC follow up, delivery by a cesarean section, perceived distance from a health facility and being from the high-wealth quintile are important determinants to seek PNC services in both urban–rural areas and at the national level in Ethiopia. It is important that efforts that aim to improve PNC utilisation should be area specific and focus on low socioeconomic rural women and those with no contact with the health system during pregnancy. A combination of both community and facility level interventions are also essential to improve maternal health service utilisation in Ethiopia.
Acknowledgments
The authors are grateful to Measure DHS, ICF International, Rockville, MD, USA for providing the data for the analysis.
Abbreviations
| ANC | Antenatal care |
| SDG | Sustainable Development Goal |
| MDG | Millennium Development Goal |
| WHO | World Health Organization |
| ICF | Inner City Fund |
| EDHS | Ethiopia Demographic and Health Survey |
| PNC | Postnatal care |
| CSA | Central Statistical Agency |
| MOH | Minster of Health |
| CIS | Confidence Interval |
| DHS | Demographic and Health Survey |
| SNNPR | Southern Nations, Nationalities, and People’s Region |
| BCC | Behavioural change communication |
Author Contributions
Initially conceived and designed the study: T.M. Methodology: T.M., T.D., J.P. and F.A.O. Data analysis: T.M. and F.A.O. Manuscript drafting: T.M. Manuscript revisions: T.M., T.D., J.P. and F.A.O. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no specific funding for this work.
Data Availability Statement
The datasets used for this study are publicly available from the DHS program website (http://dhsprogram.com/data/).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tessema G.A., Laurence C.O., Melaku Y.A., Misganaw A., Woldie S.A., Hiruye A., Amare A.T., Lakew Y., Zeleke B.M., Deribew A. Trends and causes of maternal mortality in Ethiopia during 1990–2013: Findings from the Global Burden of Diseases study 2013. BMC Public Health. 2017;17:160. doi: 10.1186/s12889-017-4071-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . Trends in Maternal Mortality: 1990–2015: Estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive Summary. World Health Organization; Geneva, Switzerland: 2015. [Google Scholar]
- 3.WHO . Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF. UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; Geneva, Switzerland: 2019. [Google Scholar]
- 4.WHO . Strategies towards Ending Preventable Maternal Mortality (EPMM) World Health Organization; Geneva, Switzerland: 2015. [Google Scholar]
- 5.Bhutta Z.A., Das J.K., Bahl R., Lawn J.E., Salam R.A., Paul V.K., Sankar M.J., Blencowe H., Rizvi A., Chou V.B., et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384:347–370. doi: 10.1016/S0140-6736(14)60792-3. [DOI] [PubMed] [Google Scholar]
- 6.Ronsmans C., Graham W.J. Maternal mortality: Who, when, where, and why. Lancet. 2006;368:1189–1200. doi: 10.1016/S0140-6736(06)69380-X. [DOI] [PubMed] [Google Scholar]
- 7.WHO . WHO Recommendations on Postnatal Care of the Mother and Newborn. World Health Organization; Geneva, Switzerland: 2014. [PubMed] [Google Scholar]
- 8.Lawn J. The State of the World’s Children. Unicef; New York, NY, USA: 2009. Saving mothers and newborn live—The crucial first days after birth; pp. 80–82. [Google Scholar]
- 9.Mekonnen T., Dune T., Perz J., Ogbo F.A. Trends and Determinants of Antenatal Care Service Use in Ethiopia between 2000 and 2016. Int. J. Environ. Res. Public Health. 2019;16:748. doi: 10.3390/ijerph16050748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bobo F.T., Yesuf E.A., Woldie M. Inequities in utilization of reproductive and maternal health services in Ethiopia. Int. J. Equity Health. 2017;16:105. doi: 10.1186/s12939-017-0602-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Regassa N. Antenatal and postnatal care service utilization in southern Ethiopia: A population-based study. Afr. Health Sci. 2011;11:390–397. [PMC free article] [PubMed] [Google Scholar]
- 12.CSA Ethiopia. ICF International USA . Ethiopia: Demographic and Health Survey 2011. Central Statistical Agency; Addis Ababa, Ethiopia: 2012. [Google Scholar]
- 13.Koblinsky M., Tain F., Tesfaye S. Reducing maternal mortality and increasing use of skilled birth attendance: Ethiopia and Mdg-5. Ethiop. J. Reprod. Health. 2018;4 [Google Scholar]
- 14.Sisay M.M., Geremew T.T., Demlie Y.W., Alem A.T., Beyene D.K., Melak M.F., Gelaye K.A., Ayele T.A., Andargie A.A. Spatial patterns and determinants of postnatal care use in Ethiopia: Findings from the 2016 demographic and health survey. BMJ Open. 2019;9:e025066. doi: 10.1136/bmjopen-2018-025066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wudineh K.G., Nigusie A.A., Gesese S.S., Tesu A.A., Beyene F.Y. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: A community-based cross-sectional study. BMC Pregnancy Childbirth. 2018;18:508. doi: 10.1186/s12884-018-2138-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bitew T., Hanlon C., Kebede E., Honikman S., Onah M.N., Fekadu A. Antenatal depressive symptoms and utilisation of delivery and postnatal care: A prospective study in rural Ethiopia. BMC Pregnancy Childbirth. 2017;17:206. doi: 10.1186/s12884-017-1383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akibu M., Tsegaye W., Megersa T., Nurgi S. Prevalence and determinants of complete postnatal care service utilization in northern Shoa, Ethiopia. J. Pregnancy. 2018;2018 doi: 10.1155/2018/8625437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berhe A., Bayray A., Berhe Y., Teklu A., Desta A., Araya T., Zielinski R., Roosevelt L. Determinants of postnatal care utilization in Tigray, Northern Ethiopia: A community based cross-sectional study. PLoS ONE. 2019;14:e0221161. doi: 10.1371/journal.pone.0221161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fekadu G.A., Ambaw F., Kidanie S.A. Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: Further analysis of the 2016 demographic and health survey. BMC Pregnancy Childbirth. 2019;19:64. doi: 10.1186/s12884-019-2216-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayele B.G., Woldu M.A., Gebrehiwot H.W., Gebre-Egziabher E.G., Gebretnsae H., Hadgu T., Abrha A.A., Medhanyie A.A. Magnitude and determinants for place of postnatal care utilization among mothers who delivered at home in Ethiopia: A multinomial analysis from the 2016 Ethiopian demographic health survey. Reprod. Health. 2019;16:162. doi: 10.1186/s12978-019-0818-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sustainable Development Goals Online United Nations. [(accessed on 28 June 2019)]; Available online: http://www.un.org/sustainabledevelopment/sustainable-development-goals/
- 22.Corsi D.J., Neuman M., Finlay J.E., Subramanian S. Demographic and health surveys: A profile. Int. J. Epidemiol. 2012;41:1602–1613. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- 23.United Nations . World Population Prospects 2019. United Nations, Affairs DoEaS; New York, NY, USA: 2019. [Google Scholar]
- 24.Central Statistical Agency [Ethiopia] Inner City Fund International . Ethiopia Demographic and Health Survey 2016. Central Statistical Agency; Addis Ababa, Ethiopia: 2016. [Google Scholar]
- 25.WHO . Postpartum Care of the Mother and Newborn: A practical Guide. WHO; Geneva, Switzerland: 1998. [Google Scholar]
- 26.Neupane S., Doku D. Utilization of postnatal care among Nepalese women. Matern. Child Health J. 2013;17:1922–1930. doi: 10.1007/s10995-012-1218-1. [DOI] [PubMed] [Google Scholar]
- 27.Andersen R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behave. 1995;36:1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 28.Otundo Richard M. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience in Kenya. SSRN. 2019:3449460. doi: 10.2139/ssrn.3449460. [DOI] [Google Scholar]
- 29.Fekadu G.A., Kassa G.M., Berhe A.K., Muche A.A., Katiso N.A. The effect of antenatal care on use of institutional delivery service and postnatal care in Ethiopia: A systematic review and meta-analysis. BMC Health Serv. Res. 2018;18:577. doi: 10.1186/s12913-018-3370-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Titaley C.R., Dibley M.J., Roberts C.L. Factors associated with non-utilisation of postnatal care services in Indonesia. J. Epidemiol. Commun. Health. 2009;63:827–831. doi: 10.1136/jech.2008.081604. [DOI] [PubMed] [Google Scholar]
- 31.Tawfik Y., Rahimzai M., Ahmadzai M., Clark P.A., Kamgang E. Integrating family planning into postpartum care through modern quality improvement: Experience from Afghanistan. Glob. Health Sci. Pract. 2014;2:226–233. doi: 10.9745/GHSP-D-13-00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarekegn S.M., Lieberman L.S., Giedraitis V. Determinants of maternal health service utilization in Ethiopia: Analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14:161. doi: 10.1186/1471-2393-14-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Say L., Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: Examining the scale of the problem and the importance of context. Bull. World Health Organ. 2007;85:812–819. doi: 10.2471/BLT.06.035659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pearson L., Gandhi M., Admasu K., Keyes E. User fees and matenity services in Ethiopia. Int. J. Gynaecol. Obstet. 2011;115:310–315. doi: 10.1016/j.ijgo.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 35.Ahmed S., Creanga A.A., Gillespie D.G., Tsui A.O. Economic status, education and empowerment: Implications for maternal health service utilization in developing countries. PLoS ONE. 2010;5:e11190. doi: 10.1371/journal.pone.0011190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used for this study are publicly available from the DHS program website (http://dhsprogram.com/data/).