Abstract
Simple Summary
Cancers of the female reproductive system are common and are responsible for a large number of deaths in women. The exact reasons why some of these cancers occur are unknown. It is, however, known that for most of these cancers, several factors interact for them to happen. These interactions involve factors external and internal to the woman. An understanding of some of the internal factors involved in how these cancers arise will not only help drive preventive strategies, but will speed the development of new treatment approaches. The endocannabinoid system is a family including chemicals (known as endocannabinoids) produced in the body that are similar to those derived from the cannabis plant. This system, which is widely distributed in the body, has been shown to be involved in various functions. Its disruption has been shown to lead to various diseases, one of which is cancer. In this review, we summarise current knowledge of this system, its various constituents, and how they are involved in reproductive events and their pathologies, especially cancers. Furthermore, we discuss the role of the endocannabinoid system in these cancers and how targeting it could lead to new approaches to diagnosis and treatment of cancers of the female reproductive system.
Abstract
Gynaecological cancers can be primary neoplasms, originating either from the reproductive tract or the products of conception, or secondary neoplasms, representative of metastatic disease. For some of these cancers, the exact causes are unknown; however, it is recognised that the precise aetiopathogeneses for most are multifactorial and include exogenous (such as diet) and endogenous factors (such as genetic predisposition), which mutually interact in a complex manner. One factor that has been recognised to be involved in the pathogenesis and progression of gynaecological cancers is the endocannabinoid system (ECS). The ECS consists of endocannabinoids (bioactive lipids), their receptors, and metabolic enzymes responsible for their synthesis and degradation. In this review, the impact of plant-derived (Cannabis species) cannabinoids and endocannabinoids on gynaecological cancers will be discussed within the context of the complexity of the proteins that bind, transport, and metabolise these compounds in reproductive and other tissues. In particular, the potential of endocannabinoids, their receptors, and metabolic enzymes as biomarkers of specific cancers, such as those of the endometrium, will be addressed. Additionally, the therapeutic potential of targeting selected elements of the ECS as new action points for the development of innovative drugs will be presented.
Keywords: cannabinoids, cervical cancer, endocannabinoids, endometrial cancer, enzymes, receptors, gynaecological cancer, ovarian cancer, signal transduction, transport
1. Introduction
1.1. Cannabis and Endocannabinoids and the Discovery of the Endocannabinoid System
Cannabis is the botanical name of an annual herbaceous plant of the Cannabaceae family that is cultivated and distributed all over the world. This genus consists of three major species, C. sativa, C. indica, and C. ruderalis, which, through interbreeding, share similar genetic backgrounds and physical traits [1]. One distinctive trait of Cannabis plants is production of secondary compounds called “phytocannabinoids”, of which over 100 are produced by the female Cannabis inflorescence [2]. The first evidence for the medical use of Cannabis dates to the Han Dynasty in ancient China, where it was recommended for pain, constipation, agitation, hysteria, spasmodic cough, disorders of the female reproductive tract, and other less defined conditions [3]. Of the 100 or so phytocannabinoids, the most potent is Δ-9-tetrahydrocannabinol (THC), which was isolated and identified as a major psychoactive compound in the 1960s [4]. This was followed by the discovery of additional phytocannabinoids, such as cannabidiol (CBD), cannabinol (CBN), cannabichromene (CBC), cannabigerol (CBG), tetrahydrocannabivirin (THCV), and Δ-8-THC [5].
In the early 1990s, two different G-protein-coupled receptors able to interact with phytocannabinoids were discovered in the central nervous system and the spleen; these receptors are now called type 1 and type 2 cannabinoid receptors (CB1 and CB2), respectively [6,7]. Their discovery was shortly followed by that of their ligands—two specific endogenous bioactive lipids, N-arachidonoylethanolamine (also known as anandamide, AEA) and 2-arachidonoylglycerol (2-AG) from animal tissues [8,9]. Later, the metabolic enzymes that regulate the production and degradation of these endogenous cannabinoids (endocannabinoids; eCBs) were discovered, followed by ancillary ligands, receptors, and transporters. These altogether represent the “endocannabinoid system (ECS)”, which is ubiquitously distributed in the body [4,10,11], including both the male and female reproductive tissues [12,13].
1.2. The Endocannabinoid System: A Multifaceted Network
Although the cannabinoid receptors were originally identified in the central nervous system (CNS for type 1 cannabinoid receptor—CB1), where they regulate the psychotropic effect of THC [14], and the spleen (type 2 cannabinoid receptor—CB2), where they have immunomodulatory functions [15], it is now clear that they are found throughout the human body [16,17]. The eCBs as ligands not only bind to CB1 and CB2, but also bind to and activate or inhibit the actions of the orphan G-protein-coupled receptors GPR55 [18] and GPR119 [19]; moreover, intracellularly, they bind to and activate the transient receptor potential (TRP) channels TRPV1, TRPV2, TRPV3, TRPV4, TRPA1, and TRPM8 [20], widely expressed in female reproductive tissues [21,22,23,24,25,26,27,28,29,30], and the nuclear peroxisome proliferator-activated receptor (PPAR) isotypes α, γ, and δ [31,32,33,34,35,36,37,38], through which they alter gene transcription [39].
One of the most studied eCBs is AEA. It is firstly synthesised through a cascade of enzymatic actions, involving cleavage of membrane phospholipid precursors by the specific action of a calcium-dependent N-acyltransferase (NAT), followed by the catalytic activity of a specific phospholipase D called N-acylphosphatidylethanolamine-specific phospholipase D (NAPE-PLD) [40]. Degradation of AEA is regulated mainly by the activity of fatty acid amide hydrolase (FAAH), and to a lesser extent by that of N-acylethanolamine acid amidase (NAAA) [17]. Both enzymes break down AEA (and other N-acylethanolamines) into arachidonic acid (for AEA) and ethanolamine. The other major eCB, 2-AG, is generated from hydrolysis of diacylglycerol by two specific sn-1 diacylglycerol-lipases (DAGL α and β), and is degraded by a specific monoacylglycerol lipase (MAGL) and, to a lesser extent and in a different way, by the α/β hydrolase domain (ABHD) proteins 2, 6, and 12 [17]. AEA and 2-AG can also be subjected to oxygenation by cyclooxygenase-2 (COX-2) and by different lipoxygenase (LOX) isozymes, as well as by several cytochrome P450 monooxygenases [4]. While additional endocannabinoids have been suggested, namely N-arachidonoyl dopamine (NADA), virodhamine, and noladin ether, their physiological role remains as yet unclear [4,17].
In common with other lipids in the body, eCBs are limited in their distribution around the body and within the aqueous intracellular cytosol by their hydrophobic properties. Intercellular transport of eCBs requires extracellular transporters, although these have not yet been identified. What is known is that when eCBs reach a cell, they cross the cell membrane via a facilitated diffusion process mediated by a putative, specific eCB membrane transporter (EMT), whose molecular identity has not yet been identified [41]. This could be because it does not even exist [42], leading others to speculate that extracellular eCBs bind to a membrane carrier protein located within caveolae lipid rafts, form vesicles, and enter cells through endocytosis [41]. When inside a cell, eCBs are transported by distinct carriers that drive them to different cellular compartments. Comprehensive reviews that summarise recent work on these transporters, such as fatty acid binding proteins (FABPs), heat shock protein 70 (HSP70), albumin, FAAH-1-like AEA transporter (FLAT-1), and sterol carrier protein 2 (SCP-2), can be found in the literature [41,43].
All of these elements and additional eCB-like compounds, such as N-palmitoylethanolamine (PEA), N-oleoylethanolamine (OEA), and N-stearoylethanolamine (SEA) (which exert a CB1-/CB2-independent “entourage effect” whereby FAAH preferentially catabolises the eCB-like compounds and potentiates the activity of other eCBs [44]), are part of the ECS orchestra involved in a growing number of physiological and pathological processes, including those occurring in the female reproductive tract.
1.3. ECS in Female Tissues and Reproductive Events
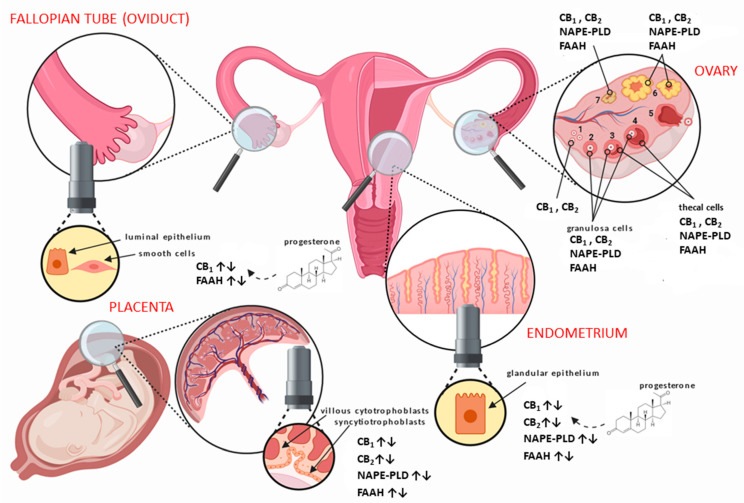
The main elements of the ECS are all expressed in human female reproductive tissues, such as the ovaries [45], Fallopian tubes (oviduct) [46], uterus [47], and placenta [48] (Figure 1). They have also been localised to areas of the hypothalamus responsible for producing hormones, which act through the hypothalamic–pituitary–gonadal (HPG) axis to control a great number of reproductive functions [38]. In the human ovaries, CB1 and CB2 have been shown to be expressed in the granulosa cells of primordial, primary, secondary, and tertiary follicles, as well as in theca cells of secondary and tertiary follicles (Figure 1), with the highest expression at the time of ovulation [45]. Additionally, both receptors are expressed in the corpus luteum and corpus albicans, even in the absence of pregnancy [45]. Moreover, FAAH has been shown to be present within theca cells, but NAPE-PLD appears only in the granulosa of secondary and tertiary follicles, the corpus luteum, and corpus albicans [45].
Figure 1.
Distribution of the main endocannabinoid system (ECS) components in human female reproductive tissues. In the ovary, the different stages of follicular development from (1) primordial/primary, (2) secondary, (3) tertiary, (4) pre-ovulatory/Graafian, to (5) ovulating follicles are depicted. After ovulation is complete, the condensing granulosa and mural thecal cells form the corpus luteum (6), a structure that produces the progesterone required for continued early pregnancy. In the absence of pregnancy, the corpus luteum degenerates into the corpus albicans (7). Throughout the ovarian cycle, CB1 (type 1 cannabinoid receptor) and CB2 (type 2 cannabinoid receptor), fatty acid amide hydrolase (FAAH), and N-acylphosphatidylethanolamine-specific phospholipase D (NAPE-PLD) are produced in the various cells of the developing follicle and corpus luteum, including the oocyte [45]. Similarly, CB1, CB2, FAAH, and NAPE-PLD are expressed in the Fallopian tube [49] and endometrium [47] throughout the menstrual cycle, where they are regulated by the actions of estradiol and progesterone. The cytotrophoblast and syncytiotrophoblast cells of the early placenta also express CB1, CB2, FAAH, and NAPE-PLD [48], where modulation of protein expression occurs when production of progesterone changes from the corpus luteum to the placenta.
In the Fallopian tube, CB1 is expressed primarily in the smooth muscle cells and in surrounding blood vessels, with lower expression in the cytoplasm of epithelial cells lining the lumen of the tube [46]. In the endometrium, CB1 mRNA and protein levels increase in the secretory phase, probably under the influence of progesterone [50], while CB2 expression is minimal at the beginning of the cycle and increases markedly during the late proliferate phase of the menstrual cycle [47]. Interestingly, CB1 mRNA is only present at low levels in both the Fallopian tube and the endometrium of women with an ectopic pregnancy [46].
In addition, growing evidence suggests that the ECS is a part of the diverse mechanisms that regulate the complexity of events that occur in the early stages of pregnancy, and especially within the placenta [51]. The first trimester trophoblast contains transcripts for both CB1 and CB2 [52], and their expression is important for the continuation of normal pregnancy [48,53]. Additionally, increased CB1 expression might cause abnormal decidualisation, which might impair trophoblast invasion and thus be involved in the pathogenesis of preeclampsia [54] and miscarriages [55]. The data thus suggest that elevated eCBs are detrimental to continued pregnancy [56,57]. Furthermore, expression of FAAH is decreased in the first-trimester placenta, extra-villous trophoblast columns, villous cytotrophoblasts, syncytiotrophoblasts, and macrophages; tissues where increased FAAH expression could normally be acting to protect the growing embryo from the detrimental effects of AEA [52,58] and can result in elevated AEA levels in pregnancy that may result in miscarriage. Overall, the main components of the ECS are expressed and indeed regulate some of the functions within the female reproductive tract, as summarised in Table 1 and discussed in detail in the next section. Unsurprisingly, dysregulation of the ECS has been associated with some pathologies of the reproductive system, such as endometriosis, adenomyosis, leiomyoma, miscarriage, ectopic pregnancy, pre-eclampsia, and different types of gynaecological cancer (Table 1) [51].
Table 1.
Summary of the main ECS components in the female reproductive tract.
| Tissue | ECS Component | Normal Tissue | Change in Cancer | Pertinent References |
|---|---|---|---|---|
| Ovary | AEA | yes | ↑ | [45,59] |
| OEA | yes | ↑ | [59,60] | |
| PEA | yes | ↑ | [59] | |
| 2-AG | yes | ↑ | [61] | |
| CB1 | yes | ? | [45] | |
| CB2 | yes | ? | [45,62] | |
| TRPV1 | yes | ↑ | [63] | |
| GPR55 | no | ↑ | [64] | |
| NAPE-PLD | yes | ? | [45] | |
| FAAH | yes | ? | [45] | |
| DAGL | ? | ? | none | |
| MAGL | ? | *↑ | [65] | |
| Fallopian Tube (Oviduct) | AEA | yes | ? | [59] |
| OEA | yes | ? | [59] | |
| PEA | yes | ? | [59] | |
| 2-AG | ? | ? | none | |
| CB1 | yes | ? | [46,49,66] | |
| CB2 | yes | ? | [49,66] | |
| TRPV1 | ? | ? | none | |
| GPR55 | ? | ? | none | |
| NAPE-PLD | yes | ? | [49] | |
| FAAH | yes | ? | [49,67] | |
| DAGL | ? | ? | none | |
| MAGL | ? | ? | none | |
| Uterus (endometrium) | AEA | yes | ↑, ± | [50,55,68,69] |
| OEA | yes | ↑ | [68] | |
| PEA | yes | ↑ | [68] | |
| 2-AG | yes | ↑ | [12] | |
| CB1 | yes | ↓, ±, ↑ | [47,70,71,72,73,74,75] | |
| CB2 | yes | ↑, ↓ | [47,72,74] | |
| TRPV1 | yes | ↓ | [76,77] | |
| GPR55 | yes | ↑ | [77] | |
| NAPE-PLD | yes | ↑ | [47,78] | |
| FAAH | yes | ↓ | [47,78,79,80] | |
| DAGL | yes | ? | [74,81] | |
| MAGL | yes | ? | [74,81] | |
| Uterus (myometrium) ** | AEA | Yes | ? | [30] |
| OEA | Yes | ? | [30] | |
| PEA | Yes | ? | [30] | |
| 2-AG | ? | ? | none | |
| CB1 | Yes | ? | [30,82,83] | |
| CB2 | Yes | ? | [30,83] | |
| TRPV1 | Yes | ? | [30] | |
| GPR55 | yes | ? | [30] | |
| NAPE-PLD | yes | ? | [30,82] | |
| FAAH | yes | ? | [30,82] | |
| DAGL | yes | ? | [81] | |
| MAGL | yes | ? | [81] | |
| Cervix | AEA | yes | ? | [84,85] |
| OEA | ? | ? | none | |
| PEA | ? | ? | none | |
| 2-AG | ? | ? | none | |
| CB1 | yes | ? | [80,84] | |
| CB2 | yes | ? | [80,84,86] | |
| TRPV1 | yes | ? | [84,85,87] | |
| GPR55 | ? | ? | none | |
| NAPE-PLD | ? | ? | none | |
| FAAH | yes | ? | [80] | |
| DAGL | ? | ? | none | |
| MAGL | ? | ? | none | |
| Vagina | AEA | ? | ? | none |
| OEA | ? | ? | none | |
| PEA | ? | ? | none | |
| 2-AG | ? | ? | none | |
| CB1 | yes | ? | [80] | |
| CB2 | ? | ? | none | |
| TRPV1 | ? | ? | none | |
| GPR55 | ? | ? | none | |
| NAPE-PLD | ? | ? | none | |
| FAAH | yes | ? | [80] | |
| DAGL | ? | ? | none | |
| MAGL | ? | ? | none | |
| Vulva | AEA | ? | ? | none |
| OEA | ? | ? | none | |
| PEA | ? | ? | none | |
| 2-AG | ? | ? | none | |
| CB1 | yes | ? | [80,88] | |
| CB2 | yes | ? | [88] | |
| TRPV1 | yes | ? | [88] | |
| GPR55 | yes | ? | [88] | |
| NAPE-PLD | ? | ? | none | |
| FAAH | yes | ? | [80] | |
| DAGL | ? | ? | none | |
| MAGL | ? | ? | none | |
| Placenta (Trophoblast) *** | AEA | yes | ? | [53,89] |
| OEA | yes | ? | [53] | |
| PEA | yes | ? | [53] | |
| 2-AG | yes | ? | [90] | |
| CB1 | yes | ? | [48,53,58,80,91] | |
| CB2 | yes | ? | [48,53,58] | |
| TRPV1 | yes | ? | [48] | |
| GPR55 | yes | ? | [92] | |
| NAPE-PLD | yes | ? | [48,53] | |
| FAAH | yes | ? | [48,53,58,80,91] | |
| DAGL | yes | ? | [93,94] | |
| MAGL | yes | ? | [93,94] |
Notes: Yes = present; No = absent; ? = currently unknown; ↑ = increases; ↓ = decreases; ± = unchanged; none = no work in this area; *↑ in aggressive tumours when compared to levels in non-aggressive tumours; ** malignant tumour known as uterine sarcoma and non-malignant precursor known as leiomyoma; *** malignant tumour known as choriocarcinoma and non-malignant precursor known as hydatiform mole.
1.4. The Endocannabinoid System in Relation to Normal Gynaecological Tissues
There have been several reviews [95] on this, and these are summarised in Table 1. All the components of the ECS are present and active in all parts of the female reproductive tract. Here, they play roles that include oocyte production [45,59,96,97,98], oviductal transport [98,99,100], and blastocyst maturity and implantation [101], as well as in preparing the endometrium for implantation [47,102,103,104,105]. When the ECS is dysfunctional or interfered with by, for example, cannabinoids [106,107], human fertility may be impaired (reviewed in [12,101,108,109]) and there may be associated reproductive-tissue-dependent pathologies, such as endometriosis, miscarriage, ectopic pregnancy, or pre-eclampsia [51,101,108,110,111,112]. Two recent reviews [12,38] on the ECS in the female reproductive tract summarise what is known on this topic, but crucially, these omit some important details on the main ECS components in gynaecological cancers, which we hope to address in this review (see Table 1). In this context, the ECS has been studied the most in the human ovary [45,59,60,61,63,64,65,113], cervix [80,84,85,86,87], and endometrium [47,50,55,68,69,70,72,73,74,75,81], the most common gynaecological cancers ([95,114,115]); however, other female cancers have not been studied, as shown in Figure 2. Although the presence and actions of the most commonly studied endogenous ligands (AEA, 2-AG, OEA, and PEA) in human reproductive tissues have been demonstrated, the presence and actions of others, such as SEA, virodhamine, stearamide, and monoolein [12,30,38,45,49,51,54,57,69,78,95,101,105,108,112,116,117,118,119,120,121,122,123] have not. Studies on receptor expression and function are few, and although there are some published studies on NAPE-PLD and FAAH expression and action in the female reproductive tract, many other (endo)cannabinoid metabolising enzymes have yet to be investigated, either in the normal female reproductive tract or in their related neoplasms (Figure 1 and Figure 2; Table 1).
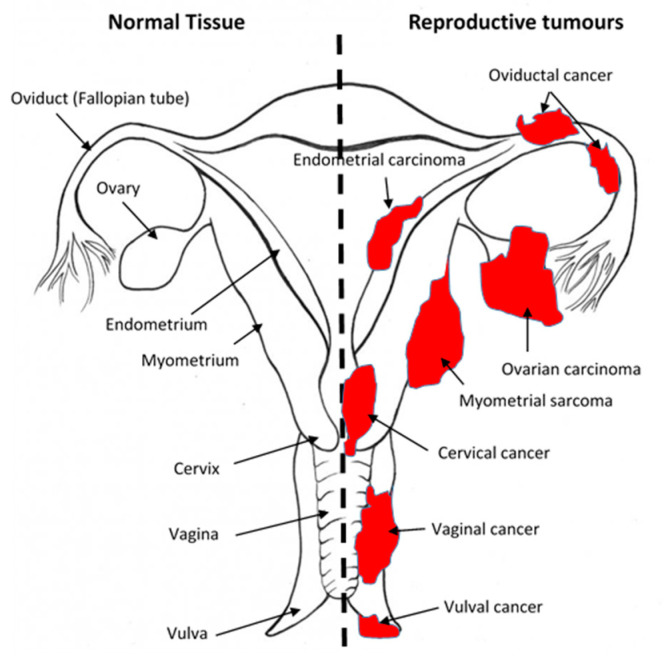
Figure 2.
Sites of gynaecological cancers in the female reproductive tract. The diagram indicates the names of the normal tissues of the female reproductive tract (left side) and the sites and names of the cancers (right side) for the corresponding normal tissues. Please add copyright if necessary.
1.5. An Overview of Gynaecological Cancers
Tumours of the female reproductive system are a diverse group of neoplasms that have different epidemiological, pathological, and clinical features and treatment options [95,124,125]. The malignant forms (Figure 2) constitute approximately one out of six cancers in women [114]. In the UK, gynaecological cancers are an important cause of morbidity and mortality, and are in the top 10 most commonly diagnosed female malignancies of the last decade [126]. Approximately 8500, 7100, and 3100 new cases of uterine, ovarian, and cervical cancers, respectively, were diagnosed in 2011 [126]. In 2012, there were 2000, 4300, and 920 deaths from uterine, ovarian, and cervical cancers, respectively [126]. These numbers are not confined only to countries with accurately collated data, such as the UK. Globally, for example, the number of patients diagnosed in 2018 with gynaecological cancers was relatively high (>295,000 ovarian, >382,000 uterine, >569,000 cervical, >17,500 vaginal, and >44,000 vulval) [115]. Mortality from these gynaecological cancers is high; for example, in 2018, approximately 185,000 women died from ovarian cancer, 90,000 from uterine cancer, 311,000 from cervical cancer, 15,000 from vulval cancer, and 8000 from vaginal cancers [115]. Unfortunately, similar data for Fallopian tube (oviductal) cancer and choriocarcinoma are unavailable, although there is increasing recognition that most surface epithelial ovarian cancers are of fimbrial origin. The global problem of increasing mortality from gynaecological cancers was recently highlighted by the World Health Organization as needing a response, and it thus pledged to eradicate cervical cancer by 2030 [127].
Significant progress has been made in reducing the incidence of some cancers, but the same cannot be said for some cancers of the female reproductive tract because a lack of a thorough understanding of their causes [128,129]. Cancers, including those of gynaecological origin, are distinguished by dysregulation of important cellular mechanisms, including those involved in the control of cell division, cellular differentiation, and apoptosis. The ECS is one of many factors thought to be involved in the development of cancers [130,131]. Interactions of this system with exogenous cannabinoids can potentially ameliorate [132] or exacerbate [133] the development or progression of cancer. We will now look at each of these interactions in some detail.
1.6. The Effects of Cannabinoids on Gynaecological Cancers
The main cannabinoids that are considered to have pharmaceutical promise in the treatment of cancer are the potent psychoactive and the commonly investigated non-psychoactive components of the Cannabis species, tetrahydrocannabinol (THC) and cannabidiol (CBD). Although there is scant evidence for their effectiveness in the treatment of gynaecological cancers, they are often promoted on medical cannabis production and distribution sites as having proven effectiveness [134,135,136,137,138,139]. Here, we examine the evidence in the scientific and clinical literature to support the current and future use of such compounds in the treatment of gynaecological cancers. These data are summarised in Table 1.
1.6.1. Cannabinoids and Ovarian Cancer
Among gynaecological cancers, those of the ovary have the highest morbidity and mortality rates [140]. In an attempt to establish if there is a possible role for the ECS in ovarian pathophysiology, we [45] studied the expression levels of different components of the ECS [50], and demonstrated expression of CB1, CB2, and the NAE-modulating enzymes NAPE-PLD and FAAH in normal human ovaries using immunohistochemistry [45]. Additionally, AEA concentrations in follicular fluid after ovarian stimulation by hormones (following an in vitro fertilisation protocol that caused an increase in follicle size) were directly correlated with follicle size, suggesting that AEA is indeed involved in the hormonal maturation of follicles and oocytes [45,50]. Furthermore, data exist to indicate that AEA, OEA, and PEA are all elevated in follicular fluids of ovarian cancer patients and women with ovarian cysts [59].
Bagavandoss and colleagues demonstrated CB1 and FAAH expression in ovarian surface epithelium, the site from which some ovarian cancers often arise, providing another clue for a possible involvement of the ECS in ovarian cancer [96]. Regarding the expression of CB1 in ovarian cancer, Messalli and coworkers [141] showed that CB1 expression was moderate in benign and borderline epithelial rat ovarian tumours, but was increased in invasive ovarian tumours, suggesting a correlation between the extent of expression of the ECS components and the prognosis for patients with more aggressive ovarian cancer [141]. The levels of lysophospholipids such as lysophosphatidylinositol (an endogenous GPR55 agonist) in blood and ascitic fluids were also found to be elevated in ovarian cancer patients compared to healthy controls, a finding associated with proliferation and the metastatic potential of ovarian cancer cells [142]. Hofman and colleagues [143] more recently found that elevated lysophosphatidylinositol levels in the ovarian cancer cell lines OVCAR-3, OVCAR-5, and COV-362 resulted in GPR55-dependent angiogenesis. Their conclusion was based on experiments where pharmacological inhibition and genetic deletion of GPR55 reduced the pro-angiogenic potential of lysophosphatidylinositol in these cell lines. Additionally, they demonstrated that the mitogen-activated protein kinase pathway triggered via GPR55 by phosphorylation of ERK1/2 and p38, which are signalling molecules known to be involved in proliferative and migratory responses, could be curtailed by chemical interventions [143]. This observation suggests that some ovarian cancers might be amenable to pharmaceutical intercession. In addition, other components of the endocannabinoid system are important here. For example, the 2-AG degrading enzyme MAGL has been shown to be upregulated in aggressive human ovary cancer cells [65], and it is also thought to be involved in oncogenic signalling and, hence, in increased migration, invasion, and survival of many other cancer cell types [144]. These data suggest that identification of an effective drug that targets the ECS to treat ovarian cancer may have applications in the treatment of other cancers too. The application of such therapies would need to be timely, because MAGL overexpression in non-aggressive cancer cells often results in tumours that subsequently exhibit an increased pathogenic phenotype [65]. Moreover, the application of an MAGL inhibitor led to a reversion of the enhanced pathogenicity [65]. Thus, the involvement of the ECS, and especially the 2-AG signalling pathways in ovarian cancer, may fuel expectations on new therapeutics to combat this and other types of cancer. Some preliminary evidence suggests that OEA and its structural analogues may also have a beneficial effect on inhibiting ovarian cancer growth, but these data need to be confirmed in vivo [60]. There is little evidence that plant-derived (phyto)cannabinoids have any effect on ovarian biology or ovarian cancer development or progression, a concept that came from a study where SKOV-3-derived tumours were grown on the chorioallantoic membrane of fertilised chicken eggs [145], and then were treated with CBD-containing nanoparticles. The data indicated that CBD caused a 1.35- to 1.50-fold reduction in tumour size depending on the type of CBD formulation used [145]. The authors indicated that these nanoparticle preparations might be useful in the treatment of peritoneal metastases of ovarian cancer, possibly with lower adverse drug effects [145]. Furthermore, the preparations also reduced SKOV-3 ovarian cancer cell numbers in vitro, to almost zero within 48 h, possibly making this a good candidate for a randomised clinical trial. Of course, many additional studies are required before any candidate CBD formulation can be used in such clinical trials.
1.6.2. Cannabinoids and Fallopian Tube Cancer
Fallopian tube cancer is a relatively rare gynaecological cancer (Figure 2). It is often categorised as being part of ovarian cancer (especially as there is emerging evidence that most surface epithelial ovarian cancers maybe of fimbrial origin), but it is important to study it as a separate entity. Just like other parts of the female reproductive tract, the oviduct (Fallopian tube) expresses all the components of the ECS, with CB1 and FAAH expression intimately associated with proper oviductal function [49,98,99]. When dysfunctional, the risk of ectopic pregnancy is markedly increased [46,49,99,100,146]. There is little evidence on the effect of cannabinoids on human oviductal function, but in the murine oviduct [100], THC reduces fertility because of the increased number of ectopically implanting embryos. In the bovine oviduct, there is gradation of AEA, OEA, and PEA concentrations in the oviductal epithelial cells with low levels in the isthmus and significantly higher levels of OEA and PEA (but not AEA) in the ampulla at the same point of the oestrous cycle [67]. These levels significantly fluctuated during the oestrous cycle [67], as they do in the human oviduct (Fallopian tube) during the menstrual cycle and along its length [49], with OEA causing a reduction in epithelial cell cilia beat frequencies [146], an effect that is likely to prevent timely movement of fertilised oocytes and precipitate ectopic pregnancy [49]. Although possible relationships between the ECS, cannabinoids, and oviductal cancer currently do not exist (Table 1), the fact that dysregulation of the ECS in the fallopian tube is related to the development of ectopic pregnancy makes us speculate that there could be a role for the ECS in oviductal cancer, and that such a possibility deserves to be investigated.
1.6.3. Cannabinoids and Endometrial Cancer
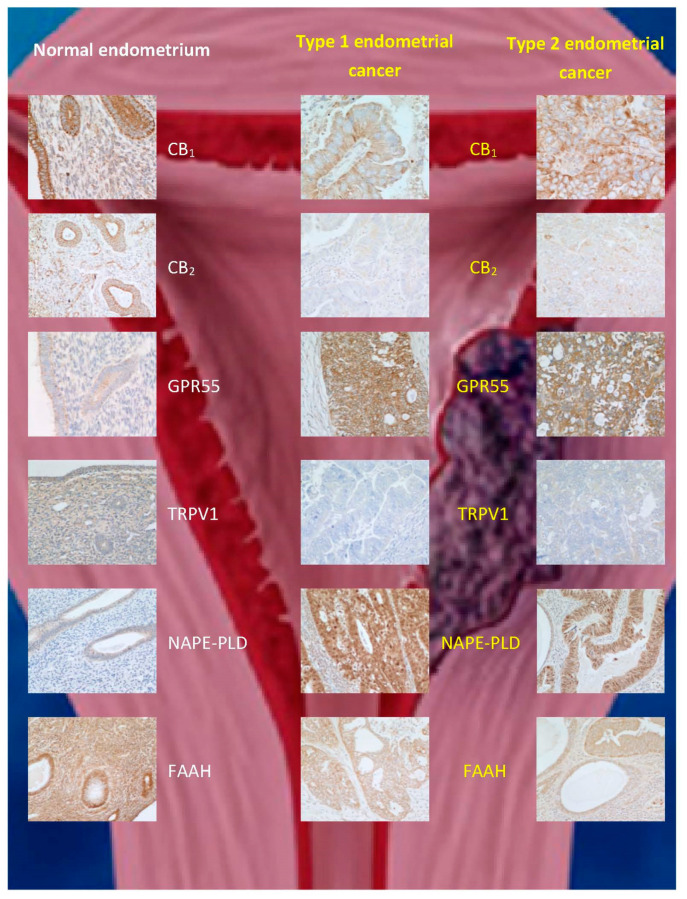
Endometrial cancer, which is classified into type 1 and 2 [147], is the fourth most common cancer in women [148] and the most common gynaecological cancer. Various therapies exist depending on the disease grade and stage. Prognosis is poor, especially in those women with late presentation/detection [147]. Guida and coworkers [74] reported an upregulation of CB2 expression in endometrial cancer, whereby immunostaining was only successful in transformed malignant cells, while being completely absent in normal endometrial tissue. Furthermore, 2-AG levels were increased, but MAGL expression was decreased in comparison to controls, while AEA levels and FAAH expression were unaffected [74]. Similarly, Jove and colleagues [117] demonstrated that CB1 and CB2 were expressed at higher levels in stage III and IV endometrial carcinoma that has a poor prognosis. Unlike Guida and coworkers, the latter researchers found, by immunohistochemistry, an increase in CB1 expression, but no change in CB2 expression in stage 1 endometrial carcinoma tissue compared to normal endometrial tissue [117]. These observations were at odds with those of Risinger and coworkers, who found a decrease in CB1 receptor at the transcriptional level in stage 1 tissue [75]. These contradictory observations prompted us to investigate the ECS in endometrial cancer, using more than a single technique to interrogate CB1 and CB2 expression in endometrial cancer [70,72,73]. Our data indicated that CB1 and CB2 expression are decreased not only at the transcript level, but also at the protein level in both types 1 and 2 (stage 1) endometrial cancers (Table 1; Figure 3). We concluded that the discrepancy between these and previous studies was due to technical issues in the different methodologies used, including tissue sampling [72,73]. Furthermore, we examined the concentrations of plasma and tumour levels of AEA, OEA, and PEA in women with and without endometrial cancer, and showed that although the levels of all three N-acylethanolamines were increased in the tumours and in blood, only AEA and PEA were significantly higher in the plasma of such patients [29,68]. These data suggest that the differential catabolism of these three N-acylethanolamines might explain the different patterns of expression in endometrial cancer and plasma. We subsequently discovered that the apparent discrepancy between the tissue levels and plasma concentrations of OEA in the sample patient cohort was due to a decrease in the expression of FAAH in the tumour [78], without any change in the expression of NAPE-PLD (Table 1; Figure 3). The latter study also allowed us to define cut-off values for plasma AEA, OEA, and PEA concentrations (>1.36, >4.97, and 27.5 nM, respectively) that could be used in the prediction of endometrial cancer in symptomatic women [39], an observation that awaits confirmation in a larger, multicentre trial.
Figure 3.
Immunohistochemical staining patterns for ECS proteins in normal endometrium and (type 1 and type 2) endometrial cancer. The data are taken from [74], where validation for the commercial antibodies and techniques used can be found. Note the reduction in CB1, CB2, TRPV1, and FAAH protein staining and increases for GPR55 and N-acylphosphatidylethanolamine-specific phospholipase D (NAPE-PLD) expression in both types of endometrial cancer when compared to that of normal tissue.
The effects of phytocannabinoids, such as THC, on the progression of endometrial cancer were recently evaluated by Zhang and collaborators [149]. They found that THC inhibited endometrial cancer cell proliferation and migration through decreased expression of matrix metalloproteinase-9, an effect mimicked by matrix metalloproteinase-9 gene silencing [149]. More recently, the effect of THC and CBD on endometrial cancer cell survival was investigated on Ishikawa and Hec50co cells [76], which are models of type 1 and type 2 endometrial cancer, respectively. The expression of all components of the ECS, including TRPV1, was demonstrated in these cells, supporting our in vivo observations (Figure 3). Additionally, treatment of the cells with AEA or CBD (>5 μM) reduced cell viability and was linked to an increase in reactive oxygen species production and caspase-3/-7 activity, which are markers of apoptosis [76]. Interestingly, in both endometrial cancer cell lines, THC had no effect on tumour cell survival, suggesting that in vitro findings in cancer cell lines cannot directly be translated to the in vivo situation. It is also interesting to note that the doses of CBD used in the in vitro study [76] greatly exceed those which are possible to achieve through recreational use of C. sativa or C. indica; this observation possibly explains the lack of anecdotal reports [136,138,139] that support anti-tumour benefits of marijuana use in patients with endometrial cancer [150]. The findings regarding the pro-apoptotic action of AEA in endometrial cancer cell lines are in keeping with the observations by Contassot and colleagues [84], who described AEA-driven cervical cancer cell apoptosis via TRPV1 activation. The danger from such studies, however, is that the data can be misinterpreted by agencies on the internet who wish to sell their Cannabis products, without an appreciation of the dangers they are potentially placing their customers in [138,139,150], and as summarised in [136], “…As always, the results must be met with scepticism and caution. The concentrations of cannabinoids used in these tests are quite high; it may not be safe to administer the amounts necessary to reach these concentrations. Furthermore, cells growing in a dish are very different from cancer cells in the body. They generate their own signals that cause them to grow out of control, which may counteract the effects of cannabinoids. In addition, individual genetic differences may influence how any particular patient will respond to medication. Nevertheless, these results point to CBD and other cannabinoids as a potential treatment for this common type of cancer…” [136]. This level of scepticism is appropriate because the drugs being promoted as anticancer therapies have not undergone the rigorous pre-clinical studies and randomised clinical trials for the treatment they are being advertised for [136,138,139,150]. The danger here is that the multiple pleiotropic effects that cannabinoids (especially THC and CBD) exert on the female body have not been discovered, and adverse side-effects of self-treatment by patients with gynaecological cancers, either by topical or oral routes, could result in serious morbidities or mortality, especially as the effects of these phytocannabinoids go well beyond the effect of apoptosis [151]. Indeed, interactions between (endo)cannabinoids and the stromal cells of the endometrium are often ignored in cancer studies, and these cells of the endometrium are also affected by (endo)cannabinoids [55,71]. It is thus essential that more laboratory-based and clinical studies in this area are performed.
1.6.4. Cannabinoids and Cervical Cancer
Cervical cancer is the second leading cause of malignancy-related deaths in women worldwide due to the lack of customisable and effective treatments (especially in low- and middle-income countries), with more than 250,000 deaths being reported annually [152]. A possible role of the ECS in the development of cervical cancer has been elucidated in recent years. Contassot and coworkers [84] reported a strong expression pattern of CB1 and CB2, as well as of TRPV1, in cervical carcinoma cell lines and biopsies. In addition, it was shown that AEA had a pro-apoptotic effect on cervical carcinoma cell lines (HeLa and Caski) [84], which were not inhibited, but were instead enhanced by CB1 and CB2 antagonists. On the other hand, the TRPV1 selective antagonist capsazepine protected the cell lines from AEA-induced apoptosis, indicating an important role of the TRPV1 channel in the pro-apoptotic action of AEA [92]. Additionally, it was demonstrated by Ramer and collaborators [153] that CBD decreased the invasiveness of cancer cells in a concentration-dependent manner. This effect was observed in the cervical cancer cell lines HeLa and C33A, as well as in the lung cancer cell line A549, and seemed to be mediated by the upregulation of TIMP-1 via CB1/CB2 and TRPV1. TIMP-1 is an inhibitor of matrix metalloproteinases, and as such, it prevents the movement of cells out of the tissue and, hence, a metastatic disease, as has been observed in a patient with ovarian cancer treated with CBD [154].
The activation of p38 and p42/44 mitogen-activated protein kinases was identified as an upstream event in TIMP-1 upregulation [153]. In agreement with these findings, it was reported that treatment of different cervical cancer cell lines (HeLa, SiHa, ME-180) with CBD led to a decrease in cell proliferation [155]. Furthermore, CBD induced cell death by the accumulation of cells in the sub-G0 phase (cell death phase) of the cell cycle, a finding that was most likely caspase-dependent because caspase-9 as well as caspase-3 were upregulated upon CBD treatment [155]. Hence, CBD may be an additional therapeutic tool for the treatment of cervical cancer, yet additional in vivo studies, similar to that performed on a single ovarian cancer patient [154], will be needed to clarify the impact of CBD on cervical cancer.
1.6.5. Cannabinoids and Vaginal Cancer
Vaginal cancer is uncommon, and the American Cancer Society estimated that >6000 women will be diagnosed with it in 2020. The estimated lifetime risk is 1 in 1100 (i.e., less than 0.1%). Of the 6000 USA women expected to be diagnosed with vaginal cancer in 2020, 1450 will die because they have this disease [156]. The role of the ECS in vaginal cancer has not been fully examined. We [80] have demonstrated that CB1 and FAAH are expressed in the normal vagina; however, there are no data on the expression of other components of the ECS (Table 1), nor on what their normal function might be. What happens to the expression of these factors or what effects cannabinoid and eCB ligands might have on the vagina or on cells of vaginal tumours is uncertain/unclear (Table 1). The internet is one source of information, and for the vagina, it is reported that some women experience a “vaginal high” when using cannabinoids, especially as a topical application [135]. The problem with these data is that only 40% of women experience this “psychological” effect [135]. Nevertheless, these statements have led some internet sites to suggest that different cannabis-containing preparations might be useful for the treatment of some of the symptoms associated with vaginal cancer [134,157]. Obviously, a lot more information is needed on the role of cannabinoids and eCBs in the human vagina, and especially in vaginal cancer.
1.6.6. Cannabinoids and Vulvar Cancer
Vulvar cancer is a less common gynaecological cancer [158]. The vulva is very similar to normal thin skin and is known to express CB1 and FAAH [80], but it is not known if it contains all the main components of the ECS (Table 1). The only existing evidence that cannabinoids have an effect on the vulva comes from a less-than-reliable internet source [137]. A C. sativa ethanolic extract and a purified CBD preparation had anti-inflammatory effects on keratinocytes and skin fibroblasts in vitro, suggesting that CBD was the main active ingredient that would be effective in wound injury [159].
This seems important because women with vulvar cancer often undergo radical surgery to remove their malignancy, which causes disfiguration of the female external genitalia, and causes significant long-term emotional and physical instability [160]. Indeed, the use of the CBD derivative VCE-004.3 on skin fibrosis and inflammation [161] demonstrated a CB2/PPARγ-dependent effect, and suggested that similar compounds might be beneficial for patients with vulvar cancer who have undergone surgery and need topical treatment for the pruritus; the latter is associated with skin fibrosis and inflammation, especially as VCE-004.3 appears to inhibit mast cell degranulation [161]. The toxicity profile of such topical administrations remains to be determined; however, ethanolic extracts of THC, CBD, and other cannabinoids appear in the blood shortly after administration; thus, some caution is advised, also in the light of the pleiotropic effects of these compounds [162]. Obviously, more detailed analysis of the role of the ECS and of plant-derived cannabinoids in the treatment of vulvar cancer is warranted.
1.6.7. Cannabinoids and Choriocarcinoma
The function of the female reproductive tract is to support the embryo and fetus during its development into an independent offspring (Figure 1). In order to do this, the coordinated actions of many interacting factors need to take place, of which the ECS is an integral part [101,108,111,163,164,165,166]. A key tissue in human reproduction is the fetoplacental unit. The entire ECS is present in the placenta [166] (see also Table 1), and modifications of its components result in obstetrical problems, such as miscarriage [56,57,113,167], babies that are small for gestational age [168,169], and pre-eclampsia [170]. In addition, dysregulated N-acylethanolamine levels may be responsible for preterm delivery [121,123]. The placenta can also undergo neoplastic changes into two clinically relevant conditions, hydatiform mole (a non-malignant transformation) and choriocarcinoma (a malignant transformation), which appear noteworthy. Currently, there are no data on the expression of the ECS in either of these tumours; there is, however, evidence that AEA and THC both affect a model for choriocarcinoma, like BeWo cells [52,93,94,171], and a model for normal trophoblast, like TCL-1 cells [172], where cell growth is affected mainly through a CB2-dependent mechanism [94,171,172]. These observations, coupled with evidence that THC decreases STAT3 signalling in mice with reduced fetus numbers and placental weights [168], support the view that cannabinoid use in human pregnancy is likely to affect the placenta in a similarly dangerous manner [173]. The increased use of CBD in pregnancy as an anti-emetic [174,175] is thus of great concern because the toxicity profile of CBD in pregnancy is not fully known [174,176,177], and especially as CBD can inactivate both placental CB1 and CB2 receptors in vitro [178].
2. Conclusions
A pivotal role of the ECS in gynaecological cancers has been demonstrated in recent years; in particular, the development, progression, and prognosis of female reproductive tract diseases seem to be associated with their dysregulation [12,30,38,56,57,95,105,108,112,113,118,119,120,122,141,179]. Due to manifold cellular and metabolic regulatory functions, the ECS represents an important therapeutic target that needs further investigation. Cannabinoids, especially plant-derived or synthetic compounds that impact eCB signalling as specific agonists or antagonists of their receptor targets, may potentially influence the functional dysregulation that is apparent in gynaecological cancers. For this reason, more research is required to shed light on the complex interactions of the ECS with respect to the administration of preparations derived from C. sativa or C. indica in order to find new therapeutic tools for effective and safe therapy of gynaecological cancers. One of the main limitations of available studies is that endogenous and exogenous cannabinoids behave differently, and their modes of action in vivo and in vitro are difficult to correlate. It has also become apparent that the effects of cannabinoids vary in a dose-dependent manner. It is thus important to keep these factors in mind when trying to reconcile inconsistent results between studies. Large systematic reviews and meta-analyses would be helpful to sift through these studies, their methods, and their results in order to reach conclusions about treatment efficacy. A recent large systematic review by Whiting and colleagues [180] concluded that the use of cannabinoids in the treatment of a variety of conditions, such as multiple sclerosis, glaucoma, and chronic pain, was associated with adverse effects, such as disorientation, gastrointestinal upset, emesis, and fatigue [180]. Unfortunately, this review did not address cannabinoid use in female reproductive conditions, nor did it supply data about adverse effects of topical cannabinoid administration (e.g., for vulvar disease [134] or the less common vaginal highs [135]). While the political and social environment is becoming more tolerant of medical cannabinoids, the stigma surrounding cannabis use and its derivatives still represents a barrier to effective clinical research [181]. More recently, this attitude has appeared to be changing, yet there is a dearth of available health-authority-regulated cannabinoid compounds [181], and, as such, many patients may look to the internet to find unregulated and untested medicinal products [134,135,136,137,138,139]. Without rigorous regulation and testing of such compounds [182], there is no way of knowing exactly what these products contain and whether they could be harmful to patients. Nevertheless, increasing research into cannabinoid treatments could potentially expand the number and variety of therapies available to cancer patients and limit the need for unregulated products.
In summary, the ECS in the female reproductive tract is fully functional, but intricate in its interactions. Current knowledge on all the components of this system in the reproductive tract is incomplete, and thus, a full picture remains elusive. Although it is composed of multiple receptors, the female reproductive tract is stimulated by numerous exogenous cannabinoids and eCBs, and multiple metabolic enzymes that regulate eCB levels and activity are known; knowledge on the various roles that each of these components have on the initiation, development, and progression of benign and malignant tumours of the female reproductive tract is lacking, or, at best, at an early stage. Much is still unknown (Table 1), and although many studies over the past two decades have highlighted the critical role of the ECS in maintaining key aspects of human and animal reproduction, including immune modulation, inflammation, cell proliferation, and differentiation [101,165,183], the precise roles of these factors in common reproductive tract cancers remain poorly defined. The roles, if any, in less common reproductive cancers (such as those of the vagina, vulva, and trophoblast/placenta) are untested and could provide fertile ground for subsequent studies. Further investigations into the specific influences of cannabinoid type, receptor affected, delivery method, chemical composition, and component concentration [184,185] will help to elucidate the intricacies of the role that the ECS plays in gynaecological cancers. Doing so will provide an excellent opportunity to expand the therapeutic arsenal for treating female neoplastic diseases.
Author Contributions
Conceptualization, A.H.T., T.A., D.T., J.C.K., and M.M.; methodology, A.H.T. and D.T; validation, A.H.T., T.A., and D.T.; writing—original draft preparation, A.H.T. and D.T.; writing—review and editing, T.A., J.C.K., and M.M.; supervision, J.C.K. and M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schilling S., Melzer R., McCabe P.F. Cannabis sativa. Curr. Biol. 2020;30:R8–R9. doi: 10.1016/j.cub.2019.10.039. [DOI] [PubMed] [Google Scholar]
- 2.Mechoulam R., Hanus L. A historical overview of chemical research on cannabinoids. Chem. Phys. Lipids. 2000;108:1–13. doi: 10.1016/S0009-3084(00)00184-5. [DOI] [PubMed] [Google Scholar]
- 3.Brand E.J., Zhao Z. Cannabis in Chinese medicine: Are some traditional indications referenced in ancient literature related to cannabinoids? Front. Pharmacol. 2017;8:108. doi: 10.3389/fphar.2017.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maccarrone M., Bab I., Biro T., Cabral G.A., Dey S.K., Di Marzo V., Konje J.C., Kunos G., Mechoulam R., Pacher P., et al. Endocannabinoid signaling at the periphery: 50 years after THC. Trends Pharmacol. Sci. 2015;36:277–296. doi: 10.1016/j.tips.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pellati F., Borgonetti V., Brighenti V., Biagi M., Benvenuti S., Corsi L. Cannabis sativa L. and nonpsychoactive cannabinoids: Their chemistry and role against oxidative stress, inflammation, and cancer. Biomed. Res. Int. 2018;2018:1691428. doi: 10.1155/2018/1691428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuda L.A., Lolait S.J., Brownstein M.J., Young A.C., Bonner T.I. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346:561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- 7.Munro S., Thomas K.L., Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365:61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- 8.Devane W.A., Hanus L., Breuer A., Pertwee R.G., Stevenson L.A., Griffin G., Gibson D., Mandelbaum A., Etinger A., Mechoulam R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 9.Mechoulam R., Ben-Shabat S., Hanus L., Ligumsky M., Kaminski N.E., Schatz A.R., Gopher A., Almog S., Martin B.R., Compton D.R., et al. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem. Pharmacol. 1995;50:83–90. doi: 10.1016/0006-2952(95)00109-D. [DOI] [PubMed] [Google Scholar]
- 10.Pandey R., Mousawy K., Nagarkatti M., Nagarkatti P. Endocannabinoids and immune regulation. Pharmacol. Res. 2009;60:85–92. doi: 10.1016/j.phrs.2009.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bab I., Ofek O., Tam J., Rehnelt J., Zimmer A. Endocannabinoids and the regulation of bone metabolism. J. Neuroendocrinol. 2008;20(Suppl. 1):69–74. doi: 10.1111/j.1365-2826.2008.01675.x. [DOI] [PubMed] [Google Scholar]
- 12.Cecconi S., Rapino C., Di Nisio V., Rossi G., Maccarrone M. The (endo)cannabinoid signaling in female reproduction: What are the latest advances? Prog. Lipid. Res. 2020;77:101019. doi: 10.1016/j.plipres.2019.101019. [DOI] [PubMed] [Google Scholar]
- 13.Silver R.J. The endocannabinoid system of animals. Animals. 2019;9:686. doi: 10.3390/ani9090686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Casajuana Köguel C., López-Pelayo H., Balcells-Olivero M.M., Colom J., Gual A. Psychoactive constituents of cannabis and their clinical implications: A systematic review. Adicciones. 2018;30:140–151. doi: 10.20882/adicciones.858. [DOI] [PubMed] [Google Scholar]
- 15.Leuti A., Fazio D., Fava M., Piccoli A., Oddi S., Maccarrone M. Bioactive lipids, inflammation and chronic diseases. Adv. Drug. Deliv. Rev. 2020 doi: 10.1016/j.addr.2020.06.028. [DOI] [PubMed] [Google Scholar]
- 16.Malfitano A.M., Basu S., Maresz K., Bifulco M., Dittel B.N. What we know and do not know about the cannabinoid receptor 2 (CB2) Semin. Immunol. 2014;26:369–379. doi: 10.1016/j.smim.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maccarrone M. Missing pieces to the endocannabinoid puzzle. Trends Mol. Med. 2020;26:263–272. doi: 10.1016/j.molmed.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Ross R.A. The enigmatic pharmacology of GPR55. Trends Pharmacol. Sci. 2009;30:156–163. doi: 10.1016/j.tips.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Syed S.K., Bui H.H., Beavers L.S., Farb T.B., Ficorilli J., Chesterfield A.K., Kuo M.S., Bokvist K., Barrett D.G., Efanov A.M. Regulation of GPR119 receptor activity with endocannabinoid-like lipids. Am. J. Physiol. Endocrinol. Metab. 2012;303:E1469–E1478. doi: 10.1152/ajpendo.00269.2012. [DOI] [PubMed] [Google Scholar]
- 20.Muller C., Morales P., Reggio P.H. Cannabinoid ligands targeting TRP channels. Front. Mol. Neurosci. 2018;11:487. doi: 10.3389/fnmol.2018.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bohonyi N., Pohoczky K., Szalontai B., Perkecz A., Kovacs K., Kajtar B., Orban L., Varga T., Szegedi S., Bodis J., et al. Local upregulation of transient receptor potential ankyrin 1 and transient receptor potential vanilloid 1 ion channels in rectosigmoid deep infiltrating endometriosis. Mol. Pain. 2017;13:1744806917705564. doi: 10.1177/1744806917705564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Clercq K., Held K., Van Bree R., Meuleman C., Peeraer K., Tomassetti C., Voets T., D’Hooghe T., Vriens J. Functional expression of transient receptor potential channels in human endometrial stromal cells during the luteal phase of the menstrual cycle. Hum. Reprod. 2015;30:1421–1436. doi: 10.1093/humrep/dev068. [DOI] [PubMed] [Google Scholar]
- 23.Ducza E., Csanyi A., Szoke E., Pohoczky K., Hajagos-Toth J., Kothencz A., Tiszai Z., Gaspar R. Significance of transient receptor potential vanilloid 4 and aquaporin 5 co-expression in the rat uterus at term. Heliyon. 2019;5:e02697. doi: 10.1016/j.heliyon.2019.e02697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han J.H., Choi H.K., Kim S.J. Topical TRPM8 agonist (icilin) relieved vulva pruritus originating from lichen sclerosus et atrophicus. Acta Derm. Venereol. 2012;92:561–562. doi: 10.2340/00015555-1244. [DOI] [PubMed] [Google Scholar]
- 25.Li C., Wu Y.T., Zhu Q., Zhang H.Y., Huang Z., Zhang D., Qi H., Liang G.L., He X.Q., Wang X.F., et al. TRPV4 is involved in levonorgestrel-induced reduction in oviduct ciliary beating. J. Pathol. 2019;248:77–87. doi: 10.1002/path.5233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meseguer V., Karashima Y., Talavera K., D’Hoedt D., Donovan-Rodriguez T., Viana F., Nilius B., Voets T. Transient receptor potential channels in sensory neurons are targets of the antimycotic agent clotrimazole. J. Neurosci. 2008;28:576–586. doi: 10.1523/JNEUROSCI.4772-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Persoons E., Hennes A., De Clercq K., Van Bree R., Vriens G., Peterse D., Vanhie A., Meuleman C., Voets T. Functional expression of TRP ion channels in endometrial stromal cells of endometriosis patients. Int. J. Mol. Sci. 2018;19:2467. doi: 10.3390/ijms19092467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teilmann S.C., Byskov A.G., Pedersen P.A., Wheatley D.N., Pazour G.J., Christensen S.T. Localization of transient receptor potential ion channels in primary and motile cilia of the female murine reproductive organs. Mol. Reprod. Dev. 2005;71:444–452. doi: 10.1002/mrd.20312. [DOI] [PubMed] [Google Scholar]
- 29.Tingaker B.K., Ekman-Ordeberg G., Facer P., Irestedt L., Anand P. Influence of pregnancy and labor on the occurrence of nerve fibers expressing the capsaicin receptor TRPV1 in human corpus and cervix uteri. Reprod. Biol. Endocrinol. 2008;6:8. doi: 10.1186/1477-7827-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ayakannu T., Taylor A.H., Marczylo T.H., Konje J.C. New insights of uterine leiomyoma pathogenesis: Endocannabinoid system. Med. Sci. Monit. Basic Res. 2019;25:76–87. doi: 10.12659/MSMBR.914019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dong K., Zhang M.X., Liu Y., Su X.L., Chen B., Zhang X.L. Peroxisome proliferator-activated receptor alpha expression changes in human pregnant myometrium. Reprod. Sci. 2013;20:654–660. doi: 10.1177/1933719112461187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Enioutina E.Y., Visic V.D., Daynes R.A. Enhancement of common mucosal immunity in aged mice following their supplementation with various antioxidants. Vaccine. 2000;18:2381–2393. doi: 10.1016/S0264-410X(00)00008-6. [DOI] [PubMed] [Google Scholar]
- 33.Nickkho-Amiry M., McVey R., Holland C. Peroxisome proliferator-activated receptors modulate proliferation and angiogenesis in human endometrial carcinoma. Mol. Cancer Res. 2012;10:441–453. doi: 10.1158/1541-7786.MCR-11-0233. [DOI] [PubMed] [Google Scholar]
- 34.Tao T., Wang Y., Xu B., Mao X., Sun Y., Liu W. Role of adiponectin/peroxisome proliferator-activated receptor alpha signaling in human chorionic gonadotropin-induced estradiol synthesis in human luteinized granulosa cells. Mol. Cell Endocrinol. 2019;493:110450. doi: 10.1016/j.mce.2019.110450. [DOI] [PubMed] [Google Scholar]
- 35.Tsibris J.C., Porter K.B., Jazayeri A., Tzimas G., Nau H., Huang H., Kuparadze K., Porter G.W., O’Brien W.F., Spellacy W.N. Human uterine leiomyomata express higher levels of peroxisome proliferator-activated receptor gamma, retinoid X receptor alpha, and all-trans retinoic acid than myometrium. Cancer Res. 1999;59:5737–5744. [PubMed] [Google Scholar]
- 36.Yin Y., Lin C., Veith G.M., Chen H., Dhandha M., Ma L. Neonatal diethylstilbestrol exposure alters the metabolic profile of uterine epithelial cells. Dis. Model. Mech. 2012;5:870–880. doi: 10.1242/dmm.009076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang G., Hou X., Gao S. Stimulation of peroxisome proliferator-activated receptor gamma inhibits estrogen receptor alpha transcriptional activity in endometrial carcinoma cells. Oncol. Rep. 2015;33:1227–1234. doi: 10.3892/or.2015.3729. [DOI] [PubMed] [Google Scholar]
- 38.Walker O.S., Holloway A.C., Raha S. The role of the endocannabinoid system in female reproductive tissues. J. Ovarian Res. 2019;12:3. doi: 10.1186/s13048-018-0478-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Sullivan S.E. An update on PPAR activation by cannabinoids. Br. J. Pharmacol. 2016;173:1899–1910. doi: 10.1111/bph.13497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Selvy P.E., Lavieri R.R., Lindsley C.W., Brown H.A. Phospholipase D: Enzymology, functionality, and chemical modulation. Chem. Rev. 2011;111:6064–6119. doi: 10.1021/cr200296t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nicolussi S., Gertsch J. Endocannabinoid transport revisited. Vitam. Horm. 2015;98:441–485. doi: 10.1016/bs.vh.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 42.Ligresti A., De Petrocellis L., Hernan Perez de la Ossa D., Aberturas R., Cristino L., Moriello A.S., Finizio A., Gil M.E., Torres A.I., Molpeceres J., et al. Exploiting nanotechnologies and TRPV1 channels to investigate the putative anandamide membrane transporter. PLoS ONE. 2010;5:e10239. doi: 10.1371/journal.pone.0010239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maccarrone M., Dainese E., Oddi S. Intracellular trafficking of anandamide: New concepts for signaling. Trends Biochem. Sci. 2010;35:601–608. doi: 10.1016/j.tibs.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Maccarrone M. Metabolism of the endocannabinoid anandamide: Open questions after 25 years. Front. Mol. Neurosci. 2017;10:166. doi: 10.3389/fnmol.2017.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.El-Talatini M.R., Taylor A.H., Elson J.C., Brown L., Davidson A.C., Konje J.C. Localisation and function of the endocannabinoid system in the human ovary. PLoS ONE. 2009;4:e4579. doi: 10.1371/journal.pone.0004579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Horne A.W., Phillips J.A., 3rd, Kane N., Lourenco P.C., McDonald S.E., Williams A.R., Simon C., Dey S.K., Critchley H.O. CB1 expression is attenuated in Fallopian tube and decidua of women with ectopic pregnancy. PLoS ONE. 2008;3:e3969. doi: 10.1371/journal.pone.0003969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taylor A.H., Abbas M.S., Habiba M.A., Konje J.C. Histomorphometric evaluation of cannabinoid receptor and anandamide modulating enzyme expression in the human endometrium through the menstrual cycle. Histochem. Cell Biol. 2010;133:557–565. doi: 10.1007/s00418-010-0695-9. [DOI] [PubMed] [Google Scholar]
- 48.Taylor A.H., Finney M., Lam P.M., Konje J.C. Modulation of the endocannabinoid system in viable and non-viable first trimester pregnancies by pregnancy-related hormones. Reprod. Biol. Endocrinol. 2011;9:152. doi: 10.1186/1477-7827-9-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gebeh A.K., Willets J.M., Marczylo E.L., Taylor A.H., Konje J.C. Ectopic pregnancy is associated with high anandamide levels and aberrant expression of FAAH and CB1 in fallopian tubes. J. Clin. Endocrinol. Metab. 2012;97:2827–2835. doi: 10.1210/jc.2012-1780. [DOI] [PubMed] [Google Scholar]
- 50.El-Talatini M.R., Taylor A.H., Konje J.C. The relationship between plasma levels of the endocannabinoid, anandamide, sex steroids, and gonadotrophins during the menstrual cycle. Fertil. Steril. 2010;93:1989–1996. doi: 10.1016/j.fertnstert.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 51.Maia J., Fonseca B.M., Teixeira N., Correia-da-Silva G. The fundamental role of the endocannabinoid system in endometrium and placenta: Implications in pathophysiological aspects of uterine and pregnancy disorders. Hum. Reprod. Update. 2020 doi: 10.1093/humupd/dmaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Habayeb O.M., Taylor A.H., Bell S.C., Taylor D.J., Konje J.C. Expression of the endocannabinoid system in human first trimester placenta and its role in trophoblast proliferation. Endocrinology. 2008;149:5052–5060. doi: 10.1210/en.2007-1799. [DOI] [PubMed] [Google Scholar]
- 53.Karasu T., Marczylo T.H., Marczylo E.L., Taylor A.H., Oloto E., Konje J.C. The effect of mifepristone (RU486) on the endocannabinoid system in human plasma and first-trimester trophoblast of women undergoing termination of pregnancy. J. Clin. Endocrinol. Metab. 2014;99:871–880. doi: 10.1210/jc.2013-2922. [DOI] [PubMed] [Google Scholar]
- 54.Fugedi G., Molnar M., Rigo J., Jr., Schonleber J., Kovalszky I., Molvarec A. Increased placental expression of cannabinoid receptor 1 in preeclampsia: An observational study. BMC Pregnancy Childbirth. 2014;14:395. doi: 10.1186/s12884-014-0395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fonseca B.M., Cunha S.C., Goncalves D., Mendes A., Braga J., Correia-da-Silva G., Teixeira N.A. Decidual NK cell-derived conditioned medium from miscarriages affects endometrial stromal cell decidualisation: Endocannabinoid anandamide and tumour necrosis factor-alpha crosstalk. Hum. Reprod. 2020;35:265–274. doi: 10.1093/humrep/dez260. [DOI] [PubMed] [Google Scholar]
- 56.Habayeb O.M., Taylor A.H., Finney M., Evans M.D., Konje J.C. Plasma anandamide concentration and pregnancy outcome in women with threatened miscarriage. JAMA. 2008;299:1135–1136. doi: 10.1001/jama.299.10.1135. [DOI] [PubMed] [Google Scholar]
- 57.Maccarrone M., Valensise H., Bari M., Lazzarin N., Romanini C., Finazzi-Agro A. Relation between decreased anandamide hydrolase concentrations in human lymphocytes and miscarriage. Lancet. 2000;355:1326–1329. doi: 10.1016/S0140-6736(00)02115-2. [DOI] [PubMed] [Google Scholar]
- 58.Helliwell R.J., Chamley L.W., Blake-Palmer K., Mitchell M.D., Wu J., Kearn C.S., Glass M. Characterization of the endocannabinoid system in early human pregnancy. J. Clin. Endocrinol. Metab. 2004;89:5168–5174. doi: 10.1210/jc.2004-0388. [DOI] [PubMed] [Google Scholar]
- 59.Schuel H., Burkman L.J., Lippes J., Crickard K., Forester E., Piomelli D., Giuffrida A. N-Acylethanolamines in human reproductive fluids. Chem. Phys. Lipids. 2002;121:211–227. doi: 10.1016/S0009-3084(02)00158-5. [DOI] [PubMed] [Google Scholar]
- 60.Kisgeropoulis E. Inhibition of Ovarian Cancer Cell Proliferation by Oleoylethanolamide and Its Metabolically Stable Analog AM3102. Ohio State, Researchgate.net . [(accessed on 23 December 2020)];2013 Available online: https://www.researchgate.net/publication/278025965_Inhibition_of_Ovarian_Cancer_Cell_Proliferation_by_Oleoylethanolamide_and_its_Metabolically_Stable_Analog_AM3102.
- 61.Bradshaw H.B., Allard C. Endogenous cannabinoid production in the rat female reproductive tract is regulated by changes in the hormonal milieu. Pharmaceuticals. 2011;4:933–949. doi: 10.3390/ph4060933. [DOI] [Google Scholar]
- 62.De Domenico E., Todaro F., Rossi G., Dolci S., Geremia R., Rossi P., Grimaldi P. Overactive type 2 cannabinoid receptor induces meiosis in fetal gonads and impairs ovarian reserve. Cell Death Dis. 2017;8:e3085. doi: 10.1038/cddis.2017.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Han G.H., Chay D.B., Nam S., Cho H., Chung J.Y., Kim J.H. Prognostic significance of transient receptor potential vanilloid type 1 (TRPV1) and phosphatase and tension homolog (PTEN) in epithelial ovarian cancer. Cancer Genom. Proteom. 2020;17:309–319. doi: 10.21873/cgp.20191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pineiro R., Maffucci T., Falasca M. The putative cannabinoid receptor GPR55 defines a novel autocrine loop in cancer cell proliferation. Oncogene. 2011;30:142–152. doi: 10.1038/onc.2010.417. [DOI] [PubMed] [Google Scholar]
- 65.Nomura D.K., Long J.Z., Niessen S., Hoover H.S., Ng S.W., Cravatt B.F. Monoacylglycerol lipase regulates a fatty acid network that promotes cancer pathogenesis. Cell. 2010;140:49–61. doi: 10.1016/j.cell.2009.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gervasi M.G., Rapanelli M., Ribeiro M.L., Farina M., Billi S., Franchi A.M., Perez Martinez S. The endocannabinoid system in bull sperm and bovine oviductal epithelium: Role of anandamide in sperm-oviduct interaction. Reproduction. 2009;137:403–414. doi: 10.1530/REP-08-0204. [DOI] [PubMed] [Google Scholar]
- 67.Gervasi M.G., Marczylo T.H., Lam P.M., Rana S., Franchi A.M., Konje J.C., Perez-Martinez S. Anandamide levels fluctuate in the bovine oviduct during the oestrous cycle. PLoS ONE. 2013;8:e72521. doi: 10.1371/journal.pone.0072521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ayakannu T., Taylor A.H., Marczylo T.H., Maccarrone M., Konje J.C. Identification of novel predictive biomarkers for endometrial malignancies: N-Acylethanolamines. Front. Oncol. 2019;9:430. doi: 10.3389/fonc.2019.00430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ayakannu T., Taylor A., Willets J., Marczylo T., Brown L., Davies Q., Moss E., Konje J. Effect of anandamide on endometrial adenocarcinoma (Ishikawa) cell numbers: Implications for endometrial cancer therapy. Lancet. 2015;385(Suppl. 1):S20. doi: 10.1016/S0140-6736(15)60335-X. [DOI] [PubMed] [Google Scholar]
- 70.Ayakannu T., Taylor A.H., Davies Q., Moss E.L., Konje J.C. Optimisation of uniplex and duplex reactions is not required for real-time PCR amplification of target genes in endometrial cancer. [(accessed on 24 December 2020)];Insights Obstet. Gynaecol. 2017 1:5.1. Available online: https://www.researchgate.net/publication/347910796. [Google Scholar]
- 71.Gentilini D., Besana A., Vigano P., Dalino P., Vignali M., Melandri M., Busacca M., Di Blasio A.M. Endocannabinoid system regulates migration of endometrial stromal cells via cannabinoid receptor 1 through the activation of PI3K and ERK1/2 pathways. Fertil. Steril. 2010;93:2588–2593. doi: 10.1016/j.fertnstert.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 72.Ayakannu T., Taylor A.H., Konje J.C. Cannabinoid receptor expression in estrogen-dependent and estrogen-independent endometrial cancer. J. Recept. Signal. Transduct. Res. 2018;38:385–392. doi: 10.1080/10799893.2018.1531890. [DOI] [PubMed] [Google Scholar]
- 73.Ayakannu T., Taylor A.H., Willets J.M., Brown L., Lambert D.G., McDonald J., Davies Q., Moss E.L., Konje J.C. Validation of endogenous control reference genes for normalizing gene expression studies in endometrial carcinoma. Mol. Hum. Reprod. 2015;21:723–735. doi: 10.1093/molehr/gav033. [DOI] [PubMed] [Google Scholar]
- 74.Guida M., Ligresti A., De Filippis D., D’Amico A., Petrosino S., Cipriano M., Bifulco G., Simonetti S., Orlando P., Insabato L., et al. The levels of the endocannabinoid receptor CB2 and its ligand 2-arachidonoylglycerol are elevated in endometrial carcinoma. Endocrinology. 2010;151:921–928. doi: 10.1210/en.2009-0883. [DOI] [PubMed] [Google Scholar]
- 75.Risinger J.I., Maxwell G.L., Chandramouli G.V., Jazaeri A., Aprelikova O., Patterson T., Berchuck A., Barrett J.C. Microarray analysis reveals distinct gene expression profiles among different histologic types of endometrial cancer. Cancer Res. 2003;63:6–11. [PubMed] [Google Scholar]
- 76.Fonseca B.M., Correia-da-Silva G., Teixeira N.A. Cannabinoid-induced cell death in endometrial cancer cells: Involvement of TRPV1 receptors in apoptosis. J. Physiol. Biochem. 2018;74:261–272. doi: 10.1007/s13105-018-0611-7. [DOI] [PubMed] [Google Scholar]
- 77.Ayakannu T. Investigation of Endocannabinoid Signalling and Their Regulations in Endometrial Carcinoma. [(accessed on 31 October 2020)]; Available online: https://leicester.figshare.com/articles/Investigation_of_Endocannabinoid_System_Signalling_Pathways_and_Their_Regulations_in_Endometrial_Carcinoma/10216328.
- 78.Ayakannu T., Taylor A.H., Bari M., Mastrangelo N., Maccarrone M., Konje J.C. Expression and function of the endocannabinoid modulating enzymes fatty acid amide hydrolase and N-acylphosphatidylethanolamine-specific phospholipase D in endometrial carcinoma. Front. Oncol. 2019;9:1363. doi: 10.3389/fonc.2019.01363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maccarrone M., DeFelici M., Klinger F.G., Battista N., Fezza F., Dainese E., Siracusa G., Finazzi-Agro A. Mouse blastocysts release a lipid which activates anandamide hydrolase in intact uterus. Mol. Hum. Reprod. 2004;10:215–221. doi: 10.1093/molehr/gah034. [DOI] [PubMed] [Google Scholar]
- 80.Habayeb O., Taylor A., Bharkhada R., Taylor D., Bell S., Konje J. Proceedings of British Congress of Obstetrics & Gynaecology Abstracts Book. Royal College of Obstetricians and Gynecologists; London, UK: 2004. Immunohistochemical localisation of cannabinoid receptor CB1 and fatty acid amide hydrolase (FAAH) in maternal and fetal tissues; p. 10. [Google Scholar]
- 81.Wang H., Xie H., Sun X., Kingsley P.J., Marnett L.J., Cravatt B.F., Dey S.K. Differential regulation of endocannabinoid synthesis and degradation in the uterus during embryo implantation. Prostaglandins Other Lipid Mediat. 2007;83:62–74. doi: 10.1016/j.prostaglandins.2006.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brighton P.J., Marczylo T.H., Rana S., Konje J.C., Willets J.M. Characterization of the endocannabinoid system, CB(1) receptor signalling and desensitization in human myometrium. Br. J. Pharmacol. 2011;164:1479–1494. doi: 10.1111/j.1476-5381.2011.01425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shen X., Duan H., Wang S., Hong W., Wang Y.Y., Lin S.L. Expression of cannabinoid receptors in myometrium and its correlation with dysmenorrhea in adenomyosis. Reprod. Sci. 2019;26:1618–1625. doi: 10.1177/1933719119833483. [DOI] [PubMed] [Google Scholar]
- 84.Contassot E., Tenan M., Schnuriger V., Pelte M.F., Dietrich P.Y. Arachidonyl ethanolamide induces apoptosis of uterine cervix cancer cells via aberrantly expressed vanilloid receptor-1. Gynecol. Oncol. 2004;93:182–188. doi: 10.1016/j.ygyno.2003.12.040. [DOI] [PubMed] [Google Scholar]
- 85.Eichele K., Ramer R., Hinz B. R(+)-methanandamide-induced apoptosis of human cervical carcinoma cells involves a cyclooxygenase-2-dependent pathway. Pharm Res. 2009;26:346–355. doi: 10.1007/s11095-008-9748-3. [DOI] [PubMed] [Google Scholar]
- 86.Yan L., Li J., Zhao T., Wang H., Lai G. [Over-expression of cannabinoid receptor 2 induces the apoptosis of cervical carcinoma Caski cells] Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2015;31:758–762. [PubMed] [Google Scholar]
- 87.Han G.H., Chay D.B., Nam S., Cho H., Chung J.Y., Kim J.H. The combination of transient receptor potential vanilloid type 1 (TRPV1) and phosphatase and tension homolog (PTEN) is an effective prognostic biomarker in cervical cancer. Int. J. Gynecol. Pathol. 2020 doi: 10.1097/PGP.0000000000000677. [DOI] [PubMed] [Google Scholar]
- 88.Milando R., Friedman A. Cannabinoids: Potential role in inflammatory and neoplastic skin diseases. Am. J. Clin. Dermatol. 2019;20:167–180. doi: 10.1007/s40257-018-0410-5. [DOI] [PubMed] [Google Scholar]
- 89.Marczylo T.H., Lam P.M., Amoako A.A., Konje J.C. Anandamide levels in human female reproductive tissues: Solid-phase extraction and measurement by ultraperformance liquid chromatography tandem mass spectrometry. Anal. Biochem. 2010;400:155–162. doi: 10.1016/j.ab.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 90.Brocato B., Zoerner A.A., Janjetovic Z., Skobowiat C., Gupta S., Moore B.M., 2nd, Slominski A., Zhang J., Schenone M., Phinehas R., et al. Endocannabinoid crosstalk between placenta and maternal fat in a baboon model (Papio spp.) of obesity. Placenta. 2013;34:983–989. doi: 10.1016/j.placenta.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Park B., Gibbons H.M., Mitchell M.D., Glass M. Identification of the CB1 cannabinoid receptor and fatty acid amide hydrolase (FAAH) in the human placenta. Placenta. 2003;24:990–995. doi: 10.1016/S0143-4004(03)00165-6. [DOI] [PubMed] [Google Scholar]
- 92.Fonseca B.M., Teixeira N.A., Almada M., Taylor A.H., Konje J.C., Correia-da-Silva G. Modulation of the novel cannabinoid receptor-GPR55-during rat fetoplacental development. Placenta. 2011;32:462–469. doi: 10.1016/j.placenta.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 93.Fonseca B.M., Correia-da-Silva G., Taylor A.H., Lam P.M., Marczylo T.H., Bell S.C., Konje J.C., Teixeira N.A. The endocannabinoid 2-arachidonoylglycerol (2-AG) and metabolizing enzymes during rat fetoplacental development: A role in uterine remodelling. Int. J. Biochem. Cell Biol. 2010;42:1884–1892. doi: 10.1016/j.biocel.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 94.Costa M.A., Fonseca B.M., Keating E., Teixeira N.A., Correia-da-Silva G. 2-arachidonoylglycerol effects in cytotrophoblasts: Metabolic enzymes expression and apoptosis in BeWo cells. Reproduction. 2014;147:301–311. doi: 10.1530/REP-13-0563. [DOI] [PubMed] [Google Scholar]
- 95.Ayakannu T., Taylor A.H., Willets J.M., Konje J.C. The evolving role of the endocannabinoid system in gynaecological cancer. Hum. Reprod. Update. 2015;21:517–535. doi: 10.1093/humupd/dmv022. [DOI] [PubMed] [Google Scholar]
- 96.Bagavandoss P., Grimshaw S. Temporal and spatial distribution of the cannabinoid receptors (CB1, CB2) and fatty acid amide hydroxylase in the rat ovary. Anat. Rec. (Hoboken) 2010;293:1425–1432. doi: 10.1002/ar.21181. [DOI] [PubMed] [Google Scholar]
- 97.Cui N., Feng X., Zhao Z., Zhang J., Xu Y., Wang L., Hao G. Restored plasma anandamide and endometrial expression of fatty acid amide hydrolase in women with polycystic ovary syndrome by the combination use of Diane-35 and metformin. Clin. Ther. 2017;39:751–758. doi: 10.1016/j.clinthera.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 98.Pirone A., Lenzi C., Briganti A., Abbate F., Levanti M., Abramo F., Miragliotta V. Spatial distribution of cannabinoid receptor 1 and fatty acid amide hydrolase in the cat ovary and oviduct. Acta Histochem. 2017;119:417–422. doi: 10.1016/j.acthis.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 99.Schuel H. Tuning the oviduct to the anandamide tone. J. Clin. Investig. 2006;116:2087–2090. doi: 10.1172/JCI29424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang H., Guo Y., Wang D., Kingsley P.J., Marnett L.J., Das S.K., DuBois R.N., Dey S.K. Aberrant cannabinoid signaling impairs oviductal transport of embryos. Nat. Med. 2004;10:1074–1080. doi: 10.1038/nm1104. [DOI] [PubMed] [Google Scholar]
- 101.Bambang K.N., Karasu T., Gebeh A., Taylor A.H., Marczylo T.H., Lam P., Willets J.M., Konje J.C. From fertilisation to implantation in mammalian pregnancy-modulation of early human reproduction by the endocannabinoid system. Pharmaceuticals. 2010;3:2910–2929. doi: 10.3390/ph3092910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Abolghasemi A., Dirandeh E., Ansari Pirsaraei Z., Shohreh B. Dietary conjugated linoleic acid supplementation alters the expression of genes involved in the endocannabinoid system in the bovine endometrium and increases plasma progesterone concentrations. Theriogenology. 2016;86:1453–1459. doi: 10.1016/j.theriogenology.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 103.Dirandeh E., Ghaffari J. Effects of feeding a source of omega-3 fatty acid during the early postpartum period on the endocannabinoid system in the bovine endometrium. Theriogenology. 2018;121:141–146. doi: 10.1016/j.theriogenology.2018.07.043. [DOI] [PubMed] [Google Scholar]
- 104.Scotchie J.G., Savaris R.F., Martin C.E., Young S.L. Endocannabinoid regulation in human endometrium across the menstrual cycle. Reprod. Sci. 2015;22:113–123. doi: 10.1177/1933719114533730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shen X., Duan H., Wang S., Gan L., Xu Q., Li J.J. Decreased expression of cannabinoid receptors in the eutopic and ectopic endometrium of patients with adenomyosis. Biomed. Res. Int. 2019;2019:5468954. doi: 10.1155/2019/5468954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Neradugomma N.K., Drafton K., Mor G.G., Mao Q. Marijuana-derived cannabinoids inhibit uterine endometrial stromal cell decidualization and compromise trophoblast-endometrium cross-talk. Reprod. Toxicol. 2019;87:100–107. doi: 10.1016/j.reprotox.2019.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Neradugomma N.K., Drafton K., O’Day D.R., Liao M.Z., Han L.W., Glass I.A., Mao Q. Marijuana use differentially affects cannabinoid receptor expression in early gestational human endometrium and placenta. Placenta. 2018;66:36–39. doi: 10.1016/j.placenta.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Taylor A.H., Amoako A.A., Bambang K., Karasu T., Gebeh A., Lam P.M., Marzcylo T.H., Konje J.C. Endocannabinoids and pregnancy. Clin. Chim. Acta. 2010;411:921–930. doi: 10.1016/j.cca.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 109.Rapino C., Battista N., Bari M., Maccarrone M. Endocannabinoids as biomarkers of human reproduction. Hum. Reprod. Update. 2014;20:501–516. doi: 10.1093/humupd/dmu004. [DOI] [PubMed] [Google Scholar]
- 110.Maccarrone M. Endocannabinoids: Friends and foes of reproduction. Prog. Lipid Res. 2009;48:344–354. doi: 10.1016/j.plipres.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 111.Maccarrone M. Endocannabinoids and reproductive biology. Hum. Reprod. 2009;24:1771. doi: 10.1093/humrep/dep111. [DOI] [PubMed] [Google Scholar]
- 112.Wang H., Dey S.K., Maccarrone M. Jekyll and hyde: Two faces of cannabinoid signaling in male and female fertility. Endocr. Rev. 2006;27:427–448. doi: 10.1210/er.2006-0006. [DOI] [PubMed] [Google Scholar]
- 113.El-Talatini M.R., Taylor A.H., Konje J.C. Fluctuation in anandamide levels from ovulation to early pregnancy in in-vitro fertilization-embryo transfer women, and its hormonal regulation. Hum. Reprod. 2009;24:1989–1998. doi: 10.1093/humrep/dep065. [DOI] [PubMed] [Google Scholar]
- 114.Sankaranarayanan R., Ferlay J. Worldwide burden of gynaecological cancer: The size of the problem. Best Pract. Res. Clin. Obstet. Gynaecol. 2006;20:207–225. doi: 10.1016/j.bpobgyn.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 115.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 116.Pertwee R.G., Howlett A.C., Abood M.E., Alexander S.P., Di Marzo V., Elphick M.R., Greasley P.J., Hansen H.S., Kunos G., Mackie K., et al. International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: Beyond CB(1) and CB(2) Pharmacol. Rev. 2010;62:588–631. doi: 10.1124/pr.110.003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jove M., Gatius S., Yeramian A., Portero-Otin M., Eritja N., Santacana M., Colas E., Ruiz M., Pamplona R., Matias-Guiu X. Metabotyping human endometrioid endometrial adenocarcinoma reveals an implication of endocannabinoid metabolism. Oncotarget. 2016;7:52364–52374. doi: 10.18632/oncotarget.10564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Leconte M., Nicco C., Ngo C., Arkwright S., Chereau C., Guibourdenche J., Weill B., Chapron C., Dousset B., Batteux F. Antiproliferative effects of cannabinoid agonists on deep infiltrating endometriosis. Am. J. Pathol. 2010;177:2963–2970. doi: 10.2353/ajpath.2010.100375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sun X., Dey S.K. Endocannabinoid signaling in female reproduction. ACS Chem. Neurosci. 2012;3:349–355. doi: 10.1021/cn300014e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang H., Xie H., Dey S.K. Endocannabinoid signaling directs periimplantation events. AAPS J. 2006;8:E425–E432. doi: 10.1007/BF02854916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bachkangi P., Taylor A.H., Bari M., Maccarrone M., Konje J.C. Prediction of preterm labour from a single blood test: The role of the endocannabinoid system in predicting preterm birth in high-risk women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019;243:1–6. doi: 10.1016/j.ejogrb.2019.09.029. [DOI] [PubMed] [Google Scholar]
- 122.Bari M., Battista N., Pirazzi V., Maccarrone M. The manifold actions of endocannabinoids on female and male reproductive events. Front. Biosci. (Landmark Ed.) 2011;16:498–516. doi: 10.2741/3701. [DOI] [PubMed] [Google Scholar]
- 123.Habayeb O.M., Taylor A.H., Evans M.D., Cooke M.S., Taylor D.J., Bell S.C., Konje J.C. Plasma levels of the endocannabinoid anandamide in women—A potential role in pregnancy maintenance and labor? J. Clin. Endocrinol. Metab. 2004;89:5482–5487. doi: 10.1210/jc.2004-0681. [DOI] [PubMed] [Google Scholar]
- 124.McCluggage W.G., Oliva E. Gynaecological pathology: Problematic areas, new concepts and emerging developments. Pathology. 2018;50:119–121. doi: 10.1016/j.pathol.2017.11.085. [DOI] [PubMed] [Google Scholar]
- 125.Ledford L.R.C., Lockwood S. Scope and Epidemiology of Gynecologic Cancers: An Overview. Semin. Oncol. Nurs. 2019;35:147–150. doi: 10.1016/j.soncn.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 126.Cancer Research UK Cancer Research Statistics, Cancer Incidence and Mortality in the UK. [(accessed on 2 September 2020)]; Available online: http://www.cancerresearchuk.org/cancer-info/cancerstats/types/uterus/
- 127.Canfell K., Kim J.J., Brisson M., Keane A., Simms K.T., Caruana M., Burger E.A., Martin D., Nguyen D.T.N., Bénard É., et al. Mortality impact of achieving WHO cervical cancer elimination targets: A comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395:591–603. doi: 10.1016/S0140-6736(20)30157-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Webb P.M. Environmental (nongenetic) factors in gynecological cancers: Update and future perspectives. Future Oncol. 2015;11:295–307. doi: 10.2217/fon.14.142. [DOI] [PubMed] [Google Scholar]
- 129.Matsuo K., Blake E.A., Machida H., Mandelbaum R.S., Roman L.D., Wright J.D. Incidences and risk factors of metachronous vulvar, vaginal, and anal cancers after cervical cancer diagnosis. Gynecol. Oncol. 2018;150:501–508. doi: 10.1016/j.ygyno.2018.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Khan M.I., Sobocińska A.A., Czarnecka A.M., Król M., Botta B., Szczylik C. The Therapeutic Aspects of the Endocannabinoid System (ECS) for Cancer and their Development: From Nature to Laboratory. Curr. Pharm. Des. 2016;22:1756–1766. doi: 10.2174/1381612822666151211094901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fraguas-Sánchez A.I., Martín-Sabroso C., Torres-Suárez A.I. Insights into the effects of the endocannabinoid system in cancer: A review. Br. J. Pharmacol. 2018;175:2566–2580. doi: 10.1111/bph.14331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Brown I., Cascio M.G., Rotondo D., Pertwee R.G., Heys S.D., Wahle K.W. Cannabinoids and omega-3/6 endocannabinoids as cell death and anticancer modulators. Prog. Lipid Res. 2013;52:80–109. doi: 10.1016/j.plipres.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 133.Suk K.T., Mederacke I., Gwak G.Y., Cho S.W., Adeyemi A., Friedman R., Schwabe R.F. Opposite roles of cannabinoid receptors 1 and 2 in hepatocarcinogenesis. Gut. 2016;65:1721–1732. doi: 10.1136/gutjnl-2015-310212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Green M. Cannabis and Your Vagina: Here’s the 411 on Cannabis Suppositories. [(accessed on 26 June 2020)]; Available online: https://www.byrdie.com/how-to-use-cannabis-suppositories-4771875.
- 135.Harper-Gold C. How to Get Your Vagina High. [(accessed on 26 June 2020)]; Available online: https://greenrushdaily.com/women/get-vagina-high/
- 136.Lowry J. Cannabinoids Can Cause Cell Death in Endometrial Cancer. [(accessed on 26 June 2020)]; Available online: https://www.cannahealth.org/cannabinoids-can-cause-cell-death-in-endometrial-cancer/
- 137.Moore G.R. Menopause: Cannabinoids & Sexual Health. [(accessed on 26 June 2020)]; Available online: https://www.foriawellness.com/blogs/learn/cbd-thc-sexual-health-menopause.
- 138.Smith D. Cannabis for Endometrial Cancer. [(accessed on 26 June 2020)]; Available online: https://cannabis.net/blog/medical/cannabis-for-endometrial-cancer.
- 139.Trassoff-Jilg V. Cannabinoids and Endometrial Cancer. [(accessed on 26 June 2020)]; Available online: https://waayb.com/cannabinoids-and-endometrial-cancer/
- 140.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2018. CA Cancer J. Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 141.Messalli E.M., Grauso F., Luise R., Angelini A., Rossiello R. Cannabinoid receptor type 1 immunoreactivity and disease severity in human epithelial ovarian tumors. Am. J. Obstet. Gynecol. 2014;211:P234.E1–P234.E6. doi: 10.1016/j.ajog.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 142.Xu Y., Xiao Y.J., Baudhuin L.M., Schwartz B.M. The role and clinical applications of bioactive lysolipids in ovarian cancer. J. Soc. Gynecol. Investig. 2001;8:1–13. doi: 10.1177/107155760100800101. [DOI] [PubMed] [Google Scholar]
- 143.Hofmann N.A., Yang J., Trauger S.A., Nakayama H., Huang L., Strunk D., Moses M.A., Klagsbrun M., Bischoff J., Graier W.F. The GPR 55 agonist, L-alpha-lysophosphatidylinositol, mediates ovarian carcinoma cell-induced angiogenesis. Br. J. Pharmacol. 2015;172:4107–4118. doi: 10.1111/bph.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Deng H., Li W. Monoacylglycerol lipase inhibitors: Modulators for lipid metabolism in cancer malignancy, neurological and metabolic disorders. Acta Pharm. Sin. B. 2020;10:582–602. doi: 10.1016/j.apsb.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Fraguas-Sanchez A.I., Torres-Suarez A.I., Cohen M., Delie F., Bastida-Ruiz D., Yart L., Martin-Sabroso C., Fernandez-Carballido A. PLGA nanoparticles for the intraperitoneal administration of CBD in the treatment of ovarian cancer: In Vitro and In Ovo assessment. Pharmaceutics. 2020;12:439. doi: 10.3390/pharmaceutics12050439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gebeh A.K., Willets J.M., Bari M., Hirst R.A., Marczylo T.H., Taylor A.H., Maccarrone M., Konje J.C. Elevated anandamide and related N-acylethanolamine levels occur in the peripheral blood of women with ectopic pregnancy and are mirrored by changes in peripheral fatty acid amide hydrolase activity. J. Clin Endocrinol. Metab. 2013;98:1226–1234. doi: 10.1210/jc.2012-3390. [DOI] [PubMed] [Google Scholar]
- 147.Bokhman J.V. Two pathogenetic types of endometrial carcinoma. Gynecol. Oncol. 1983;15:10–17. doi: 10.1016/0090-8258(83)90111-7. [DOI] [PubMed] [Google Scholar]
- 148.Leslie K.K., Thiel K.W., Goodheart M.J., De Geest K., Jia Y., Yang S. Endometrial cancer. Obstet. Gynecol. Clin. N. Am. 2012;39:255–268. doi: 10.1016/j.ogc.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhang Y., Zheng W., Shen K., Shen W. 9-tetrahydrocannabinol inhibits epithelial-mesenchymal transition and metastasis by targeting matrix metalloproteinase-9 in endometrial cancer. Oncol. Lett. 2018;15:8527–8535. doi: 10.3892/ol.2018.8407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rosado J. Endometrial Cancer. [(accessed on 26 June 2020)]; Available online: https://www.marijuanadoctors.com/conditions/endometrial-cancer/
- 151.Freimuth N., Ramer R., Hinz B. Antitumorigenic effects of cannabinoids beyond apoptosis. J. Pharmacol. Exp. Ther. 2010;332:336–344. doi: 10.1124/jpet.109.157735. [DOI] [PubMed] [Google Scholar]
- 152.International Agency for Research on Cancer [Internet] GLOBOCAN 2012 v1.0 (2013): IARC Publications Website—Cancer Today (powered by GLOBOCAN 2018)–IARC CancerBase No. 15. [(accessed on 24 December 2020)]; Available online: https://publications.iarc.fr/577.
- 153.Ramer R., Merkord J., Rohde H., Hinz B. Cannabidiol inhibits cancer cell invasion via upregulation of tissue inhibitor of matrix metalloproteinases-1. Biochem. Pharmacol. 2010;79:955–966. doi: 10.1016/j.bcp.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 154.Barrie A.M., Gushue A.C., Eskander R.N. Dramatic response to Laetrile and cannabidiol (CBD) oil in a patient with metastatic low grade serous ovarian carcinoma. Gynecol. Oncol. Rep. 2019;29:10–12. doi: 10.1016/j.gore.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lukhele S.T., Motadi L.R. Cannabidiol rather than Cannabis sativa extracts inhibit cell growth and induce apoptosis in cervical cancer cells. BMC Complement. Altern. Med. 2016;16:335. doi: 10.1186/s12906-016-1280-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.American Cancer Society Key Statistics for Vaginal Cancer. [(accessed on 26 June 2020)]; Available online: https://www.cancer.org/cancer/vaginal-cancer/about/key-statistics.html.
- 157.Rosado J. Vaginal Cancer. [(accessed on 26 June 2020)]; Available online: https://www.marijuanadoctors.com/conditions/vaginal-cancer/
- 158.Rogers L.J., Cuello M.A. Cancer of the vulva. Int. J. Gynaecol. Obstet. 2018;143 (Suppl. 2)(Suppl. 2):4–13. doi: 10.1002/ijgo.12609. [DOI] [PubMed] [Google Scholar]
- 159.Sangiovanni E., Fumagalli M., Pacchetti B., Piazza S., Magnavacca A., Khalilpour S., Melzi G., Martinelli G., Dell’Agli M. Cannabis sativa L. extract and cannabidiol inhibit in vitro mediators of skin inflammation and wound injury. Phytother. Res. 2019;33:2083–2093. doi: 10.1002/ptr.6400. [DOI] [PubMed] [Google Scholar]
- 160.Stabile C., Gunn A., Sonoda Y., Carter J. Emotional and sexual concerns in women undergoing pelvic surgery and associated treatment for gynecologic cancer. Transl. Androl. Urol. 2015;4:169–185. doi: 10.3978/j.issn.2223-4683.2015.04.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Del Rio C., Cantarero I., Palomares B., Gomez-Canas M., Fernandez-Ruiz J., Pavicic C., Garcia-Martin A., Luz Bellido M., Ortega-Castro R., Perez-Sanchez C., et al. VCE-004.3, a cannabidiol aminoquinone derivative, prevents bleomycin-induced skin fibrosis and inflammation through PPARgamma- and CB2 receptor-dependent pathways. Br. J. Pharmacol. 2018;175:3813–3831. doi: 10.1111/bph.14450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Stinchcomb A.L., Valiveti S., Hammell D.C., Ramsey D.R. Human skin permeation of Delta8-tetrahydrocannabinol, cannabidiol and cannabinol. J. Pharm. Pharmacol. 2004;56:291–297. doi: 10.1211/0022357022791. [DOI] [PubMed] [Google Scholar]
- 163.Fonseca B.M., Correia-da-Silva G., Taylor A.H., Lam P.M., Marczylo T.H., Konje J.C., Teixeira N.A. Characterisation of the endocannabinoid system in rat haemochorial placenta. Reprod. Toxicol. 2012;34:347–356. doi: 10.1016/j.reprotox.2012.05.036. [DOI] [PubMed] [Google Scholar]
- 164.Battista N., Bari M., Rapino C., Trasatti F., D’Agostino A., Maccarrone M. Regulation of female fertility by the endocannabinoid system. Hum. Fertil. (Camb.) 2007;10:207–216. doi: 10.1080/14647270701429879. [DOI] [PubMed] [Google Scholar]
- 165.Battista N., Pasquariello N., Di Tommaso M., Maccarrone M. Interplay between endocannabinoids, steroids and cytokines in the control of human reproduction. J. Neuroendocrinol. 2008;20(Suppl. 1):82–89. doi: 10.1111/j.1365-2826.2008.01684.x. [DOI] [PubMed] [Google Scholar]
- 166.Maccarrone M. Endocannabinoids and reproductive endocrinology. Curr. Opin. Investig. Drugs. 2009;10:305–310. [PubMed] [Google Scholar]
- 167.Lockwood C.J. Prediction of pregnancy loss. Lancet. 2000;355:1292–1293. doi: 10.1016/S0140-6736(00)02108-5. [DOI] [PubMed] [Google Scholar]
- 168.Costa M.A., Fonseca B.M., Marques F., Teixeira N.A., Correia-da-Silva G. The psychoactive compound of Cannabis sativa, Delta(9)-tetrahydrocannabinol (THC) inhibits the human trophoblast cell turnover. Toxicology. 2015;334:94–103. doi: 10.1016/j.tox.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 169.Frank D.A., Bauchner H., Parker S., Huber A.M., Kyei-Aboagye K., Cabral H., Zuckerman B. Neonatal body proportionality and body composition after in utero exposure to cocaine and marijuana. J. Pediatrics. 1990;117:622–626. doi: 10.1016/S0022-3476(05)80702-4. [DOI] [PubMed] [Google Scholar]
- 170.Sidney S. Cardiovascular consequences of marijuana use. J. Clin. Pharmacol. 2002;42:64S–70S. doi: 10.1002/j.1552-4604.2002.tb06005.x. [DOI] [PubMed] [Google Scholar]
- 171.Taylor A.H., Abbas M.S., Bell S.C., Konje J.C. The inhibitory effect of delta9-tetrahydrocannabinol on trophoblast cell proliferation and transcription is mediated via the CB-2 receptor. Br. J. Obstet. Gynaecol. 2006;114:1040. [Google Scholar]
- 172.Taylor A.H., Abbas M.S., Bell S.C., Konje J.C. The inhibitory effect of delta9-tetrahydrocannabinol on trophoblast cell proliferation and transcription is mainly mediated via the CB-2 receptor. Reprod. Sci. 2007;14:720. [Google Scholar]
- 173.Maia J., Midao L., Cunha S.C., Almada M., Fonseca B.M., Braga J., Goncalves D., Teixeira N., Correia-da-Silva G. Effects of cannabis tetrahydrocannabinol on endocannabinoid homeostasis in human placenta. Arch. Toxicol. 2019;93:649–658. doi: 10.1007/s00204-019-02389-7. [DOI] [PubMed] [Google Scholar]
- 174.Sarrafpour S., Urits I., Powell J., Nguyen D., Callan J., Orhurhu V., Simopoulos T., Viswanath O., Kaye A.D., Kaye R.J., et al. Considerations and implications of cannabidiol use during pregnancy. Curr. Pain Headache Rep. 2020;24:38. doi: 10.1007/s11916-020-00872-w. [DOI] [PubMed] [Google Scholar]
- 175.Taylor B.N., Mueller M., Sauls R.S. StatPearls. Statpearls Publishing; Treasure Island, FL, USA: 2020. Cannaboinoid antiemetic therapy. [PubMed] [Google Scholar]
- 176.Almada M., Amaral C., Oliveira A., Fernandes P.A., Ramos M.J., Fonseca B.M., Correia-da-Silva G., Teixeira N. Cannabidiol (CBD) but not tetrahydrocannabinol (THC) dysregulate in vitro decidualization of human endometrial stromal cells by disruption of estrogen signaling. Reprod. Toxicol. 2020;93:75–82. doi: 10.1016/j.reprotox.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 177.Feinshtein V., Erez O., Ben-Zvi Z., Erez N., Eshkoli T., Sheizaf B., Sheiner E., Huleihel M., Holcberg G. Cannabidiol changes P-gp and BCRP expression in trophoblast cell lines. PeerJ. 2013;1:e153. doi: 10.7717/peerj.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Thomas A., Baillie G.L., Phillips A.M., Razdan R.K., Ross R.A., Pertwee R.G. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br. J. Pharmacol. 2007;150:613–623. doi: 10.1038/sj.bjp.0707133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Correa F., Wolfson M.L., Valchi P., Aisemberg J., Franchi A.M. Endocannabinoid system and pregnancy. Reproduction. 2016;152:R191–R200. doi: 10.1530/REP-16-0167. [DOI] [PubMed] [Google Scholar]
- 180.Whiting P.F., Wolff R.F., Deshpande S., Di Nisio M., Duffy S., Hernandez A.V., Keurentjes J.C., Lang S., Misso K., Ryder S., et al. Cannabinoids for medical use: A systematic review and meta-analysis. JAMA. 2015;313:2456–2473. doi: 10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- 181.Blake E.A., Ross M., Ihenacho U., Figueroa L., Silverstein E., Flink D., Mendez-Ishizaki Y., Yessaian A., Brunette L.L., Matsuo K., et al. Non-prescription cannabis use for symptom management amongst women with gynecologic malignancies. Gynecol. Oncol. Rep. 2019;30:100497. doi: 10.1016/j.gore.2019.100497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Totorikaguena L., Olabarrieta E., Lolicato F., Romero-Aguirregomezcorta J., Smitz J., Agirregoitia N., Agirregoitia E. The endocannabinoid system modulates the ovarian physiology and its activation can improve in vitro oocyte maturation. J. Cell Physiol. 2020 doi: 10.1002/jcp.29663. [DOI] [PubMed] [Google Scholar]
- 183.Maccarrone M., Falciglia K., Di Rienzo M., Finazzi-Agro A. Endocannabinoids, hormone-cytokine networks and human fertility. Prostaglandins Leukot. Essent. Fatty Acids. 2002;66:309–317. doi: 10.1054/plef.2001.0354. [DOI] [PubMed] [Google Scholar]
- 184.Guzman M. Cannabis for the management of cancer symptoms: THC version 2.0? Cannabis Cannabinoid Res. 2018;3:117–119. doi: 10.1089/can.2018.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Maccarrone M. Phytocannabinoids and endocannabinoids: Different in nature. Rend. Lincei. 2020;31:931–938. doi: 10.1007/s12210-020-00957-z. [DOI] [Google Scholar]