Abstract
Severe illnesses in children and adolescents/young adults (AYAs) may represent a complex burden for patients and their caregivers, including a wide range of mental disorders, particularly post-traumatic stress disorder (PTSD). Few events are as potentially traumatizing as having a son or a daughter diagnosed with a severe, life-threatening, or disabling disease. The presence of PTSD symptoms in caregivers may compromise their efficacy as caregivers and negatively affect the child’s well-being. This systematic review aims at outlining potential risk and protective factors for the development of PTSD symptoms in caregivers of children and AYAs affected by severe acute or chronic illnesses. Thirty-one studies on caregivers of children and AYAs affected by severe, acute, or chronic diseases were included. Socio-demographic and socio-economic characteristics, illness-related distress, psychiatric symptoms, support, and coping styles were found as potential risk/protective factors across studies. It is crucial to consider risk factors affecting caregivers of severely ill young patients, in order to plan focused interventions aimed at preventing an adverse clinical outcome in caregivers and at enhancing caregivers’ coping skills, in order to ultimately improve their quality of life.
Keywords: post-traumatic stress disorder (PTSD), post-traumatic stress symptoms (PTSS), caregiving burden, parents, psychological distress
1. Introduction
Severe acute or chronic illnesses represent a stressful burden for patients and their caregivers. Moreover, they may favor the onset of a wide range of psychological problems in carers, such as depression, anxiety, sleep disturbances, and post-traumatic stress disorder (PTSD) [1,2,3,4,5,6,7,8,9]. PTSD is a condition that may occur after traumatic events, life-threatening events, or painful experiences [10,11,12]. Subjects with PTSD are not necessarily the victims of an event: witnessing, being involved, or being informed of a traumatic event happened to a beloved one may trigger the onset of PTSD [13]. In this regards, few events are as potentially traumatizing as having a child diagnosed with a possibly life-threatening or disabling disease [14]. Particularly, the Diagnostic and Statistical Manual of Mental Disorders—fifth edition (DSM-5) introduced illness in one’s child among the events considered as traumatic (“a medical catastrophe concerning one’s child”), specifying that the event must represent a condition that endangers life at the moment [15]. Consequently, this definition overcame the previous DSM-IV-TR statement that required learning that one’s child has a life-threatening disease [16,17], highlighting the need for the traumatic event to be sudden and dangerous, focusing on the urgency and abruptness of the perceived threat [18,19]. However, many authors have also discussed the clinical relevance of so-called “minor” events in the development of full and, similarly disabling, partial post-traumatic symptomatology, adopting a wide approach of spectrum to trauma and traumatic event, focused on individual experience vulnerability [20]. In this perspective, increasing attention has been deserved to PTSD among parents and caregivers of paediatric patients affected by severe but heterogeneous medical conditions characterized by a severe impairment or a chronic course, even a significant risk of mortality, as cancer, leukaemia/lymphoma, diabetes, neurological acute (ischemic, haemorrhagic, traumatic injury) or chronic (epilepsy) conditions, psychiatric and neurodevelopment disorders (such as autism), sex development disorders, burn injury, severe asthma crisis, illnesses that needed transplant surgery, pointing out the potential traumatic role of such experiences [21,22,23,24]. Severe medical conditions occurring to loved ones could be one of the strongest factors associated to PTSD [24]. However, only recently researchers began to focus on PTSD in parents of children with chronic illnesses [14,21,22,23]. Studies using the DSM criteria for PTSD diagnosis reported incidences of current cancer-related PTSD ranging from 6.2% to 25% parents’ childhood cancer survivors, while clinically severe levels of PTSD symptoms ranged from 9.8% to 44% [21]. Similarly, in diabetes type 1 studies, up to a quarter of the parents met the DSM criteria for PTSD diagnosis 6 weeks after their child’s diagnosis, while 15% of mothers still met criteria for a partial diagnosis of PTSD and 10% met criteria for the full diagnosis up to 5 years after [23].
Post-traumatic stress symptoms (PTSS) include nuanced or attenuated symptomatology belonging to the traumatic reaction, as intrusion symptoms, persistent avoidance, negative alterations in cognitions and mood, alterations in arousal and activity. Nevertheless, growing findings suggest partial or sub-threshold PTSD conditions being related to an impairment in family, work, and social adjustment as full-blown syndromes, often representing a problem not only during the acute phase but also across extended periods after the traumatic exposure [25,26]. PTSS in parents may affect their caregiver role and adversely impact on the child’s behavior, response to treatment, and treatment outcome. Arousal or re-experiencing symptoms, in fact, may compromise the caregiver’s adherence to medical guidelines or to report essential information to health professionals [27]. Hyper-vigilant caregivers may request frequent doctor visits or make an excessive number of accesses to medical services [28]. On the other hand, caregivers with active avoidance may pass over medical visits or refuse necessary medical procedures [29]. Parallel, the impact of parent’s stress on the child may be detrimental for the child’s well-being [30], and PTSD symptoms in parents can have negative implications for their child’s behavior or adjustment in the long-term, as well as impair the parent–child relationship [31]. Moreover, while struggling with their difficulties in dealing with stress, caregivers often have a reduced access to support and resources [32,33]. Furthermore, PTSD has been positively associated to an increased risk of other psychopathological conditions and substance abuse, leading to a well-being impairment [34,35,36]. In this line, increasing evidence suggests that PTSD or PTSS could be associated to the onset of depression, suicidal behavior, anxiety, sleep problems, and other conditions in cares that worse their quality of life [1,2,4,7,9].
Although a lack of studies in this research area [37], interventions to prevent PTSS, and enhance resilience are likely to relieve the suffering of the parents (and indirectly of the young patients) and maintain their caregiver ability. Indeed, some studies found a role of resilience-focused interventions in improving caregivers’ quality of life [38,39]. It seems primary to recognize possible PTSD risk factors (such as gender, age, carers’ mental health history, characteristics of the child’s illness, and other factor that could be positively associated to PTSD), as well as other variables that could represent protective factors for PTSD development in cares (as positive coping styles or availability of familiar of healthcare service support, and other variables which could be negatively associated to PTSD). Therefore, the present systematic review aimed at exploring the possible risk and protective factors for the development of PTSD and PTSS in caregivers of children and adolescents/young adults (AYAs) affected by severe illnesses, in order to plan interventions aimed at promoting the mental well-being of both caregivers and young patients.
2. Materials and Methods
2.1. Literature Search
A systematic search was conducted from 1st September 2020 to 30th September 2020 by searching the electronic databases PubMed, Ovid, and EMBASE. All studies from 1 January 1990 to 31 August 2020 were included in the databases search. The combination of search terms without filters, restrictions, or limits was utilized: (PTSD OR post-traumatic stress OR post-traumatic stress disorder OR post-traumatic stress symptoms OR PTSS OR post-traumatic stress reaction) AND (caregiver OR caregivers OR parents OR mothers OR fathers).
2.2. Eligibility Criteria
The following criteria were utilized to include studies in the present review:
Full-text publications reporting data related to PTSD and PTSS in caregivers of children and AYAs (aged between 0–25 years) affected by severe illnesses (i.e., chronic or acute, life threatening or disabling diseases).
Articles assessing possible risk (positively associated) and/or protective (negatively associated) factors for PTSD and PTSS in caregivers.
Articles available in English.
2.3. Screening and Selection Process
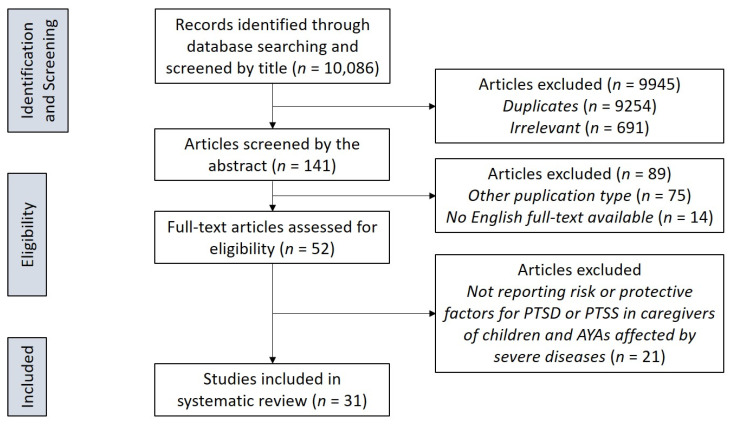
The primary database search provided a total of 10,086 records. Whereupon, 10,034 publications were removed after titles and abstracts screening because they were duplicates (N = 9254) or not relevant (i.e., they did not investigate the PTSD symptoms, or caregivers or were not research studies) (N = 691), or because full-text was not available or not in English (N = 14), or were reviews or metanalyses (N = 75). Fifty-two articles passed the initial screening. The relevant references cited in the selected studies, besides in review and metanalyses found in the initial search, were also manually screened to complete our search. However, no further eligible studies emerged in the process of manual screening. Data extraction and eligibility assessment were performed independently by two raters. Any disagreements highlighted during the process was discussed, and consensus reached. Finally, 31 studies were included in the present review. Details of the screening process are summarized in Figure 1, illustrating a flow chart according to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) recommendations [40].
Figure 1.
PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) flowchart of the study selection process.
3. Results
The search yielded 31 studies that were included in the review (see Figure 1). In our search, the large majority of the studies analyzed was on caregivers of children and AYAs affected by tumors, investigated by fourteen studies [41,42,43,44,45,46,47,48,49,50,51,52,53,54]. The remaining diagnostic categories of children and AYAs whose caregivers were investigated for PTSD were very heterogeneous and less numerous, and included neonatal intensive care unit (NICU) patients [55,56], epilepsy [57,58], burn injuries, and other accidents [41,59,60,61], disorders of sex development [62,63], asthma [64], transplants [65,66,67,68], HIV [66], Sickle cell disease [66], diabetes mellitus type 1 [41], and neuro-psychiatric disorders [69,70,71]. Characteristics of included studies are described in Table 1.
Table 1.
Characteristics of the reviewed studies divided by study type.
| Study | Year | Country | Sample | PTSD/PTSS Measures |
PTSD/PTSS Rates |
Risk/Protective Factors |
|---|---|---|---|---|---|---|
| Longitudinal studies | ||||||
| De Young et al. [60] | 2014 | Australia | 120 parents of children with burn injuries | PDS | PTSD: 22% at 1 month post-injury 5% at 6 months | Risk factors:
|
| Harper et al. [45] | 2013 | USA | 75 parents of pediatric cancer patients on the day of each of three medical procedures | IES-R | Not reported | Protective factors:
|
| Malin et al. [56] | 2019 | USA | 162 parents three months after discharge from ≥14 days of NICU | PPQ | PTSD: 25% | Risk factors:
|
| Young et al. [65] | 2003 | USA | 170 caregivers of pediatric transplant recipients | PDS | PTSD: 27.1% | Risk factors:
|
| Cross-sectional studies | ||||||
| Aftyka and Rozalska [55] | 2020 | Poland | 82 parents of infants previously treated in NICU | IES-R | PTSD: 68.5% fathers, 82.9% mothers | Risk factors:
|
| Bruce et al. [44] | 2011 | UK | 52 parents of children with brain tumor | IES-R | PTSD: 29% | Risk factors:
|
| Carmassi et al. [57] | 2018 | Italy | 134 Parents of children with a diagnosis of epilepsy | SCID-5 TALS-SR |
PTSD: 10.4% parents (13.3% of the mothers and 4.5% of the fathers). Partial PTSD 37.3% (mothers 43.3% and fathers 25.0%) | Risk factors:
|
| Casey et al. [69] | 2012 | USA | 265 parents of children with ASD | IES-R | PTSS: 20% | Risk factors:
|
| Dell’Osso et al. [58] | 2018 | Italy | 134 parents (90 mothers and 44 fathers), of patients aged below 18 years old diagnosed with an epileptic syndrome |
SCID-5; TALS-SR |
PTSD: 10.4% (13.3% mothers and 4.5% fathers); 37.3% (43.3% of the mothers and 25.0% of the fathers) partial PTSD | Risk factors:
|
| Hawkins et al. [61] | 2019 | UK | 91 parents and primary caregivers (63 mothers, 25 fathers, 3 other) of children during the first 8 weeks following child’s burn injury |
IES-R | PTSD: 32.8% of women, 40% of men | Risk factors:
|
| Ingerski et al. [66] | 2010 | USA | 64 parents of children with chronic illnesses | IES-R | PTSD: 12.9% (14.3% transplantation, 7.7% HIV, 14.3% SCD) | Risk factors:
|
| Jurbergs et al. [43] | 2009 | USA | 199 parents of children with cancer | IES-R | Not reported | Risk factors:
|
| Juth et al. [47] | 2015 | USA | 110 caregivers of AYAs cancer patients | PCL | Not reported | Risk factors:
|
| Khalifa et al. [46] | 2014 | Egypt | 96 parents of children with acute lymphoblastic leukemia and 22 parents of healthy controls. Patients divided into five groups according to disease phase |
PTSD Assessment Scale | Not reported | Risk factors:
|
| Landolt et al. [41] | 2003 | Switzerland | 355 parents of children 5–6 weeks after an accident or a new diagnosis of cancer or diabetes mellitus type 1 | PDS | PTSD: 39.9% (16% fathers and 23.9% mothers) | Risk factors:
|
| Malpert et al. [48] | 2015 | USA | 127 parents of long-term survivors of childhood Acute Lymphoblastic Leukemia | IES-R | PTSS: 3.9% | Risk factors:
|
| Masa’deh and Jarrah [50] | 2017 | Jordan | 416 parents of children with cancer | PCL-C | Not reported | Risk factors:
|
| McCarthy et al. [49] | 2016 | Australia | 204 parent caregivers of AYAs diagnosed with cancer | PCL-S | PTSS: 42% | Risk factors:
|
| McCarthy et al. [52] | 2018 | Australia | 204 parent caregivers of AYAs diagnosed with cancer | PCL-S | Not reported | Risk factors:
|
| Odar et al. [59] | 2013 | USA | 45 parents of children with burn injuries | PCL-S | PTSD: 4.44% | Risk factors:
|
| Pasterski et al. [62] | 2014 | UK | 47 parents of children diagnosed with disorders of sex development | IES-R | PTSD: 49% | Risk factors:
|
| Perez et al. [53] | 2018 | USA | 59 caregivers of pediatric cancer patients | IES-R | PTSS: 25.42% | Risk factors:
|
| Perez et al. [63] | 2019 | USA | 139 parents (76 mothers and 63 fathers) of children with disorders of sex development | IES-R | PTSS: 17% | Risk factors:
|
| Perez et al. [54] | 2020 | USA | 145 caregivers of children diagnosed with cancer | IES-R | PTSS: 27.4% | Risk factors:
|
| Phipps et al. [42] | 2005 | USA | 120 parents of children with cancer | IES-R | Not reported | Risk factors:
|
| Sawyer et al. [51] | 2017 | Australia | 204 parents of AYAs with cancer | PCL-S | Not reported | Risk factors:
|
| Steinberg et al. [64] | 2012 | USA | 120 caregivers of children with asthma | SCID-I | PTSD: 20.83% (lifetime diagnosis, prior to the past 12-months) | Risk factors:
|
| Stewart et al. [71] | 2020 | Australia | 395 parents of children with ASD and rare diseases | PCL-5 | PTSD: 40.8% (ASD 23.5%; Rare diseases: 17.3%) | Risk factors:
|
| Taskiran et al. [68] | 2016 | Turkey | 27 mothers of children who underwent bone marrow transplantation | CAPS | PTSD: 57.6% | Risk factors:
|
| Tutus & Goldbeck [70] | 2016 | Germany | 113 parents of children and adolescents with PTSD | PDS | PTSS: 48.6% | Risk factors:
|
| Virtue et al. [67] | 2014 | USA | 215 caregivers of children undergoing hematopoietic stem cell transplant (HSCT) | IES-R | PTSS: 54% | Risk factors:
|
IES-r, Impact of Event Scale-Revised; PPQ, Perinatal PTSD Questionnaire; PCL-5, PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders 5th edition; PCL-C, PTSD Checklist-Civilian Version; PCL-S, Post-traumatic stress disorder checklist, version S; PDS, Post-traumatic Diagnostic Scale; PTSD, Post-Traumatic Stress Disorder; PTSS, Post-Traumatic Stress Symptoms; SCID-5, Structured Clinical Interview for DSM-5; SCID-I, Clinical Interview for DSM-IV-TR Axis I Disorders; SCID-IV, Structured Clinical Interview for DSM-IV; TALS-SR Trauma and Loss Spectrum—Self Report.
A large majority of the studies adopted the Impact of Event Scale- Revised (IES-R) [42,43,44,45,48,53,54,55,61,62,63,66,67,69], a self-report questionnaire used to assess probable PTSD by covering all three symptoms clusters (intrusion, avoidance, hyperarousal) through 22 items and in which individuals with a score equal or above 24 were considered to have clinically significant post-traumatic stress symptoms (PTSS), while those with a score equal or higher than 33 a probable PTSD diagnosis [72]. Other tools used in the studies included in the present review were various version of the Posttraumatic Stress Disorder Checklist (PCL) [47,49,50,51,52,59,71]. Particularly, the PCL, the PCL-civilian (PCL-C) and the PCL- specific (PCL-S) are self-report rating scale for assessing the 17 DSM-IV symptoms of PTSD. The cut-off for assessing PTSD diagnosis among studies. The PCL for the DSM-5 (PCL-5) is a 20-item self-report measure that assesses the 20 DSM-5 symptoms of PTSD. A cut-off of >33 combined to the endorsement of a cluster criteria represents a good predictor of a PTSD diagnosis [73,74]. Moreover, with this scale PTSD symptoms were identified as clinically significant (PTSS) if the participant was at least “moderately bothered” by at least one reexperiencing cluster symptom, three avoidance cluster symptoms, or two arousal cluster symptoms [59]. Four studies used the post-traumatic diagnostic scale (PDS), a 49 item self-report questionnaire corresponding to the DSM-IV PTSD criteria and in which individuals received a probable PTSD diagnosis if their answers met DSM-IV PTSD Criteria A-F, while a score equal or higher than 21 was considered predictive of at-least moderate-severe PTSS [60]. Two studies used the trauma and loss spectrum-self report (TALS), a self-report tool including 116 items that explores the lifetime experience of losses, traumatic events and PTSD symptoms, behaviors and personal characteristics that might represent manifestations and/or risk factors for the development of PTSD [26]. With this instrument, DSM-5 PTSD diagnosis was assessed utilizing a matching system between symptom criteria and TALS-SR items, and a probable partial PTDS diagnosis was predicted if individuals met two or three of the DSM-5 B, C, D, and E criteria for PTSD [57,58]. Finally, the remaining tools were used only once, and two were self-report measures: the Post-traumatic Stress Disorder Assessment Scale [46], the Post-traumatic stress disorder questionnaire (PPQ) [56], and the Clinician-Administered PTSD Scale (CAPS) [68], a questionnaire administered by a trained clinician.
Particularly, PTSD prevalence rates ranged from 4.44% [59] to 82.9% [55], and PTSS prevalence rates from 3.9% [48] to 54% [67].
3.1. Risk Factors for PTSD/PTSS
We identified the following risk factors for PTSD and PTSS: socio-demographic and socio-economic characteristics; illness-related distress; psychiatric symptoms and negative/maladaptive coping.
3.1.1. Socio-Demographic and Socio-Economic Characteristics
Women were found to be at statistically significantly higher risk of developing PTSS with respect to men in five studies [42,46,50,58,63]. In a sample of 134 parents of pediatric patients with epilepsy, Carmassi et al. reported PTSD in 13.3% of mothers and 4.5% of fathers, and an additional 43.3% of the mothers and 25.0% of the fathers, presented partial PTSD [58]. Younger age of one’s child/AYA was found to be a risk factor for developing PTSD in caregivers in four studies [51,59,61,62]. Moreover, other authors found that younger age of parents too was related to an increased risk of PTSD [50]. Furthermore, some authors [49], examining a sample of 204 parent caregivers of AYAs with cancer, found that the presence of other life stressors, a more severe impact of patient’s illness on plans for the future and on the broader family, was associated with increased PTSS levels. These authors also highlighted an association between PTSS and living outside the metropolitan area. A study on a sample of 265 parents of children with autism spectrum disorder (ASD) showed that having other life stressors, as having one biological parent not living in the home, having two or more children diagnosed with ASD, difficulties finding or holding a job or marital problems, were related to an increased risk of PTSS [69]. Moreover, having a lower household income and increased expenses related to the disease, were found to be associated to PTSD symptoms severity in fathers [53,63]. More widely, some other authors investigating a sample of 45 parents of children post-burn, found that the level of familiar stress prior to the burn event was related to higher PTSS in caregivers [59]. Finally, only one study pointed out that married subjects had an increased risk of developing PTSS [67].
3.1.2. Illness-Related Distress
Longer stays in hospital [61] as well as objective illness severity [56] have been associated to increased risk of PTSD. Ingerski et al. [66], in a sample of 64 caregivers of children experiencing a chronic illness, found that being caregivers of transplant candidates was a risk factor for developing PTSD. Moreover, another study on 215 caregivers of children undergoing hematopoietic stem cell transplant, highlighted higher PTSS levels in caregivers of allogeneic transplant patients, a procedure associated with greater medical complications and risk of mortality than autologous transplant [67]. Perez et al. [53], in a study on 59 parents of children with cancer, found that illness uncertainty acted indirectly as a risk factor, through ruminations, in enhancing PTSS. Moreover, in a more recent study on the same sample expanded up to 145 caregivers of children with cancer, authors found a significant direct relationship between illness uncertainty and PTSS [54]. The disease status was also found to be an important factor, as parents of relapsed children [51] and parents of patients with a greater number of tumor recurrences [44] were at higher risk of PTSS, as well as parents of recently diagnosed patients [42]. Conversely, being no longer on active treatment was associated to a reduction in PTSS [43]. De Young et al. [60], in a sample of 120 parents of children with burn injuries, found that having a higher number of invasive procedures was related to higher PTSS. Another study found an association between objective severity of disease and PTSS. Indeed, Landolt et al. [41] found in a sample of 355 parents of children 5–6 weeks after an accident or a new diagnosis of cancer or diabetes mellitus type 1, that having a diagnosis of cancer were related to higher PTSS in caregivers with respect to the other diagnosis or a poorer functional status of the child. Furthermore, Carmassi et al. [57], in a study on 134 parents of children with epilepsy, highlighted the subjective impact of medical event as a factor enhancing PTSS and, similarly, a greater subjective illness severity was found to be a risk factor by two other studies [47,56]. Indeed, Juth et al. [47] on a sample of 110 caregivers of AYA cancer patients undergoing active treatment at an outpatient clinic, found an association between caregivers’ subjective illness severity and their own PTSS. Malin et al. [56], examining a sample of parents of infants who were in the NICU for more than 14 days, found that parent perceptions of illness were associated with PTSD symptoms, after adjusting for objective measures of illness. As concerns the unknown diagnosis, in another study on a sample of 139 parents of young children with disorders of sex development researchers found that, in fathers, lack of identifiable etiology underlying the disease increased the risk of developing PTSD symptoms [63]. Finally, Stewart et al. [71], investigating a sample of 395 parents of children with ASD and rare diseases, found that challenging behaviors (i.e., persistent and pervasive maladaptive behavior(s)—including physical aggression, self-injurious behaviors, suicidal behaviors, sexually inappropriate behavior, offending behavior such as arson or stealing, elopement, pica—that has a significant adverse effect on the quality of life and/or health and safety of the individual or others) in the child were related to increased risk of PTSD in the caregivers.
3.1.3. Psychiatric Symptoms and Negative/Maladaptive Coping
Psychiatric symptoms, such as depressive and anxiety symptoms [67,69], manic symptoms among fathers [57] and acute distress symptoms [60] were found to be risk factors for PTSS, as well as having a prior trauma history [60] or having a family mental health diagnosis [59]. Other authors found, in a study on 82 parents of infants previously treated in NICU, that PTSS in one partner was related to PTSS in the spouse [55]. Psychiatric symptoms in young patients also resulted as a risk factor for PTSD in parents, as shown by many authors [42,59,60,68]. Indeed, De Young et al. [60] highlighted as child PTSS were associated to higher PTSS in caregivers, and similar findings were shown by Phipps et al. [42] in a sample of 120 parents of children with cancer and by Taskiran et al. [68] in a sample of 27 mothers of children who underwent a bone marrow transplantation. Moreover, Malpert et al. [48], in a sample of 127 parents of long-term survivors of childhood acute lymphoblastic leukemia, found that perceived caregiver strain was significantly associated with PTSS and another study highlighted as, in fathers, the level of perceived stress was related to PTSS [55]. Ruminations as well, resulted to be associated to PTSD symptoms [53] and, in one study, ruminations were found to be associated to higher PTSS in fathers [58]. Negative attitudes and perceptions [65], as well as feelings of guilt and shame [61] and dysfunctional cognitions [70] have shown a correlation with PTSS. Particularly, Young et al. [65] reported, in a sample of 170 caregivers of pediatric transplant recipients, that parents who had more negative attitudes about their health care services and about health care in general were more likely to report more severe PTSD symptoms. Moreover, Pasterski et al. [62] found in a sample of 47 parents of children diagnosed with a disorder of sex development, that having a cognitive response to the diagnosis characterized by confusion and disbelief was associated to an increased risk of PTSD. Another study on 120 caregivers of children with asthma found that following beliefs congruent with a lay model of asthma management, instead of a professional model of disease management, was associated with an increased risk of developing PTSS [64]. Finally, some authors found that some maladaptive coping styles were related to higher PTSS, particularly emotion-oriented coping in fathers and avoidance-oriented coping style in mothers [55].
In conclusion, female gender, a younger age (both of young patients and caregivers), the presence of other stressor and the severity of the illness are the most recognized risk factors for PTSD or PTSS. Furthermore, various kinds of psychiatric symptoms or maladaptive coping strategies are also reported to be associated to PTSD/PTSS.
3.2. Protective Factors for PTSD/PTSS
For what concerns the protective factors, we found factors as social status, support, and positive coping emerging across studies.
3.2.1. Social Status
Khalifa et al. [46], in a sample of 96 parents of children with acute lymphoblastic leukemia, reported that higher professional and educational levels were associated with lower PTSS.
3.2.2. Support
Some studies highlighted the importance of support in reducing PTSS. Particularly, reducing barriers to treatment for their child with cancer was found to reduce PTSS [54]. Sawyer et al. [51], on a sample of 204 parents of AYAs with cancer, found that self and child unmet needs of practical support from healthcare services was related to higher PTSS levels. McCarthy et al. [52], analyzing the same study sample, highlighted the important role of meeting the information needs of parents in reducing their PTSS levels.
3.2.3. Positive Coping
Harper et al. [45], examining 75 parents of pediatric cancer patients, found that parents’ caregiving self-efficacy reduced immediate and longer-term PTSD symptoms related to one’s child treatment procedures. Moreover, Bruce et al. [44], in a sample of 52 parents of children with brain tumor, found that having more positive parent–child interactions, as shown by a higher score of “Conflict Resolution”, was related to a reduction in PTSS. Another study on 91 parents and primary caregivers of children recruited in the wards or outpatient clinics during the first 8 weeks following their child’s burn injury, found that parents who rated high in self-compassion reported fewer PTSS [61].
In general, protective factors are less investigated in literature than risk ones. Most of the existent evidence concern positive coping style and support provided by medical staff. Moreover, education levels were negatively associated with PTSS in one study.
4. Discussion
The present review summarizes the relevant risk or protective factors for PTSD/PTSS in caregivers of children/AYAs affected by severe, life-threatening, or chronic diseases. We found some risk or protective factors were supported by many studies, while other factors had scant evidence, highlighting the need for further research on this topic. Particularly, although several factors, such as the presence of psychiatric symptoms or support by medical staff could be modified, they are not extensively investigated. In our opinion further studies on these variables are needed to corroborate the previous findings and identify the possible strategies to reduce PTSS.
In regard to sociodemographic factor, our review found women to be at higher risk of developing PTSD symptoms with respect to men [42,46,50,58,63], with rates up to 13.3% of the mothers reporting full-PTSD and 43.3% partial PTSD [58]. This heightened risk of PTSD in women was highlighted in many studies [75,76,77] and has been related to a greater fear conditioning in women than in men [78]. On the other hand, the effect of age on the risk of PTSD/PTSS was investigated with a minor extent. In some studies, younger age of caregivers or patients were a risk factor for PTSD. However, usually studies do not distinguish their results for children, adolescents, or young adults. Moreover, in some cases age range of patients was not clearly reported, hence the effect of age cannot be assessed. Future studies would evaluate if risk factors change in caregivers of young patients with different age, in order to improve specific management strategies. Another major finding was the relevant role of life stressors in increasing parents’ PTSS levels and distress, such as the impact of patient’s illness on plans for the future, the effect of the illness on the broader family [49], and having a lower income while facing the great amount of expenses related to the disease [54,63]. Other authors found that having one biological parent not living in the home, having two or more children diagnosed with ASD, difficulties finding or holding a job or marital problems, were risk factors, reinforcing the role of other life stressors in determining PTSD onset [69]. These results highlight the considerable and complex burden parents may carry out while facing their child’s severe illnesses, and point out the importance of assess all possible stressor and negative life event in such population, in order to detect subjects at risk of PTSD. Considering these data we would suggest a family-centered supportive care for patients and parents, to avoid negative outcomes [79].
Interestingly, we found that illness uncertainty, a cognitive appraisal strongly related to parental distress [80], acted both directly and indirectly, through ruminations, in enhancing PTSS [53,54]. Illness uncertainty mediated the relationship between barriers to care and PTSS, suggesting that greater perceived barriers were related to higher illness uncertainty, which in turn increased parent psychological distress [54]. Moreover, these results suggest that it could be beneficial to the establishment of services aimed at minimizing medical care barriers and consequently at reducing the parental uncertainty [81].
Furthermore, we found that some studies focused on the role of ruminations in developing PTSS [53,58]. Rumination is considered a maladaptive attempt to cope with distress, widely investigated as a potential emotion regulation method, or a possible strategy to cope distressing emotions [82,83]. PTSD symptoms may also been triggered by perseverative thoughts [84,85,86] and, as we found in our review, a significant relationship between PTSS and caregiver rumination emerged [87,88].
Interestingly, feelings of guilt and shame were also found to be associated to higher PTSS in caregivers [60,61]. Feelings of guilt and shame have been recognized by the DSM-5 as having a central role in PTSD psychopathology [15]. Particularly, they were highly reported by patients with PTSD and strongly associated with maladaptive behaviors [89]. Consequently, more recognition should be given to parents’ subjective appraisals of their child’s injury/disease [90]. Moreover, with shame the entire self is seen as at fault, while with guilt the focus is just on specific behaviors [91]. Therefore, shame was found to be a stronger predictor of psychological distress, maybe because it is a more aversive emotional experience compared to guilt [92]. However, as this finding was supported only by two studies, further research should be added on this topic. Guilt and shame feelings were, in fact, related to PTSD development and severity in other populations [25,89] and can also be treated [93], but more specific studies are needed in caregivers.
As concerns protective factors, some studies found the important role of meeting the support needs of caregivers in protecting against PTSD symptoms [51,52,54]. Particularly, access to a social worker for practical support, access to a mental health clinician, and access to an education and vocational advisor for both caregivers and ill young patients have been related to a reduction in the emotional distress of caregivers. These studies also highlighted the important protective role of meeting information needs of caregivers, particularly about the financial impacts of disease for the family. This supports other findings that have reported as families experience significant financial concerns toward the future and have difficulties in accessing income support measures while managing a severe illness in their child [94].
With regard to positive coping styles, some authors [45] found that parents’ caregiving self-efficacy reduced their immediate and longer-term PTSD symptoms related to their children’s treatment procedures. Difficult situations are more likely to be viewed as “challenges to be mastered rather than threats to be avoided” in individuals with high self-efficacy [95]. As previously reported in pediatric cancer context [96,97,98], highly self-efficacious parents may feel relatively comfortable with their ability to cope with the situation, with lower levels of negative affective reactions, included PTSS. Self-compassion, defined as the capacity to assume a warm and understanding attitude toward him/herself in response to negative events or perceived self-inadequacy, was reported as a protective factor in parents [61,98,99]. Better psychological functioning has been related to higher scores in self-compassion [98].
In our review, we found only three studies addressing PTSD in caregivers of children affected by psychiatric disorders, namely one study on parents of children with PTSD [70] and two studies on parents of children with ASD and other rare diseases [69,71]. Although parenting distress has been widely investigated in research studies on caregivers of children affected by ASD [100,101,102,103,104], it seems as the post-traumatic stress burden in caregivers of children and AYAs affected by ASD needs further investigations. Indeed, ASD is a neurodevelopmental disorder that presents an often chronic and disabling clinical picture, characterized by deficits in socio-communicative behaviors, the presence of stereotypical behaviors, and a restricted range of interests [15] but also could be associated to challenging behaviors. The last ones are a range of not socially acceptable conduct that can be physically dangerous to the child or the family, and which have been associated with elevated parenting stress [104,105]. Challenging behaviors that place the child and/or the parent at risk of harm include physical aggression and self-injurious behaviors, suicidal behaviors, elopement, and pica [106,107,108,109]. These behaviors can have a greater physical and emotional impact on parents than core ASD symptoms, bringing a high risk of PTSD [71]. It could be important to identify and treat these subjects with appropriate interventions, as some data report that problem-solving skills training may be beneficial to parents of children with autism spectrum disorder [110].
This review has some limitations that need to be addressed. The first one is the fact that the number of studies was relatively small. In particular, as we described above, only few evince exist on several possible protective or risk factors, and more studies are needed to confirm such results. Furthermore, we found studies on different types of severe diseases, with different prognosis and outcomes, and on different types of young patients (children vs AYAs), that could account for a difference in psychic burden on family caregivers. However, the data reported in literature do not consent a comparison of these categories. Finally, due to the wide heterogeneity of the samples and of the procedures used to assess PTSD and PTSS in the included studies, a meta-analysis process could not be performed.
5. Conclusions
Severe illnesses in children and AYAs may represent a complex psychic burden for patients and their caregivers, leading to PTSD and PTSS. Illness related-distress may represent an important risk factor for the development of PTSD symptoms, particularly in subjects with other life stressors and in the presence of other psychiatric symptoms or negative coping styles while facing a great distressing situation, as a severe disease in own’s child. The presence of even a few PTSS in caregivers may compromise their efficacy as caregivers and negatively affect their child’s as well as their own well-being. Identification of risk/protective factors for the development of PTSD may give the opportunity to target particularly at-risk individuals with focused interventions aimed at enhancing potentials for family caregivers to reduce adverse psychic outcomes and to feed psychological well-being in both caregivers and young patients. For this reason, future studies will focus on several relevant risk and protective factors that have not been sufficiently investigated.
Acknowledgments
Current research (RC) 2000 of Italian Ministry of Health and 5 for thousand of Stella Maris Foundation, Pisa, Italy.
Author Contributions
C.C.: conceptualization, methodology, investigation, writing—original draft, writing—review and editing, supervision; V.D.: conceptualization, methodology, investigation, writing—original draft, writing—review and editing; C.F.: conceptualization, methodology, investigation, writing—original draft; C.A.B.: investigation, writing—original draft, writing—review and editing; E.C.: investigation, writing—original draft; S.C.: investigation, writing—original draft; R.B.: investigation, writing—original draft, writing—review and editing; L.D.: conceptualization, supervision. All authors have read and agreed to the published version of the manuscript.
Funding
The research leading to this work has received funding from the University of Pisa, “Bando PRA—Progetti di Ricerca di Ateneo” (Institutional Research Grants) 2020–2021, Project PRA 2020–2021 “Multimodal non-invasive approach in young females with autism and their parents: a feasibility study”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Celik G., Annagur B.B., Yılmaz M., Demir T., Kara F. Are sleep and life quality of family caregivers affected as much as those of hemodialysis patients? Gen. Hosp. Psychiatry. 2012;34:518–524. doi: 10.1016/j.genhosppsych.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 2.Olawale K.O., Mosaku K.S., Fatoye O., Mapayi B.M., Oginni O.A. Caregiver burden in families of patients with depression attending Obafemi Awolowo University teaching hospitals complex Ile-Ife Nigeria. Gen. Hosp. Psychiatry. 2014;36:743–747. doi: 10.1016/j.genhosppsych.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Jia M., Li J., Chen C., Cao F. Post-traumatic stress disorder symptoms in family caregivers of adult patients with acute leukemia from a dyadic perspective. Psychooncology. 2015;24:1754–1760. doi: 10.1002/pon.3851. [DOI] [PubMed] [Google Scholar]
- 4.Jasemi M., Aazami S., Zabihi R.E. The effects of music therapy on anxiety and depression of cancer patients. Indian J. Palliat. Care. 2016;22:455–458. doi: 10.4103/0973-1075.191823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson A.E., Morton R.P., Broadbent E.A. Illness perceptions and coping predict post-traumatic stress in caregivers of patients with head and neck cancer. Support Care Cancer. 2016;24:4443–4450. doi: 10.1007/s00520-016-3285-0. [DOI] [PubMed] [Google Scholar]
- 6.Jansen L., Dauphin S., van den Akker M., De Burghgraeve T., Schoenmakers B., Buntinx F. Prevalence and predictors of psychosocial problems in informal caregivers of older cancer survivors—A systematic review: Still major gaps in current research. Eur. J. Cancer Care. 2018;27:e12899. doi: 10.1111/ecc.12899. [DOI] [PubMed] [Google Scholar]
- 7.Santos G.D., Ladeira R.B., Almeida J.G., Aprahamian I., Forlenza O.V., Lafer B. Caregiver burden regarding elderly with bipolar disorder: An underrecognized problem. Gen. Hosp. Psychiatry. 2018;51:134–135. doi: 10.1016/j.genhosppsych.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Meyers E.E., Shaffer K.M., Gates M., Lin A., Rosand J., Vranceanu A.M. Baseline Resilience and Posttraumatic Symptoms in Dyads of Neurocritical Patients and Their Informal Caregivers: A Prospective Dyadic Analysis. Psychosomatics. 2020;61:135–144. doi: 10.1016/j.psym.2019.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carmassi C., Foghi C., Dell’Oste V., Bertelloni C.A., Fiorillo A., Dell’Osso L. Risk and Protective Factors for PTSD in Caregivers of Adult Patients with Severe Medical Illnesses: A Systematic Review. Int. J. Environ. Res. Public Health. 2020;17:5888. doi: 10.3390/ijerph17165888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown S.M., Webb A., Mangoubi R., Dy J. A sparse combined regression-classification formulation for learning a physiological alternative to clinical posttraumatic stress disorder scores; Proceedings of the Twenty-Ninth AAAI Conference on Artificial Intelligence; Austin, TX, USA. 25–30 January 2015. [Google Scholar]
- 11.Perkins-Porras L., Joekes K., Bhalla N., Sutherland C., Pollard M. Reporting of posttraumatic stress disorder and cardiac misconceptions following cardiac rehabilitation. J. Cardiopulm. Rehabil. Prev. 2015;35:238–245. doi: 10.1097/HCR.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 12.Carmassi C., Bertelloni C.A., Dell’Oste V., Foghi C., Diadema E., Cordone A., Pedrinelli V., Dell’Osso L. Post-traumatic stress burden in a sample of hospitalized patients with Bipolar Disorder: Which impact on clinical correlates and suicidal risk? J. Affect. Disord. 2019;262:267–272. doi: 10.1016/j.jad.2019.10.044. [DOI] [PubMed] [Google Scholar]
- 13.Johnson H., Thompson A. The development and maintenance of posttraumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clin. Psychol. Rev. 2008;28:36–47. doi: 10.1016/j.cpr.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 14.Pelcovitz D., Goldenberg B., Kaplan S., Weinblatt M., Mandel F., Meyers B., Vinciguerra V. Posttraumatic stress disorder in mothers of pediatric cancer survivors. Psychosomatics. 1996;37:116–126. doi: 10.1016/S0033-3182(96)71577-3. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, DSM-5. American Psychiatric Press; Washington, DC, USA: 2013. [Google Scholar]
- 16.Friedman M.J. Finalizing PTSD in DSM-5: Getting here from there and where to go next. J. Trauma Stress. 2013;26:548–556. doi: 10.1002/jts.21840. [DOI] [PubMed] [Google Scholar]
- 17.Kilpatrick D.G., Resnick H.S., Milanak M.E., Miller M.W., Keyes K.M., Friedman M.J. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV-TR and DSM-5 criteria. J. Trauma Stress. 2013;26:537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedman M.J., Resick P.A., Bryant R.A., Brewin C.R. Considering PTSD for DSM-5. Depress Anxiety. 2011;28:750–769. doi: 10.1002/da.20767. [DOI] [PubMed] [Google Scholar]
- 19.Carmassi C., Bertelloni C.A., Cordone A., Cappelli A., Massimetti E., Dell’Oste V., Dell’Osso L. Exploring mood symptoms overlap in PTSD diagnosis: ICD-11 and DSM-5 criteria compared in a sample of subjects with Bipolar Disorder. J. Affect. Disord. 2020;276:205–211. doi: 10.1016/j.jad.2020.06.056. [DOI] [PubMed] [Google Scholar]
- 20.Dell’Osso L., Carmassi C., Massimetti G., Daneluzzo E., Di Tommaso S., Rossi A. Full and partial PTSD among young adult survivors 10 months after the L’Aquila 2009 earthquake: Gender differences. J. Affect. Disord. 2011;131:79–83. doi: 10.1016/j.jad.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 21.Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin. Psychol. Rev. 2006;26:233–256. doi: 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Cernvall M., Alaie I., von Essen L. The factor structure of traumatic stress in parents of children with cancer: A longitudinal analysis. J. Pediatr. Psychol. 2012;37:448–457. doi: 10.1093/jpepsy/jsr105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horsch A., McManus F., Kennedy P. Cognitive and non-cognitive factors associated with posttraumatic stress symptoms in mothers of children with type 1 diabetes. Behav. Cogn. Psychother. 2012;40:400–411. doi: 10.1017/S1352465812000112. [DOI] [PubMed] [Google Scholar]
- 24.Carmassi C., Corsi M., Gesi C., Bertelloni C.A., Faggioni F., Calderani E., Massimetti G., Saggese G., Bonuccelli A., Orsini A., et al. DSM-5 criteria for PTSD in parents of pediatric patients with epilepsy: What are the changes with respect to DSM-IV-TR? Pt AEpilepsy Behav. 2017;70:97–103. doi: 10.1016/j.yebeh.2017.02.025. [DOI] [PubMed] [Google Scholar]
- 25.Carmassi C., Rossi A., Pedrinelli V., Cremone I.M., Dell’Oste V., Stratta P., Bertelloni C.A., Dell’Osso L. PTSD in the aftermath of a natural disaster: What we learned from the Pisa-L’Aquila Collaboration Project. J. Psychopathol. 2020;26:99–106. doi: 10.36148/2284-0249-377. [DOI] [Google Scholar]
- 26.Carmassi C., Barberi F.M., Cordone A., Maglio A., Dell’Oste V., Dell’Osso L. Trauma, PTSD and post-traumatic stress spectrum: 15 years’ experience on a multidimensional approach to trauma related psychopathology. J. Psychopathol. 2020;26:4–11. doi: 10.36148/2284-0249-376. [DOI] [Google Scholar]
- 27.Kazak A.E., Alderfer M., Rourke M.T., Simms S., Streisand R., Grossman J.R. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J. Pediatr. Psychol. 2004;29:211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- 28.Pelcovitz D., Libov B., Mandel F., Kaplan S., Weinblatt M., Septimus A. Posttraumatic stress disorder and family functioning in adolescent cancer. J. Trauma Stress. 1998;11:205–221. doi: 10.1023/A:1024442802113. [DOI] [PubMed] [Google Scholar]
- 29.Stuber M.L., Christakis D., Houskamp B., Kazak A.E. Posttraumatic symptoms in childhood leukemia survivors and their parents. Psychosomatics. 1996;37:254–261. doi: 10.1016/S0033-3182(96)71564-5. [DOI] [PubMed] [Google Scholar]
- 30.ZafarianMoghaddam E., BehnamVashani H.R., Reihani T., NamaziZadegan S. The Effect of Spiritual education on depression, anxiety, and stress of caregivers of children with leukemia. J. Torbat Heydariyeh Univ. Med Sci. 2016;4:1–7. [Google Scholar]
- 31.Santacroce S. Uncertainty, anxiety and symptoms of posttraumatic stress in parents of children recently diagnosed with cancer. J. Pediatr. Oncol. Nurs. 2002;19:104–111. doi: 10.1177/104345420201900305. [DOI] [PubMed] [Google Scholar]
- 32.Salmani N., Ashketorab T., Hasanvand S. The burden of caregiver and related factors of oncology patients of Shah Vali hospital. Adv. Nurs. Midwifery. 2014;24:11–18. [Google Scholar]
- 33.Rha S.Y., Park Y., Song S.K., Lee C.E., Lee J. Caregiving burden and the quality of life of family caregivers of cancer patients: The relationship and correlates. Eur. J. Oncol. Nurs. 2015;19:376–382. doi: 10.1016/j.ejon.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Carmassi C., Dell’Oste V., Barberi F.M., Pedrinelli V., Cordone A., Cappelli A., Cremone I.M., Rossi R., Bertelloni C.A., Dell’Osso L. Do somatic symptoms relate to PTSD and gender after earthquake exposure? A cross-sectional study on young adult survivors in Italy. CNS Spectr. 2020:1–7. doi: 10.1017/S1092852920000097. [DOI] [PubMed] [Google Scholar]
- 35.Carmassi C., Dell’Oste V., Pedrinelli V., Barberi F.M., Rossi R., Bertelloni C.A., Dell’Osso L. Is Sexual Dysfunction in Young Adult Survivors to the L’Aquila Earthquake Related to Post-traumatic Stress Disorder? A Gender Perspective. J. Sex. Med. 2020;17:1770–1778. doi: 10.1016/j.jsxm.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 36.Carmassi C., Dell’Oste V., Bertelloni C.A., Foghi C., Diadema E., Mucci F., Massimetti G., Rossi A., Dell’Osso L. Disrupted Rhythmicity and Vegetative Functions Relate to PTSD and Gender in Earthquake Survivors. Front. Psychiatry. 2020;11:492006. doi: 10.3389/fpsyt.2020.492006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kazak A.E., Aldefer M., Streisand R., Simms S., Rourke M.T., Barakat L.P., Gallagher P., Cnaan A. Treatment of posttraumatic stress symptoms in adolescent survivors of childhood cancer and their families: A randomized clinical trial. J. Fam. Psychol. 2004;18:493–504. doi: 10.1037/0893-3200.18.3.493. [DOI] [PubMed] [Google Scholar]
- 38.Kim S.Y., Kim J.M., Kim S.W., Kang H.J., Shin I.S., Shim H.J., Cho S.H., Chung I.J., Yoon J.S. Determinants of a hopeful attitude among family caregivers in a palliative care setting. Gen. Hosp. Psychiatry. 2014;36:165–171. doi: 10.1016/j.genhosppsych.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 39.Zale E.L., Heinhuis T.J., Tehan T., Salgueiro D., Rosand J., Vranceanu A.M. Resiliency is independently associated with greater quality of life among informal caregivers to neuroscience intensive care unit patients. Gen. Hosp. Psychiatry. 2018;52:27–33. doi: 10.1016/j.genhosppsych.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 40.Moher D., Liberati A., Tetzla J., Altman D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Landolt M., Vollrath M., Ribi K., Gnehm H., Sennhauser F. Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. J. Child Psychol. Psychiatry. 2003;44:1199–1207. doi: 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- 42.Phipps S., Long A., Hudson M., Rai S.N. Symptoms of post-traumatic stress in children with cancer and their parents: Effects of informant and time from diagnosis. Pediatr. Blood Cancer. 2005;45:952–959. doi: 10.1002/pbc.20373. [DOI] [PubMed] [Google Scholar]
- 43.Jurbergs N., Long A., Ticona L., Phipps S. Symptoms of posttraumatic stress in parents of children with cancer: Are they elevated relative to parents of healthy children? J. Pediatr. Psychol. 2009;34:4–13. doi: 10.1093/jpepsy/jsm119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bruce M., Gumley D., Isham L., Fearon P., Phipps K. Post-traumatic stress symptoms in childhood brain tumour survivors and their parents. Child Care Health Dev. 2011;37:244–251. doi: 10.1111/j.1365-2214.2010.01164.x. [DOI] [PubMed] [Google Scholar]
- 45.Harper F.W., Peterson A.M., Uphold H., Albrecht T.L., Taub J.W., Orom H., Phipps S., Penner L.A. Longitudinal study of parent caregiving self-efficacy and parent stress reactions with pediatric cancer treatment procedures. Psychooncology. 2013;22:1658–1664. doi: 10.1002/pon.3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khalifa A.S., Bishry Z., Tantawy A.A., Ghanem M.H., Effat S.M., El Shahawy H., Ebeid F.S. Psychiatric morbidity in Egyptian children with acute lymphoblastic leukemia and their care providers. Hematol. Oncol. Stem Cell Ther. 2014;7:76–84. doi: 10.1016/j.hemonc.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 47.Juth V., Silver R.C., Sender L. The shared experience of adolescent and young adult cancer patients and their caregivers. Psychooncology. 2015;24:1746–1753. doi: 10.1002/pon.3785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malpert A.V., Kimberg C., Luxton J., Mullins L.L., Pui C.-H., Hudson M.M., Krull K.R., Brinkman T.M. Emotional distress in parents of long-term survivors of childhood acute lymphoblastic leukemia. Psychooncology. 2015;24:1116–1123. doi: 10.1002/pon.3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McCarthy M.C., McNeil R., Drew S., Dunt D., Kosola S., Orme L., Sawyer S.M. Psychological Distress and Posttraumatic Stress Symptoms in Adolescents and Young Adults with Cancer and Their Parents. J. Adolesc. Young Adult Oncol. 2016;5:322–329. doi: 10.1089/jayao.2016.0015. [DOI] [PubMed] [Google Scholar]
- 50.Masa’deh R., Jarrah S. Post Traumatic Stress Disorder in Parents of Children With Cancer in Jordan. Arch. Psychiatr. Nurs. 2017;31:8–12. doi: 10.1016/j.apnu.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 51.Sawyer S.M., McNeil R., McCarthy M., Orme L., Thompson K., Drew S., Dunt D. Unmet need for healthcare services in adolescents and young adults with cancer and their parent carers. Support Care Cancer. 2017;25:2229–2239. doi: 10.1007/s00520-017-3630-y. [DOI] [PubMed] [Google Scholar]
- 52.McCarthy M.C., McNeil R., Drew S., Orme L., Sawyer S.M. Information needs of adolescent and young adult cancer patients and their parent-carers. Support Care Cancer. 2018;26:1655–1664. doi: 10.1007/s00520-017-3984-1. [DOI] [PubMed] [Google Scholar]
- 53.Perez M.N., Sharkey C.M., Tackett A.P., Delozier A.M., Bakula D.M., Gamwell K.L., Mayes S., McNall R., Chaney J.M., Clawson A.H., et al. Post-traumatic stress symptoms in parents of children with cancer: A mediation model. Pediatr. Hematol. Oncol. 2018;35:231–244. doi: 10.1080/08880018.2018.1524954. [DOI] [PubMed] [Google Scholar]
- 54.Perez M.N., Traino K.A., Bakula D.M., Sharkey C.M., Espeleta H.C., Delozier A.M., Mayes S., McNall R., Chaney J.M., Mullins L.L. Barriers to care in pediatric cancer: The role of illness uncertainty in relation to parent psychological distress. Psychooncology. 2020;29:304–310. doi: 10.1002/pon.5248. [DOI] [PubMed] [Google Scholar]
- 55.Aftyka A., Rozalska I. Post-traumatic stress symptoms in a partner as an essential predictor for post-traumatic stress symptoms in the mothers and fathers of children previously treated in NICU. JNN. 2020;26:259–262. doi: 10.1016/j.jnn.2020.04.002. [DOI] [Google Scholar]
- 56.Malin K.J., Johnson T.S., McAndrew S., Westerdahl J., Leuthner J., Lagatta J. Infant illness severity and perinatal post-traumatic stress disorder after discharge from the neonatal intensive care unit. Early Hum. Dev. 2019;140:104930. doi: 10.1016/j.earlhumdev.2019.104930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Carmassi C., Corsi M., Bertelloni C.A., Carpita B., Gesi C., Pedrinelli V., Massimetti G., Peroni D.G., Bonuccelli A., Orsini A., et al. Mothers and fathers of children with epilepsy: Gender differences in post-traumatic stress symptoms and correlations with mood spectrum symptoms. Neuropsychiatr. Dis. Treat. 2018;14:1371–1379. doi: 10.2147/NDT.S158249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dell’Osso L., Corsi M., Gesi C., Bertelloni C.A., Massimetti G., Peroni D., Bonuccelli A., Orsini A., Carmassi C. Adult Autism Subthreshold Spectrum (AdAS Spectrum) in parents of pediatric patients with epilepsy: Correlations with post-traumatic stress symptoms. Compr. Psychiatry. 2018;83:25–30. doi: 10.1016/j.comppsych.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 59.Odar C., Kirschman K.J., Pelley T.J., Butz C., Besner G.E., Fabia R.B. Prevalence and correlates of posttraumatic stress in parents of young children postburn. J. Burn Care Res. 2013;34:299–306. doi: 10.1097/BCR.0b013e31825ae15d. [DOI] [PubMed] [Google Scholar]
- 60.De Young A.C., Hendrikz J., Kenardy J.A., Cobham V.E., Kimble R.M. Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. J. Child Adolesc. Psychopharmacol. 2014;24:9–17. doi: 10.1089/cap.2013.0066. [DOI] [PubMed] [Google Scholar]
- 61.Hawkins L., Centifanti L.C.M., Holman N., Taylor P. Parental Adjustment following Pediatric Burn Injury: The Role of Guilt, Shame, and Self-Compassion. J. Pediatr. Psychol. 2019;44:229–237. doi: 10.1093/jpepsy/jsy079. [DOI] [PubMed] [Google Scholar]
- 62.Pasterski V., Mastroyannopoulou K., Wright D., Zucker K.J., Hughes I.A. Predictors of posttraumatic stress in parents of children diagnosed with a disorder of sex development. Arch. Sex. Behav. 2014;43:369–375. doi: 10.1007/s10508-013-0196-8. [DOI] [PubMed] [Google Scholar]
- 63.Perez M.N., Delozier A.M., Aston C.E., Austin P., Baskin L., Chan Y.-M., Cheng E.Y., Diamond D.A., Fried A., Greenfield S., et al. Predictors of Psychosocial Distress in Parents of Young Children with Disorders of Sex Development. J. Urol. 2019;202:1046–1051. doi: 10.1097/JU.0000000000000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Steinberg D.M., Sidora-Arcoleo K., Serebrisky D., Feldman J.M. The relationship between caregivers’ post-traumatic stress disorder and their asthma health beliefs in an ethnic minority inner-city sample. J. Asthma. 2012;49:724–730. doi: 10.3109/02770903.2012.696169. [DOI] [PubMed] [Google Scholar]
- 65.Young G.S., Mintzer L.L., Seacord D., Castañeda M., Mesrkhani V., Stuber M.L. Symptoms of posttraumatic stress disorder in parents of transplant recipients: Incidence, severity, and related factors. Pt 1Pediatrics. 2003;111:e725–e731. doi: 10.1542/peds.111.6.e725. [DOI] [PubMed] [Google Scholar]
- 66.Ingerski L.M., Shaw K., Gray W.N., Janicke D.M. A pilot study comparing traumatic stress symptoms by child and parent report across pediatric chronic illness groups. J. Dev. Behav. Pediatr. 2010;31:713–719. doi: 10.1097/DBP.0b013e3181f17c52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Virtue S.M., Manne S.L., Mee L., Bartell A., Sands S., Gajda T.M., Darabos K. Psychological distress and psychiatric diagnoses among primary caregivers of children undergoing hematopoietic stem cell transplant: An examination of prevalence, correlates, and racial/ethnic differences. Gen. Hosp. Psychiatry. 2014;36:620–626. doi: 10.1016/j.genhosppsych.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Taskiran G., Surer Adanir A., Ozatalay E. Living with the unknown: Posttraumatic stress disorder in pediatric bone marrow transplantation survivors and their mothers. Pediatr. Hematol. Oncol. J. 2016;33:209–218. doi: 10.3109/08880018.2016.1149749. [DOI] [PubMed] [Google Scholar]
- 69.Casey L.B., Zanksas S., Meindl J.N., Parra G.R., Cogdal P., Powell K. Parental symptoms of posttraumatic stress following a child’s diagnosis of autism spectrum disorder: A pilot study. Res. Autism Spectr. Disord. 2012;6:1186–1193. doi: 10.1016/j.rasd.2012.03.008. [DOI] [Google Scholar]
- 70.Tutus D., Goldbeck L. Posttraumatic symptoms and cognitions in parents of children and adolescents with PTSD. Eur. Child Adolesc. Psychiatr. 2016;25:997–1005. doi: 10.1007/s00787-016-0821-x. [DOI] [PubMed] [Google Scholar]
- 71.Stewart M., Schnabel A., Hallford D.J., McGillivray J.A., Forbes D., Foster M., Shandley K., Gardam M., Austin D.W. Challenging child behaviours positively predict symptoms of posttraumatic stress disorder in parents of children with Autism Spectrum Disorder and Rare Diseases. Res. Autism Spectr. Disord. 2020;69:101467. doi: 10.1016/j.rasd.2019.101467. [DOI] [Google Scholar]
- 72.Weiss D.S. The impact of event Scale-revised. In: Wilson J.P., Keane T.M., editors. Assessing Psychological Trauma and PTSD. 2nd ed. Guilford Press; New York, NY, USA: 2004. pp. 168–189. [Google Scholar]
- 73.Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress. 2015;28:489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 74.Weathers F.W., Litz B.T., Keane T.M., Palmieri P.A., Marx B.P., Schnurr P.P. The PTSD Checklist for DSM-5 (PCL-5) National Center for PTSD; Washington, DC, USA: 2013. [(accessed on 18 December 2020)]. Available online: www.ptsd.va.gov. [Google Scholar]
- 75.Tolin D.F., Foa E.B. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychol. Bull. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- 76.Tekin A., Karadağ H., Süleymanoğlu M., Tekin M., Kayran Y., Alpak G., Şar V. Prevalence and gender differences in symptomatology of posttraumatic stress disorder and depression among Iraqi Yazidis displaced into Turkey. Eur. J. Psychotraumatol. 2016;7:28556. doi: 10.3402/ejpt.v7.28556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Carpita B., Muti D., Muscarella A., Dell’Oste V., Diadema E., Massimetti G., Signorelli M.S., Fusar Poli L., Gesi C., Aguglia E., et al. Sex Differences in the Relationship between PTSD Spectrum Symptoms and Autistic Traits in a Sample of University Students. Clin. Pract. Epidemiol. Ment. Health. 2019;15:110–119. doi: 10.2174/1745017901915010110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Inslicht S.S., Metzler T.J., Garcia N.M., Pineles S.L., Milad M.R., Orr S.P., Marmar C.R., Neylan T.C. Sex differences in fear conditioning in posttraumatic stress disorder. J. Psychiatr. Res. 2013;47:64–71. doi: 10.1016/j.jpsychires.2012.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Grinyer A. Contrasting parental perspectives with those of teenagers and young adutls with cancer: Comparing the findings from two qualitative studies. Eur. J. Oncol. Nurs. 2009;13:200–206. doi: 10.1016/j.ejon.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 80.Tackett A.P., Cushing C.C., Suorsa K.I., Mullins A.J., Gamwell K.L., Mayes S., McNall-Knapp R., Chaney J.M., Mullins L.L. Illness uncertainty, global psychological distress, and posttraumatic stress in pediatric cancer: A preliminary examination using a path analysis approach. J. Pediatr. Psychol. 2015;41:309–318. doi: 10.1093/jpepsy/jsv093. [DOI] [PubMed] [Google Scholar]
- 81.Molzon E.S., Mullins L.L., Cushing C.C., Chaney J.M., McNall R., Mayes S. The relationship between barriers to care, caregiver distress, and child health-related quality of life in caregivers of children with cancer: A structural equation modeling approach. Child Health Care. 2018;47:1–15. doi: 10.1080/02739615.2016.1275639. [DOI] [Google Scholar]
- 82.Diamond L.M., Aspinwall L.G. Emotion regulation across the life span: An integrative perspective emphasizing self-regulation, positive affect, and dyadic processes. Motiv. Emot. 2003;27:125–156. doi: 10.1023/A:1024521920068. [DOI] [Google Scholar]
- 83.Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 84.Michael T., Halligan S.L., Clark D.M., Ehlers A. Rumination in posttraumatic stress disorder. Depress Anxiety. 2007;24:307–317. doi: 10.1002/da.20228. [DOI] [PubMed] [Google Scholar]
- 85.Dell’Osso L., Cremone I.M., Carpita B., Dell’Oste V., Muti D., Massimetti G., Barlati S., Vita A., Fagiolini A., Carmassi C., et al. Rumination, posttraumatic stress disorder, and mood symptoms in borderline personality disorder. Neuropsychiatr. Dis. Treat. 2019;15:1231–1238. doi: 10.2147/NDT.S198616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carmassi C., Bertelloni C.A., Salarpi G., Diadema E., Avella M.T., Dell’Oste V., Dell’Osso L. Is There a Major Role for Undetected Autism Spectrum Disorder with Childhood Trauma in a Patient with a Diagnosis of Bipolar Disorder, Self-Injuring, and Multiple Comorbidities? Case Rep. Psychiatry. 2019:4703795. doi: 10.1155/2019/4703795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Clohessy S., Ehlers A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. Br. J. Clin. Psychol. 1999;38:251–265. doi: 10.1348/014466599162836. [DOI] [PubMed] [Google Scholar]
- 88.Murray J., Ehlers A., Mayou R.A. Dissociation and post-traumatic stress disorder: Two prospective studies of road traffic accident survivors. Br. J. Psychiatry. 2002;180:363–368. doi: 10.1192/bjp.180.4.363. [DOI] [PubMed] [Google Scholar]
- 89.Carmassi C., Bertelloni C.A., Gesi C., Conversano C., Stratta P., Massimetti G., Rossi A., Dell’Osso L. New DSM-5 PTSD guilt and shame symptoms among Italian earthquake survivors: Impact on maladaptive behaviors. Psychiatry Res. 2017;251:142–147. doi: 10.1016/j.psychres.2016.11.026. [DOI] [PubMed] [Google Scholar]
- 90.Tangney J.P. Conceptual and methodological issues in the assessment of shame and guilt. Behav. Res. Ther. 1996;34:741–754. doi: 10.1016/0005-7967(96)00034-4. [DOI] [PubMed] [Google Scholar]
- 91.Øktedalen T., Hagtvet K.A., Hoffart A., Langkaas T.F., Smucker M. The trauma related shame inventory: Measuring trauma-related shame among patients with PTSD. J. Psychopathol. Behav. Assess. 2014;36:600–615. doi: 10.1007/s10862-014-9422-5. [DOI] [Google Scholar]
- 92.Hibbard J.H., Greene J. What the evidence shows about patient activation: Better health outcomes and care experience; fewer data on costs. Health Aff. 2013;32:207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 93.Allard C.B., Norman S.B., Thorp S.R., Browne K.C., Stein M.B. Mid-Treatment Reduction in Trauma-Related Guilt Predicts PTSD and Functioning Following Cognitive Trauma Therapy for Survivors of Intimate Partner Violence. J. Interpers. Violence. 2018;33:3610–3629. doi: 10.1177/0886260516636068. [DOI] [PubMed] [Google Scholar]
- 94.McNeil R., McCarthy M.C., Dunt D., Thompson K., Kosola S., Orme L., Drew S., Sawyer S.M. Financial challenges of cancer for adolescents and young adults and their parent caregivers. Soc. Work. Res. 2019;43:17–30. doi: 10.1093/swr/svy027. [DOI] [Google Scholar]
- 95.Bandura A. Self-Efficacy: The Exercise of Control. Freeman; New York, NY, USA: 1997. [Google Scholar]
- 96.Kwok S., Wong D. Mental health of parents with young children in Hong Kong: The roles of parenting stress and parenting self-efficacy. Child Fam. Soc. Work. 2000;5:57–65. doi: 10.1046/j.1365-2206.2000.00138.x. [DOI] [Google Scholar]
- 97.Best M., Streisand R., Catania L., Kazak A.E. Parental distress during pediatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. J. Pediatr. Psychol. 2001;26:299–307. doi: 10.1093/jpepsy/26.5.299. [DOI] [PubMed] [Google Scholar]
- 98.Neff K.D. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Identity. 2003;2:85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- 99.Neff K.D., Kirkpatrick K.L., Rude S.S. Selfcompassion and adaptive psychological functioning. J. Res. Pers. 2007;41:139–154. doi: 10.1016/j.jrp.2006.03.004. [DOI] [Google Scholar]
- 100.Gray D.E. ‘Everybody just freezes. Everybody is just embarrassed’: Felt and enacted stigma among parents of children with high functioning autism. Sociol. Health Illn. 2002;24:734–749. doi: 10.1111/1467-9566.00316. [DOI] [Google Scholar]
- 101.Micali N., Chakrabarti S., Fombonne E. The Broad Autism Phenotype. Autism. 2004;8:21–37. doi: 10.1177/1362361304040636. [DOI] [PubMed] [Google Scholar]
- 102.Sawyer M., Bittman M., La Greca A., Crettenden A., Harchak T., Martin J. Time Demands of Caring for Children with Autism: What are the Implications for Maternal Mental Health? J. Autism Dev. Disord. 2010;40:620–628. doi: 10.1007/s10803-009-0912-3. [DOI] [PubMed] [Google Scholar]
- 103.Sharpe D.L., Baker D.L. The Financial Side of Autism: Private and Public Costs. In: Mohammadi M.R., editor. A Comprehensive Book on Autism Spectrum Disorders. InTech; Rijeka, Croatia: 2011. pp. 275–296. [Google Scholar]
- 104.Hayes S., Watson S. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism Spectrum disorder. J. Autism Dev. Disord. 2013;43:629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- 105.Nereo N.E., Fee R.J., Hinton V.J. Parental stress in mothers of boys with Duchenne Muscular Dystrophy. J. Pediatr. Psychol. 2003;28:473–484. doi: 10.1093/jpepsy/jsg038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.McClintock K., Hall S., Oliver C. Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study. J. Intellect. Disabil. Res. 2003;47:405–416. doi: 10.1046/j.1365-2788.2003.00517.x. [DOI] [PubMed] [Google Scholar]
- 107.Mayes S.D., Gorman A.A., Hillwig-Garcia J., Syed E. Suicide ideation and attempts in children with Autism. Res. Autism Spectr. Disord. 2013;7:109–119. doi: 10.1016/j.rasd.2012.07.009. [DOI] [Google Scholar]
- 108.Mayes S.D., Zickgraf H. Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Res. Autism Spectr. Disord. 2019;64:76–83. doi: 10.1016/j.rasd.2019.04.002. [DOI] [Google Scholar]
- 109.Schnabel A., Hallford D.J., Stewart M., McGillivray J.A., Forbes D., Austin D.W. An Initial Examination of Post-Traumatic Stress Disorder in Mothers of Children with Autism Spectrum Disorder: Challenging Child Behaviors as Criterion A Traumatic Stressors. Autism Res. 2020 doi: 10.1002/aur.2301. [DOI] [PubMed] [Google Scholar]
- 110.Nguyen C.T., Fairclough D.L., Noll R.B. Problem-solving skills training for mothers of children recently diagnosed with autism spectrum disorder: A pilot feasibility study. Autism. 2016;20:55–64. doi: 10.1177/1362361314567134. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.