The use of mobile applications for patients with chronic illness could improve medication adherence and clinical outcome/patient-related outcome measures. Well-designed randomized controlled studies are needed.
Keywords: Health disparities, Rural health, Weight management, Diabetes Prevention Program
Abstract
Residents of rural communities generally have limited access to preventive health services such as lifestyle programs for weight management. In 2009, the U.S. Congress authorized the Centers for Disease Control and Prevention (CDC) to partner with local community organizations to disseminate the Diabetes Prevention Program (DPP), an evidence-based lifestyle intervention for weight management. Given that the National DPP (NDPP) was designed to broaden nationwide access to weight-loss treatment for adults at high risk for developing diabetes, the present study examined the implementation of the NDPP in rural and urban counties across the USA. The names and locations of NDPP community partnership sites were collected from the CDC website and cross-referenced with the U.S. Census Bureau’s classification of counties as rural versus urban. Results showed that overall 27.9% of the 3,142 counties in the USA contained one or more NDPP partnership sites. However, significantly fewer rural counties had access to a NDPP site compared with urban counties (14.6% vs. 48.4%, respectively, p < .001). This disparity was evident across all types of partnership sites (ps < .001). These findings indicate that implementation of the NDPP has expanded the overall availability of evidence-based weight-management programs across the USA. However, this increase has been disproportionately greater for urban counties versus rural counties, thereby widening the rural/urban disparity in access to preventive health services. Alternative dissemination strategies that address the special barriers to implementation faced by rural communities are needed to increase access to the NDPP.
Implications.
Practice: New approaches, such as partnerships with existing community organizations and expanded use of telehealth interventions, are needed to provide rural communities with greater access to effective weight-management programs such as the National Diabetes Prevention Program.
Policy: Funding for the National Diabetes Prevention Program should earmark support for rural communities and other populations disproportionately affected by obesity-related health conditions.
Research: Ongoing dissemination and implementation research is needed to evaluate the effectiveness and cost efficiency of telehealth interventions for weight management and diabetes prevention in rural communities.
INTRODUCTION
Type 2 diabetes impairs health, diminishes quality of life, reduces life expectancy, and represents a major threat to the health of the U.S. population [1,2]. The Centers for Disease Control and Prevention (CDC) estimates that 30.3 million people in the USA currently have diabetes and an additional 84.1 million others may have prediabetes, a condition characterized by elevated blood glucose that increases risk for type 2 diabetes, heart disease, and stroke [1].
In 2002, the Diabetes Prevention Program (DPP), a landmark randomized trial conducted with adults at high risk for type 2 diabetes, demonstrated that an intensive lifestyle intervention for weight management could significantly delay or prevent progression to type 2 diabetes [3]. Moreover, the beneficial long-term impact of the DPP lifestyle intervention on the prevention or delay of diabetes remained evident at a 15-year follow-up [4]. In 2009, the U.S. Congress approved funding for the CDC to disseminate the DPP lifestyle intervention via partnerships with local community organizations [5, 6]. This initiative, known as the National DPP (NDPP), was designed to broaden nationwide access to weight-loss treatment for adults at high risk for type 2 diabetes [7, 8]. The NDPP’s CDC-approved curriculum mirrors the content of the original DPP lifestyle program and includes 16 hr-long sessions delivered over 6 months, followed by six additional sessions over the subsequent 6 months. The program targets a 5%–7% weight loss over 12 months, and the intervention content focuses on teaching participants how to use behavioral strategies (e.g., goal setting, self-monitoring) to decrease energy intake and increase energy expenditure (for details, see [8, 9]).
The 60 million Americans who reside in rural communities make up 19.3% of the country’s population [10] and constitute one of the largest medically underserved populations in the nation [11]. Residents of rural areas have less access to medical care, including evidence-based lifestyle programs for weight management [11]. Moreover, obesity—arguably the single greatest controllable risk factor for type 2 diabetes—disproportionately affects rural Americans with a substantially higher prevalence observed in rural compared to urban areas [12]. The higher obesity prevalence among adults from rural areas contributes to higher rates of chronic diseases, poorer overall health and quality of life, and higher mortality rates (vs. urban residents) for four of the five leading causes of death, including heart disease, cancer, respiratory disease, and stroke [13]. Thus, a pressing need exists for the dissemination of evidence-based weight-management programs, such as the NDPP, into rural communities.
The primary aim of the present study was to examine implementation of the NDPP across the USA. We were particularly interested in determining whether access to NDPP sites varied across rural and urban counties and whether the number of NDPP sites per county varied across rural and urban counties. An additional exploratory objective of this study entailed an examination of whether NDPP access and the number of NDPP sites per county varied in rural and urban counties according to type of community partnership (e.g., hospitals, health department, YMCAs).
METHODS
Names and locations of NDPP sites were collected from the CDC website [14] as of July 16, 2018. NDPP sites located outside the 50 states and the District of Columbia were excluded. NDPP sites were categorized as (a) hospitals/medical centers, (b) medical clinics, (c) health departments, (d) YMCAs, (e) community wellness/fitness centers, (f) pharmacies, (g) online programs, and (h) “other” types of partnership (e.g., Cooperative Extension Service offices, supermarkets, retirement homes). The city or town for each NDPP site was cross-referenced with the county of its location. Counties were classified as rural versus urban according to the U.S. Census Bureau’s categorization of census tracts as “completely rural,” “mostly rural,” or “mostly urban” [15]. Classification by the Census Bureau is based on a formula that includes population size, population density, land use, and distance from an urban or urbanized area [15]. In the present study, “completely rural” and “mostly rural” were combined into a single category labeled as “rural” to simplify the comparison between rural versus urban counties. We operationally defined “access” to the NDPP as the existence of a site within a county.
Descriptive statistics were used to determine the number of NDPP sites overall, the percentages of urban and rural counties with NDPP sites, and the number of NDPP sites per urban and rural counties. Descriptive statistics were also used to examine NDPP access (i.e., availability of one or more partnership sites within a county) and numbers of sites per urban and rural counties according to type of community partnership. Inferential testing was carried out to determine (a) whether the overall percentage of counties with access to a NDPP site differed between rural and urban areas and (b) whether the numbers of NDPP sites per county differed between rural and urban counties. Chi-square tests were used to examine whether access to at least one NDPP site differed in rural versus urban counties, with Fisher’s exact p used when expected cell counts were less than five. Independent sample t-tests were used to investigate rural/urban differences in the total number of NDPP sites per county, with Satterthwaite corrections made to degrees of freedom when unequal variances were observed.
RESULTS
Of the 3,142 counties in the USA, 1,885 were categorized as mostly or completely rural and 1,257 as mostly urban. A total of 1,775 NDPP sites were identified and then coded by partnership type. Types of partnership sites included 475 hospitals/medical centers, 315 community wellness/fitness centers, 315 medical clinics, 204 YMCAs, 164 health departments, 61 pharmacies, 51 online programs, and 190 other types of sites (e.g., 20 Cooperative Extension Service offices).
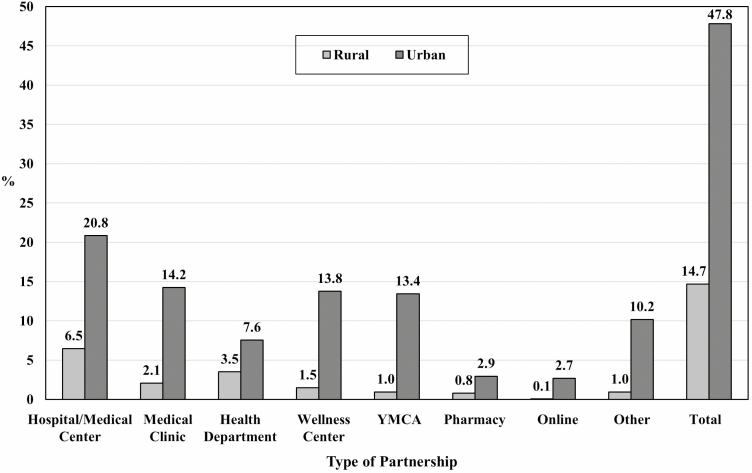
Overall, 878 (27.9%) of the 3,142 counties in the USA had access to one or more NDPP partnership sites. A significantly smaller percentage of rural counties (14.7%, n = 277) had access to at least one NDPP partnership site compared to urban counties (47.8%, n = 601), χ2(1) = 410.8, p < .001. Similarly, the mean number of NDPP sites per county was significantly lower in rural versus urban counties (Ms = 0.17 vs. 1.15, respectively), t(1,320.2) = −14.70, p < .001. Across all types of partnerships, the percentages of rural counties with access to the NDPP were significantly lower than the percentages of urban counties with access (all ps < .001; see Figure 1). Likewise, across all partnership types, there were fewer NDPP sites per county in rural versus urban areas (all ps < .001; see Table 1). Proportionally, the most frequent partnership types represented in urban areas were hospitals/medical centers, followed by wellness centers and then, in third place, medical clinics. Although hospital/medical centers were also the top partnership type in rural areas, the second most frequent partnership type in these areas were health departments, followed by medical clinics and wellness centers (tied for third place). Online programs were the least frequently represented partnership site in rural areas, and online sites were tied with pharmacies for the least represented partnership sites in urban areas.
Figure 1.
Percentage of rural and urban countries with National Diabetes Prevention Program access according to partnership type. The percentage of sites with access was higher in urban versus countries across all partnership types, all ps < .0001.
Table 1.
Mean number of National Diabetes Prevention Program sites in rural and urban counties according to partnership type
| Partnership type | Rural counties (N = 1,889) | Urban counties (N = 1,253) | Cohen’s d | t | df | p |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | |||||
| Hospital or medical center | .07 (.27) | .27 (.63) | 0.45 | −10.81 | 1,576.3 | <.001 |
| Medical clinic | .02 (.16) | .22 (.71) | 0.42 | −9.59 | 1,339.6 | <.001 |
| Health department | .04 (.19) | .08 (.27) | 0.19 | −4.71 | 2,041.0 | <.001 |
| Wellness center | .02 (.15) | .23 (.77) | 0.42 | −9.45 | 1,318.2 | <.001 |
| YMCA | .01 (.11) | .15 (.39) | 0.52 | −12.01 | 1,396.0 | <.001 |
| Pharmacy | .01 (.09) | .04 (.24) | 0.17 | −4.10 | 1,494.6 | <.001 |
| Online program | <.01 (.02) | .04 (.31) | 0.20 | −4.53 | 1,265.5 | <.001 |
| Other | .01 (.10) | .14 (.48) | 0.41 | −9.26 | 1,324.8 | <.001 |
| Total | .17 (.46) | 1.15 (2.33) | 0.65 | −14.70 | 1,320.2 | <.001 |
Means are expressed as the number of National Diabetes Prevention Program partnership sites per county. Satterthwaite approximations were used for degrees of freedom to adjust for unequal variances.
We also examined rural/urban access to NDPP programs with “full” recognition by the CDC’s Diabetes Prevention Recognition Program (i.e., achievement of all requirements with respect to staffing, training, and achievement of participant attendance and weight-loss outcomes) [8]. Nationwide, only 228 sites (12.9%) had achieved full recognition; the remainder had “preliminary” or “pending” status. A significantly smaller percentage of rural counties (2.6%, n = 48) had access to at least one site with full recognition compared to urban counties (11.1%, n = 139), χ2 (1) = 97.61, p < .001.
DISCUSSION
The results of the current study showed that as of July 2018—9 years after Congressional approval—implementation of the NDPP has extended access to evidence-based weight-management programs to 27.9% of all counties in the USA. The findings, however, also indicated that NDPP implementation has led to disproportionately greater access to treatment for residents of urban versus rural counties. More than three times as many urban counties had access to at least one NDPP partnership site than rural counties (47.8% vs. 14.7%, respectively). This pattern of findings was consistent across all types of community partnerships and across programs with “full” recognition versus those with “preliminary” or “pending” status.
Overall, implementation of the NDPP has succeeded in increasing the availability of evidence-based weight management services to adults at high risk for diabetes. From 2012 through 2016, more than 35,000 adults took part in weight-management programs offered through NDPP partnership sites, highlighting the growing reach of this important nationwide, community-based initiative [16]. However, a significant disparity in access remains with respect to implementation in rural versus urban communities. Implementation of the NDPP has resulted in an important unintended consequence—an increase in the disparity between rural and urban counties in access to evidence-based weight management programs.
The consistent pattern of lower access to health care in rural areas versus urban areas remains a major national concern [17]. Unfortunately, multiple barriers exist with respect to the dissemination and implementation of the NDPP in rural communities [18]. The paucity of economic resources in many rural communities affect a broad array of factors that impede the availability of preventive health services, and the low population density of rural communities serves as a disincentive for the private and nonprofit sectors to invest in infrastructure. Thus, new alternatives are needed to achieve the CDC’s commitment “to ensuring health equity by increasing access to Type 2 diabetes prevention lifestyle change programs among . . . those living in geographically hard to reach or rural areas” [8].
Toward this end, the U.S. Cooperative Extension Service (CES), with offices in more than 2,900 counties, represents a potential partner that could play a more prominent role in the dissemination of lifestyle programs in rural areas [19]. The CES commonly offers its health promotion programs to community residents at no cost, enjoys a highly favorable reputation in rural areas, and has demonstrated its ability to deliver behavioral lifestyle programs [20, 21]. To date, implementation of the NDPP via CES offices has been limited, yet it would appear to have the potential to serve as an important NDPP partner in rural America [22].
In rural communities, extended travel distance often constitutes a significant barrier to health care, frequently leading to the neglect of preventive services [11]. In hard-to-reach locales, in-person delivery of lifestyle programs faces substantial implementation barriers associated with distance, transportation, and cost, as well as the availability of trained health counselors [18], suggesting that new treatment delivery formats are needed. Telehealth [23] and web-based programs [24] may overcome barriers to implementation in rural locales and thereby improve the reach of the NDPP. Compared with Internet programs, however, phone-based treatment may have superior long-term engagement and effectiveness [25, 26] as well as greater reach in rural areas where 39% of residents still do not have broadband Internet service [27].
The present study has several limitations. First, combining “completely rural” and “mostly rural” counties into a single category of “rural” may present a more favorable view of access to the NDPP than is the case for those living in completely rural counties. Second, simply cataloging the presence of a NDPP partnership site in a particular county may not fully reflect “access” in that locale due to direct and indirect costs of participation, which represent salient factors for individual with limited economic resources. Third, although very few online NDPP sites exist in rural counties, residents from rural locales may have the opportunity to participate in those emanating from urban areas. Finally, because certification as an official NDPP partnership site entails significant program costs [8], there may be organizations in rural communities that offer lifestyle programs for weight management but have not sought recognition as a NDPP partnership site.
The results of the present study indicate that across the USA, implementation of the NDPP has increased access to an effective lifestyle treatment for weight management and diabetes prevention. However, the findings also show that existing efforts at dissemination have widened the disparity in access between rural and urban counties. Alternative approaches are required to overcome the unique barriers to implementation of the NDPP in rural locales. Successfully addressing this important disparity will provide residents of rural communities with greater access to an evidence-based treatment with the potential to prevent disease and enhance health and well-being.
Funding:
This study was supported by the National Heart, Lung and Blood Institute (grant R18HL112720).
Compliance with Ethical Standards
Conflicts of Interest: All authors declare that they have no conflicts of interest.
Human Rights: This article does not contain any studies with human participants performed by any of the authors.
Informed Consent: This study does not involve human participants and informed consent was therefore not required.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
References
- 1. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention; 2017. Available at https://www.cdc.gov/diabetes/data/statistics/statistics-report.html. Accessibility verified June 6, 2019. [Google Scholar]
- 2. Tancredi M, Rosengren A, Svensson AM, et al. Excess mortality among persons with type 2 diabetes. N Engl J Med. 2015;373(18):1720–1732. [DOI] [PubMed] [Google Scholar]
- 3. Knowler WC, Barrett-Connor E, Fowler SE, et al. ; Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The diabetes prevention program outcomes study. Lancet Diabetes Endocrinol. 2015;3:866–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: The National Diabetes Prevention Program. Am J Prev Med. 2013;44(4 suppl 4):S346–S351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. United States Congress. H.R.4124 – Diabetes Prevention Act of 2009. 2009. Available at https://www.congress.gov/bill/111th-congress/house-bill/4124. Accessibility verified June 6, 2019. [Google Scholar]
- 7. Vojta D, Koehler TB, Longjohn M, Lever JA, Caputo NF. A coordinated national model for diabetes prevention: Linking health systems to an evidence-based community program. Am J Prev Med. 2013;44(4 suppl 4):S301–S306. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention Diabetes Prevention Recognition Program: Standards and Operating Procedures 2018. Available at https://www.cdc.gov/diabetes/prevention/pdf/dprp-standards.pdf. Accessibility verified June 6, 2019.
- 9. Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. United States Census Bureau. American Community Survey: 2015 2016. Available at https://www.census.gov/newsroom/press-releases/2016/cb16-210.html. Accessibility verified June 6, 2019.
- 11. Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural healthy people 2020: New decade, same challenges. J Rural Health. 2015;31(3):326–333. [DOI] [PubMed] [Google Scholar]
- 12. Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: Findings from NHANES (2005–2008). J Rural Health. 2012;28(4):392–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moy E. Leading Causes of Death in Nonmetropolitan and Metropolitan Areas – United States, 1999–2014. MMWR Surveillance Summary [Internet] 2017. Available at http://www.cdc.gov/mmwr/volumes/66/ss/ss6601a1.htm. Accessibility verified June 6, 2019.
- 14. Centers for Disease Control and Prevention. National Diabetes Prevention Program, 2018 2018. Available at https://www.cdc.gov/diabetes/prevention/index.html. Accessibility verified June 6, 2019.
- 15. Ratcliffe M, Burd C, Holder K, Fields A. Defining Rural at the US Census Bureau. American Community Survey and Geography Brief US Census Bureau; 2016:1–8. Available at https://www2.census.gov/geo/pdfs/reference/ua/Defining_Rural.pdf. Accessibility verified June 6, 2019. [Google Scholar]
- 16. Ely EK, Gruss SM, Luman ET, Gregg EW, Ali MK, Nhim K, Albright AL. A national effort to prevent type 2 diabetes: Participant-level evaluation of CDC’s National Diabetes Prevention Program. Diabetes Care. 2017;40(10):1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention. Rural Health Basics Available at https://www.cdc.gov/ruralhealth/about.html. Accessibility verified June 6, 2019.
- 18. Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. [DOI] [PubMed] [Google Scholar]
- 19. Braun B, Bruns K, Cronk L, Fox LK, Koukel S, LeMenestrel S, Warren T. Cooperative Extension’s National Framework for Health and Wellness Available at http://www.aplu.org/members/commissions/food-environment-and-renewable-resources/CFERR_Library/national-framework-for-health-and-wellness/file. Accessibility verified June 6, 2019.
- 20. Perri MG, Limacher MC, Durning PE, et al. Extended-care programs for weight management in rural communities: The treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med. 2008;168(21):2347–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perri MG, Limacher MC, von Castel-Roberts K, et al. Comparative effectiveness of three doses of weight-loss counseling: Two-year findings from the rural LITE trial. Obesity (Silver Spring). 2014;22(11):2293–2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. United States Department of Agriculture. Cooperative Extension System. 2015. Available at https://nifa.usda.gov/cooperative-extension-system. Accessibility verified June 6, 2019. [Google Scholar]
- 23. Vadheim LM, Patch K, Brokaw SM, et al. Telehealth delivery of the diabetes prevention program to rural communities. Transl Behav Med. 2017;7(2):286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sepah SC, Jiang L, Ellis RJ, McDermott K, Peters AL. Engagement and outcomes in a digital Diabetes Prevention Program: 3-Year update. BMJ Open Diabetes Res Care. 2017;5(1):e000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Svetkey LP, Stevens VJ, Brantley PJ, et al. ; Weight Loss Maintenance Collaborative Research Group Comparison of strategies for sustaining weight loss: The weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139–1148. [DOI] [PubMed] [Google Scholar]
- 26. Aneni EC, Roberson LL, Maziak W, et al. A systematic review of internet-based worksite wellness approaches for cardiovascular disease risk management: Outcomes, challenges & opportunities. PLoS One. 2014;9(1):e83594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Federal Communications Commission. 2018 Broadband Deployment Report. 2018. Available at https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2018-broadband-deployment-report. Accessibility verified June 6, 2019. [Google Scholar]