Abstract
Background
The coronavirus disease-2019 (COVID-19) pandemic has generated enormous pressure on healthcare establishments, prompting the restructuring of services to rationalise resources. Complex head and neck reconstructive surgery in this setting may carry substantial risk to patients and staff. This paper outlines the management strategy and outcomes of major head and neck oncological cases at a single regional tertiary referral centre.
Methods
A database review was undertaken of consecutive patients undergoing major head and neck surgery and reconstruction during the COVID-19 pandemic at St Andrew's Centre for Plastic Surgery & Burns, Chelmsford UK. Patient demographics, tumour and reconstruction characteristics as well as peri‑operative information were determined. Patients were prospectively contacted with regard to COVID-related symptoms and investigations.
Results
Twenty-two patients (15 males and 7 females) with a mean age of 67 years (range: 36–92 years) were included between March 1 and June 13, 2020. Patients underwent pre-operative throat swabs at 72 h and 24 h as well as chest CT scanning as part of a robust protocol. Twelve free flaps, four loco-regional flaps, four parotidectomies and 23 cervical lymphadenectomies were performed. Two patients required a return to theatre. No post-operative deaths occurred and flap survival rate was 100%. A single patient tested positive for COVID-19 pre-operatively and no post-operative COVID-19 infections occurred.
Conclusion
Although head and neck surgery represents a high-risk procedure to patients and healthcare professionals, our institutional experience suggests that in the presence of a robust peri‑operative protocol and judicious patient selection, major head and neck surgery, including free tissue transfer reconstruction, may be performed safely.
Keywords: Head and neck, Free flap, Microsurgery, COVID-19, Coronavirus, Outcomes
Introduction
In December 2019, a cluster of cases of pneumonia was reported by the Wuhan Municipal Health Commission in China, caused by the Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2).1 The subsequent rapid spread of the virus globally prompted the World Health Organisation to declare a coronavirus disease-2019 (COVID-19) pandemic on March 11, 2020.2 Common manifestations of the disease included fever, dry cough, myalgia, and radiological evidence of pneumonia with complications, including acute respiratory distress syndrome, shock, renal failure and death.3 The underlying pathophysiology and spectrum of clinical features have largely been attributed to microvascular thrombi.4 The COVID-19 pandemic has brought unprecedented disruption to the National Health Service (NHS), with 41,662 reported COVID-19-associated deaths in the United Kingdom by June 14, 2020.5 Extensive restructure of health service has been essential to rationalise resources, reduce viral transmission, create capacity and protect patients and staff.6
Major ablative and reconstructive surgery which involves the head and neck, has posed a unique challenge due to the two-team approach often involved, close proximity to aerosol-generating organs, heavy use of personal protective equipment (PPE) and post-operative need for precious intensive care facilities for a potentially highly co-morbid patient group undergoing high-risk procedures. In addition, concerns were raised about the performance of microvascular surgery in COVID-19-positive patients with pro-thrombotic tendencies. This paper summarises the local strategy adopted at our institution and the outcomes of major head and neck procedures performed during the COVID-19 pandemic so far.
Methods
Patients who underwent major head and neck oncological surgery and reconstruction between March 1 and June 13, 2020 at St Andrew's Centre for Plastic Surgery and Burns, Chelmsford, UK were prospectively contacted regarding COVID-related symptoms and investigations, having reached a period of 28 days post-operatively. This investigation period represented the peak of the UK COVID-19 pandemic.5 Major surgery was defined as surgery for malignancies of the upper aero-digestive tract requiring flap reconstruction, parotidectomies and cervical lymphadenectomies. A database review was also undertaken to establish details, including demographics, tumour and reconstruction characteristics and peri‑operative management. Gathered data included age, ethnicity, gender, co-morbidities, body mass index (BMI), smoking status, American Society of Anaesthesiologists (ASA) grade, tumour site, flap reconstruction characteristics, requirement for lymphadenectomy and tracheostomy, intensive care unit requirements, procedure duration, length of inpatient stay, return to theatre, flap loss and complications.
St. Andrew's peri‑operative protocol for surgery of the head and neck
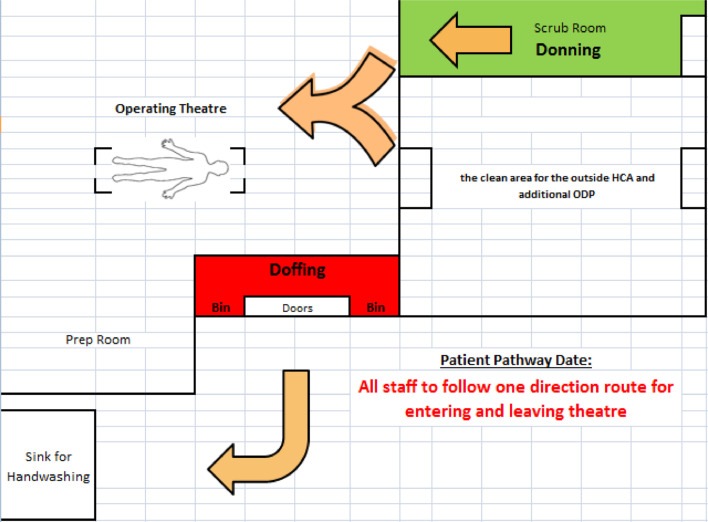
A clear hospital peri‑operative protocol was introduced at the end of March 2020. Pre-operatively, patients are advised to self-isolate for a period of two weeks and screened for signs and symptoms of COVID-19 as stated by Public Health England (PHE).7 Following successful anaesthetic pre-assessment review, all patients listed for major head and neck surgery underwent throat swabbing at 72 h and 24 h pre-operatively (2019-nCoV RNA Real Time PCR test) with additional chest computed tomography (CT) at 24 h pre-operatively. In case of clinical, radiological or molecular evidence of COVID-19 infection, the patient would be advised to self-isolate for four weeks before undergoing repeat testing or admitted for inpatient care if clinically indicated. A clear operating theatre team briefing was conducted by the lead surgeon on the morning of surgery, theatre personnel were kept to a minimum and a robust one-way traffic pathway was observed in the operating theatre to minimise the cross-contamination risk (Figure 1 ). Every staff member in the operating room had a specific designated role at the team briefing for every step of the procedure. Use of PPE, including filtering face piece grade 3 mask, facial shield, gown and gloves was compulsory with clear donning/doffing instructions. There were strict rules during any planned aerosol-generating procedures (AGP), with only minimal and essential staff members present while performing AGPs such as intubation or tracheostomy. We aimed to minimise staff exposure and PPE wastage by adhering to our protocols. Staff positioned themselves outside the operating theatre exit door, supervised shoe cleaning, hand washing and safe masque disposal. Patients were induced and extubated on the table in the operating room with minimal contamination. Following intubation, the throat was packed with a betadine-soaked throat pack. Once intraoral resection had been completed, a clear tegaderm dressing was applied to seal the oral and nasal cavities to further minimise any contamination due to endotracheal tube cuff leaks. All procedures were undertaken in a ‘Green’ operating theatre, with the availability of a ‘Green’ post-operative recovery and high-dependency unit. The ‘Green’ status referred to asymptomatic patients who had tested negative on their pre-operative screening. Patients with a tracheostomy were nursed in a side room on a ‘Green’ ward with staff wearing appropriate PPE.
Figure 1.
One-way traffic operation theatre.
Results
Patient demographics and operation dates are presented (Table 1 ). There were 22 patients (15 males and 7 females) who underwent surgery; the mean age was 67 years (range 36–92 years). Twenty patients were ethnically identified as Caucasian and two were within the Black, Asian and Minority Ethnic (BAME) ethnic groups. Of the 22 patients, 8 were smokers and 14 were non-smokers; the mean ASA risk score was 2.18 and the mean BMI was 26.2.
Table 1.
Patient Demographics and Operation Dates.
| Date of operation | Age | Sex | Ethnicity | Co-morbidities | ASA | BMI | Smoker |
|---|---|---|---|---|---|---|---|
| 04/03/2020 | 62 | M | Caucasian | Previous SCC tongue | 2 | 25 | No |
| 04/03/2020 | 78 | M | Caucasian | Hypertension Benign prostatic hyperplasia Recurrent SCC parotid |
3 | 34 | Yes |
| 09/03/2020 | 76 | M | Caucasian | Previous SCC tongue | 2 | 24 | No |
| 16/03/2020 | 92 | M | Caucasian | Benign prostatic hyperplasia Hypothyroidism |
3 | 26 | No |
| 18/03/2020 | 49 | F | Caucasian | Nil | 2 | 18 | Yes |
| 18/03/2020 | 69 | M | Caucasian | Nil | 1 | 29 | Yes |
| 19/03/2020 | 81 | F | Caucasian | Nil | 2 | 25 | No |
| 20/03/2020 | 78 | M | Caucasian | Nil | 2 | 32 | No |
| 23/03/2020 | 76 | F | Caucasian | Hypertension Bipolar affective disorder Arthritis |
3 | 25 | No |
| 24/03/2020 | 76 | M | Caucasian | Hypertension | 2 | 31 | Yes |
| 25/03/2020 | 64 | F | Caucasian | Nil | 2 | 20 | Yes |
| 27/03/2020 | 72 | M | Caucasian | Bowel cancer Liver metastases |
3 | 24 | No |
| 28/03/2020 | 70 | M | Caucasian | Intermittent claudication | 3 | 25 | Yes |
| 22/04/2020 | 60 | F | Caucasian | Nil | 2 | 26 | No |
| 29/04/2020 | 60 | M | Caucasian | Hypertension Hypothyroid Pyriform fossa carcinoma |
3 | 27 | No |
| 13/05/2020 | 76 | M | Caucasian | Atrial fibrillation B12 deficiency Hypertension |
2 | 25 | No |
| 27/05/2020 | 67 | M | Caucasian | Hypertension | 2 | 30 | No |
| 01/06/2020 | 36 | F | Caucasian | Nil | 1 | 28 | No |
| 01/06/2020 | 48 | M | Caucasian | Nil | 1 | 25 | Yes |
| 03/06/2020 | 67 | M | Asian | Hypertension | 2 | 24 | Yes |
| 10/06/2020 | 56 | M | African | Hypertension | 2 | 29 | No |
| 10/06/2020 | 64 | F | Caucasian | Hypertension Atrial fibrillation |
2 | 25 | No |
ASA=American Society of Anaesthesiologists and SCC=squamous cell carcinoma.
Operative details and indications for surgery are presented (Table 2 ). Of the primary tumour resections performed, there were 23 cervical lymphadenectomies (19 unilateral and 2 bilateral on a total of 21 patients), four parotidectomies, 11 free flap reconstructions, four loco-regional flaps and nine patients required a tracheostomy. The surgical team comprised of a consultant plastic surgeon, consultant maxillofacial or ENT surgeon, a senior microsurgical fellow and a Plastic Surgery Specialist Registrar. Post-operative details are presented (Table 3 ). The mean operative duration was 6.5 h and inpatient stay was 12 days. Of the 22 patients who received operations, only two required post-operative ICU admission. Of the patients who required tracheostomy, the mean time to decannulation was seven days. Two patients required a return to theatre. The first patient developed a pharyngeal fistula following a pectoralis major flap reconstruction for a laryngo-pharyngectomy and required additional reconstruction with a contralateral pectoralis major flap. The second patient developed tip necrosis of a pedicled pectoralis major flap following mastoidectomy; this patient required a further return to theatre to undergo debridement of the necrotic tip, advancement of the remaining pectoralis major flap and a temporalis flap turnover with split thickness skin grafting.
Table 2.
Operation Details and Indications for Surgery.
| Tumour site | TNM staging | Free flap type | Regional flap type | Neck dissection | Tracheostomy required | Operation duration (hours) |
|---|---|---|---|---|---|---|
| FOM | T2N0M0 | ALT | – | 1–4 | Yes | 9 |
| Mastoid & Parotid | T2N1M0 | – | Pectoralis major | 2–5 | No | 9 |
| Tongue | T2N0M0 | RF | – | 1–4 | No | 8 |
| Parotid | T2N1M0 | – | – | 2–5 | No | 3 |
| Tongue | T2N0M0 | RF | – | 2–4 | No | 7 |
| Hypopharynx | T3N0M0 | – | Pectoralis major | 2–4 (bilateral) | Yes | 9 |
| Tongue | T2N0Mx | – | – | 1–4 | No | 9 |
| Parotid | T2M0M0 | – | Cervicofacial | N/A | No | 4 |
| Tongue, FOM | T4N2Mx | RF | – | 1–4 | Yes | 9 |
| Hypopharynx | T4N2cM0 | – | Pectoralis major | 2–4 | Yes | 7 |
| Tongue, FOM | T2N0M0 | RF | – | 1–4 | Yes | 9 |
| SCC scalp | T2N0M0 | – | – | 2–5 | No | 3 |
| FOM | T4N0M0 | RF | – | 1–4 (bilateral) | Yes | 7 |
| FOM | T3N0M0 | RF | – | 1–4 | Yes | 8 |
| Hypopharynx | T3N0M0 | RF | – | 2–4 | Yes | 9 |
| Maxilla & Orbit | T4N0M0 | ALT | – | 1–4 | No | 8 |
| FOM | T3N0M0 | RF | – | 1–4 | No | 7 |
| Tongue | T2N0M0 | – | – | 1–4 | No | 4 |
| Tongue | T1N0M0 | – | – | 1–4 | No | 4 |
| Salivary duct | T2N1M0 | – | – | 5 | No | 3 |
| Tongue | T2N1M0 | RF | – | 1–4 | Yes | 8 |
| Parotid | T2N1M0 | – | – | 2–4 | No | 3 |
SCC=squamous cell carcinoma, FOM=floor of mouth, ALT=anterolateral thigh and RF=radial forearm.
Table 3.
Post-operative Details.
| Post-operative Tracheostomy De-cannulation (days) | ICU Required | Return to Theatre | Flap Loss | Complications | Inpatient Stay (days) |
|---|---|---|---|---|---|
| 6 | Yes | No | No | – | 21 |
| – | No | Yes | No | Flap tip necrosis and Facial nerve palsy | 17 |
| – | Yes | No | No | – | 15 |
| – | No | No | No | – | 9 |
| – | No | No | No | – | 10 |
| Permanent | No | No | No | – | 18 |
| – | No | No | No | – | 6 |
| – | No | No | No | – | 3 |
| 7 | No | No | No | – | 11 |
| Permanent | No | Yes | No | Pharyngeal fistula | 39 |
| 6 | No | No | No | – | 10 |
| – | No | No | No | – | 4 |
| 6 | No | No | No | – | 16 |
| 10 | No | No | No | – | 17 |
| Permanent | No | No | No | – | 20 |
| – | No | No | No | – | 8 |
| – | No | No | No | – | 9 |
| – | No | No | No | – | 3 |
| – | No | No | No | – | 4 |
| – | No | No | No | – | 5 |
| 7 | No | No | No | – | 12 |
| – | No | No | No | – | 6 |
ICU=intensive care unit.
COVID-related data are presented (Table 4 ). Because of our evolving understanding of patient management over the course of the UK pandemic, a change in the testing policy over the study period occurred. Therefore, only the penultimate 10 of 22 patients included in this series self-isolated prior to operation. In addition, nine patients had preoperative 72 h and 24 h swabs and pre-operative CT chest; this came into effect during the end of March. Six patients had a pre-operative CT chest; of note, it was decided by the head and neck multidisciplinary team that only patients who required free flap reconstruction would undergo this investigation. In addition, nine patients had a 24 h pre-operative COVID-19 swab and seven patients had one at 72 h pre-operatively. Two patients did not undergo a 72 h pre-operative COVID-19 swab and instead underwent one at 24 h pre-operatively only, as testing at this interval was deemed satisfactory because their surgery involved only a tongue wedge resection with no reconstruction. Post-operatively, only one patient required readmission for shortness of breath but tested COVID-19 negative. Of note, there were no positive COVID-19 test results post-operatively.
Table 4.
COVID-related details.
| Preoperative |
Post-Operative |
||||||
|---|---|---|---|---|---|---|---|
| Isolated | Swab at 72h | Swab at 24h | CT chest at 24h | Signs/Symptoms | Swab performed | Signs/Symptoms | Readmission |
| No | No | No | No | No | No | ||
| No | No | No | No | Yes | No | ||
| No | No | No | No | No | No | ||
| No | No | No | No | No | No | ||
| No | No | No | No | Yes | Yes | ||
| No | No | No | No | No | No | ||
| No | No | No | No | No | Loose stool | No | |
| No | No | No | No | No | No | ||
| No | No | No | No | No | No | ||
| No | No | No | No | Yes | No | ||
| No | No | No | No | No | No | ||
| No | No | No | No | No | No | ||
| Yes | No | No | No | No | No | ||
| Yes | Yes | Yes | Yes | No | No | ||
| Yes | Yes | Yes | Yes | Pyrexia, SOB | Yes | No | |
| Yes | Yes | Yes | Yes | Yes | No | ||
| Yes | Yes | Yes | Yes | Yes | No | ||
| Yes | No | Yes | No | Yes | No | ||
| Yes | No | Yes | No | No | No | ||
| Yes | Yes | Yes | No | Yes | No | ||
| Yes | Yes | Yes | Yes | No | No | ||
| Yes | Yes | Yes | Yes | No | No | ||
SOB=shortness of breath and CT=computed tomography.
Discussion
The COVID-19 pandemic has presented the health service with unprecedented challenges. Judicious reallocation of valuable resources has been undertaken to prioritise cases based on clinical significance. The majority of low acuity elective procedures have been postponed, with precedence given to operations where a delay could potentially have a negative impact on the clinical outcome.8 This has created a unique clinical and ethical dilemma for patients and healthcare professionals. Head and neck ablative and reconstructive surgery represents a field with a high-risk of disease transmission, involving multiple surgical teams performing lengthy and complex procedures on patients with multiple co-morbidities. Furthermore, this subset of patients often requires AGP such as tracheostomy and immediate microvascular reconstructive procedures to prevent life-threatening complications, thereby prolonging surgical and anaesthetic time. The bulky and uncomfortable PPE equipment worn over several hours may also limit the ability to undertake these highly technical procedures, which demand a high level of dexterity.
A careful risk-benefit assessment was undertaken for each patient as part of our Centre's multidisciplinary team meeting. Delays in the treatment initiation of aggressive head and neck SCC may result in progression and increased mortality, while patients who contract COVID-19 post-operatively are known to have a very poor outcome due to the immunosuppressive nature of surgery.9 An international study by the COVIDSurg collaborative noted a mortality rate of 20.4% in elective patients with a post-operative diagnosis of COVID-19.10 To facilitate and streamline this complex decision-making process, the Intercollegiate Body, NHS England and NHS Improvement have developed a surgical prioritisation guideline to stratify the urgency of surgical procedures into subgroups11 (Table 5 ).
Table 5.
Summary of National Surgical Prioritisation Guidelines.
| Priority Level | Procedure Timeline | Examples |
|---|---|---|
| 1a Emergency | Within 24 h | Orbital compartment syndrome, necrotising fasciitis and free flap revascularisation |
| 1b Urgent | Within 72 h | Facial fractures (unsuitable for conservative treatment) and primary tendon repair |
| 2 | Up to 4 weeks | Oropharyngeal/tonsil/tongue cancer resection +/- reconstruction |
| 3 | Up to 3 months | Low-grade salivary gland tumours and moderately/well differentiated skin cancer resection |
| 4 | More than 3 months | All orthognathic surgery and breast reconstruction |
The General medical council put forward several considerations before resuming elective services. We adopted these principles in our unit to successfully and safely continue our head and neck service. The key considerations are12:
-
•
Timing: There should be a sustained reduction in the rate of new COVID-19 cases for a period of time past the peak, to ensure necessary staff and associated facilities (e.g. ICU) are available.
-
•
Testing: Hospitals should know their diagnostic testing availability and develop clear policies for addressing testing requirements and frequency for staff and patients.
-
•
PPE: Hospitals should be satisfied that they have adequate PPE and surgical supplies appropriate to the number and type of procedures performed, and clear policies on how and when to use them.
-
•
Availability of core interdependent services: Care needs to be taken so that essential peri‑operative services (e.g. diagnostic imaging, anaesthesia, critical care and sterile processing) are also ready to commence operations before resuming elective surgery. Where these are not ready, it might be useful to consider engaging with external partners for temporary support.
-
•
Local coordination: To ensure the above requirements are in place, and the patients’ care pathway is appropriately managed so that the resumption of services is safe and efficient.
A total of 22 patients underwent major oncological surgery of the head and neck at our institution during the COVID-19 pandemic, with a 0% mortality rate. All operations were led by consultant surgeons, who allowed the surgical trainees and Fellows to undertake parts of the operations where appropriate, in an effort to preserve essential teaching and training. Only two patients experienced post-operative complications that required surgical intervention. These occurred in two out of three patients who underwent pedicled regional flap reconstruction. These complications, however, occurred in patients without COVID-19 symptoms, and therefore were deemed unrelated to the infection. Eleven patients underwent immediate reconstruction with free microvascular tissue transfer with a 100% flap survival rate. A total of 23 cervical lymphadenectomies were performed with no associated complications. Nine patients required a tracheostomy, six of which were temporary, with no associated complications or delays in tracheostomy decannulation. Only a single patient was diagnosed with a positive COVID-19 throat swab test pre-operatively and was successfully operated on after a period of four weeks of self-isolation, as per our protocol.
The crucial role of adopting a robust peri‑operative protocol and optimising patient selection in minimising major complications and patient mortality has been supported by Shrikhande13 and colleagues, who reported no post-operative deaths in their series of 484 patients undergoing major oncological surgery during the COVID-19 pandemic. The high rate of false-negative results associated with RT-PCR testing for COVID-19 have been well reported.14 To improve diagnostic accuracy, our protocol included two separate throat swabs at 72 h and 24 h preoperatively. Moreover, performing throat swabs at 72 h could potentially facilitate the detection of COVID-19-positive patients early enough to aid the restructuring of our surgical theatre list or redeployment of vital healthcare staff to areas of need. Furthermore, to further improve pre-operative screening, radiological testing with a CT scan of the chest at 24 h pre-operatively was also included in our protocol. Finally, patients (along with members of their household) were asked to self-isolate for 2 weeks prior to surgery; upon admission to the ward, they were also temperature-checked.
Our pre-operative screening protocol resulted in a change in the operative course for two patients.
The first patient was a 53-year-old male with a background of alcohol abuse and intravenous drug use who developed leucocytosis (21 × 109 per L) and reduced oxygen saturations (89%) the day before the planned surgery. As the surgery involved an extensive intraoral excision, which requires a mandibular split and bilateral cervical lymphadenectomies with free flap reconstruction, it was deemed too risky to proceed with surgery, and the procedure was postponed for four weeks, despite negative COVID-19 swab testing.
The second patient was a 76-year-old female due to undergo superficial parotidectomy and cervical lymphadenectomy for metastatic cutaneous SCC of the cheek. As she failed to adhere to the pre-operative self-isolation protocol, she was postponed on the morning of the procedure, despite negative pre-operative COVID-19 swab testing.
Both patients later underwent their original planned procedures with an uneventful recovery. These two cancellations resulted in the gap in activity during April (Table 1).
Of note, one patient was diagnosed with COVID-19 infection pre-operatively by doing a positive throat swab test shortly before the study period. This 60-year-old male patient, with a background of hypertension and hypothyroidism, developed a fever (39 °C), dry cough and tested positive for COVID-19 following a throat swab. His procedure was postponed and four weeks later, following negative swab testing, he underwent a successful uncomplicated total laryngo-pharyngectomy and reconstruction with a tubed free flap.
The COVID-19 pandemic also poses a significant risk to healthcare professionals involved in the peri‑operative care of head and neck oncology patients. Indeed, a high rate of transmission to otolaryngologists has been reported in China, Italy and Iran, with reports of morbidity and death.15 No member of staff involved in the care of patients in our cohort developed symptoms suggestive of COVID-19 infection.
The consideration of less complex reconstructive options, such as regional flaps instead of free tissue transfer in head and neck patients during the COVID-19 pandemic was highlighted by Desai.16 In our experience, a radial forearm flap was our primary choice of free flap where possible as it provides a simple, quick and reliable option with consistent anatomy and a long and large pedicle, thereby making it a safe choice in our patient cohort. A single patient who underwent a partial laryngo-pharyngectomy was reconstructed with a pedicled pectoralis major flap, instead of free tissue transfer.
It should be noted that our cases were performed at an institution also responsible for the acute care of inpatients with COVID-19 infection, where the diversion of essential staff and resources to treat such patients during the peak of the pandemic resulted in severe restriction in the operation theatre capacity at times. A higher number of cases may have been performed at other institutions, designated as ‘Super Green’, where no cases of COVID-19 infection were treated, thereby allowing uninterrupted surgical operating lists.
Conclusion
The COVID-19 global pandemic continues to present an enormous challenge to the NHS, which has witnessed major restructural changes to adapt and continue to provide safe care to patients. Major surgery involving the head and neck represents a high-risk field both to patients and involved healthcare professionals, with information regarding transmission and outcomes evolving on a daily basis. We recommend the combination of preoperative throat swabs at 72 h and 24 h as well as chest CT scanning to enhance the quality of screening for COVID-19, improve planning of services and potentially maximise the efficiency of vital resources. Our institutional experience also suggests that in the presence of a robust peri‑operative protocol and careful patient selection, major surgery to the head and neck, including reconstruction with free tissue transfer may be performed safely. Thus, in the absence of obvious clinical indicators, clinicians may safely undertake their usual reconstructive flap option without the need to downgrade to a less complex alternative. We would welcome larger, international, collaborative studies to further support our experience.
Declaration of Competing Interest
None declared.
Acknowledgments
Funding
None.
Ethical approval
Not required.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in china. N Engl J Med. 2019;382(8):2020727–2020733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lei S., Jiang F., Su W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection [published online ahead of print, 2020 Apr 5] EClinicalMedicine. 2020;21 doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magro C., Mulvey J.J., Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UK government website – coronavirus (COVID-19) cases in the UK . 2020. https://coronavirus.data.gov.uk/?_ga=2.253308233.1325178548.1594057616-1125096213.1594057616. [Google Scholar]
- 6.Armstrong A., Jeevaratnam J., Murphy G. A plastic surgery service response to COVID-19 in one of the largest teaching hospitals in Europe. J Plast Reconstr Aesthet Surg. 2020;73(6):1174–1205. doi: 10.1016/j.bjps.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Public Health England Official Website https://publichealthmatters.blog.gov.uk/2020/01/23/wuhan-novel-coronavirus-what-you-need-to-know/.
- 8.Moletta L., Pierobon E.S., Capovilla G. International guidelines and recommendations for surgery during COVID-19 pandemic: a Systematic Review. Int J Surg. 2020;79:180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen A.R.1., Nellemann H.M., Overgaard J. Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol. 2007;84(1):5–10. doi: 10.1016/j.radonc.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 10.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study [published correction appears in Lancet. 2020 Jun 9] Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Royal college of surgeons website - clinical guide to surgical prioritisation during the coronavirus pandemic . 2020. https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance Last accessed 23/07/ [Google Scholar]
- 12.Royal college of surgeons website - recovery of surgical services during and after COVID-19 https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/#s1.
- 13.Shrikhande S.V., Pai P.S., Bhandare M.S. Outcomes of elective major cancer surgery during COVID 19 at Tata memorial centre: implications for cancer care policy [published online ahead of print, 2020 Jun 8] Ann Surg. 2020;10:1097. doi: 10.1097/SLA.0000000000004116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.He J.L., Luo L., Luo Z.D. Diagnostic performance between CT and initial real-time RT-PCR for clinically suspected 2019 coronavirus disease (COVID-19) patients outside Wuhan, China. Respir Med. 2020;168 doi: 10.1016/j.rmed.2020.105980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AAO-HNS . American Academy of Otolaryngology-Head and Neck Surgery; 2020. Position Statement: otolaryngologists-head and neck surgeons and the COVID-19 pandemic. http://www.entnet.org/content/aao-hns-position-statement-otolaryngologists-head+and+neck+surgeons-and-covid-19-pandemic. Published March 23. [Google Scholar]
- 16.Desai S.C., Seth R. Shifting paradigms in head and neck reconstructive surgery during the COVID-19 Crisis. Facial Plast Surg Aesthet Med. 2020;22(3):152–154. doi: 10.1089/fpsam.2020.0186. [DOI] [PubMed] [Google Scholar]