Abstract
Purpose:
The purpose of this study was to descriptively quantify experiences of injured workers with permanent impairment during their first year of work reintegration.
Methods:
A representative survey was conducted to characterize health, disability, pain, employment, reinjury, and economic outcomes for 598 workers with permanent impairment who had returned to work during the year after workers’ compensation claim closure. Survey responses were summarized by degree of whole body impairment (<10% vs. ≥10%).
Results:
Injured workers who had returned to work reported that permanent impairment made it difficult to get a job (47%) and to keep their job (58%). A year after claim closure, 66% reported moderate to very severe pain; 40% reported pain interference with work. About 13% reported new work injuries; over half thought permanent impairment increased their reinjury risk. Asked to compare current to pre-injury work status, workers with a higher degree of impairment more frequently reported working fewer hours (OR: 1.60; 95% CI: 1.06, 2.42), earning less (OR: 1.56; 95% CI: 1.04, 2.36), and being at higher risk of losing their current job due to their impairment (OR: 1.66; 95% CI: 1.01, 2.71).
Conclusions:
Injured workers with permanent impairment face long-term challenges related to health limitations, chronic pain, work reintegration, and economic impacts. Workers with a higher degree of impairment more frequently reported several economic and job security challenges. Developing workplace and workers’ compensation-based interventions that reduce return-to-work interruption and reinjury for workers with permanent impairment should be prioritized as an important public health and societal goal.
Keywords: occupational injuries, workers’ compensation, return to work, chronic pain, health status
Introduction
Roughly 10% of the nearly 3 million annual nonfatal occupational injuries and illnesses in the U.S. result in permanent impairment and a permanent partial disability (PPD) award [1]. Workers’ compensation (WC)-based PPD awards are intended to compensate injured workers for permanent impairment resulting from work injuries or illnesses (e.g., vision or hearing loss, amputation, spinal impairment) that prevent a worker from working at full physical capacity, but do not completely preclude returning to work. Throughout this paper, permanent impairment is used specifically in the context of a WC-based PPD award, while disability is used to refer to functional limitations more generally.
Workers disabled by an occupational injury face substantial employment challenges, even after vocational retraining to facilitate returning to work [2]. After initial return to work following a work injury, many workers with permanent impairment face return-to-work interruption (breaks in employment due to reinjury, disability, lay-off, etc.) [3]. Permanent impairment puts workers at higher risk of mortality [4], in addition to higher risk of return-to-work challenges related to unstable health, functional disability, and pain [2, 3, 5–7]. Disabled workers have unemployment rates that are 50% higher than other workers, and are more likely to work part-time and in entry-level jobs [8, 9]. Workplace functional limitations are prevalent—reported by 22% of employed U.S. workers [10]. Physical disability is the most common reason to exit the workforce before age 60 [11]. Among Canadian workers who were 50-64 years of age and had a permanent impairment, a higher (more severe) impairment rating was associated with earlier labor force exit [12].
Although reinjury rates specific to workers with permanent impairment are unknown, workers with disabilities are more than twice as likely to incur work injuries as those without disabilities [6]. Occupational injuries are more common, more severe, and more costly among workers with hearing and visual impairments [13–15] and other persistent disabilities [16, 17]. Subsequent work injuries are generally more severe and more costly than initial injuries [18, 19]. Injured workers are at heightened risk of both injury exacerbation/repetition and new injuries during the first 12 to 18 months after initial injury [18, 20–22].
Employment is a critical social determinant of health [23], and successful return to work is important for the health and economic stability of workers and for workplace productivity. The purpose of this study was to descriptively quantify the self-reported experiences of injured workers during their first year of work reintegration after WC claim closure with a PPD award—a time period that may involve particularly high risks of reinjury and job loss, and which may also determine long-term employment prospects. We used a representative exploratory survey to characterize health, disability, pain, return-to-work interruption, reinjury, and economic outcomes for these workers. In addition, we summarized survey responses by degree of whole body impairment (<10% WBI vs. ≥10% WBI).
Methods
Study design
We conducted a representative descriptive cross-sectional survey designed to gather information about the first year of work reintegration for a retrospective cohort of Washington State workers with a work-related permanent impairment and associated PPD award recorded by the Washington State Department of Labor and Industries (L&I). The degree of permanent impairment was rated at workers’ compensation claim closure (see Data definitions section), and the initial sample was identified by L&I staff, who delivered contact information along with administrative WC claims data to the research team. The survey was conducted about a year after PPD rating and claim closure.
Administrative data source
Washington State has a single payer WC system (the State Fund) that covers approximately 70% of workers specified by Washington’s Industrial Insurance Act [24]. L&I performs the functions of an insurer for State Fund claims and administers the state WC system for both State Fund and self-insured employers (who account for the remaining 30%). Private WC insurers do not operate in Washington State, which facilitates population-based research [25].
Several months before the survey, we obtained L&I administrative data associated with the qualifying closed claim for all potentially eligible workers, including contact information, claim descriptors (e.g., injury date, State Fund or self-insured coverage, claim status), sociodemographic information (e.g., gender, age, county of residence), employment information at time of the pertinent injury (e.g., occupation, industry), vocational rehabilitation involvement, and PPD data (e.g., body part, impairment percentages). For State Fund claims only, we also obtained data regarding total medical costs and total number of compensated days for time lost from work.
Study population and sample frame
Workers were potentially eligible for this study if they met inclusion criteria by having (1) an accepted Washington State WC claim (either State Fund or self-insured) that (2) closed between January 1, 2018 and April 30, 2018 with (3) an associated PPD award. Prior to delivering contact information and administrative data for potentially eligible workers to the research team, L&I staff applied six exclusion criteria: (1) no valid phone number on record; (2) under age 18 when injured; (3) fatal or total permanent disability claims; (4) residence outside Washington State; (5) L&I employees and other confidentiality exclusions imposed by L&I; and (6) deceased workers. After applying inclusion and exclusion criteria, L&I staff identified 2,541 workers who were potentially eligible for the survey during the specified time period. This served as the initial sample frame. We attempted to interview all eligible workers in this sample, and no probability sampling was conducted. Two additional exclusion criteria could be determined only during eligibility screening by survey interviewers: (1) language or comprehension barrier; and (2) no return to work since the impairment, as determined by a worker’s affirmative response to the question, “Have you returned to work since the injury that caused your impairment or disability, even if only very briefly?” Although only workers who had returned to work were surveyed, eligibility questions were structured to allow for estimation of the percentage of workers with permanent impairment who had not returned to work at all since claim closure.
Survey development and survey domains
The worker survey was developed in collaboration with L&I experts and stakeholders, and by consulting the relevant research and grey literature. Where feasible, questions were drawn from previously conducted surveys [26–35]. We queried respondents about eight of the 18 conditions from the Functional Comorbidity Index, which is a validated instrument for predicting functional outcomes in community-based adult populations [36]. We selected the eight conditions (i.e., arthritis, chronic back pain/disease, depression, anxiety, obesity, upper gastrointestinal disease, asthma, diabetes) because they were identified as the most prevalent (at least 5%) among workers with Washington State WC claims for (1) carpal tunnel syndrome, and (2) upper extremity fractures [37]. Survey content was also developed using findings from previous surveys and qualitative interviews of workers who returned to work after vocational rehabilitation, with a focus on patterns of employment and return-to-work interruption, reinjury, and potentially modifiable workplace and WC-based risk factors [7, 20, 34, 35]. Expert consultation was provided by the Survey Research Division of the Social Development Research Group, an interdisciplinary research team based in the University of Washington School of Social Work. Survey questions were finalized after internal testing and timing by Survey Research Division staff. Results presented herein focus on five domains: (1) worker and injury characteristics; (2) health, function, impairment, and pain; (3) chronic health conditions and their effect on ability to work; (4) workforce reintegration, return-to-work interruption, and reinjury; and (5) economic outcomes.
Survey administration and response bias assessment
Computer-assisted interviews were conducted by Survey Research Division staff from February 6 through April 20, 2019. There were at least 4 to 8 call attempts per worker, which varied by day (weekday/weekend) and time of day. Workers were interviewed about a year (11-15 months) after claim closure (mean: 12.8 months). Interviews averaged 39 minutes each. Advance recruitment letters offered mechanisms to opt-out or schedule an interview and described the 30 USD gift card for participation, which was provided by mail or email after the interview. Respondents contacted by phone were given the option to reschedule the interview at a convenient time.
In total, 599 interviews were conducted (582 complete and 17 partial interviews). Sample exclusions and attrition are depicted in Fig. 1. The response rate was calculated following recommendations published by the American Association for Public Opinion Research (AAPOR) [38]. The overall adjusted response rate was 53.8%, following the standard AAPOR formula for Response Rate 4, selected because it (1) includes partial surveys in the numerator (enough questions were answered that they were usable for many purposes), and (2) includes an adjustment for the estimated proportion of workers with unknown eligibility that were eligible (e), which we calculated using the conservative AAPOR default method (proportion of eligible workers among all workers in the sample for which a definitive determination of status was obtained), resulting in e=0.438 (609 eligible/609 eligible+780 ineligible). The Response Rate 4 formula is: (Complete interviews [n=582] + partial interviews [n=17])/((Complete interviews [n=582] + partial interviews [n=17]) + (Eligible, non-interview [n=10]) + e(Unknown eligibility, non-interview [n=1,152])) [38].
Fig. 1.
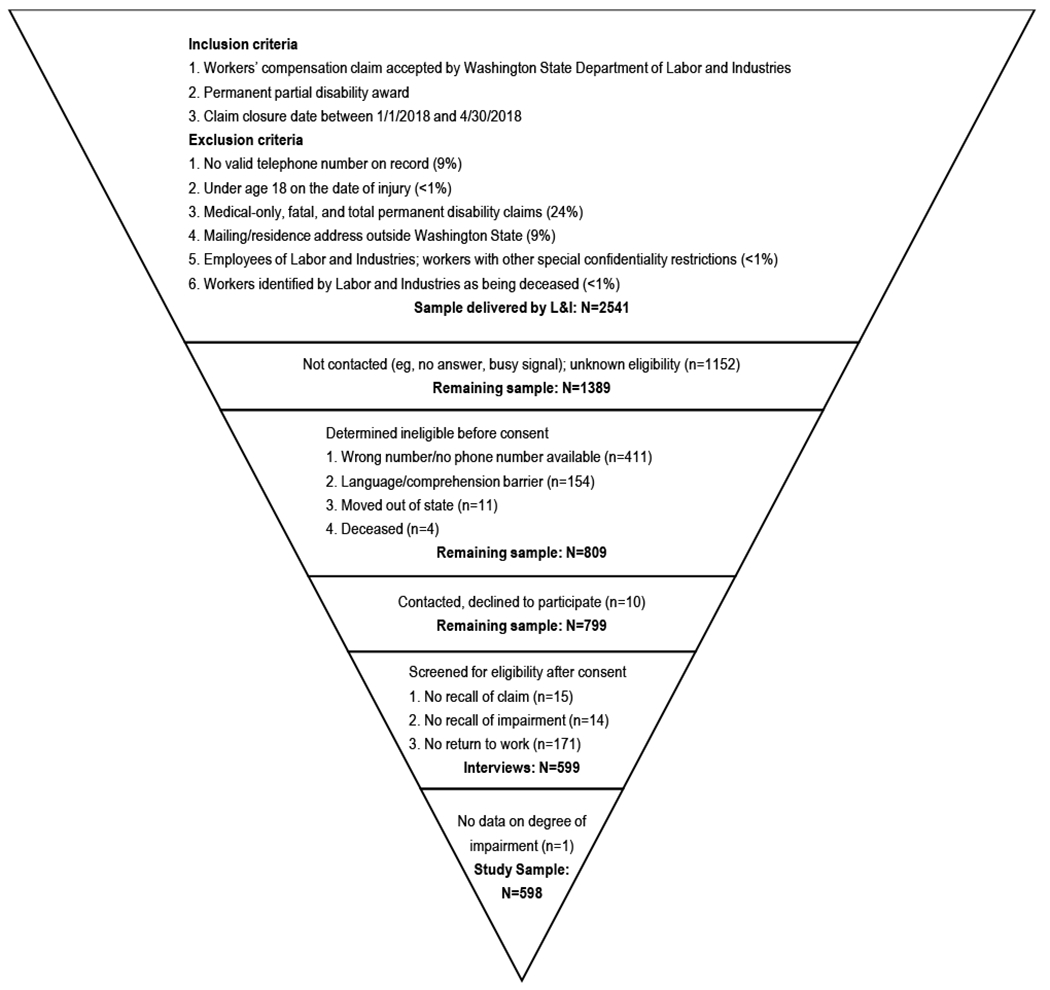
Study sample selection
After excluding workers found ineligible during screening, survey respondents (N=599) were compared to nonrespondents (N=1,573) using administrative WC data. On average, respondents were about one year younger when surveyed (49.3 years old; SD 11.6) compared to nonrespondents (50.7 years old; SD 11.6). For both respondents and nonrespondents, 2016 was the median injury year. Respondents did not substantially or significantly differ from nonrespondents with regard to any of the following characteristics: age when injured, State Fund vs. self-insured coverage, whether the qualifying closed claim was their first Washington State WC claim, age at injury, gender, adjusted pre-injury wage, urban-rural residence, whether a vocational rehabilitation plan was completed, and—among State Fund claims only, due to data availability—traumatic injury vs. other injury type, and injury severity (maximum Abbreviated Injury Scale).
Data definitions
Washington State defines impairment as permanent anatomic or functional abnormality or loss of function after maximum medical improvement has been achieved [39]. Workers may be rated with regard to degree of impairment for a PPD award if treatment has been completed and the worker is still able to work, but has suffered a permanent loss of function [40]. Washington State uses two different PPD rating systems, depending on the type of impairment: (1) specified PPD, and (2) unspecified PPD [39]. Awards for specified PPD impairments are listed in state rule, and include amputation, loss of function of extremities, hearing loss, and vision loss. Impairment for loss of function of extremities or partial hearing or vision loss is rated using the AMA Guides to the Evaluation of Permanent Impairment, 5th Edition [41], unless otherwise mandated by L&I. Unspecified PPD impairments include internal injuries, back injuries, mental health conditions, respiratory disorders, and other disorders affecting the internal organs; these are rated using category award schedules that are updated each fiscal year and applied based on injury date [40].
Administrative WC PPD data are difficult to summarize for various reasons (i.e., there were frequently multiple entries for the same PPD award, which were often indistinguishable as to whether they represented duplicate entries, multiple/bilateral injuries, pre-existing unpaid impairment based on evaluation, protests, repayments, or other subsequent increases or decreases in the PPD award). We constructed a measure of WBI that would allow us to compare workers based on a conservative estimate of WBI percentage, regardless of the rating system used to produce an individual worker’s rating or award. L&I PPD data contained the following information for each eligible impairment (workers could have multiple impaired body parts): (1) PPD benefit eligibility effective dates (per L&I guidance, only records for the most recent date were used when there were multiple effective dates for the same claim—generally representing updates due to protests/appeals); (2) award amounts for each impaired body part; (3) percent impairment for each impaired body part; and (4) major body part code corresponding to each impaired body part. For example, the major body part code might be finger, with the impaired body part code specifying which joint level of which finger(s). We calculated WBI percentage in three main steps. First, we calculated the WBI percentage multiplier for all major body part codes found in the data, using three methods. For impairments listed in the L&I PPD Category Awards list [40], the multiplier was set to 1.0 (for category awards, percent impairments in the database were equal to WBI percentage). For other impairments, we used the AMA Guides to identify WBI percentage multipliers for each major body part code [41]. When multipliers were not available in the AMA Guides for a specific impairment (e.g., loss of one eye by enucleation), the multiplier was estimated by dividing the award amount listed for a particular impairment in the L&I PPD Awards Schedule by the statutory award amount for 100% impairment, using amounts specific to the fiscal year of each worker’s injury date. Fiscal year-specific amounts are available online [40]. The second step was to multiply the resulting WBI percentage multiplier (specific to major body part code) by the percent impairment for each impaired body part, thus assigning an estimated WBI percentage to each impaired body part for each worker. For the 5.0% of claims having a PPD award but missing percent impairment data for an impaired body part, the WBI percentage was estimated by dividing the actual PPD award for a particular impairment by the fiscal year-specific statutory award amount for 100% impairment [40]. Third, for workers with multiple impaired body parts, we retained only the impaired body part with the highest WBI percentage. Although this likely introduced some underestimation of WBI, we took a conservative approach and did not sum all WBI percentages for each worker, due to the inability to distinguish duplicate entries or pre-existing injuries from multiple eligible impairments. The resulting estimate can best be thought of as a lower bound estimate of WBI, based on the single largest contribution from the single impaired body part contributing most to WBI The highest calculated WBI percentage estimate was 49.2% (median 5.0%, mean 6.2%, SD 5.4%). For purposes of comparing workers with a higher degree of impairment to workers with a lower degree of impairment, we cut the estimated WBI percentage at the 80th percentile, thereby comparing workers with an estimated WBI percentage below 10% to workers with an estimated WBI percentage of 10% and above. One surveyed worker did not have administrative data available for calculation of WBI, and was excluded from this study.
Body part categories (upper extremity, lower extremity, spine, mental health, other) were based on the body part used for the WBI percentage estimate. Urban-rural residence was based on residence county indicated in the WC claims data, and classified using the 6-level 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties [42]. Reinjury was defined as any self-reported work injury resulting in at least one missed day of work.
Data analysis
Survey measures excluded those who responded, “Don’t know,” or refused to answer, resulting in varying numbers of responses for each question. For many survey questions, responses were collapsed into binary variables or fewer categories for ease of presentation. Response patterns for workers with an estimated WBI percentage below 10% were compared to those for workers with an estimated WBI percentage of 10% and above using unadjusted logistic regression models; robust variance estimates were used to produce 95% confidence intervals (CI) for crude odds ratios (OR). Analyses were conducted using Stata/MP 15.1 for Windows (StataCorp, College Station, TX, USA) [43].
Results
Of workers contacted and otherwise eligible for the survey, 22.2% (171 of 770) were ineligible specifically because they had not returned to work even briefly during the first year after claim closure (Fig. 1). Year of injury ranged from 1991 to 2018; 4.5% were injured before 2011. Upper extremity impairment contributed most to the WBI rating for nearly half (48.7%) of the study sample of 598 workers (Table 1). The distributions of sociodemographic characteristics were roughly similar across the two WBI categories (Table 1).
Table 1.
Worker and injury characteristics for Washington State workers surveyed about a year after workers’ compensation claim closure with a permanent partial disability (PPD) award
| Characteristic | Data source | N | Overall (N=598) | WBI <10% (N=464) | WBI ≥10% (N=134) |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Gender | Admin | 598 | |||
| Men | 403 (67.4) | 306 (66.0) | 97 (72.4) | ||
| Women | 195 (32.6) | 158 (34.1) | 37 (27.6) | ||
| Age at survey | Admin | 598 | |||
| 19-24 | 15 (2.5) | 14 (3.0) | 1 (0.8) | ||
| 25-34 | 62 (10.4) | 50 (10.8) | 12 (9.0) | ||
| 35-44 | 116 (19.4) | 91 (19.6) | 25 (18.7) | ||
| 45-54 | 165 (27.6) | 133 (28.7) | 32 (23.9) | ||
| 55-64 | 206 (34.5) | 149 (32.1) | 57 (42.5) | ||
| 65-73 | 34 (5.7) | 27 (5.8) | 7 (5.2) | ||
| Educational level | Survey | 579 | |||
| Not HS graduate/no GED | 23 (4.0) | 19 (4.2) | 4 (3.1) | ||
| HS graduate/GED | 144 (24.9) | 117 (26.0) | 27 (20.9) | ||
| Some college | 297 (51.3) | 230 (51.1) | 67 (51.9) | ||
| College graduate | 115 (19.9) | 84 (18.7) | 31 (24.0) | ||
| Pre-tax earnings during past year | Survey | 559 | |||
| < 20,000 USD | 75 (13.4) | 53 (12.2) | 22 (17.5) | ||
| 20,000 to < 40,000 USD | 124 (22.2) | 99 (22.9) | 25 (19.8) | ||
| 40,000 to < 60,000 USD | 147 (26.3) | 115 (26.6) | 32 (25.4) | ||
| 60,000 to < 80,000 USD | 88 (15.7) | 73 (16.9) | 15 (11.9) | ||
| 80,000+ USD | 125 (22.4) | 93 (21.5) | 32 (25.4) | ||
| Race/ethnicity | Survey | 598 | |||
| White/Caucasian | 467 (78.1) | 358 (77.2) | 109 (81.3) | ||
| Black/African American | 20 (3.3) | 17 (3.7) | 3 (2.2) | ||
| Asian | 15 (2.5) | 10 (2.2) | 5 (3.7) | ||
| American Indian/Alaska Native | 7 (1.2) | 7 (1.5) | 0 (0.0) | ||
| Native Hawaiian/Pacific Islander | 9 (1.5) | 6 (1.3) | 3 (2.2) | ||
| Latino (any race) | 34 (5.7) | 31 (6.7) | 3 (2.2) | ||
| Multiple | 20 (3.3) | 16 (3.5) | 4 (3.0) | ||
| Unknown/vague | 26 (4.4) | 19 (4.1) | 7 (5.2) | ||
| Nativity | Survey | 579 | |||
| Born in U.S. | 526 (90.9) | 405 (90.0) | 121 (93.8) | ||
| Born outside U.S. | 53 (9.2) | 45 (10.0) | 8 (6.2) | ||
| Urban/rural residence | Admin | 590 | |||
| Large central metro | 122 (20.7) | 98 (21.4) | 24 (18.1) | ||
| Large fringe metro | 209 (35.4) | 154 (33.7) | 55 (41.4) | ||
| Medium metro | 126 (21.4) | 100 (21.9) | 26 (19.6) | ||
| Small metro | 60 (10.2) | 44 (9.6) | 16 (12.0) | ||
| Micropolitan | 56 (9.5) | 47 (10.3) | 9 (6.8) | ||
| Noncore | 17 (2.9) | 14 (3.1) | 3 (2.3) | ||
| Body part | Admin | 598 | |||
| Upper extremity | 291 (48.7) | 245 (52.8) | 46 (34.3) | ||
| Lower extremity | 178 (29.8) | 147 (31.7) | 31 (23.1) | ||
| Spine | 95 (15.9) | 51 (11.0) | 44 (32.8) | ||
| Mental health | 6 (1.0) | 0 (0.0) | 6 (4.5) | ||
| Other | 28 (4.7) | 21 (4.5) | 7 (5.2) | ||
Admin, administrative workers’ compensation data; GED, General Education Diploma; HS, high school; metro, metropolitan; PPD, permanent partial disability; U.S., United States; USD, United States Dollar; WBI, whole body impairment.
Note: Column percentages do not always sum to exactly 100% due to rounding.
Total days of time-loss compensation and total medical costs for the WC claim that closed with a PPD award were available only for the 62.4% of surveyed workers (373 of 598) covered by the State Fund (vs. self-insurance). State Fund workers had 374 mean days of time-loss compensation (SD 598 days); workers with a higher degree of impairment had substantially more time-loss days on average (710 days for workers with ≥10% WBI, vs. 260 days for workers with <10% WBI; mean difference 450 days, 95% CI [259, 642]). Mean total medical costs were 35,077 USD (SD 18,648 USD) for State Fund workers; workers with a higher degree of impairment had substantially higher medical costs on average (67,970 USD for workers with ≥10% WBI, vs. 23,995 USD for workers with <10% WBI; mean difference 43,975 USD, 95% CI [27,515 USD, 60,436 USD]).
Workers with a higher degree of impairment more frequently reported fair to poor health status and work functioning (vs. good to excellent), both at claim closure (retrospectively) and at the time of their interview (Table 2). Notably, 47.5% of those surveyed reported that their permanent impairment made it difficult to get a job, and 58.0% reported that their permanent impairment made it difficult to keep their job. Nearly two-thirds of workers reported moderate to very severe bodily pain during the past four weeks, and 39.9% reported at least some pain interference with work during that timeframe. With a 95% level of confidence, we found that workers with a higher degree of impairment had a higher odds of reporting poorer health status, poorer work-related functional ability, and difficulty getting or keeping a job, relative to workers with a lower degree of impairment. Further, although the 95% confidence interval included the null, the same direction of effect was seen for several other survey questions reported in Table 2, including continuing to experience (1) disability, pain or work limitations; (2) moderate to severe bodily pain, and (3) pain interference with work. Overall, 10.6% (N=61) reported taking chronic opioids (60 or more days in a row over the past year), and only 36.1% of that subset reported that taking opioids helped them work or function at their best (Table 2).
Table 2.
Health, function, impairment, and pain, as reported by Washington State workers surveyed about a year after workers’ compensation claim closure with a permanent partial disability (PPD) award; crude odds ratios (OR) with 95% confidence intervals (CI) comparing response patterns for workers with a higher degree of whole body impairment (≥10% WBI) to those with a lower degree of impairment (WBI <10%)
| Survey question | N | Overall (N=598) | WBI <10% (N=464) | WBI ≥10% (N=134) | Crude OR (95% CI) |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Health status at claim closure | 595 | ||||
| Fair/poor | 166 (27.9) | 119 (25.8) | 47 (35.1) | 1.55 | |
| Good/very good/excellent | 429 (72.1) | 342 (74.2) | 87 (64.9) | (1.03, 2.34) | |
| Current health status | 594 | ||||
| Fair/poor | 165 (27.8) | 117 (25.4) | 48 (36.1) | 1.66 | |
| Good/very good/excellent | 429 (72.2) | 344 (74.6) | 85 (63.9) | (1.10, 2.51) | |
| Work function ability at claim closure | 592 | ||||
| Fair/poor | 215 (36.3) | 153 (33.3) | 62 (46.6) | 1.75 | |
| Good/very good/excellent | 377 (63.7) | 306 (66.7) | 71 (53.4) | (1.18, 2.59) | |
| Current work function ability | 590 | ||||
| Fair/poor | 186 (31.5) | 131 (28.6) | 55 (41.7) | 1.78 | |
| Good/very good/excellent | 404 (68.5) | 327 (71.4) | 77 (58.3) | (1.19, 2.66) | |
| Still have disability/pain/limitation due to work injury | 597 | ||||
| Yes | 553 (92.6) | 426 (92.0) | 127 (94.8) | 1.58 | |
| No | 44 (7.4) | 37 (8.0) | 7 (5.2) | (0.69, 3.62) | |
| Impairment/disability/pain | 550a | ||||
| Made it difficult to get a job | 261 (47.5) | 190 (44.2) | 71 (59.2) | 1.83 | |
| Did not make it difficult to get a job | 289 (52.6) | 240 (55.8) | 49 (40.8) | (1.21, 2.76) | |
| Impairment/disability/pain | 590 | ||||
| Made it difficult to stay at work or keep a job | 342 (58.0) | 248 (54.0) | 94 (71.8) | 2.16 | |
| Did not make it difficult to stay at work or keep a job | 248 (42.0) | 211 (46.0) | 37 (28.2) | (1.42, 3.30) | |
| Bodily pain in past 4 weeks | 594 | ||||
| Moderate/severe/very severe | 389 (65.5) | 293 (63.6) | 96 (72.2) | 1.49 | |
| Very mild or no pain | 205 (34.5) | 168 (36.4) | 37 (27.8) | (0.97, 2.27) | |
| Pain interfered with work in past 4 weeks | 592 | ||||
| Some what/quite a bit/very much | 236 (39.9) | 181 (39.3) | 55 (42.0) | 1.12 | |
| Not at all/a little bit | 356 (60.1) | 280 (60.7) | 76 (58.0) | (0.75, 1.66) | |
| Pain in past 4 weeks was impairment-related | 536b | ||||
| Sometimes/always | 453 (84.5) | 337 (81.6) | 116 (94.3) | 3.74 | |
| Never/almost never | 83 (15.5) | 76 (18.4) | 7 (5.7) | (1.67, 8.34) | |
| Took opioids for pain 60+ days in a row in past year | 593 | ||||
| Yes | 63 (10.6) | 44 (9.6) | 19 (14.3) | 1.58 | |
| No | 530 (89.4) | 416 (90.4) | 114 (85.7) | (0.88, 2.81) | |
| Opioid medication taken for pain | 61c | ||||
| Helped me work/function at my best | 22 (36.1) | 14 (32.6) | 8 (44.4) | 1.66 | |
| Had no effect or made work/function more difficult | 39 (63.9) | 29 (67.4) | 10 (55.6) | (0.53, 5.17) | |
CI, confidence interval; OR, odds ratio; PPD, permanent partial disability; WBI, whole body impairment.
Many workers still working for their pre-injury employer answered this question “Don’t Know.”
Queried only if reported any pain.
Queried only if reported taking opioids for 60+ days in a row.
Note: In each unadjusted logistic regression model, the independent variable was WBI percentage, comparing responses for workers with higher WBI to those with lower WBI (the reference category). ORs are shown on the row containing the response that was coded as 1; CIs are shown on the row containing the response that was coded as 0. Column percentages do not always sum to exactly 100% due to rounding.
The vast majority of workers surveyed (87.6%) were working for pay when interviewed, and 82.5% reported that their current or most recent job was full-time (Table 3). When asked to estimate the average percent time they had worked over the year since claim closure, respondents reported working 82.2% of full-time (SD 28.1), on average. The number of distinct jobs held since claim closure ranged from one to six; 79.0% of workers surveyed had a single job during the past year. At the time of the interview, 42.5% reported being a union member. We found that workers with a higher degree of impairment had a 70% higher odds of working in a different occupation than when they were injured, relative to workers with a lower degree of impairment (95% CI [1.13, 2.56]). Although the 95% confidence interval included the null, workers with a higher degree of impairment had an estimated 44% higher odds of their first job after claim closure being with a new employer, rather than with the employer where they were injured (95% CI [0.95, 2.19]). Among those working at the time of the interview (N=500), workers with a higher degree of impairment had a 66% higher odds of reporting that their impairment put them at higher risk of losing their job, relative to workers with a lower degree of impairment (95% CI [1.01, 2.71]). During the year since claim closure, 13.4% of workers reported at least one new work injury that involved at least one missed day of work (Table 3).
Table 3.
Workforce reintegration, return-to-work interruption, and reinjury, as reported by Washington State workers surveyed about a year after workers’ compensation claim closure with a permanent partial disability (PPD) award; crude odds ratios (OR) with 95% confidence intervals (CI) comparing response patterns for workers with a higher degree of whole body impairment (≥10% WBI) to those with a lower degree of impairment (WBI <10%)
| Survey question | N | Overall (N=598) | WBI <10% (N=464) | WBI ≥10% (N=134) | Crude OR (95% CI) |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Working for pay when interviewed | 589 | ||||
| Currently working | 516 (87.6) | 402 (87.6) | 114 (87.7) | 1.01 | |
| Not currently working | 73 (12.4) | 57 (12.4) | 16 (12.3) | (0.56, 1.83) | |
| Current/most recent employment type | 590 | ||||
| Full-time traditional | 487 (82.5) | 381 (83.2) | 106 (80.3) | 0.82 | |
| Part-time, temporary, seasonal, or self-employed | 103 (17.5) | 77 (16.8) | 26 (19.7) | (0.50, 1.35) | |
| Union membership | 588 | ||||
| Currently a union member | 250 (42.5) | 191 (41.9) | 59 (44.7) | 1.12 | |
| Not currently a union member | 338 (57.5) | 265 (58.1) | 73 (55.3) | (0.76, 1.66) | |
| Industry sector now versus when injureda | 588 | ||||
| Industry sector now different than when injured | 258 (43.9) | 201 (44.1) | 57 (43.2) | 0.96 | |
| Industry sector not different | 330 (56.1) | 255 (55.9) | 75 (56.8) | (0.65, 1.43) | |
| Occupation now versus when injured | 588 | ||||
| Occupation now different than when injured | 177 (30.1) | 126 (27.5) | 51 (39.2) | 1.70 | |
| Occupation not different | 411 (69.9) | 332 (72.5) | 79 (60.8) | (1.13, 2.56) | |
| Employer for initial RTW versus when injured | 591 | ||||
| Initial RTW with different employer | 166 (28.1) | 121 (26.4) | 45 (34.1) | 1.44 | |
| Initial RTW with same employer | 425 (71.9) | 338 (73.6) | 87 (65.9) | (0.95, 2.19) | |
| New work injuriesb since claim closure | 590 | ||||
| One or more new work injuries | 79 (13.4) | 60 (13.1) | 19 (14.5) | 1.13 | |
| No new work injuries | 511 (86.6) | 399 (86.9) | 112 (85.5) | (0.65, 1.97) | |
| Risk of being reinjured at work due to impairment | 569 | ||||
| At higher risk now compared to before injury | 371 (65.2) | 285 (64.2) | 86 (68.8) | 1.23 | |
| Not at higher risk now compared to before injury | 198 (34.8) | 159 (35.8) | 39 (31.2) | (0.80, 1.88) | |
| Risk of being reinjured at work due to impairment | 561 | ||||
| At higher risk compared to others doing same job | 305 (54.4) | 236 (53.9) | 69 (56.1) | 1.09 | |
| Not at higher risk compared to others doing same job | 256 (45.6) | 202 (46.1) | 54 (43.9) | (0.73, 1.64) | |
| Risk of losing current job due to impairment | 500c | ||||
| At higher risk due to impairment | 102 (20.4) | 72 (18.5) | 30 (27.3) | 1.66 | |
| Not at higher risk due to impairment | 398 (79.6) | 318 (81.5) | 80 (72.7) | (1.01, 2.71) | |
| Will be working in 6 months | 567 | ||||
| Certain | 456 (80.4) | 355 (80.7) | 101 (79.5) | 0.93 | |
| Uncertain | 111 (19.6) | 85 (19.3) | 26 (20.5) | (0.57, 1.52) | |
RTW, returned to work; CI, confidence interval; OR, odds ratio; PPD, permanent partial disability; WBI, whole body impairment.
Survey response for industry sector was compared to administrative workers’ compensation data for industry sector when injured.
For this question, qualifying work injuries were defined as those resulting in at least one missed day from work.
Queried only if currently working.
Note: In each unadjusted logistic regression model, the independent variable was WBI percentage, comparing responses for workers with higher WBI to those with lower WBI (the reference category). ORs are shown on the row containing the response that was coded as 1; CIs are shown on the row containing the response that was coded as 0. Column percentages do not always sum to exactly 100% due to rounding.
Workers were asked whether they had been diagnosed with, affected by, or treated for eight specified chronic health conditions, during the year since claim closure. Arthritis (rheumatoid or osteoarthritis) was reported as most prevalent, and diabetes (type I or II) as least prevalent (Fig. 2). The self-reported effect of each condition on ability to work in the past year followed roughly the same ordering, except that chronic back pain/disease and depression were most frequently reported as interfering with ability to work, both more so than arthritis. Chronic back pain/disease was reported by 24.1% of the sample (144 of 598). The spine was the main impaired body part for 15.9% of the sample (95 of 598); fully half of that subset (48 of 95) reported chronic back pain/disease (which may have resulted from the primary spine impairment as opposed to representing a distinct comorbidity).
Fig. 2.
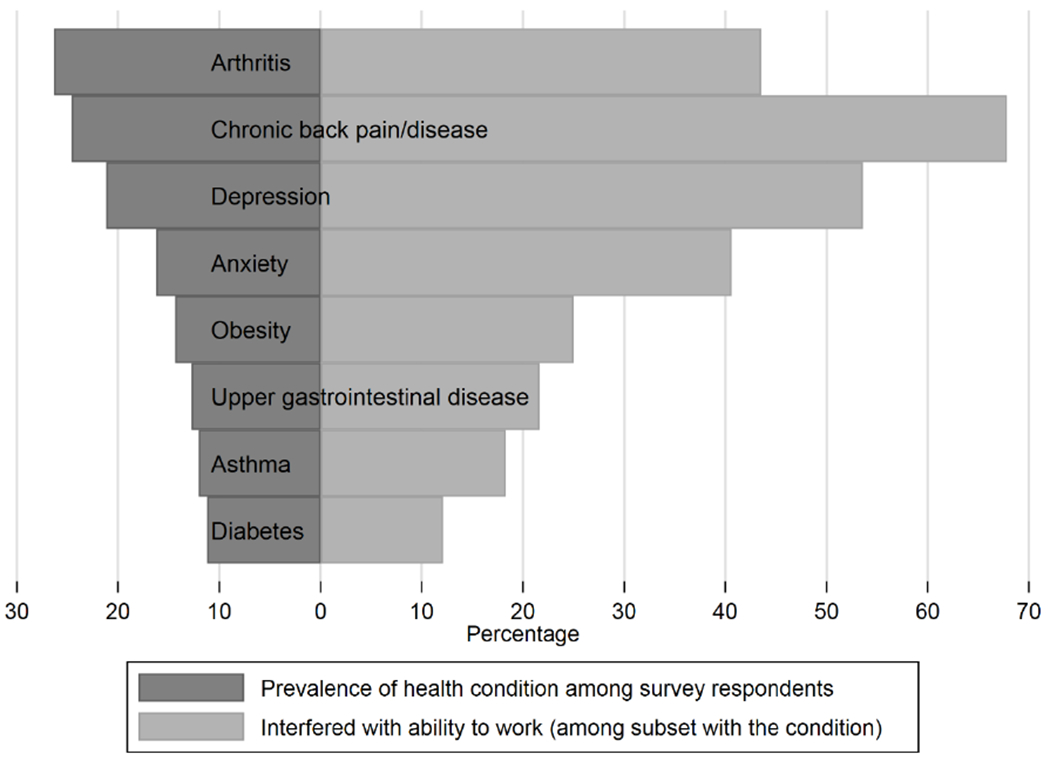
Chronic health conditions, as reported by Washington State workers surveyed about a year after workers’ compensation claim closure with a permanent partial disability (PPD) award
More than a quarter of workers reported working fewer hours and earning less at the time they were interviewed, compared to before the injury, and 28.8% reported often worrying about their total income not being enough to meet expenses. Workers with a higher degree of impairment more frequently reported both working fewer hours and earning less at the time they were interviewed, compared to before the injury (Table 4). Among all workers surveyed, 37.4% reported having no health insurance coverage via their employer, and 9.1% reported having no health insurance coverage at all (Table 4).
Table 4.
Economic outcomes, as reported by Washington State workers surveyed about a year after workers’ compensation claim closure with a permanent partial disability (PPD) award; crude odds ratios (OR) with 95% confidence intervals (CI) comparing response patterns for workers with a higher degree of whole body impairment (≥10% WBI) to those with a lower degree of impairment (WBI <10%)
| Survey question | N | Overall (N=598) | WBI <10% (N=464) | WBI ≥10% (N=134) | Crude OR (95% CI) |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Number of work hours now versus before impairment | 580 | ||||
| Working fewer hours now | 171 (29.5) | 122 (27.2) | 49 (37.4) | 1.60 | |
| Working the same or more hours now | 409 (70.5) | 327 (72.8) | 82 (62.6) | (1.06, 2.42) | |
| Earnings now versus before impairment | 583 | ||||
| Earning less now | 170 (29.2) | 122 (27.0) | 48 (36.6) | 1.56 | |
| Earning the same or more now | 413 (70.8) | 330 (73.0) | 83 (63.4) | (1.04, 2.36) | |
| Worry about total income not being enough to meet expenses | 579 | ||||
| Often worry | 167 (28.8) | 123 (27.3) | 44 (34.1) | 1.38 | |
| Sometimes/never worry | 412 (71.2) | 327 (72.7) | 85 (65.9) | (0.90, 2.09) | |
| Contacted by collection agency in past 3 months | 579 | ||||
| Yes | 102 (17.6) | 77 (17.1) | 25 (19.4) | 1.16 | |
| No | 477 (82.4) | 373 (82.9) | 104 (80.6) | (0.71, 1.92) | |
| Housing at risk due to underpaid rent/mortgage in past 3 months | 582 | ||||
| Yes | 57 (9.8) | 43 (9.5) | 14 (10.8) | 1.15 | |
| No | 525 (90.2) | 409 (90.5) | 116 (89.2) | (0.61, 2.17) | |
| Health insurance coverage from employer | 580 | ||||
| No | 217 (37.4) | 170 (37.8) | 47 (36.2) | 0.93 | |
| Yes | 363 (62.6) | 280 (62.2) | 83 (63.9) | (0.62, 1.40) | |
| Health insurance coverage from any source | 581 | ||||
| No | 53 (9.1) | 46 (10.2) | 7 (5.4) | 0.50 | |
| Yes | 528 (90.9) | 405 (89.8) | 123 (94.6) | (0.22, 1.14) | |
CI, confidence interval; OR, odds ratio; PPD, permanent partial disability; WBI, whole body impairment.
Note: In each unadjusted logistic regression model, the independent variable was WBI percentage, comparing responses for workers with higher WBI to those with lower WBI (the reference category). ORs are shown on the row containing the response that was coded as 1; CIs are shown on the row containing the response that was coded as 0. Column percentages do not always sum to exactly 100% due to rounding.
Discussion
Based on reports by workers contacted for the survey, 22.2% of otherwise eligible workers with permanent impairment had not returned to work even briefly during the first year after WC claim closure. This likely underestimates the percentage of workers with permanent impairment who had not returned to work, because the survey recruitment letters described at least brief return to work as an eligibility criterion, and workers who already knew they were ineligible may not have answered the call. An earlier study, using state wage data (2006 through 2011) for Washington State Fund workers eligible for vocational retraining (not all of whom had permanent impairments), found that roughly 60% did not have any reported wages during the first year after WC claim closure [44].
The vast majority (87.6%) of workers responding to our survey were working when interviewed. Respondents estimated they had worked 82.2% of full-time when averaged over the past year, which could reflect either some delay in return to work after claim closure, and/or gaps in employment. Nearly half (47.5%) of those surveyed reported that their permanent impairment made it difficult to get a job, and 58.0% reported that their permanent impairment made it difficult to keep their job.
More than half of workers surveyed thought their permanent impairment put them at higher risk of being reinjured at work, compared to before their injury (65.2%), or to coworkers in the same job (54.4%). During the year since claim closure, about 13.4% of all surveyed workers reported one or more new work injuries that resulted in at least one missed day of work. We were unable to identify comparable estimates that were both specific to the first year after initial injury or claim closure, and that included workers across all industries with all types of injuries. However, in a study of Veterans Health Administration nursing employees (2002-2005), 19.9% of registered nurses and 29.8% of nursing assistants had a second administratively reported occupational injury/illness (not restricted to those involving time lost from work) occurring within a year of an initial injury/illness report [22]. In a survey of Washington State Fund workers with back injuries (2002-2004), 25.8% of workers reported reinjuring their back at work (not restricted to injuries involving time lost from work) during the year since the initial injury [20].
More than a quarter of surveyed workers (27.8%) reported fair to poor health status at the time they were interviewed. This compares unfavorably with the most recent available Behavioral Risk Factor Surveillance System (2013-2015) estimate of 10.2% among all employed adults [45]. Nearly two-thirds of workers surveyed reported moderate to severe bodily pain during the past four weeks, and the vast majority attributed this pain to the injury that resulted in PPD. Of workers surveyed, 39.9% reported at least some pain interference with work during the same timeframe. Notably, only 36.1% of the subset who had taken chronic opioids during the past year (10.6% of the study sample) reported that taking opioids helped them work or function at their best.
We queried workers regarding the eight chronic health conditions from the Functional Comorbidity Index [36] that were identified by Marcum et al. [37] as most prevalent among workers with Washington State workers’ compensation claims. Arthritis was reported by surveyed workers as the most prevalent of the eight conditions, followed closely by chronic back pain/disease; while chronic back pain/disease and depression were the most frequently reported as interfering with ability to work. With the sole exception of arthritis, the prevalence of each chronic health condition was higher than in the Marcum et al. study. Two possible reasons may be contributory: (1) Marcum et al. used medical billing diagnoses rather than self-report to identify comorbidities, and diagnosis codes for conditions unrelated to treatment of the work-related injury may not be systematically included on WC medical bills; and (2) the Marcum et al. study included all workers who had any compensated temporary or permanent disability (which could be as temporary as missing four days from work), while our study included only workers with some degree of permanent impairment. The Marcum et al. study found that claimants with multiple chronic comorbidities had higher odds of not working after injury, as well as poorer hours and earnings recovery, compared to those with no chronic comorbidities [37].
More than a quarter of workers surveyed (and more than a third of those with ≥10% WBI) reported (1) often worrying about their total income not being enough to meet expenses, and (2) working fewer hours and earning less than before they were injured. These findings comport with a Canadian study documenting that about 12% of permanently impaired workers surveyed (N=494) had poverty-level individual incomes prior to injury, rising to about 27% to 40% after injury (estimate varied by poverty measure) [46].
Of workers surveyed, 9.1% reported having no health insurance, compared to an estimated 7% of the Washington State population, and 9% of the U.S. population (based on 2018 American Community Survey data [47]). Of workers surveyed, 62.6% reported having health insurance via their employer, compared to an estimated 52% of the Washington State population, and 49% of the U.S. population [47].
One unusual characteristic of the survey sample was union membership, which, at 42.5%, was more than double the estimated 19.8% of Washington State employed workers who were union members in 2018 (10.5% for the U.S. overall) [48]. We did not have data on union membership available for survey non-respondents, but we did not observe any noteworthy differences in the many other characteristics used to assess response bias. We do not know whether union membership may be associated with either incurring a permanent impairment or successfully obtaining a PPD award for that impairment.
Although our WBI measure was crude, we did find several interesting, if unsurprising, patterns of association with degree of impairment—supporting content validity. As would be expected, workers with a higher degree of impairment (≥10% WBI) had substantially more time-loss days and higher medical costs for the WC claim that closed with a PPD award, on average, compared to workers with a lower degree of impairment (<10% WBI). Workers with a higher degree of impairment more frequently reported working in a different occupation than when they were injured. Workers with a higher degree of impairment more frequently reported fair to poor health status and work functioning (vs. good to excellent), both at claim closure (retrospectively) and at the time of the interview. Workers with a higher degree of impairment more frequently reported that their permanent impairment made it difficult to get a job (59.2%), and nearly three-quarters (71.8%) reported that their permanent impairment made it difficult to keep their job. When asked to compare their current status to pre-injury status, workers with a higher degree of impairment more frequently reported negative outcomes, including: (1) working fewer hours, (2) earning less, and (3) being at higher risk of losing their job due to permanent impairment.
Strengths and limitations
Many studies have focused on initial return to work after occupational injury; however, this is one of few studies delving into the issues of sustained return to work and return-to-work interruption among injured workers with permanent impairment. This study contributes to a more complete description of the long-term burden of worker injury by focusing on return-to-work interruption and reinjury for workers with permanent impairment—topics which have received little attention but which affect the productivity and economic interests of large numbers of workers and employers. Conducting a worker survey enabled the characterization of work reintegration and reinjury during the year following WC claim closure—a time period which is typically opaque for studies relying solely on WC administrative data. Our inclusion of workers with any type and degree of permanent partial impairment enhances generalizability to a broad range of injuries and conditions, and indications of response bias were negligible. Though representative, the survey was relatively small-scale and exploratory, and may involve some recall bias due to the inclusion of many retrospective questions. Due to data limitations, our estimated WBI percentages represented a lower bound, based solely on the body part contributing most to WBI, which would have a conservative effect on our ability to detect differences in response patterns associated with degree of impairment.
Conclusions
A substantial number of injured workers return to the workplace with lingering or permanent disability. This study describes the long-term challenges related to health limitations, chronic pain, barriers to sustained return to work, and ongoing economic impacts faced by injured workers with permanent impairment. Many of these challenges were exacerbated for injured workers with a higher degree of impairment. In forthcoming related studies, we plan to assess various modifiable workplace factors and WC programs with regard to their relative contributions toward enhancing successful and sustained return to work and reducing reinjury. Employment is a critical social determinant of health, and the development of workplace and WC system interventions that promote sustained return to work and reduce reinjury for workers with permanent impairment should be prioritized as an important public health and societal goal.
Acknowledgements
We thank all survey participants for their time and input. We thank the following Washington State Department of Labor and Industries personnel, who facilitated access to the necessary administrative data and provided extensive data documentation: Gary Franklin (Medical Director), Lisann Rolle (Program Manager, Research and Data Services), and Sarah West (Data Analyst, Research and Data Services). This work was supported by the National Institute for Occupational Safety and Health (NIOSH) under Grant R21OH011355. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. The authors declare no conflicts of interest.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of interest All authors declare that they have no conflicts of interest.
Compliance with Ethical Standards
Ethical approval All procedures followed were in accordance with the ethical standards of the institutional review board (University of Washington IRB Committee J; IRB00005647; FWA #00006878) and with the 1964 Helsinki declaration and its later amendments. All survey participants gave their informed consent prior to their inclusion in the study.
References
- 1.Weiss E, Murphy G, Boden LI. Workers’ Compensation: Benefits, Costs, and Coverage (2017 data). Washington, D.C.: National Academy of Social Insurance; 2019. [Google Scholar]
- 2.MacEachen E, Kosny A, Ferrier S, Lippel K, Neilson C, Franche RL, et al. The 'ability' paradigm in vocational rehabilitation: Challenges in an Ontario injured worker retraining program. J Occup Rehabil. 2012;22(1): 105–117. [DOI] [PubMed] [Google Scholar]
- 3.Butler R, Johnson W, Baldwin M. Managing work disability: Why first return to work is not a measure of success. Industrial and Labor Relations Review. 1995;48(3):452–469. [Google Scholar]
- 4.Scott-Marshall HK, Tompa E, Wang Y, Liao Q. Long-term mortality risk in individuals with permanent work-related impairment. Can J Public Health. 2014;105(5):e330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casey R, Ballantyne PJ. Diagnosed chronic health conditions among injured workers with permanent impairments and the general population. J Occup Environ Med. 2017;59(5):486–496. [DOI] [PubMed] [Google Scholar]
- 6.Price J, Shi J, Lu B, Smith GA, Stallones L, Wheeler KK, et al. Nonoccupational and occupational injuries to US workers with disabilities. Am J Public Health. 2012;102(9):e38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young AE. Return to work following disabling occupational injury—facilitators of employment continuation. Scand J Work Environ Health. 2010;36(6):473–483. [DOI] [PubMed] [Google Scholar]
- 8.Organisation for Economic Co-operation and Development (OECD). Sickness, Disability and Work: Breaking the Barriers. A Synthesis of Findings across OECD Countries. Paris: OECD Publishing; 2010. [Google Scholar]
- 9.Kaye HS. Stuck at the bottom rung: Occupational characteristics of workers with disabilities. J Occup Rehabil. 2009;19(2): 115–128. [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Occupational Safety and Health. Morbidity and disability among workers 18 years and older in the Healthcare and Social Assistance sector, 1997–2007. DHHS (NIOSH) Publication No. 2012-161. October 2012; http://www.cdc.gov/niosh/docs/2012-161/pdfs/2012-161.pdf. Accessed April 30, 2017.
- 11.Bohle P, Pitts C, Quinlan M. Time to call it quits? The safety and health of older workers. Int J Health Serv. 2010;40(1):23–41. [DOI] [PubMed] [Google Scholar]
- 12.Scott KA, Liao Q, Fisher GG, Stallones L, DiGuiseppi C, Tompa E. Early labor force exit subsequent to permanently impairing occupational injury or illness among workers 50–64 years of age. Am J Ind Med. 2018;61(4):317–325. [DOI] [PubMed] [Google Scholar]
- 13.Zwerling C, Sprince NL, Davis CS, Whitten PS, Wallace RR, Heeringa SG. Occupational injuries among older workers with disabilities: A prospective cohort study of the Health and Retirement Survey, 1992 to 1994. Am J Public Health. 1998;88(11): 1691–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zwerling C, Sprince NL, Wallace RB, Davis CS, Whitten PS, Heeringa SG. Risk factors for occupational injuries among older workers: An analysis of the health and retirement study. Am J Public Health. 1996;86(9):1306–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zwerling C, Whitten PS, Davis CS, Sprince NL. Occupational injuries among older workers with visual, auditory, and other impairments. A validation study. J Occup Environ Med. 1998;40(8):720–723. [DOI] [PubMed] [Google Scholar]
- 16.Shi J, Gardner S, Wheeler KK, Thompson MC, Lu B, Stallones L, et al. Characteristics of nonfatal occupational injuries among U.S. workers with and without disabilities. Am J Ind Med. 2015;58(2): 168–177. [DOI] [PubMed] [Google Scholar]
- 17.Shi J, Wheeler KK, Lu B, Bishai DM, Stallones L, Xiang H. Medical expenditures associated with nonfatal occupational injuries among U.S. workers reporting persistent disabilities. Disabil Health J. 2015;8(3):397–406. [DOI] [PubMed] [Google Scholar]
- 18.Ruseckaite R, Collie A. Repeat workers' compensation claims: Risk factors, costs and work disability. BMC Public Health. 2011;11:492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruseckaite R, Collie A. The incidence and impact of recurrent workplace injury and disease: A cohort study of WorkSafe Victoria, Australia compensation claims. BMJ Open. 2013;3(3):e002396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keeney BJ, Turner JA, Fulton-Kehoe D, Wickizer TM, Chan KC, Franklin GM. Early predictors of occupational back reinjury: Results from a prospective study of workers in Washington State. Spine (Phila Pa 1976). 2013;38(2):178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lipscomb HJ, Cameron W, Silverstein B. Incident and recurrent back injuries among union carpenters. Occup Environ Med. 2008;65(12):827–834. [DOI] [PubMed] [Google Scholar]
- 22.Welch CE 3rd. Long-term risk of repeat occupational injury or illness incidents among Veterans Health Administration nursing employees. AAOHN J. 2010;58(8):323–329. [DOI] [PubMed] [Google Scholar]
- 23.Hergenrather K, Zeglin R, McGuire-Kuletz M, Rhodes S. Employment as a social determinant of health: A systematic review of longitudinal studies exploring the relationship between employment status and physical health. Rehabilitation Research, Policy, and Education. 2015;29(1):2–26. [Google Scholar]
- 24.State of Washington. RCW Title 51: Chapter 51.12. Employments and occupations covered.; http://apps.leg.wa.gov/rcw/default.aspx?Cite=51.12. Accessed July 29, 2019.
- 25.Franklin GM, Wickizer TM, Fulton-Kehoe D, Turner JA. Policy-relevant research: When does it matter? NeuroRx. 2004;1(3):356–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fishbain DA, Cutler RB, Rosomoff HL, Khalil T, Steele-Rosomoff R. Prediction of “intent”, “discrepancy with intent”, and “discrepancy with nonintent” for the patient with chronic pain to return to work after treatment at a pain facility. Clin J Pain. 1999;15(2):141–150. [DOI] [PubMed] [Google Scholar]
- 27.Kominski G, Pourat N, Roby D, Cameron M. Access to Medical Treatment in the California Workers’ Compensation System, 2006. Los Angeles, California: UCLA Center for Health Policy Research; 2006. [Google Scholar]
- 28.National Survey of Families and Households. Wave 3 Codebook Files. Madison, Wisconsin: Center for Demography, University of Wisconsin; 2005. [Google Scholar]
- 29.Ware J Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 30.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 31.Washington State Office of Financial Management. Washington State Population Survey. 2010; http://www.ofm.wa.gov/sps/. Accessed August 20, 2012.
- 32.Wickizer T Updated Report on the Outcome Evaluation for the Western Washington COHE (prepared for: Occupational Health Services Project, Washington State Department of Labor and Industries). 2007; Available at: http://www.lni.wa.gov/ClaimsIns/Files/Providers/ohs/UwReportRentonCohe.pdf. Accessed June 15, 2008.
- 33.Workers’ Compensation Board. Companion Document to Strengthening Vocational Rehabilitation: A Vocational Rehabilitation Program Review. Ontario, Canada; 1992. [Google Scholar]
- 34.Young AE. Employment maintenance and the factors that impact it after vocational rehabilitation and return to work. Disabil Rehabil. 2010;32(20): 1621–1632. [DOI] [PubMed] [Google Scholar]
- 35.Sears JM, Wickizer TM. Evaluation of the Vocational Rehabilitation Pilot Program. Report to the Washington State Legislature as required by ESSB 5920 (Chapter 72, Laws of 2007). Tumwater, WA: Washington State Department of Labor and Industries; 2012. [Google Scholar]
- 36.Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58(6):595–602. [DOI] [PubMed] [Google Scholar]
- 37.Marcum JL, McHugh A, Foley M, Adams D, Bonauto D. The economic effect of chronic comorbidities in carpal tunnel syndrome workers' compensation claimants, Washington State. JOccup Environ Med. 2018;60(12):1128–1135. [DOI] [PubMed] [Google Scholar]
- 38.The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th edition. Oakbrook Terrace, IL: AAPOR; 2016. [Google Scholar]
- 39.Washington State Department of Labor and Industries. Medical Examiners’ Handbook. Publication F252-001-000; 2019. [Google Scholar]
- 40.Washington State Department of Labor and Industries. Permanent Partial Disability. PPD Award Schedules. https://lni.wa.gov/claims/for-workers/claim-benefits/permanent-partial-disability. Accessed May 17, 2020.
- 41.American Medical Association. Guides to the Evaluation of Permanent Impairment. Fifth ed. Chicago, IL: AMA Press; 2017. [Google Scholar]
- 42.Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Health Statistics. Washington, DC: National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 43.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 44.Sears JM, Wickizer TM, Schulman BA. Improving vocational rehabilitation services for injured workers in Washington State. Evaluation and Program Planning. 2014;44:26–35. [DOI] [PubMed] [Google Scholar]
- 45.National Institute for Occupational Safety and Health. NIOSH Worker Health Charts: Health Status Charts, Behavioral Risk Factor Surveillance System (BRFSS), 2013-2015. https://wwwn.cdc.gov/NIOSH-WHC/chart/brfss-status/status?OU=_RFHLTH_r&T=A&V=R. Accessed November 7, 2019.
- 46.Ballantyne PJ, Casey R, O’Hagan FT, Vienneau P. Poverty status of worker compensation claimants with permanent impairments. Critical Public Health. 2016;26(2): 173–190. [Google Scholar]
- 47.Kaiser Family Foundation. Health Insurance Coverage of the Total Population, 2018. https://www.kff.org/other/state-indicator/total-population/. Accessed November 7, 2019.
- 48.Bureau of Labor Statistics (BLS). Union Membership (Annual) News Release, 2018. https://www.bls.gov/news.release/archives/union2_01182019.htm. Accessed November 7, 2019.


