Abstract
Objective:
To determine if the declining trend in US youth cigarette smoking changed after e-cigarettes were introduced, and if youth e-cigarette users would have been likely to smoke cigarettes based on psychosocial and demographic predictors of smoking.
Methods:
An interrupted time series analysis was used for cross-sectional data from the 2004 to 2018 National Youth Tobacco Surveys (NYTS) to assess changes in cigarette and e-cigarette use over time. A multivariable logistic regression model used 2004–2009 NYTS data on psychosocial risk factors to predict individual-level cigarette smoking risk from 2011–2018. Model-predicted and actual cigarette smoking behavior were compared.
Results:
The decline in current cigarette smoking slowed in 2014 (−.75 [95% CI: −.81, −.68] to −.26 [95% CI: −.40, .12] percentage points per year). The decline in ever cigarette smoking accelerated after 2012 (−1.45 [95% CI: 1.59, −1.31] to −1.71 [95% CI: −1.75, −1.66]). Ever and current combined cigarette and/or e-cigarette use declined during 2011–2013 and increased during 2013–2014 with no significant change during 2014–2018 for either variable. The psychosocial model estimated that 69.0% of current cigarette smokers and 9.3% of current e-cigarette users (who did not smoke cigarettes) would smoke cigarettes in 2018.
Conclusions:
The introduction of e-cigarettes was followed by a slowing decline in current cigarette smoking, a stall in combined cigarette and e-cigarette use, and an accelerated decline in ever cigarette smoking. Traditional psychosocial risk factors for cigarette smoking suggest that e-cigarette users do not fit the traditional risk profile of cigarette smokers.
INTRODUCTION
Since the introduction of e-cigarettes to the US market, use has increased rapidly among youth. Among US high school students, the prevalence of current (past 30-day) e-cigarette use significantly increased from 1.5% in 2011 to 20.8% in 2018, including a relative increase of 78% during 2017–2018 alone.1,2 Following this surge, the Food and Drug Administration (FDA) called for regulatory actions to prevent youth tobacco product initiation,3 and the US Surgeon General identified youth e-cigarette use as an epidemic.4
The US Surgeon General has concluded that e-cigarette aerosol is not harmless, and that youth use of any tobacco product, including in e-cigarettes, is unsafe.5 Most e-cigarettes contain nicotine, which is highly addictive, can harm the developing adolescent brain and prime the brain for addiction to other drugs.5 A meta-analysis of 16 longitudinal studies and 1 cross-sectional study from the US and elsewhere found strong evidence of an association between e-cigarette use in nonsmoking youth and young adults and later cigarette smoking (OR: 4.59, 95% CI 3.60–5.85).6
It has been suggested7 that the steady decline in US youth cigarette smoking observed since 19998 accelerated following the introduction of e-cigarettes, but evidence is mixed. Data from the 2004–2014 National Youth Tobacco Survey (NYTS) demonstrated that the rate of decline in cigarette smoking among youth did not change with the introduction of e-cigarettes.9 Furthermore, the study9 posited that youth who used e-cigarettes, but not cigarettes, did not share the same psychosocial characteristics10–14 as youth cigarette smokers. In contrast, using aggregate data from multiple nationally representative studies through 2017, Levy et al.15 concluded that, because e-cigarettes entered the market, the decline in current cigarette smoking prevalence of high school students accelerated by 2 to 4 times during 2014–2017.
Given the changes in youth e-cigarette use since 2011, including the substantial increase in use during 2017–2018,1 this paper updates the Dutra and Glantz9 analysis by adding 4 years of data (through 2018), and attempting to improve the psychosocial model. Specifically, this paper assesses: (1) whether the historical declining trend in cigarette smoking and combined use of cigarettes and/or e-cigarettes changed after the uptake of e-cigarettes by youth; and (2) whether the risk profile of youth e-cigarette users would match established demographic and psychosocial predictors of youth cigarette smoking.
METHODS
Sample
Data from the 2004 to 2018 (2004, 2006, 2009, and annually from 2011 to 2018) NYTS, a school-based, paper-and-pencil, cross-sectional survey of US middle and high school students, were used. Sample sizes ranged from 27,933 (2004) to 17,711 (2015) participants per year, and overall response rates ranged from 84.8% (2009) to 63.4% (2015). A stratified 3-stage cluster sampling procedure (counties, schools, and students within classes) was used to generate a nationally-representative sample of US public and private school students in 6th to 12th grade.16,17 All respondents present in each NYTS survey year were included in these analyses; analytic sample sizes for each analysis are presented in eTables 1, 2, and 3, and demographic and psychosocial characteristic distributions are in eTable 4.
Measures
Cigarette smoking
Ever smokers were those who responded “Yes” to the question “Have you ever tried cigarette smoking, even 1 or 2 puffs?” Participants who responded “No” were classified as never smokers.
Current smokers were those who reported using cigarettes on 1 or more of the past 30 days.
E-cigarette use
E-cigarettes were first included in the NYTS in 2011. Due to the rapidly morphing e-cigarette market, the e-cigarette questions and introductory preambles changed over time.16 During 2011–2013, participants were considered ever e-cigarette users if they replied, “Electronic Cigarettes or E-cigarettes” to the question “Which of the following tobacco products have you ever tried, even just one time?” Beginning in 2014, e-cigarettes were assessed as their own product class. Those who responded “Yes” to a question assessing ever use were classified as ever e-cigarette users.
For all years, participants were defined as current e-cigarette users if they reported using e-cigarettes on 1 or more of the past 30 days.
Combined cigarette and/or e-cigarette use
Combined ever or current use includes youth who were using cigarettes only (i.e., no e-cigarette use), e-cigarettes only (i.e., no cigarette smoking), or using both cigarettes and e-cigarettes (dual users).
Psychosocial and demographic predictors
Psychosocial variables included the questions, “If one of your best friends offered you a cigarette, would you smoke it?” and “Do you think you will smoke a cigarette at any time during the next year?” Both questions were modeled as continuous predictors (0=definitely not, 1=probably not, 2=probably yes, 3=definitely yes). The question, “Does anyone who lives with you now smoke cigarettes?” (1=yes, 0=no) was modeled as a dichotomous predictor. All variables were coded so higher values reflected a higher risk of cigarette smoking.
Sociodemographic variables (sex [reference female]; non-Hispanic Black, Hispanic, or non-Hispanic other race [reference non-Hispanic white]; and age [continuous variable]) and ever and current use of all other tobacco products (smokeless tobacco; cigars; pipes; or bidis) were included as covariates. Respondents who reported ever using 1 or more of these products were considered ever “other” tobacco users; those who reported using any of these other products on 1 or more of the past 30 days were considered current “other” tobacco users.
Analysis
Weighted prevalence estimates for ever and current use of cigarettes, e-cigarettes, and combined use were generated using SAS 9.4 (SAS Institute Inc., Cary, NC) We used the NYTS weights to account for differential probabilities of selection, nonresponse, and match sample characteristics to national estimates.17
Interrupted time series analysis
We estimated and tested models of ever and current youth cigarette smoking prevalence and combined use over time using the SAS AUTOREG procedure. The model simulates an interrupted time series by specifying an offset (i.e., change in prevalence at the “break” year) and measuring the slope change at the specified “break” year while enabling us to specify 2 autoregressive terms to account for correlated residuals. To determine the breakpoint for each outcome, the models specified each year between 2011 and 2015 as the potential break year; the final break year was chosen to minimize the Akaike Information Criterion corrected (AICc), a version of the AIC that accommodates small sample sizes.18 We also conducted a second interrupted time series analysis of ever and current use of one or more tobacco products using all products captured by the NYTS (eTable 5).
Psychosocial model to predict cigarette smoking
A psychosocial model of cigarette smoking was used to estimate the probability of cigarette smoking among e-cigarette users but not cigarette smokers, never users of either product, and cigarette smokers during 2011–2018 based on the predictors of cigarette smoking in the 2004–2009 NYTS, before e-cigarettes achieved widespread use among youth.
Two models were tested using multivariable logistic regression, the original model proposed by Dutra and Glantz9 and a model that attempted to improve upon the original. The updated model included demographic variables, use of other tobacco products, and a three-item construct of cigarette smoking susceptibility (students who responded with an answer other than “definitely not” to any of the following three questions were coded as “cigarette smoking susceptible”: “Do you think you will smoke a cigarette at anytime during the next year?,” “If one of your best friends offered you a cigarette, would you smoke it?,” and “Do you think that you will try a cigarette soon?”). As detailed in eTable 6, this model did not improve upon the fit of the original model; fit was measured by percent concordance (a measure of the association of predicted probabilities and observed responses). As a result, the final model used in the current study included all psychosocial and demographic variables from the Dutra and Glantz model that were available for all years of data (2004–2018).
As detailed in the supplementary materials (eTable 7 and eTable 8), interactions between time and psychosocial predictor variables were tested to assess potential changes in the effects of these predictor variables across time. These interaction terms did not substantially improve the predictive ability of the model and thus, were not included in the final models.
The logistic regression equations from the psychosocial models were applied to the 2011–2018 data to predict respondents’ odds of ever or current smoking (log-odds >0 classified as probable smokers, log-odds <0 classified as probable nonsmokers, and log odds =0 set to missing). Model-estimated smoking status was compared to self-reported ever and current cigarette and e-cigarette use.
RESULTS
Cigarette and e-cigarette use over time
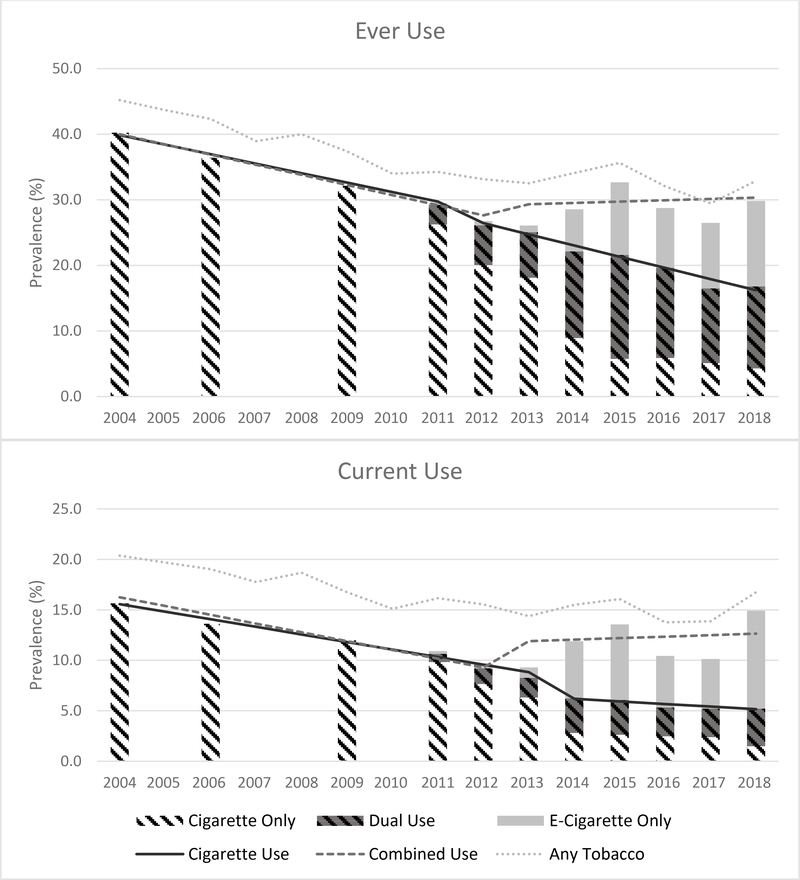
Ever cigarette smoking decreased from 40.2% in 2004 to 17.1% in 2018, while ever e-cigarette use increased from 3.3% in 2011 to 25.7% in 2018 (Figure 1). Ever combined use was 30.7% in 2011 and 30.6% in 2018.
Figure 1: Prevalence of Cigarette, E-cigarette, and Use of Cigarettes and/or E-cigarettes, US Middle School and High School Students, 2004–2018 NYTS.
Solid and dotted lines are fit from the autoregressive interrupted time series analysis. These lines are predicted values
Current cigarette smoking decreased from 15.6% in 2004 to 5.4% in 2018, while current e-cigarette use increased from 1.1% in 2011 to 13.4% in 2018. Current combined use was 11.7% in 2011 and 15.6% in 2018.
Rate of change in cigarette, e-cigarette and combined use after the introduction of e-cigarettes
Ever cigarette smoking showed a continuous decline during 2004–2018. The breakpoint for ever cigarette smoking occurred in 2012. Before 2012, ever cigarette smoking was declining at a rate of 1.45 percentage points per year (95% CI: −1.59, −1.31). In 2012, prevalence of ever cigarette smoking dropped 1.83 percentage points (95% CI: −2.52, −1.14), and after 2012, prevalence declined at a rate of 1.71 percentage points per year (95% CI: −1.75, −1.66), indicating that the decline in ever cigarette smoking was decreasing faster (−.26 [95% CI: −.39, −.12]) after the breakpoint in 2012 (Table 1).
Table 1—
Time Series Analysis of Trends in Cigarette and Combined Use of Cigarettes and/or E-Cigarettes, US Middle School and High School Students, National Youth Tobacco Survey, 2004–2018
| Time Series Analysis | Ever Cigarette Smoking a | Current Cigarette Smoking b | Combined Ever use of cigarettes and/or e- cigarettes c | Combined Current use of cigarettes and/or e- cigarettes d |
|---|---|---|---|---|
| Year of break (breakpoint) | 2012 | 2014 | 2013 | 2013 |
| b (SE), 95% CI | b (SE), 95% CI | b (SE), 95% CI | b (SE), 95% CI | |
| Slope pre-break, percentage points per yeare | −1.45 (.07), (−1.59, −1.31) | −.75 (.03), (−.81, −.68) | −1.55 (.14), (−1.82, −1.27) | −.87 (.09), (−1.04, −.70) |
| Slope post-break f | −1.71 (.02), (−1.75, −1.66) | −.26 (.07), (−.40, −.12) | .20 (.23), (−.24, .65) | .15 (.08), (.00, .30) |
| Slope change g | −.26 (.07), (−.39, −.12) | .49 (.07), (.35, .63) | 1.75 (.24), (.97, 5.52) | 1.02 (.09), (.84, 1.20) |
| Offset h | −1.83 (.30), (−2.52, −1.14) | −1.89 (.20), (−2.36, −1.41) | 3.24 (1.16), (1.29, 2.21) | 3.48 (.55), (2.40, 4.55) |
Ever smoking was defined as ≥1 puff of a cigarette, includes dual use of e-cigarettes after 2011
Current smoking was defined as smoking cigarettes in the past 30 days, includes dual use of e-cigarettes after 2011
Ever use of cigarettes, e-cigarettes or both (dual use)
Current use of cigarettes e-cigarettes or both (dual use)
Slope of the trend before the identified breakpoint
Slope of the trend line after the identified breakpoint
Slope change is the slope post-break minus slope pre-break
Change in prevalence (post minus pre) at the breakpoint
Additionally, there was a continuous decline in current cigarette smoking since 2004, with the breakpoint for current cigarette smoking occurring in 2014. Before 2014, the prevalence of current cigarette smoking was declining at a rate of .75 percentage points per year (95% CI: −.81, −.68). In 2014, the prevalence dropped 1.89 percentage points (95% CI: −2.36, −1.41); the rate of decline then slowed significantly (.49 [.35, .63]) to .26 percentage points per year (95% CI: −.40, −.12).
The breakpoint for ever combined use occurred in 2013. Before 2013, ever combined use declined at a rate of 1.55 percentage points per year (95% CI: −1.82, −1.27), but at the breakpoint the prevalence of ever combined use increased 3.24 percentage points (95% CI: 1.29, 2.21). After 2013, the previous decline stalled, with no significant change in the prevalence of ever combined use observed over time (1.75 percentage points per year [95% CI: .97, 5.52]).
Similarly, for current combined use, the breakpoint occurred in 2013. Before 2013, current combined use was declining at a rate of .87 percentage points per year (95% CI: −1.04, −.70). At the breakpoint, the prevalence increased 3.48 percentage points (95% CI: 2.40, 4.55). After 2013, there was no significant shift in the rate of change (1.02 [95% CI: .84, 1.20), indicating that the previous decline in current combined use had stalled.
As detailed in eTable 5, a separate analysis was conducted that accounted for all tobacco products available in the NYTS 2004–2018. Similar to the combined use analyses, the break point for ever and current any tobacco product use occurred in 2013. After 2013 there was a slowing of the decline observed for ever any tobacco use, but for current any use there was no significant shift in the rate of change indicating that the decline in current any use had stalled before the breakpoint.
Psychosocial predictive model
During 2004–2009, the following characteristics were significantly associated with higher odds of ever and current cigarette smoking (Table 2): being male, older age, living with a smoker, likelihood of smoking a cigarette in the next year, likelihood of accepting a cigarette from a friend, and other tobacco product use. Hispanic or non-Hispanic Black youth had significantly higher odds of ever smoking, but not current smoking.
Table 2—
Predictors of Cigarette Smoking Produced by a Psychosocial Model Based on Pooled Data for Predictors of Cigarette Smoking Between 2004 and 2009, US Middle School and High School Students, National Youth Tobacco Survey
| Predictor | Outcome a | |||
|---|---|---|---|---|
| Ever Smoking b | Current Smoking c | |||
| Unadjusted OR (95% CI) | AOR (95% CI) | Unadjusted OR (95% CI) | AOR (95% CI) | |
| Male | .91 (.88-.95) | 1.30 (1.22–1.39) | .90 (.85-.96) | 1.27 (1.14–1.42) |
| Race/Ethnicity | ||||
| Non-Hispanic White | Ref | Ref | ||
| Hispanic | 1.25 (1.12–1.39) | 1.53 (1.40–1.68) | 1.00 (.88–1.14) | .97 (.84–1.12) |
| Non-Hispanic black | .96 (.84–1.10) | 1.75 (1.51–2.02) | .49 (.42-.56) | .95 (.77–1.17) |
| Non-Hispanic other | .70 (.62-.79) | .98 (.84–1.13) | .72 (.61-.85) | 1.04 (.81–1.33) |
| Age (years) | 1.43 (1.40–1.46) | 1.36 (1.33–1.39) | 1.43 (1.40–1.46) | 1.34 (1.30–1.38) |
| Live with a smoker | 2.64 (2.48–2.82) | 2.45 (2.28–2.63) | 2.81 (2.60–3.04) | 2.01 (1.82–2.22) |
| Intend to smoke in next year | 4.86 (4.67–5.06) | 1.90 (1.80–2.01) | 8.40 (7.78–9.07) | 3.05 (2.75–3.39) |
| Likely to smoke a cigarette from a friend | 5.43 (5.21–5.66) | 2.42 (2.27–2.57) | 9.04 (8.54–9.57) | 3.16 (2.93–3.41) |
| Other tobacco use d | 18.68 (17.4919.96) | 7.27 (6.78–7.80) | 19.96 (18.45–21.59) | 4.37 (3.92–4.87) |
| Year (centered on 2009) | .93 (.90–.96) | .92 (.89–.94) | .94 (.91–.97) | .93 (.90–.95) |
| Concordance % | 89.2 | 95.5 | ||
Abbreviations: Adjusted odds ratio (AOR), 95% Confidence Interval (95% CI).
All models include NYTS-provided weights, stratification, design variables, male, race/ethnicity, age, living with a smoker, intention to smoke in the next year, likelihood to smoke a cigarette when offered from a friend, other tobacco use, and year (centered on 2009).
Ever smoking was defined as ≥1 puff of a cigarette
Current smoking was defined as smoking cigarettes in the past 30 days
Other tobacco product defined as use of products other than cigarettes or e-cigarettes that are consistent across survey years (2004–2018): chewing tobacco, snuff, or dip; cigars, cigarillos, or little cigars; tobacco in a pipe; or bidis
By year, the percentage of the psychosocial model predicted between 73.7% (2018) and 87.4% (2011) of individuals who reported ever smoking cigarettes to be ever smokers (Table 3). The psychosocial model predicted between 8.7% (2018) and 32.4% (2011) of self-reported never users of e-cigarettes or cigarettes to be ever cigarette smokers. Between 35.9% (2018) and 64.2% (2012) of youth who reported ever using e-cigarettes but not cigarettes were predicted to be ever cigarette smokers from the psychosocial model (Table 3).
Table 3:
Psychosocial model prediction of cigarette smoking status, by actual cigarette or e-cigarette use status, US Middle School and High School Students, National Youth Tobacco Survey, 2004–2018
| Predicted Cigarette Smoking Statusab | ||||||||
| Ever Smokerc | ||||||||
| Actual Participant Smoking Status | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Actual ever smoker d | 87.4 (85.7, 89.1) | 85.0 (83.5, 86.5) | 82.5 (80.7, 84.4) | 80.3 (78.3, 82.4) | 78.1 (75.4, 80.9) | 75.3 (73.4, 77.2) | 75.9 (73.3, 78.5) | 73.7 (71.6, 75.8) |
| Actual never smoker/ never e-cigarette user e | 32.4 (29.0, 35.8) | 21.7 (20.2, 23.3) | 19.2 (17.7, 20.7) | 14.9 (13.4, 16.5) | 11.4 (9.8, 13.0) | 10.4 (9.3, 11.5) | 10.2 (9.1, 11.4) | 8.7 (7.8, 9.6) |
| Actual ever e-cigarette only user f | -- | 64.2 (54.5, 74.0) | 66.7 (53.4, 79.9) | 52.1 (13.4, 16.5) | 43.7 (40.3, 47.2) | 40.8 (37.7, 43.9) | 41.4 (38.2, 44.6) | 35.9 (32.9, 38.8) |
| Current Smokerg | ||||||||
| Actual Participant Smoking Status | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Actual current smoker h | 85.2 (82.2, 88.2) | 81.0 (79.0, 83.0) | 78.7 (75.9, 81.5) | 76.8 (72.9, 80.7) | 74.0 (70.4, 77.6) | 77.6 (74.4, 80.7) | 73.0 (69.6, 76.5) | 69.0 (65.4, 72.6) |
| Actual noncurrent smoker/ noncurrent e-cigarette user i | 3.5 (2.8, 4.3) | 2.5 (2.2, 2.9) | 4.4 (3.7, 5.0) | 1.4 (1.1, 1.7) | .9 (.7, 1.2) | 1.1 (.9, 1.4) | 1.2 (1.0, 1.5) | .8 (.7, 1.0) |
| Actual current e-cigarette only user j | -- | 15.7 (7.4, 24.0) | 26.3 (16.2, 36.4) | 11.1 (9.0, 13.3) | 7.9 (5.9, 9.9) | 11.5 (8.2, 14.9) | 10.7 (8.0, 13.4) | 9.3 (7.5, 11.0) |
Data are presented as percentages (95% CIs). All analyses adjusted for NYTS-provided weights, stratification, and design variables.
Estimated likelihood of smoking cigarettes based on a psychosocial model of smoking created by using 2004–2009 NYTS data on sex, race/ethnicity, age, living with a smoker, intention to smoke cigarettes in the next year, likelihood of smoking a cigarette offered by a friend, other tobacco product use (besides cigarettes and e- cigarettes), and time (centered on 2009).
Model-estimated likelihood of ever taking a puff of a cigarette.
Reported taking ≥1 puff of a cigarette in lifetime, including dual users of cigarettes and e-cigarettes.
Reported never taking a puff of a cigarette or e-cigarette.
Endorsed having ever taken ≥1 puff of an e-cigarette but not smoking ≥1 puff of a cigarette.
Model-estimated likelihood of having smoked cigarettes in the past 30 days.
Reported smoking cigarettes in the past 30 days, includes dual users of cigarettes and e-cigarettes.
Did not report smoking cigarettes or using an e-cigarette in the past 30 days.
Reported using an e-cigarette in the past 30 days but not smoking cigarettes in the past 30 days.
-- indicates an unstable estimate either due to an RSE >.3 or unweighted denominator < 50
For youth who reported current cigarette smoking, the model predicted between 69.0% (2018) and 85.2% (2011) of youth to be current cigarette smokers. The proportion of youth who reported no current use of cigarettes or e-cigarettes predicted to be current smokers ranged between .8% (2018) and 4.4% (2013). For youth who reported current e-cigarette use but no current cigarette smoking, the model predicted between 7.9% (2015) and 26.3% (2013) to be current cigarette smokers (Table 3).
DISCUSSION
The introduction of e-cigarettes was followed by a faster decline in ever use of cigarettes, but a slower decline in current cigarette smoking. Current use of cigarettes and/or e-cigarettes in 2018 (15.6%) equaled the prevalence of current cigarette smoking alone in 2004 (15.6%). In addition, the psychosocial risk profile of individuals using only e-cigarettes differed from individuals smoking cigarettes, indicating that it was unlikely that these youth would have smoked cigarettes.
This study provides updated data and methods to the previous Dutra and Glantz9 study that only included NYTS data up to 2014, when e-cigarettes surpassed all other tobacco products as the most commonly used tobacco product among US youth.1 Dutra and Glantz9 did not observe any changes in the declining trend in cigarette smoking after the introduction of e-cigarettes. However, the current analyses indicated that 2014 was the breakpoint for current cigarette smoking, resulting in a slower decline in current cigarette smoking after 2014 among US youth. The additional 4 years of data show that use of cigarettes and/or e-cigarettes had stalled, while the decline of ever cigarette smoking accelerated following the introduction of e-cigarettes.
The accelerating decline in ever smoking could, in part, reflect youth beginning tobacco product experimentation with e-cigarettes rather than cigarettes. However, as is the case with previous declines in cigarette smoking, research suggests that these declines are likely due to comprehensive and sustained tobacco control strategies and policies enacted over the last several decades, such as raising the minimum purchasing age; comprehensive smoke-free air laws; fully-funded state-tobacco control programs; and targeted mass-media campaigns aimed at educating the public about the harms of tobacco product use.5,19 These efforts, combined with FDA regulation of tobacco products, can continue to have positive and significant effects on youths tobacco product use.
The slowed decline in current cigarette smoking suggests that e-cigarettes are not acting as a substitute for conventional cigarettes among US youth. E-cigarette products have characteristics that attract youth, and low-risk youth who begin nicotine use with e-cigarettes may be more likely to transition to cigarette smoking than those who never use e-cigarettes.6 Our data show that, rather than participating in product switching, youth nicotine exposure from cigarettes and/or e-cigarettes may have increased following the introduction of e-cigarettes due to the increased prevalence of combined use since 2011.
Ever cigarette smoking shifted in 2012, and current cigarette smoking shifted in 2014. Previous analyses have shown that it can take up to 1 year for changes in the tobacco marketplace and policies to have an effect on behavior.20,21 As a result, events in 2011 and 2013 may have influenced the trends observed in 2012 and 2014. In 2011, the first evidence exists for the use of e-cigarettes in the US among youth; this is one possible explanation for the shift in cigarette smoking.6 Later shifts in current cigarette smoking may reflect increased prevalence of e-cigarette use in 2013.5,22,23 Additionally, modifications to the wording of the e-cigarette questionnaire items may partly explain the changes in trends, including the introduction of an e-cigarette-specific module on the NYTS beginning in 2014. We were unable to identify any e-cigarette specific policy changes between 2011 and 2014 that could account for these changes.23,24
Two studies have examined the relationship between e-cigarette availability and cigarette smoking among youth, concluding that e-cigarettes were contributing to the decline in cigarette smoking among youth.25,26 One of these studies examined a similar research question using several nationally representative surveys and concluded that the prevalence of current smoking in youth decreased faster after e-cigarettes were introduced.15 There are several differences between that study and the current analysis. Levy et al.15 used data through 2017, whereas the current study analyzed trends through 2018. Importantly, the current study included data from before the prevalence of e-cigarettes surpassed cigarette smoking, whereas Levy et al.15 only included e-cigarette data starting in 2014, when the Monitoring the Future survey began assessing e-cigarettes. Thus, the trends reported in the Levy et al.15 study may have already been influenced by youths’ e-cigarette use. Furthermore, the inclusion of the 2018 data point in the current study is particularly important; a slight decline of e-cigarette use occurred during 2015–2017, before the substantial increase in youth e-cigarette use during 2017–2018.1 In addition, the current study tested multiple breakpoint years to objectively determine when trends changed, and also accounted for autocorrelation in the time series analysis, while Levy et al.15 did not.
The psychosocial model based on data during 2004–2009 reasonably predicted current cigarette smoking and demonstrated that e-cigarette users who did not smoke cigarettes did not share the same psychosocial risk profile as current cigarette smokers. These findings are consistent with prior literature indicating that e-cigarette only users differ in psychosocial and demographic characteristics from cigarette smokers9,10,27,28 Together, these findings may suggest that most current e-cigarette users may have been unlikely to have smoked cigarettes. However, due to the cross-sectional nature of NYTS data, this hypothesis cannot be fully tested using this data source. Alternatively, these findings may demonstrate that e-cigarette users do not display the same characteristics as cigarette smokers and therefore, traditional predictors of cigarette smoking may not work well for predicting e-cigarette use. A divergence of the characteristics of cigarette and e-cigarette users over time, particularly as the e-cigarette marketplace evolved,5 could explain the decreasing efficacy of the psychosocial model in predicting cigarette smoking. However, the decreasing efficacy of the model is also likely to be due to the use of characteristics observed in a given year to attempt to predict behavior in later years.
Given the prominent use of e-cigarettes by youth and slowing decline in youth cigarette smoking and all tobacco product use, continued efforts are warranted to prevent the initiation of all tobacco products, including e-cigarettes, among youth. Additionally, it is important to note that, while this analysis concentrated on e-cigarettes and cigarettes, youth may also initiate tobacco use with other tobacco products (hookah, non-cigarette combustible tobacco, or smokeless tobacco), and are also at increased risk of becoming dual and polytobacco users.29 However, in 2018, the most common combination of products among both middle (14.4%) and high school (14.8%) tobacco users was e-cigarettes and cigarettes.1 Youth use of tobacco products should be prevented given the harmful effects of nicotine on the developing brain. Evidence-based and population-based strategies to reduce youth tobacco use include restricting young peoples’ access to tobacco products in retail settings, implementing comprehensive smokefree indoor air policies that include e-cigarettes, licensing retailers, implementing price policies, and developing educational initiatives targeting young people.19 The Surgeon General also suggests implementing strategies to curb e-cigarette marketing that appeals to young people, and to reduce access to flavored tobacco products.30,36 Educational efforts should inform youth, parents, healthcare professionals, and policy makers of the risks of all tobacco product use, including e-cigarettes, among youth.4
Limitations
These data are cross-sectional; thus, changes in individual behaviors over time (e.g., switching from cigarettes to e-cigarettes) cannot be assessed. Some of the NYTS survey items changed over time; therefore, some of the psychosocial characteristics previously identified9 to create the psychosocial model could not be included in the present analysis. We were limited in the variables included to those asked in all years of NYTS, which did not include any general risk-taking measures. We used data from 2004–2009 to estimate the parameters in the psychosocial model, then used this model to estimate the likelihood of cigarette smoking among youth sampled from 2011–2018. The approach assumes that the predictors of smoking remain constant over the whole 2004–2018 time period. In addition, the time-series analyses did not account for demographic characteristic changes over time, yet all analyses utilized the weighting procedures to ensure these accounted for complex survey procedures and were nationally representative. NYTS findings are subject to self-report bias, and the NYTS is a school-based survey; findings may not generalize to youth not enrolled in school and those in alternative education settings.
Conclusions
The introduction of e-cigarettes was followed by changes in the trends in youth cigarette smoking, including a slowing of the decline in current cigarette smoking and an acceleration in the ever cigarette smoking trend. Most youth who use e-cigarettes but not cigarettes may have been at low risk of smoking cigarettes had e-cigarettes not been available. Together, these findings indicate that youths’ exposure to nicotine is expanding through the use of new products, thereby contributing to nicotine dependence among youth.
Supplementary Material
Acknowledgments
Funding and Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Dr. Delucchi’s work was supported by grant U54HL147127 from the National Heart, Lung, and Blood Institute, and from the Food and Drug Administration (FDA) Center for Tobacco Products. Dr. Glantz’s work was supported by grants R01DA043950 from the National Institute of Drug Abuse, U54HL147127 from the National Heart, Lung, and Blood Institute, and from the Food and Drug Administration (FDA) Center for Tobacco Products. Dr. Dutra’s work was funded by a contract between RTI International and the CDC’s Office of Smoking and Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH or FDA. The funding agencies played no role in study design, collection, analysis, and interpretation of data, writing the report, or the decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Gentzke AS, Creamer M, Cullen KA, et al. Vital Signs: Tobacco product use among middle and high school students—United States, 2011–2018. MMWR: Morbidity and Mortality Weekly Report. 2019;68(6):157. doi: 10.15585/mmwr.mm6806el. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: Use of electronic cigarettes and any tobacco product among middle and high school students—United States, 2011–2018. MMWR: Morbidity and Mortality Weekly Report. 2018;67(45):1276. doi: 10.15585/mmwr.mm6745a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.FDA. Statement from FDA Commissioner Scott Gottlieb, M.D., on proposed new steps to protect youth by preventing access to flavored tobacco products and banning menthol in cigarettes. https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottliebmd-proposed-new-steps-protect-youth-preventing-access Published 2018. Accessed 16 May 2019.
- 4.U.S. Department of Health and Human Services. Surgeon General releases advisory on e-cigarette epidemic among youth, https://www.hhs.gov/about/news/2018/12/18/surgeon-general-releasesadvisory-e-cigarette-epidemic-among-youth.html Published 2018. Updated December 18, 2018. Accessed 16 May 2019.
- 5.U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion;2016. [Google Scholar]
- 6.Khouja JN, Suddell SF, Peters SE, Taylor AE, Munafo MR. Is e-cigarette use in non-smoking young adults associated with later smoking? A systematic review and meta-analysis. Tob Control. 2020. doi: 10.1136/tobaccocontrol-2019-055433. [DOI] [PMC free article] [PubMed]
- 7.Levy DT, Borland R, Villanti AC, et al. The application of a decision-theoretic model to estimate the public health impact of vaporized nicotine product initiation in the United States. Nicotine & Tobacco Research. 2017;19(2):149–159. doi: 10.1093/ntr/ntwl58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Creamer MR, Perry CL, Harrell MB, Diamond PM. Trends in multiple tobacco product use among high school students. Tobacco regulatory science. 2015;1(3):204–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dutra LM, Glantz SA. E-cigarettes and national adolescent cigarette use:2004–2014. Pediatrics. 2017;139(2):e20162450. doi: 10.1542/peds.2016-2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrington-Trimis JL, Berhane K, Unger JB, et al. Psychosocial factors associated with adolescent electronic cigarette and cigarette use. Pediatrics. 2015;136(2):308–317. doi: 10.1542/peds.2015-0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine & Tobacco Research. 2015;17(2):228–235. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coleman BN, Apelberg BJ, Ambrose BK, et al. Association between electronic cigarette use and openness to cigarette smoking among US young adults. Nicotine & Tobacco Research. 2015;17(2):212–218. doi: 10.1093/ntr/ntu211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moore GF, Littlecott HJ, Moore L, Ahmed N, Holliday J. E-cigarette use and intentions to smoke among 10–11-year-old never-smokers in Wales. Tobacco control. 2016;25(2):147–152. doi: 10.1136/tobaccocontrol-2014-052011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135(1):e43–e51. doi: 10.1542/peds.2014-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levy DT, Warner KE, Cummings KM, et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tobacco Control. 2018:tobaccocontrol-2018–054446. doi: 10.1136/tobaccocontrol-2018-054446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. National Youth Tobacco Survey(NYTS). Smoking & Tobacco Use Web site. https://www.cdc.gov/tobacco/data_statistics/surveys/nyts/ Published 2019. Updated 28 February 2019. Accessed 27 Mar 2019.
- 17.Centers for Disease Control and Prevention. Historical NYTS Data and Documentation. https://www.cdc.gov/tobacco/data_statistics/surveys/nyts/data/index.html Published 2019. Accessed 16 May 2019.
- 18.Burnham K, Anderson D. Model selection and multi-model inference: A practical information-theoretic approach 2nd ed. New York: Springer; 1994. [Google Scholar]
- 19.U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health;2012. [Google Scholar]
- 20.Song AV, Dutra LM, Neilands TB, Glantz SA. Association of smoke-free laws with lower percentages of new and current smokers among adolescents and young adults: an 11-year longitudinal study. JAMA pediatrics. 2015;169(9):e152285–e152285. doi: 10.1001/jamapediatrics.2015.2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dutra LM, Glantz SA, Arrazola RA, King BA. Impact of e-cigarette minimum legal sale age laws on current cigarette smoking. Journal of Adolescent Health. 2018;62(5):532–538. doi: 10.1016/j.jadohealth.2017.11.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arrazola RA, Neff LJ, Kennedy SM, et al. Tobacco use among middle and high school students--United States, 2013. MMWR - Morbidity & Mortality Weekly Report. 2014;63(45):1021–1026. [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services. The Health Consequences of Smoking--50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health;2014. [Google Scholar]
- 24.Enforcement Priorities for Electronic Nicotine Delivery Systems(ENDS) and Other Deemed Products on the Market Without Premarket Authorization (Revised)*. In: U.S. Department of Health and Human Services Food and Drug Administration Center for Tobacco Products; 2020.
- 25.Friedman AS. How does electronic cigarette access affect adolescent smoking? Journal of Health Economics. 2015;44:300–308. doi: 10.1016/j.jhealeco.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Pesko MF, Hughes JM, Faisal FS. The influence of electronic cigarette age purchasing restrictions on adolescent tobacco and marijuana use. Preventive Medicine. 2016;87:207–212. doi: 10.1016/j.ypmed.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 27.Wills TA, Sargent JD, Knight R, Pagano I, Gibbons FX. E-cigarette use and willingness to smoke: A sample of adolescent non-smokers. Tobacco Control. 2015;25(e1):e52–e59. doi: 10.1136/tobaccocontrol-2015-052349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berry KM, Fetterman JL, Benjamin EJ, et al. Association of electronic cigarette use with subsequent initiation of tobacco cigarettes in US youths. JAMA Network Open. 2019;2(2):e187794–e187794. doi: 10.1001/jamanetworkopen.2018.7794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Watkins SL, Glantz SA, Chaffee BW. Association of Noncigarette Tobacco Product Use With Future Cigarette Smoking Among Youth in the Population Assessment of Tobacco and Health (PATH) Study, 2013–2015. JAMA Pediatrics. 2018;172(2):181–187. doi: 10.1001/jamapediatrics.2017.4173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang YT, Glantz S. San Francisco voters end the sale of flavored tobacco products despite strong industry opposition. Ann Intern Med. 2018;169(10):708–709. doi: 10.7326/m18-2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.