Abstract
Purpose:
To provide radiologic-pathologic correlation of brain injury in the Papez circuit in hypoxic-ischemic encephalopathy (HIE) neonates, and correlate radiologic findings with long-term neurodevelopmental outcomes.
Methods:
Twenty full-term HIE neonates were evaluated. Cerebral blood flow (CBF) values, obtained through pulsed arterial spin labeling (ASL) perfusion-weighted MRI, were compared by permutation test to identify brain regions with statistically significant perfusion changes between 14 HIE neonates without evidence of developmental delay by Bayley-III(mean age 8.2±7.2 days) and 6 HIE neonates with evidence of developmental delay(mean age 13.1±8.0 days). Four histopathologic studies on specimens were taken from post-mortem brains of another group of infants(mean age 10±6.8 days) with HIE. The infants were not the same ones who had MRIs.
Results:
Significantly decreased perfusion in Papez circuit was found in HIE neonates with developmental delay compared with HIE neonates without delay. Decreased ASL perfusion values were seen in Papez circuit structures of the fornix (p=0.002), entorhinal cortex(p=0.048), amygdala(p=0.036), hippocampus(p=0.033), and thalamus(p=0.036). In autopsy specimens of neonates with HIE, anoxic (eosinophilic) neurons, reactive astrocytes, and white matter rarefaction were observed in these regions, providing pathology correlation to the imaging findings of HIE.
Conclusion:
The Papez circuit is susceptible to hypoxic-ischemic injury in neonates as demonstrated by perfusion-weighted imaging and histopathology. This sheds new light onto a possible non-familial mechanism of neuropsychiatric disease evolution initiated in the infant period and raises the potential for early identification of at-risk children.
Keywords: hypoxic-ischemic encephalopathy, pulsed arterial spin labeling, cerebral blood flow, neonates, Papez circuit, pathology
Introduction
The Papez circuit is a complex neural circuit comprising brain structures that are now categorized as part of the limbic system[1, 2]. Its multitude of connections have been demonstrated by fiber dissection techniques on cadaveric brain specimens[3] and invivo magnetic resonance imaging techniques of diffusion tensor tractography[4], and super-resolution track density imaging[5]. The circuit includes fibers extending from the hippocampus into the fornix to the mamillary bodies, the mammillothalamic tract connecting the mammillary bodies and anterior thalamus, and the anterior thalamic radiations linking the anterior thalamus to the cingulum. The cingulum connects to the entorhinal cortex, which communicates with the hippocampus, thus completing the Papez circuit[3]. The various brain structures and neural tracts that constitute this circuit are generally located lateral to the thalamus, deep to the cerebral cortex, and superior to the brainstem[6]. MacLean integrated the amygdala and other structures ascribed to the Papez circuit in his conception of the limbic system[7]. The circuit receives inputs from diverse areas of the neuraxis and participates in complex behaviors, such as emotion, memory, and social interaction[8].
A few studies have reported radiologic evidence of Papez circuit injury in adult patients with memory impairments. Using diffusion tensor tractography, neural injury of the Papez circuit was demonstrated in a patient with memory impairment following hypoxic-ischemic brain injury[9]. Patients with traumatic brain injury and memory impairment can injury of Papez circuit structures[10]. Furthermore, cognitive dysfunction after cerebral ischemia secondary to ischemic stroke or cardiac arrest can also be associated with damage to neural networks in the Papez circuit[11]. In comparison, there is paucity of literature investigating the effects of neonatal hypoxic-ischemic encephalopathy (HIE) on the Papez circuit and its implications on long-term neurodevelopmental outcomes.
The study of Papez circuit injury following neonatal HIE may shed new light onto an important non-familial mechanism of neuropsychiatric disease evolution initiated in the infant period. Specifically, birth asphyxia is a neonatal factor associated with autism spectrum disorder (ASD)[12]. Recent studies have demonstrated a high proportion of children with moderate or severe neonatal encephalopathy who develop an ASD[13]. Besides ASD, studies on humans and animals have demonstrated that hypoxic-ischemic fetal and neonatal complications are associated with a high risk of developing schizophrenia[14], and mood disorders[15]. Pre- and perinatal hypoxia is also associated with decreased volumes of the hippocampus and amygdala in bipolar disorder[16].
Here, we examine injury to the Papez circuit in neonates with a clinical diagnosis of HIE using both pulsed arterial spin labeled (PASL) perfusion-weighed imaging and pathology specimens. We hypothesized that the Papez circuit is susceptible to hypoxic-ischemic injury in neonatal patients with both radiologic and pathologic evidence of brain injury. In addition, we hypothesized that there would be perfusion alterations in imaging from patients with developmental delay defined by the Bayley-III scoring system.
Methods
Participants and Pathology
Twenty term neonates were identified for a retrospective case-control study following an IRB-approved protocol. A waiver of consent/parental permission, assent and HIPAA authorization has been approved by our institutional review board. Of these patients, there were 14 HIE neonates without evidence of developmental delay on Bayley-III (Group A, 8/6 males/females, mean age 8.2±7.2 days, 12 neonates underwent hypothermia, 13 neonates have normal conventional MRI of T1, T2 and DWI images), defined as “good” outcomes, and 6 HIE neonates with developmental delay by Bayley-III scores (Group B, 4/2 males/females, mean age 13.1±8.0 days, 5 neonates underwent hypothermia, 4 neonates have normal conventional MRI of T1, T2 and DWI images), defined as “poor” outcomes. Linear regression was performed to eliminate the effect of age and gender on the PASL data. Developmental assessments were performed using the Bayley Scales of Infant and Toddler Development, 3rd Edition[17], which provides cognitive, language, and motor composite scores at a mean age of 16 months, ranging from 6–40 months. The good and poor outcomes were stratified by a threshold score of 80, and the patients were identified with good outcomes only when all cognitive, language, and motor composite scores were greater than 80.
In addition, post-mortem histologic evaluation was performed on brains of another group of infants (Group C, 1/3 males/females, mean age 10±6.8 days) with HIE. The infants were not the same ones who had MRIs.
PASL data acquisition and processing
The PASL images were acquired with perfusion model of PICORE Q2T from a 32-channel coil 3T Siemens scanner using the following parameters: bolus time TI1=700ms, inversion time TI =1800ms, TR/TE=2600/14ms, 14 slices, FOV=200×200mm, 64×64 matrix, voxel size=3.1×3.1×6.0mm3, flip angle=90°, 45 label/control image pairs. The cerebral blood flow (CBF) map was computed from the pulsed PASL images with a single-compartment model[18] with image preprocessing by ASL data processing toolbox (ASLtbx)[19]. The parameters utilized in calculating the CBF map were: The blood-brain partition coefficient λ = 1.10 mL/g for neonates[20], T1b = 1825ms and T2b = 191ms for neonates[21], labeling efficiency α = 0.98 for PASL[18]. The relaxed equilibrium magnetization M0b was calculated on cerebrospinal fluid (CSF), white matter (WM), and gray matter (GM) separately from the proton density-weighted image, with the signal ratios of the tissue type being RCSF = 0.87, RWM = 1.19, RGM = 0.98 [22] and T2CSF = 250ms, T2WM = 222 ms, T2GM = 143 m [23] used for neonates.
Statistical analysis
A Penn-CHOP neonatal brain atlas[24] was adopted to identify brain regions for statistical comparison between HIE neonates grouped by good and poor outcomes. The regional CBF map of each subject was normalized to their own mean whole brain CBF value before group comparison. The mean perfusion values in segmented brain structures were compared by permutation test to identify brain regions with statistically significant perfusion changes. P-value of less than 0.05 was considered statistically significant.
Results
Cerebral hypoperfusion in Papez circuit results in poor long-term outcomes in neonates with HIE
Significantly decreased perfusion in the Papez circuit was found in the HIE neonates with poor long-term neurodevelopmental outcomes when compared with HIE neonates with good outcomes. Decreased ASL perfusion values were seen in Papez circuit structures, including the fornix (p=0.002), entorhinal cortex (p=0.048), amygdala (p=0.036), hippocampus (p=0.033), and thalamus (p=0.036) (Table 1 and Figure 1). Figure 2 showed the hyperperfusion and hypoperfusion in Papez circuit by anatomy and CBF maps, correlating to good and poor outcomes, respectively.
Table 1.
Brain regions with significant perfusion differences between HIE neonates grouped by good and poor outcomes.
| Brain regions | Normalized | CBF (mean±std) | p-value |
|---|---|---|---|
| Group A: HIE neonates with good outcomes |
Group B: HIE neonates with poor outcomes |
P<0.05 | |
| fornix | 1.86±0.41 | 1.14±0.34 | 0.002 |
| thalamus | 2.25±0.58 | 1.60±0.20 | 0.036 |
| entorhinal cortex | 2.14±0.59 | 1.48±0.21 | 0.048 |
| amygdala | 2.06±0.51 | 1.43±0.30 | 0.036 |
| hippocampus | 2.09±0.39 | 1.58±0.36 | 0.033 |
HIE=hypoxic-ischemic encephalopathy, CBF=cerebral blood flow
Figure 1.
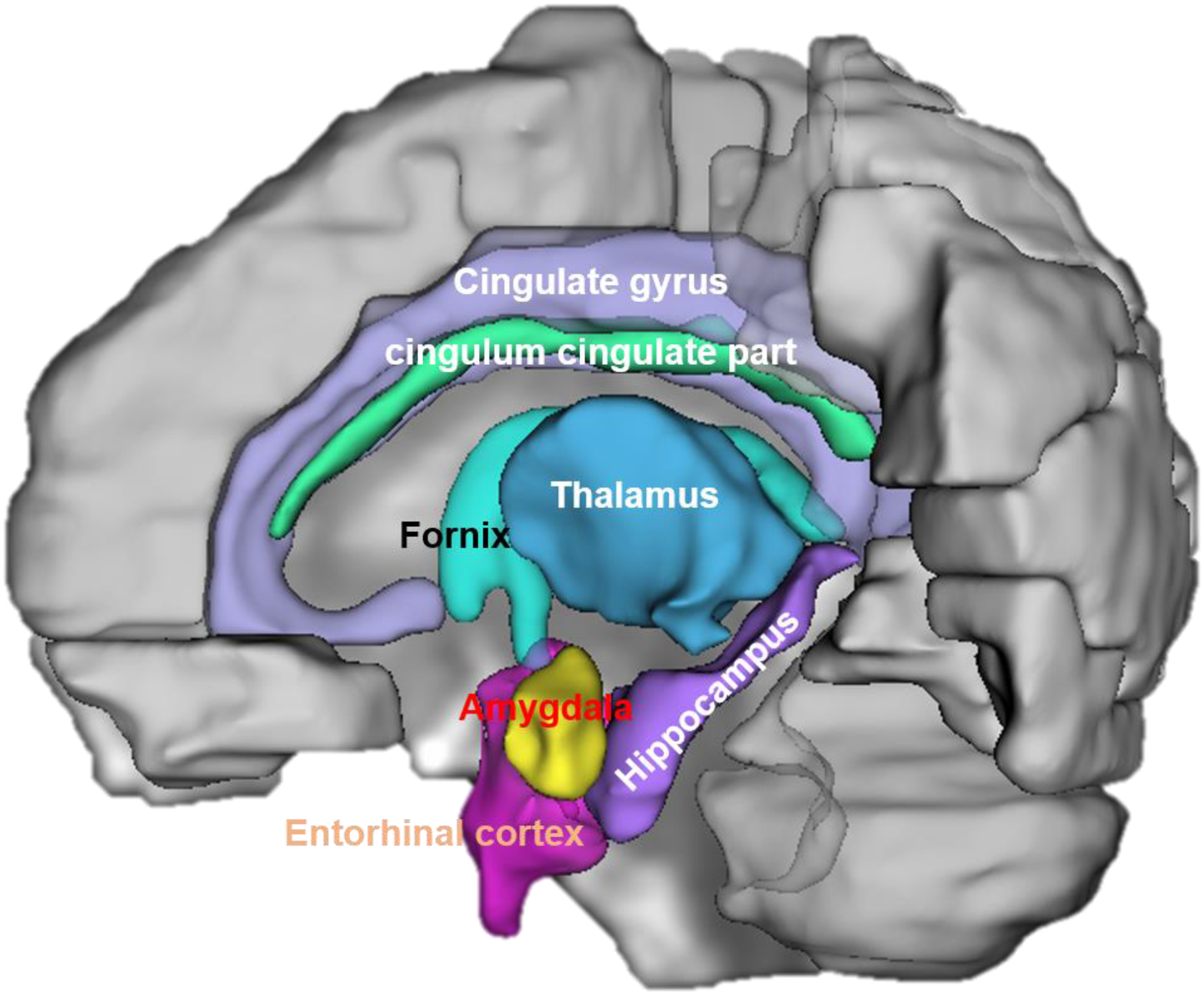
An example of Papez circuit regions with 3D segmentation.
Figure 2.
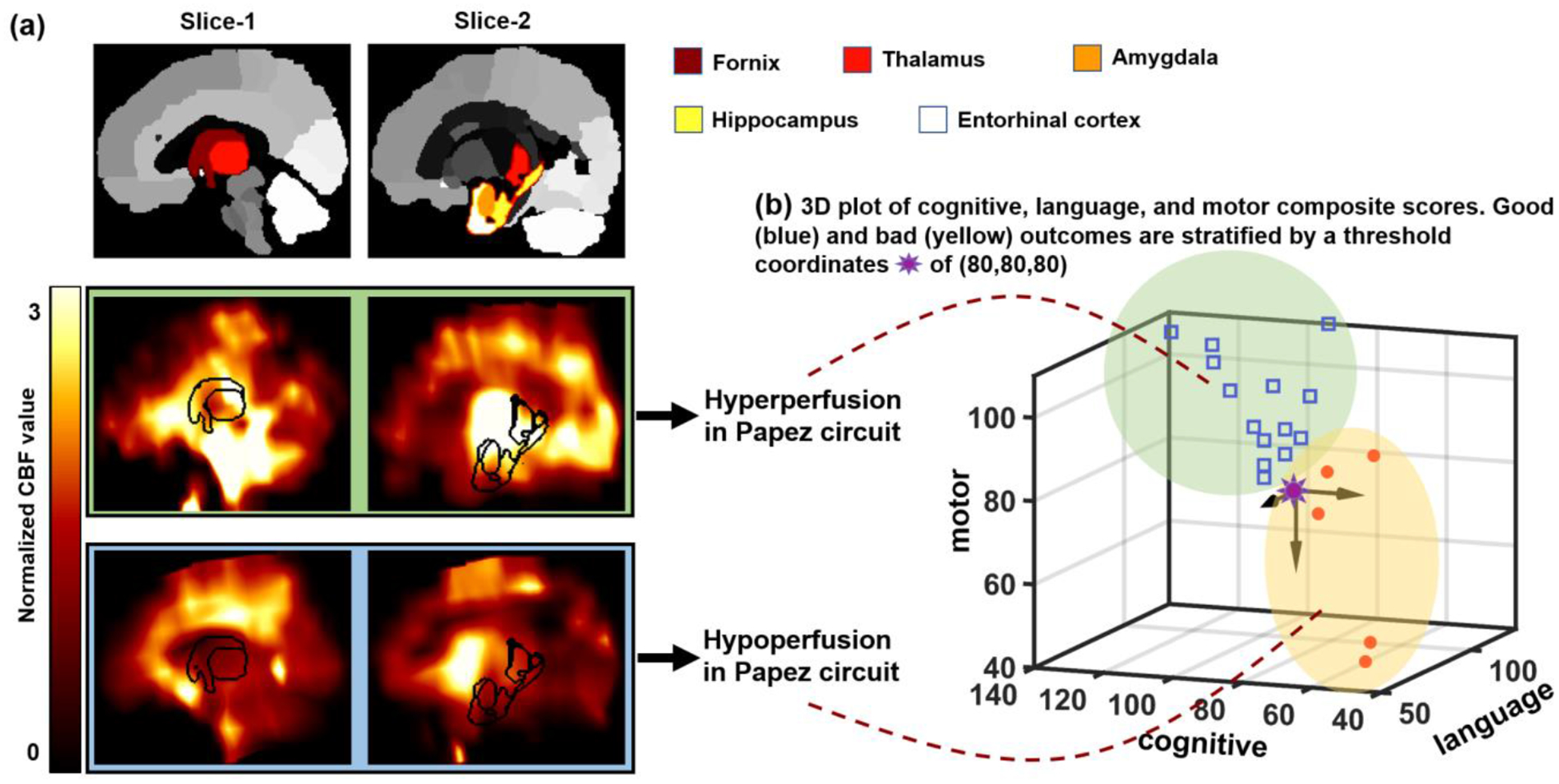
Hyper/hypoperfusion in Papez circuit correlate to good/poor outcome. (a) Hyperperfusion and hypoperfusion in Papez circuit in different slices shown by anatomy and CBF maps. (b) 3D plot of cognitive, language, and motor composite scores. The scores are stratified to good and bad outcomes by threshold of 80.
Histopathologic evidence of HIE in Papez circuit
We observed abnormalities in the fornix, entorhinal cortex, amygdala, hippocampus, thalamus, and cingulum cingulate part in an autopsy series (Figure 3). Specifically, a section of fornix showed reactive astrocytes and rarefaction. The entorhinal cortex demonstrated severe neuronal loss and edema, and nearly all remaining neurons showed hypoxic-ischemic changes. A section from amygdala demonstrated neuronal loss and several eosinophilic neurons, and a section taken from the CA1 region of hippocampus displayed pyramidal neurons with brightly eosinophilic cytoplasm and pyknotic nuclei. In addition, thalamus showed brightly eosinophilic neurons, and an example of the cingulum cingulate part demonstrated several reactive astrocytes and edema.
Figure 3.
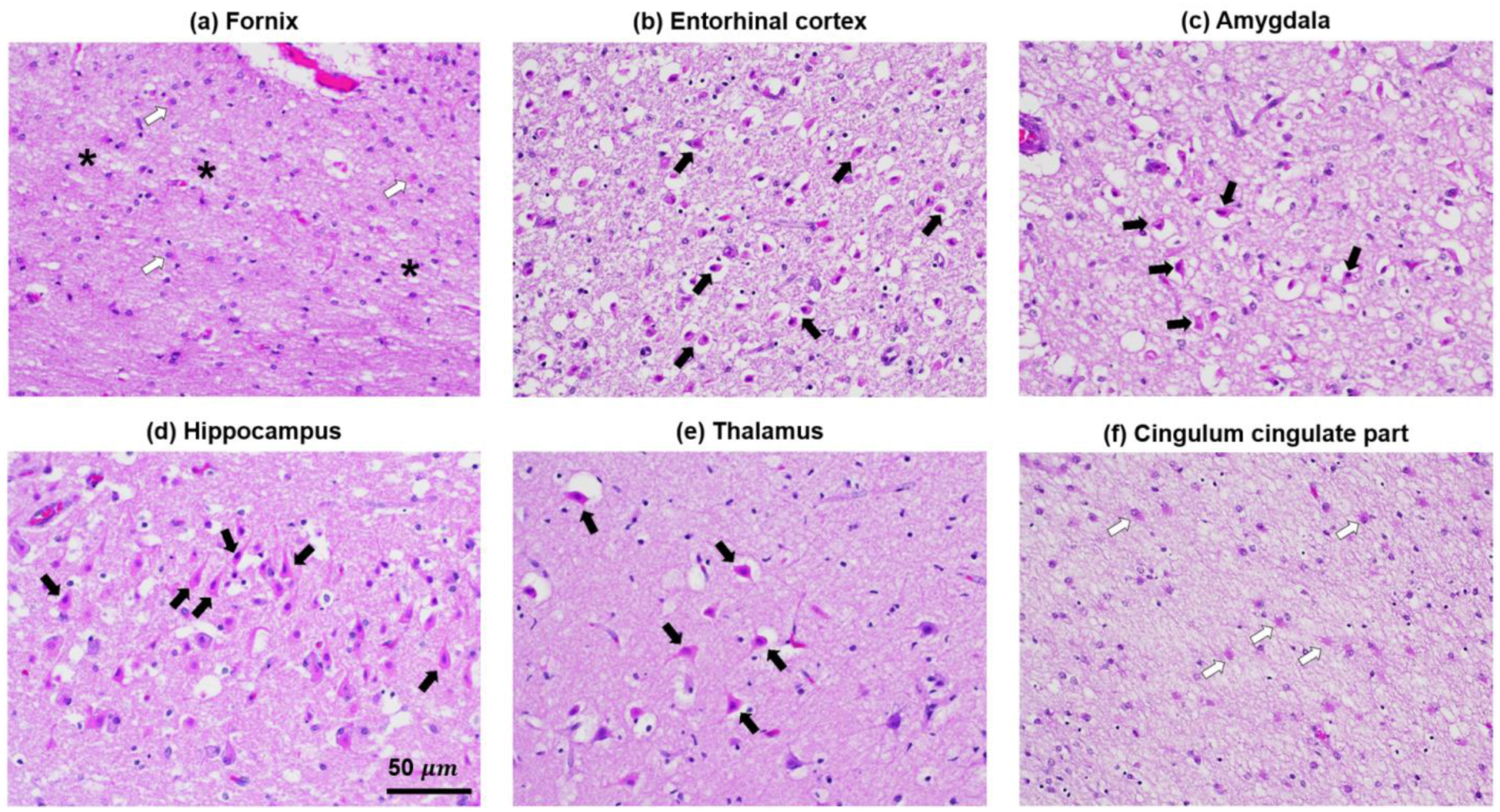
Histopathologic evidence of HIE in the fornix, entorhinal cortex, amygdala, and hippocampus, thalamus, and cingulum cingulate part. All images are of hematoxylin and eosin-stained sections taken at 200x magnification. Black arrows in (b-e) designate examples of eosinophilic (anoxic) neurons in each image. White arrows in (a) and (f) designate examples of reactive astrocytes. Asterisks in (a) designate regions of tissue rarefaction. The scale bar in (d) applies to all images.
For all cases illustrated, the damage in the limbic regions was equal to or greater than the damage in other brain regions. The most significant damage in these cases was often seen within the hippocampus and entorhinal cortex. For the subset of cases where damage was also present outside of the limbic regions, the involved areas were other cortical regions, basal ganglia and cerebellum.
Discussion and Conclusion
HIE is a leading cause of morbidity and mortality in the neonatal population, occurring with an incidence of 3 per 1000 live births in developed countries[25]. Neonatal HIE has been studied extensively and divided into two subtypes: watershed-predominant and central grey nuclei-predominant[26]. Prolonged HIE is typically associated with watershed injury, and acute HIE with central grey nuclei involvement. However, less is known about the involvement of the effect of HIE on the Papez circuit or limbic system, which includes a group of interconnected cortical and subcortical structures dedicated to linking visceral states and emotion to cognition and behavior[27]. The present study demonstrates that the structures of the Papez circuit are injured in neonatal HIE with radiologic-pathologic correlation.
In addition, our results support the role of ASL perfusion-weighted imaging in the detection of neonatal HIE and its potential guidance of prognostication and treatment. Cerebral hypoperfusion was observed within multiple structures of the Papez circuit, including the fornix, entorhinal cortex, amygdala, hippocampus, and thalamus, in neonates with neurodevelopmental delay as suggested by Bayley-III scores below 80. Persistent hypoperfusion may be associated with irreversible cell death and brain injury[28, 29]. Since injury to the Papez circuit has been associated with a variety of disorders, such as ASD[13], short- and long-term memory impairment[30], cerebellar cognitive affective syndrome[31], depression[32], schizophrenia[33], and Alzheimer’s disease[34], the study of injury of the Papez circuit following neonatal HIE may elucidate an important non-familial mechanism of neuropsychiatric disease evolution.
Neuronal cell death has been deeply studied in neonatal HIE[35]. In the present study, entorhinal cortex, amygdala, hippocampus, and thalamus demonstrated neuronal loss and neurons with eosinophilic cytoplasm, shrunken cell bodies, and pyknotic nuclei[35, 36], with the shrunken, eosinophilic neuron (anoxic neuron) being the hallmark of HIE. In addition, the fornix and cingulum cingulate part demonstrated reactive astrocytes, indicative of brain injury. Astrocytes provide structural, trophic, and metabolic support to neurons and modulate synaptic activity, and impairment of these functions during brain ischemia can critically influence neuron survival[37]. The fornix also contained regions of rarefaction, an abnormality which can be caused by hypoxic/ischemia[38]. It is still unclear to what degree apoptotic or necrotic mechanisms of cell death account for damage triggered by neonatal HIE[39].
Interestingly, hyperperfusion to the Papez circuit was associated with good neurodevelopmental outcomes. Reperfusion following a hypoxic ischemic insult can be restorative or harmful, depending on the extent to which it triggers the reperfusion injury cascade [40]. It may be that the increased perfusion to the circuit is a restorative process following HIE in the group with favorable neurodevelopmental outcome. The finding should be interpreted with caution, however, as hyperperfusion to brain regions following HIE has been implicated in poor neurodevelopmental outcomes likely due to reperfusion injury [40]. Hence, such perfusion based prediction of clinical outcomes will depend on a more complete understanding of the spatiotemporal evolution of cerebral perfusion, and that in the context of therapeutic interventions, co-morbidities, inherent vulnerability (i.e. gender, genetic, or metabolic), complications such as intracranial hemorrhage or seizures, and/or neurobehavioral interventions.
A few limitations existed in the present study. (1) The hypoperfusion in the cingulum cingulate part was not demonstrated on ASL imaging, while abnormality in the cingulum was demonstrated by pathology. The cingulum is a core part of the limbic system[41]. The cingulum contains long fiber tracts, and the areas of injury may have been sufficiently small to be below the resolution of ASL. This could be further studied by diffusion tensor tractography with fiber tracking. (2) The Bayley-III scores are widely ranging from 6–40 months, and not all post-mortem cases had available ASL data to perform individual-specific radiologic-pathologic correlation. (3) ASL data of neonatal brain is low resolution, which may raise questions of the validity of perfusion values in small anatomic structures. Nonetheless, our initial findings reveal important insights into the long-term implications of early injury to the Papez circuit.
In summary, we demonstrate that the Papez circuit is susceptible to hypoxic-ischemic injury in neonatal patients both on imaging and in pathology specimens. Bayley-III scores suggestive of developmental delay are associated with significantly lower perfusion values on ASL in the circuit. This finding raises the possibility of using perfusion-weighted imaging for detection of at-risk children who could benefit from further surveillance and interventions to improve long-term neurocognitive and neuropsychiatric outcomes.
Acknowledgments:
This work was supported by National Institutes of Health (KL2TR001879), National Natural Science Foundation of China (61802330, 61802331), and Natural Science Foundation of Shandong (ZR2018BF008).
Funding: This work was supported by National Institutes of Health (KL2TR001879), National Natural Science Foundation of China (61802330, 61802331), and Natural Science Foundation of Shandong (ZR2018BF008).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of interest: The authors have no conflict of interest.
Ethics approval: The retrospective case-control study followed an IRB-approved protocol.
Consent to participate: A waiver of consent/parental permission, assent and HIPAA authorization was approved by our institutional review board.
Consent for publication: Not applicable
Availability of data and material: Not applicable
Code availability: Not applicable
References
- [1].Papez JW (1937) A proposed machanism for emotion. Arch Neurol Psychiatry 38: 725–743 [Google Scholar]
- [2].MacLean PD (1949) Psychosomatic disease and the “visceral brain”: recent developments bearing on the Papez theory of emotion. Psychosom Med 11: 338–353 [DOI] [PubMed] [Google Scholar]
- [3].Shah A, Jhawar SS, Goel A (2012) Analysis of the anatomy of the Papez circuit and adjoining limic system by fiber dissection techniques. J Clin Neurosci 19: 289–298 [DOI] [PubMed] [Google Scholar]
- [4].Concha L, Gross DW, Beaulieu C (2005) Diffusion tensor tractography of the limbic system. AJNR Am J Neuroradiol 26: 2267–2274 [PMC free article] [PubMed] [Google Scholar]
- [5].Choi SH, Kim YB, Paek SH, Cho ZH (2019) Papez circuit observed by in vivo human brain with 7.0T MRI super-resolution track density imaging and track tracing. Front Neuroanat 18: 13–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Torrico TJ, Abdijadid S (2019) Neuroanatomy, limbic system. StatPearls [PubMed] [Google Scholar]
- [7].Roxo MR, Franceschini PR, Zubaran C, Kleber FD, Sander JW (2011) The limbic system conception and its historical evolution. ScientificWorldJournal 11: 2428–2441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bubb EJ, Kinnavane L, Aggleton JP (2017) Hippocampal-diencephalic-cingulate networks for memory and emotion: An anatomical guide. Brain Neurosci Adv 1: 2398212817723443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yang DS, Kwon HG, Jang SH (2016) Injury of the thalamocingulate tract in the Papez circuit in patients with mild traumatic brain injury. Am J Phys Med Rehabil 95: e34–e38 [DOI] [PubMed] [Google Scholar]
- [10].Jang SH, Kwon HG (2018) Injury of the Papez circuit in a patient with traumatic spinal cord injury and concomitant mild traumatic brain injury. Neural Regen Res 13: 161–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Escobar I, Xu J, Jackson CW, Perez-Pinzon MA (2019) Altered neural networks in the Papez circuit: Implications for cognitive dysfunction after cerebral ischemia. J Alzheimers Dis 67: 425–446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hisle-Gorman E, Susi A, Stokes T, Gorman G, Erdie-Lalena C, Nylund CM (2018) Prenatal, perinatal, and neonatal risk factors of autism spectrum disorder. Pediatr Res 84: 190–198 [DOI] [PubMed] [Google Scholar]
- [13].Badawi N, Dixon G, Felix JF, Keogh JM, Petterson B, Stanley FJ, Kurinczuk JJ (2006) Autism following a history of newborn encephalopathy: more than a coincidence? Dev Med Child Neurol 48: 85–89 [DOI] [PubMed] [Google Scholar]
- [14].Zornberg GL, Buka SL, Tsuang MT (2000) Hypoxic-ischemia-related fetal/neonatal complications and risk of schizophrenia and other nonaffective psychoses: A 19-year longitudinal study. Am J Psychiatry 157: 196–202 [DOI] [PubMed] [Google Scholar]
- [15].Zhao F, Yang J, Cui R (2017) Effect of hypoxic injury in mood disorder. Neural Plast 2017: 1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Haukvik UK, McNeil T, Lange EH, Melle I, Dale AM, Andreassen OA, Agartz I (2014) Pre- and perinatal hypoxia associated with hippocampus/amygdala volume in bipolar disorder. Psychol Med 44: 975–985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bayley N (2006) Bayley scales of infant and toddler development, third edition San Antonio, TX: Harcourt Assessment, Inc [Google Scholar]
- [18].Alsop DC, Detre JA, Golay X, Gunther M, Hendrikse J, Hernandez-Garcia L, Lu H, Maclntosh BJ, Parkes LM, Smits M, Osch MJv, Wang DJ, Wong EC, Zaharchuk G (2015) Recommended implementation of arterial spin labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med 73: 102–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang Z, Aguirre GK, Rao H, Wang J, Fernandez-Seara MA, Childress AR, Detre JA (2008) Empirical optimization of ASL data analysis using an ASL data processing toolbox: ASLtbx. Magn Reson Imaging 26: 261–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Herscovitch P, Raichle ME (1985) What is the correct value for the brain blood partition coefficient for water. J Cereb Blood Flow Metab 5: 65–69 [DOI] [PubMed] [Google Scholar]
- [21].Liu P, Chalak LF, Krishnamurthy LC, Mir I, Peng SL, Huang H, Lu H (2016) T1 and T2 values of human neonatal blood at 3 Tesla: Dependence on hematocrit, oxygenation, and temperature. Magn Reson Med 75: 1730–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cavusoglu M, Pfeuffer J, Ugurbil K, Uludag K (2009) Comparison of pulsed arterial spin labeling encoding schemes and absolute perfusion quantification. ScienceDirect 27: 1039–1045 [DOI] [PubMed] [Google Scholar]
- [23].Counsell SJ, Kennea NL, Herlihy AH, Allsop JM, Harrison MC, Cowan FM, Hajnal JV, Edwards B, Edwards AD, Rutherford MA (2003) T2 relaxation values in the developing preterm brain. AJNR Am J Neuroradiol 24: 1654–1660 [PMC free article] [PubMed] [Google Scholar]
- [24].Feng L, Li H, Oishi K, Mishra Y, Song L, Peng Q, Ouyang M, Wang J, Slinger M, Jeon T, Lee L, Heyne R, Chalak L, Peng Y, Liu S, Huang H (2019) Age-specific gray and white matter DTI atlas for human brain at 33, 36 and 39 postmenstrual weeks. Neuroimage 185: 685–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kurinzcuk JJ, White-Koning M, Badawi N (2010) Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum Dev 86: 329–338 [DOI] [PubMed] [Google Scholar]
- [26].Miller SP, Ramaswarmy V, Michelson D, Barkovich AJ, Holshouser B, Wycliffe N, Glidden DV, Deming D, Partridge JC, Wu YW, Ashwal S, Ferriero DM (2005) Patterns of brain injury in term neonatal encephalopathy. J Pediatr 146: 453–460 [DOI] [PubMed] [Google Scholar]
- [27].Catani M, Dell’acqua F, Schotten MTd (2013) A revised limbic system model for memory, emotion and behaviour. Neurosci Biobehav Rev 37: 1724–1737 [DOI] [PubMed] [Google Scholar]
- [28].Tortora D, Mattei PA, Navarra R, Panara V, Salomone R, Rossi A, Detre JA, Caulo M (2017) Prematurity and brain perfusion: Arterial spin labeling MRI. Neuroimage Clin 15: 401–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Massaro AN, Jeromin A, Kadom N, Vezina G, Hayes RL, Wang KK, Streeter J, Johnston MV (2013) Serum biomarkers of MRI brain injury in neonatal hypoxic ischemic encephalopathy treated with whole-body hypothermia: a pilot study. Pediatr Crit Care Med 14: 310–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Delcour M, Russier M, Amin M, Baud O, Paban V, Barbe MF, Coq JO (2012) Impact of prenatal ischemia on behavior, cognitive abilities and neuroanatomy in adult rats with white matter damage. Behav Brain Res 232: 233–244 [DOI] [PubMed] [Google Scholar]
- [31].Schmahmann JD, Sherman JC (1998) The cerebellar cognitive affective syndrome. Brain 121: 561–579 [DOI] [PubMed] [Google Scholar]
- [32].Bhatia KD, Henderson LA, Hsu E, Yim M (2018) Reduced integrity of the uncinate fasciculus and cingulum in depression: A stem-by-stem analysis. J Affect Disord 235: 220–228 [DOI] [PubMed] [Google Scholar]
- [33].Whitford TJ, Lee SW, Oh JS, Luis-Garcia Rd, Savadjiev P, Alvarado JL, Westin CF, Niznikiewicz M, Nestor PG, McCarley RW, Kubicki M, Shenton ME (2014) Localized abnormalities in the cingulum bundle in patients with schizophrenia: a diffusion tensor tractography study. Neuroimage Clin 5: 93–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Catheline G, Periot O, Amirault M, Braun M, Dartigues JF, Auriacombe S, Allard M (2010) Distinctive alterations of the cingulum bundle during aging and Alzheimer’s disease. Neurobiol Aging 31: 1582–1592 [DOI] [PubMed] [Google Scholar]
- [35].Northington FJ, Chavez-Valdez R, Martin LJ (2011) Neuronal cell death in neonatal hypoxia-ischemia. Ann Neurol 69: 743–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Greer DM (2006) Mechanisms of injury in hypoxic-ischemic encephalopathy: implications to therapy. Semin Neurol 26: 373–379 [DOI] [PubMed] [Google Scholar]
- [37].Chen Y, Swanson RA (2003) Astrocytes and brain injury. J Cereb Blood Flow Metab 23: 137–149 [DOI] [PubMed] [Google Scholar]
- [38].Zhang F, Liu C, Qian L, Hou H, Guo Z (2016) Diffusion Tensor Imaging of White Matter Injury Caused by Prematurity-Induced Hypoxic-Ischemic Brain Damage. Med Sci Monit 22: 2167–2174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Nakajima W, Ishida A, Lange MS, Gabrielson KL, Wilson MA, Martin LJ, Blue ME, Johnston MV (2000) Apoptosis has a prolonged role in the neurodegeneration after hypoxic ischemia in the newborn rat. J Neurosci 20: 7994–8004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ambrosio ALD, Pinsky DJ, Connolly ES (2001) The role of the complement cascade in ischemia/reperfusion injury: Implications for neuroprotection. Mol Med 7: 367–382 [PMC free article] [PubMed] [Google Scholar]
- [41].Bubb EJ, Metzler_baddeley C, Aggleton JP (2018) The cingulum bundle: Anatomy, function, and dysfunction. Neurosci Biobehav Rev 104: 104–127 [DOI] [PMC free article] [PubMed] [Google Scholar]


