Abstract
Background
Since the global outbreak of coronavirus disease-2019 (COVID-19), plastic surgeons were forced to transition from traditional didactics to virtual lectures to practice “social distancing.” As this method of education continues to be widely used, understanding the current trend of its usage is critical. In this study, we performed a survey study of virtual lecture attendees and presenters to determine current usage and general consensus on virtual lectures in plastic surgery education.
Methods
An electronic survey was sent to attendees and presenters of virtual lectures using Google Forms. Demographic data, webinar usage patterns, and views on virtual lectures were collected.
Results
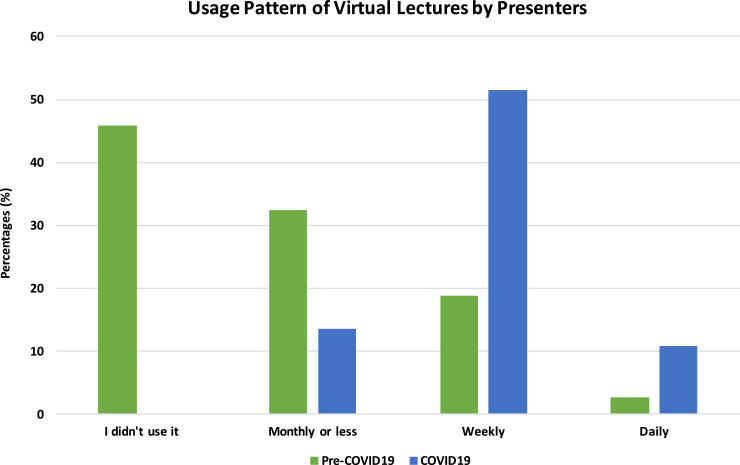
A total of 417 surveys were received. Prior to the COVID-19 era, 39.1percent of attendees did not use virtual lectures and 45.6percent of presenters did not give webinars at all. Both groups reported that the lack of opportunities and need were the most common cause of no use of lectures or webinars. After the outbreak, 35.4percent of attendees now use virtual lectures daily and 51.4percent of presenters give lectures weekly. Over 90percent of the study population reported a positive experience with the virtual lectures due to increased interaction, convenience, outreach, and usability. Finally, over 75percent stated that virtual lectures might replace classroom lectures in the future.
Conclusion
Our study shows that a majority of plastic surgeons have begun to use and give virtual lectures daily after the COVID-19 outbreak. Virtual education is a powerful and versatile tool that has great potentials, and it may continue to serve as a part of surgical training in the future.
Keywords: COVID-19, Plastic surgery education, Social media, Zoom, Webinar, Virtual classroom
Introduction
On December 2019 at Wuhan, Hubei province, China, what is now known as the Coronavirus Disease-2019 (COVID-19) outbreak started.1 The virus rapidly spread around the globe, inflicting up to 2.2 million people by mid-April of 2020.2 COVID-19 is known to spread from person to person, and it can remain on the surface of plastics for up to 72 h. 3 , 4 Because of its high transmission rate, governments across the globe executed orders to ban leaving the home for anything other than essential activities such as grocery shopping.5 Plastic surgeons have stopped any elective surgeries to preserve personal protective equipment and joined the fight against the COVID-19 by taking care of critically ill patients at the Intensive Care Units.6
As the COVID-19 outbreak continued, the question of how to continue plastic surgery education during the outbreak arose. Plastic surgery trainees at North America traditionally attend classroom didactics, followed by online modules on the American Society Plastic Surgeons (ASPS) Education Network (EdNet).7, 8, 9 In addition, trainees have visiting professors to participate in hands on courses and attend national conferences.7 In contrast, offline learning maybe limited to countries without an established plastic surgery community and resources to train a large number of residents. In these countries, online platforms such as social media and online community are widely used to seek guidance and learn from the experts online.10, 11, 12, 13
To adhere to the rules of “social distancing,” plastic surgeons have rapidly transitioned from teaching offline to online. American Council of Academic Plastic Surgeons (ACAPS) now provides a combined calendar that shows lectures provided by multiple societies.14 Webinars are given by experts almost daily, and the participation in these lectures continues to increase exponentially.15 As this method of education continues to be widely used, to understand the current trend of its usage will help determine how the specialty can better implement and identify its risks. Therefore, the goal of this study was to determine the current virtual lecture usage and general consensus on virtual lectures in plastic surgery.
Methods
An electronic survey was sent to the attendees of virtual lectures at 12 international institutions (Barcelona, Israel, United Kingdom, United States, Taiwan, Thailand, South Korea) and International Microsurgery Journal Club webinar using Google Forms (Google LLC, Mountain View, CA, USA). The survey consisted of 12 questions written with skip logic, in which the following question depended on the answer to a current question. In addition, the surveys were sent to a group of presenters (112 lecturers) who had given virtual lectures since the COVID-19 outbreak (esthetic surgery, craniofacial surgery, reconstruction, and microsurgery). The survey consisted of 10 questions, and Google Form was used. The surveys were deployed once by email, and the responses were collected from April 7 to May 16, 2020.
Statistical analyses were performed using the SPSS (version 24; SPSS, Inc., Chicago, IL) software. Nonparametric data were described with frequency and percentage. Descriptive analyses were conducted by using chi square tests, and a p-value of <0.05 was considered statistically significant.
Results
Demographic data
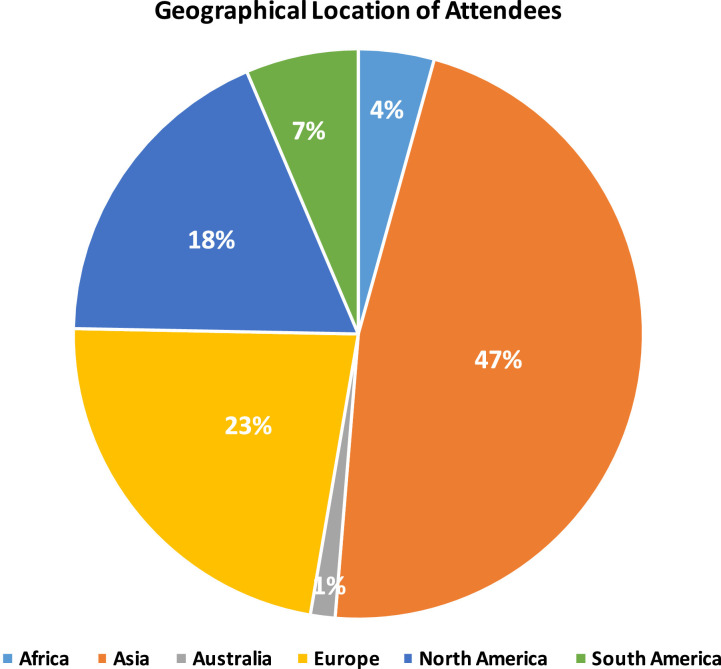
Of the 465 attendees, we received 345 total responses. Of these, 2 responses were discounted due to technical errors in the survey (Table 1 ). Therefore, we had a total response rate of 74.1 percent (345 out of 465). Of the 343 attendees, the majority of the study population was from Asia, followed by Europe, North America, South America, Africa, and Australia (Figure 1 ). The majority of respondents were in practice, followed by fellowship, last year of residency, mid-residency, early years of residency, and medical school.
Table 1.
Characteristics of survey respondents
| Characteristic | Percentage of Attendees (N = 343) | Percentage of Presenters (N = 74) |
|---|---|---|
| Distribution of participants | ||
| Practicing surgeon | 54.2 | - |
| Fellow | 10.5 | - |
| Resident | 31.2 | - |
| Medical student | 4.1 | - |
| Geographic location | ||
| Africa | 4.3 | 0 |
| Asia | 47 | 13.5 |
| Australia | 1.4 | 1.4 |
| Europe | 22.6 | 17.6 |
| North America | 18.3 | 47.3 |
| South America | 6.4 | 20.3 |
| Use of live virtual lectures before the COVID-19 Outbreak | ||
| I did not use it | 39.1 | 45.9 |
| Monthly or less | 38.3 | 32.4 |
| Weekly | 16.5 | 18.9 |
| Daily | 6.1 | 2.7 |
| Use of live virtual lectures after the COVID-19 Outbreak | ||
| I did not use it | 2.9 | 0 |
| Monthly or less | 9.6 | 13.5 |
| Weekly | 52.2 | 51.4 |
| Daily | 35.4 | 10.8 |
| Difficulty with assessing virtual lectures | ||
| Yes | 11.9 | 8.1 |
| No | 88.1 | 91.9 |
| Experience with virtual lectures | ||
| Excellent | 42.9 | 40.5 |
| Good | 49.6 | 50 |
| Fair | 4.9 | 9.5 |
| Poor | 2.3 | 0 |
| Very poor | 0.3 | 0 |
Figure 1.
Geographical location of attendees.
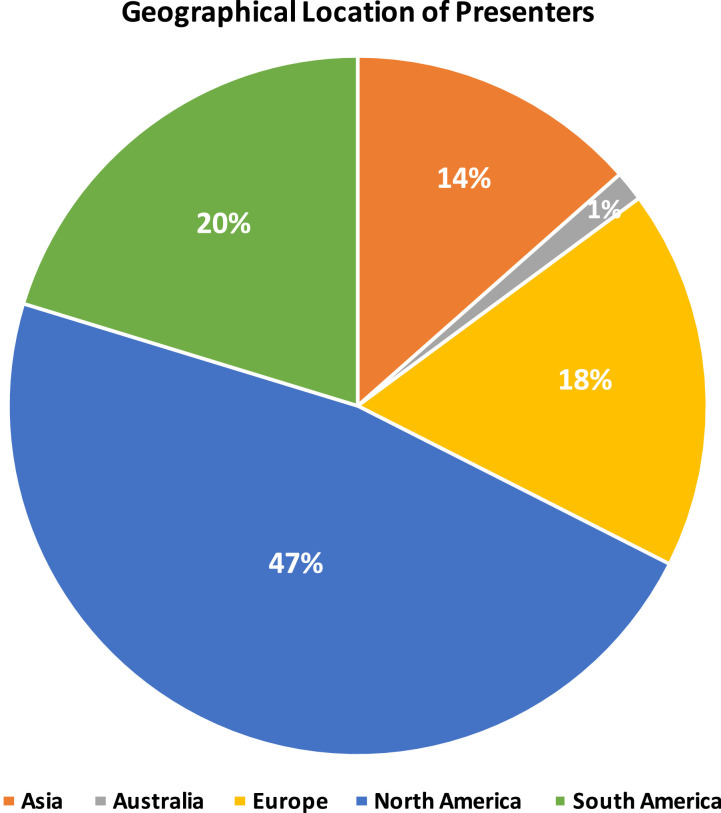
For the presenters, the survey was sent to the 112 lecturers, and we received 76 total responses. Of these, 2 responses were discounted due to the lack of giving virtual lectures before or after the outbreak. Therefore, we had a total response rate of 66.1 percent for the presenters. Of the 74 respondents, the majority of the presenters are from North America, followed by South America, Europe, Asia, and Australia (Figure 2 ). The majority of presenters are in microsurgery (87.8 percent), general reconstruction (47.3 percent), hand (25.7 percent), aesthetic (23 percent), craniofacial (6.8 percent), and orthopedics (1.4 percent).
Figure 2.
Geographical location of presenters.
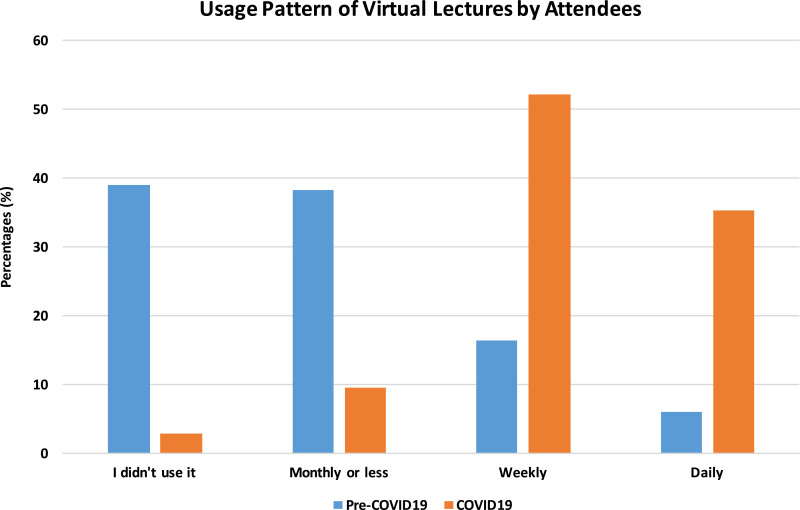
Virtual lecture usage patterns during Pre- COVID-19 outbreak
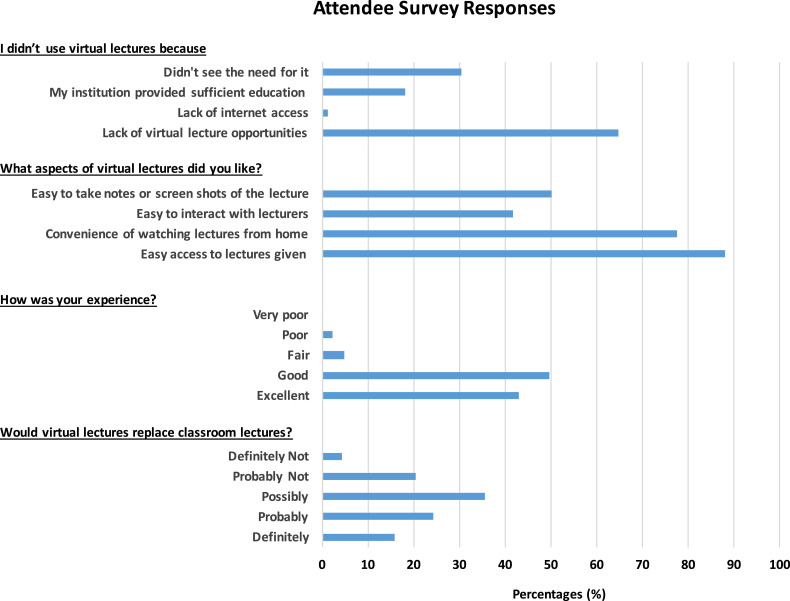
Prior to the COVID-19 outbreak, 39.1 percent of attendees did not use virtual lectures at all and 38.3 percent of them used virtual lectures monthly (Figure 3 ). Only 6.1 percent of the attendees used online lectures daily. The majority of attendees reported that the lack of virtual lecture opportunities (64.8 percent) was the cause of non-use (Figure 4 ). In addition, 30.3 percent did not see the need for virtual lectures and 18 percent felt that they have enough education materials from their institutions.
Figure 3.
Usage Patterns Pre vs. Post COVID-19 Outbreak by attendees.
Figure 4.
Survey responses by attendees.
When compared across the continents, South America attendees used virtual lectures most frequently prior to the outbreak. In all, 86.4 percent of them used virtual lectures to some degree when about 54 percent-67.9 percent of each continent's users did. The range of daily users was 0 percent to 9.1 percent of each continent's users, and usage patterns were similar across the continents (p = 0.183).
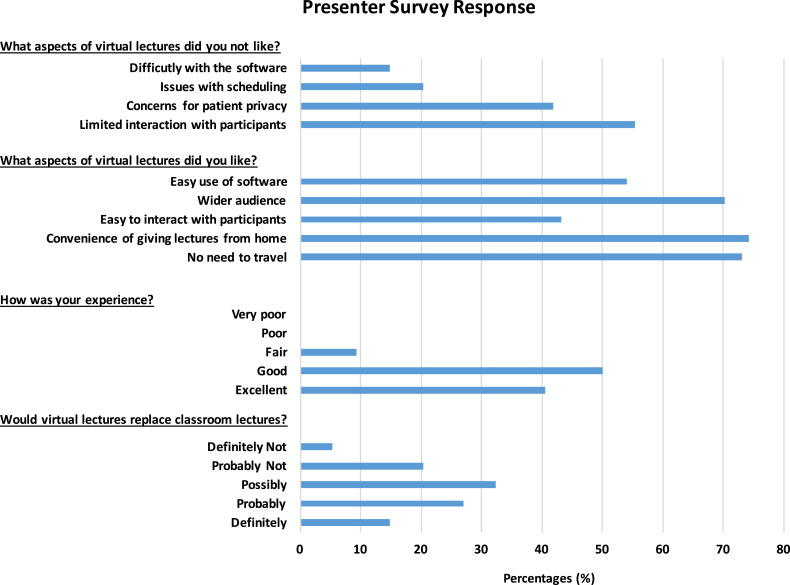
Similarly, virtual lectures were not frequently given prior to the outbreak; 45.9 percent of presenters did not give any virtual lectures (Figure 5 ). The presenters reported that limited opportunities, lack of appropriate platforms, sufficient teaching opportunities in national conferences, and the lack of need were the reasons of non-use (Figure 6 ).
Figure 5.
Usage Patterns Pre vs. Post COVID-19 Outbreak by presenters.
Figure 6.
Survey responses by presenters.
Virtual lecture usage pattern during the COVID-19 outbreak
After the outbreak, 35.4 percent of the attendees use virtual lectures daily and 52.2 percent use them weekly. The percentages of those who do not use virtual lectures at all have decreased from 39.1 percent to 2.9 percent after the outbreak. Interestingly, practicing plastic surgeons were using virtual lectures more frequently than trainees (p<0.05).
Since the outbreak, presenters now give lectures weekly (51.4 percent) and monthly or less (35.1 percent). Thus far, 45.9 percent of the lecturers have given at least 5-10 virtual lectures, 31.1 percent have given less than 5, and 9.5 percent have given over 20 lectures. A total of 91.9 percent reported that they did not have any difficulty with giving virtual lectures.
Positive views on virtual lectures
Overwhelming number of the attendees had a positive experience with virtual lectures: 42.9 percent (excellent) and 49.6 percent (good). The majority of these attendees reported that they liked virtual lectures due to easy access to lectures given by international experts, convenience of watching lectures from home, ability to take notes/screen shots, and interaction with lecturers (Figure 5). Overall views on virtual sessions were similar across different levels of training (p = 0.541).
Equivalently, over 90 percent of presenters at least had good experience with virtual lectures: 40.5 percent (excellent) and 50 percent (good). They reported that there was no need to travel, convenience of giving lectures from home, wider audience, interaction with attendees, and easy use of software were the major benefits of virtual lectures (Figure 6).
Negative views on virtual lectures
A minority of attendees had a negative experience: 4.9 percent (fair), 2.3 percent (poor), and 2.3 percent (very poor). Only few attendees did not like virtual lectures (9 attendees), and they attributed causes to lack of interaction with lecturers (55.6 percent). For the presenters, only 9.5 percent had a fair experience with virtual sessions. None reported poor or very poor experience so far. They reported that difficulty in interacting with attendees (55.4 percent), concerns for patient privacy (41.9 percent), and issues with scheduling (20.3 percent) were the aspects of virtual lectures that they did not like (Figure 6).
Need for virtual lectures post COVID-19 outbreak
Lastly, respondents were asked whether virtual lectures would replace classroom lectures after the COVID-19 outbreak. A large percentage of both attendees and presenters had very positive views on the future of virtual lectures; over 75 percent believed that virtual lectures would probably replace traditional lectures. Only 24.6 percent of the attendees and 20.3 percent of the lecturers reported that they do not think classroom lectures can be replaced.
When compared across the levels of training, there was no difference in views toward the future of virtual lectures (p = 0.541). Interestingly, Africa and Australia had less enthusiastic views toward virtual lectures. Over 46.7 percent of African attendees and 40 percent of Australian attendees reported that they do not think virtual lectures would replace classroom lectures while 21.9 percent of Asian, 20.5 percent of European, 30.1 percent of North American, and 22.7 percent of South American attendees had negative views. However, no statistical significance was achieved (p = 0.77).
Discussion
As many inventions have sprouted in times of difficulty, the COVID-19 has completely changed the way medicine is practiced now. Drive-through screening tests, 3D printed medical devices, and hands-free door openers are just a few to name.16 , 17 Similarly, the way students are learning has changed completely. Across the globe, schools, from elementary school to colleges, have closed and moved to virtual classrooms in efforts to limit the spread of the COVID-19.18, 19, 20 Similarly, plastic surgeons have also joined this movement and begun to institute virtual lectures such as ASPS Grand Round series, ASJ webinars, and multi-institutional grand rounds. As virtual lectures are being widely used, understanding current usage, general consensus, and its risks is paramount.
In our study, we sent an electronic survey to the attendees of virtual lectures at 12 international institutions and International Microsurgery Journal Club webinar. Our study shows that a large number of plastic surgeons did not use virtual learning sessions prior to the COVID-19 (39.1 percent) or give virtual lectures (45.9 percent). This finding is not surprising as the majority of educational curriculum consists of didactics in classrooms, operating in the operating room, specialty-specific conferences, and hands on labs. However, the number of plastic surgeons using the webinars exponentially increased after the outbreak. The majority of attendees became a daily user (35.4 percent) and 52.2 percent use weekly. Interestingly, practicing plastic surgeons were using virtual lectures more frequently than trainees (p<0.05) prior to the outbreak. However, about 50 percent of residents did not use virtual lectures prior to the outbreak but over 40 percent of residents now use lectures daily. Similarly, the majority of presenters now give virtual lectures weekly (51.4 percent) or daily (10.8 percent).
Both attendees and presenters reported the lack of live lecture opportunities as the most common cause of not using virtual lectures prior to the outbreak. This finding can be secondary to the number of courses and specialty-specific conferences that are available. Currently, there are numerous conferences available for different fields of plastic surgery: esthetic, craniofacial, hand, and reconstructive surgery. Residents typically attend 1-2 conferences per year as a part of their educational conference. They frequently use this opportunity to network, discuss, and learn from experts of the field.7 , 21 Given that numerous opportunities are available to learn in person, virtual lectures, although available, were not offered or used frequently. This phenomenon is also reflected on how 30.2 percent of attendees and 36.2 percent of presenters did not see the need for virtual lectures. In addition, over 50 percent of residents did not use virtual lectures at all prior to the outbreak.
Despite the lack of use prior to the outbreak, the future of virtual lecture is promising. Over 90 percent of both attendees and presenters had at least good experience, and 75 percent believe that virtual lectures can possibly replace the traditional classroom in the future. Currently, there are different platforms available to set up virtual classrooms: GoToMeeting, Skype, WebEx, and Zoom (Table 2 ). All four platforms work similarly. Typically, the number of attendees varies from 50 to 100 attendees for a free plan, and it can go up to 1,000 attendees with a monthly plan. Presenters can share their content, and attendees can participate through microphone, text their questions, record the lecture with the presenter's permission, and take screen shots of the lectures. In addition, the majority of attendees reported that its advantages include easy access, convenience, usability, and increased interaction with lecturers. A similar trend was observed from the presenters. Many attendees agree that virtual lectures allow many advantages over traditional classrooms: 1) ability to freely join or leave lectures; 2) opportunity to listen from international experts whom they can only meet at international or national conferences; 3) ability to ask questions without feeling shy; 4) chance to listen to answers to all questions without interruptions; and 5) having the access of world-class experts from their smartphones. For the presenters, the benefits were as follows: 1) no traveling; 2) convenience of giving lectures from home; 3) wider audience; and 4) increased interaction with attendees. These features are not available in prerecorded lectures.22
Table 2.
Comparison of traditional didactics vs. virtual learning sessions
| Traditional didactic sessions | Virtual learning sessions | |
|---|---|---|
| Location | Conference room |
|
| Number of attendees | Limited by the occupancy capacity of the room | Based on the type of platformGoToMeeting
|
| Multimedia | Can take photos during lectures but typically in a low resolution |
|
| Interactive | Can interact with lecturers by asking questions | Can interact with lecturers using text or microphone |
| Cost |
|
|
| Security |
|
|
In contrast, there are concerns for virtual lectures: lack of interaction with lecturers, limited Internet access, and difficulty with the software in those who did not have a positive experience. Because of the nature of virtual platforms, respondents reported that these platforms do not provide the same level of interaction and interpersonal relationship as the in-person lectures do. In addition, each presenter may use different types of platforms, and attendees need to be well versed at using all types of platforms if they want to maximize their experience. There are also concerns for online security and privacy. There has been multiple reports of “Zoombombing,” in which intruders hijack Zoom sessions and show profanity.23 In response, FBI recommends increasing the security by requiring a meeting password and managing screen sharing by the meeting organizer. Furthermore, some of the lectures include identifiable patient information, and taking screen shots or recording these lectures may not be Health Insurance Portability and Accountability ACT (HIPAA) compliant. In all, 41.9 percent of presenters expressed concerns of patient privacy.
Despite the benefits and concerns, the main challenge of using virtual lectures is lack of hands on opportunities and meeting colleagues in person. No virtual sessions can replicate the operating experience, and clinical experience is critical for the surgical training. While virtual lectures can include videos of procedures, it is not the same as being in the operating room, planning for the procedure, managing complications, and taking care of patients. To fight the outbreak, many plastic surgery residents and faculty have been redeployed and elective procedures have been stopped. Therefore, virtual lectures are serving as the primary means of surgical education at this time. If the outbreak continues, live-streaming lectures, which have been extensively used and found to be safe in the fields of urology and cardiothoracic surgery, may need to be implemented to supplement the training.24, 25, 26
Therefore, what does this finding mean for the future of plastic surgery training? According to the survey, the majority feels that this method of education and training will be able to replace some aspects of direct, face-to-face training. There will be commoditized lectures and resources available to trainees all over the world. They could watch and study at their own pace and place and have access to international experts leading in that field. These changes will allow trainees to better prepare themselves for the actual surgery or training. Most of all, with the current reduction in training time, this may perhaps allow an improved allocation of trainees’ time and enable them to prepare accordingly. Additionally, it will also allow professors and teachers to dedicate more time for mentorship, research, and other matters that can be more valuable than just basic teaching. The authors believe that this unexpected change in learning and teaching due to the COVID-19 pandemic perhaps can be an opportunity to change the delivery of education in a more efficient manner in future.
Lastly, many presenters agree with Dr Andrew Hart's sentiment: “It's an exciting opportunity to democratize education and bring the world closer together in what is already a more international specialty than most.” Additionally, it has allowed “people from less fortunate countries have access to teaching by super academic teachers” as Dr Hinne Rakhorst said. However, “[Virtual education] is here to stay but it needs refinement” as Dr Rod Rohrich said. Many lecturers also agree with Dr Justin Sacks’ sentiment: “[online education] is nice but not the same. [We] want to walk the earth, meet the people, sample the cuisine of the cities, and cultures we interact with. However, online virtual education is here to stay and will become an important part of what we do and making the world even smaller than it already is for us.” Dr Scott Levin also agrees that “experiencing each other's cultures, customs, and family cannot be underestimated.”
There are few limitations in this study. First, survey responses regarding pre-COVID era can be biased by memory recall. In addition, the outbreak started at different time points for each country, which can further lead to increased variation among survey respondents. Second, survey questions were not open-ended, and this study may not have captured the scope of potential responses for the positives and negatives of virtual lectures.
Conclusion
Given the current situation of the COVID-19 global pandemic, plastic surgery trainees and faculty have changed the way plastic surgery education is performed. Overall, our study shows that virtual lectures provide numerous benefits at this time, and many respondents believe that this method of education can possibly substitute traditional classrooms beyond the COVID-19 pandemic. It has allowed those with years of experience to share their wisdom and pearls selflessly with those who are seeking to learn during this unprecedented time. While virtual education has been adapted to continue education during this unprecedented time, we believe that the benefit of using this type of learning is paramount and may serve as an adjunct to traditional classroom lectures in the future. However, the study also shows that there are concerns for online security and patient privacy, and the involvement of professional societies maybe warranted to ensure patient privacy.
Financial disclosure and products
The authors have no financial interest to declare in relation to the content of this article.
Author's role/participation in the authorship
M.J.C. conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
J.P.H. conceptualized and designed the study, critically revised the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Ethical approval
N/A.
Funding
None.
Declaration of Competing Interest
None.
Acknowledgments
The authors would like to thank all survey participants for providing their valuable insights and experience of using virtual lectures during the COVID-19 pandemic.
References
- 1.Organization WH. Coronavirus disease (COVID-2019) situation reports. 2020. URL (accessed 08 March 2020): https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.2020.
- 2.New Cases of COVID-19 In World Countries. 2020; [Online]. Available at: https://coronavirus.jhu.edu/data/new-cases, 2020.
- 3.van Doremalen N, Bushmaker T, Morris DH. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fauci AS, Lane HC, Redfield RR. Covid-19 - navigating the uncharted. N Engl J Med. 2020;382(13):1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee A. Wuhan novel coronavirus (COVID-19): why global control is challenging? Public Health. 2020;179:A1–a2. doi: 10.1016/j.puhe.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CMS issues guidance for elective surgery; PPE conservation strategies. 2020; Available at: https://www.aha.org/news/headline/2020-03-19-cms-issues-guidance-elective-surgery-ppe-conservation-strategies. Accessed April 17, 2020
- 7.Luce EA. The future of plastic surgery resident education. Plast Reconstr Surg. 2016;137(3):1063–1070. doi: 10.1097/01.prs.0000479982.67922.8a. [DOI] [PubMed] [Google Scholar]
- 8.Larvin M. E-learning in surgical education and training. ANZ J Surg. 2009;79(3):133–137. doi: 10.1111/j.1445-2197.2008.04828.x. [DOI] [PubMed] [Google Scholar]
- 9.Khansa I, Janis JE. Maximizing technological resources in plastic surgery resident education. J Craniofacial Surg. 2015;26(8):2264–2269. doi: 10.1097/SCS.0000000000002198. [DOI] [PubMed] [Google Scholar]
- 10.Tang ET, Goh M, Goh R. International microsurgery club: an effective online collaboration system. J Reconstr Microsurg. 2020 doi: 10.1055/s-0040-1702158. [DOI] [PubMed] [Google Scholar]
- 11.Kwon SH, Goh R, Wang ZT. Tips for making a successful online microsurgery educational platform: the experience of international microsurgery club. Plast Reconstr Surg. 2019;143(1):221e–233e. doi: 10.1097/PRS.0000000000005109. [DOI] [PubMed] [Google Scholar]
- 12.Cho MJ, Furnas HJ, Rohrich RJ. A primer on social media use by young plastic surgeons. Plast Reconstr Surg. 2019;143(5):1533–1539. doi: 10.1097/PRS.0000000000005533. [DOI] [PubMed] [Google Scholar]
- 13.Cho M-J, Li A, Furnas H. Current trends in the use of social media by plastic surgeons. Plast Reconstr Surg. 2020;146(1):83e–91e. doi: 10.1097/PRS.0000000000006936. [DOI] [PubMed] [Google Scholar]
- 14.Free Virtual Grand Rounds Programming. 2020; Available at: https://acaplasticsurgeons.org/Resources/virtual-grand-rounds.cgi. Accessed April 18th, 2020.
- 15.Cho M-J, Hong JP. Plastic surgery education during the COVID-19 outbreak: leveling the playing field. Plast Reconstr Surg – Glob Open. 2020;8(5) doi: 10.1097/GOX.0000000000002925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham C.: Johns Hopkins engineers develop 3D-pritned ventilator splitters. 2020; Available at: https://hub.jhu.edu/2020/04/02/3d-printed-ventilator-splitters-for-covid-19/. Accessed April 18, 2020.
- 17.Watson I, Jeong S.: South korea pioneers coronavirus drive-through testing station. 2020; Available at: https://www.cnn.com/2020/03/02/asia/coronavirus-drive-through-south-korea-hnk-intl/index.html. Accessed April 18, 2020.
- 18.Iyer P, Aziz K, Ojcius DM. Impact of COVID-19 on dental education in the united states. J Dent Educ. 2020 doi: 10.1002/jdd.12163. [DOI] [PubMed] [Google Scholar]
- 19.Ahmed H, Allaf M, Elghazaly H. COVID-19 and medical education. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mousa AY, Broce M. The impact of COVID-19 on vascular training. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waltzman JT, Tadisina KK, Zins JE. The rise of technology in plastic surgery education: is the textbook dead on arrival (DOA)? Aesthet Surg J. 2016;36(2):237–243. doi: 10.1093/asj/sjv144. [DOI] [PubMed] [Google Scholar]
- 22.Kircher MF, Hines-Peralta A, Boiselle PM. Implementation of screen-capture video recordings of resident conferences in an academic radiology department: pilot experience. Acad Radiol. 2010;17(2):255–263. doi: 10.1016/j.acra.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 23.Bond S.: A must for millions, zoom has a dark side — and an FBI warning. 2020; https://www.npr.org/2020/04/03/826129520/a-must-for-millions-zoom-has-a-dark-side-and-an-fbi-warning. Accessed April 18, 2020.
- 24.Andolfi C, Gundeti MS. Live-case demonstrations in pediatric urology: ethics, patient safety, and clinical outcomes from an 8-year institutional experience. Investig Clin Urol. 2020;61(Suppl 1):S51–s56. doi: 10.4111/icu.2020.61.S1.S51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kallmes DF, Cloft HJ, Molyneux A. Live case demonstrations: patient safety, ethics, consent, and conflicts. Lancet (London, England) 2011;377(9776):1539–1541. doi: 10.1016/S0140-6736(11)60357-7. [DOI] [PubMed] [Google Scholar]
- 26.Seeburger J, Diegeler A, Dossche K. Live broadcasting in cardiac surgery does not increase the operative risk. Eur J Cardio-Thorac Surg : Off J Euro Assoc Cardio-thorac Surg. 2011;40(2):367–371. doi: 10.1016/j.ejcts.2010.11.069. [DOI] [PubMed] [Google Scholar]