Abstract
Purpose
The COVID-19 pandemic restrictions had negative impact on the psychopathology of people with Eating Disorders (EDs). Factors involved in the vulnerability to stressful events have been under-investigated in this population. We aimed to assess which factors contributed to COVID-19-induced worsening in both general and specific psychopathology.
Methods
Three-hundred and twelve people with a clinically defined diagnosis of an ED and undergoing a specialist ED treatment in different Italian ED services before the spreading of COVID-19 pandemic filled in an online survey. ED specific and general psychopathology changes after COVID-19 quarantine were retrospectively evaluated. Factors related to COVID-19 concerns (financial condition, fear of contagion, perceived social isolation/support, satisfaction in peer, family or sentimental relationships), illness duration and treatment-related variables (type of treatment provided, type of access to care, satisfaction with therapeutic relationships) were included as predicting factors in a structural equational model, which included latent variables consisting of general and ED psychopathology items as outcomes.
Results
A perceived low quality of therapeutic relationships, fear of contagion and increased isolation were positively associated with psychopathology worsening. Reduced satisfaction with family and with friends’ relationships and reduced perceived social support were associated with ED and general symptoms deterioration, respectively. No significant effect emerged for intimate relationships, illness duration, economic condition and type of treatment.
Conclusions
This study provides a comprehensive evaluation of clinical variables associated with psychopathological changes during the COVID-19 lockdown period highlighting potential risk and resilience factors and, possibly, informing treatment as well as prevention strategies for EDs.
Level of evidence IV
Evidence obtained from multiple time series analysis such as case studies
Keywords: Eating disorders, COVID-19, Risk factors, Vulnerability, Resilience, Psychopathology
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has seriously affected people’s mental health. Although general population has reported increased levels of stress, anxiety, depression and worries [1–3], populations with a prior psychiatric condition showed higher vulnerability in terms of physical and mental health [4–6]. Data from past similar outbreaks (i.e. SARS or Ebola) also suggested long-lasting effects of pandemics on psychopathology in psychiatric patients [7].
Several studies have documented the effects of the current COVID-19 pandemic on people with Eating Disorders (EDs). Termorshuizen et al. [8] showed increased eating restriction in people with anorexia nervosa (AN) and more frequent binge-eating episodes in those with bulimia nervosa (BN) or binge-eating disorder (BED). Consistently, more severe ED core symptoms since the emergence of pandemic were found in a population with a past self-reported history of ED [9], in people with a current diagnosis of AN or BN [10] and in subjects with current BN [11]. In our recent multicentre study (Monteleone et al. submitted) the worsening of ED specific psychopathology induced by confinement was confirmed together with a marked impairment in general psychopathology. Moreover, we documented also a persistence of the general psychopathology worsening after the end of the lock-down period and highlighted the emergent role of internalizing symptoms in ED people (Monteleone et al. submitted). These findings point to the COVID-19 pandemic as a traumatic event, which disrupted the mental health of people with EDs.
Rodgers et al. [12] hypothesized that the observed worsening of ED symptoms during the COVID-19 pandemic may be promoted by restriction of daily activities and movements, exposure to social media and emotional distress. In the general population the impact of COVID-19 restrictions on psychopathology was predicted by low educational levels, high fear of contagion, high punishment sensitivity and insecure attachment experiences [13–15]. To the best of our knowledge, only two studies have assessed risk factors that may contribute to the vulnerability of people with EDs to the impact of COVID-19 pandemic. Castellini et al. [10] found that COVID-related factors, such as household arguments and fear for the safety of loved ones, were significant positive predictors of eating symptoms while individual related measures, such as insecure attachment and childhood trauma experiences, were positively associated with post-traumatic symptoms during quarantine. In another study [16], low self-directedness negatively predicted COVID-19-induced eating symptoms deterioration. However, some putative risk factors related to the COVID-19 pandemic were not taken into account in those works, which were also affected by their low sample size. Indeed, a wide body of literature has pointed to the perception of social support, socio-economic condition or illness and treatment-related variables [17, 18] as potential risk factors affecting the ability to cope with stressful events in people with psychiatric disorders. In people with EDs, interpersonal sensitivity, familiar conflicts, emotion regulation abilities, childhood sexual abuse and teasing experiences have been recognized as general risk factors for impaired capacity to cope with stressful situations [19–22]. Furthermore, the post-traumatic nature of ED psychopathology has been suggested by both review [23] and recent network studies [24, 25]. However, as highlighted by Glashouwer et al. [26], there is a need to identify factors promoting vulnerability or resilience in response to stressful conditions through experimental studies. The exposure to the COVID-19 lock-down represents an ideal condition to reproduce a stressful condition and to investigate which factors affect the response to such a severe acute stressor. Thus, in the present study we aimed to investigate potential risk factors associated with ED specific and general psychopathology worsening during the COVID-19 lock-down. In line with literature suggestions [10, 16, 19, 22] and in order to provide a more comprehensive evaluation than those drawn in previous studies [10, 16], different elements contributing to the stressful experience of the COVID-19 lockdown period (such as socio-economic condition, fear of contagion, isolation, satisfaction with family, friends or intimate relationships and perceived social support) as well as factors associated with illness (illness duration) and treatment (type of treatment and perceived therapeutic relationships during quarantine) were investigated. The latter variables were included in the model in the light of the effects of illness duration and treatment on the course of ED psychopathology [27, 28]. No previous study has assessed the independent contribution of each variable included in our model. Given the exploratory nature of our study, we had no a priori hypothesis.
Methods
Participants
Patients who were in charge of different Italian ED services were invited to take part into an anonymous online survey. The study was introduced as aiming to assess whether patients’ psychopathology changed during the COVID-19 lockdown period and whether factors associated with the COVID-19 restrictions affected the course of symptoms. Patients were invited through an email advertising or during the clinical examination. They were diagnosed with AN or atypical AN, BN, BED or Other Specified Feeding or Eating Disorders (OSFED) according to Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5) criteria. The diagnosis was made through face to face clinical interviews provided by expert clinical psychiatrists in each ED unit. Patients had started specialized treatments for EDs before the COVID-19 lockdown. Inclusion criteria for the presented study were the following: (a) no comorbid schizophrenia or bipolar disorder; (b) no intellectual disability; (c) absence of severe medical conditions not related to the ED condition. Participants were invited to complete the online survey at the end of the COVID-19 confinement period, between June 1st 2020 and June 21st 2020. The Italian government declared the end of the lockdown period, the so-called Phase 1 of lockdown itself, on May 4th 2020.
The Ethics approval was not required for this kind of survey as per local legislation and national guidelines.
Design and measures
The online survey was designed to assess the impact of restrictions induced by the COVID-19 pandemic on the mental health of people suffering from EDs. In order to keep the survey anonymous and to avoid self-reported diagnoses, four different survey data collectors (one for each main ED diagnosis) were developed. Given that local investigators were aware of the current ED diagnosis of patients followed at their ED service, they sent them an email including a hyperlink to the survey from the data collector of the corresponding ED diagnosis. Patients were obliged to answer all the survey questions; otherwise, they could not complete the survey. In this way no missing data could result.
Participants had to rate each psychopathological item three times referring their responses to three different time periods: (1) two weeks before the spread of COVID-19 pandemic restrictions, “T0” (that in Italy started at the end of February 2020); (2) the confinement period or “Phase 1”, “T1” (that in Italy lasted between the beginning of March and the end of April 2020); (3) two weeks after the end of lockdown or “Phase 2”, “T2” that in Italy was gradually declared starting from the 4th of May 2020).
The online survey included information on participants’ socio-demographic characteristics (age, gender identity, geographic location [Italian Region], ethnicity, marital status, housing condition, employment status). Participants had to report variations in different areas of daily living and impact of lockdown on study/work, financial condition, physical health condition, fear of contagion, perceived social isolation/support, satisfaction in peer, family or sentimental relationships. Furthermore, information related to the impact of lockdown on current treatment (type of treatment provided, type of access to care, satisfaction with therapeutic relationship) were included. Types of provided treatment were psychotherapy, nutritional counselling, pharmacotherapy or a combination of psychotherapy with other treatments. Given that psychotherapy is considered the first line approach in EDs (NICE 2017), we categorized the access to treatment as a dichotomous variable consisting of the following`: a) psychotherapy with or without other treatments, or b) nutritional counselling with or without pharmacotherapy.
General psychopathology was investigated by means of questions derived from the following standardized and validated questionnaires: Generalized Anxiety Disorder 7 (i.e., “how often have you been bothered by feeling nervous, anxious, or on edge”) [29], Patient Health Questionnaire 9 (i.e., “how often have you been feeling down, depressed, or hopeless”) [30], PTSD Checklist for DSM-5 (i.e., “related to a stressful life experience, how much have you been bothered by avoiding memories, thoughts, or feelings related to the stressful experience, and/or avoiding external reminders of the stressful experience”) [31] and Obsessive–Compulsive Inventory (i.e., “how much have you been bothered by unpleasant thoughts that come into your mind against your will and you cannot get rid of them”) [32]. Items selected from these questionnaires were those referring to the DSM-5 criteria of each Axis I mental disorder. Anxiety, depression, obsessive–compulsive (OC) symptoms, panic symptoms, post-traumatic stress (PTS) symptoms, insomnia and stress were investigated. Questions related to specific ED psychopathology were derived from the Eating Disorders Inventory (EDI-2) (i.e., “have you been satisfied with your body shape”) [33]. One item representative of each EDI-2 subscale was included in the survey. Furthermore, participants were asked to report the amount (number of daily hours) of physical exercise. General psychopathological items were rated on a 10-point scale (0: not at all, 10: maximum) while ED specific psychopathological items were rated on a 6-point scale, which was consistent with the original version of the EDI-2 [33].
Statistical analyses
For the purpose of the present study, we did not take into account data referring to T2. In order to evaluate if socio-demographic and clinical variables changed between T0 and T1 according to the ED diagnosis (AN or other EDs), a two-way ANOVA for repeated measures was run for those variables that were measured at T0 and T1. T-test for independent samples or chi-square test were performed to compare variables assessed only at T1 between the two study groups. Given the low number of participants with an ED diagnosis different from AN or atypical AN, people with BN, with BED or with OSFED were merged in a unique group.
Structural equational modelling (SEM) was employed to assess whether the change in risk factors associated with COVID-19 confinement (economic condition, fear of contagion, isolation, satisfaction with family, friends or intimate relationships and perceived social support), illness duration or treatment related variables (type of treatment and therapeutic relationship at T1) were associated with the worsening of general psychopathology and eating-related psychopathology. SEM can be interpreted as a set of simultaneous multiple regression equations, in which variables can serve as predictors or outcomes. They allow to statistically test the hypothesized model through a simultaneous analysis of the entire system of variables and determining the extent to which it is consistent with the data [34]. If goodness-of-fit is adequate, the model suggests the plausibility of hypothesized relations between variables [34]. These relations can be graphically represented to enable a clearer conceptualization of the model. Furthermore, SEM allowed to use latent variables: this is appropriate when observed measures are presumed to represent an underlying construct [34]. Indeed, they allow a reduction of the measurement error and a more accurate estimation of the true value of the construct than it would be possible using a single variable [35]. Worsening in general psychopathology and in eating-related psychopathology were defined as the latent variables, which allow us to account for covariation among the included manifested variables. We did not include risk factors in a latent variable in order to investigate the specific relationships between each observed risk variable and symptoms worsening. General psychopathology latent variable included the difference between T0 and T1 scores of depression, anxiety, post-traumatic stress symptoms, obsessive–compulsive symptoms and insomnia. The eating-related psychopathology latent variable included the difference between T0 and T1 scores of ineffectiveness, body satisfaction, social security, purging behaviors and impulsivity. Psychopathology variables which did not show significant difference between T0 and T1 (drive to thinness, perfectionism, interoceptive awareness, ascetism, binge eating and physical activity dimensions) (Monteleone et al. submitted) were not included in the latent variables.
The model was evaluated using the MLM method [36]. To assess the adequacy of the model, the criteria of goodness of fit indices were the following: a non-significant chi-square (χ2), chi-square/degrees of freedom (χ2/d.f.) values < 2, comparative fit index (CFI) and Tucker-Lewis Index (TLI) values > 0.95, and standardized root-mean-square residual (SRMR) values < 0.08, root-mean-square error of approximation (RMSEA) values < 0.06 [37].
SEM was performed through R, version 3.4.4 (R core Team, Vienna, Austria), using lavaan package version 0.6–5 [38].
Results
Characteristics of the study sample
Three hundred and twelve people with EDs completed the survey. Three hundred reported themselves as female, 11 as male and 1 as non-binary. Participants into the study were as follows: 171 from Northern Italy, 49 from Central Italy and 92 from Southern Italy. The study sample included 179 participants (57.4% of the sample) with current AN or atypical AN, 63 (20.2% of the sample) with current BN, 48 (15.4% of the sample) with current BED and 22 (7.05% of the sample) with current OSFED.
Demographic characteristics of the study population already reported in our previous study (Monteleone et al., submitted) are summarized in Table 1.
Table 1.
Demographic characteristics of the participants during the COVID-19 confinement period expressed as mean ± sd or frequency
| AN | Other EDs | ||
|---|---|---|---|
| Age | 26.92 ± 10.28 | 32.24 ± 13.53 | t = − 3.94; p < 0.001 |
| Illness Duration | 8.95 ± 8.48 | 10.35 ± 10.30 | t = − 2.05; p = 0.06 |
| Paid Job, yes (%) | 47 (26) | 52 (39) | χ2 = 5.80; p = 0.01 |
| Student, yes (%) | 100 (56) | 65 (49) | χ2 = 1.49; p = 0.22 |
| Marital status, n (%) | χ2 = 8.34; p = 0.01 | ||
| Single | 144 (80) | 88 (66) | |
| Married or cohabit | 30 (17) | 37 (28) | |
| Divorced | 5 (3) | 8 (6) | |
| Housing condition, n (%) | χ2 = 0.73; p = 0.39 | ||
| Alone | 46 (26) | 40 (30) | |
| With family | 133 (74) | 93 (70) | |
|
COVID-19 Diagnosis, yes (%) Patient |
4 (2) | 8 (6) | χ2 = 2.95; p = 0.09 |
| COVID-19 Diagnosis, yes (%) | χ2 = 0.11; p = 0.74 | ||
| Family member | 21 (12) | 14 (11) | |
| Economic change | 3.39 ± 2.98 | 3.81 ± 2.96 | t = − 1.22; p = 0.22 |
| Fear of contagion | 3.31 ± 3.37 | 3.96 ± 3.15 | t = − 1.74; p = 0.08 |
| Direct access to care, yes (%) | 127 (71) | 78 (59) | χ2 = 5.12; p = 0.02 |
| Type of treatment provided, Psychotherapy, yes | 135 | 90 | χ2 = 2.28; p = 0.13 |
| Therapeutic relationship during “phase 1” | 6.01 ± 2.87 | 5.24 ± 3.06 | t = 2.08; p = 0.06 |
AN Anorexia Nervosa, ED Eating Disorder
Comparison of clinical variables
Changes in general and ED psychopathological variables were reported in our previous study (Monteleone et al. submitted), which found a significant worsening of both general and ED-specific symptoms (excepted for items related to drive to thinness, perfectionism, interoceptive awareness, asceticism, binge eating and physical activity dimensions) from T0 to T1.
Two-way ANOVA for repeated measures showed significant effects of time for all the assessed risk factors. Indeed, risk factors significantly worsened between T0 and T1 (Table 2), revealing that they were negatively affected by the COVID-19 pandemic confinement. Time x diagnosis interaction was not significant: thus, the risk factor worsening was not influenced by the ED diagnosis (Table 2). A significant effect of diagnosis was shown only for isolation (F1,310 = 6.5; p = 0.01): people with AN exhibited heightened social isolation in comparison to those with other EDs at both T0 and T1 (Table 2).
Table 2.
Clinical characteristics of the participants before the spread of COVID-19 pandemic restrictions (T0) and during the confinement period (T1) expressed as mean ± sd
| T0 (mean ± SD) |
T1 (mean ± SD) |
ANOVA | |||
|---|---|---|---|---|---|
| AN | Other EDs | AN | Other EDs | ||
| Isolation | 4.17 ± 3.10 | 3.41 ± 2.67 | 7.21 ± 2.82 | 6.57 ± 3.04 | Time: F1.310 = 265.12; p < 0.001 |
| Diagnosis: F1.310 = 6.5; p = 0.01 | |||||
| TimexDiagnosis: F1.310 = 0.097; p = 0.75 | |||||
| Satisfaction with family relationships | 5.84 ± 2.40 | 5.53 ± 2.49 | 5.54 ± 2.65 | 5.15 ± 2.67 | Time: F1.310 = 6.44; p = 0.01 |
| Diagnosis: F1.310 = 1.82; p = 0.18 | |||||
| TimexDiagnosis: F1.310 = 0.09; p = 0.76 | |||||
| Satisfaction with friends’ relationships | 5.45 ± 2.80 | 6.11 ± 2.38 | 4.08 ± 2.77 | 4.27 ± 2.43 | Time: F1.310 = 110.7; p < 0.001 |
| Diagnosis: F1.310 = 2.74; p = 0.099 | |||||
| TimexDiagnosis: F1.310 = 2.27; p = 0.132 | |||||
| Satisfaction with sentimental relationships | 3.58 ± 3.61 | 4.45 ± 3.38 | 2.99 ± 3.35 | 3.48 ± 3.38 | Time: F1.310 = 38.87; p < 0.001 |
| Diagnosis: F1.310 = 3.32; p = 0.069 | |||||
| TimexDiagnosis: F1.310 = 2.29; p = 0.131 | |||||
| Entrusting others | 5.51 ± 2.55 | 5.23 ± 2.70 | 4.64 ± 2.77 | 4.31 ± 2.89 | Time: F1.310 = 51.02; p < 0.001 |
| Diagnosis: F1.310 = 1.12; p = 0.292 | |||||
| TimexDiagnosis: F1.310 = 0.02; p = 0.878 | |||||
AN Anorexia Nervosa, ED Eating Disorder
Structural equational modelling analysis
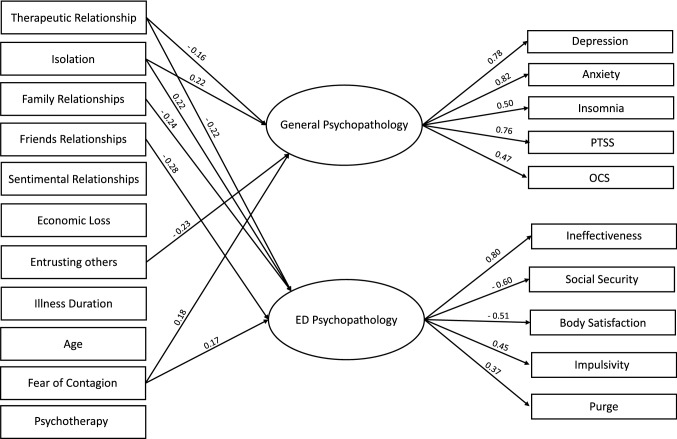
SEM is reported in Fig. 1. The model has good fit indices [χ2 = 140.21, d.f. 114, p = 0.06; robust TLI = 0.96; robust CFI = 0.97; RMSEA = 0.02; SRMR = 0.03], accounting for a total of 30% of the variance of worsening in general psychopathology and 45% of the variance of worsening in eating-related psychopathology.
Fig. 1.
SEM model representing the association between risk factors associated with COVID-19 confinement, illness duration or treatment related variables and the worsening in general psychopathology and eating-related psychopathology with standardized estimates
Significant negative effects of perceived therapeutic relationship quality at T1 were found on general psychopathology (β = − 0.16; se = 0.04; p = 0.007) and eating-related psychopathology worsening (β = − 0.22; se = 0.03; p = 0.001). Significant positive effects of heightened isolation and fear of contagion were found on general psychopathology worsening (β = 0.22; se = 0.04; p = 0.002 and β = 0.16; se = 0.03; p = 0.003, respectively) and eating-related psychopathology worsening (β = 0.22; se = 0.02; p = < 0.001 and β = 0.17; se = 0.02; p = 0.002, respectively). Significant negative effects of reduced satisfaction with family relationships and friends’ relationships were found only on eating-related psychopathology worsening (β = − 0.24; se = 0.07; p < 0.001; β = − 0.27; se = 0.03; p < 0.001, respectively). Significant negative effect of reduced entrusting of others was found only on general psychopathology worsening (β = − 0.23; se = 0.06; p = 0.001). No effects of economic loss, illness duration, access to psychotherapy and satisfaction with sentimental relationships were found on the latent variables.
Discussion
The present study investigated putative risk factors associated with eating and general psychopathology impairment experienced by people with EDs during the lockdown due to the COVID-19 pandemic. A perceived low quality of therapeutic relationship, fear of contagion and increased isolation were the variables positively associated with both eating and general psychopathology worsening observed during COVID-19 induced confinement. Reduced satisfaction with family and friends’ relationships and reduced perceived social support were associated with ED and general symptoms’ deterioration, respectively. On the other hand, economic condition, illness duration, satisfaction with sentimental relationships and type of treatment provided were not associated with any psychopathology change during quarantine.
The innovative aspect of this study was the evaluation of symptoms and risk factors in terms of dimensional change between the COVID-19 lockdown and the previous period. Although the retrospective nature of our findings may limit their validity, the collection of data has been done at the end of the COVID-19 lockdown period, which in Italy lasted about 2 months. This implies that data were collected referring to a recently lasted period, thus possibly reducing recalling biases. Two previous studies [10, 16] have assessed the variables predicting eating and general psychopathology changes during the COVID-19 lockdown period in people undergoing treatment for an ED. As in our study, participants in those two previous studies were affected by different ED diagnoses and were recruited among those undergoing treatment for an ED before the COVID-19 pandemic onset. However, we conducted a multicentre investigation study, which included a number of participants markedly larger than those previous studies. Moreover, Baenas et al. [16] performed a structured equational model revealing that COVID-related concerns, anxiety, depression and less adaptive coping strategies to confinement situation significantly contributed to a latent variable, which was associated with ED symptom worsening and partially accounted for the association between low self-directedness and ED symptoms outcome. Differently with that study, we assessed the contribution of manifested variables on psychopathological changes including also non COVID-related risk factors, such as illness duration, treatment and perceived quality or type of the therapeutic relationship during the COVID-19 lockdown period. Furthermore, unlike the previously conducted categorical assessment by Baenas et al. [16], we employed a dimensional scoring of study measures: this allowed us to explore COVID-19 related psychopathological changes correcting for baseline symptomatology. Castellini et al. [10] employed a different method of analysis to investigate longitudinal data and showed that insecure attachment (the anxious dimension in BN and the avoidant one in AN) and childhood traumatic experience significantly accounted for post-traumatic symptomatology during the COVID-19 lockdown period, while environmental factors (household arguments and fear of contagion) were associated with a higher increase in physical exercise and binge-eating. However, the use of linear mixed model investigation did not make possible to take into account the covariation between risk factors and between symptoms, as we did in the present study via the use of SEM.
The present findings corroborate the contribution of quality of family relationships and fear of contagion on psychopathological changes related to COVID-19 confinement [10, 16]. As a matter of fact, we identified the role of social support and social isolation as important risk factors for people with EDs. Indeed, the COVID-19 related worsening of satisfaction with family and friends’ relationships was associated with ED specific psychopathology worsening; the reduced support perceived in relationships was associated with general psychopathology worsening and the increased social isolation experience predicted the worsening of all psychopathological dimensions. These data possibly reflect the COVID-19 confinement-induced change in the social network of people with EDs consisting in reduced time spent with friends in favor of that with family. As suggested by literature studies [39, 40], familiar conflicts or the parents’ attempt to manage their son/daughter behaviors may exacerbate ED symptoms. Our findings are also consistent with literature studies assessing social difficulties through self-report measures [41, 42] or experimental tasks [43–45] and identifying this variable as a risk and maintaining factor for EDs. Across factors related to social functioning, only satisfaction with intimate relationships was not associated with symptoms change. This is not surprising given the largely consistent demonstration of difficulties or even the lack of intimate relationships in people with EDs [42, 46, 47].
This is the first study assessing the potential contribution of treatment-related factors to the COVID-19 related psychopathology changes. We found that not the type of treatment provided (nutritional counseling, pharmacological treatment versus psychotherapy or a combination of psychotherapy with these interventions) during the COVID-19 lockdown period but a higher quality of perceived therapeutic relationship was associated with a lower increase of psychopathology severity. These findings corroborate the importance of the therapeutic relationship which has been described as a non-specific factor significantly contributing to treatment outcome in EDs [48]. It is important to highlight that participants into this study were undergoing different types of treatments and that two-thirds of the sample had direct access to care during the COVID-19 lockdown, while the majority of the remaining sample was provided with a telehealth treatment. Hence, the present results may have been affected by the different types of treatment delivered in each ED service, although recent meta-analyses failed to identify outcome differences among evidence-based treatment for EDs [49, 50]. Finally, illness duration and economic condition were not found associated with the study outcomes. We may suggest that the response to COVID-19 confinement in people with EDs is not affected by these factors, although illness duration is an important factor promoting the progress of AN [28] and economic status was associated with psychopathology change during COVID-19 confinement in other psychiatric conditions [51, 52]. However, it is not possible to rule out that the self-report nature of these data collection affected the present findings.
Limitations of the present study need to be acknowledged. First of all, as mentioned above, the retrospective nature of data collection may have affected our findings and limit the possibility to infer causality from regression analyses of the SEM. Second, we have not assessed personality and individual-related measures (i.e., attachment and childhood adverse experiences), which can be related to the psychopathology change during COVID-19 confinement [10, 16]. Third, given the low number of participants with diagnosis different from AN, we did not account for possible differences between the main (AN, BN, BED and OSFED) ED diagnoses but only between AN and other diagnoses. This is an area that needs to be addressed by future studies, since also previous studies [10, 16] did not investigate ED diagnosis differences. Finally, a possible selection bias should be recognized given that it was not possible to verify whether patients who participated into the survey differed in their symptomatology from those who did not accept to take part into the study.
The main strengths of this study are the inclusion of a large number of participants with a face to face defined clinical diagnosis and the use of latent variables, which allows to consider for covariation between symptoms.
To conclude, this is the first study providing a comprehensive evaluation of clinical variables associated with ED specific and general psychopathology changes during the COVID-19 lockdown period, taking into account the levels of the assessed variables before the beginning of COVID-19 confinement. We highlighted potential vulnerability factors to the stress induced by the COVID-19 confinement, such as social isolation, family conflict and fear of contagion, as well as putative protective factors, such as the therapeutic relationship. These findings strengthen the need of further studies assessing risk and protective factors for EDs [21, 26]. Indeed, although the variables identified in our study are risk factors common to other psychiatric conditions, our findings support those ED pathogenetic models (i.e., the interpersonal model [53] or the cognitive-interpersonal maintenance model [54]) pointing to interpersonal sensitivity and socio-emotional processing as central variables promoting the maintenance of psychopathology.
Furthermore, the present study may inform treatment as well prevention strategies recently proposed [5, 55, 56] for people with EDs undergoing similar outbreaks or stressful periods. Indeed, our study findings may encourage clinicians to keep their care to ED patients, regardless of the type of the intervention (i.e., psychotherapy with or without other interventions) or the treatment delivering strategy (i.e., physical access to care or telehealth medicine). Indeed, the quality of perceived therapeutic relationships and not the type or the treatment delivering strategy was found as one of the most important protective factors towards psychopathology worsening. This is also consistent with the high relevance of social support as a risk factor during the confinement period, which suggests the need to target interpersonal problems relative to the reduced quality of peer relationships or to the burden of familiar conflicts. These recommendations could be taken into account by clinicians without differences across ED people with different age or illness duration.
What is already known on this subject?
Personality characteristics, fear of contagion and childhood attachment and traumatic experiences have been suggested as risk factors during the COVID-19 lockdown period in small samples with EDs. Studies are needed to assess further putative risk factors related to the COVID-19 pandemic in a more enlarged sample.
What does this study add?
Social isolation and perceived quality of therapeutic relationships are risk and protective factors for general and ED specific psychopathology worsening during the COVID-19 lockdown period. Treatment-related factors (type of intervention or treatment delivering strategy) as well as patients’ age, economic condition and illness duration are not associated with symptoms deterioration.
Acknowledgements
None.
Authors’ contributions
AMM, FM, GC and PM designed the study, wrote the protocol, and wrote the manuscript. GA-D, MB, MB, EB, SB, BC, GC, GC, SDG, AF, CG, EM, PM, FM, MGO, FP, MR, CAR, CR, VR, PS, EB, CS-G, PT, UV, PZ collected data. GC did statistical analyses. All authors read and approved the final manuscript
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Compliance with ethical standards
Ethics approval and consent to participate
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of University of Salerno who determined that our study did not need ethical approval.
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mowbray H. In Beijing, coronavirus 2019-nCoV has created a siege mentality. BMJ. 2020;368:m516. doi: 10.1136/bmj.m516. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Heal Med. 2020 doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- 4.De-Girolamo G, Cerveri G, Clerici M, Monzani E, Spinogatti F, Starace F, Tura G, Vita A. Mental health in the coronavirus disease 2019 emergency-The Italian response. JAMA Psychiatry. 2020;77:974–976. doi: 10.1001/jamapsychiatry.2020.1276. [DOI] [PubMed] [Google Scholar]
- 5.Fernández-Aranda F, Casas M, Claes L, Clark-Bryan D, Favaro A, Granero R, Gudiol C, Jiménez-Murcia S, Karwautz A, La Grange D, Menchòn JM, Tchanturia K, Treasure J. COVID-19 and implications for eating disorders. Eur Eat Disord Rev. 2020;28:239–245. doi: 10.1002/erv.2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry wps. 2020 doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS. Focus on Mental Health During the Coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12:e7405. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Termorshuizen JD, Watson HJ, Thornton LM, et al. Early impact of COVID-19 on individuals with self-reported eating disorders: a survey of ~1,000 individuals in the United States and the Netherlands. Int J Eat Disord Eat. 2020 doi: 10.1101/2020.05.28.20116301. [DOI] [PubMed] [Google Scholar]
- 9.Phillipou A, Meyer D, Neill E, Tan EJ, Toh WL, Van-Rheenen TE, Rossell SL. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int J Eat Disord. 2020;53:1158–1165. doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castellini G, Cassioli E, Rossi E, Innocenti M, Gironi V, Sanfilippo G, Felciai F, Monteleone AM, Ricca V. The impact of COVID-19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int J Eat Disord. 2020 doi: 10.1002/eat.23368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schlegl S, Meule A, Favreau M, Voderholzer U. Bulimia nervosa in times of the COVID-19 pandemic-Results from an online survey of former inpatients. Eur Eat Disord Rev. 2020 doi: 10.1002/erv.2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodgers RF, Lombardo C, Cerolini S, et al. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53:1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Özdin S, Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66:504–511. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bacon AM, Corr PJ. Coronavirus (COVID-19) in the United Kingdom: a personality-based perspective on concerns and intention to self-isolate. Br J Health Psychol. 2020 doi: 10.1111/bjhp.12423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moccia L, Janiri D, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baenas I, Caravaca-Sanz E, Granero R, Sanchez I, Riesco N, Testa G, Vintrò-Alcaraz C, Treasure J, Jiménez-Murcia S, Fernandéz-Aranda F. COVID-19 and eating disorders during confinement: analysis of factors associated with resilience and aggravation of symptoms. Eur Eat Disord Rev. 2020 doi: 10.1002/erv.2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gianaros PJ, Manuck SB. Neurobiological pathways linking socioeconomic position and health. Psychosom Med. 2010;72:450–461. doi: 10.1097/PSY.0b013e3181e1a23c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fava GA, Cosci F, Sonino N. Current Psychosomatic Practice. Psychother Psychosom. 2017;86:13–30. doi: 10.1159/000448856. [DOI] [PubMed] [Google Scholar]
- 19.Cardi V, Tchanturia K, Treasure J. Premorbid and illness-related social difficulties in eating disorders: an overview of the literature and treatment developments. Curr Neuropharmacol. 2018;16:1122–1130. doi: 10.2174/1570159X16666180118100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Culbert KM, Racine SE, Klump KL. Research Review: What we have learned about the causes of eating disorders—a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry Allied Discip. 2015;56:1141–1164. doi: 10.1111/jcpp.12441. [DOI] [PubMed] [Google Scholar]
- 21.Solmi M, Radua J, Stubbs B, Ricca V, Moretti D, Busatta D, Carvalho AF, Dragioti E, Favaro A, Monteleone AM, Shin JI, Fusar-Poli P, Castellini G. Risk factors for eating disorders: an umbrella review of published meta-analyses. Braz J Psychiatry. 2020 doi: 10.1590/1516-4446-2020-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Treasure J, Nazar BP. Interventions for the carers of patients with eating disorders. Curr Psychiatry Rep. 2016;18:1–7. doi: 10.1007/s11920-015-0652-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trottier K, MacDonald DE. Update on psychological trauma, other severe adverse experiences and eating disorders: state of the research and future research directions. Curr Psychiatry Rep. 2017;19:45. doi: 10.1007/s11920-017-0806-6. [DOI] [PubMed] [Google Scholar]
- 24.Vanzhula IA, Calebs B, Fewell L, Levinson CA. Illness pathways between eating disorder and post-traumatic stress disorder symptoms: Understanding comorbidity with network analysis. Eur Eat Disord Rev. 2019;27:147–160. doi: 10.1002/erv.2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monteleone AM, Mereu A, Cascino G, et al. Re-conceptualization of anorexia nervosa psychopathology: a network analysis study in adolescents with short duration of the illness. Int J Eat Disord. 2019;52:1263–1273. doi: 10.1002/eat.23137. [DOI] [PubMed] [Google Scholar]
- 26.Glashouwer KA, Brockmeyer T, Cardi V, et al. Time to make a change: a call for more experimental research on key mechanisms in anorexia nervosa. Eur Eat Disord Rev. 2020;28:361–367. doi: 10.1002/erv.2754. [DOI] [PubMed] [Google Scholar]
- 27.Murray SB, Loeb KL, Le Grange D. Treatment outcome reporting in anorexia nervosa: time for a paradigm shift? J Eating Disorders. 2018;6(1):10. doi: 10.1186/s40337-018-0195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Treasure J, Willmott D, Ambwani S, et al. Cognitive interpersonal model for anorexia nervosa revisited: the perpetuating factors that contribute to the development of the severe and enduring illness. J Clin Med. 2020;9:630. doi: 10.3390/jcm9030630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP (2013) The PTSD Checklist for DSM-5 (PCL-5) – Standard [Measurement instrument]. Available from https://www.ptsd.va.gov/
- 32.Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive-compulsive disorder scale: the obsessive-compulsive inventory. Psychol Assess. 1998;10:206–214. doi: 10.1037/1040-3590.10.3.206. [DOI] [Google Scholar]
- 33.Garner D (1991) Eating disorder inventory-2. Retrieved from http://www.dottorgianfrancodelorenzis.it/doc/questionari psicologici/EDI-2 protocollo.pdf
- 34.Byrne BM. Structural equation modeling with Mplus: Basic concepts, applications, and programming. New York: Routledge; 2013. [Google Scholar]
- 35.Galderisi S, Rossi A, Rocca P, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13:275–287. doi: 10.1002/wps.20167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.MacKinnon DP. Integrating mediators and moderators in research design. Res Soc Work Pract. 2011;21:675–681. doi: 10.1177/1049731511414148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weston R, Gore PA. A brief guide to structural equation modeling. Couns Psychol. 2006;34:719–751. doi: 10.1177/0011000006286345. [DOI] [Google Scholar]
- 38.Rosseel Y. Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA) J Stat Soft. 2012;48:1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- 39.Anastasiadou D, Medina-Pradas C, Sepulveda AR, Treasure J. A systematic review of family caregiving in eating disorders. Eat Behav. 2014;15:464–477. doi: 10.1016/j.eatbeh.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 40.Salerno L, Rhind C, Hibbs R, Micali N, Schmidt U, Gowers S, Macdonald P, Goddard E, Todd G, Lo Coco G, Treasure J. An examination of the impact of care giving styles (accommodation and skilful communication and support) on the one year outcome of adolescent anorexia nervosat the assumptions of the cognitive interpersonal model in anorexia nervosa. J Affect Disord. 2016;191:230–236. doi: 10.1016/j.jad.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 41.Arcelus J, Haslam M, Farrow C, Meyer C. The role of interpersonal functioning in the maintenance of eating psychopathology: A systematic review and testable model. Clin Psychol Rev. 2013;33:156–167. doi: 10.1016/J.CPR.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 42.Cardi V, Mallorqui-Bague N, Albano G, Monteleone AM, Fernandéz-Aranda F. Social difficulties as risk and maintaining factors in anorexia nervosa: a mixed-method investigation. Front Psychiatry. 2018;9:12. doi: 10.3389/fpsyt.2018.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monteleone AM, Treasure J, Kan C, Cardi V. Reactivity to interpersonal stress in patients with eating disorders: a systematic review and meta-analysis of studies using an experimental paradigm. Neurosci Biobehav Rev. 2018 doi: 10.1016/j.neubiorev.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 44.Monteleone AM, Cascino G, Ruzzi V, Pellegrino F, Carfagno M, Raia M, Del Giorno C, Monteleone P, Maj M. Multiple levels assessment of the RDoC “system for social process” in Eating Disorders: Biological, emotional and cognitive responses to the Trier Social Stress Test. J Psychiatr Res. 2020;130:160–166. doi: 10.1016/j.jpsychires.2020.07.039. [DOI] [PubMed] [Google Scholar]
- 45.Monteleone AM, Ruzzi V, Patriciello G, Cascino G, Pellegrino F, Vece A, Monteleone P, Maj M. Emotional reactivity and eating disorder related attitudes in response to the trier social stress test: an experimental study in people with anorexia nervosa and with bulimia nervosa. J Affect Disord. 2020;274:23–30. doi: 10.1016/j.jad.2020.05.051. [DOI] [PubMed] [Google Scholar]
- 46.Cassioli E, Rossi E, Castellini G, Sensi C, Mancini M, Lelli L, Monteleone AM, Ricca V, Stanghellini G. Sexuality, embodiment and attachment style in anorexia nervosa. Eat Weight Disord. 2019 doi: 10.1007/s40519-019-00805-6. [DOI] [PubMed] [Google Scholar]
- 47.Castellini G, Lelli L, Corsi E, Campone B, Ciampi E, Fisher A, Mallardo L, Monteleone AM, Rotella F, Tofani T, Vignozzi L, Zamponi F, Maggi M, Ricca V. Role of Sexuality in the Outcome of Anorexia Nervosa and Bulimia Nervosa: A 3-Year Follow-Up Study. Psychother. Psychosom. 2017;86:376–378. doi: 10.1159/000477176. [DOI] [PubMed] [Google Scholar]
- 48.Graves TA, Tabri N, Thompson-Brenner H, et al. A meta-analysis of the relation between therapeutic alliance and treatment outcome in eating disorders. Int J Eat Disord. 2017;50:323–340. doi: 10.1002/eat.22672. [DOI] [PubMed] [Google Scholar]
- 49.Zeeck A, Herpertz-Dahlmann B, Friederich HC, et al. Psychotherapeutic treatment for anorexia nervosa: a systematic review and network meta-analysis. Front Psychiatry. 2018;9:158. doi: 10.3389/fpsyt.2018.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grenon R, Carlucci S, Brugnera A, et al. Psychotherapy for eating disorders: a meta-analysis of direct comparisons. Psychother Res. 2018 doi: 10.1080/10503307.2018.1489162. [DOI] [PubMed] [Google Scholar]
- 51.Di Crosta A, Palumbo R, Marchetti D, Ceccato I, La Malva P, Maiella R, Cipi M, Roma P, Mammarella N, Verrocchio MC, Di Domenico A. Individual Differences, Economic Stability, and Fear of Contagion as Risk Factors for PTSD Symptoms in the COVID-19 Emergency. Front Psychol. 2020;11:2329. doi: 10.3389/fpsyg.2020.567367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Rheenen TE, Meyer D, Neill E, Philippou A, Tan EJ, Toh WL, Rossell SL. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J Affect Disord. 2020;275:69–77. doi: 10.1016/j.jad.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rieger E, Van Buren DJ, Bishop M, et al. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. Clin Psychol Rev. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 54.Treasure J, Schmidt U. The cognitive-interpersonal maintenance model of anorexia nervosa revisited: a summary of the evidence for cognitive, socio-emotional and interpersonal predisposing and perpetuating factors. J Eat Disord. 2013;1:13. doi: 10.1186/2050-2974-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weissman RS, Bauer S, Thomas JJ. Access to evidence-based care for eating disorders during the COVID-19 crisis. Int J Eat Disord. 2020;53:639–646. doi: 10.1002/eat.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Todisco P, Donini LM. Eating disorders and obesity (ED&O) in the COVID-19 storm. Eat Weight Disord. 2020;1:1. doi: 10.1007/s40519-020-00938-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.