Abstract
China is faced with heavy burdens caused by lung cancer, which has climbed to the top of both cancer incidence and mortality spectrums. The age-standardized rates of incidence and mortality have shown a trend of gradual up-trends in the last decades, while the crude rates rise much quickly due to the aging of population. Although the improvement in health care has contributed to better survival of lung cancer, its prognosis is still challenging. Apart from the common risk factors such as tobacco use, air pollution, and occupational hazards, some specific factors like Chinese-style cooking also have posed great threats to human health. In light of such national conditions, specific interventions should be conducted to curb the burden of lung cancer including smoking cessation, improvement of air quality, early detection and effective treatment of lung cancer.
Keywords: Burden of disease, China, lung cancer, risk factors, trend
Introduction
Lung cancer has posed a heavy burden of disease to global health. According to the GLOBOCAN 2018 estimates (1), lung cancer is the primary cause of new cancer cases (2,093,876) and deaths (1,761,007) worldwide, with an incidence rate of 27.4/100,000 (the age-standardized incidence rate by world standard population, ASIRW: 22.5/100,000) and mortality rate of 23.1/100,000 (the age-standardized mortality rate by world standard population, ASMRW: 18.6/100,000). China has the heaviest lung cancer burden, representing 36.98% of cases and 39.21% of deaths globally (2). Given the grim situation of lung cancer burden, the government has promulgated and promoted a series of policies and activities such as environmental improvement, emission limitation, smoking prohibition, and tobacco control. Thus, the purpose of this study is to describe the current burden of lung cancer and its temporary trend in China, report the distributions of major risk factors, and put forward several preventive suggestions.
Burden and its trends of lung cancer in China
Incidence of lung cancer
National Cancer Center of People’s Republic of China is in charge of the data collection, analysis, and publishing of national cancer statistics (3). Based on the reported data from 368 qualified cancer registries in China (4), lung cancer ranked the first in male cancer incidence spectrum (24.17%) and the second in females (15.02%), as breast cancer was the most common cancer (17.10%). As is shown in Table 1 , there were 787,000 new cases of lung cancer in China in 2015, accounting for 20.03% of all cancer cases. The crude incidence of lung cancer and the age-standardized incidence rates by Chinese standard population (ASIRC) were 57.26/100,000 and 35.96/100,000, respectively.
1. Incidence of lung cancer in China by gender and area*.
| Areas | New cases (×104) | Proportion (%) | Rank | Crude incidence (1/105) | ASIRC (1/105) |
| *, Source: Report by National Cancer Center of People’s Republic of China (4); ASIRC, the age-standardized incidence rates by Chinese standard population (China National Population Census, 2000). | |||||
| Nation wide | |||||
| Total | 78.7 | 20.03 | 1 | 57.26 | 35.96 |
| Male | 52.0 | 24.17 | 1 | 73.90 | 48.68 |
| Female | 26.7 | 15.02 | 2 | 39.78 | 23.77 |
| Urban areas | |||||
| Total | 46.0 | 19.56 | 1 | 59.68 | 36.07 |
| Male | 30.0 | 23.83 | 1 | 76.35 | 48.25 |
| Female | 16.0 | 14.64 | 2 | 42.31 | 24.44 |
| Rural areas | |||||
| Total | 32.7 | 20.74 | 1 | 54.16 | 35.77 |
| Male | 22.0 | 24.66 | 1 | 70.80 | 49.24 |
| Female | 10.7 | 15.62 | 1 | 36.51 | 22.82 |
Lung cancer incidence presented significant differences in genders and regional distributions. Lung cancer incidence in males (73.9/100,000) was about twice that of females (39.78/100,000). For both genders, the age-specific incidence remained at a low level before the age of 40 years and started to rise rapidly after that. The incidence spectrum of malignant tumors in urban and rural areas also varied in China. The ASIRC of urban (59.68/100,000) and rural areas (54.16/100,000) were similar, but the former was slightly higher.
According to the cancer registry annual report (5) compiled by National Cancer Center, the rates in the central and eastern regions were higher than those in the western region. Specifically, the highest lung cancer incidence was observed in northeast China and the lowest in northwest China. In all cases of lung cancer, 49.28% had an exact pathological classification. Adenocarcinoma accounted for over half of lung cancer (53.40%), followed by squamous cell carcinoma (30.24%) and small cell carcinoma (11.72%) (5). Moreover, only 25.59% of the cases reported specific subsites. Among that, nearly half were distributed in the upper lobe (48.01%), followed by the lower lobe (30.74%) and the middle lobe (11.90%).
Mortality of lung cancer
Lung cancer ranked the first in the cancer death spectrum of China for both genders (male: 29.26%, female: 22.96%) and combined. In 2015, 631,000 new lung cancer deaths were reported in China, accounting for 26.99% of all cancer deaths (4). As is shown in Table 2 , the crude mortality from lung cancer was 45.87/100,000, whereas the mortality showed obvious decrease after adjusted by age, and the age-standardized mortality rate by Chinese standard population (ASMRC) was 28.16/100,000. Consistent with the incidence, lung cancer mortality in Chinese males (61.52/100,000) was significantly higher than that in females (29.43/100,000), and the gap enlarged in the age group over 40 years old. The age-standardized mortality in rural areas was a little higher than that in urban areas (28.44/100,000 and 27.93/100,000, respectively). Similarly, the lung cancer mortality in the eastern and central regions was close and higher than that in the western region. Moreover, the highest lung cancer mortality was observed in northeast China and the lowest in northwest China (5).
2. Mortality of lung cancer in China by gender and area*.
| Areas | Death (×104) | Proportion (%) | Rank | Crude incidence (1/105) | ASMRC (1/105) |
| *, Source: Report by National Cancer Center of People’s Republic of China (4); ASMRC, the age-standardized mortality rates by Chinese standard population (China National Population Census, 2000). | |||||
| Nation wide | |||||
| Total | 63.1 | 26.99 | 1 | 45.87 | 28.16 |
| Male | 43.3 | 29.26 | 1 | 61.52 | 40.15 |
| Female | 19.7 | 22.96 | 1 | 29.43 | 16.77 |
| Urban areas | |||||
| Total | 36.6 | 27.50 | 1 | 47.45 | 27.93 |
| Male | 25.1 | 30.06 | 1 | 63.68 | 39.81 |
| Female | 11.5 | 23.19 | 1 | 30.53 | 16.66 |
| Rural areas | |||||
| Total | 26.5 | 26.34 | 1 | 43.58 | 28.44 |
| Male | 18.3 | 28.42 | 1 | 58.79 | 40.56 |
| Female | 8.2 | 22.65 | 1 | 28.00 | 16.91 |
Trends of lung cancer incidence
The Global Burden of Disease (GBD) study is the most comprehensive worldwide observational epidemiological study to date, led by the Institute for Health Metrics and Evaluation (IHME). Based on estimates by GBD study (6), the crude incidence of lung cancer in China was increasing significantly from 1990 to 2019, regardless of gender. However, the ASIRW has levelled off in recent years (Figure 1 ). Zhang et al. (7) also found that lung cancer incidence in China increased dramatically for both genders based on data from 22 cancer registries in China from 2000 to 2014, but the extent of rising decreased after age standardization.
1.
Trends of lung cancer incidence in China between 1990 and 2019 for male, female and combined. Data were extracted from the GBD study (Available online: http://ghdx.healthdata.org/gbdresults-tool). The age-standardized rates were calculated by using the GBD world population age standard. GBD, Global Burden of Disease.
The change trends of lung cancer incidence varied by sex. It is reported that both crude incidence and ASIRC in females were on the rise with different degrees, with an average annual percent change (AAPC) of 4.5% [95% confidence interval (95% CI): 4.1%−5.0%] and 1.4% (95% CI: 1.0%−1.9%), respectively, whereas ASIRC among males decreased from 48.43/100,000 in 2000 to 46.85/100,000 in 2014 (7). Furthermore, AAPC of lung cancer incidence of rural areas in China was 1.76 times that of urban areas, which were 5.8% and 3.3%, respectively. Conversely, there was no significant change in age-standardized incidence in urban areas, and the overall incidence in male declined (7). Liu et al. reported similar trends by analysis of lung cancer incidence between 2008 and 2012 (8).
As for histological subtypes, in general, the proportion of adenocarcinoma increased significantly and has become the primary subtype, while the proportion of squamous cell carcinoma dropped gradually (9-12). However, no consistent changes were observed in surveys conducted in other areas (13,14).
The decrease on lung cancer incidence among males suggests that previous interventions to control male-related risk factors may be proved effective in some way, such as changes in smoking rate and cigarette types. And more attention should be paid to risk factors among females, mainly exposure to secondhand smoke and indoor combustion products. However, although the lung cancer incidence of both genders increased with age in all age groups, there was no noticeable change in each age group from 2000 to 2014 (7), suggesting that population aging is likely to contribute to the lung cancer burden. The regional differences may be associated with stronger controls and higher levels of policy enforcement in urban areas. Considering that the main histological subtype distinguished from gender, the inconsistency of the existing studies is likely due to the regional differences in gender composition or smoking rates, as well as the variation between their sample sizes and reporting years.
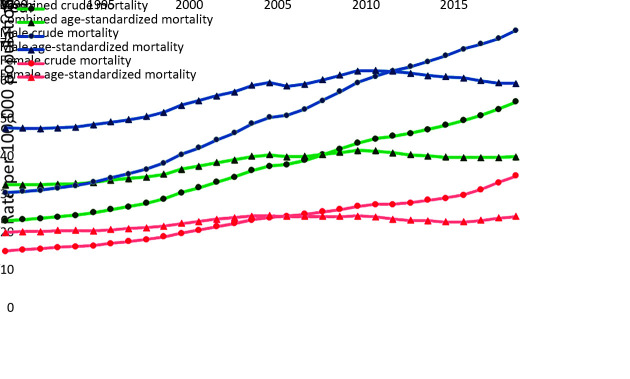
Trends of lung cancer mortality
Lung cancer is one of the malignancies with the fastest increase in mortality in the last decades, and has become the leading cancer-related deaths. Figure 2 shows the trends of lung cancer mortality in China from 1990 to 2019, based on estimates by GBD study (6). To sum up, the crude mortality stayed relatively constant in the last century and showed an obvious increased trend in the latest two decades. The age-standardized mortality was also generally on an upward trend during 1990−2019, but has shown a decline trend since 2005. In fact, lung cancer has risen to the top of the death spectrum of malignant tumors in many regions of China (15,16). However, analysis based on cancer registry data pointed out there was no apparent upward trend or a significant change in lung cancer mortality (8,17).
2.
Trends of lung cancer mortality in China between 1990 and 2019 for male, female and combined. Data were extracted from the GBD study (Available online: http://ghdx.healthdata.org/gbdresults-tool). The age-standardized rates were calculated by using the GBD world population age standard. GBD, Global Burden of Disease.
To be specific, lung cancer mortality showed an increasing trend in males and females, and the annual percent change (APC) of female mortality was higher, which led to a decrease in the mortality ratio between genders (17). As for age-specific mortality, a downward trend has been observed among those under the age of 35 years, while lung cancer mortality of those at the age of 65 years and over has shown an upward trend (18). The reported trends in mortality of age group of 35−65 years were not consistent (19,20). From the perspective of regional distribution, Cen et al. (21) found that the age-standardized lung cancer mortality in urban areas declined from 1990 to 2017 with AAPC of −0.36%, whereas the lung cancer mortality in rural regions during the same period increased significantly. Similar findings based on cancer registry data were also given by Xin et al. (17), showing that the gap narrowed due to different trends, although the lung cancer mortality stayed substantially higher in urban areas than in rural areas. Nevertheless, Zhang et al. (18) reported an opposite trend.
As for the inconsistent trends reported by studies, one possible reason is that lung cancer mortality in China has fluctuated up and down in different degrees over several decades with the changes of risk and prevention factors, so various results were observed in different periods. Differences in the regions covered by the survey can also partly explain the inconsistency. Besides, the gap between the crude and adjusted rate was also in favor of the possible influence of population aging on the burden of lung cancer. Given distinctions among changes of each age group, decline in young people is probably a benefit of both improving medical technology and adopting of a three-early strategy (early detection, early diagnosis, and early treatment). Moreover, since older patients are more likely to be diagnosed with advanced cancer, the circumstances remain serious. A research (15) pointed out that the increase in lung cancer deaths was mainly caused by non-population factors, accounting for 70.00% of the total increase. Thus, the fact that lung cancer mortality has no distinct decline among middle-aged Chinese males can mainly ascribe to the steadily high smoking rates.
Survival and its trends of lung cancer in China
The overall 5-year survival rate of cancer patients in China was about 40.5%, significantly higher than that of lung cancer (19.7%), showing a comparatively poor prognosis among all cancers (22). Median survival time was generally less than 2 years (23-26). The 5-year survival rate of patients with lung cancer decreased with age at diagnosis. In addition, survival in females (25.1%) was better than males (16.8%) (22), which is likely to be related to their physiological characteristics (e.g., hormone levels), healthier lifestyles and less exposure to occupational hazards (26-28). However, some studies have conflicting opinions (29,30), pointing out that the exact effect of gender and age on lung cancer survival is still controversial. It is also found that the survival rate of urban residents was higher than those in rural areas because the former tended to have higher health awareness and better access to health services (31).
The survival may differ between each histological subtype. The prognosis of squamous carcinoma is the best, followed by adenocarcinoma with a high recurrence rate and prone to distant metastasis, and small cell carcinoma has the worst prognosis (24,26,32,33). However, other studies (34) did not find significant differences in survival among the above histological subtypes. Treatment is also an important factor for lung cancer survival. The survival rate of patients with low differentiation degree of lung cancer (stage I) was higher than those with other stage transitions (24,26,35). Furthermore, the survival of patients undergoing surgery was significantly improved (35), which may also be associated with the generally low stage.
According to the analysis conducted by Zeng et al. (22), the age-standardized 5-year relative survival of lung cancer increased from 16.1% (95% CI, 15.6−16.6) in 2003−2005 to 19.7% (95% CI, 19.3−20.1) in 2012−2015, with an APC of 1.3% (95% CI, −0.8−3.5). In both urban and rural areas of China, upward trends of lung cancer survival were observed, from 19.5% to 23.8% in urban areas and from 11.2% to 15.4% in rural areas, respectively. Similar trends were also observed in both genders, and the increase significantly accelerated after the 1990s (23,26). Such favorable results may be contributed by the continuous improvement of medical technology and adopting strategies for early detection and cancer treatment. For example, Asian populations have been found to have a higher proportion of epidermal growth factor receptor mutations and are more likely to benefit from the targeted drug, such as Gefitinib and Erlotinib (36). Therefore, research and development of targeted therapies may have made great contributions to higher survival.
Main risk factors of lung cancer and distributions in China
Tobacco use
Tobacco use is one of the major threats to public health, especially in China (37). It is estimated that 366,980 deaths (26.4%) in males and 32,510 deaths (4.0%) in females are attributable to smoking, and ever-smoking contributed to approximately 42.7% of lung cancer deaths (38). China is the largest producer and consumer of tobacco, as well as the most severe victim (39,40). Thus, Chinese government has made efforts to curb tobacco epidemic, including signing of World Health Organization (WHO) Framework Convention on Tobacco Control, developing a range of anti-smoking policies, and carrying out tobacco control activities. However, the situation of tobacco control in China is still not optimistic, particular in northern and northeastern China (41).
Since the last century, there have been several National Tobacco Epidemic Surveys (39,42-45), reporting that the current smokers were over 300 million in 2002, and still increased. Although the overall smoking rate shows a downward trend from 1996 to 2018, the current rate remains high in China, which falls short of the target rate in Health China 2030 and other plans. Furthermore, WHO reported that the western Pacific region (where China is located) was expected to experience the slowest decline between 2010 and 2025 and would soon replace South-East Asia as the region with the highest average smoking rate (46).
Moreover, teenagers are an important reserve for smokers. The smoking rate of Chinese youth aged 15−24 years has increased significantly in recent years, with more than half of young daily smokers (20−34 years old) turning to heavy smokers before the age of 20 years, so it is particularly important to monitor tobacco use among the teenagers (44). The latest nationwide surveys (47,48) found that both the proportion of junior high school students trying cigarette smoking and the current smoking rate have declined in the past five years, while more students have heard about or even tried electronic cigarette, probably owing to the curiosity about new things. Besides, lower prices and greater access to tobacco advertising pose new challenges to teen smoking control.
Exposure to secondhand (passive) smoke is also a matter of concern. Almost 70% of Chinese adults were exposed to secondhand smoke (39,42-45) and nearly 60,000 lung cancer deaths (8%) in China each year were linked to secondhand smoking (6). Higher passive smoking rates are reported even in places where smoking is explicitly prohibited, such as public transport and indoor public places. Regardless of improvements in household secondhand smoke exposure, education should be strengthened to protect the health of nonsmokers in policy-free settings.
Indoor air pollution
Environmental exposure to radon is the leading cause of lung cancer among nonsmokers, and the second strongest cause for people who smoke (49), which is responsible for 3.78% of lung cancer deaths in China (6). It is a colorless and odorless radioactive gas and is ubiquitous because it is naturally occurring and can be released in rock, soil, and water. The concentration of radon is diluted to a very low level in the outdoor air and is not a serious concern (50). However, more and more gangue, steel slag, and other industrial waste being used in construction and decoration materials, resulted in a rapid increasing risk of exposure to radon for indoor workers. There are few nationwide indoor radon pollutants investigation in China. The survey (51) conducted in 26 cities of China during May 2002 and November 2004 reported that the radon level in residence in part of China was 43.8±37.7 (range: 6.6−596) Bqm−3, with 6.4% of the monitoring rooms higher than 100 Bqm−3. Another survey (52) conducted from 2006 to 2010, covering 12% of the whole Chinese population, reported that the weighted mean level by population was 30.7±4.3 (range: 5.3−183.0) Bqm−3, with 1.8% of the monitoring rooms higher than 100 Bqm−3. The ratio between results of this survey and measurements in the 1980s and 1990s was 1.80 (52), suggesting an overall increasing trend of the indoor radon level. It also found that the high radon region in China was scattered. Specifically, the content of uranium (radium) in rock soil contributed to the high level in southern regions, while in the north, it depended on the type of building, ventilation, and decoration materials (51).
Another important cause of indoor air pollution is solid fuels (mainly coal and unprocessed biomass fuel) for cooking, heating, or lighting. When incompletely combusted, they may produce carbon monoxide, particulate matter (PM), and other toxic organic compounds (including polycyclic aromatic hydrocarbons, and heterocyclic aromatic compounds), which have been reported to be associated with lung toxicity and cancer risk (53,54). According to WHO (55), about 45% of the population in China still used solid fuels in 2013, with an even higher proportion in rural areas (79%). However, there are less than 5% of population using solid fuels in most developed countries. In 2010, emissions from burning coal were classified as carcinogenic to humans (group 1) by the International Agency for Research on Cancer (IARC) (56). Considering that females usually play a leading role in domestic cooking, the high lung cancer incidence among Chinese females with a low prevalence of smoking may be explained by relatively high exposure to solid fuel smoke.
Moreover, economically underdeveloped areas tend to face problems of both low utilization of non-clean energy and poor or absent ventilation (54), increasing the local disease burden of lung cancer. Improving ventilation is also proven to be effective in the houses using clean energy since indoor air pollution is unavoidable (57,58). Also, Chinese-style cooking is a noteworthy risk factor for lung cancer because it often involves more volatilization of heated non-refined oil and exposure to more fumes (53,59).
Outdoor air pollution
Outdoor air pollution is also the focus of environmental issues catching global attention and has been classified as carcinogen to humans (IARC Group 1) (60). It has been reported that both long-term (61,62) and short-term (63-66) exposure to air pollutants have posed a great threat to human health, especially the cardiopulmonary system, which involved several mechanisms including genetic changes, stimulation of inflammatory, immune, and oxidative stress response, and epigenetic effects (67).
Air quality in China is among the worst in the world (63,68). In recent years, the government has adopted such strategies as bulk coal control, emission reduction, vehicle flow limitation, and other comprehensive methods to improve air quality. The ambient monitoring data collected from 388 cities across the country show that the compliance rate of annual air quality in China has doubled in the past five years, with a nearly 28% dropping in the average concentration of PM (Table 3 ) (69). In addition, the proportion of days when the concentration of each pollutant exceeded the standard has decreased significantly, and several pollutants (SO2 NO2 and CO) were even less than 0.1%. Such trends affirm the effectiveness of national governance. However, health damage can be observed even at a low level of exposure to outdoor pollutants. Besides, due to the co-existence of factors such as the development of coal-fired industries and the rise of automobile utilization rate, a more complex mix of air contaminants were discharged (70), which also poses new challenges to the governance.
3. Mean concentration and percentage of days exceeding limit of primary pollutants in outdoor air in China between 2015 and 2019*.
| Variables | 2015 | 2016 | 2017 | 2018 | 2019 |
| *, Source: Ministry of Ecology and Environment of the People’s Republic of China (http://www.mee.gov.cn/hjzl/sthjzk/zghjzkgb/). | |||||
| Compliance rate of air quality (%) | 21.6 | 24.9 | 29.3 | 35.8 | 46.6 |
| Mean concentration (μg/m3) | |||||
| PM2.5 | 50 | 47 | 43 | 39 | 36 |
| PM10 | 87 | 82 | 75 | 71 | 63 |
| O3 | 134 | 138 | 149 | 151 | 148 |
| SO2 | 25 | 22 | 18 | 14 | 11 |
| NO2 | 30 | 30 | 31 | 29 | 27 |
| CO | 2.1 | 1.9 | 1.7 | 1.5 | 1.4 |
| Percentage of days exceeding the limit (%) | |||||
| PM2.5 | 17.5 | 14.7 | 12.4 | 9.4 | 8.5 |
| PM10 | 12.1 | 10.4 | 7.1 | 6 | 4.6 |
| O3 | 4.6 | 5.2 | 7.6 | 8.4 | 7.6 |
| SO2 | 0.7 | 0.5 | 0.3 | <0.1 | <0.1 |
| NO2 | 1.6 | 1.6 | 1.5 | 1.2 | 0.6 |
| CO | 0.5 | 0.4 | 0.3 | 0.1 | <0.1 |
Occupational hazard
The respiratory tract is a primary pathway that carcinogen enters the human body and the organ of direct action. Correspondingly, lung cancer is one of the most common types of occupational cancer. In China, there are six risk factors included in the current occupational disease catalogue, covering asbestos (all forms), bis (chloromethyl) ether and chloromethyl methyl ether, arsenic and inorganic arsenic compounds, chromium (VI) compounds, erionite, and coke oven emission, which have been basically identified as a class I carcinogen by IARC (71). Those working in light industries, chemical industries, and coke oven workers tend to face higher exposure to such occupational hazards, given the wide range of sources including raw materials, end products, and unexpected by-products.
As reported in the China Statistical Yearbook 2019 (72), more than 120 million people were employed in mining, manufacturing, construction, and energy supply industries, which suggests that there are still quite numbers of people facing the risk of developing occupational lung cancer. According to the annual occupational disease report issued by the Chinese Center for Disease Control and Prevention (73), taking no account of unidentified cases, there were dozens of occupational lung cancer cases every year, accounting for about half of all diagnosed occupational tumors. In addition, other occupations have not yet been included but are also at high risk of lung cancer, for instance, traffic police, welding workers, painters, and workers in metal smelting industry and rubber factory.
Other risk factors of lung cancer
Given that cancer is the result of long-term interaction between internal factors and external environment, there are also other risk factors that may contribute to the burden of lung cancer. For one thing, dietary habits, such as drinking water containing arsenic, taking high-dose beta-carotene supplements for smokers, and consuming red meat, processed meat and alcoholic drinks, have been reported to increase the risk of lung cancer (74). It is reported that about 27% of lung cancer deaths in China can be attribute to low vegetable intake (38). For another, internal factors are also of great importance, including genetics (41) and a history of lung disease (mainly emphysema, chronic bronchitis, tuberculosis or pneumonia) (75), which have been reported as independent causes of lung cancer.
Prevention strategies for lung cancer
Smoking cessation
Primary prevention is also the most fundamental prevention, aiming to reduce exposure to risk factors. The priority is to control smoking rates and secondhand smoke exposure. The incidence of lung cancer in the United States has declined in recent years, which is significantly attributable to the effective control of tobacco use (76). Considering that China has the fastest-growing cigarette ability to pay on a world scale (77), there is still much room for the flowing of tobacco tax, which will exert a constraint effect on people of all ages. Smoking bans in public places and some special places should also be strengthened to create more smoke-free environment. In addition, comprehensive education on dangers of tobacco use, together with a total ban on tobacco advertising is also urgently needed, particularly for teenagers.
Improvement in air quality
First, more publicity should be given to the dangers of radon, because many people have not yet paid attention to this invisible health killer. At the same time, the experience of the United States should be learned (78). In this regard, a special department for examining and improving indoor radon content should be established to monitor radon exposure in all regions of the country and take measures timely. Setting standard should also be strengthened, such as the approval of construction in areas with high background contamination and the level limit of radon level in building materials.
Second, it has been reported that a significant reduction occurred in mortality from cardiopulmonary diseases after withdrawing solid fuels (57). Although the utilization rate of clean energy in China has been increasing from 43% to 64% between 2000 and 2018 (79), there is still a big gap between China and the United States, Europe, and other developed countries (with a proportion over 95%), indicating that promoting the use of clean energy (e.g., electricity and natural gas) can effectively alleviate the burden of lung cancer disease in China, which is of great urgency.
Third, even though the current air quality has been improved to a certain extent, the pollutants may cause damages to health even at low levels of exposure (within the recommended range), so the existing comprehensive treatment plan should be maintained in consideration of the rapid ongoing development of urbanization and modern industry in China. In addition, more importance should be attached to the monitoring and analysis of air pollutants in order to better deal with the degradation of complex compounds and the exploration of their sources.
Early detection and effective treatment
Early diagnosis and treatment of lung cancer were also of vital significance. The prognosis of lung cancer was poor because most cases were initially asymptomatic and typically discovered at advanced stages (80). A large prospective randomized screening trial found a 20% decrease in lung cancer mortality in the screening group by low-dose computed tomography, compared with unscreened group (81). This result was also verified by another large-scale randomized trial conducted in Netherland (82).
There are already several ongoing lung cancer screening programs in China, including Early Detection and Early Treatment of Cancer in Urban Areas, and Early Detection and Early Treatment of Cancer in Rural Cancer. It will be of great help for such programs being promoted on a larger scale. Besides, attention should be paid to monitoring the health status of high-risk groups, such as regular medical examinations and job rotation among relevant occupational groups, to reduce morbidity and mortality. For lung cancer patients detected through screening, it is responsible for public health providers to urge them to receive standardized treatment as early as possible, so as to prolong their survival.
Conclusions
Lung cancer incidence and mortality presented an increased trend over the past decade, which can partly be attributed to the exposure to those persistent-existing risk factors, including high smoking rate, the use of solid fuel, indoor radon level. Additionally, emerging health threats continue to threaten human health. Therefore, the Chinese government is supposed to synthesize all aspects of measures, such as etiology control, the implementation of lung cancer screening and increasing the investment on researches of treatment and rehabilitation, to change this situation.
Acknowledgements
This work was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS) (No. 2016-I2M-2-004), Sanming Project of Medicine in Shenzhen (No. SZSM201911015).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Contributor Information
Ji Peng, Email: pengji126@126.com.
Wanqing Chen, Email: chenwq@cicams.ac.cn.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Global Cancer Observatory: Cancer Today. Lyon: International Agency for Research on Cancer, 2018. Available online: https://gco.iarc.fr/today
- 3.Gao S, Li N, Wang S, et al Lung Cancer in People’s Republic of China. J Thorac Oncol. 2020;15:1567–76. doi: 10.1016/j.jtho.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 4.Zheng R, Sun K, Zhang S, et al Report of cancer epidemiology in China, 2015. Zhonghua Zhong Liu Za Zhi. 2019;41:19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 5.2018 China Cancer Registry Annual Report: Cancer Incidence and Mortality in Chinese Cancer Registration Areas in 2015. Beijing: People’s Medical Publishing House, 2019.
- 6.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019(GBD 2019) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020. Available online: http://ghdx.healthdata.org/gbd-results-tool
- 7.Zhang S, Zheng R, Yang Z, et al Trend analysis on incidence and age at diagnosis for lung cancer in cancer registration areas of China, 2000-2014. Zhonghua Yu Fang Yi Xue Za Zhi. 2018;52:579–85. doi: 10.3760/cma.j.issn.0253-9624.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Liu S, Chen Q, Guo L, et al Incidence and mortality of lung cancer in China, 2008-2012. Chin J Cancer Res. 2018;30:580–7. doi: 10.21147/j.issn.1000-9604.2018.06.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou XN, Lin D, Chao A, et al Histological subtypes of lung cancer in Chinese women from 2000 to 2012. Thorac Cancer. 2014;5:447–54. doi: 10.1111/1759-7714.12121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou XN, Lin DM, Wan X, et al Histological subtypes of lung cancer in Chinese males from 2000 to 2012. Biomed Environ Sci. 2014;27:3–9. doi: 10.3967/bes2014.010. [DOI] [PubMed] [Google Scholar]
- 11.Ji X Dynamic analysis of clinical epidemiology and the distribution of pathology types of patients with primary lung cancer in Peking University Cancer Hospital from 2000 to 2013. Zhonghua Zhong Liu Fang Zhi Za Zhi. 2017;24:1687–92. doi: 10.16073/j.cnki.cjcpt.2017.24.001. [DOI] [Google Scholar]
- 12.Gao J, Zhang S, Wu W Investigation of dynamic constituent ratio changes of lung cancer in Ningxia, 2000-2014. Zhong Liu Fang Zhi Yan Jiu. 2016;43:984–9. doi: 10.3971/j.issn.1000-8578.2016.11.013. [DOI] [Google Scholar]
- 13.Wang Y, Huang J, Hu W, et al Clinical epidemiological analysis of 2403 cases of lung cancer. Guo Ji Zhong Liu Xue Za Zhi. 2019;46:460–5. doi: 10.3760/cma.j.issn.1673-422X.2019.08.003. [DOI] [Google Scholar]
- 14.Li F, Huang L, Hu C, et al Comparative analysis of clinical epidemiology and pathological characteristics of 908 patients with primary lung cancer of Hunan province in 1997 and 2007. Zhongguo Fei Ai Za Zhi. 2010;13:326–30. doi: 10.3779/j.issn.1009-3419.2010.04.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo X, Fu Z, Sun J, et al Trend of mortality and decomposition on malignant tumors in Shandong province, 1970-2013. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:924–9. doi: 10.3760/cma.j.issn.0254-6450.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Huang C, Wang L, Lu Y, et al Epidemiological characteristics and trend of cancer mortality in Suzhou 1987-2017. Zhongguo Zhong Liu. 2020;29:90–5. doi: 10.11735/j.issn.1004-0242.2020.02.A002. [DOI] [Google Scholar]
- 17.Xin W, Huang L, Yan Y Analysis for the time trends of lung cancer epidemic and disease burden in China, 2005-2013. Zhonghua Zhong Liu Fang Zhi Za Zhi. 2019;26:1059–65. doi: 10.16073/j.cnki.cjcpt.2019.15.001. [DOI] [Google Scholar]
- 18.Zhang D, Qian X, Chu S, et al Level and trend of respiratory diseases mortality in China from 2002 to 2016. Zhonghua Yi Xue Za Zhi. 2020;100:1895–900. doi: 10.3760/cma.j.cn112137-20191108-02430. [DOI] [PubMed] [Google Scholar]
- 19.Liang W, Song B, Yang C, et al Analysis of trend on mortality of lung cancer and cause-eliminated life expectancy from 1987 to 2017 in Harbin. Zhongguo Zhong Liu. 2020;29:689–94. doi: 10.11735/j.issn.1004-0242.2020.09.A009. [DOI] [Google Scholar]
- 20.Zhang Y, Zhu J, Chen J, et al Epidemiologic features for lung cancer mortality in Qidong City of Jiangsu from 1972 to 2016. Xian Dai Yu Fang Yi Xue. 2020;47:2521–5, 44. [Google Scholar]
- 21.Cen X, Wang D, Sun W, et al The trends of mortality and years of life lost of cancers in urban and rural areas in China, 1990-2017. Cancer Med. 2020;9:1562–71. doi: 10.1002/cam4.2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeng H, Chen W, Zheng R, et al Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6:e555–e67. doi: 10.1016/s2214-109x(18)30127-x. [DOI] [PubMed] [Google Scholar]
- 23.Zhu J, Zhang Y, Chen Y, et al Analysis on lung cancer survival from 2001 to 2007 in Qidong, China. Zhongguo Fei Ai Za Zhi. 2011;14:23–7. doi: 10.3779/j.issn.1009-3419.2011.01.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peng H, Han B, Li X, et al Analysis of clinical characteristics and survival rates in 1 279 lung cancer patients. Zhongguo Ai Zheng Za Zhi. 2011;21:354–8. doi: 10.3969/j.issn.1007-3969.2011.05.007. [DOI] [Google Scholar]
- 25.Wang Y, Bi Y, Wang Z, et al Survival analysis of lung cancer patients in Shandong Province. Zhongguo Wei Sheng Tong Ji. 2018;35:111–3, 6. [Google Scholar]
- 26.Zhang M, Wu C, Gong Y, et al Survival analysis of patients with lung cancer in Shanghai. Zhongguo Ai Zheng Za Zhi. 2017;27:326–33. doi: 10.19401/j.cnki.1007-3639.2017.05.002. [DOI] [Google Scholar]
- 27.Micheli A, Ciampichini R, Oberaigner W, et al The advantage of women in cancer survival: an analysis of EUROCARE-4 data. Eur J Cancer. 2009;45:1017–27. doi: 10.1016/j.ejca.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 28.Adami HO, Bergström R, Holmberg L, et al The effect of female sex hormones on cancer survival. A register-based study in patients younger than 20 years at diagnosis. JAMA. 1990;263:2189–93. doi: 10.1001/jama.1990.03440160051036. [DOI] [PubMed] [Google Scholar]
- 29.Hanagiri T, Sugio K, Uramoto H, et al Gender difference as a prognostic factor in patients undergoing resection of non-small cell lung cancer. Surgery Today. 2007;37:546–51. doi: 10.1007/s00595-006-3453-9. [DOI] [PubMed] [Google Scholar]
- 30.Ou SH, Zell JA, Ziogas A, et al Prognostic factors for survival of stage I nonsmall cell lung cancer patients : a population-based analysis of 19, 702 stage I patients in the California Cancer Registry from 1989 to 2003. Cancer. 2007;110:1532–41. doi: 10.1002/cncr.22938. [DOI] [PubMed] [Google Scholar]
- 31.Campbell NC, Elliott AM, Sharp L, et al Rural factors and survival from cancer: analysis of Scottish cancer registrations. Br J Cancer. 2000;82:1863–6. doi: 10.1054/bjoc.1999.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Francisci S, Minicozzi P, Pierannunzio D, et al Survival patterns in lung and pleural cancer in Europe 1999-2007: Results from the EUROCARE-5 study. Eur J Cancer. 2015;51:2242–53. doi: 10.1016/j.ejca.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 33.Marquette D, Pichon E, Deschasse G, et al Lung cancer in adults: Better prognosis of patients aged 45 and under related to good condition and lower TNM stage (a comparative and retrospective study) Presse Med (in French) 2012;41:e250–6. doi: 10.1016/j.lpm.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 34.Nesbitt JC, Putnam JB Jr., Walsh GL, et al Survival in early-stage non-small cell lung cancer. Ann Thorac Surg. 1995;60:466–72. doi: 10.1016/0003-4975(95)00169-l. [DOI] [PubMed] [Google Scholar]
- 35.Jia X, Xie Z, Zhang B, et al Survival rate and prognostic factors of 2209 non-smokers with lung cancer. Yi Xue Yu Zhe Xue (B) (in Chinese) 2017;38:51–5. doi: 10.12014/j.issn.1002-0772.2017.03b.15. [DOI] [Google Scholar]
- 36.Dillman RO, McClure SE Steadily improving survival in lung cancer. Clin Lung Cancer. 2014;15:331–7. doi: 10.1016/j.cllc.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 37.Chen W, Xia C, Zheng R, et al Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health. 2019;7:e257–e269. doi: 10.1016/s2214-109x(18)30488-1. [DOI] [PubMed] [Google Scholar]
- 38.Islami F, Chen W, Yu XQ, et al Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol. 2017;28:2567–74. doi: 10.1093/annonc/mdx342. [DOI] [PubMed] [Google Scholar]
- 39.Tobacco Control Resource Center of China. 2015 Chinese Adult Tobacco Survey Report. Available online: http://www.tcrc.org.cn/html/zy/cbw/jc/3259.html
- 40.Wang M, Luo X, Xu S, et al Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7:35–45. doi: 10.1016/s2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 41.She J, Yang P, Hong Q, et al Lung cancer in China: challenges and interventions. Chest. 2013;143:1117–26. doi: 10.1378/chest.11-2948. [DOI] [PubMed] [Google Scholar]
- 42.Yang G, Fan L, Tan J, et al Smoking in China: findings of the 1996 national prevalence survey. JAMA. 1999;282:1247–53. doi: 10.1001/jama.282.13.1247. [DOI] [PubMed] [Google Scholar]
- 43.Yang G. Deaths and Their Risk Factors among Chinese Population. Beijing: China Union Medical University Press, 2005.
- 44.Global Adult Tobacco Survey (GATS) — China 2010 Country Report. Available online: http://www.notc.org.cn/newjcpg/201304/W020121108628365808856.pdf
- 45.Chinese Center for Disease Control and Prevention. Results Release of the 2018 China Adult Tobacco Survey. Available online: http://www.chinacdc.cn/yw_9324/201905/t20190530_202932.html
- 46.World Health Organization. WHO global report on trends in prevalence of tobacco use 2000-2025, third edition. Available online: https://www.who.int/publications/i/item/who-global-report-on-trends-in-prevalence-of-tobacco-use-2000-2025-third-edition
- 47.Tobacco Control Resource Center of China. Chinese Adolescent Tobacco Survey Report in 2014. Available online: http://www.tcrc.org.cn/Item/Show.asp?m=1&d=2827
- 48.Chinese Center for Disease Control and Prevention. Results of the 2019 Tobacco Survey of Middle school Students in China. Available online: http://www.chinacdc.cn/jkzt/sthd_3844/slhd_4152/202006/t20200601_216956.html
- 49.United States Environmental Protection Agency. Basic Radon Facts 2016(updated July 2016). Available online: https://www.epa.gov/radon/basic-radon-facts
- 50.Jiang Y Radon exposure in indoor circumstance. Huan Jing Yu Jian Kang Za Zhi. 2007;24:277–9. doi: 10.3969/j.issn.1001-5914.2007.04.045. [DOI] [Google Scholar]
- 51.Xu D, Shang B, Cao Z Investigation of key indoor air pollutants in residence in part of the cities in China. Wei Sheng Yan Jiu. 2007;36:473–6. doi: 10.3969/j.issn.1000-8020.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 52.Wang C, Pan Z, Liu S, et al Investigation on indoor radon levels in some parts of China. Fu She Fang Hu. 2014;34:65–73. doi: 10.3969/j.issn.1000-8187.2014.02.001. [DOI] [Google Scholar]
- 53.Kim C, Gao YT, Xiang YB, et al Home kitchen ventilation, cooking fuels, and lung cancer risk in a prospective cohort of never smoking women in Shanghai, China. Int J Cancer. 2015;136:632–8. doi: 10.1002/ijc.29020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gordon SB, Bruce NG, Grigg J, et al Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014;2:823–60. doi: 10.1016/S2213-2600(14)70168-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.World Health Organization. THE GLOBAL HEALTH OBSERVATORY: Population using solid fuels (%). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/population-using-solid-fuels-(-)
- 56.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Household use of solid fuels and high-temperature frying. IARC Monogr Eval Carcinog Risks Hum. 2010;95:1–430. [PMC free article] [PubMed] [Google Scholar]
- 57.Yu K, Lv J, Qiu G, et al Cooking fuels and risk of all-cause and cardiopulmonary mortality in urban China: a prospective cohort study. Lancet Glob Health. 2020;8:e430–e9. doi: 10.1016/S2214-109X(19)30525-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lan Q, Chapman RS, Schreinemachers DM, et al Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst. 2002;94:826–35. doi: 10.1093/jnci/94.11.826. [DOI] [PubMed] [Google Scholar]
- 59.Zhong L, Goldberg MS, Gao YT, et al Lung cancer and indoor air pollution arising from Chinese-style cooking among nonsmoking women living in Shanghai, China. Epidemiology. 1999;10:488–94. doi: 10.1097/00001648-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 60.Loomis D, Grosse Y, Lauby-Secretan B, et al The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14:1262–3. doi: 10.1016/s1470-2045(13)70487-x. [DOI] [PubMed] [Google Scholar]
- 61.Guo Y, Zeng H, Zheng R, et al The association between lung cancer incidence and ambient air pollution in China: A spatiotemporal analysis. Environ Res. 2016;144:60–5. doi: 10.1016/j.envres.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 62.Hamra GB, Guha N, Cohen A, et al Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014;122:906–11. doi: 10.1289/ehp/1408092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang N, Mengersen K, Tong S, et al Short-term association between ambient air pollution and lung cancer mortality. Environ Res. 2019;179:108748. doi: 10.1016/j.envres.2019.108748. [DOI] [PubMed] [Google Scholar]
- 64.Liu C, Chen R, Sera F, et al Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381:705–15. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang L, Liu C, Meng X, et al Associations between short-term exposure to ambient sulfur dioxide and increased cause-specific mortality in 272 Chinese cities. Environ Int. 2018;117:33–9. doi: 10.1016/j.envint.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 66.Yin P, Chen R, Wang L, et al Ambient ozone pollution and daily mortality: A nationwide study in 272 Chinese cities. Environ Health Perspect. 2017;125:117006. doi: 10.1289/EHP1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.DeMarini DM Genotoxicity biomarkers associated with exposure to traffic and near-road atmospheres: a review. Mutagenesis. 2013;28:485–505. doi: 10.1093/mutage/get042. [DOI] [PubMed] [Google Scholar]
- 68.van Donkelaar A, Martin RV, Brauer M, et al Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environ Health Perspect. 2015;123:135–43. doi: 10.1289/ehp.1408646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ministry of Ecology and Environment of the People’s Republic of China. Bulletin of the Ecology and Environment of the People’s Republic of China. Available online: http://www.mee.gov.cn/hjzl/sthjzk/zghjzkgb/
- 70.Han L, Zhou W, Pickett ST, et al Multicontaminant air pollution in Chinese cities. Bull World Health Organ. 2018;96:233–42E. doi: 10.2471/blt.17.195560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.World Health Organization. Human Cancer: Known Causes and Prevention by Organ Site. Available online: https://monographs.iarc.who.int/human_cancer_known_causes_and_prevention_organ_site/
- 72.National Bureau of Statistics of China. China Statistical Yearbook 2019. Beijing: China Statistics Press, 2019. Available online: http://www.stats.gov.cn/tjsj/ndsj/2019/indexch.htm
- 73.National Institute for Occupational Health and Poison Control. Information policy for Occupational Health. Available online: http://niohp.chinacdc.cn/zyws/4ydnb/index.htm
- 74.World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: a Global Perspective (The Third Expert Report). Available online: https://www.wcrf.org/dietandcancer
- 75.Brenner DR, Boffetta P, Duell EJ, et al Previous lung diseases and lung cancer risk: a pooled analysis from the International Lung Cancer Consortium. Am J Epidemiol. 2012;176:573–85. doi: 10.1093/aje/kws151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bade BC, Dela Cruz CS Lung cancer 2020: Epidemiology, etiology, and prevention. Clin Chest Med. 2020;41:1–24. doi: 10.1016/j.ccm.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 77.Research on the Paying Ability of Cigarettes in China, 2001-2016. Available online: http://www.catcprc.org.cn/upload/file/2019-05/%E4%B8%AD%E5%9B%BD%E5%8D%B7%E7%83%9F%E6%94%AF%E4%BB%98%E8%83%BD%E5%8A%9B%E7%A0%94%E7%A9%B6%E6%8A%A5%E5%91%8A.pdf
- 78.United States Environmental Protection Agency. A Citizen’s Guide to Radon: The Guide to Protecting Yourself and Your Family from Radon. Available online: https://www.epa.gov/sites/production/files/2016-02/documents/2012_a_citizens_guide_to_radon.pdf
- 79.World Health Organization. THE GLOBAL HEALTH OBSERVATORY: Population with primary reliance on clean fuels and technologies (%) (Public health and environment: Air popllution). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/proportion-of-population-with-primary-reliance-on-clean-fuels-and-technologies-(-)
- 80.Nasim F, Sabath BF, Eapen GA Lung cancer. Med Clin North Am. 2019;103:463–73. doi: 10.1016/j.mcna.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 81.The National Lung Screening Trial Research Team Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ru Zhao Y, Xie X, de Koning HJ, et al NELSON lung cancer screening study. Cancer Imaging. 2011;11 Spec No A(1A):S79–84. doi: 10.1102/1470-7330.2011.9020. [DOI] [PMC free article] [PubMed] [Google Scholar]