Perspective
Healthcare services globally are combating the impact of SARS-CoV-2 and associated COVID-19 infection, which has caused significant morbidity and mortality across all affected countries.1 Whilst the medical community and resources have focused on this pandemic, it is important to consider that cardiovascular disease remains the most common cause of death globally and accounts for in excess of 17.8 million deaths annually.2 Of concern, there was an alarming reduction in healthcare seeking behaviours during the enforced lockdown period to contain viral spread.3–5 Admissions to hospital with an acute coronary syndrome significantly dropped and individuals who eventually sought medical help experienced a higher fatality rate.3–6 These observations are difficult to accept when prognostically important therapies such as primary percutaneous coronary intervention were widely used prior to the pandemic. Moreover, as lockdown measures are tentatively eased we enter a precarious period when delivery of cardiovascular care will face several challenges and will need to constantly adapt to the pandemic’s evolution. In this article, we aim to provide an overview of these challenges and suggest potential solutions based on current models of care.
Healthcare service delivery
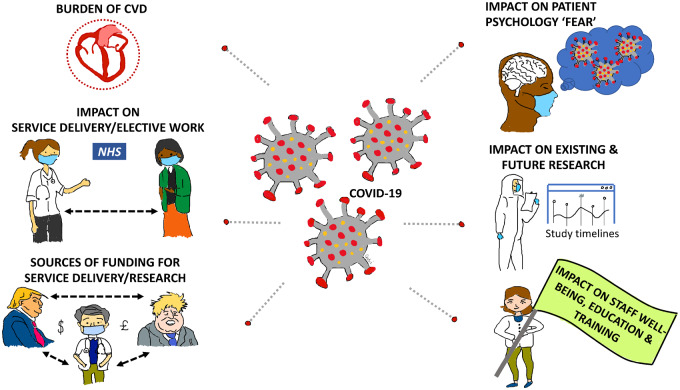
It has been well established that there is a higher incidence of COVID-19 related complications, including death, amongst individuals with cardiovascular disease.7–9 Fear of this increased risk has resulted in a reluctance in patients seeking healthcare which has been associated with an increase in morbidity and mortality independent of COVID-19 status, therefore, strategies to engage with patients, which facilitate their trust in the medical infrastructure to serve them effectively and efficiently whilst minimizing the risk of developing COVID-19 infection are of paramount importance going forwards (Figure 1).
Figure 1.
The challenges ahead in the COVID-19 era.
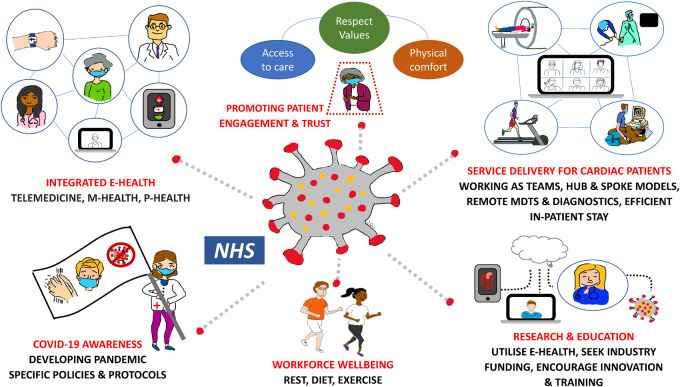
The pandemic compromised delivery of acute care across the breadth of cardiology and has resulted in a backlog of elective work, including outpatient clinics, routine investigations, and procedures. As clinical and service demands increase, cardiologists must prioritize patient care on a case-by-case basis whilst ensuring patients are kept informed regarding the evolving service. The restoration of normal services is plagued with potential obstacles and requirements for social distancing in waiting rooms, day wards and the cardiac catheterization laboratory (Figure 2). These challenges necessitate optimization of referral pathways whilst ensuring appropriate frameworks are in place for determining procedural urgency. As such, it is essential for the cardiovascular community to remain appraised with the epidemiology of COVID-19 infection at a local and national level through close liaison with public health institutions.
Figure 2.
Potential solutions. e-health: the use of information and communications technology in support of health and health-related fields; m-health: the use of mobile wireless technologies for health; MDT: multidisciplinary team; p-health: personalized health including wearables and sensors.
During the pandemic, there has been extraordinary teamwork across healthcare systems. The community has witnessed successful hub and spoke models of care, extra capacity for intensive care beds built in record time, rapid integration of much-needed additional staff, restructuring of working rotas, procurement of medical supplies and equipment as well as reinvigorated infection control practices. Clinicians from Italy adopted innovative strategies within a few weeks of the COVID-19 outbreak to reorganize the care of heart failure patients in their unit.10 Patients were admitted into three different designated areas (red/pink/green) depending on their infectivity status—which might have been confirmed (red zone)/suspected (pink zone) or excluded (green zone). Patients changed between zones based on clinical, radiological, and biochemical testing data. This innovative model of care took into account local personal protective equipment (PPE) issues and optimization of the local workforce. These experiences should be an impetus to continue working in the new normal and transform the delivery and sustainability of cardiovascular care. Throughout the process, it will be essential to utilize up to date policies and guidance from local and national bodies regarding the care of COVID-19 positive and negative patients with a focus on infection prevention and containment.11,12 Furthermore, hospitals should anticipate a need for appropriate PPE in advance to ensure their workforce is operating in a safe environment.
E-health
As a consequence of the COVID-19 pandemic, healthcare systems globally have adopted aspects of e-Health, which utilizes information technology and communication technology to aid patient care (Figure 2).13
There has been a particular focus on telemedicine, which has been largely responsible for the buoyancy in maintaining outpatient services through virtual consultations. The benefits of m-Health, which includes mobile applications for health surveillance and p-health, which utilizes wearable devices such as patch monitors have been realized at the global level.13,14 These have the added benefits of longer surveillance, a theoretical reduction in risk of infection, reduced pressure on resources, and empowering patients in their management. Cardiac pacing teams have developed successful remote interrogation and remote monitoring systems which has reduced patient attendance for routine device follow-ups.15,16
The exponential increase in the number of elderly individuals in our population means that there will be an increasing requirement to manage such vulnerable individuals remotely to reduce their risk of infection. In this respect, several innovative electronic monitoring and remote assessment systems have facilitated the management of several chronic conditions such as atrial fibrillation and heart failure during the pandemic. Researchers from the Netherlands established a simple, user-friendly mobile health programme to manage atrial fibrillation using a smartphone app (TeleCheck-AF Project).17 Using the index finger and the phone camera, this app can interpret heart rate and rhythm and is used to assist the physician in guiding the teleconsultation and monitor AF management remotely. Designed during the pandemic, the app has now been utilized across 36 centres and empowered over 1000 patients.17 Importantly the team plans on collecting outcome data to perform a retrospective analysis of the safety and impact of this approach on patient care.
In an attempt to reduce transmission risk, COVID-19 halted cardiac rehabilitation services, which are traditionally delivered in hospitals or outpatient settings.18 Home-based cardiac rehabilitation (HBCR), a concept that has been utilized in low-moderate risk patients in some countries, has emerged during the pandemic as an effective telehealth solution.19 Indeed guidelines produced in 2019 prior to the pandemic, clearly emphasized that interventions involved in HBCR translate into targeted behaviours and eventually into improvements in secondary prevention goals such as improved quality of life and reduced cardiovascular morbidity and mortality.19 Some centres have used such models of care during the pandemic with great success and there is no doubt that telehealth can play an important role in primary and secondary prevention of cardiovascular disease.20,21
Electronic technologies have also transformed methods of conducting multidisciplinary team meetings and have encouraged participation from an even broader audience, compared to historical meetings which were held in confined spaces. Such practices have the potential to improve both patient care and healthcare professional education through sharing expertise, particularly outside the context of specialized referral centres.
With the expedition of remote monitoring and assessment systems, healthcare staff and patients, alike, will require education for utilising such systems including potential logistical issues such as connectivity. In addition, there will be a requirement for further guidance from regulatory bodies with respect to certain medico-legal implications and guidance on the use of specific technology, which accounts for licensed platforms and issues around confidentiality and data protection.
Research
There will be several obstacles from a research perspective including patient recruitment and engagement into existing and future trials, which will impact on study timelines and completion. The temporal variation of COVID-19 infection globally might also impact upon the demographics of the cohorts included in studies with the potential to bias study outcome. Indeed, funding for research has reduced as government resources have justifiably been diverted to research focused at COVID-19 and charities funding cardiovascular research have suffered a considerable reduction in their resources as a result of the financial impact of the pandemic. As we adapt to this new reality, the academic world needs to learn from the resourcefulness demonstrated by clinical services and come up with new, more efficient strategies of conducting research. This should include harnessing collaborations between individuals, institutions, utilizing aspects of e-health and seeking other sources of funding such as from industry- in an open and transparent manner.
Education
The impact of COVID-19 has been significant on the training of medical students and healthcare staff across the board. Training programmes and research fellowships have been stalled to supplement the much needed manpower to manage this crisis. Training committees and regulatory boards will need to ensure that a pragmatic approach is adopted with adequate remuneration, opportunities to train and ensure close dialogue with those impacted.
Cardiovascular medicine remains a rapidly evolving field. During the COVID-19 pandemic, there has been an explosion of available online learning resources. Despite the fact that most face-to-face scientific conferences were cancelled, most were replaced by on-line delivery in a variety of different formats. The continued delivery of scientific meetings, conferences, and courses on web-based platforms has been warmly received. Such events are likely to evolve rapidly and mature into sophisticated on-line educational experiences, which will be available to a wider audience at a lower cost and avidly demonstrates our ethos as cardiologists towards lifelong learning, education, and adapting to change for the benefit of patients.
The personal cost
The challenges of maintaining the extra capacity and capability of healthcare systems has inevitably impacted on the wellbeing of the workforce and should not be underestimated. Proactive strategies are required to engage and support individuals during these unprecedented times, which include an emphasis on optimal rest, nutrition, and exercise. Apart from protecting healthcare workers, such approaches will ensure sustainable patient care.
Conclusion
Amid a pandemic, there has been phenomenal innovation and commitment from clinicians, overcoming historical barriers to change for the greater good of patient care. This has resulted in a newfound appreciation for healthcare workers by society as well as a vigour and sense of compassion being reborn into the health service. Given the uncertainty surrounding the duration of the COVID-19 pandemic, safe and effective integrated models of care which include remote methods of clinical management, disease surveillance and appropriate staff training should be engraved into our daily practice whilst ensuring staff wellbeing is not neglected.
Supplementary Material
Acknowledgements
R.T.B. is funded by a research grant from the charitable organization Cardiac Risk in the Young (CRY) and would like to thank the organization for continuing to support cardiovascular research during these challenging times.
Conflict of interest: none declared.
References
References are available as supplementary material at European Heart Journal online.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.