Abstract
Background
Weeks after issuing social distancing orders to suppress severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission and reduce growth in cases of severe coronavirus disease 2019 (COVID-19), all US states and the District of Columbia partially or fully relaxed these measures.
Methods
We identified all statewide social distancing measures that were implemented and/or relaxed in the United States between 10 March and 15 July 2020, triangulating data from state government and third-party sources. Using segmented linear regression, we estimated the extent to which relaxation of social distancing affected epidemic control, as indicated by the time-varying, state-specific effective reproduction number (Rt).
Results
In the 8 weeks prior to relaxation, mean Rt declined by 0.012 units per day (95% confidence interval [CI], −.013 to −.012), and 46/51 jurisdictions achieved Rt < 1.0 by the date of relaxation. After relaxation of social distancing, Rt reversed course and began increasing by 0.007 units per day (95% CI, .006–.007), reaching a mean Rt of 1.16. Eight weeks later, the mean Rt was 1.16 and only 9/51 jurisdictions were maintaining an Rt < 1.0. Parallel models showed similar reversals in the growth of COVID-19 cases and deaths. Indicators often used to motivate relaxation at the time of relaxation (eg, test positivity rate <5%) predicted greater postrelaxation epidemic growth.
Conclusions
We detected an immediate and significant reversal in SARS-CoV-2 epidemic suppression after relaxation of social distancing measures across the United States. Premature relaxation of social distancing measures undermined the country’s ability to control the disease burden associated with COVID-19.
Keywords: COVID-19, SARS-CoV-2, basic reproductive number, public health regulations, social distancing
The United States is home to the largest epidemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) globally, having surpassed 7 million reported cases and 200 000 deaths by late September [1]. The burden of the coronavirus disease 2019 (COVID-19) epidemic in the United States has been disproportionately and inequitably borne by Black, Latin, and American Indian populations [2]. After experiencing large, localized epidemics in March and April, all 50 US states and the District of Columbia implemented social distancing measures, with inadequate social protection [3], in an attempt to interrupt transmission and reduce morbidity and mortality from COVID-19. Several studies from the United States [4–7] and elsewhere [4, 8, 9] have demonstrated the effectiveness of social distancing measures in reducing COVID-19 case growth and the resulting morbidity and mortality, although the effectiveness of these behavioral responses has been conditioned by income [10].
Concerns about adverse economic, population health, and social spillover consequences of social distancing [11–15] have undermined adherence to social distancing guidelines and prompted efforts to relax these restrictions [16–18]. Beginning in late April, state governments and the District of Columbia began relaxing the social distancing measures that had, up to that point, successfully slowed the spread of SARS-CoV-2 [5]. Relaxation of such measures is intended to be accompanied by appropriate behavioral practices (eg, mask wearing and physical distancing) and control measures (eg, contact tracing and increased availability of testing), so that epidemic control can be maintained [19–26].
However, there has not been a coherent national strategy to promote appropriate behavioral practices, nor has an effective control infrastructure been coordinated at the federal level. As a result, recent decisions about relaxing social distancing measures have been challenged, and the burden of reopening is disproportionately borne by racialized minority populations [27]. Critical unanswered questions remain about if and how relaxation of social distancing measures can be carried out while effectively maintaining epidemic control. To address this gap in the literature, we abstracted state-level data on the implementation and relaxation of social distancing measures and undertook a longitudinal pretest-posttest comparison group study to determine the extent to which relaxation of social distancing measures has led to a recrudescence in COVID-19 transmission in the United States.
METHODS
The unit of analysis was each US state (or the District of Columbia). We identified all statewide social distancing measures that were implemented and/or relaxed between 10 March and 15 July 2020, triangulating data from state government and third-party sources [5] (see Supplementary Appendix for full details of the search procedures). Our primary explanatory variable of interest was time in days, which we divided into 2 time periods relative to the first date of relaxation of social distancing measures: (a) The prerelaxation observation period began on the date social distancing measures were first implemented in the state. For states where social distancing measures were implemented early in the epidemic, the prerelaxation period was specified as beginning 56 days prior to the date any of the social distancing measures were first relaxed in the state. We selected this 8-week threshold to ensure that all jurisdictions had a roughly similar amount of observation time during the period prior to relaxation of social distancing measures. (b) The postrelaxation observation period began the day after any of the social distancing measures were first relaxed and extended through to 9 July 2020. For states where any statewide social distancing measure was reimposed prior to 9 July, the postrelaxation period was specified as ending on the date any statewide social distancing measure was reimposed. Analysis was restricted to days on which a state had at least 100 cumulative cases reported, to minimize any effects of volatile rate changes early in the epidemic [28].
We then summarized state-specific patterns of implementation and relaxation of statewide social distancing measures. To determine the extent to which states were able to maintain epidemic control after relaxation of social distancing, we used segmented linear regression: we fitted mixed-effects linear regression models, specifying the time-varying, state-specific effective reproduction number (Rt) as our outcome of interest, and a random effect by jurisdiction to account for within-state differences in behavior, policies, or epidemic reporting. Rt corresponds to the expected number of secondary infections generated by each index case [29]. We selected Rt (using a Bayesian semimechanistic model of the infection cycle, as estimated by Unwin et al [30]) as our primary outcome to avoid reliance on crude case detection, which is susceptible to biases resulting from differential testing availability and delays in result reporting, both of which are known to be problematic in the United States [31, 32]. In contrast to reported cases, the methods described by Unwin et al [30] estimate disease transmission patterns based on observed SARS-CoV-2-related deaths [8] and thus partially mitigate bias due to testing and reporting patterns. The Rt value for a given day reflects the secondary cases generated by individuals infected on that day. The primary explanatory variables of interest were time in days, relaxation period, a time-by-relaxation-period product term. We also adjusted for day of the week [33] and state-level population density (estimated from 2018 US population data).
We conducted a number of sensitivity analyses to probe the robustness of our findings and to further explore patterns of epidemic transmission after measures were relaxed (see Supplementary Appendix for a full description of all sensitivity and secondary analyses). In brief, these analyses included (1) stratifying analyses by the type of measures first relaxed; (2) examining days since relaxation of shelter-in-place orders (ie, restrictions on internal movement) as the primary explanatory variable of interest; (3) using an alternate method of measuring Rt as derived by Abbott et al [34]; (4) using the method of generalizing estimating equations in lieu of a linear mixed effects model; (5) varying the prerelaxation time period to account for state-level patterns; (6) specifying log change in cases and log change in deaths as our outcome of interest while accounting for incubation periods and times to death after infection [35–37]; and (7) investigating epidemic size (ie, cases, deaths, and zenith Rt) and epidemic indicators (current Rt and the test positive rate [38]) to assess the extent to which they might drive differences in COVID-19 recrudescence after relaxation of social distancing.
RESULTS
Between 19 March and 7 April 2020, all 51 jurisdictions implemented at least 1 social distancing measure, and most (45 [88%]) implemented a statewide restriction on internal movement (Supplementary Table 1). A median of 47 days after social distancing measures were first implemented (interquartile range [IQR], 41–53), between 20 April and 1 June 2020, all 51 jurisdictions relaxed at least one statewide social distancing measure (Supplementary Figure 1). The median number of cumulative cases per state on the date of relaxation was 7883 (IQR, 3160–23 650). The median number of cumulative COVID-19-attributable deaths per state on the date of first relaxation was 272 (IQR, 113–1056). There was variation in which social distancing measures were initially relaxed. Easing of work restrictions was the most common element of initial relaxation orders in 40 (78%) jurisdictions, followed by reopening of service industry establishments (32 [63%]), reopening outdoor recreational facilities (22 [43%]), rescission of statewide restrictions on internal movement (16 [31%]), and sanctioning of public events (14 [27%]). Only 4 states (8%) reopened public schools, and none rescinded mandatory quarantines for interstate travel, as part of their initial relaxation orders.
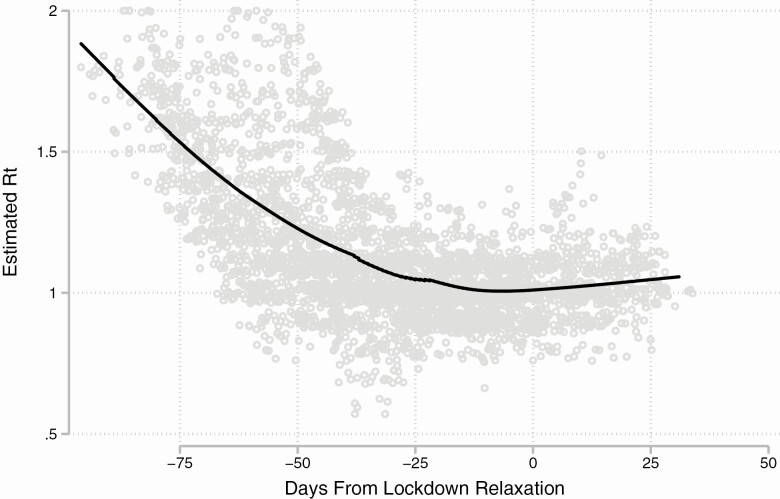
Figure 1 displays a scatterplot of the estimated Rt for each state by day, before versus after the first social distancing measures were relaxed, along with a smoothed line derived from locally weighted scatterplot smoothing. During the 8 weeks prior to the first date in each state that social distancing measures were initially relaxed, the estimated Rt declined by an average of 0.012 per day (95% confidence interval [CI], −.013 to −.012) (Table 1). This period corresponded with a decline from a modeled mean Rt across all states of 1.44 (95% CI, 1.41–1.48) to .75 (95% CI, .72–.78). After the first social distancing measures were relaxed, the estimated Rt reversed course and began increasing by an average of .019 per day (95% CI, .018–.020) compared with the prerelaxation period, such that the mean increase in Rt in the postrelaxation period was .007 units per day (95% CI, .006–.007), and reached a mean of 1.16 (95% CI, 1.13–1.18) by 56 days after relaxation. If these trends were to continue, the estimated mean Rt would cross 1.50 by approximately 16 weeks after relaxation.
Figure 1.
Scatterplot of the estimated Rt for each state by day before and after the first date of relaxation of social distancing measures, along with a smoothed line derived from locally weighted scatterplot smoothing.
Table 1.
Mixed Effects Linear Regression Models for the Estimated Rt Before Versus After Relaxation of Social Distancing Measures
| Coefficienta | 95% Confidence Interval | P value | |
|---|---|---|---|
| Constant term (day prior to relaxation) | .761 | .728, .793 | <.001 |
| Prerelaxation period (days relative to relaxation) | −.012 | −.013, −.012 | <.001 |
| Postrelaxation period intercept | .032 | .010, .054 | .005 |
| Time × postrelaxation period (days relative to relaxation) | .019 | .018, .020 | <.001 |
| Postrelaxation period (days relative to relaxation)b | .007 | .006, .007 | <.001 |
aEstimates adjusted for day of the week and population density.
bThe postrelaxation term represents the linear combination of the prerelaxation period and the time × postrelaxation period coefficient.
Results were qualitatively similar irrespective of the nature of the first social distancing measures relaxed (Table 2). For each of these regression models, we estimated a statistically significant reversal of Rt from negative to positive after the change from the pre- to postrelaxation period, with estimates ranging from .015 (95% CI, .013–.016) for the 4 jurisdictions that reopened public schools as part of their initial relaxation orders, to a maximum of .022 (95% CI, .021–.023) for the 16 jurisdictions that rescinded statewide restrictions on internal movement as part of their initial relaxation orders.
Table 2.
Mixed Effects Linear Regression Models for the Estimated Rt Before Versus After Relaxation of Social Distancing Measures, Stratified by Characteristics of the First Relaxation Order
| Measure Relaxeda | Jurisdictions in Which This Element Was Included in the Initial Relaxation | Mean Estimated Daily Change in Rt prior to Relaxation | 95% Confidence Interval | P value | Mean Estimated Daily Change in Rt Following Relaxationb | 95% Confidence Interval | P value |
|---|---|---|---|---|---|---|---|
| Reopening public schools | 4 | −.005 | −.007, −.004 | <.001 | .009 | .008, .010 | <.001 |
| Easing of work restrictions | 40 | −.011 | −.012, −.011 | <.001 | .007 | .006, .007 | <.001 |
| Reopening of service industry establishment | 32 | −.011 | −.012, −.010 | <.001 | .007 | .006, .007 | <.001 |
| Sanctioning public events | 14 | −.008 | −.009, −.007 | <.001 | .008 | .008, .009 | <.001 |
| Reopening of outdoor recreational facilities | 22 | −.015 | −.016, −.014 | <.001 | .006 | .005, .006 | <.001 |
| Rescission of statewide restrictions on internal movement | 16 | −.012 | −.013, −.011 | <.001 | .010 | .009, .010 | <.001 |
aEach line corresponds to a separate regression model in which the primary explanatory variables of interest were time in days, relaxation period (relative to the specific type of social distancing measure described in the row header), and a time-by-relaxation-period product term. Estimates were also adjusted for day of the week and population density.
bThe postrelaxation term represents the linear combination of the prerelaxation period and the time × postrelaxation period coefficient.
Our estimates were robust to several sensitivity analyses (Supplementary Table 2). When we redefined the primary explanatory variable of interest as the period before versus after rescission of statewide restrictions on internal movement, the estimated Rt declined by an average of .004 per day (95% CI, −.005 to −.004) in the prerelaxation period. After statewide restrictions on internal movement were lifted, the estimated Rt reversed course and began increasing by an average of .013 per day (95% CI, .011–.014) compared with the prerelaxation period. The estimated regression coefficient on the time-by-post-relaxation period product term was attenuated in magnitude, and slightly attenuated in statistical significance, when we used the Rt estimates based on the daily number of infections and an uncertain generation time, as calculated by Abbott et al [34]. The generalized estimating equations specification changed little. Finally, our results remained similar after varying the duration of the prerelaxation period from 14 to 42 days, with a downward slope in the prerelaxation period as we shorted its duration but with persistently significant reversals in the postrelaxation period. When we specified log change in cases and log changes in deaths as the primary outcome of interest, we similarly found a strongly significant conversion from a downward slope to a flattening of the growth rate, corresponding to a consistent rate of increase in cases and deaths.
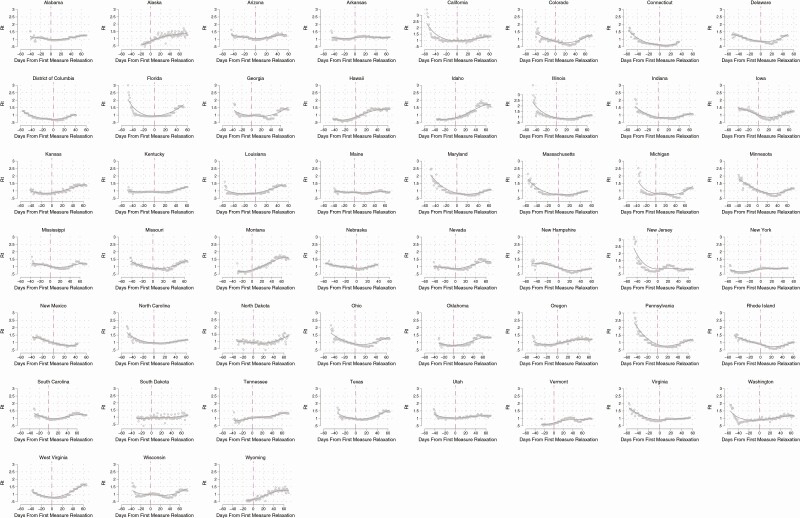
State-specific trajectories of Rt during the pre- and post-relaxation periods are depicted in Figure 2. Forty-four (86%) jurisdictions successfully established a mean downward trajectory in Rt in the prerelaxation period and nearly all (46 [90%])—save Arkansas, Minnesota, Mississippi, Tennessee, and Wisconsin—achieved an Rt < 1.0, by the time they begun relaxing social distancing measures. However, only 4 states (8%) maintained a negative trend in Rt after relaxation of social distancing: Alaska, New York, South Dakota, and Tennessee. Nine jurisdictions (18%) maintained an Rt < 1.0 at 8 weeks following relaxation: Connecticut, the District of Columbia, Maine, Massachusetts, New Hampshire, New Jersey, New Mexico, New York, and Vermont.
Figure 2.
State-specific scatterplots of the estimated Rt by day, before vs after the first date that social distancing measures were relaxed, along with a smoothed line derived from locally weighted scatterplot smoothing.
When we modeled Rt in the postrelaxation period to identify correlates of epidemic control after relaxation, we found that states with a lower number of cases and deaths at the time of relaxation, and a lower zenith Rt in the prerelaxation period, had slightly greater increases in the daily Rt during the postrelaxation period compared with jurisdictions in which the epidemic was more severe prior to or at the time of initial relaxation (Supplementary Table 3). Only 9 states (18%) states had achieved a 14-day test-positive rate of <5% at the time of relaxation. Both Rt < 0.9 and a test positive rate <5% on the date of relaxation correlated with greater epidemic growth after relaxation (Supplementary Table 3, Supplementary Figure 2).
DISCUSSION
In this national study observing the COVID-19 epidemic during the period April—July 2020 in the United States, we found that relaxation of statewide social distancing measures was associated with a reversal of the downward trend in transmission of SARS-CoV-2 that had been achieved after these measures were implemented. In all but 9 states, the reversal returned the estimated Rt back above 1.0 within 8 weeks of the initial relaxation of social distancing measures—leading to increased transmission, an increased number of cases, and an increased number of deaths. These patterns were apparent irrespective of the specific kinds of social distancing measures that were rescinded and also irrespective of key indicators of epidemic severity (eg, test positivity rate) that have been heretofore used by many jurisdictions to guide relaxation decisions [38]. Our findings, in combination with prior data noting the strong and significant effect on epidemic interruption after implementation of measures [4–9], should motivate policy makers to reconsider the rapid pace at which states are reopening their economies. Furthermore, in the states that are currently experiencing a recrudescence of SARS-CoV-2 transmission, strong consideration should be given to the reimposition of social distancing measures—in the setting of appropriate social protection measures—so that new infections of COVID-19 do not overwhelm the local healthcare system. Intermittent social distancing regulations may be necessary to control the COVID-19 epidemic in the United States until more effective treatments or an effective vaccine become available and achieve widespread dissemination in the population [25].
Little data exist to inform the US exit strategy from its current state of social distancing measures. The city of Wuhan in Hubei Province, China, was the first to enter a regime of strict social distancing (beginning 23 January 2020), but the relaxation of these measures has not resulted in a resurgence of SARS-CoV-2 transmission [39]. Within 2 months, the Chinese government was able to achieve the milestone of having 5 consecutive days in which there were no new locally transmitted cases in the country [40]. Modeling studies, however, suggest that stringent social distancing should have been maintained for longer than the median duration observed in the United States and that social distancing should have been leveraged as a strategy for suppressing SARS-CoV-2 transmission so that additional nonpharmaceutical interventions (eg, contact tracing and increased availability of testing) could be deployed [19–25]. Moreover, deconfinement should have occurred gradually and, in the setting of contiguously connected jurisdictions (eg, countries in Europe or states in the US), should have been coordinated across jurisdictions to maximize the probability of successful deconfinement [41].
We found that states with more severe epidemics at the time social distancing measures were relaxed had reduced postrelaxation epidemic growth, compared with states that had experienced smaller epidemics. These differences were small in magnitude but precisely estimated. This finding suggests that individuals living in states with large epidemics might be more likely to maintain social distancing even after local orders are formally lifted. These results are in keeping with data from survey respondents in New York City and Los Angeles during the peak of their epidemics, who showed near unanimous support for such measures in locations that had suffered severe epidemics [42]. There may be other phenomena underlying this finding, each of which may have partial explanatory power, such as the possibility that a strong local response could have improved trust in scientists and government [43] or that people living in these states would have been more likely to adhere to social distancing guidelines even if their state governments had not, contrary to fact, implemented statewide social distancing measures [16, 18, 44, 45].
We also explored whether epidemic indicators can be used to guide reopening. One such indicator, recommended by the World Health Organization [38] and multiple US states, is a test positive rate <5% over the previous 14 days. Although only a handful of states met this recommended threshold at the time their social distancing measures were first relaxed, those that did unexpectedly experienced a greater increase in epidemic transmission following relaxation. Similarly, states with a lower Rt at the time of relaxation saw a faster subsequent increase. In summary, in the United States there appeared to be a paradoxical inverse correlation between indicators of epidemic control at the time social distancing measures were relaxed and subsequent trajectories of SARS-CoV-2 transmission. Indeed, these data might suggest that if people interpret state government-ordered relaxation of social distancing measures as a signal that the local epidemic is under control and, as a result, disregard social distancing practices that are not otherwise mandated (eg, mask wearing and physical distancing), a counterintuitive worsening of the local epidemic might follow the rescission of state-ordered social distancing measures [46].
The primary limitation of our analysis is the potential for confounding by phenomena that may have occurred simultaneously with relaxation of social distancing measures and that also influenced the trajectories of Rt. For example, if a social movement supportive of a reopening agenda [47] advocates for relaxation of state-mandated social distancing measures and independently influences nonmandated social distancing behaviors [16, 18], our estimates of the effect of rescission on epidemic control would be biased away from the null. However, we found similar effect sizes and time-specific reversal in Rt trends across most states, irrespective of political and demographic characteristics. Moreover, because relaxation of social distancing measures took place across a wide range of dates, such potentially confounding factors would have had to have occurred independently across multiple states and coincided with relaxation of multiple state measures.
Notwithstanding this potential limitation, our findings suggest that suppression of SARS-CoV-2 after rescission of statewide social distancing measures has failed. Robust surveillance programs are needed so that, should the observed trends continue, state and local public health policy makers can continuously evaluate the stringency of social distancing measures required to prevent subsequent epidemic surges [19–26] while minimizing the extent of social and economic harms [11–15, 48]. Considering the current projected timelines for vaccine development [49], the low levels of cumulative population infection even in countries that have experienced severe epidemics [50, 51], and the disproportionate manner in which the burden of reopening has been shouldered by racialized minority populations [27], thoughtful public health leadership will be needed to ensure that COVID-19-attributed mortality and intersecting harms are maximally prevented [3].
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Financial support. This work was supported by the National Institutes of Health (R01 AI058736). ACT receives funding from the Sullivan Family Foundation.
Potential conflicts of interest. A. C. T. acknowledges funding from the Sullivan Family Foundation. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020; 20:533–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gravlee CC. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am J Hum Biol 2020:e23482. doi: 10.1002/ajhb.23482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tsai AC, Venkataramani AS. US elections: treating the acute-on-chronic decompensation. Lancet Public Health 2020; 5:E519–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hsiang S, Allen D, Annan-Phan S, et al. . The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020; 584:262–7. [DOI] [PubMed] [Google Scholar]
- 5. Siedner MJ, Harling G, Reynolds Z, et al. . Social distancing to slow the US COVID-19 epidemic: longitudinal pretest-posttest comparison group study. PLoS Med 2020; 17:e1003244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood) 2020; 39:1237–46. [DOI] [PubMed] [Google Scholar]
- 7. Yehya N, Venkataramani A, Harhay MO. Statewide interventions and COVID-19 mortality in the United States: an observational study. Clin Infect Dis 2020; doi: 10.1093/cid/ciaa923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flaxman S, Mishra S, Gandy A, et al. ; Imperial College COVID-19 Response Team . Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020; 584:257–61. [DOI] [PubMed] [Google Scholar]
- 9. Chinazzi M, Davis JT, Ajelli M, et al. . The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020; 368:395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weill JA, Stigler M, Deschenes O, Springborn MR. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proc Natl Acad Sci U S A 2020; 117:19658–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Roberton T, Carter ED, Chou VB, et al. . Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020; 8:e901–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bonaccorsi G, Pierri F, Cinelli M, et al. . Economic and social consequences of human mobility restrictions under COVID-19. Proc Natl Acad Sci U S A 2020; 117:15530–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chetty R, Friedman JN, Hendren N, Stepner M; The Opportunity Insights Team. How did COVID-19 and stabilization policies affect spending and employment? A new real-time economic tracker based on private sector data. NBER Working Paper No. 27431. Cambridge: National Bureau of Economic Research, 2020. [Google Scholar]
- 14. Bartik AW, Bertrand M, Cullen Z, Glaeser EL, Luca M, Stanton C. The impact of COVID-19 on small business outcomes and expectations. Proc Natl Acad Sci U S A 2020; 117:17656–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ettman CK, Gradus JL, Galea S. Reckoning with the relation between stressors and suicide attempts in a time of COVID-19. Am J Epidemiol 2020; doi: 10.1093/aje/kwaa147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Allcott H, Boxell L, Conway J, Gentzkow M, Thaler M, Yang D. Polarization and public health: partisan differences in social distancing during the coronavirus pandemic. J Public Econ 2020; doi: 10.1016/j.jpubeco.2020.104254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Li HL, Jecker NS, Chung RY. Reopening economies during the COIVD-19 pandemic: reasoning about value tradeoffs. Am J Bioeth 2020; 20:136–8. [DOI] [PubMed] [Google Scholar]
- 18. Kavanagh NM, Goel RR, Venkataramani AS. Association of county-level socioeconomic and political characteristics with engagement in social distancing for COVID-19. medRxiv 2020; doi: 10.1101/2020.04.06.20055632. [DOI] [Google Scholar]
- 19. Aleta A, Martín-Corral D, Pastore Y Piontti A, et al. . Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat Hum Behav 2020; 4:964–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tuite AR, Fisman DN, Greer AL. Mathematical modelling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. CMAJ 2020; 192:E497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baqaee D, Farhi E, Mina MJ, Stock JH.. Reopening scenarios. NBER Working Paper 27244. Cambridge: National Bureau of Economic Research, 2020. [Google Scholar]
- 22. López L, Rodó X. The end of social confinement and COVID-19 re-emergence risk. Nat Hum Behav 2020; 4:746–55. [DOI] [PubMed] [Google Scholar]
- 23. Gilbert M, Dewatripont M, Muraille E, Platteau JP, Goldman M. Preparing for a responsible lockdown exit strategy. Nat Med 2020; 26:643–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lai S, Ruktanonchai NW, Zhou L, et al. . Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020; 585:410–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020; 368:860–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tuite AR, Greer AL, De Keninck S, Fisman DN. Risk for COVID-19 resurgence related to duration and effectiveness of physical distancing in Ontario, Canada. Ann Intern Med 2020; doi: 10.7326/M20-2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Williams JC, Anderson N, Holloway T, Samford E 3rd, Eugene J, Isom J. Reopening the United States: Black and Hispanic workers are essential and expendable again. Am J Public Health 2020; 110:1506–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chowell G, Viboud C, Hyman JM, Simonsen L. The Western Africa Ebola virus disease epidemic exhibits both global exponential and local polynomial growth rates. PLoS Curr 2015; 7. doi: 10.1371/currents.outbreaks.8b55f4bad99ac5c5db3663e916803261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gostic KM, McGough L, Baskerville E, et al. . Practical considerations for measuring the effective reproductive number, Rt. medRxi 2020; doi: 10.1101/2020.06.18.20134858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Unwin HJT, Mishra S, Bradley VC, et al. . State-level tracking of COVID-19 in the United States. medRxiv 2020; doi: 10.1101/2020.07.13.20152355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Havers FP, Reed C, Lim T, et al. . Seroprevalence of antibodies to SARS-CoV-2 in 10 sites in the United States, March 23–May 12, 2020. JAMA Int Med 2020; doi: 10.1001/jamainternmed.2020.4130. [DOI] [PubMed] [Google Scholar]
- 32. Maxmen A. Thousands of coronavirus tests are going unused in US labs. Nature 2020; 580:312–3. [DOI] [PubMed] [Google Scholar]
- 33. Buckingham-Jeffery E, Morbey R, House T, Elliot AJ, Harcourt S, Smith GE. Correcting for day of the week and public holiday effects: improving a national daily syndromic surveillance service for detecting public health threats. BMC Public Health 2017; 17:477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Abbott S, Hellewell J, Thompson RN, et al. . Estimating the time-varying reproduction number of SARS-CoV-2 using national and subnational case counts. Wellcome Open Res 2020; 5:112. [Google Scholar]
- 35. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill 2020; 25:2000062. Available at: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lauer SA, Grantz KH, Bi Q, et al. . The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020; 172:577–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zhou F, Yu T, Du R, et al. . Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. World Health Organization. Public health criteria to adjust public health and social measures in the context of COVID-19: annex to “Considerations in adjusting public health and social measures in the context of COVID-19.” Geneva: World Health Organization, 2020. [Google Scholar]
- 39. Ainslie KEC, Walters CE, Fu H, et al. . Evidence of initial success for China exiting COVID-19 social distancing policy after achieving containment. Wellcome Open Res 2020; 5:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Normile D. As normalcy returns, can China keep COVID-19 at bay? Science 2020; 368:18–9. [DOI] [PubMed] [Google Scholar]
- 41. Ruktanonchai NW, Floyd JR, Lai S, et al. . Assessing the impact of coordinated COVID-19 exit strategies across Europe. Science 2020; 369:1465–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Czeisler MÉ, Tynan MA, Howard ME, et al. . Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance–United States, New York City, and Los Angeles, May 5–12, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:751–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sibley CG, Greaves LM, Satherley N, et al. . Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am Psychol 2020; 75:618–30. [DOI] [PubMed] [Google Scholar]
- 44. Bierwiaczonek K, Kunst JR, Pich O. Belief in COVID-19 conspiracy theories reduces social distancing over time. Appl Psychol Health Well Being 2020; doi: 10.1111/aphw.12223. [DOI] [PubMed] [Google Scholar]
- 45. Rothgerber H, Wilson T, Whaley D, et al. . Politicizing the COVID-19 pandemic: ideological differences in adherence to social distancing. PsyArXiv 2020; doi: 10.31234/osf.io/k23cv. [DOI] [Google Scholar]
- 46. Glaeser EL, Jin GZ, Leyden BT, Luca M.. Learning from deregulation: the asymmetric impact of lockdown and reopening on risky behavior during COVID-19. NBER Working Paper No. 27650. Cambridge: National Bureau of Economic Research, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tanne JH. Covid-19: US cases soar as Trump pushes for schools to open. BMJ 2020; 370:m2803. [DOI] [PubMed] [Google Scholar]
- 48. Akbarpour M, Cook C, Marzuoli A, et al. . Socioeconomic network heterogeneity and pandemic policy response. NBER Working Paper No. 27374. Cambridge: National Bureau of Economic Research, 2020. [Google Scholar]
- 49. Corey L, Mascola JR, Fauci AS, Collins FS. A strategic approach to COVID-19 vaccine R&D. Science 2020; 368:948–50. [DOI] [PubMed] [Google Scholar]
- 50. Pollán M, Pérez-Gómez B, Pastor-Barriuso R, et al. ; ENE-COVID Study Group . Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet 2020; 396:535–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Silveira MF, Barros AJD, Horta BL, et al. . Population-based surveys of antibodies against SARS-CoV-2 in Southern Brazil. Nat Med 2020; 26:1196–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.