Abstract
Background
As much as the world was hoping that COVID-19 would quickly burn out, it is becoming increasingly likely that there will be no magic bullet to bring the pandemic to an end. Although recent vaccine developments have been encouraging, the persistence of the virus appears to be likely with the severe acute respiratory syndrome coronavirus 2 virus becoming endemic throughout the world.
Methods
This article summarizes a presentation at the American Association of Hip and Knee Surgeons 2020 Annual Meeting on “Optimizing Hip and Knee Arthroplasty in the COVID Era”. This new reality presents an opportunity for arthroplasty surgeons to leverage new technologies and change practice habits to keep patients and providers safe.
Results
Both early discharge and telehealth can be leveraged in the COVID-19 era to help address some of the challenges of the pandemic. However, concerns and limitations with both approaches need to be considered when implementing in practice.
Conclusions
The continued practice of elective hip and knee arthroplasty relies on providers adapting to “the new normal.” The extent to which these technologies and changes in practice will persist beyond the pandemic is unclear.
Keywords: rapid discharge, length of stay, telehealth, telemedicine, COVID
The COVID-19 pandemic has stressed the practice of total joint arthroplasty in ways that could not have been predicted or anticipated. The desire to provide safe care to arthroplasty patients while minimizing personal contact has fueled interest in further minimizing length of stay and expanding the use of telemedicine. This manuscript is a summary of a symposium presentation on these topics from the American Association of Hip and Knee Surgeons 2020 Annual Meeting on November 7, 2020.
Early Discharge
The movement toward reduced length of stay and same-day discharge is not new. Efforts to reduce the time spent in the hospital postoperatively have been going on for decades and remarkable progress has been made. A decade ago the average length of stay in the United States after total knee arthroplasty was 3.3 days [1]; at the start of 2020 prior to the COVID-19 pandemic, the average length of stay at our institution was down to 1.7 days, with select patients being discharged on the same day of surgery. The American Joint Replacement Registry has shown a similar trend, with a 1 day reduction in mean length of stay for both primary hip and knee arthroplasty since 2012 [2]. Despite concerns about early discharge, a simultaneous decrease in early complication and readmission rates has been documented [1].
Although eliminating unnecessary inpatient services and improving efficiency of care has always been important, the COVID-19 pandemic has served to heighten the importance of early discharge. With many hospitals having a reduced capacity to care for non-COVID patients, the ability to keep beds open is crucial for both COVID and non-COVID care alike. Avoiding repeat moratoriums on elective arthroplasty surgery requires adequate personal protective equipment, bed availability, and staffing availability. Early discharge is a way to conserve all of these critical resources.
As one might expect during a pandemic with a highly transmissible virus, patients are typically aligned with hospital and providers in not wanting to spend more time in the hospital or ambulatory surgery center than is absolutely necessary. The risk of hospital-acquired transmission of COVID has shifted the mindset of patients who historically may have been predisposed to a longer hospital stay. How patients cope with the stress of an illness or surgery is dependent on the threats that concern the patient; what a person does to cope depends upon the context in which the disease occurs [3]. Patients’ willingness to cope with pain and reduced mobility at home is likely to correlate with their perception of risk of COVID transmission with a prolonged stay in a healthcare environment. This factor alone is likely to accelerate efforts at early discharge as having a motivated patient is perhaps the most important factor in same-day surgery. However, patient and provider enthusiasm for early discharge must not override medical concerns. Appropriate protocols and patient selection tools must still be used to ensure patient safety [4].
Nosocomial transmission of severe acute respiratory syndrome coronavirus 2 virus is certainly a real threat and a concern for surgeons and patients. Good epidemiological data about the rates of hospital-acquired disease is sparse at this point. The implementation of comprehensive infection prevention and control measures by hospitals has reduced the transmission rates [5]. Some reports have suggested that community transmission is more common than nosocomial spread, with whole genome sequencing studies suggesting that widespread nosocomial spread is unlikely to be occurring [6]. Patients can thus be reassured that the absolute risk of hospital transmission with arthroplasty appears low and is likely lower than in the community, assuming a low underlying prevalence of the disease and the implementation of rigorous infection prevention and control measures.
Although early or same-day discharge may be an option for young and healthy patients, elderly patients with multiple comorbidities may not be safe for early discharge candidates. These are the same patients who have a dramatically increased risk for hospitalization and death due to COVID-19 [7]. Many of these patients may also live in a congregate living environment such as an assisted living center or skilled nursing facility. Consideration should be given to postponing elective surgery for patients coming from these environments if there are local outbreaks of disease. Shared decision-making with these patients is particularly important when weighing the risks of elective surgery during a pandemic. Extra time should also be spent on discharge planning preoperatively to ensure a safe discharge to home and avoidance of discharge to skilled nursing or rehab facilities.
Telehealth Technology
COVID-19 has resulted in a dramatic acceleration in the use of telehealth in medicine. The desire to avoid personal contact and the potential for virus transmission led to a rapid adoption of virtual visits in all aspects of healthcare including total joint arthroplasty. Telemedicine allowed for convenient and safe access to both urgent and routine care without the risk of exposure. Besides eliminating the potential for virus transmission, telemedicine also offers the promise of increased access, convenience, and reduced overall costs.
Prior to COVID-19, telemedicine had not been widely adopted in arthroplasty practices. A notable disconnect existed between provider and patient interest in telemedicine and actual utilization of this technology. Despite over 80% of employers offering health benefits that cover telemedicine and the increasing use of digital technology in our daily lives, only 2%-10% of employees with eligible coverage had actually tried at least one annual telemedicine visit [8]. Early in the pandemic there was the sense that COVID would provide the tipping point that would finally push telemedicine into regular everyday practice. The assumption was that the necessary implementation of telemedicine would raise awareness and improve comfort with this technology, leading to widespread and sustained adoption that would persist long after the pandemic had subsided.
When the pandemic hit, several articles were published in the orthopedic literature that outlined how to establish outpatient telemedicine practices for the arthroplasty population and the factors and barriers that had to be overcome [9]. Table 1 lists some of these factors that need to be considered when implementing telemedicine. The implementation of a telemedicine program can be complex and time consuming and is beyond the scope of this article. The American Medical Association has published a playbook for the implementation of telemedicine which provides a detailed pathway for those embarking on this journey [10]. Implementing telemedicine requires effort and input from a team that includes the surgeon and care team in addition to financial, administrative, information technology, and legal champions.
Table 1.
Factors to Consider and Barriers to Overcome When Implementing Telemedicine in an Arthroplasty Practice.
| Patient readiness and informed consent |
| Technology and equipment |
| Technical support |
| Staff and provider training |
| Compliance issues (HIPAA, Stark, Anti-Kickback) |
| Licensure and liability |
| Reimbursement |
Multiple federal and state policy changes were made at the start of the pandemic to encourage the adoption of telemedicine. These changes expanded Current Procedural Terminology codes, allowed home to be an eligible patient origination site, and relaxed The Health Insurance Portability and Accountability Act and Stark provisions. Favorable changes in reimbursement in response to the pandemic may have assisted in the rapid adoption of telemedicine. The Coronavirus Preparedness and Response Supplemental Appropriations Act, passed on March 6, 2020, expanded funding to support all telemedicine services to Medicare patients during the pandemic. Many Medicaid programs mirrored Medicare. Several insurance companies also waived patient cost-sharing for telehealth and expanded their coverage and reimbursement for telehealth services.
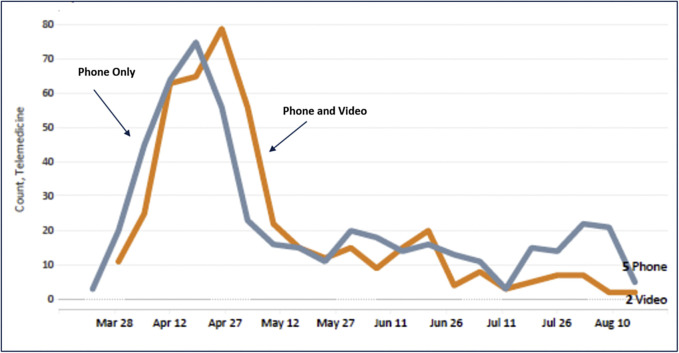
The pandemic and efforts to deregulate telemedicine resulted in a dramatic increase in the use of telehealth across the country. Figure 1 shows the telemedicine experience of a large orthopedic department at an academic medical center. It is notable that the rapid increase in use of virtual visits was followed by a slow decline in the use of telemedicine following the reopening of clinics and the return to elective orthopedic surgery. This pattern of telemedicine utilization—rapid uptick in use in March, peak in April, and steady decline in utilization since—has been shown in national studies across different patient demographics and in multiple medical and surgical specialties [11]. By October, telehealth usage as a percentage of total visits during the baseline week was only 1% in orthopedic surgery, with orthopedic surgeons appearing less amenable to telehealth than providers in other specialties [11]. It is thus not clear that the shift to telehealth will persist in the arthroplasty community after the immediate crisis has passed. As arthroplasty clinics learn how to safely reopen with masking and social distancing in effect, many practices have shifted the majority of patient visits back to in-person encounters.
Fig. 1.
Telehealth visits performed by one orthopedic surgery practice at a large academic medical center between March and August 2020.
Why the lack of sustained use of telemedicine? There are likely multiple reasons. Certainly some of the resistance and lack of sustained enthusiasm rests with the clinicians. Although an emergency situation may be enough motivation to adopt new technology, the duration of adoption may not have been long enough for clinicians and their staff to get comfortable with the new telehealth platforms. Additionally, as the perceived risk of COVID decreased and the mitigation efforts were implemented, telemedicine appointments were likely seen as inferior to in-person visit for certain patients, including those who require a physical examination or radiographs. Even at the height of the pandemic, orthopedic providers reported that only one-third of their patients were appropriate for telemedicine visits [12]; it is hard to make a substantial investment in a patient care delivery model that is perceived as inferior for the majority of patients. Long-term adoption of telemedicine will require physician acceptance and health system efforts to make this technology available and convenient for the majority of patients.
Patients may also be a driving force in the lack of sustained demand for telemedicine. Some have asserted that increasingly tech-savvy patients will drive the adoption of this technology through increasing consumer demand [13]. However, a recent survey of arthroplasty patients during the COVID-19 pandemic suggested that a large majority prefer in-person visits; only 28% of patients who had completed a telemedicine visit reported that they would prefer future visits to be conducted via telemedicine for reasons unrelated to COVID-19 [14]. Another separate survey of arthroplasty patients revealed that 80% of patients rank in-person visits as their first choice [15]. The underlying reason for this lack of enthusiasm may be due to the older age of arthroplasty patients; patients over the age of 65 years are less likely to voluntarily choose telemedicine compared to younger patients [11]. The lack of personal contact and emotional connection to their caregivers, as well as a perception that telemedicine provides a lower level of care, may underlie patient preference for in-person visits.
Conclusion
As the slow burn of the COVID-19 pandemic continues, it is clear that many behavioral changes, such as wearing masks, hand washing, and social distancing, will persist for a long time to come. Conserving resources and minimizing personal contact have become ingrained in our practices. It is likely that the accelerated trend to short stay and outpatient arthroplasty will continue and is unlikely to reverse course. However, the future of telemedicine is less clear, particularly if many of the policy changes favorable to telemedicine are reversed. Although telemedicine has been an important tool during this pandemic, and will no doubt continue to have an important role as the waves of the pandemic continue, it seems that the majority of arthroplasty visits will remain in person for the foreseeable future.
Footnotes
This talk was part of the AAHKS 2020 Annual Meeting Symposium “Optimizing Hip and Knee Arthroplasty in the COVID Era”.
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2021.01.009.
Appendix A. Supplementary Data
References
- 1.Sarpong N.O., Boddapati V., Herndon C.L., Shah R.P., Cooper H.J., Geller J.A. Trends in length of stay and 30-day complications after total knee arthroplasty: an analysis from 2006 to 2016. J Arthroplasty. 2019;34:1575–1580. doi: 10.1016/j.arth.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 2.American Joint Replacement Registry (AJRR): 2020 annual report. https://www.aaos.org/registries/publications/ajrr-annual-report/ [accessed 10.11.20]
- 3.Lazarus R.S. Coping theory and research: past, present, and future. Psychosom Med. 1993;55:234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Meneghini R., Gibson W., Halsey D., Padgett D., Berend K., Della Valle C.J. The American Association of Hip and Knee Surgeons, Hip Society, Knee Society, and American Academy of Orthopaedic Surgeons position statement on outpatient joint replacement. J Arthroplasty. 2018;33:3599–3601. doi: 10.1016/j.arth.2018.10.029. [DOI] [PubMed] [Google Scholar]
- 5.Rickman H.M., Rampling T., Shaw K., Martinez-Garcia G., Hail L., Coen P., et al. Nosocomial transmission of COVID-19: a retrospective study of 66 hospital-acquired cases in a London teaching hospital. Clin Infect Dis. 2020 Jun 20 doi: 10.1093/cid/ciaa816. ciaa816. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sikkema R.S., Pas S.D., Nieuwenhuijse D.F., O’Toole Á, Verweij J, van der Linden A, et al. COVID-19 in health-care workers in three hospitals in the south of The Netherlands: a cross-sectional study [published online ahead of print, 2020 Jul 2] [published correction appears in Lancet Infect Dis. 2020;20(11):1273-1280. doi: 10.1016/S1473-3099(20)30527-2. Epub 2020 Jul 2. Erratum in: Lancet Infect Dis. Lancet Infect Dis. 2020;20:e215. doi: 10.1016/S1473-3099(20)30527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html [accessed 21.08.20]
- 8.Makhni M.C., Riew G.J., Sumathipala M.G. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. 2020;102:1109–1115. doi: 10.2106/JBJS.20.00452. [DOI] [PubMed] [Google Scholar]
- 9.Rao S.S., Loeb A.E., Amin R.M., Golladay G.J., Levin A.S., Thakkar S.C. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020 doi: 10.1016/j.artd.2020.04.014. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Medical Association Digital Health Implementation Playbook Series. https://www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf [accessed 10.11.20]
- 11.Mehotra A., Chernew M., Linetsky D., Hatch H., Cutler D., Schneider E.C. Commonwealth Fund; 2020. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. [accessed 10.11.20] [DOI] [Google Scholar]
- 12.Loeb A.E., Rao S.S., Ficke J.R., Morris C.D., Riley L.H., 3rd, Levin A.S. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wongworawat M.D., Capistrant G., Stephenson J.M. The opportunity awaits to lead orthopaedic telehealth innovation: AOA critical issues. J Bone Joint Surg Am. 2017;99:e93. doi: 10.2106/JBJS.16.01095. [DOI] [PubMed] [Google Scholar]
- 14.Buchalter DB, Sicat C, Moses MJ, Aggarwal VK, Hepinstall M, Lajam CM, et al. Telemedicine during the COVID-19 pandemic: adult reconstructive surgery perspective. Presented at the 2020 Knee Society Members Meeting, Sept 11, 2020.
- 15.Barrack RL. Telemedicine for total hip and knee arthroplasty patients: access, ability and preferences. Presented at the Hip Society Summer Meeting, October 2, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.