Abstract
Extraocular muscle (EOM) entrapment with resulting reduction in motility and diplopia is a known complication of orbital fractures. Less commonly, transection of the EOMs due to trauma, iatrogenic injury, or intentional myotomy may lead to persistent diplopia. The inferior oblique (IO) is often encountered during orbital surgery along the medial wall and floor, and may be disinserted to aid in visualization. The authors present a case of IO entrapment which occurred during zygomaticomaxillary fracture reduction. Intraoperatively, an IO transection was performed and the muscle was reattached within the orbit. Postoperatively, the patient did not develop diplopia or motility disruption. This technique may provide a useful solution to an unusual problem during orbital fracture repair.
Keywords: orbital fracture, orbital trauma, extraocular muscle entrapment
Introduction
Transection of the extraocular muscles (EOMs) occurs due to trauma, iatrogenic injury, or intentional disinsertion or myotomy during orbital surgery. Patients may sustain residual motility dysfunction and resulting diplopia, especially in cases involving the recti muscles. Disinsertion of the inferior oblique (IO) during orbital surgery is a well-established technique to improve visualization and access to the orbital floor and medial wall.1,2 Diplopia is less common in these cases, despite techniques ranging from re-suturing the cut muscle, to simply repositing the muscle in the orbit without additional fixation.1
Herein, the authors present a case of IO transection and repair during a complex facial fracture repair. This report was performed in compliance with the Declaration of Helsinki, and patient information is presented in accordance with HIPPA regulations.
Case
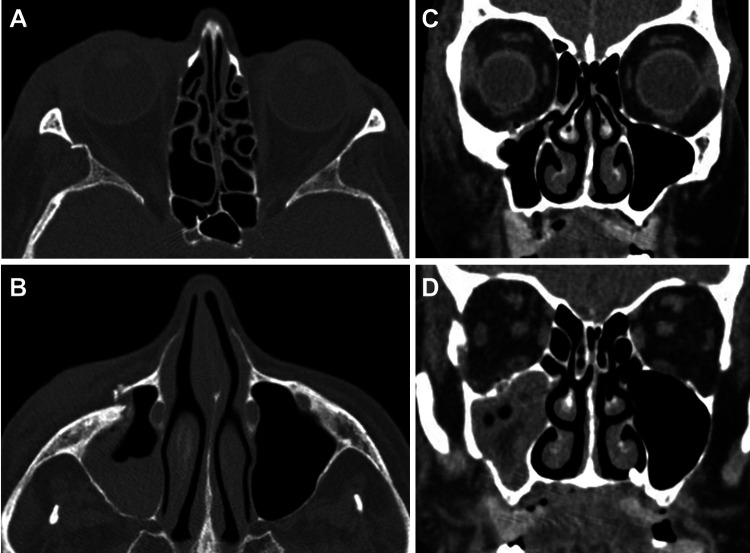
An 84-year-old woman presented to the emergency department after sustaining a fall with loss of consciousness. On examination, she had right periorbital ecchymosis, periorbital edema, and a small laceration below the right lateral eyebrow. Vision was 20/40 bilaterally with no afferent pupillary defect. Her extraocular motility was full and she denied diplopia. She had a right subconjunctival hemorrhage, but the remainder of her anterior and posterior segment exam was normal. Computed tomography (CT) of the head and orbits demonstrated an acute, comminuted, and depressed fracture of the anterior and posterolateral wall of the maxillary sinus, as well as acute fracture of the right orbital floor, orbital rim, and lateral orbital wall (Figure 1). There was no sign of EOM entrapment. It was decided to proceed with surgical repair of her facial fractures.
Figure 1.
Preoperative CT scans demonstrating: (A) axial section with right lateral orbital wall fracture with free-floating segment, (B) axial section with right displaced inferior orbital rim, (C) coronal section with depressed fracture of the lateral wall of the maxillary sinus, and (D) coronal section showing posterior lateral maxillary sinus fracture, lateral orbital wall fracture, and small orbital floor fracture adjacent to the infraorbital canal. CT indicates computed tomography.
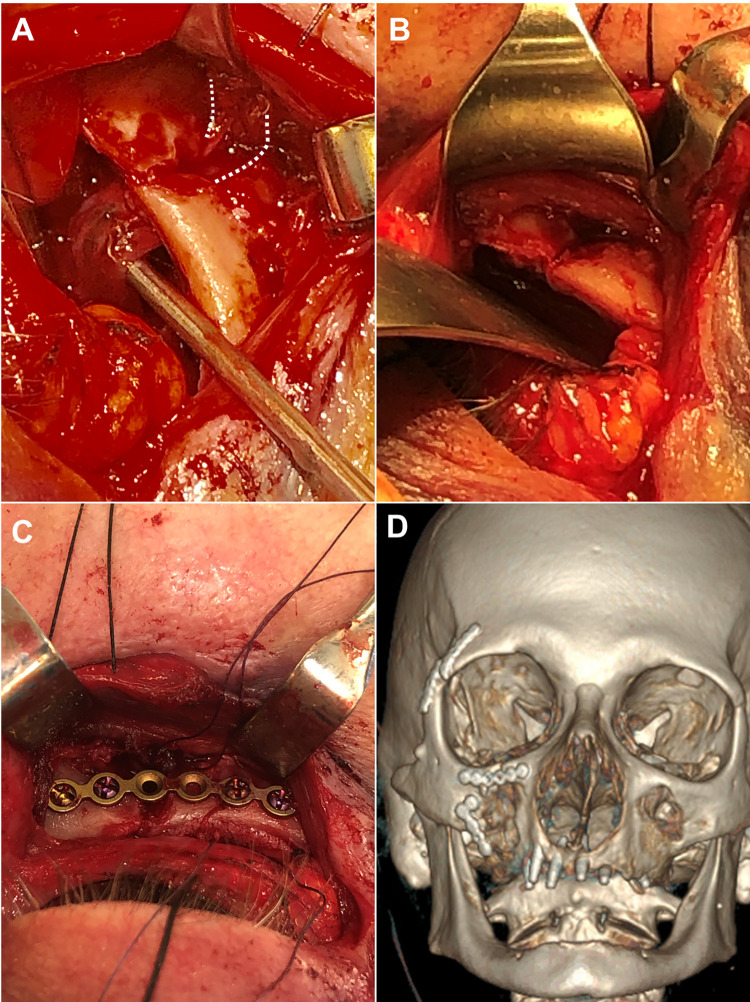
An extended lateral canthotomy transconjunctival incision was made and the rim was exposed. The lateral orbital rim was noted to be fractured in 3 pieces with a middle free-floating segment. Dissection was carried down to the inferior orbital rim and the orbital floor was exposed. There was a large fracture with displacement of the inferior orbital rim (Figure 1B). Finally, a gingivobuccal sulcus incision was made to expose the comminuted fracture of the maxilla. Once all fractures were exposed, a Gillies elevator was used to reduce the lateral orbital rim; this also brought the inferior orbital rim into good position. At this time, it was noted that during the reduction, the IO muscle had herniated through the orbital floor fracture and its origin on the periosteum had been displaced anteriorly through the maxillary face fracture onto the opposite side, causing the muscle to be entrapped side (Figure 2A). In order to reposition the IO, the fracture would have to be opened again. Because of the patient’s age and bone fragility, as well as the comminuted nature of the fracture, further manipulation and reduction of the fracture was undesirable; it was decided to leave the reduced lateral and inferior orbital rim in place, as further manipulation would likely cause additional trauma. The IO was then transected and reposited within the orbit. Two double-armed 5-0 vicryl sutures were used to imbricate the IO in a standard fashion,3 anterior to the maxillary face. The muscle was transected between the two sutures which allowed both ends to be freed from the fracture site and repositioned along the orbital floor. The inferior orbital rim was fixated with a 6-hole 1.2-mm plate (Figure 2B and C). A porous polyethylene and titanium mesh implant was shaped to fit the orbital floor fracture, positioned along the orbital floor, and secured to the plate. Finally, the IO was repaired by tying the ends of the vicryl sutures together. The lateral orbital rim was repaired with 1.2-mm plates, and a 1.7-mm plate was used to secure the maxillary fractures. Forced duction testing was performed and there was no restriction noted. At the conclusion of the procedure, the lateral canthus was reformed and secured, periosteum was closed over the plates, and a frost suture was placed.
Figure 2.
Intraoperative photos demonstrate: (A) reduced inferior orbital rim fracture with inferior oblique elevated along the orbital floor, but tethered through the fracture onto the face of the maxilla. Dotted lines demonstrate outline of the muscle through the anterior face of the fracture. (B) Inferior oblique has been released and repositioned along the orbital floor. The muscle is no longer visible through the fracture. (C) Inferior orbital rim fixated with 1.2-mm plate. (D) Postoperative 3D rendering shows plates along the right lateral orbital rim, inferior rim, and lateral maxillary wall.
One month postoperatively, vision was 20/25 in both eyes. The patient denied any diplopia and demonstrated full extraocular motility in both eyes. Sadly, the patient sustained a second fall 2 months later which necessitated hospitalization, and she passed away.
Discussion
Extraocular muscle entrapment with resulting reduction in motility and diplopia is a known complication of orbital fractures. Less commonly, penetrating trauma or blunt trauma may result in EOM transection.4–6 Multiple reports of traumatic EOM transection, most commonly involving the inferior rectus (IR) muscle, have been documented in the literature.7–12 Carrere and Lewis described a patient with IR transection after orbital blowout fracture. Despite surgical repair of the muscle, the patient had persistent motility deficits and diplopia.6 De Haller et al examined patients with medial wall and orbital floor fractures who underwent transconjunctival–transcaruncular repair. Regarding motility deficits associated with disinsertion or myotomy of the IO during this procedure, they found IO underaction in 50% of patients, although none of the patients were bothered to the point of requiring strabismus surgery.13 Another case of IO disinsertion during transcaruncular approach for orbital fracture repair lead to an IO palsy which required surgical correction of the persistent hypotropia and incyclotropia.14 However, other reports of intentional IO disinsertion followed by muscle reposition within the orbit showed no lasting postoperative motility deficits or diplopia.1,15 The IO is often regarded as a forgiving muscle and may be less likely to elicit diplopia when injured, compared with other EOMs.
Conclusions
The authors present a unique case of IO entrapment secondary to zygomaticomaxillary complex (ZMC) fracture reduction. The oblique was successfully transected and repositioned within the orbit with no resulting damage to extraocular motility or subjective diplopia. Although the patient was unable to be followed greater than 1 month postoperatively, much of her orbital healing was complete and she was unlikely to develop diplopia later on. Division and reattachment of the IO is a safe and effective procedure. The technique presented herein may be a useful addition to the armamentarium of the facial reconstructive surgeon.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Andrea A. Tooley, MD  https://orcid.org/0000-0001-5818-0073
https://orcid.org/0000-0001-5818-0073
References
- 1. Shorr N, Baylis HI, Goldberg RA, Perry JD. Transcaruncular approach to the medial orbit and orbital apex. Ophthalmology. 2000;107(8):1459–1463. [DOI] [PubMed] [Google Scholar]
- 2. Alameddine RM, Tsao JZ, Ko AC, Lee BW, Kikkawa DO, Korn BS. Incidence of diplopia after division and reattachment of the inferior oblique muscle during orbital fracture repair. J Craniomaxillofac Surg. 2018;46(8):1247–1251. doi:10.1016/j.jcms.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 3. Apt L, Gaffney WL, Dora AF. Experimental suture studies in strabismus surgery. I. Reattachment rate of extraocular muscles after recession and resection operations. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1976;201(1):11–17. [DOI] [PubMed] [Google Scholar]
- 4. Helveston EM, Grossman RD. Extraocular muscle lacerations. Am J Ophthalmol. 1976;81(6):754–760. [DOI] [PubMed] [Google Scholar]
- 5. Chen J, Kang Y, Deng D, Shen T, Yan J. Isolated total rupture of extraocular muscles. Medicine. 2015;94(39):e1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jonathan MC, Lewis KT. Complete inferior rectus muscle transection secondary to orbital blowout fracture. Orbit. 2018;37(6):444–446. doi:10.1080/01676830.2017.1423360 [DOI] [PubMed] [Google Scholar]
- 7. Sloan B, McNab AA. Inferior rectus rupture following blowout fracture. Aust N Z J Ophthalmol. 1998;26(2):171–173. doi:10.1111/j.1442-9071.1998.tb01537.x [DOI] [PubMed] [Google Scholar]
- 8. Awadein A. Clinical findings, orbital imaging, and intraoperative findings in patients with isolated inferior rectus muscle paresis or underaction. JAAPOS. 2012;16(4):345–349. [DOI] [PubMed] [Google Scholar]
- 9. Ludwig IH, Brown MS. Flap tear of rectus muscles: an underlying cause of strabismus after orbital trauma. Ophthal Plast Reconstr Surg. 2002;18(6):443–449. doi:10.1097/00002341-200211000-00011 [DOI] [PubMed] [Google Scholar]
- 10. Kashima T, Akiyama H, Kishi S. Longitudinal tear of the inferior rectus muscle in orbital floor fracture. Orbit. 2012;31(3):171–173. doi:10.3109/01676830.2011.648804 [DOI] [PubMed] [Google Scholar]
- 11. Tomasetti P, Metzler P, Jacobsen C. Isolated inferior rectus muscle rupture after blunt orbital trauma. J Surg Case Rep. 2013;2013(9):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yip C-C, Jain A, McCann JD, Demer JL. Inferior rectus muscle transection: a cause of diplopia after non-penetrating orbital trauma. Graefe’s Arch Clin Exp Ophthalmol. 2006;244(12):1698–1700. [DOI] [PubMed] [Google Scholar]
- 13. de Haller R, Imholz B, Scolozzi P. Pseudo-Brown syndrome: a potential ophthalmologic sequel after a transcaruncular-transconjunctival approach for orbital fracture repair. J Oral Maxillofac Surg. 2012;70(8):1909–1913. [DOI] [PubMed] [Google Scholar]
- 14. Tiedemann LM, Lefebvre DR, Wan MJ, Dagi LR. Iatrogenic inferior oblique palsy: intentional disinsertion during transcaruncular approach to orbital fracture repair. JAAPOS. 2014;18(5):511–514. doi:10.1016/j.jaapos.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 15. Alameddine RM, Tsao JZ, Ko AC, Lee BW, Kikkawa DO, Korn BS. Incidence of diplopia after division and reattachment of the inferior oblique muscle during orbital fracture repair. J Craniomaxillofac Surg. 2018;46(8):1247–1251. doi:10.1016/j.jcms.2018.05.026 [DOI] [PubMed] [Google Scholar]