Abstract
Given the need to understand both the negative and positive psychological consequences of the current global COVID-19 pandemic (Brewin et al. in Perspectives in Public Health 10.1177/1757913920957365 2020), the aim of this study was to test a cognitive model of post-traumatic symptoms (PTS) and post-traumatic growth (PTG) during confinement caused by the SARS-COV-2 epidemic. In line with cognitive models of trauma elaboration (Park in Psychological Bulletin 10.1037/a0018301), we included in our model some beliefs associated to the world (e.g., primal beliefs about a good world), to the self (e.g., death anxiety or orientation toward the future) and to others (e.g., suspiciousness or identification with humanity). To evaluate the explanatory model, a national representative sample of adults between the ages of 18 and 75 (N = 1951) was surveyed between 7th and 13th April, 2020, in the middle of a strict 7-week national confinement. Structural equation modelling yielded a very similar model to the one initially specified. The results highlight the role of both negative and positive core beliefs, which are pertinent to the current pandemic threat, in the appearance of PTS and PTG, respectively. In short, primal beliefs about a good world, openness to the future and identification with humanity were associated with PTG; while suspiciousness, intolerance of uncertainty, anxiety about death and also identification with humanity were associated with PTS and consequent impairment. This is an innovative study of different pathways to traumatic responses and growth during a pandemic. Future research is needed to replicate its findings.
Keywords: Post-traumatic growth, Post-traumatic stress symptoms, Trust, Optimism, COVID-19
Introduction
By the time this study was launched, on April 7th 2020, over 1,391,890 people across the world had become infected with SARS-COV-2, resulting in 81,478 deaths (Johns Hopkins Coronavirus Resource Center 2020). At the time of conducting the survey, Spain was one of the countries worst hit by the pandemic with 14,792 dead, a number surpassed only in Italy. To curb the spread of the virus, and following World Health Organization’s recommendations (WHO 2020), on March 14th 2020 the government officially declared a state of emergency and asked its citizens to lock themselves in their homes for a 7-week period with few exemptions (i.e., health professionals attending work, dog walking, and shopping in grocery stores). Analyses of mobility data showed that the population of the country rigidly adhered to these confinement rules (Google’s COVID-19 Community Mobility Reports 2020). Although the COVID-19 pandemic has been preceded by other pandemics (such as SARS in 2002, Ebola in 2013, influenza A/H1N1 in 2015, or Zika in 2015) the virus’ rapid spread and lethality has put global health systems and the global economy under unprecedented strain. Throughout the world, there has been already literally thousands of studies on the effects of the COVID-19 pandemic (Odone et al. 2020), including aspects of mental health and well-being (Nieto et al. 2020). For instance, an initial meta-analysis of 17 studies published until May 2020 (Salari et al. 2020) has shown high levels of prevalence of symptoms of stress (29.6%), anxiety (31.9%), and depression (33.7%) among the general population.
There are compelling reasons to expect significant increases in mental health problems in many sectors of the population during and after the current pandemic crisis (Galea et al. 2020), particularly in countries with higher levels of economic vulnerability (Codagnone et al. 2020). First, a permanent and universal threat of infection can have lasting psychological effects because of the inherently associated uncertainty (Taha et al. 2014). Second, preventive containment measures and social distancing, almost universally used to control the spread of COVID-19 (Brooks et al. 2020), have likely increased loneliness and problems of anxiety and depression (WHO 2020) and reduced life satisfaction (Zhang et al. 2020) in the general population. Third, there is evidence that economic crises, clearly caused by this pandemic, have significant psychological consequences in the population (Chaves et al. 2018). Besides, there are serious additional reasons why the psychological effects might be long lasting. Added to the high figures of human losses, in many cases accompanied by horrifying images of overwhelmed hospitals’ staff and mass graves, COVID-19 poses an existential threat that affects our way of living, our future and that of our children (Shevlin et al. 2020). Also, the lack of vaccines at the time of conducting this study, made the virus a potentially permanent life-threatening menace permeating our existence. Yet, individuals’ responses to the pandemic are far from be uniform and we need models to explain variations in patterns of response. Some studies have shown the moderating role of variables like having children at home, loss of income because of the pandemic, having a pre-existing health condition, exposure to the virus or high estimates of personal risk (Shevlin et al. 2020; Valiente et al. 2020a). Thus, models of response must consider this type of variables to provide robust results.
Given the nature of the pandemic threat, models of post-traumatic stress disorder (PTSD) or post-traumatic symptoms (PTS) seem pertinent in the current pandemic context. The International Classification of Diseases (ICD-11, WHO 2018) describes PTSD as a disorder that can develop “following exposure to an extremely threatening or horrific event or series of events.” As Shevlin et al. (2020) have recently argued, there are solid arguments for considering exposure to the SARS-COVID-19 pandemic, and its associated consequences, a valid potentially traumatic event as described in classification systems like the ICD-11. In fact, epidemiological studies have shown that 17% of adults in the general population have experienced PTSD symptoms during the early stages of the current pandemic (Karatzias et al. 2020).
Studying how the general population responds psychologically to the pandemic is important because the consequences of trauma-related symptoms may extend beyond the psychological distress and the interference with normal life that they produce (Qian 2020). In particular, PTSD is a psychological problem of enormous clinical impact and strongly comorbid with other lifetime disorders (Kessler 1995). Research on PTSD has shown that about a third of people fail to recover after many years (Kessler 1995). Along with generating distress, PTSD is associated with poor physical health and quality of life, suicidal attempts as well as short- and long-term impairment and disabilities such as incapacity for work or hospitalisation (Ferry et al. 2015; Sareen et al. 2007). In the context of other recent epidemics, Betancourt et al. (2016) found, in a relatively large random sample of adults from Sierra Leone (N = 1008), that having significant PTSD symptoms predicted a higher frequency of risk behaviours and fewer Ebola-related healthy behaviours. Thus, despite some inconsistent findings (e.g., Liao et al. 2014), the assessment of stress-related symptoms seems relevant, from a public health perspective, as they may predict compliance with health-related behaviours in pandemics such as the current COVID-19 pandemic (Peterson et al. 2012; Whetten et al. 2013).
Explanatory models of trauma have conceptually evolved in recent years (Vazquez 2013). Whereas, until the 1990s, traumatic responses were seen as an inevitable consequence of traumatic events (Bonanno et al. 2011), epidemiological evidence on PTSD rates in exposed individuals, in both the USA (Kessler et al. 1995) and Europe (Darves-Bornoz et al. 2008), showed that the onset of a full-blown PTSD occurs only in a small fraction of the general population who have been exposed to potentially traumatic events (PTE). An important development of the new ways of conceptualizing trauma is the consideration of positive factors (e.g., positive emotions) in moderating psychopathological responses when dealing with PTE (Tugade and Fredrickson 2004; Vazquez and Hervás 2010). It is even possible, as these new approaches have shown, that individuals feel some sort of posttraumatic growth (PTG) as a consequence of the encounter with traumatic events (Tedeschi and Calhoun 1996, 2004). PTG reflects the perceived benefits or changes in self-perception, in interpersonal relationships and in life philosophy after a traumatic event (Tedeschi et al. 2018) and has been found in individuals facing serious medical conditions like cancer (Casellas-Grau et al. 2017) or HIV (Rzeszutek and Gruszczyńska 2018). In general, as metanalytic evidence has shown, 50%-60% of people exposed to PTE may develop PTG in some domains (Helgeson et al. 2006).
There are different ways to understand what PTG is and how this concept can be pertinent to the analysis of the effects of the COVID-19 pandemic. In their seminal theoretical approach, Tedeschi and Calhoun (1996, 2004) considered PTG as a long-term outcome but also as a process that requires some effortful elaboration of the traumatic event. Yet, other authors have suggested different frameworks to understand PTG. For instance, Nolen-Hoeksema and Davis (2004) defined it as a coping strategy similar to positive reappraisal, whereas Blackie et al. (2017) associated PTG to possible enduring personality-like consequences after experiencing a trauma. Some authors have even considered that, in some cases, PTG could be the manifestation of compensatory illusions (Maercker and Zoellner 2004). We believe that these are not mutually exclusive models as PTG, measured soon after the onset of the crisis might be an initial coping strategy that allows the development of longer-term outcomes such as the enduring positive changes in personality or in philosophical views of the world. This is a perspective that is congruent with the dual process-outcome model delineated by Tedeschi and Calhoun (1996). Interestingly, recent research has identified some predictors of PTG in response to natural disasters. In a study conducted with survivors of the 2010 tsunami that devastated the coast of Chile, García et al. (2015) showed that the presence of cognitive factors like brooding (i.e., the negative component of rumination) or constructive reflection (i.e., thinking of solutions for school children or how to rebuild one’s own home) may lead, respectively, to persistent trauma-related symptoms or to post-traumatic growth.
In contrast to other common PTE associated with PTS (Galea et al. 2020; DePierro et al. 2020), the threat from COVID-19 is continuous, invisible, and universal. Moreover, as in other medical conditions, such as cancer (Cordova et al. 2017) or chronic pain (Rzeszutek et al. 2015), the reactions associated with the current virus are probably not limited to the diagnosis of a serious disease, but are also a by-product of the constant awareness of our susceptibility to be infected and the multiple medical, psychological and social consequences of the condition (Edmondson 2014). In the case of the SARS-CoV-2, the life-threat is aggravated because, beyond confinement and/or social distancing, there are no known ways to prevent the spread of the virus and there is a high degree of uncertainty about its impact. Thus, based on previous research showing the predictive role of perceived uncertainty on PTS (Oglesby et al. 2017), we explored in the present study the role of intolerance to uncertainty (i.e., negative unpredictable events that may occur) (Carleton et al. 2007). Furthermore, given the relatively high rates of lethality and contagiousness of the COVID-19, it was thought that death anxiety might also be relevant to the development of PTS. Death anxiety is a concept reflecting the apprehension generated by death awareness (Abdel-Khalek 2005), a fear associated with the development and maintenance of different psychological disorders (Iverach et al. 2014). In fact, previous research has shown that traumatic events may make existential concerns and death anxiety more salient (Edmondson et al. 2011) which, in turn, may predict the onset of PTSD (Pyszczynski et al. 2015).
Periods of uncertainty and threat can lead to increases in conspiracy theories and suspiciousness (van Prooijen and Dougla 2017), and this has been the case in the current pandemic (Depoux et al. 2020) and also in previous epidemic crises (e.g., Sharma et al. 2017). While there is extensive evidence about the protective role of social support in the development of PTSD (Brewin et al. 2000; Ozer et al. 2003), it is likely that its buffering effect may be hampered by distrust in others. Therefore, we included a measure of suspiciousness in this study. Suspiciousness can be considered as a part of the paranoia continuum, from interpersonal ordinary everyday beliefs of harm to strange and impossible beliefs such as persecutory delusions (Bebbington et al. 2013). It has been associated with a general mistrust about others, with poor social cohesion and worse physical and mental health (Westermann et al. 2012).
The role of positive beliefs is also relevant in the current crisis. Janoff-Bulman (1989) reported that traumatic events can have a profound negative impact on the protective positive beliefs about the world (e.g., that it is a benevolent place), the self (e.g., self-worth), and others (e.g., trust) and this observation has recently been supported by both theoretical models on the role global beliefs have on meaning-making after trauma (Park 2010) and prospective research in the general population (Poulin and Silver 2019). These positive beliefs can be encompassed in what Clifton et al. (2019) calls primal or primal world beliefs, which can be defined as the individual’s most basic beliefs about the general character of the world as a whole. In relation to positive beliefs about others, identification with all humanity is relevant construct that is more than an absence of ethnocentrism and more than the presence of dispositional empathy, moral reasoning or universalism. It encompasses concerns of a global nature, priority given to human rights over national self-interest, greater knowledge regarding global humanitarian concerns, among other things (McFarland et al. 2012). A recent national representative study, aimed at exploring psychological patterns of response in the current COVID-19 pandemic, has shown that having higher levels of psychological well-being and high identification with all humanity predicts resilience (Valiente et al. 2020c). Therefore, we expected that having a strong identification with all humans and a sense that, despite suffering a worldwide epidemic, one lives in a good world (Clifton et al. 2019) might also be related to PTG.
Positive beliefs about the future seems also highly relevant in the current pandemic. Thus, based on meta-analytic evidence on the role of optimism in PTG (Helgeson et al. 2006; Prati and Pietrantoni 2009), the role of being open to the future was also analysed in the present study. Openness to the future is a construct developed by Botella et al. (2018) and characterized by a positive affectivity towards the future, which could be a key ingredient of resilience, wellbeing, and readiness for behavioural planning aimed at solving or facing difficulties, under circumstances of uncertainty.
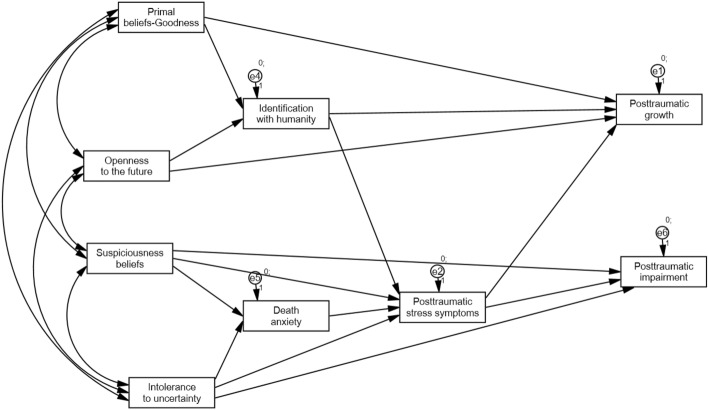
In sum, the current pandemic scenario seems adequate to test models of both trauma-related symptoms (PTS) and trauma-related growth (PTG) in response to the COVID-19 pandemic. Our study included variables specifically selected to be particularly relevant to the pandemic, which have not been systematically explored in previous studies. Based on the above review of the literature, we propose a model (Fig. 1) in which positive cognitions (i.e., beliefs about living in a good world, openness to the future and identification with humanity) are positively associated with PTG whereas more negative cognitions (i.e., suspiciousness, intolerance to uncertainty and death anxiety) are positively related to PTS and subsequent impairment. For the PTG path, it was hypothesised that there would be both direct effects as well as indirect effects mediated by identification with humanity. For the PTS path, death anxiety was hypothesised to be a potential mediator of the effects.
Fig. 1.
Hypothesised model
Materials and Methods
A cross-sectional design was used to assess the psychological impact of the COVID-19 virus in the adult general population in Spain as part of an international consortium’s protocol (McBride et al. 2020). The study involved an online-based panel and was launched 26 days after the state of emergency was declared by the government. All responses were completed between 7 and 13 April 2020. The study was approved by the University Ethics Committee, being conducted in compliance with the Declaration of Helsinki.
Participants
Individuals between 18 and 75 years old from a large online research panel were invited to participate (selected by sex, age and political region stratified quotas, according to National Institute of Statistics census of 1 January 2019, to assure representativeness of the national population). The sample consisted of 2122 individuals, representative of the entire national population, with a maximum sampling error of ± 2.2% at 95% confidence. Participants had to live in the country and be older than 18 at the time of the survey.
Procedure
The recruitment of the sample was carried out by Sondea, a company that provides online samples for research, based on a large national panel of participants. The methodology used in our study was a quota stratified sampling. Once each quota was completed, new participants were not admitted in the study to ensure that the prefixed quotas were met and not exceeded. After giving their written consent, participants completed the survey online (https://www.qualtrics.com). Completers received a small financial reward for their time (1 euro). In order to ensure the validity of the responses, we followed a time-limit method (Edwards 2019) and calculated the minimum time needed to complete the entire questionnaire. We concluded, through several pilot tests conducted by volunteers and members of the team, that it would take a minimum of 20 min. Therefore, we discarded those participants (N = 145) who took less than that time to complete the survey. Also, subjects who completed the survey several times (N = 26) were discarded. Thus, the final sample used in the analyses was N = 1951. The average time for the survey completion was 42.5 min, (SD = 15.2 min). Participants’ socio-demographic characteristics are shown in Table 1.
Table 1.
Socio-demographic characteristics of the sample
| Participants (N = 1951) | |
|---|---|
|
Gender [n (%)] Male Female Other |
1028 (52.7) 918 (47.1) 5 (0.2) |
| Age [Mean (SD, range)] | 45.16 (12.78, 18–75) |
|
Civil Status [n (%)] Single Married/Unmarried partner Separated/Divorced/Widower |
779 (40) 1003 (51.4) 169 (8.6) |
| Immigrant status [Yes; n (%)] | 137 (7) |
|
Educational level [n (%)] No formal education Primary High school University graduate University postgraduate Vocational training |
6 (0.3) 55 (2.8) 622 (31.9) 704 (37.2) 252 (12.9) 292 (15) |
|
Religion [n, (%)] Catholic Agnostic or Atheist Other |
1036 (53.1) 778 (40.9) 117(6.0) |
|
Urbanicity of residential location [n (%)] Urban Rural |
1,644 (84.3) 307 (15.7) |
|
Household composition [n (%)] Alone Accompanied by one or more adults With children at home |
257 (13.2) 1694 (86.8) 1131 (58) |
|
Current economic activity [n (%)] Full time job Part time job Unemployed Pensioner Student |
1126 (57.7) 195 (10) 333 (17.0) 187 (9.6) 110 (5.6) |
|
Gross annual household income in euros, 2019 [n (%)] 12,450–20,200 20,200–35,200 35,200–60,000 Over 60,000 |
694 (35.6) 673 (34.5) 456 (23.4) 128 (6.6) |
Measures
Socio-demographic characteristics and health status. In addition to data relating to gender, age and civil status, respondents provided information about their civil status, immigration status, highest level of educational attainment, religious affiliation, urbanicity of residential location, household composition, current economic activity and gross annual household income. All respondents were also asked about their history of mental health difficulties and had to indicate whether they had received treatment for mental health problems.
The International Trauma Questionnaire (ITQ; Cloitre et al. 2018), was used to assess stress-related reactions associated with the COVID-19 pandemic (McBride et al. 2020). The scale includes six symptom indicators of possible PTSD (two measuring Re-experiencing, two measuring Avoidance, two measuring Sense of threat). Also, we included the three ITQ items measuring impairment (e.g., “since the beginning of lockdown, have the above symptoms affected your work or ability to work?”). All items are measured on a 5-point, Likert-type scale (0 = Not at all; 4 = Extreme) and were worded in relation to the COVID-19 with statements like “Having upsetting dreams that replay part of the COVID-19 experience or are clearly related to the COVID-19 experience. A total post-traumatic stress severity score was generated by adding the six PTSD symptoms items (range from 0 to 24) and used as a continuous measure of PTSD severity. A total disturbance/impairment PTSD score was obtained by adding the three PTSD impairment items (range from 0 to 12) and used as a continuous measure of PTSD disturbance. Following standard practice in trauma research (Karatzias et al. 2017), item scores ≥ 2 (Moderately) on any of the PTSD items was used to indicate the presence of a symptom. In this study, the Cronbach´s alpha for PTSD symptoms or severity and impairment were good (α = 0.89; α = 0.86), respectively.
The Short-form Persecution and Deservedness Scale (SF-PaDS; McIntyre et al. 2018) is a 5-item instrument to assess suspiciousness in clinical and general population samples, based on a previous longer version of the scale validated in clinical and nonclinical samples (Melo et al. 2009). Both the original scale reliability (α = 0.84) and its adaptation (α = 0.85) (Valiente et al. 2020b) were good. Participants rate their agreement on a 5-point scale (1 = strongly disagree; 5 = strongly agree) with statements such as “I’m often suspicious of other people’s intentions towards me.” By adding up the scores, an overall SF-PaDS (range from 5 to 20) provides a measure of suspiciousness severity. In this study, the Cronbach´s alpha was good (α = 0.85).
Intolerance of uncertainty scale (IUS-short version; Carleton et al. 2007) is a 12-item instrument for assessing intolerance of uncertainty on a 5-point Likert scale (1 = not at all characteristic of me; 5 = entirely characteristic of me) with excellent psychometric properties (α = 0.91). It has items such as “I always want to know what the future has in store for me.” A total score is calculated by summing up the 12 items score (range from 12 to 60). In this study, the Cronbach´s alpha was excellent (α = 0.91).
The Death Anxiety Inventory (DAI; Tomás-Sábado and Gómez-Benito 2005) assessed attitudes towards death using 17-items, which form five factors (externally generated death anxiety, meaning and acceptance of death, thoughts about death, life after death, and brevity of life) with excellent internal consistency (α = 0.90). Responses are scored on a 5-point Likert scale (1 = totally disagree to 5 = totally agree). In the current study, only five items like “I think I am more afraid of death than most people” were selected (one from each of the five factors is identified in the original validation study). A total DAI score is calculated by adding the score of each item (range from 5 to 25). In this study, the Cronbach´s alpha was good (α = 0.81).
The Primal World Beliefs Inventory (PI; Clifton et al. 2019) is a 99-item instrument that measures major primal world beliefs with excellent psychometric properties (α = 0.90) and test–retest stability. For the present study, we used the six items corresponding to the perception of goodness of the world with statements such as “The good things in the world outweigh the bad.” Participants were asked to respond on a 6-point Likert scale (0 = strongly disagree; 5 = strongly agree). A total score of perception of goodness of the world is obtained with the average of the items scores (range from 0 to 5). In this study, the Cronbach´s alpha was good (α = 0.85).
The Identification with all humanity scale (IWAH; McFarland et al. 2012) is a 3-item questionnaire exploring respondents’ identification with three different groups (people in my community; people from my country; and all humans everywhere) with good psychometric properties for the three groups (α = 0.89; α = 0.83; α = 0.81), respectively. For each group, three different subscales are presented to respondents (“How much do you identify with (feel a part of, feel love toward, have concern for …?”; “How much would you say you care (feel upset, want to help) when bad things happen to …?”; and “When they are in need, how much do you want to help…?).” Response scale uses a 5-point Likert (1 = not at all; 5 = very much). Averaged scores were calculated for the three subscales (range from 1 to 5). In this study, the Cronbach´s alpha was good (α = 0.86).
The Openness to the Future Scale (OF; Botella et al. 2018) is a 10-item instrument with good psychometric properties in general population (α = 0.87) and clinical population (α = 0.82). The OF assesses positive views of the future with statements like “I'm usually confident that things will work out.” Response options ranged on a 5-point Likert scale (1 = strongly disagree; 5 = strongly agree). An OF total score is calculated by adding all the item scores (range from 10 to 50). In this study, the Cronbach´s alpha was good (α = 0.87).
The Post-traumatic Growth Inventory- Short Form (PTGI-SF; García and Wlodarczyk 2016; Cann et al. 2010) is a 10-item instrument with excellent psychometric properties (α = 0.94), on which respondents are asked to rate their beliefs about positive self-related changes (e.g., “I appreciate the value of my life more”). The construction of the scale helped capture information relevant to each of the five factors usually found in factor analyses of the original 21-item scale (Tedeschi and Calhoun 1996): relating to others, new possibilities, personal strength, spiritual change, appreciation of life. Each factor is represented with two items in the PTGI-SF. As the original PTGI does not cover the possibility that individuals may have worsened in the domains assessed (Baker et al. 2008), we replaced the response format with a bipolar rating scale, as used by Boals and Schuler (2018) in their Stress-Related Growth Scale–Revised (SRGS-R), which allows for the possibility to measure both positive and negative changes thereby reducing the probability of an illusory growth due to a format of response bias. A 7-point rating scale was used (0 = A very important negative change; 3 = No change; 6 = A very important positive change). Following Cann et al.’s (2010) criteria, the total score of the scale (range from 0 to 60), rather than subscores, was used for the analyses. In this study, the Cronbach´s alpha was good (α = 0.87).
Data analyses
A series of descriptive analyses were first conducted. Then, path models were tested to assess their fit using path analysis through Structural Equation Modelling (SEM). The Mardia coefficient (Mardia 1970) was used for assessing multivariate normality, using the suggested score of less than 70 to assume normality (Ayán and Díaz 2008).
In order to assess the fit of the hypothesised model, the Maximum Likelihood Estimation Method was used using the following fit indices and criteria (Hu and Bentler 1999; Yu 2002): (a) χ2/df: an acceptable fit is indicated by values ≥ 5, and a good fit is indicated by values ≥ 2; (b) Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI): an acceptable fit is indicated by values ≥ 0.90, and a good fit is indicated by values ≥ 0.95; (c) Root Mean Square Error of Approximation (RMSEA): an acceptable fit is indicated by values ≤ 0.08 (90% CI ≤ 0.10), and a good fit is indicated by values ≤ 0.05 (90% CI ≤ 0.08); (d) Standardized Root Mean Square Residual (SRMR): an acceptable fit is indicated by values ≤ 0.08 and a good fit is indicated by values ≤ 0.05. The model was then re-specified considering the values in the path coefficients and the values of the modification indexes.
To analyse indirect effects, a bias-corrected bootstrap estimation (2,000 bootstrap samples with 95% confidence interval) was performed. When zero is not included in the confidence interval, mediation is supported (MacKinnon et al. 2004). All analyses were carried out using SPSS v.21 (IBM Corp 2011) and AMOS SPSS v. 23 (Arbuckle 2014).
Results
Characteristics of the sample
Socio-demographic characteristics of the study sample are reported in Table 1. From the total sample, the mean age was 45 years and 1028 (52.7%) were male. Regarding civil status and educational level, 51.4% had a partner and 37.2% had a university degree. In addition, 57.7% had a full-time job and 35.6% reported having low socioeconomic income. 55 participants (2.8%) had been infected by the virus, and 586 (30.1%) knew someone close who had been infected.
Description of variables included in the model
A descriptive analysis of the variables selected in the model is shown in Table 2. Based on published scoring methods for the ITQ symptoms subscale (Cloitre et al. 2018) (score of ≥ 2) in the six stress-related symptoms of the scale, 19.7% of the total sample had significant stress-related symptoms. which is slightly higher than the score obtained by Cloitre et al. (2018) in their nationally representative trauma-exposed community sample (18.3%).
Table 2.
Ranges, means and standard deviations (N = 1951)
| Variable | Min | Max | M | SD |
|---|---|---|---|---|
| Post-traumatic symptoms (ITQ) | 0 | 24 | 4.79 | 5.00 |
| Post-traumatic impairment (ITQ) | 0 | 12 | 2.22 | 2.78 |
| Suspicious beliefs (SF-PaDS) | 0 | 20 | 5.97 | 4.43 |
| Intolerance to uncertainty (IUS) | 12 | 60 | 33.01 | 9.36 |
| Death anxiety (DAI) | 5 | 25 | 11.76 | 4.49 |
| World beliefs–Goodness (PI) | 0 | 5 | 3.38 | 0.86 |
| Identification with humanity (IWAH) | 1 | 5 | 3.78 | 0.64 |
| Openness to the future (OF) | 10 | 50 | 38.18 | 6.07 |
| Post-traumatic growth (PTGI-SF) | 0 | 60 | 36.51 | 7.60 |
ITQ International Trauma Questionnaire; SF-PADS short-form persecution and deservedness scale; IUS intolerance of uncertainty scale; DAI death anxiety inventory; PI primals inventory; IWAH identification with all humanity scale; OF openness to the future scale; PTGI-SF post-traumatic growth inventory- short form
Measurement model
Mardia’s coefficient obtained a value of 18.35, well under the critical value of 70 recommended to use the Maximum Likelihood Estimation Method. The predictive model of PTG and Post-traumatic impairment was tested. The following goodness-of-fit indices were obtained: (1) χ2/df = 7.90; (2) CFI = 0.98; (3) TLI = 0.95; (4) RMSEA = 0.06 (IC = 0.05 to 0.07), (5) SRMR = 0.04.
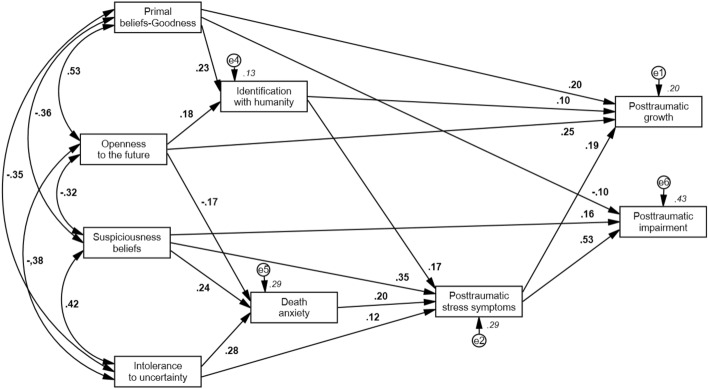
The model was then re-specified by eliminating a path with non-significant p values: Intolerance to uncertainty → Post-traumatic impairment (β = 0.03) and, following the recommendations of the modification indices, two new significant paths were added: Openness to the future → Death anxiety (β = -0.17), and Primal beliefs-Goodness → Post-traumatic impairment (β = -0.10). The re-specified model (see Fig. 2) obtained the following goodness-of-fit indices: (1) χ2/df = 3.20; (2) CFI = 0.99; (3) TLI = 0.98; (4) RMSEA = 0.03 (IC = 0.02 to 0.05), (5) SRMR = 0.02.
Fig. 2.
Final model. Shown above are the standardised regression coefficients for each path of the model
To analyse whether the indirect effects were significant, a bias-corrected bootstrap estimation was performed. Results showed that most of the indirect effects were significant, except for the indirect effect of the openness to the future on post-traumatic stress symptoms and post-traumatic impairment, so that in the latter two cases, if there is a direct effect on the mediator(s), there is no mediation with the dependent variable (Table 3).
Table 3.
Standardised indirect effects, 95% confidence interval for the estimates (lower and upper limit), their standard errors and the p value
| Variables | Indirect effect | CI (95%) | Standard error | p value |
|---|---|---|---|---|
| Primal beliefs-Goodness → PTG | .03 | .020–.043 | .006 | < .001 |
| Primal beliefs-Goodness → PTS | .04 | .029–.052 | .008 | < .001 |
| Primal beliefs-Goodness → PTI | .02 | .015–.028 | .004 | < .001 |
| Openness to the future → PTG | .02 | .008–.027 | .006 | < .001 |
| Openness to the future → PTS | − .004 | − .017 to .009 | .008 | .62 |
| Openness to the future → PI | − .002 | − .009 to .005 | .004 | .63 |
| Suspicious beliefs → PTG | .08 | .060–.093 | .010 | < .001 |
| Suspicious beliefs → PTS | .05 | .038–.062 | .007 | < .001 |
| Suspicious beliefs → PTI | .21 | .190–.236 | .014 | < .001 |
| Intolerance to uncertainty → PTG | .03 | .024–.045 | .006 | < .001 |
| Intolerance to uncertainty → PTS | .06 | .045–.072 | .008 | < .001 |
| Intolerance to uncertainty → PI | .09 | .072–.116 | .014 | < .001 |
| Identification with humanity → PTG | .03 | .025–.043 | .006 | < .001 |
| Identification with humanity → PTI | .09 | .074–.111 | .011 | < .001 |
| Death anxiety → PTG | .04 | .028–.050 | .006 | < .001 |
| Death anxiety → PI | .11 | .086–.129 | .013 | < .001 |
PTG Post-traumatic growth; PTS post-traumatic stress symptoms; PTI post-traumatic impairment; PI primals inventory
Discussion
The aim of this study was to test an explanatory model for PTS and PTG reactions related to the SARS-CoV-2 epidemic crisis in the general population. The study was designed to include variables that might be specifically pertinent to the current life-threatening pandemic. Thus, a model was created in which, on the one hand, it was hypothesised that variables related to positive fundamental beliefs (i.e., about the positive nature of the world, identification with humanity, and openness to the future) would be associated with a sense that the current crisis was promoting personal growth. On the other hand, the model also hypothesised that negative core beliefs (i.e., about the intrinsic uncertainty of the world, suspicions about others, and death anxiety) would be associated with post-traumatic stress.
Regarding PTS, the resulting model highlighted the importance of negative beliefs about others in explaining these responses. Suspiciousness was directly related to both PTS and the associated post-traumatic impairment. This finding is congruent with previous evidence showing that lack of social support is one of the best predictors of PTSD (Brewin et al. 2000; Ozer et al. 2003). Our results suggest that a related variable that is opposite in nature to empathy and connectedness (i.e., suspiciousness), which is typically associated not only to a lack of interpersonal trust but also to low levels of perceived social support (Lamster et al. 2017), may also be predictive of PTS. It is likely that suspiciousness, partially fed by paranoid rumours in social media about the origins of the epidemic (Sharma et al. 2017), may contribute to seeing others as a threat for contagion. In this way, suspiciousness may discourage individuals from seeking help from others and reduce the beneficial effects of social support. Thus, our model suggests that suspiciousness may be a specific factor directly related to trauma-related symptoms and might be an obstacle to follow efficacious quarantine recommendations from authorities (Webster et al. 2020).
Our results also confirm the important role of intolerance of uncertainty in relation to PTS (Taha 2014) and, more specifically, to anxiety in the current pandemic (Valle et al. 2020). Yet, both suspiciousness and difficulties in coping with uncertainty also have an effect that is mediated by death anxiety. The lethality and contagiousness of the COVID-19 is relatively high, which may easily activate salience of mortality (Pyszczynski et al. 2015). In fact, it could be argued that death anxiety is in some sense an extreme form of intolerance to the most uncertain condition that happens to us in our existence. This finding also highlights the potentially traumatic nature of being exposed to the SARS-CoV-2 (Shevlin et al. 2020). Interestingly, the reformulated model (Fig. 2) revealed that being optimistic about the future was negatively associated with death anxiety which seems to confirm the salutogenic role of optimism (Carver and Scheier, 2014). In this line, a recent study has found that intolerance to uncertainty, death anxiety, loneliness, suspiciousness and identification with all humanity as well as presence of well-being are all significant predictors of a resilient response to COVID-19 (Valiente et al. 2020b).
Regarding psychological growth, previous studies on trauma-related events have shown that most individuals exposed develop positive changes in their attitudes, behaviours, and values (Helgeson et al. 2006). Previous research has also shown that positive appraisals, social support and optimism (Prati and Pietrantoni 2009) as well as reflective modes of thinking (García et al. 2015), among other factors, may predict these positive changes. The reformulated model found in our study (Fig. 2), revealed that beliefs about living in a good world, which is a ‘primal’ belief (Clifton et al. 2019), is directly related to PTG. Thus, it seems that unshattered beliefs about the world not only protect against trauma-related symptoms (Janoff-Bulman 1989; Poulin and Silver 2019) but can also promote growth. Also, interestingly, and not initially predicted in our model, this positive primal belief is negatively associated with functional impairment (PTI) associated with the symptoms. Our model also confirmed that identification with humanity was positively associated with PTG. Yet, an interesting and unexpected finding emerged in the reformulated model. These beliefs of identification with humanity were also positively associated with PTS. Thus, it seems that beliefs of being well connected with humanity may have double-edge consequences by facilitating feelings of growth (Páez et al. 2015) but also, given the contagiousness of a virus, increasing the feelings of vulnerability of oneself and others. The dual role of a “positive” variable as beliefs of identification with humanity seems to support the idea that the results found in our study are not trivial or tautological. On the one hand, positive thoughts of being connected to others are not univocally or simplistically associated with positive outcomes. On the other hand, the study included a rather large set of variables related to psychological symptoms and difficulties, as well as variables related to positive functioning that were empirically discarded in building up the models. Therefore, the study reveals that some of the selected positive and negative cognitions are uniquely associated to psychological growth and symptoms and impairment related to COVID-19.
It is possible that, in our study, feelings of growth, framed in the questions specifically related to the confinement, might be related not only to the processing of threat-related information about COVID-19 and its consequences, but also to the positive emotions and positive experiences that individuals had during the confinement. As a recent meta-analysis has shown, psychological growth does not require suffering as some positive experiences (e.g., marriage or childbirth) are also identifiable sources of growth (Mangelsdorf et al. 2019). It is possible that some of the daily positive experiences that citizens have been experiencing during confinement (e.g., giving and taking social support, daily applause to health workers, feelings of contribution to contain the epidemic, etc.) may also feed positive ideas about human nature which, in turn, may reinforce ideas of identification with humanity.
Finally, both the initial and the resulting model revealed a positive association between PTS and PTG which is consistent with the extant literature (Shakespeare-Finch and Lurie-Beck 2014; Wu et al. 2019). In fact, in relation to negative events, perceiving an event as traumatic seems to be a prerequisite for growth (Zoellner and Maercker 2006; Helgeson et al. 2006). Shakespeare-Finch and Lurie-Beck's (2014) meta-analysis showed that the association between PTS and PTG appears to be curvilinear in nature, being stronger when the traumatic event is of a mass nature, such as natural disasters. Perceiving that the event was severe appears to influence both the development of PTS and PTG (García et al. 2015), which might reflect that both symptoms and growth appear to occur precisely because of the suffering produced by a highly stressful event. In some cases, perhaps mediated by specific cognitive processes that are ignited after the event (Park 2010; García et al. 2015), the perceived severity of the event itself leads to the questioning and changing of certain beliefs about oneself, others and spirituality (Helgeson et al. 2006), with positive and negative changes co-existing.
The study has some strengths and some limitations which, in part, are due to the difficulties of launching a large-scale study during the initial stages of the pandemic, in the midst of difficult circumstances. Regarding the strengths, it includes some variables related to general beliefs about the world that have not usually been considered in trauma-related studies and which were thought to be relevant in a pandemic characterised by the universality of the threat and the lack of effective preventive therapeutics at the time (i.e., vaccines). Also, the study is a national representative sample in terms of sex, age, income, and region of the country, which is important given the uneven distribution of the pandemic in almost any country (https://coronavirus.jhu.edu/map.html). The representativeness of the sample is an asset of the study given that, as the systematic review by Nieto et al. (2020) has revealed, most of the studies that have been published so far on mental health problems associated to the COVID-19 have small or unrepresentative samples which limits their generalizability. Furthermore, the instruments selected have shown in previous studies to provide robust estimations of the variables under study.
Regarding the limitations of the study, it was cross-sectional (which limits our ability to infer causality) and exclusively based on self-reported information (which may lead to common method biases) Podsakoff et al. (2003). Furthermore, information was gathered in a retrospective manner which, as it has been found in the case of PTG, may not be congruent with other sources of information (Frazier et al. 2009). Given the rather immediate assessment conducted in the present study (i.e., one month after the onset of the pandemic in the country), it is unlikely that participants, even those who felt more threatened or exposed to the virus, have had enough time for further cognitive elaboration of the effects of the pandemic in their lives (Park 2010). Thus, our data are not adequate to test concepts of PTG that are associated to long-term outcomes or even personality changes (Jayawickreme and Blackie 2014; Jayawickreme et al. 2020). In this study we have evaluated perceived growth when the stressful situation (i.e., the Covid-19 pandemic) is still present, so we must necessarily consider that, at this point, we are basically measuring a coping strategy that might facilitate, in the future, the development of more adaptive responses to adversity, as proposed by longitudinal studies (Bussell and Naus 2010; Stephenson et al. 2017).
The specific circumstances of the confinement (e.g., home comfort, living with children, alone, or with abusive partners, etc.) may influence almost any psychological outcome (Galea et al. 2020) beyond the impact of the variables included in this study. Also, all measures included in the study were self-reported ones. Although we acknowledge the limitations of estimating depression or traumatic responses exclusively through self-reports, we are simply focusing on symptoms of clinical significance without any inference about clinical diagnosis. Similarly, although there is an already long debate on the real or illusory nature of post-traumatic growth (Sumalla et al. 2009), our results are congruent, as we have shown, with previous literature on the configurations of psychological variables associated with this concept. Also, the mere existence of the belief that the current epidemic may have brought some benefits could be important in facilitating the ability to overcome this challenging situation. Future studies complementing these self-reported assessments (Frazier et al. 2009) may shed light on the psychological and behavioural consequences of those initial beliefs of positive changes associated to the COVID-19. Lastly, while one of the strengths of this study is the large size of the sample, the fact that it is an online study may reduce its representativeness, particularly among older respondents.
In sum, the current study has aimed to shed light on both the negative and positive psychological consequences of the current COVID-19 worldwide crisis, which must be understood for the purposes of pandemic planning (Brewin et al. 2020). To our knowledge, this is the first study that has attempted to identify how core beliefs about the world may lead to either traumatic responses or traumatic growth during a pandemic. While we are still far from fully understanding how individuals' belief systems may affect their psychological adjustment during times of crisis, there is little doubt about the relevance of both positive and negative beliefs about the world and others. For instance, there is already evidence showing that suspiciousness and conspiracy beliefs have a negative effect on preventive measures such as social distancing (Bierwiaczonek et al. 2020). Based on our results, we can hypothesise that interventions aimed at promoting primal ideas about the goodness of the world and human nature might facilitate PTG. Further research is required to establish whether these beliefs are influenced by childhood experiences, whether they can be affected by education, or whether specific messaging by governments and public health agencies can promote these beliefs. It can also be hypothesised that reducing ambiguity in official messages might mitigate the potentially traumatic impact of the pandemic, by decreasing uncertainty, which in turn might mitigate anxiety about death. Finally, as misinformation has exacerbated the spread of the virus and slowed responses to the pandemic (Motta et al. 2020), it seems plausible that messages providing reliable and non-accusatory information on the origins of the infection could reduce the intensity of PTS in the general population by deactivating suspiciousness in vulnerable individuals. Future correlational or experimental studies to test these hypotheses might contribute to an effective psychologically-informed approach to promoting population coping during pandemics and other public health emergencies.
Given the diversity of pre-existing social, economic and health conditions in different countries (Brewin et al. 2020), we cannot guarantee the generalisability of the current study results to other societies or to other moments in a dynamic threat that will endure for some time with long-lasting social and economic consequences for the world as we know it. It will be useful to replicate these findings in different countries and during different stages of the current crisis.
Acknowledgements
This research was supported by grants from the Ministry of Science and Innovation (PSI2016-74987-P) and Instituto de Salud Carlos III (COV20/00737) to Carmen Valiente and funds from the UCM for consolidated research groups (GR29/20) to Carmelo Vazquez. Richard Bentall received grant funding from the Economic and Social Research Council (grant number ES/V004379/1). Almudena Trucharte had an Universidad Complutense doctoral fellowship (CT42/18) and Vanesa Peinado had a Ministry of Economy and Competitiveness doctoral Fellowship (BES-2017082015). We also thank Jamie O’Grady for his help in editing the paper and to the COVID-19 Psychological Research International Consortium (C19PRC) Study for allowing us to use key parts of their study protocol (https://doi.org/10.31234/osf.io/z3q5p).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the University Ethics Committee, being conducted in compliance with the Declaration of Helsinki.
Informed Consent
All participants gave their informed consent to participate in the survey.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abdel-Khalek AM. Death anxiety in clinical and non-clinical groups. Death Studies. 2005;29(3):251–259. doi: 10.1080/07481180590916371. [DOI] [PubMed] [Google Scholar]
- Arbuckle, J. L. (2014). IBM SPSS AMOS 23.0 [Computer Program]. Chicago, IL: IBM Corps.
- Ayán MNR, Díaz MAR. The reduction of skewness and kurtosis of observed variables by data transformation: Effect on factor structure. Psicológica. 2008;29(2):205–227. [Google Scholar]
- Baker JM, Kelly C, Calhoun LG, Cann A, Tedeschi RG. An examination of posttraumatic growth and posttraumatic depreciation: Two exploratory studies. Journal of Loss and Trauma. 2008;13:450–465. doi: 10.1080/15325020802171367. [DOI] [Google Scholar]
- Bebbington PE, McBride O, Steel C, Kuipers E, Radovanovič M, Brugha T, Jenkins R, Meltzer HI, Freeman D. The structure of paranoia in the general population. British Journal of Psychiatry. 2013;202(6):419–427. doi: 10.1192/bjp.bp.112.119032. [DOI] [PubMed] [Google Scholar]
- Betancourt TS, Brennan RT, Vinck P, VanderWeele TJ, Spencer-Walters D, Jeong J, Akinsulure-Smith AM, Pham P. Associations between mental health and Ebola-related health behaviors: A regionally representative cross-sectional survey in post-conflict Sierra Leone. PLoS Medicine. 2016;13(8):e1002073. doi: 10.1371/journal.pmed.1002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierwiaczonek K, Kunst JR, Pich O. Belief in COVID-19 conspiracy theories reduces social distancing over time. Applied Psychology: Health and Well-Being. 2020 doi: 10.1111/aphw.12223. [DOI] [PubMed] [Google Scholar]
- Blackie LER, Jayawickreme E, Tsukayama E, Forgeard MJC, Roepke AM, Fleeson W. Post-traumatic growth as positive personality change: Developing a measure to assess within-person variability. Journal of Research in Personality. 2017;69:22–32. doi: 10.1016/j.jrp.2016.04.001. [DOI] [Google Scholar]
- Boals A, Schuler KL. Reducing reports of illusory posttraumatic growth: A revised version of the stress-related growth scale (SRGS-R) Psychological Trauma: Theory, Research, Practice, and Policy. 2018;10(2):190–198. doi: 10.1037/tra0000267.supp. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual Review of Clinical Psychology. 2011;7(1):511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Botella C, Molinari G, Fernández-Álvarez J, Guillén V, García-Palacios A, Baños RM, Tomás JM. Development and validation of the openness to the future scale: A prospective protective factor. Health and Quality of Life Outcomes. 2018;16(1):72. doi: 10.1186/s12955-018-0889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–766. doi: 10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Brewin CR, DePierro J, Pirard P, Vazquez C, Williams R. Why we need to integrate mental health into pandemic planning. Perspectives in Public Health. 2020 doi: 10.1177/1757913920957365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussell VA, Naus MJ. A longitudinal investigation of coping and posttraumatic growth in breast cancer survivors. Journal of Psychosocial Oncology. 2010;28(1):61–78. doi: 10.1080/07347330903438958. [DOI] [PubMed] [Google Scholar]
- Cann A, Calhoun LG, Tedeschi RG, Taku K, Vishnevsky T, Triplett KN, Danhauer SC. A short form of the posttraumatic growth inventory. Anxiety, Stress and Coping. 2010;23(2):127–137. doi: 10.1080/10615800903094273. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Sharpe D, Asmundson GJ. Anxiety sensitivity and intolerance of uncertainty: Requisites of the fundamental fears? Behaviour Research and Therapy. 2007;45(10):2307–2316. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. Dispositional optimism. Trends in Cognitive Sciences. 2014;18(6):293–299. doi: 10.1016/j.tics.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casellas-Grau A, Ochoa C, Ruini C. Psychological and clinical correlates of posttraumatic growth in cancer: A systematic and critical review. Psycho-oncology. 2017;26(12):2007–2018. doi: 10.1002/pon.4426. [DOI] [PubMed] [Google Scholar]
- Chaves C, Castellanos T, Abrams M, Vazquez C. The impact of economic recessions on depression and individual and social well-being: The case of Spain (2006–2013) Social Psychiatry and Psychiatric Epidemiology. 2018;53(9):977–986. doi: 10.1007/s00127-018-1558-2. [DOI] [PubMed] [Google Scholar]
- Clifton JDW, Baker JD, Park CL, Yaden DB, Clifton ABW, Terni P, Seligman MEP. Primal world beliefs. Psychological Assessment. 2019;31(1):82–99. doi: 10.1037/pas0000639. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Shevlin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, Hyland P. The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica. 2018;138(6):536–546. doi: 10.1111/acps.12956. [DOI] [PubMed] [Google Scholar]
- Codagnone C, Bogliacino F, Gómez C, Charris R, Montealegre F, Liva G, Veltri GA. Assessing concerns for the economic consequence of the COVID-19 response and mental health problems associated with economic vulnerability and negative economic shock in Italy, Spain, and the United Kingdom. PLoS ONE. 2020;15(10):e0240876. doi: 10.1371/journal.pone.0240876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordova MJ, Riba MB, Spiegel D. Post-traumatic stress disorder and cancer. The Lancet Psychiatry. 2017;4(4):330–338. doi: 10.1016/S2215-0366(17)30014-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darves-Bornoz J-M, Alonso J, de Girolamo G, de Graaf R, Haro J-M, Kovess-Masfety V, Gasquet I. Main traumatic events in Europe: PTSD in the European study of the epidemiology of mental disorders survey. Journal of Traumatic Stress. 2008;21(5):455–462. doi: 10.1002/jts.20357. [DOI] [PubMed] [Google Scholar]
- DePierro J, Lowe S, Katz C. Lessons learned from 9/11: Mental health perspectives on the COVID-19 pandemic. Psychiatry Research. 2020;288:113024. doi: 10.1016/j.psychres.2020.113024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depoux A, Martin S, Karafillakis E, Preet R, Wilder-Smith A, Larson H. The pandemic of social media panic travels faster than the COVID-19 outbreak. Journal of Travel Medicine. 2020 doi: 10.1093/jtm/taaa031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmondson D. An enduring somatic threat model of posttraumatic stress disorder due to acute life-threatening medical events. Social and Personality Psychology Compass. 2014;8(3):118–134. doi: 10.1111/spc3.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Valle MV, Andrés ML, Urquijo S, Yerro-Avincetto M, López-Morales H, Canet-Juric L. Intolerance of uncertainty over covid-19 pandemic and its effect on anxiety and depressive symptoms. Interamerican Journal of Psychology. 2020;54(2):1–17. doi: 10.30849/ripijp.v54i2.1335. [DOI] [Google Scholar]
- Edmondson D, Chaudoir SR, Mills MA, Park CL, Holub J, Bartkowiak JM. From shattered assumptions to weakened worldviews: Trauma symptoms signal anxiety buffer disruption. Journal of Loss and Trauma. 2011;16(4):358–385. doi: 10.1080/15325024.2011.572030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JR. Response invalidity in empirical research: Causes, detection, and remedies. Journal of Operations Management. 2019;65(1):62–76. doi: 10.1016/j.jom.2018.12.002. [DOI] [Google Scholar]
- Ferry FR, Brady SE, Bunting BP, Murphy SD, Bolton D, O'Neill SM. The economic burden of PTSD in Northern Ireland. Journal of Traumatic Stress. 2015;28(3):191–197. doi: 10.1002/jts.22008. [DOI] [PubMed] [Google Scholar]
- Frazier P, Tennen H, Gavian M, Park C, Tomich P, Tashiro T. Does self-reported posttraumatic growth reflect genuine positive change? Psychological Science. 2009;20(7):912–919. doi: 10.1111/j.1467-9280.2009.02381.x. [DOI] [PubMed] [Google Scholar]
- Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing. JAMA Internal Medicine. 2020;28(8):666–675. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- García FE, Cova F, Rincón P, Vázquez C. Trauma or growth after a natural disaster? The mediating role of rumination processes. European Journal of Psychotraumatology. 2015;6(1):26557. doi: 10.3402/ejpt.v6.26557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García FE, Wlodarczyk A. Psychometric properties of the posttraumatic growth inventory-short form among chilean adults. Journal of Loss and Trauma. 2016;21(4):303–314. doi: 10.1080/15325024.2015.1108788. [DOI] [Google Scholar]
- Google COVID-19 community mobility reports (2020). Retrieved May 5, 2020, from https://www.google.com/covid19/mobility/.
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Iverach L, Menzies R, Menzies RE. Death anxiety and its role in psychopathology: Reviewing the status of a transdiagnostic construct. Clinical Psychology Review. 2014;34(7):580–593. doi: 10.1016/j.cpr.2014.09.002. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R. Assumptive worlds and the stress of traumatic events: applications of the schema construct. Social Cognition. 1989;7(2):113–136. doi: 10.1521/soco.1989.7.2.113. [DOI] [Google Scholar]
- Jayawickreme E, Infurna FJ, Alajak K, Blackie LER, Chopik WJ, Chung JM, Dorfman A, Fleeson W, Forgeard MJC, Frazier P, Furr RM, Grossmann I, Heller AS, Laceulle OM, Lucas RE, Luhmann M, Luong G, Meijer L, McLean KC, Zonneveld R. Post-traumatic growth as positive personality change: Challenges, opportunities, and recommendations. Journal of Personality. 2020 doi: 10.1111/jopy.12591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayawickreme E, Blackie LER. Post-traumatic growth a positive personality change: Evidence, controversies and future directions. European Journal of Personality. 2014;28(4):312–331. doi: 10.1002/per.1963. [DOI] [Google Scholar]
- Johns Hopkins Coronavirus Resource Center. Retrieved April 9 2020, from https://coronavirus.jhu.edu/map.html.
- Karatzias T, Shevlin M, Fyvie C, Hyland P, Efthymiadou E, Wilson D, Roberts N, Bisson JI, Brewin CR, Cloitre M. Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ) Journal of Affective Disorders. 2017;207:181–187. doi: 10.1016/j.jad.2016.09.032. [DOI] [PubMed] [Google Scholar]
- Karatzias T, Shevlin M, Murphy J, McBride O, Ben-Ezra M, Bentall RP, Hyland P. Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: A population-based study. Journal of Traumatic Stress. 2020;33(4):365–370. doi: 10.1002/jts.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52(12):1048. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Lamster F, Lincoln TM, Nittel CM, Rief W, Mehl S. The lonely road to paranoia. A path-analytic investigation of loneliness and paranoia. Comprehensive Psychiatry. 2017;74:35–43. doi: 10.1016/j.comppsych.2016.12.007. [DOI] [PubMed] [Google Scholar]
- Liao Q, Cowling BJ, Lam WW, Ng DM, Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: ten cross-sectional surveys. BMC Infectious Diseases. 2014;14(1):169. doi: 10.1186/1471-2334-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker A, Zoellner T. The Janus face of self-perceived growth: Toward a two-component model of posttraumatic growth. Psychological Inquiry. 2004;15(1):41–48. [Google Scholar]
- Mangelsdorf J, Eid M, Luhmann M. Does growth require suffering? A systematic review and meta-analysis on genuine posttraumatic and postecstatic growth. Psychological Bulletin. 2019;145(3):302–338. doi: 10.1037/bul0000173. [DOI] [PubMed] [Google Scholar]
- Mardia KV. Measures of multivariate skewness and kurtosis with applications. Biometrika. 1970;57(3):519–530. doi: 10.1093/biomet/57.3.519. [DOI] [Google Scholar]
- McBride O, Murphy J, Shevlin M, Gibson-Miller J, Hartman TK, Hyland P, Levita L, Mason L, Martinez AP, McKay R, Stocks TV, Bennett KM, Vallières F, Karatzias T, Valiente C, Vazquez C, Bentall RP. Monitoring the psychological, social, and economic impact of the COVID-19 pandemic in the population: Context, design and conduct of the longitudinal COVID-19 psychological research consortium (C19PRC) study. International Journal of Methods in Psychiatric Research. 2020 doi: 10.1002/mpr.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland S, Webb M, Brown D. All humanity is my ingroup: A measure and studies of identification with all humanity. Journal of Personality and Social Psychology. 2012;103(5):830–853. doi: 10.1037/a0028724. [DOI] [PubMed] [Google Scholar]
- McIntyre JC, Wickham S, Barr B, Bentall RP. Social identity and psychosis: Associations and psychological mechanisms. Schizophrenia Bulletin. 2018;44(3):681–690. doi: 10.1093/schbul/sbx110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo S, Corcoran R, Bentall RP. The Persecution and deservedness scale. Psychology and Psychotherapy: Theory, Research and Practice. 2009;82:247–260. doi: 10.1348/147608308X398337. [DOI] [PubMed] [Google Scholar]
- Motta M, Stecula D, Farhart C. How right-leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the US. Canadian Journal of Political Science. 2020;53(2):335–342. doi: 10.1017/S0008423920000396. [DOI] [Google Scholar]
- Nieto I, Navas JF, Vazquez C. The quality of research on mental health related to the COVID-19 pandemic: A note of caution after a systematic review. Brain, Behavior, and Immunity—Health. 2020 doi: 10.1016/j.bbih.2020.100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Davis CG. Theoretical and methodological issues in the assessment and interpretation of posttraumatic growth. Psychological Inquiry. 2004;15:60–64. doi: 10.1207/s15327965pli1501_02. [DOI] [Google Scholar]
- Odone A, Signorelli C, Stuckler D, Galea S, Amerio A, Bellini L, Bucci D, Capraro M, Gaetti G, Salvati S. The first 10,000 COVID-19 papers in perspective: Are we publishing what we should be publishing? European Journal of Public Health. 2020;30(5):849–850. doi: 10.1093/eurpub/ckaa170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oglesby ME, Gibby BA, Mathes BM, Short NA, Schmidt NB. Intolerance of uncertainty and post-traumatic stress symptoms: An investigation within a treatment seeking trauma-exposed sample. Comprehensive Psychiatry. 2017;72:34–40. doi: 10.1016/j.comppsych.2016.08.011. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Páez D, Rimé B, Basabe N, Wlodarczyk A, Zumeta L. Psychosocial effects of perceived emotional synchrony in collective gatherings. Journal of Personality and Social Psychology. 2015;108(5):711–729. doi: 10.1037/pspi0000014. [DOI] [PubMed] [Google Scholar]
- Park CL. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin. 2010;136(2):257–301. doi: 10.1037/a0018301. [DOI] [PubMed] [Google Scholar]
- Peterson K, Togun T, Klis S, Menten J, Colebunders R. Depression and posttraumatic stress disorder among HIV-infected Gambians on antiretroviral therapy. AIDS Patient Care and STDs. 2012;26(10):589–596. doi: 10.1089/apc.2012.0089. [DOI] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Poulin MJ, Silver RC. When are assumptions shaken? A prospective, longitudinal investigation of negative life events and worldviews in a national sample. Journal of Research in Personality. 2019;83:103866. doi: 10.1016/j.jrp.2019.103866. [DOI] [Google Scholar]
- Prati G, Pietrantoni L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta-analysis. Journal of Loss and Trauma. 2009;14(5):364–388. doi: 10.1080/15325020902724271. [DOI] [Google Scholar]
- Pyszczynski, T., Solomon, S., & Greenberg, J. (2015). Thirty years of terror management theory. In Advances in Experimental Social Psychology, 1st ed., Vol. 52, pp. 1–70.
- Qian M. Psychological responses, behavioral changes and public perceptions during the early phase of the COVID-19 outbreak in China: a population based cross-sectional survey. MedRxiv. 2020;1:1–9. doi: 10.1101/2020.02.18.20024448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rzeszutek M, Oniszczenko W, Schier K, Biernat-Kałuza E, Gasik R. Trauma symptoms, temperament traits, social support and the intensity of pain in a Polish sample of patients suffering from chronic pain. Personality and Individual Differences. 2015;83:13–17. doi: 10.1016/j.paid.2015.03.036. [DOI] [Google Scholar]
- Rzeszutek M, Gruszczyńska E. Paradoxical effect of social support among people living with HIV: A diary study investigating the buffering hypothesis. Journal of Psychosomatic Research. 2018;109:25–31. doi: 10.1016/j.jpsychores.2018.03.006. [DOI] [PubMed] [Google Scholar]
- Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, Rasoulpoor S, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJ. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine. 2007;69(3):242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- Shakespeare-Finch J, Lurie-Beck J. A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. Journal of Anxiety Disorders. 2014;28(2):223–229. doi: 10.1016/j.janxdis.2013.10.005. [DOI] [PubMed] [Google Scholar]
- Sharma M, Yadav K, Yadav N, Ferdinand KC. Zika virus pandemic—analysis of facebook as a social media health information platform. American Journal of Infection Control. 2017;45(3):301–302. doi: 10.1016/j.ajic.2016.08.022. [DOI] [PubMed] [Google Scholar]
- Shevlin M, Hyland P, Karatzias T. Is posttraumatic stress disorder meaningful in the context of the COVID-19 pandemic? A response to Van Overmeire's commentary on Karatzias et al (2020) Journal of Traumatic Stress. 2020;33(5):866–868. doi: 10.1002/jts.22592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M, McBride O, Murphy J, Miller J, Hartman T, Levita L, Bentall R. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6(6):E125. doi: 10.1192/bjo.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson E, DeLongis A, Steele R, Cadell S, Andrews GS, Siden H. Siblings of children with a complex chronic health condition: Maternal posttraumatic growth as a predictor of changes in child behavior problems. Journal of Pediatric Psychology. 2017;42(1):104–113. doi: 10.1093/jpepsy/jsw053. [DOI] [PubMed] [Google Scholar]
- Sumalla EC, Ochoa C, Blanco I. Posttraumatic growth in cancer: Reality or illusion? Clinical Psychology Review. 2009;29(1):24–33. doi: 10.1016/j.cpr.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. British Journal of Health Psychology. 2014;19(3):592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- Tedeschi R, Calhoun L. The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Tedeschi R, Calhoun L. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004;15(1):1–18. doi: 10.1207/s15327965pli1501_01. [DOI] [Google Scholar]
- Tedeschi RG, Shakespeare-Finch J, Taku K, Calhoun LG. Posttraumatic growth. Routledge. 2018 doi: 10.4324/9781315527451. [DOI] [Google Scholar]
- Tomás-Sábado J, Gómez-Benito J. Construction and validation of the death anxiety inventory (DAI) European Journal of Psychological Assessment. 2005;21(2):108–114. doi: 10.1027/1015-5759.21.2.108. [DOI] [Google Scholar]
- Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology. 2004;86(2):320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valiente, C., Contreras, A., Peinado, V., Trucharte, A., Martinez, A. P., & Vázquez, C. (2020a). Psychological adjustment in Spain during the COVID-19 pandemic: Positive and negative mental health outcomes in the general population. Spanish Journal of Psychology (in press). [DOI] [PubMed]
- Valiente C, Contreras A, Trucharte A, Peinado V, Espinosa R. Psychometric properties and normative data of the Spanish version of short form persecution and deservedness scale. Psychosis. 2020 doi: 10.1080/17522439.2020.1834605. [DOI] [Google Scholar]
- Valiente C, Vázquez C, Contreras A, Peinado V, Trucharte A. A symptom-based definition of resilience in times of pandemics: Patterns of psychological responses over time and their predictors. European Journal of Psychotraumatology. 2020 doi: 10.1080/20008198.2020.1871555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Prooijen J-W, Douglas KM. Conspiracy theories as part of history: The role of societal crisis situations. Memory Studies. 2017;10(3):323–333. doi: 10.1177/1750698017701615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vazquez C. A new look at trauma: From vulnerability models to resilience and positive changes. In: Moore KA, Kaniasty K, Buchwald P, Sese A, editors. Stress and anxiety: Applications to health and well-being, work stressors and assessment. Berlin: Logos Verlag; 2013. pp. 27–40. [Google Scholar]
- Vázquez C, Hervás G. Perceived benefits after terrorist attacks: The role of positive and negative emotions. The Journal of Positive Psychology. 2010;5(2):154–163. doi: 10.1080/17439761003630060. [DOI] [Google Scholar]
- Webster RK, Brooks SK, Smith LE, Woodland L, Wessely S, Rubin GJ. How to improve adherence with quarantine: Rapid review of the evidence. Public Health. 2020;182:163–169. doi: 10.1016/j.puhe.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westermann S, Kesting ML, Lincoln TM. Being deluded after being excluded? How emotion regulation deficits in paranoia-prone individuals affect state paranoia during experimentally induced social stress. Behavior Therapy. 2012;43(2):329–340. doi: 10.1016/j.beth.2011.07.005. [DOI] [PubMed] [Google Scholar]
- Whetten K, Shirey K, Pence BW, Yao J, Thielman N, Whetten R, Reddy E. Trauma history and depression predict incomplete adherence to antiretroviral therapies in a low income country. PLoS ONE. 2013;8(10):e74771. doi: 10.1371/journal.pone.0074771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2018). International statistical classification of diseases and related health problems (11th rev.). https://icd.who.int/browse11/l-m/en.
- World Health Organization. Regional office for Europe. (2020). Retrieved April 8, 2020, from http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19.
- Wu X, Kaminga AC, Dai W, Deng J, Wang Z, Pan X, Liu A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. Journal of Affective Disorders. 2019;243:408–415. doi: 10.1016/j.jad.2018.09.023. [DOI] [PubMed] [Google Scholar]
- Yu, C.Y. (2002). Evaluating cut-off criteria of model fit indices for latent variable models with binary and continuous outcomes. Unpublished doctoral dissertation, University of California, Los Angeles.
- Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Research. 2020;288:112958. doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner T, Maercker A. Posttraumatic growth in clinical psychology—A critical review and introduction of a two component model. Clinical psychology review. 2006;26(5):626–653. doi: 10.1016/j.cpr.2006.01.008. [DOI] [PubMed] [Google Scholar]