Abstract
Background
Acute kidney injury (AKI) is an important complication of coronavirus disease 2019 (COVID-19), which could be caused by both systematic responses from multi-organ dysfunction and direct virus infection. While advanced evidence is needed regarding its clinical features and mechanisms. We aimed to describe two phenotypes of AKI as well as their risk factors and the association with mortality.
Methods
Consecutive hospitalized patients with COVID-19 in tertiary hospitals in Wuhan, China from 1 January 2020 to 23 March 2020 were included. Patients with AKI were classified as AKI-early and AKI-late according to the sequence of organ dysfunction (kidney as the first dysfunctional organ or not). Demographic and clinical features were compared between two AKI groups. Their risk factors and the associations with in-hospital mortality were analyzed.
Results
A total of 4020 cases with laboratory-confirmed COVID-19 were included and 285 (7.09%) of them were identified as AKI. Compared with patients with AKI-early, patients with AKI-late had significantly higher levels of systemic inflammatory markers. Both AKIs were associated with an increased risk of in-hospital mortality, with similar fully adjusted hazard ratios of 2.46 [95% confidence interval (CI) 1.35–4.49] for AKI-early and 3.09 (95% CI 2.17–4.40) for AKI-late. Only hypertension was independently associated with the risk of AKI-early. While age, history of chronic kidney disease and the levels of inflammatory biomarkers were associated with the risk of AKI-late.
Conclusions
AKI among patients with COVID-19 has two clinical phenotypes, which could be due to different mechanisms. Considering the increased risk for mortality for both phenotypes, monitoring for AKI should be emphasized during COVID-19.
Keywords: AKI, COVID-19, epidemiology, renal failure, SARS-CoV-2
KEY LEARNING POINTS
What is already known about this subject?
Acute kidney injury (AKI) is an important complication of coronavirus disease 2019 (COVID-19) that could be caused by both systematic responses from multi-organ dysfunction and direct virus infection.
What this study adds?
While advanced evidence is needed regarding its clinical features and mechanisms, we aimed to describe two phenotypes of AKI, as well as their risk factors and the association with mortality.
What impact this may have on practice or policy?
Considering the asymptomatic nature of kidney disease and lack of urinary abnormalities for almost half of patients with AKI, especially for AKI-early, the kidney involvement in COVID-19 patients is likely to be overlooked. Therefore, monitoring markers for AKI should be emphasized for patients with COVID-19.
INTRODUCTION
Acute kidney injury (AKI) is rapidly emerging as a key threat in coronavirus disease 2019 (COVID-19) in addition to respiratory diseases. The reported incidence of AKI ranged from 0.5% to 46% among hospitalized patients with COVID-19 [1–6] and 25–29% among critically ill patients [7–9]. AKI occurred a median of 7–15 days from onset of symptoms [1–5] and was associated with mortality [4, 10].
The mechanisms underlying the effect of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection on kidney injury, however, remain incompletely understood. One possibility to consider is that the probable pathogenesis of kidney involvement may be similar to the SARS-CoV infection, which includes cytokine release syndrome (CRS), organ crosstalk and systemic effects [11, 12]. AKI could be a result of hemodynamic fluctuations leading to ischemic tubular injury [13], which is assumed to be a severe systemic inflammatory response, and microvascular thrombosis of SARS-CoV-2 infection [14]. Crosstalk between the injured lungs and heart and comorbid with chronic kidney disease (CKD) can also occur in AKI, because of the intrarenal inflammation, increased vascular permeability, volume depletion and cardiomyopathy [15].
However, the high incidence of AKI in COVID-19 prompted speculation that direct SARS-CoV-2 virus transduction of renal tubular epithelial cells and podocytes may play an important role in kidney involvement. This hypothesis was supported by histopathology findings and the presence of angiotensin-converting enzyme 2 (ACE2) in the proximal kidney tubules, as the functional receptor acts as a receptor for SARS-CoV-2 spike protein attachment, through which the virus gains access to the host cell [16, 17]. A systematic review of the pathological conclusions in COVID-19 has shown that the most common pathological manifestations were varying degrees of acute tubular necrosis that predominantly presented in the proximal tubules [18]. Inclusions resembling viral particles were visualized in tubular cells on electron microscopy in autopsy specimens [16, 19], but this finding could not be replicated initially [20–23]. The putative SARS-CoV-2 particles have been interpreted as clathrin-coated vesicles or multivesicular bodies by other researchers [20, 24, 25]. The kidney tropism of SARS-CoV-2 was confirmed as the viral RNA was found in all kidney compartments (glomeruli, tubules and vascular compartments), mainly in glomerular cells [26]. The largest autopsy series on post-mortem kidney tissue from 63 patients found that 60% of the kidney samples contained SARS-CoV-2 mRNA, which provided the evidence of direct infection of kidneys [27].
Since the pathogenesis of AKI onset is unknown, and morphologic correlates are few and limited to patient reports or autopsy series, we hypothesized the sequence of AKI versus other organ dysfunctions could be explained by indirect factors (e.g. cytokine-mediated injury) and by direct viral infection and replication in kidney epithelial cells. In this study, the clinical features of AKI and its association with overall mortality were investigated and compared between different phenotypes.
MATERIALS AND METHODS
Data collection
The National Health Commission of China collected COVID-19-related medical records from the designated tertiary hospital (>500 beds) in Wuhan, China to provide scientific evidence for medical treatment on COVID-19 patients. The standardized in-patient discharge summaries and the electronic full medical records of confirmed COVID-19 cases were required to be submitted to the COVID-19 reporting system of the National Health Commission of China. The retrospective analysis was based on the national database of the COVID-19 reporting system and the data cutoff for the study was 23 March 2020.
All the data, including demographic characteristics, comorbidities, laboratory tests, treatments, morbidities and survival status, were extracted from the database. Two researchers (S.P. and H.W.) independently reviewed the data collection and extraction forms for quality control purposes.
This study was approved by the National Health Commission of China and the institutional review board of Peking University Health Science Centre (IRB00001052-20032).
Study population
We identified all the patients in the national electronic health record who had COVID-19 test results recorded from 1 January 2020 to 23 March 2020. Patients were deemed to be COVID-19-positive if any test was positive for SARS-CoV-2 RNA. Those patients who did not have available medical information, had duplicate records or had received renal replacement therapy were excluded from this study. The flow chart of the study population is shown in Figure 1.
FIGURE 1.
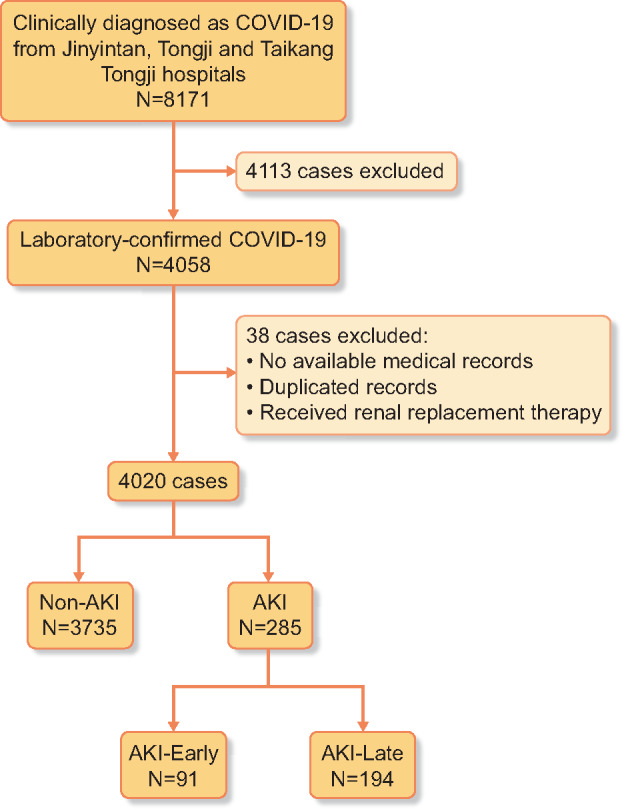
Flow chart of study population. The laboratory-confirmed cases of COVID-19 were included in this study. For those patients who did not have available medical information, the duplicated records and the patients had received renal transplantation were excluded.
The severity of COVID-19 was classified by the National Health Commission of China guidance version 7.0 [28]. Cases were defined as mild if the clinical symptoms were mild and without any sign of pneumonia on imaging; moderate if pneumonia, with symptoms such as fever and respiratory symptoms, was radiologically identified; severe if the patient had respiratory distress (≥30 breaths/min), oxygen saturation ≤93% at rest or arterial oxygen tension (PaO2)/fraction of inspired oxygen ≤300 mmHg; and critical as meeting any of the following criteria: respiratory failure and requiring mechanical ventilation, shock or other organ failures that required intensive care unit care.
Definition of AKI
The 2012 Kidney Disease: Improving Global Outcomes (KDIGO) guideline of AKI was used [29] and AKI was defined as an increase in serum creatinine of 0.3 mg/dL (or 26.5 μmol/L) within 48 h or a 50% increase in serum creatinine from the baseline within 7 days. Baseline medical history and laboratory data were extracted on admission to determine whether the AKI event occurred. For those who did not have a repeat serum creatinine assay within 7 days, we expanded the criteria to an increase in serum creatinine of 50% during the hospital stay [30]. Furthermore, patients who had a decreasing trend of serum creatinine after hospital admission and serum creatinine had decreased by >50% of its peak level were also identified as having AKI [31, 32].
The onset date of AKI was defined by the first date when serum creatinine met the criteria of diagnosis. For those who had a decreasing trend of serum creatinine and met the criteria for AKI, the admission date was designated as the onset date of AKI [30], which could indicate the onset of AKI before admission [31].
Two phenotypes of AKI were identified by the sequence of organ dysfunction. AKI-early was defined as AKI onset before the onset date of any other organ dysfunction and AKI-late was for all other circumstances.
Comorbidities and complications
Comorbidities, including hypertension, diabetes, cardiovascular disease, carcinoma and CKD, were identified by International Classification of Diseases (ICD) codes or self-report. The ICD codes for CKD from the China Kidney Disease Network [33] and other relevant ICD codes, including kidney transplantation, are listed in Supplementary data, Tables S1 and S2.
Information on antihypertensive medication use, including ACE inhibitors (ACEis) or angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs), beta-blockers and thiazide diuretics, was obtained from the medical records and summarized at baseline on admission (Supplementary data, Table S3).
Information on antiviral medication use, including interferon alfa, lopinavir–ritonavir, ribavirin, umifenovir and neuraminidase inhibitor, was obtained according to the National Health Commission of China guidance version 7.0 (Supplementary data, Table S4) [28].
The complications were manually adjudicated by clinicians, including septic shock, acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation, heart failure, acute myocardial injury and multiple organ dysfunction syndrome (MODS), and the diagnostic criteria are provided in the Supplementary data, Description 1.
Statistical analysis
Continuous variables were expressed as mean [standard deviation (SD)] if normally distributed and as median [interquartile range (IQR)] for skewed distributions. Categorical variables were expressed as frequencies and percentages. Continuous variables were compared using analyses of variance and Kruskal–Wallis tests for those with normal and skewed distributions, respectively. Categorical variables were analyzed by the chi-square test or Fisher’s exact test, as appropriate. Multinomial logistic regression analyses were conducted to explore the potential predictors for AKI. Covariates in the models included age (continuous), sex (male or female), hypertension (yes or no), diabetes (yes or no), cardiovascular disease (yes or no), CKD (yes or no), mean arterial pressure (continuous), ACEi/ARB use (yes or no), other antihypertension medication use (yes or no for either CCBs, beta-blockers or thiazide diuretics) and biomarkers of inflammation above the reference range [yes or no for high sensitivity C-reactive protein (hs-CRP; 10 mg/L), interleukin-6 (IL-6; 7 pg/mL), ferritin (300 ng/mL)]. Crude and adjusted relative risk ratios (RRRs) with 95% confidence intervals (CIs) were reported.
Cox proportional hazards models were used to investigate the association between AKI and all-cause in-hospital mortality. Covariates in the models also included age (continuous), sex (male or female), comorbidities (yes or no for hypertension, diabetes, cardiovascular disease and carcinoma) and other organ dysfunctions (yes or no for ARDS, acute myocardial injury, heart failure). Crude and adjusted hazard ratios (HRs) with 95% CIs were reported. Inflammation biomarkers in the regression analysis were dummy coded, including hs-CRP, IL-6 and ferritin. The proportional hazards assumption was fulfilled for all analyses tested using the time-dependent covariate method [34].
All P-values were two-sided and P < 0.05 was considered to indicate statistical significance. The analyses were performed with R software version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria) and Stata version 14.1 (StataCorp, College Station, TX, USA).
RESULTS
Demographic and clinical characteristics
A total of 4020 patients with laboratory-confirmed COVID-19 were included (Table 1). The median age was 61 years (IQR 50–60) and 1912 (47.6%) patients were male. Hypertension was the most common comorbidity (21.2%), followed by diabetes (10.5%) and cardiovascular disease (6.7%). Regarding the complications of COVID-19, ARDS was the most common (16.3%), followed by MODS (12.2%). The overall in-hospital mortality was 4.8% (n = 193).
Table 1.
Clinical characteristics of study patients
| Total (n = 4020) | Non-AKI (n = 3735) | AKI-early (n = 91) | AKI-late (n = 194) | P-value | |
|---|---|---|---|---|---|
| Demographics and clinical characteristics | |||||
| Age (years), median (IQR), years | 61 (50–69) | 61 (50–68) | 71 (63–79) | 70 (63–78) | <0.001 |
| <18, n (%) | 23 (0.6) | 23 (0.6) | 0 (0.0) | 0 (0.0) | – |
| 18–44, n (%) | 648 (16.1) | 638 (17.1) | 5 (5.5) | 5 (2.6) | – |
| 45–64, n (%) | 1788 (44.5) | 1711 (45.8) | 22 (24.2) | 55 (28.4) | – |
| ≥65, n (%) | 1561 (38.8) | 1363 (36.5) | 64 (70.3 ) | 134 (69.1) | – |
| Male, n (%) | 1912 (47.6) | 1751 (46.9) | 52 (57.1) | 109 (56.2) | 0.007 |
| Comorbidity, n (%) | |||||
| Hypertension | 852 (21.2) | 757 (20.3) | 35 (38.5) | 60 (30.9) | <0.001 |
| Diabetes | 424 (10.5) | 379 (10.1) | 14 (15.4) | 31 (16.0) | 0.011 |
| Cardiovascular disease | 270 (6.7) | 235 (6.3) | 9 (9.9) | 26 (13.4) | <0.001 |
| Carcinoma | 40 (1.0) | 37 (1.0) | 1 (1.1) | 2 (1.0) | 0.67 |
| CKD | 100 (2.5) | 72 (1.9) | 8 (8.8) | 20 (10.3) | <0.001 |
| ACEI/ARBs use history | 79 (2.0) | 69 (1.8) | 4 (4.4) | 6 (3.1) | 0.094 |
| Laboratory result in admission, n (%) | |||||
| Glycosuria | 246 (10.6) | 207 (9.6) | 5 (9.8) | 34 (31.2) | <0.001 |
| Proteinuria | 941 (33.6) | 778 (30.2) | 36 (51.4) | 127 (84.7) | <0.001 |
| Creatinine (μmol/L), median (IQR) | 64.265 (53–78.505) | 63.2 (52.15–76) | 101 (75.67–133) | 93 (70–135) | <0.001 |
| Serum potassium (mmol/L), median (IQR), mmol/L | 4.18 (3.84–4.48) | 4.175 (3.85–4.46) | 4.3 (3.8–4.57) | 4.13 (3.68–4.74) | 0.26 |
| White blood cell count (×109/L), median (IQR) | 5.77 (4.57–7.34) | 5.705 (4.55–7.18) | 6.37 (4.86–8.07) | 7.99 (5.46–12.28) | <0.001 |
| Lymphocyte count (×109/L), median (IQR) | 1.31 (0.87–1.79) | 1.36 (0.92–1.81) | 0.9 (0.65–1.34) | 0.61 (0.43–0.89) | <0.001 |
| Platelet count (×109/L), median (IQR) | 214.5 (167.5–271) | 217 (171–273) | 212.5 (160.5–253) | 154 (119–217) | <0.001 |
| hs-CRP (mg/L), median (IQR) | 13.5 (1.8–60.1) | 10.1 (1.6–49.5) | 49.5 (13.6–91.9) | 98.2 (45.7–160) | <0.001 |
| IL-6 (pg/mL), median (IQR) | 5.6 (2.01–12.4) | 5.03 (1.88–11.4) | 11.155 (7.82–25.8) | 16.52 (9.19–50.08) | <0.001 |
| Ferritin (ng/mL), median (IQR) | 489 (255.47–936.75) | 447.3 (233.2–841.6) | 583.99 (359.6–1087.45) | 1264.7 (611.59–2000) | <0.001 |
| High sensitivity cardiac troponin I (ng/mL), median (IQR) | 4.5 (1.9–11) | 3.9 (1.9–9.5) | 9.6 (4.15–19.35) | 27.3 (11.5–74.1) | <0.001 |
| Mean arterial pressure (mmHg), median (IQR) | 122 (103–123) | 122 (104–123) | 110 (105–123) | 109.5 (95–121) | 0.019 |
| Stages of AKI, n (%) | <0.001 | ||||
| Stage 1 | 152 (53.3) | 0 | 75 (82.4) | 77 (39.7) | – |
| Stage 2 | 66 (23.2) | 0 | 10 (11.0) | 56 (28.9) | – |
| Stage 3 | 67 (23.5) | 0 | 6 (6.6) | 61 (31.4) | – |
| Disease severity statues, n (%) | <0.001 | ||||
| Mild | 175 (4.4) | 174 (4.7) | 1 (1.1) | 0 (0.0) | – |
| Moderate | 1716 (42.7) | 1693 (45.3) | 16 (17.6) | 7 (3.6) | – |
| Severe | 1492 (37.1) | 1422 (38.1) | 43 (47.3) | 27 (13.9) | – |
| Critical | 637 (15.8) | 446 (11.9) | 31 (34.1) | 160 (82.5) | – |
| Complications, n (%) | |||||
| Septic shock | 25 (0.6) | 12 (0.3) | 0 (0.0) | 13 (6.7) | <0.001 |
| ARDS | 656 (16.3) | 523 (14.0) | 20 (22.0) | 113 (58.2) | <0.001 |
| DIC | 15 (0.4) | 5 (0.1) | 1 (1.1) | 9 (4.6) | <0.001 |
| Conscious disturbance | 56 (1.4) | 34 (0.9) | 2 (2.2) | 20 (10.3) | <0.001 |
| Heart failure | 479 (11.9) | 293 (7.8) | 21 (23.1) | 165 (85.1) | <0.001 |
| Acute myocardial injury | 432 (10.7) | 291 (7.8) | 14 (15.4) | 127 (65.5) | <0.001 |
| MODS | 491 (12.2) | 258 (6.9) | 39 (42.9) | 194 (100) | <0.001 |
| Treatment, n (%) | |||||
| Antiviral therapy | 2685 (66.8) | 2477 (66.3) | 75 (82.4) | 133 (68.6) | 0.005 |
| Glucocorticoid therapy | 877 (21.8) | 715 (19.1) | 38 (41.8) | 124 (63.9) | <0.001 |
| Chloroquine/hydroxychloroquine | 453 (11.3) | 424 (11.4) | 12 (13.2) | 17 (8.8) | 0.45 |
| Tocilizumab | 98 (2.4) | 76 (2.0) | 6 (6.6) | 16 (8.2) | <0.001 |
| Mechanical ventilation, n (%) | |||||
| Invasive | 208 (5.2) | 83 (2.2) | 14 (15.4) | 111 (57.2) | <0.001 |
| Non-invasive | 500 (12.4) | 345 (9.2) | 24 (26.4) | 131 (67.5) | <0.001 |
| CRRT | 83 (2.1) | 16 (0.4) | 7 (7.7) | 60 (30.9) | <0.001 |
| All-cause in-hospital death, n (%) | 193 (4.8) | 81 (2.2) | 13 (14.3) | 99 (51.0) | <0.001 |
Also, 66.8% of patients received antiviral treatment (either interferon-α, lopinavir–ritonavir, ribavirin, arbidol, oseltamivir or peramivir) and 21.8% received systematic glucocorticoid therapy. Invasive ventilation was used in 208 (5.2%) patients and continuous renal replacement therapy (CRRT) was used in 83 (2.1%) patients.
Two phenotypes of AKI
A total of 285 (7.1%) patients were diagnosed with AKI, 91 of whom were identified as AKI-early and 194 as AKI-late. Compared with non-AKI patients, patients with AKI were observed to be older, with more underlying comorbidities. Also, AKI patients tended to have more severe clinical manifestations, were more likely to receive life-sustaining treatment (i.e. mechanical ventilation, CRRT) and had higher mortality rates (Table 1).
Compared with the AKI-early group, the AKI-late group had significantly higher levels of systemic inflammatory response (peripheral white blood cell count, hs-CRP, IL-6 and ferritin); a higher percentage of proteinuria and glucosuria; lower mean arterial pressure on admission; higher rates of lymphocytopenia, thrombocytopenia and coagulation disorders on admission and higher mortality.
AKI and all-cause mortality
The association of AKI and all-cause mortality is shown in Table 2. Compared with non-AKI patients, AKI patients appeared to have a greater risk of all-cause mortality in both unadjusted and adjusted analyses. The age- and sex-adjusted HRs for mortality were higher in the AKI-late group compared with the AKI-early group and was similar in the fully adjusted model, which were 2.46 (95% CI 1.35–4.49) and 3.09 (95% CI 2.17–4.40), respectively.
Table 2.
Cox proportional hazards models of all-cause in-hospital mortality
| Group | Crude HR (95% CI) | Adjusted HR (95% CI) Model 1a | Adjusted HR (95% CI) Model 2b | Adjusted HR (95% CI) Model 3c |
|---|---|---|---|---|
| Non-AKI | Ref. | Ref. | Ref. | Ref. |
| AKI-early | 5.08 (2.82–9.13) | 3.57 (1.97–6.46) | 3.64 (2.01–6.59) | 2.46 (1.35–4.49) |
| AKI-late | 22.05 (16.43–29.60) | 15.75 (11.56–21.46) | 15.51 (11.37–21.15) | 3.09 (2.17–4.40) |
Model adjusted for age and sex.
Model adjusted for age, sex and comorbidities (i.e. hypertension, diabetes, cardiovascular disease and carcinoma).
Model adjusted for age, sex, comorbidities and other organ dysfunction (i.e. ARDS, acute myocardial injury and heart failure).
Risk factors of AKI
Hypertension was independently associated with a significant risk of AKI-early, with a fully adjusted RRR of 2.29 (95% CI 1.12–4.67). No other variables were found to be independently associated with an increased risk of AKI-early (Table 3).
Table 3.
Independent predictors of AKI development from multivariable logistic regression analysis
| Variables | Crude RRR (95% CI)a |
Adjusted RRR (95% CI) modelb |
||
|---|---|---|---|---|
| AKI-early | AKI-late | AKI-early | AKI-late | |
| Age (years) | 1.024 (0.996–1.050) | 1.06 (1.04–1.07) | 1.023 (0.996–1.050) | 1.05 (1.04–1.07) |
| Sex (Ref = female) | 0.84 (0.44–1.61) | 0.89 (0.58–1.36) | 0.85 (0.45–1.61) | 0.90 (0.59–1.37) |
| Comorbidity | ||||
| Hypertension | 2.37 (1.17–4.80) | 1.591 (0.997–2.543) | 2.29 (1.12–4.67) | 1.54 (0.96–2.47) |
| Diabetes | 1.26 (0.58–2.73) | 1.43 (0.82–2.47) | 1.25 (0.58–2.72) | 1.41 (0.82–2.45) |
| Cardiovascular disease | 0.92 (0.37–2.28) | 1.29 (0.69–2.43) | 0.92 (0.37–2.26) | 1.29 (0.69–2.42) |
| CKD | 2.96 (0.82–10.63) | 4.40 (1.74–11.68) | 2.85 (0.79–10.27) | 4.21 (1.67–10.64) |
| Mean arterial pressure (mmHg) | 1.00 (0.98–1.02) | 0.987 (0.974–1.001) | 1.001 (0.980–1.022) | 0.988 (0.975–1.001) |
| ACEI/ARB use history | 2.62 (0.72–9.58) | 0.92 (0.24–3.52) | 2.05 (0.49–8.62) | 0.74 (0.18–2.99) |
| Biomarkers of inflammation | ||||
| hs-CRP ≥10 mg/L | 2.95 (0.93–9.37) | 7.77 (2.71–22.30) | 2.98 (0.93–9.51) | 7.81 (2.72–22.44) |
| IL-6 ≥7 pg/mL | 1.99 (0.91–4.37) | 1.59 (0.91–2.81) | 1.98 (0.90–4.34) | 1.60 (0.91–2.81) |
| Ferritin ≥300 ng/mL | 0.98 (0.37–2.59) | 4.50 (1.94–10.44) | 0.99 (0.37–2.64) | 4.59 (1.97–10.68) |
Reference group comprised non-AKI group (RRR = 1.00).
Model adjusted for the use of other baseline antihypertensive medications (i.e. CCBs, beta-blockers and thiazide diuretics).
Age, CKD and elevated levels of hs-CRP and ferritin contributed to the risk of AKI-late, with fully adjusted RRRs of 1.05 (per year increase; 95% CI 1.04–1.07), 4.21 (95% CI 1.67–10.64), 7.81 (95% CI 2.72–22.44) and 4.59 (95% CI 1.97–10.68), respectively. A history of ACEi or ARB use and the levels of mean arterial pressure were not independently associated with the increased risk of AKI-late.
DISCUSSION
This study demonstrates that for patients with COVID-19, AKI is a common complication with two clinical phenotypes that are both independently associated with an increased risk of mortality. Hence, monitoring for AKI should be emphasized during the COVID-19 pandemic.
The incidence of AKI has been reported by previous studies, ranging from 0.5 to 46% among hospitalized patients with COVID-19 [1–6]. The variation in the reported incidence may be due to a relatively small sample size, a short period of follow-up for most studies (especially for early reviews), different practice patterns that may affect the ability to identify AKI and variations in the severity of COVID-19. In our multicenter study based on 4020 patients of COVID-19, the total incidence of AKI was 7.09%, which is similar to a more recent systematic review [8.9% (95% CI 4.6–14.5)] [35] and is close to the incidence rate of AKI in patients with community-acquired pneumonia and SARS infection [36, 37].
The US-based studies demonstrated a much greater incidence of AKI and associated mortality than the reviews from China. That can be attributed to the following reasons. First, the higher burden of comorbidities in the US population [6, 13, 38] compared with the Chinese population [1, 4]. Second may be the differences in ACE2 expression between Asian and Caucasian individuals in various nephron segments. This would suggest that the susceptibility to kidney injury from SARS-CoV-2 might be higher in Caucasians compared with Asians.
Furthermore, AKI developed at a median of 3 (IQR 1–10) days from admission among the COVID-19 patients in our cohort, which was much earlier than that in previous studies, with a median of 7–15 days from the first appearance of symptoms [2, 4]. There are several possible explanations for this.
In the early days of COVID-19 outbreak in Wuhan, China the healthcare needs due to the pandemic outbreak exceeded the capabilities of the Wuhan hospitals and therefore could have lead to delays in hospitalization of patients. According to an early descriptive study from China, there was an average of 1 week elapsed between the initial appearance of symptoms and admission to the hospital [2]. Also, at the beginning of the outbreak, medical staff tended to focus on the respiratory symptoms, which could also have contributed to delayed diagnoses of AKI. A recent study showed that one-third of AKI developed within 24 h of admission [6]. Thus the early detection and identification of AKI are essential.
Due to the phylogenetic homogeneity between SARS-CoV-2 and SARS-CoV (the pathogen of SARS), the mechanisms of AKI in COVID-19 and SARS are somewhat similar. It was confirmed that the release of inflammatory cytokines could be intensely induced after SARS-CoV infection, which in turn leads to organ dysfunction [39, 40]. The overproduction of cytokines was regarded to be simultaneously involved in lung–kidney crosstalk. The increase in systemic immune mediators that caused inflammation, oxidative stress and increased pulmonary vascular permeability facilitated and exacerbated kidney function [41]. It is generally accepted that the AKI among patients with COVID-19 is due to similar mechanisms [11, 15]. IL-6 is the major driver of CRS, and the use of IL-6 inhibitor has been shown to be effective in the treatment of severe COVID-19 cases [42]. In our study, the association between elevated inflammatory markers (including hs-CRP and ferritin) and increased risk of AKI-late also supported this hypothesis.
Furthermore, our study revealed another phenotype of AKI without obvious systematic inflammation that occurred before other organ dysfunction, which had been seldom reported previously. SARS-CoV-2 can be detected in multiple organs, including the lungs, pharynx, heart and kidneys, which indicates a broad organotropism of SARS-CoV-2 [43]. Histopathological data from COVID-19 have confirmed the presence of coronavirus-like particles with 80–160 nm diameters in the tubular epithelium or podocytes, as well as the accumulation of SARS-CoV-2 nucleocapsid protein in the tubules. Also, varying degrees of diffuse proximal tubule necrosis with the loss of brush border, nonisometric vacuole degeneration and even frank necrosis can be observed [16, 20]. While the hypothesis of direct infection of kidneys is controversial, some researchers believe that the identification of SARS-CoV-2 particles by electron microscopy or the presence of viral RNA or proteins should not be considered conclusive evidence of infection. However, a recent study that documented replication-competent SARS-CoV-2 isolated from a post-mortem kidney [27] provides definitive proof that kidney tissue in patients with COVID-19 contains infective SARS-CoV-2 virus. The detection of viral RNA by in situ hybridization and polymerase chain reaction in various kidney compartments of autopsy specimens implies that SARS-CoV-2 can replicate in the human kidney.
The cellular target of SARS-CoV-2 replication in the kidney is still unclear. AKI could be a result of hemodynamic fluctuations leading to ischemic tubular injury, which has been confirmed by several pathologic series [13, 44]. The infiltration of proinflammatory cells, such as the CD68+ macrophages, CD8+ T cells and CD56+ natural killer cells, may also accelerate tubular damage. An observation study shows that higher baseline levels of inflammatory markers, such as ferritin, CRP, procalcitonin and lactate dehydrogenase, are associated with AKI and AKI-related renal replacement therapy, indicating that hemodynamic instability leading to ischemic acute tubular injury is the predominant cause of AKI [13]. While it is also plausible that specific immunological glomerular injury is mediated by immunocomplexes of viral antigen or virus-induced immunological effectors, the development of collapsing focal segmental glomerulosclerosis in people with COVID-19 who have the high-risk APOL1 genotype (G1/G1) has been reported [45, 46]. These findings only exist in sporadic cases and have not been validated in large cohorts. Also, the possibility this patient had APOL1 nephropathy prior to the SARS-CoV-2 infection could not be excluded. In our study, the phenotype of AKI-early could be caused by the direct effect of SARS-CoV-2 on kidney cells. Regarding predictors of AKI-early, only hypertension (after adjusting for the use of ACEis or ARBs) was identified. Considering the asymptomatic nature of kidney disease and the lack of urinary abnormalities for almost half of patients with AKI-early, it is not unlikely that those patients were treated as asymptomatic infections. Therefore monitoring markers for AKI should be emphasized for patients with COVID-19.
COVID-19 was also increasingly reported among patients with AKI, with higher mortality rates than those seen in the general population [4, 6]. Cheng et al. [4] first reported that AKI patients had an excess risk of mortality among COVID-19 patients. In addition, a meta-analysis that evaluated the summarized data from Chinese cases with COVID-19 (including the study mentioned above) showed that patients with severe AKI (KDIGO Stage 3) have a significant 4-fold increased risk of death compared with non-AKI or mild to moderate AKI [47]. Our study supported the independent association with the presence of AKI and all-cause mortality after adjusting for multiple potential confounders.
Our study has the advantages of a relatively large sample size and detailed information on various variables based on electronic medical records of tertiary hospitals. However, certain limitations need to be addressed. First, the incidence of AKI might be underestimated due to the real-world nature of data collection. Second, there was uncertainty regarding the time of onset of AKI before admission. Third, 52.9% of the study population were severe or critical cases of COVID-19, therefore the generalizability of our results is limited. Finally, the possibility of residual confounding exists for our observational study.
This study demonstrates that AKI is a common complication of COVID-19. Although the exact mechanisms of AKI need to be further explored, our findings suggest that AKI could be either a sentinel of sequential organ dysfunction or the consequence of multi-organ dysfunction. Our study highlights the importance of monitoring for AKI during the COVID-19 pandemic. Further studies are needed to investigate the kidney involvement in mild or asymptomatic cases, as well as active intervention for AKI among patients with COVID-19.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the healthcare professionals on the front lines of this pandemic.
FUNDING
This study was supported by grants from Special Research Fund of Peking University for Prevention and Control of COVID-19 and the Fundamental Research Funds for the Central Universities (PKU2020PKYZX003, BMU2020HKYZX007), the National Natural Science Foundation of China (91846101, 81771938, 81301296, 81900665, 81570667, 81470948, 81670633), Major Research Plan of the National Natural Science Foundation of China (91742204), the International (Regional) Cooperation and Exchange Projects (NSFC-DFG, 81761138041), Beijing Nova Program Interdisciplinary Cooperation Project (Z191100001119008), the National Key Research and Development Program of the Ministry of Science and Technology of China (2016YFC1305405, 2019YFC2005000, 2018YFC1314003-1, 2015BAI12B07, 2016YFC0906103), the University of Michigan Health System–Peking University Health Science Center Joint Institute for Translational and Clinical Research (BMU20160466, BMU2018JI012, BMU2019JI005), Beijing Advanced Discipline Construction Project (BMU2019GJJXK001), Peking University–Baidu Fund (2019BD017) and Peking University (BMU2018MX020, PKU2017LCX05).
CONFLICT OF INTEREST STATEMENT
None of the authors declare any conflicts of interest.
REFERENCES
- 1. Guan WJ, Ni ZY, Hu Y. et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhou F, Yu T, Du R. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang D, Hu B, Hu C. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cheng Y, Luo R, Wang K. et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int 2020; 97: 829–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arentz M, Yim E, Klaff L. et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020; 323: 1612–1614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hirsch JS, Ng JH, Ross DW. et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int 2020; 98: 209–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yang X Yu Y Xu J et al. . Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen T, Wu D, Chen H. et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020; 368: m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li Z, Wu M, Yao J. et al. Caution on kidney dysfunctions of COVID-19 patients. medRxiv 2020; 10.1101/2020.02.08.20021212 [DOI]
- 10. Naicker S, Yang CW, Hwang SJ. et al. The novel coronavirus 2019 epidemic and kidneys. Kidney Int 2020; 97: 824–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ronco C, Reis T.. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat Rev Nephrol 2020; 16: 308–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bhatia M, Moochhala S.. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J Pathol 2004; 202: 145–156 [DOI] [PubMed] [Google Scholar]
- 13. Mohamed MMB, Lukitsch I, Torres-Ortiz AE. et al. Acute kidney injury associated with coronavirus disease 2019 in urban New Orleans. Kidney360 2020; 1: 614–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li H, Liu L, Zhang D. et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet 2020; 395: 1517–1520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Merad M, Martin JC.. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol 2020; 20: 355–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Su H, Yang M, Wan C. et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int 2020; 98: 219–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Batlle D, Soler MJ, Sparks MA. et al. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J Am Soc Nephrol 2020; 31: 1380–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Polak SB, Van Gool IC, Cohen D. et al. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Mod Pathol 2020; 33: 2128–2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Farkash EA, Wilson AM, Jentzen JM.. Ultrastructural evidence for direct renal infection with SARS-CoV-2. J Am Soc Nephrol 2020; 31: 1683–1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Calomeni E, Satoskar A, Ayoub I. et al. Multivesicular bodies mimicking SARS-CoV-2 in patients without COVID-19. Kidney Int 2020; 98: 233–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kudose S, Batal I, Santoriello D. et al. Kidney biopsy findings in patients with COVID-19. J Am Soc Nephrol 2020; 31: 1959–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sharma P, Uppal NN, Wanchoo R. et al. COVID-19-associated kidney injury: a case series of kidney biopsy findings. J Am Soc Nephrol 2020; 31: 1948–1958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu H, Larsen CP, Hernandez-Arroyo CF. et al. AKI and collapsing glomerulopathy associated with COVID-19 and APOL 1 high-risk genotype. J Am Soc Nephrol 2020; 31: 1688–1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roufosse C, Curtis E, Moran L. et al. Electron microscopic investigations in COVID-19: not all crowns are coronas. Kidney Int 2020; 98: 505–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Goldsmith CS, Miller SE, Martines RB. et al. Electron microscopy of SARS-CoV-2: a challenging task. Lancet 2020; 395: e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Puelles VG, Lutgehetmann M, Lindenmeyer MT. et al. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med 2020; 383: 590–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Braun F, Lutgehetmann M, Pfefferle S. et al. SARS-CoV-2 renal tropism associates with acute kidney injury. Lancet 2020; 396: 597–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Health Commission. Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7) Beijing, China: National Health Commission, 2020
- 29. et al. Kidney Disease: Improving Global Outcomes Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2012; 2: 1–138 [Google Scholar]
- 30. Yang L, Xing G, Wang L. et al. Acute kidney injury in China: a cross-sectional survey. Lancet 2015; 386: 1465–1471 [DOI] [PubMed] [Google Scholar]
- 31. Ronco C, Bellomo R, Kellum JA.. Acute kidney injury. Lancet 2019; 394: 1949–1964 [DOI] [PubMed] [Google Scholar]
- 32. James MT, Levey AS, Tonelli M. et al. Incidence and prognosis of acute kidney diseases and disorders using an integrated approach to laboratory measurements in a universal health care system. JAMA 2019; 2: e191795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang L, Zhao MH, Zuo L. et al. China Kidney Disease Network (CK-NET) 2015 annual data report. Kidney Int Suppl 2019; 9: e1–e81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ng'andu NH. An empirical comparison of statistical tests for assessing the proportional hazards assumption of Cox's model. Stat Med 1997; 16: 611–626 [DOI] [PubMed] [Google Scholar]
- 35. Chen YT, Shao SC, Hsu CK. et al. Incidence of acute kidney injury in COVID-19 infection: a systematic review and meta-analysis. Crit Care 2020; 24: 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Akram AR, Singanayagam A, Choudhury G. et al. Incidence and prognostic implications of acute kidney injury on admission in patients with community-acquired pneumonia. Chest 2010; 138: 825–832 [DOI] [PubMed] [Google Scholar]
- 37. Chu KH, Tsang WK, Tang CS. et al. Acute renal impairment in coronavirus-associated severe acute respiratory syndrome. Kidney Int 2005; 67: 698–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chan L, Chaudhary K, Saha A. et al. AKI in hospitalized patients with COVID-19. J Am Soc Nephrol 2020; 31: 2145–2157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Huang KJ, Su IJ, Theron M. et al. An interferon-γ-related cytokine storm in SARS patients. J Med Virol 2005; 75: 185–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kong SL, Chui P, Lim B. et al. Elucidating the molecular physiopathology of acute respiratory distress syndrome in severe acute respiratory syndrome patients. Virus Res 2009; 145: 260–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Domenech P, Perez T, Saldarini A. et al. Kidney-lung pathophysiological crosstalk: its characteristics and importance. Int Urol Nephrol 2017; 49: 1211–1215 [DOI] [PubMed] [Google Scholar]
- 42. Xu X, Han M, Li T. et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA 2020; 117: 10970–10975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gupta A, Madhavan MV, Sehgal K. et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020; 26: 1017–1032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Werion A, Belkhir L, Perrot M, et al. SARS-CoV-2 causes a specific dysfunction of the kidney proximal tubule. Kidney Int 2020; 98: 1296–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kissling S, Rotman S, Gerber C. et al. Collapsing glomerulopathy in a COVID-19 patient. Kidney Int 2020; 98: 228–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Friedman DJ, Pollak MR. APOL1 and kidney disease: from genetics to biology. Annu Rev Physiol 2020; 82: 323–342 [DOI] [PubMed] [Google Scholar]
- 47. Ali H, Daoud A, Mohamed MM. et al. Survival rate in acute kidney injury superimposed COVID-19 patients: a systematic review and meta-analysis. Ren Fail 2020; 42: 393–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


