Abstract
Background
Recent evidence points to the relevance of poverty and inequality as factors affecting the spread and mortality of the COVID-19 pandemic in Latin America. This study aimed to determine whether COVID-19 patients living in Mexican municipalities with high levels of poverty have a lower survival compared with those living in municipalities with low levels.
Methods
Retrospective cohort study. Secondary data was used to define the exposure (multidimensional poverty level) and outcome (survival time) among patients diagnosed with COVID-19 between 27 February and 1 July 2020. Crude and adjusted hazard ratios (HR) from Cox regression were computed.
Results
Nearly 250 000 COVID-19 patients were included. Mortality was 12.3% reaching 59.3% in patients with ≥1 comorbidities. Multivariate survival analyses revealed that individuals living in municipalities with extreme poverty had 9% higher risk of dying at any given time proportionally to those living in municipalities classified as not poor (HR 1.09; 95% CI 1.06–1.12). The survival gap widened with the follow-up time up to the third to fourth weeks after diagnosis.
Conclusion
Evidence suggests that the poorest population groups have a lower survival from COVID-19. Thus, combating extreme poverty should be a central preventive strategy.
Keywords: COVID-19, Mexico, mortality, pandemic, poverty, survival analysis
Introduction
In December 2019, a group of patients with pneumonia of unknown etiology was detected in Wuhan, China, and on 7 January 2020, a new coronavirus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified as the cause. The World Health Organization (WHO) named this illness COVID-19.1–3
The infection spread rapidly throughout the world, and on March 11 the WHO declared the global pandemic.2 The first imported case in Mexico was described on February 28, but local transmission began on March 24.4 A month later, there were 12 872 diagnosed cases and 1221 reported fatalities in Mexico, from the nearly 12.6 million cases and 182 000 deaths worldwide.2,5 By early October, Latin America and the Caribbean (LAC) had seen almost 10 million cases and more than 350 000 fatalities (34% of all deaths in the world), becoming one of the most affected regions,6 with Brazil and Mexico occupying the second and fourth places, in terms of number of deaths with nearly 150 000 and 82 000, respectively.7
Cases and fatalities in the region continue to grow due to various factors, including the limited impact of the mitigation strategies deployed, the high prevalence of chronic conditions associated with the susceptibility to acquire and develop a symptomatic and severe infection (e.g. obesity, diabetes and hypertension), the poorly developed public health systems and the structural poverty and inequality that affects large segments of the population. In fact, widespread poverty and inequality have fueled the pandemic and are likely to worsen in the near future as a result of its economic impact.8–11
The relationship between socioeconomic status and morbidity and mortality has been established for many health conditions,12–14 including non-communicable (NCDs) and infectious diseases.15–17 In fact, 85% of all premature deaths from NCDs occur in low- and middle-income countries (LMICs); the United Nations Development Program reported that the probability of dying from NCDs in people aged 30–69 years was 60% for LMICs, compared with 10% for developed countries.18 There is also evidence of differences for infectious respiratory diseases by socioeconomic status and poverty level. One study investigating the relationship between poverty and flu showed that flu vaccines were less available to people living in the poorest counties compared with residents of wealthier areas in the USA.19
Recent studies have also looked at how COVID-19 has affected population groups differentially by socioeconomic and ethnic background. For instance, a study with the Navajo Indians in the Southwest of the USA reported a mortality rate of 57 per 100 000 already in mid-May.20 There are also reports of higher hospitalization and death rates from COVID-19 in African-Americans and among individuals of lower socioeconomic status living in poverty.21
Recent published evidence points to the relevance of poverty and inequality as factors affecting the spread of the COVID-19 pandemic and the mortality rates observed in the LAC region; one study evaluating the spread of SARS-CoV-2 in various cities of this region suggested that income inequality and poverty levels were related positively and negatively, respectively.9 Another relevant study looking at the evolution of the pandemic in LAC during the first 90 days showed that the proportion of the population living on less than 1 USD per day was associated with a higher crude mortality rate, with Mexico leading the highest increase (16.2%).22
In this context, we conducted a secondary data analysis to determine whether COVID-19 patients living in municipalities with high levels of poverty have a lower chance of survival compared with those living in municipalities with low levels of poverty.
Methods
Study design
Retrospective cohort study. Secondary data was used to define the exposure (poverty level) and outcome (survival time) among patients diagnosed with COVID-19 in Mexico between 27 February to 1 July 2020. Diagnosis was made using the WHO definition,23 based on a positive polymerase chain reaction (PCR) test24 with samples processed at the National Network of Epidemiological Surveillance Laboratories.
Study population and eligibility
It comprised 231 772 individuals diagnosed with COVID-19 during the study period. These were patients attended at any public or private health facility, whose clinical records were registered electronically by the General Directorate of Epidemiology of the Ministry of Health of Mexico.
All patients diagnosed with COVID-19 regardless of age, sex, comorbidities and municipality of residence were eligible. Individuals with unknown municipality were excluded from the analyses, since poverty level (i.e. exposure) was based on the classification of the municipality.
Data sources
Data from two open electronic sources administered by governmental agencies was extracted:
1) Open Data from the General Directorate of Epidemiology of the Mexican Ministry of Health (www.gob.mx/salud/documentos/datos-abiertos-152127): Clinical and demographic data were extracted from the dataset including type of patient (hospitalized or ambulatory), date of onset of symptoms, diagnosis and admission, presence of comorbidities, occurrence of complications such as pneumonia, need for intensive care or mechanical ventilation, final outcome (survival or death), municipality of residence, age, sex and ethnicity (indigenous versus non-indigenous).
2) Open data from the National Council for the Evaluation of Social Policy (CONEVAL) (www.coneval.org.mx/Medicion/Paginas/AE_pobreza_municipal.aspx): This dataset was used to extract data about the poverty level of all municipalities in the country in 2015. The proportion of poverty observed in each municipality was categorized as extremely poor, poor and not poor.
Poverty data, namely, the proportion of poor and extremely poor populations living in each municipality, was assigned to the municipality of residence for each individual diagnosed with COVID-19. This was possible because both datasets used the same system to code the municipalities. In this way, the aggregated value of a municipality was allocated to each individual living within that municipality.
Exposure
Multidimensional (i.e. economic well-being, social deprivation and territorial context) poverty and extreme poverty were defined using the CONEVAL criteria.25 A detailed description of the methodology used can be read elsewhere.26 In summary, poverty was defined when individuals lack of at least one of the following: An adequate educational development (I), access to health services (II), access to social security (III), access to food (IV), a household of sufficient size and quality (V) with access to basic services (VI), and when the individual has insufficient income to buy the goods and services required to satisfy feeding and non-feeding needs. Extreme poverty was defined when the individual lacks of three or more of the aforementioned items, and when the income is insufficient to even cover feeding needs.
Statistical analysis
Nominal data was reported using frequencies and proportions. Crude odds ratios (OR) with 95% confidence intervals (95% CI) was used for bivariate analysis. For the main analyses crude and adjusted hazard ratios (HR) with 95% CI from Cox regression were computed. Poverty level was used as the main independent variable, and survival time (i.e. time from the onset of symptoms to the outcome: survive or death) as the outcome variable. Observations with inconsistent dates (n = 61) and poverty levels (n = 4554) were excluded from the analysis. The adjusted model included sex, age and comorbidities. Comorbidities included chronic medical conditions such as obesity, diabetes, asthma, immunosuppression, hypertension, cardiovascular disease and renal failure and were included in the model as a categorical variable (one, two, three, four or more). Kaplan–Meier curves were used to graphically depict survival differences by poverty level. All data were processed and analyzed using the SPSS v.25 (IBM, USA).
Results
By 1 July 2020, 231 772 individuals infected with SARS-CoV-2 were admitted to health facilities in Mexico. Most patients were men (54.6%), 61.3% were ≥40 years old, 35.6% had a poverty level >40% and 30.1% extreme poverty level >4%. Indigenous speakers accounted for 1.1% of the sample (Table 1).
Table 1.
Basic sociodemographic characteristics of COVID-19 patients in Mexico diagnosed between 27 February and 1 July 2020
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Sex | Female | 105 223 | 45.4 |
| Male | 126 549 | 54.6 | |
| Age group in years | 0–19 | 7265 | 3.1 |
| 20–39 | 82 232 | 35.5 | |
| 40–59 | 95 548 | 41.2 | |
| 60–79 | 40 631 | 17.5 | |
| ≥80 | 6096 | 2.6 | |
| Ethnicitya | Indigenous | 2547 | 1.1 |
| Non-indigenous | 229 225 | 98.9 | |
| Poverty in municipality (%)b | 0–20 | 24 736 | 10.7 |
| 20.1–40 | 124 585 | 53.8 | |
| 40.1–60 | 59 381 | 25.6 | |
| >60 | 23 070 | 10.0 | |
| Extreme poverty in municipality (%)b | 0–2 | 97 461 | 42.1 |
| 2.1–4 | 64 635 | 27.9 | |
| 4.1–6 | 20 478 | 8.8 | |
| 6.1–8 | 11 262 | 4.9 | |
| >8 | 37 936 | 16.4 | |
| Total | 231 770 | 100 |
aSpeaks an indigenous language.
bDefined based on the National Council for the Evaluation of Social Policy (CONEVAL) (25).
Most patients received ambulatory care (69.3%), but 30.7% had to be hospitalized. Hypertension was the most common comorbidity (20.1%) followed by obesity (19.5%) and diabetes (16.4%). One out of four patients (23.8%) developed pneumonia, 9.7% had to be intubated and 8.6% were admitted for intensive care. Mortality was 12.3%, reaching 59.3% among those with ≥1 comorbidities. Nearly 95% of patients received care in public facilities, including social security institutions (42.3%); only 3% received care in a private facility (Table 2).
Table 2.
Clinical characteristics of COVID-19 patients in Mexico diagnosed between 27 February and 1 July 2020
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Type of patient | Ambulatory | 160 541 | 69.3 |
| Hospitalized | 71 231 | 30.7 | |
| Comorbidities | Hypertension | 46 526 | 20.1 |
| Obesity | 45 160 | 19.5 | |
| Diabetes | 37 993 | 16.4 | |
| Smoking | 17 848 | 7.7 | |
| Asthma | 6352 | 2.7 | |
| Cardiovascular | 5381 | 2.3 | |
| Chronic kidney disease | 5019 | 2.2 | |
| Chronic obstructive pulmonary disease | 4016 | 1.7 | |
| Complications | Pneumonia | 55 085 | 23.8 |
| Intubation | 6898 | 9.7 | |
| Intensive care | 6092 | 8.6 | |
| Deaths | Overall | 28 510 | 12.3 |
| With ≥1 comorbidity | 16 954 | 59.5 | |
| Health sector | Public, ministry of health | 123 165 | 53.1 |
| Public, social security institutionsa | 98 157 | 42.3 | |
| Private | 6858 | 3.0 | |
| Other and unspecified | 3590 | 1.6 | |
| Total | 231 770 | 100 |
aIt includes the Mexican Institute of Social Security (IMSS), the Institute of Security and Social Services for Federal Workers (ISSSTE), health services for workers of the public oil company (PEMEX) and the Ministry of Defense (SEMAR and SEDENA) and State Health Services.
Statistically significant increased crude ORs were observed for all six variables studied for both, poverty (>40%) and extreme poverty (>4%) in the municipality where patients lived. The probability of developing pneumonia and being hospitalized showed the largest odds for both levels of poverty, but especially for extreme poverty with 1.34 (95% CI 1.32–1.37) and 1.29 (95% CI 1.26–1.31), respectively (Table 3).
Table 3.
Odds ratios (OR) with 95% confidence intervals (CI) from bivariate analyses for factors potentially associated with the levels of poverty and extreme poverty of the municipality where the COVID-19 patients live between 27 February and 1 July 2002, in Mexico
| Variables | Percent | N (%) | OR (95% CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Level of poverty in the municipality where patients lived | ||||
| Comorbidity (at least one) | 0–40 | 67 711 (45.3) | 81 610 (54.7) | 1.00 |
| >40 | 37 977 (46.1) | 44 474 (53.9) | 1.03 (1.01–1.05) | |
| Developed pneumonia | 0–40 | 33 135 (22.2) | 116 186 (77.8) | 1.00 |
| >40 | 21 950 (26.6) | 60 501 (73.4) | 1.27 (1.25–1.30) | |
| Patient was hospitalized | 0–40 | 43 884 (29.4) | 105 437 (70.6) | 1.00 |
| >40 | 27 347 (33.2) | 55 104 (66.8) | 1.19 (1.17–1.21) | |
| Patient was intubated | 0–40 | 4102 (9.3) | 39 782 (90.7) | 1.00 |
| >40 | 2796 (10.2) | 24 551 (89.8) | 1.10 (1.05–1.16) | |
| Patient was in intensive care unit | 0–40 | 3583 (8.2) | 40 301 (91.8) | 1.00 |
| >40 | 2509 (9.2) | 24 838 (90.8) | 1.13 (1.08–1.20) | |
| Patient died | 0–40 | 18 035 (12.1) | 131 286 (87.9) | 1.00 |
| >40 | 10 475 (12.7) | 71 976 (87.3) | 1.06 (1.03–1.09) | |
| Level of extreme poverty in the municipality where patients lived | ||||
| Comorbidity (at least one) | 0.1–4 | 32 289 (46.3) | 37 387 (53.7) | 1.04 (1.02–1.06) |
| >4 | 73 399 (45.3) | 88 697 (54.7) | 1.00 | |
| Developed pneumonia | 0.1–4 | 19 250 (27.6) | 50 426 (72.4) | 1.34 (1.32–1.37) |
| >4 | 35 835 (22.1) | 126 261 (77.9) | 1.00 | |
| Patient was hospitalized | 0.1–4 | 24 068 (34.5) | 45 608 (65.5) | 1.29 (1.26–1.31) |
| >4 | 47 163 (29.1) | 114 933 (70.9) | 1.00 | |
| Patient was intubated | 0.1–4 | 2406 (10.0) | 21 662 (90.0) | 1.05 (1.00–1.11) |
| >4 | 4492 (9.5) | 42 671 (90.5) | 1.00 | |
| Patient was in intensive care unit | 0.1–4 | 2138 (8.9) | 21 930 (91.1) | 1.06 (1.01–1.13) |
| >4 | 3954 (8.4) | 43 209 (91.6) | 1.00 | |
| Patient died | 0.1–4 | 9181 (13.2) | 60 495 (86.8) | 1.12 (1.09–1.15) |
| >4 | 19 329 (11.9) | 14 2767 (88.1) | 1.00 | |
Table 4 presents crude and adjusted HRs with 95% CI from Cox regression for the survival of patients diagnosed with COVID-19 during the study period adjusted for sex, age in years and number of comorbidities. Extreme poverty, but not poverty, was associated with a statistically significant adjusted HR (1.09; 1.06–1.12).
Table 4.
Crude and adjusted hazard ratios (HR) with 95% confidence intervals (CI) from Cox regression for the survival of patients diagnosed with COVID-19 (n = 227 132a) in Mexico between 26 February and 1 July 2020
| Variable | Category | HR (95% CI) | |
|---|---|---|---|
| Crude | Adjusted | ||
| Poverty levelb | No poverty | 1.00 | 1.00 |
| Poverty | 0.99 (0.95–1.04) | 0.98 (0.94–1.03) | |
| Extreme poverty | 1.13 (1.10–1.16) | 1.09 (1.06–1.12) | |
| Sex | Female | 1.00 | 1.00 |
| Male | 1.30 (1.27–1.33) | 1.25 (1.22–1.28) | |
| Age | Years | 1.03 (1.03–1.03) | 1.03 (1.03–1.03) |
| Comorbiditiesc | None | 1.00 | 1.00 |
| One | 1.48 (1.44–1.52) | 1.19 (1.16–1.23) | |
| Two | 2.14 (2.07–2.21) | 1.43 (1.39–1.48) | |
| Three | 2.57 (2.46–2.69) | 1.57 (1.50–1.65) | |
| Four or more | 3.05 (2.84–3.27) | 1.72 (1.60–1.84) | |
aObservations with inconsistent dates (n = 61) and poverty levels (n = 4554) were excluded from the analysis.
bDefined by the patient’s municipality of residence using CONEVAL data (25).
cIt includes obesity, smoking, hypertension, diabetes, asthma, cardiovascular disease, renal disease, immunosuppression and COPD, among others.
Figure 1 displays Kaplan–Meier curves. While virtually no difference in cumulative survival was observed between patients living in poor and non-poor municipalities, those living in municipalities with extreme poverty clearly showed a lower survival.
Fig. 1.
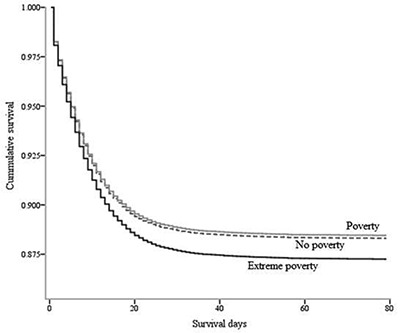
Survival curves for patients diagnosed with COVID-19 between 26 February and 1 July 2020, by poverty levels in Mexico (n = 227 132).
Discussion
Main finding of this study
This study was conducted to determine whether patients diagnosed with COVID-19 living in Mexican municipalities with high levels of poverty and extreme poverty had a lower chance of survival during the first 3 months of the pandemic. Multivariate regression survival analyses revealed that extreme poverty was associated with decreased survival, namely, that individuals living in municipalities with extreme poverty have a 9% higher risk of dying at any given time proportionally to those living in municipalities classified as not poor (HR 1.09; 95% CI 1.06–1.12). Results also showed that the survival gap widened as the follow-up time increased up to the third or fourth week after diagnosis.
These findings relate to the principles of the ‘Theory of Fundamental Causes’ applied to the analysis of gradients of inequality in mortality.27 This theory assumes that social differences in mortality levels had been constant throughout time but that new economic factors have caused the relatively recent differences observed, having an independent (after adjusting for other risk factors) and sustained effect over time, namely, that such effect remains in spite of changes in disease mechanisms (e.g. preventive measures, health treatments, use of medical technology, etc.).
For instance, a longitudinal study conducted in 20 European countries showed that mortality rates increased between 1980 and 2010, and that the poorest social segments of the population were the most vulnerable, even in places offering extensive facilities for preventive interventions.28
What is already known on this topic
The results are consistent with those of three specific studies that analyzed combined epidemiological and socio-spatial data to investigate the association between poverty and mortality from COVID-19 in the USA and Brazil under the theoretical approach of Social Vulnerability and Social Determinants of Health. The first, conducted in the USA, examined the relationship between the county poverty level and the mortality rate during the first weeks of the pandemic finding that deaths increased over time in those counties with more poverty and extreme poverty.29 The second study produced a predictive model for the risk of mortality from COVID-19 in poor and highly segregated African-American communities in the city of Chicago;30 the results showed significant correlations for four covariates (areas with the highest proportion of African-American residents, highest social vulnerability, highest exposure to risk factors and high mortality rates). The third, done in an urban municipality in northeastern Brazil, showed that poorer neighborhoods had lower COVID-19 records, but higher mortality rates compared with neighborhoods with lower poverty levels; the authors suggested that poor living conditions contributed to the spread of the infection and led to the higher mortality in vulnerable populations.31
On the other hand, one study with data from 40 European countries found no correlation between variables measuring socioeconomic vulnerability (e.g. Gini indices of social inequality and poverty rates) and differentials in mortality rates by COVID-19; the adjusted linear regression model showed that the speed for the implementation of response strategies to the outbreak was the main predictor of mortality.32
What this study adds
The preceding studies analyzed the cross-sectional association between levels of poverty and the presence of the mortality event, or mortality incidence rates. Our study adds, as a novelty, the analysis of the association between poverty and survival time in a cohort diagnosed with COVID-19.
Evidence shows that the poorest population groups have a lower survival from COVID-19. This suggest that the relationship between poverty and survival risk is not linear, as previously reported in a longitudinal study from the USA whereby levels of urban poverty and the risk of mortality were documented only when poverty levels exceeded the threshold of 20%.33
The results also replicate findings published in the international literature on COVID-19, including the effect of comorbidities, older age and sex (i.e. being male), as risk factors for higher mortality, 34,35 but now reflected in survival rates.
Limitations of this study
Some strengths and limitations ought to be mentioned for a fair interpretation of the results. The main limitation relates to the allocation of aggregated values of poverty to individuals based on the place of residence, which can lead to an ecological fallacy; misclassification could be a real threat to internal validity, as there can be no certainty that individuals living in poor or extremely poor municipalities were indeed poor themselves, and also those living in the other municipalities could actually be extremely poor. On the other hand, major strengths relate to the large sample comprising the full COVID-19 mortality from a large country such as Mexico, the uniform definitions and procedures used to collect and record data, the standard coding of municipalities that allowed merging data from the two registers used and the use of a multidimensional instrument to measure poverty and extreme poverty. The findings of the present study could be complemented with a qualitative research that investigates the effect of cultural meanings and beliefs on risk and protection practices against COVID-19 in municipalities of extreme poverty.
In conclusion, the results show that individuals who lived in municipalities with a large proportion of extreme poverty who were diagnosed with COVID-19 and sought medical care during the first 3 months of the pandemic in Mexico had a lower survival compared with those living in all other municipalities. This could impact several health and socioeconomic indicators resulting in a vicious cycle of more poverty and extreme poverty.36 Thus, combating extreme poverty should be a central preventive strategy.
Regrettably, in spite of international community awareness and formal willingness to tackle this problem, reducing extreme poverty continues to be a relatively neglected issue. In fact, during the last three decades, poverty in the world has only been reduced slightly, to a large extent due to poor redistribution policies.37 Efforts should persist to continue trying to tackle extreme poverty through structural and systematic efforts based on a better and fairer distribution of the income and wealth.
Authors’ contribution
ROM-G conceived and the research protocol. R.C.-H. conceived and designed the research protocol, downloaded the datasets from the open sources, built the merged database, and performed the univariate and bivariate analyses. He performed the univariate and bivariate analyses of the data. J.M.-E. built the merged database, produced the survival curves, and carried out the Cox regression analyses. All the authors wrote the first version of the manuscript, contributed to its improvement, and approved the final version.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
No conflict of interest has been declared by the author(s).
Acknowledgements
None.
Rebeca Olivia Millán-Guerrero, Researcher and Proffesor
Ramiro Caballero-Hoyos, Associate Researcher
Joel Monárrez-Espino, Researcher and Proffesor
Contributor Information
Rebeca Olivia Millán-Guerrero, Faculty of Medicine, University of Colima, Colima, Col, 28040, Mexico.
Ramiro Caballero-Hoyos, Clinical Epidemiology Research Unit, Mexican Institute of Social Security, Colima, Col, 28000, Mexico.
Joel Monárrez-Espino, Health Sciences Division, University of Monterrey, Monterrey, N.L., 66238, Mexico; Public Health Research Group, Claustro Universitario, Chihuahua, Chih., 31320, Mexico.
References
- 1. Wang D, Hu B, Hu C et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus- infected pneumonia in Wuhan, China. JAMA 2020;323:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization Situation Reports. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 3. Koo JK, Cook AR, Park M et al. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis 2020;20:678–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dirección General de Epidemiología Aviso Epidemiológico Enfermedad COVID-19 por SARS-CoV-2 (Actualización). Available from: https://www.gob.mx/salud/documentos/aviso-epidemiologico-enfermedad-covid-19-por-sars-cov-2-actualizacion.
- 5. Unidad de Inteligencia Epidemiológica y Sanitaria Comunicado Técnico Diario COVID-19. Available from: https://www.gob.mx/cms/uploads/attachment/file/548251/Comunicado_Tecnico_Diario_COVID-19_2020.04.24.pdf.
- 6. Dyer O. Covid-19 hot spots appear across Latin America. BMJ 2020;369:m2182. [DOI] [PubMed] [Google Scholar]
- 7. Johns Hopkins University Coronavirus Resource Center. Global Map. Available from: https://coronavirus.jhu.edu/map.html.
- 8. Pablos-Méndez A, Vega J, Aranguren FP et al. Covid-19 in Latin America. Responses are complicated by poverty, comorbidity, and political dynamics. BMJ 2020;370:m2939. [DOI] [PubMed] [Google Scholar]
- 9. Bolaño-Ortiz TR, Camargo-Caicedo Y, Puliafito SE et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: a look from its economic conditions, climate and air pollution indicators. Environ Res 2020;191:109938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pereira M, Oliveira AM. Poverty and food insecurity may increase as the threat of COVID-19 spreads. Public Health Nutr 2020;1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abedi V, Olulana O, Avula V et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities 2020;1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yu T, Wei Z, Xu T et al. The association between the socioeconomic status and body pain: a nationwide survey. Medicine 2020;99(12):e19454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Salgado-Barreira Á, Estany-Gestal A, Figueiras A. Efecto del nivel socioeconómico sobre la mortalidad en áreas urbanas: revisión crítica y sistemática. Cad Saude Publica 2014;30(8):1609–21. [DOI] [PubMed] [Google Scholar]
- 14. Wang S, Zhai H, Wei L et al. Socioeconomic status predicts the risk of stroke death: a systematic review and meta-analysis. Prev Med Rep 2020;19:101124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. World Health Organization The Global Report for Research for Infectious Diseases of Poverty. 2012. Available from: https://apps.who.int/iris/bitstream/handle/10665/44850/9789241564489_eng.pdf?sequence=1.
- 16. Williams J, Allen L, Wickramasinghe K et al. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J Glob Health 2018;8(2):020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Allen L, Williams J, Townsend N et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health 2017;5(3):e277–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization Guidance Note on the Integration of Non-communicable Diseases into the United Nations Development Assistance Framework. Available from: https://www.who.int/nmh/ncd-task-force/guidance-note.pdf.
- 19. Lee BY, Brown ST, Bailey RR et al. The benefits to all of ensuring equal and timely access to influenza vaccines in poor communities. Health Aff 2011;30(6):1141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shaw G. Neurologists on the front lines: the burden of COVID-19 on native American communities. Neurology Today 2020;20(11):16–7. [Google Scholar]
- 21. Alsan M, Stantcheva S, Yang D et al. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw Open 2020;3(6):e2012403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Acosta LD. Capacidad de respuesta frente a la pandemia de COVID-19 en América Latina y el Caribe. Rev Panam Salud Publica 2020;44:e109. doi: 10.26633/RPSP.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. World Health Organization Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (2019-nCoV) Infection is suspected: interim Guidance. Available from: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf.
- 24. Sharfstein JM, Becker SJ, Mello MM. Diagnostic testing for the novel coronavirus. JAMA 2020;323(15):1437–8. [DOI] [PubMed] [Google Scholar]
- 25. Consejo Nacional de Evaluación de la Política de Desarrollo Social Informes de Pobreza y Evaluación 2020. Available from: https://www.coneval.org.mx/.../Informes_Pobreza_Evaluacion_2020.aspx.
- 26. Consejo Nacional de Evaluación de la Política de Desarrollo Social Metodología para la medición de la pobreza en los municipios de México, 2015. Available from: https://www.coneval.org.mx/Medicion/Documents/Pobreza_municipal/Metodologia_municipal_2015.pdf.
- 27. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav 2010;51(Suppl):S28–40. [DOI] [PubMed] [Google Scholar]
- 28. Mackenbach JP, Looman C, Artnik B et al. ‘Fundamental causes’ of inequalities in mortality: an empirical test of the theory in 20 European populations. Sociol Health Illn 2017;39(7):1117–33. [DOI] [PubMed] [Google Scholar]
- 29. Finch WH, Hernández-Finch ME. Poverty and Covid-19: rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Front Sociol 2020;5:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kim SJ, Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ Behav 2020;47(4):509–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Martins-Filho PR, Souza-Araújo AA, Quintans-Júnior LJ et al. COVID-19 fatality rates related to social inequality in Northeast Brazil: a neighborhood-level analysis. J Travel Med 2020;taa128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fountoulakis KN, Fountoulakis NK, Koupidis SK et al. Factors determining different death rates because of the COVID-19 outbreak among countries. J Public Health 2020;fdaa119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Do DP, Wang L, Elliott MR. Investigating the relationship between neighborhood poverty and mortality risk: a marginal structural modeling approach. Soc Sci Med 2013;91:58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020;8(7):659–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mallapaty S. The coronavirus is most deadly if you are old and male. Nature 2020;586:16–7. Available at https://www.nature.com/articles/d41586-020-02483-2. [DOI] [PubMed] [Google Scholar]
- 36. Ahmed F, Ahmed N, Pissarides C et al. Why inequality could spread COVID-19. Lancet Public Health 2020;5(5):e240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Alston P. The parlous state of poverty eradication Report of the Special Rapporteur on extreme poverty and human rights. Human Rights Council; Forty-fourth sessions 15 June–3 July 2020. Available from: https://www.ohchr.org/EN/Issues/Poverty/Pages/parlous.aspx. [Google Scholar]


