Abstract
The growing number of cancer survivors and the high prevalence of cancer-related physical and psychosocial effects pose important and pressing challenges to health systems. The coronavirus disease 2019 (COVID-19) pandemic has led to further stressors on cancer survivors and health care systems. As the pandemic continues to have substantial impact on the world, it is critical to focus attention on the health care needs of cancer survivors. In this commentary, we propose an adoption of essential steps that should be part of a continuous adaptive approach to promote effective cancer survivorship care during ongoing COVID-19 waves and beyond.
Over 17 million individuals in North America (1) and millions more around the world (2,3) are living with a personal history of cancer. Before coronavirus disease 2019 (COVID-19), the growing number of cancer survivors along with the high prevalence of cancer-related side effects posed important and pressing challenges to health care systems. The pandemic has led to further stressors on cancer survivors and health care systems (4-6). Earlier in the pandemic, several editorials were written to highlight the potential effects of COVID-19 on the health and health care of cancer survivors (4,6,7). Although suspected yet unconfirmed at the time, recent studies identified cancer diagnosis as a risk factor for acquiring COVID-19 (8) and for its associated negative outcomes, including morbidity and mortality (9-12). Specifically, people at risk are older, have comorbidities, currently receiving chemotherapy, have lung cancer or hematological malignancies, and have completed therapy within 5 years (11-14). After the initial disruptions and delays in routine cancer treatment and follow-up (9,15,16), strategies were implemented to reduce risk of exposure and minimize in-person visits (15,17) along with the development of pandemic-focused priority care guidelines (18,19). While necessary, the potential negative consequences of these changes in health care delivery are concerning. These concerns were highlighted in a recent editorial by Norman Sharpless, Director of the US National Cancer Institute, in which he noted a substantial decline in screening tests resulting in delayed diagnosis and suboptimal care for people with cancer since the start of the pandemic, which will likely have an impact on cancer mortality (20). Further, a recent article that examined the impact of COVID-19 on cancer care across the globe found 88% of centers faced challenges in providing usual cancer care, and up to 80% of patients in some centers had exposure to potential harm (15). Survivors have also reported negative consequences of COVID-19 on cancer care and follow-up (21,22). Because the duration and course of the pandemic are uncertain, it is crucial that attention be placed on resumption of services along the cancer care continuum when safe and feasible (20,23).
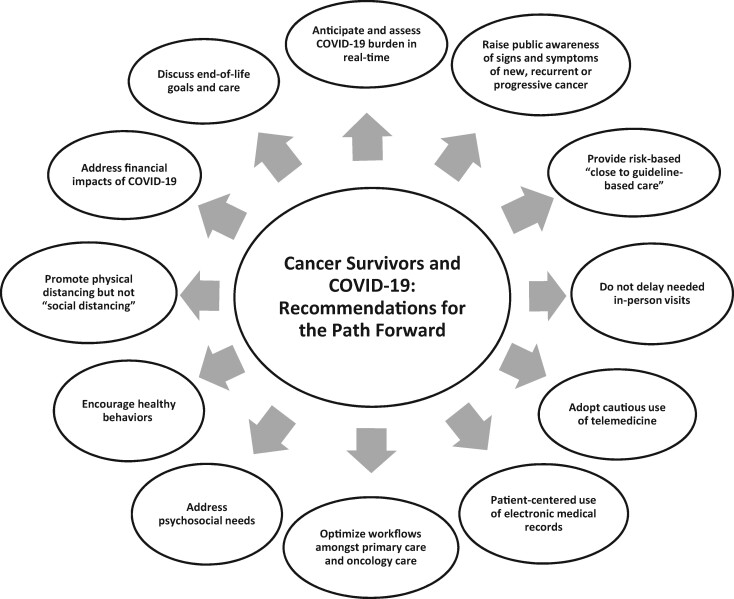
In this commentary, we go beyond the previously published perspectives to propose the adoption of essential steps that should be part of a continuous adaptive approach to find the optimal balance between minimizing the negative impact of the fluctuating COVID‐19 pandemic while promoting effective cancer survivorship care (see Figure 1). Our approach is based on a previously published model for cancer diagnostic services (24).
Figure 1.
Readdressing the needs of cancer survivors: recommendations for the path forward.
Proposed Path Forward
In guiding this commentary, we sought to capture the rapidly evolving evidence and to include perspectives of multiple stakeholders. First, we reviewed numerous sources, including relevant literature and national and international guidance statements (ie, American Society of Clinical Oncology [ASCO], European Society of Medical Oncology, American Society of Therapeutic Radiation Oncology, and Cancer Australia) and advocacy group recommendations (eg, National Coalition of Cancer Survivorship, and American Cancer Society). Second, we drew insights from 2 Twitter chats focused on COVID-19 and its impact on cancer survivors. The first was hosted by Cancer Survivor Social Media (#CSSMchat) on April 15, 2020; the second was hosted on May 16-17, 2020, by the Radiation Oncology Journal Club (#radonc #jc). Both events included participation by the authors, patients and advocates, and colleagues around the globe, and discussions were based around the themes of potential impact on survivors and the need for action to mitigate the impact.
Anticipate and Assess COVID-19 Burden in Real-Time
With the global pandemic marked by ongoing temporal and spatial variation, the development of appropriate policy and health care delivery planning requires projections of possible COVID-19 scenarios at the community, regional, and national levels (25). The use of consistent measurements of objective and comparable data is vital to assess the effectiveness of mitigation strategies and inform ongoing efforts (26). Because the prevalence of COVID-19 is critical in driving decisions, collaboration and sharing of accurate data among health care providers and public health agencies are paramount. This, in turn, results in a risk-based triaging of available resources and an assessment of care capacity for cancer survivors.
Raise Public Awareness of Signs and Symptoms of New, Recurrent, or Progressive Cancer
COVID-19 has led to decreased use of health care services, with priority placed on initial cancer diagnosis and treatment (15). Cancer survivors may have also been fearful of coming into health care settings due to concerns about susceptibility, leaving them to manage physical and practical issues and worries on their own (5,27-29). While there has been recent public messaging advising patients to report unusual symptoms, these have not focused on those with prior cancers. Effective outreach involves collaboration on local, regional, and national levels targeted to both patients and caregivers and must be a priority across the cancer care continuum. Although patient education is an important aspect of delivering quality oncologic care, it is now even more important to educate patients to monitor and report any suspicious symptoms indicative of new, recurrent, or progressive disease. Public health agencies, cancer societies, charitable organizations, and academic centers should develop and disseminate information specifically tailored for those patients with prior cancer.
Provide Risk-Based “Close to Guideline Care”
Posttreatment follow-up care of cancer survivors has dramatically changed as a result of COVID-19, and many surveillance visits and imaging have been delayed or cancelled (5). Although the majority of the guidelines provide specific frequency ranges for surveillance testing (such as every 3-6 months), most are based on consensus rather than evidence. As such, it may be reasonable to delay surveillance during COVID-19 surges based on medical providers’ consideration for individual factors, including disease type and treatment exposures as well as COVID-19 risk factors. Symptom-based monitoring, which may be remote, may offer benefits over routine, “traditional” surveillance (30). It is important that in considering surveillance modifications, medical providers take caution in that some patients might perceive this as lack of standard care and thus experience anxiety. Sensitivity toward and adjustment of surveillance modalities to patient preference may be needed. Patient resources regarding the impact of COVID-19 on cancer care have been developed and can be helpful in preparing patients and their families to understand how the pandemic will affect care provision (ie, European Society of Medical Oncology, ASCO Cancer.Net).
Adopt Cautious Use of Telemedicine
Telemedicine with bidirectional messaging to facilitate self-reported monitoring of cancer patients with COVID-19, including any disease-specific or social concerns (31,32), can play a meaningful role for cancer survivors. Although telemedicine is not new, its accelerated dissemination was precipitated by the pandemic (33), and it is poised to become an important pillar of cancer care (34). However, although secure telemedicine with its incorporation of risk–benefit balance has been a useful and important tool to deliver care since the onset of the pandemic, it is not in itself the solution (35). Efficient and meaningful telemedicine requires training for patients, caregivers, and clinicians as well as having the “right” technology, appropriate infrastructure, and private space for the virtual visits. Impaired hearing and vision, linguistic barriers, cultural limitations, and cognitive deficits in patients pose further challenges necessitating a more personalized virtual approach. Often there are digital inequalities or disparities in both the ability to access and to use telemedicine within local, regional, national, and global populations (36,37). In such cases, alternative routes of communication such as telephone conversation can be potentially helpful. Communication guides that may assist clinicians with oncology-specific language to respond to patient questions about changes in delivery of cancer care during the pandemic are available online (38,39).
There continue to be widespread issues with regulations regarding financial incentives and reimbursement associated with telemedicine. To address this evolving situation, ASCO recently issued an interim position statement on telemedicine in cancer care that included recommendations on federal and state coverage, health equity, patient education, and research (40). With the current crisis posing additional challenges to communities that have traditionally faced barriers to health care access, sole reliance on telemedicine is not advised, and appropriate triaging considering the risk of COVID-19, the urgency of the patient needs, and patient preferences should dictate the route of communication (4). Moving forward, it is important that health care organizations expand beyond the traditional center walls to leverage multidisciplinary community-based care to serve those for whom virtual care is inappropriate or inaccessible (41).
Do Not Delay Needed In-Person Visits
Although remote monitoring using telemedicine may be adopted, when required, physical examination should not be avoided (42). There has been a rapid reorganization of cancer systems to ensure timely and essential cancer care while minimizing risk of exposure to COVID-19 (23). Recent guidance from organizations such as ASCO provides immediate and short-term recommendations that cancer centers and oncology practices can adopt (19). It is important to emphasize that there is no “one size fits all” approach to delivering cancer care during the COVID-19 surges, and individualized treatment decisions must be made. Priority should be given to those whose treatments and testing have been delayed during “shutdown” and driven by benefit vs risk analysis as well as therapeutic intent (43-45). In cases where face-to-face clinical encounters are warranted, safety should be optimized through patient outreach and education. Patients should be given practical advice and instructions to encourage safe behavior when coming in for routine checks or other follow-up care. Health care facilities can promote adaptation to the “new normal” by delivering “care with caution” following standard COVID-19 precautions.
Patient-Centered Use of Electronic Medical Records
Recognizing the challenges of telemedicine, an opportunity to empower patients is provided by availability of real-time online access to electronic records, including encounter notes written by clinicians (referred to as “open notes”) through patient portals (46). Such practice exists in Nordic countries as well as several institutions in the United States and continues to grow worldwide (47-49). Encouragingly, new federal laws in the United States mandate that providers must extend open notes to all patients starting from November 2, 2020 (50). Although there is concern that patients’ access to their oncology notes will trigger anxiety or confusion, research to date suggests that patients find this access to be useful; report improved understanding about their diagnosis, treatment risks, and side effects; and learn important information that they had missed during clinical visits (51-54). Accessibility to open notes has been cited as crucial for patients’ mental well-being (46). For patients with reliable internet access, patient portals can also allow remote communication, education, and scheduling of follow-up appointments and could support the electronic collection of patient-reported outcomes. The value of open notes can be optimized by improving both oncology professionals’ clarity in online documentation and maximizing their use of tooltips as well as patients’ understanding of the benefits and risks of accessing their medical records (50). The use of open notes is highlighted by the pandemic and has the potential to serve patients in the future.
Optimize Workflows Among Primary Care and Oncology Care
Adoption of evidence-based, innovative models of care, including shared follow-up and survivorship care along with streamlined collaborative workflows among primary care and oncology services, was insufficient in the pre-COVID era. The need for such a workflow has been intensified by the pandemic and can facilitate timely evaluation of potential cancer symptoms as well as divert COVID-19 evaluations for cancer patients to nononcologic settings, thus decreasing risk of transmissions among this vulnerable cohort. The fundamental role of primary care may also be well-poised to identify cancer survivors at risk of suboptimal or delayed surveillance due to noncompliance. Further, optimization of primary care with efficient use of triage-based telemedicine or personal interaction may support cancer patient follow-up and assist in sustaining their physical (ie, management of chronic medical conditions) and mental health. To support this, it is important to establish and embed processes and infrastructure that encourage the development and sharing of patient follow-up care plans between multidisciplinary health professionals who are providing survivorship care. Resources and education of multidisciplinary health care providers to support delivery of person-centered and evidence-based models of follow-up and survivorship care are needed (42). Development and use of standardized templates to support care coordination and agreement of alternative follow-up shared care arrangements have been proposed (42). Further, processes to support rapid communication between primary and tertiary care settings for clinical issues requiring cancer specialist consultation or advice need to be established (42).
Address Psychosocial Needs
The United Nations has warned of a global mental health crisis due to COVID-19 (55). Cancer survivors already face uncertainty and are at higher risk of depression and anxiety compared with the general population (56-58). COVID‐19 has likely exacerbated this due to lack of access to screening and recommended care coupled with worry over increased susceptibility to contracting COVID-19 (7,59). Physical distancing protocols, which continue in most areas of the world, have the potential to amplify anxiety, distress, and depression. Additionally, socioeconomic and sociopolitical disparities can further exacerbate psychological morbidity in cancer patients (60-62).
Proactive steps can be taken to address the psychosocial needs of cancer survivors (63). To begin, it is important to validate the anxiety that individuals are feeling; compassion and value-based approaches may be beneficial (64). The next steps involve identifying those who need extra support can be facilitated through simple screening tools (ie, distress thermometer) as well as emerging tools to assess fear related to COVID-19 (65). Moving forward, it is critical that expansion of mental health services is prioritized to increase the capacity to address the challenges caused by the pandemic. The use of triaging and stepped care approaches (66) will require systems that are well designed to screen, identify, and deliver this care. Initiatives such as Helplines (ie, Cancer Support Community Helpline) and peer “check-in” could make a difference in the early stages of social isolation (67). Further, the use of telemedicine and other technology platforms can be vital components of stepped care for acute mental health crisis management as well as nonurgent care and support (63).
Encourage Healthy Behaviors
For many, COVID-19 and the need to self-isolate or quarantine has had a very negative impact on lifestyle behaviors, including physical activity, diet, sleep, and alcohol consumption (68-74). Given the importance of promoting physical and mental health and overall well-being (75), scientific and medical organizations including the World Health Organization have released recommendations to promote physical activity at home during the COVID-19 pandemic. The recovery and quality of life of cancer survivors can be at risk with surges of COVID-19, and cancer survivors may be particularly vulnerable to the impact of the pandemic on lifestyle behaviors. Physical inactivity, sedentary behavior, and poor nutrition are already highly prevalent in cancer survivors both during and after treatment (76) and are associated with chronic medical conditions as well as overall poor physical and mental health and increased mortality risk (77-80). With limited access to gyms and exercise programs along with the need to enact more strict physical distancing measures, participation in healthy behaviors among cancer survivors is likely to further decline. At the same time, social distancing may present an opening to make lifestyle changes because some typical barriers that interfere with an active lifestyle adoption (eg, lack of time, work, traffic) have been removed (81). Clinicians and other health care practitioners should proactively prescribe physical activity to their patients during the pandemic and encourage other healthy strategies such as sleep hygiene and nutrition (7). Verbal coaching, brochures and pamphlets, and effective use of social media platforms can assist with promoting healthy behaviors. Remotely supported home-based exercise programs that integrate safe and simple exercises may be recommended (82). Cancer survivors who are exercise-naïve or who have preexisting health problems and/or exercise contraindications should consult with their primary care provider, oncologist, and/or an exercise professional before starting any new exercise program; initial supervision is recommended for these individuals (83). As with any lifestyle change, cancer survivors should be encouraged to develop small realistic goals that can be progressed over time (84).
Promote Physical Distancing, Not “Social Distancing”
Cancer survivors should be counseled that social interactions are not just acceptable but also beneficial (as long as local health strategies and measures taken to ensure safety are not violated). As with the exercise activities described above, the use of virtual social platforms may be helpful in increasing social interactions in a safe manner (85). Many gyms, places of worship, and social groups such as book clubs have transitioned to online platforms. Workplaces are conducting meetings and creating virtual workspaces for people to connect over video connections. Cancer centers and community cancer support programs have also developed online programs that should be encouraged to help support cancer survivors. Future efforts should be geared towards developing more engaging and intuitive platforms to encourage meaningful social interactions during pandemic waves and beyond.
Address Financial Impacts of COVID-19
Cancer survivors already face hardship associated with financial burdens and are particularly at risk for additional negative financial effects as a result of COVID-19, thus affecting quality of life as well as morbidity and mortality (86-89). Survivors whose employment is deemed “essential” and cannot be conducted from home may have to weigh the benefits of work with potential increased exposure depending on their occupational risks and may be forced into temporary unemployment. For others, their financial situation gives them no option but to continue going to work, potentially resulting in increased risk of COVID-19 transmission and associated distress (41,90). This must be considered in light of the research that shows that gaining new employment after job loss is more difficult for cancer survivors compared with the general healthy population (91). Those individuals who are self-employed or work for small employers may also face unique short- and long-term uncertainties. Being able to work has been shown to affect the quality of life of cancer survivors because having a job contributes to feelings of normalcy, resilience, and meaning (92). Being unemployed can also result in loss of health insurance benefits, particularly for those in the United States. Such a financial situation can be detrimental for survivors who depend on insurance benefits for care and can result in psychological stress. Moving forward, it will be essential to assess and discuss access to care and risk of financial toxicity and to facilitate access to social work and resources about loss of health coverage (ie, National Coalition of Cancer Survivorship).
Discuss End-of-Life Goals and Care
Although engaging patients in goals of care discussions has long been emphasized, the pandemic has highlighted the importance of goal-concordant care in several ways. The additional risk of COVID-19 has underscored the importance of proactive advance care planning for all oncology patients (93). As previously noted, cancer survivors most likely to develop severe COVID-19 will be older and have greater burden of chronic illness. These may (or not) be the same individuals who may wish to forgo prolonged life support and/or who may find their quality of life unacceptable after prolonged life support (94). In the context of the pandemic, advance care planning prior to and at the onset of serious acute illness should be a key objective. Clinicians should include clear documentation of these discussions, especially if they take place during a telemedicine visit. Several online resources can guide providers to carry out these conversations (39,95-98).
As the COVID‐19 pandemic continues to evolve and emerge in new areas or reemerge or abate in others, active cancer treatment as well as other urgent and emergent conditions will likely take priority. The pandemic has uncovered and exacerbated many challenges and highlighted the limitations of traditional health care delivery systems. While focusing on the needs of all survivors, it is vital to address and readdress the needs of long-term cancer survivors who are already vulnerable to the physical, psychological, and financial effects of cancer that are now amplified by the COVID-19 pandemic. Health care professionals, policymakers, and patient groups must take a systematic approach to evaluate, adopt, and refine measures needed to improve the health of cancer survivors during and beyond this pandemic.
Funding
Not applicable.
Notes
Role of funder: Not applicable.
Disclosures: No disclosures.
Prior presentations: None.
Disclaimers: Not applicable.
Author contributions: JMJ, HS, LN wrote the first draft of the manuscript. VJF, MBL and MSK reviewed and revised the manuscript.
Data Availability
Not applicable.
References
- 1. Miller K, Nogueira L, Mariotto A, et al. Cancer treatment and survivorship statistics. CA Cancer J Clin. 2019;69(5):363–385. [DOI] [PubMed] [Google Scholar]
- 2.The American Cancer Society. Cancer atlas. Cancer survivorship. 2019. https://canceratlas.cancer.org/the-burden/cancer-survivorship/. Accessed March 31, 2020.
- 3.World Health Organization. The global cancer observatory. 2018. http://gco.iarc.fr/. Accessed March 31, 2020.
- 4. Nekhlyudov L, Duijts S, Hudson S, et al. Addressing the needs of cancer survivors during the COVID-19 pandemic. J Cancer Surviv. 2020;14(5):601–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chan A, Ashbury F, Fitch M, Koczwara B, Chan R; MASCC Survivorship Study Group. Cancer survivorship care during COVID-19—perspectives and recommendations from the MASCC survivorship study group. Support Care Cancer. 2020;28(8):3485–3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koczwara B. Cancer survivorship care at the time of the COVID-19 pandemic. Med J Aust. 2020;213(3):107–108.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Young A, Ashbury F, Schapira L, Scotté F, Ripamonti C, Olver I.. Uncertainty upon uncertainty: supportive care for cancer and COVID-19. Support Care Cancer. 2020;28(9):4001–4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dai M, Chen Z, Leng Y, et al. Patients with lung cancer have high susceptibility of COVID-19: a retrospective study in Wuhan, China . Cancer Control. 2020;27(1):1073274820960467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saini K, Tagliamento M, Lambertini M, et al. Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. Eur J Cancer. 2020;139:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. de Lusignan S, Joy M, Oke J,D, et al. Disparities in the excess risk of mortality in the first wave of COVID-19: cross sectional study of the English sentinel network. J Infect. 2020;81(5):785–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kuderer N, Choueiri T, Shah D, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Albiges L, Foulon S, Bayle A, et al. Determinants of the outcomes of patients with cancer infected with SARS-CoV-2: results from the Gustave Roussy cohort. Nat Cancer. 2020;1(10):965–975. [DOI] [PubMed] [Google Scholar]
- 13. Mehta V, Goel S, Kabarriti R, et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020;10(7):935–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Williamson E, Walker A, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jazieh A, Akbulut H, Curigliano G, et al. ; on behalf of the International Research Network on COVID-19 Impact on Cancer Care. Impact of the COVID-19 pandemic on cancer care: a global collaborative study. J Clin Oncol Global Oncol. 2020;6(6):1428–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jacobson J. Suffering, systems, and safety: applying the principles of systems safety to improve the care of patients with cancer. J Clin Oncol Pract. 2020;16(3):115–120. [DOI] [PubMed] [Google Scholar]
- 17. Al-Shamsi H, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an International Collaborative Group. Oncologist. 2020;25(6):e936–e945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Burki T. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020;21(5):629–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Society of Clinical Oncology. ASCO Special Report: Guide to Cancer Care Delivery during the COVID-19 Pandemic. 2020.https://www.asco.org/sites/new-www.asco.org/files/content-files/2020-ASCO-Guide-Cancer-COVID19.pdf. Accessed May 20, 2020.
- 20. Sharpless N. COVID-19 and cancer. Cancer. 2020;368(6497):1290. [DOI] [PubMed] [Google Scholar]
- 21. de Joode K, Dumoulin D, Engelen V, et al. Impact of the coronavirus disease 2019 pandemic on cancer treatment: the patients' perspective. Eur J Cancer. 2020;136:132–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. American Cancer Society Cancer Action Network. COVID-19 pandemic impact on cancer patients and survivors. Survey findings summary. 2020. https://www.fightcancer.org/sites/default/files/National%20Documents/Survivor%20Views.COVID19%20Polling%20Memo.Final_.pdf. Accessed November 18, 2020.
- 23. Richards M, Anderson M, Carter P, Ebert B, Mossialos E.. The impact of the COVID-19 pandemic on cancer care. Nat Cancer. 2020;1(6):565–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Helsper C, Campbell C, Emery J, et al. Cancer has not gone away: a primary care perspective to support a balanced approach for timely cancer diagnosis during COVID‐19. Eur J Cancer Care. 2020;29(5):e13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Angulo F, Finelli L, Swerdlow D.. Reopening society and the need for real-time assessment of COVID-19 at the community level. JAMA. 2020;323(22):2247–2248. [DOI] [PubMed] [Google Scholar]
- 26. Leon D, Shkolnikov V, Smeeth L, Magnus P, Pechholdová M, Jarvis C.. COVID-19: a need for real-time monitoring of weekly excess deaths. Lancet. 2020;395(10234):e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Islam J, Camacho-Rivera M, Vidot D.. Examining COVID-19 preventive behaviors among cancer survivors in the United States: an analysis of the COVID-19 impact survey. Cancer Epidemiol Biomarkers Prev. 2020;29(12):2583–2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Society of Clinical Oncology. Cancer screening, diagnosis, staging and surveillance. 2020. https://www.asco.org/asco-coronavirus-resources/care-individuals-cancer-during-covid-19/cancer-screening-diagnosis-staging. Accessed August 18, 2020.
- 29. Miaskowski C, Paul S, Snowberg K, et al. Oncology patients’ perceptions of and experiences with COVID-19. Support Care Cancer 2020. 10.1007/s00520-020-05684-7. Accessed September 8, 2020. [DOI] [PMC free article] [PubMed]
- 30. Denis F, Basch E, Septans A, et al. Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer. JAMA. 2019;321(3):306–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Scotté F, Minvielle E, Mir O, André F, Barlesi F, Soria J.. A patient reported outcome platform, a useful tool to improve monitoring and effective management of Covid-19-positive patients with cancer. Eur J Cancer. 2020;132:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lkaddoum R, Haddad F, Eid R, Kourie H.. Telemedicine for cancer patients during COVID-19 pandemic: between threats and opportunities. Futur Oncol. 2020;16(18):1225–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liu R, Sundaresan T, Reed M, Trosman J, Weldon C, Kolevska T.. Telehealth in oncology during the COVID-19 outbreak: bringing the house call back virtually. J Clin Oncol Pract. 2020;16(6):289–293. [DOI] [PubMed] [Google Scholar]
- 34. Pareek P, Vishnoi J, Kombathula S, Vyas R, Misra S.. Teleoncology: the youngest pillar of oncology. J Clin Oncol Glob Oncol. 2020;6(6):1455–1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shachar C, Engel J, Elwyn G.. Implications for telehealth in a postpandemic future. JAMA. 2020;323(23):2375. [DOI] [PubMed] [Google Scholar]
- 36. Gray D, Joseph J, Olayiwola J.. Strategies for digital care of vulnerable patients in a COVID‐19 world—keeping in touch. JAMA Health Forum. 2020;1(6):e200734. [DOI] [PubMed] [Google Scholar]
- 37. Velasquez D, Mehrotra A. Ensuring the growth of telehealth during COVID‐19 does not exacerbate disparities in Care. Health Affairs Blog2020. healthaffairs.org/do/10.1377/hbog20200505.591306/full/. Accessed August 20, 2020.
- 38. Gharzai L, Resnicow K, An L, Jagsi R.. Perspectives on oncology-specific language during the coronavirus disease 2019 pandemic: a qualitative study. JAMA Oncol. 2020;6(9):1424–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Back A. VITALtalk. COVID Ready Communication Playbook. 2020. https://www.vitaltalk.org/wp-content/uploads/VitalTalk_COVID_English.pdf. Accessed October 1, 2020.
- 40.American Society for Clinical Oncology. Greater coverage, patient education, and research for telemedicine needed during pandemic and beyond. https://www.asco.org/about-asco/press-center/news-releases/greater-coverage-patient-education-and-research-telemedicine. Last updated August 14, 2020. Accessed October 2, 2020.
- 41. Baddour K, Kudrick LD, Neopaney A, et al. Potential impact of the COVID-19 pandemic on financial toxicity in cancer survivors. Head Neck. 2020;42(6):1332–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cancer Australia. Shared Follow-up Care and Survivorship Care. 2020. https://www.canceraustralia.gov.au/affected-cancer/information-about-cancer-and-covid-19/covid-19-recovery-implications-cancer-care/shared-follow-care-and-survivorship-care. Accessed September 15, 2020.
- 43. Hanna TP, Evans GA, Booth CM.. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17(5):268–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Institute for Health and Care Excellence (NICE). COVID-19 rapid guideline: delivery of systemic anticancer treatments. https://www.nice.org.uk/guidance/ng161/chapter/6-Prioritising-systemic-anticancer-treatments. Last updated November 9, 2020. Accessed November 24, 2020. [PubMed]
- 45.American Society for Radiation Oncology. Targeting cancer care. COVID-19 FAQs. https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/COVID-19-FAQ-Updates/COVID-19-FAQs#q8. Last updated June 2020. Accessed August 20, 2020.
- 46. Rexhepi H, Åhlfeldt R-M, Cajander Å, Huvila I.. Cancer patients’ attitudes and experiences of online access to their electronic medical records: a qualitative study. Health Informatics J. 2018;24(2):115–124. [DOI] [PubMed] [Google Scholar]
- 47. Walker J, Leveille S, Bell S, et al. OpenNotes after 7 years: patient experiences with ongoing access to their clinicians’ outpatient visit notes. J Med Internet Res. 2019;21(5):e13876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Essén A, Scandurra I, Gerrits R, et al. Patient access to electronic health records: differences across ten countries. Health Policy Technol. 2018;7(1):44–56. [Google Scholar]
- 49. Kriegel G, Bell S, Delbanco T, Walker J.. Covid-19 as innovation accelerator: cogenerating telemedicine visit notes with patients. NEJM Catal Innov Care Deliv. 2020;1Published 2020 May 12. doi:10.1056/CAT.20.0154. Accessed August 20, 2020. [Google Scholar]
- 50. Blease C, Salmi L, DesRoches C.. Open notes in cancer care: coming soon to patients. Lancet Oncol. 2020;21(9):1136–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McCleary N, Healey M, Weng S, et al. Perceptions of oncologists about sharing clinic notes with patients. Oncologist. 2019;24(1):e46–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kayastha N, Pollak K, LeBlanc T.. Open oncology notes: a qualitative study of oncology patients’ experiences reading their cancer care notes. J Oncol Pract. 2018;14(4):e251–e258. [DOI] [PubMed] [Google Scholar]
- 53. Gerard M, Fossa A, Folcarelli P, Walker J, Bell S.. What patients value about reading visit notes: a qualitative inquiry of patient experiences with their health information. J Med Internet Res. 2017;19(7):e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Shaverdian N, Chang E, Chu F, et al. Impact of open access to physician notes on radiation oncology patients: results from an exploratory survey. Pract Radiat Oncol. 2019;9(2):102–107. doi:10.1016/j.prro.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 55.United Nations News. UN leads call to protect most vulnerable from mental health crisis during and after COVID-19. May 14, 2020. https://news.un.org/en/story/2020/05/1063882.Accessed September 17, 2020.
- 56. Mitchell A, Ferguson D, Gill J, Paul J, Symonds P.. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. 2013;14(8):721–732. [DOI] [PubMed] [Google Scholar]
- 57. Gotze H, Friedrich M, Taubenheim S, Dietz A, Lordick F, Mehnert A.. Depression and anxiety in long-term survivors 5 and 10 years after cancer diagnosis. Support Care Cancer. 2020;28(1):211–220. [DOI] [PubMed] [Google Scholar]
- 58. Hartung T, Brahler E, Faller H, et al. The risk of being depressed is significantly higher in cancer patients than in the general population: prevalence and severity of depressive symptoms across major cancer types. Eur J Cancer. 2017;72:46–53. [DOI] [PubMed] [Google Scholar]
- 59. Ballal D, Gulia S, Gulia A.. The psychosocial implications on cancer patients: the hidden collateral of the war on coronavirus disease 2019. Indian J Palliat Care. 2020;26(5):126–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Patel J, Nielsen F, Badiani A, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020;183:110–11112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. AlWaheidi S, Sullivan R, Davies E.. Additional challenges faced by cancer patients in Gaza due to COVID-19. Ecancermedicalscience. 2020;14(ed100):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Poulson M, Geary A, Annesi C, et al. National disparities in COVID-19 outcomes between Black and White Americans. J Natl Med Assoc. 2020;S0027-9684(20):30148–30149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Galea S, Merchant R, Lurie N.. The mental health consequences of COVID-19 and physical distancing the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. [DOI] [PubMed] [Google Scholar]
- 64. Polizzi Cl S, Perry A.. Stress and coping in the time of COVID-19: pathways to resilience and recovery. Clin Neuropsychiatry. 2020;17(2):59–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Soraci P, Ferrari A, Abbiati F, et al. Validation and psychometric evaluation of the Italian version of the fear of COVID-19 scale. Int J Ment Health Addict. 2020. May4;1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Cohen G, Tamrakar S, Lowe S, et al. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry. 2017;74(12):1251–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kowitt S, Ellis K, Carlisle V, et al. Peer support opportunities across the cancer care continuum: a systematic scoping review of recent peer-reviewed literature. Support Care Cancer. 2019;27(1):97- 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.The Policy Institute, King's College London. Life under lockdown: Coronavirus in the UK. 2020. https://www.kcl.ac.uk/policy-institute/assets/coronavirus-in-the-uk.pdf. Accessed April 9, 2020.
- 69. Arora T, Grey I.. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J Health Psychol. 2020;25(9):1155–1163. [DOI] [PubMed] [Google Scholar]
- 70.Agriculture and Horticulture Development Board. An early look at how the coronavirus is affecting household spending. 2020. https://www.commbank.com.au/guidance/business/an-early-look-at-how-the-coronavirus-is-affecting-household-spen-202003.html.
- 71.Delaney, B. Drinking in coronavirus isolation: experts warn Australians to monitor their intake. https://www.theguardian.com/lifeandstyle/2020/apr/07/drinking-in-coronavirus-isolation-experts-warn-australians-to-monitor-their-intake. Accessed August 20, 2020.
- 72.British Broadcasting Commission. Coronavirus: shoppers stock up on alcohol amid lockdown. April 9, 2020. https://www.bbc.com/news/business-52226488. Accessed August 20, 2020.
- 73. Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 2020;6(6):e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Stanton R, To Q, Khalesi S, et al. Depression, anxiety and stress during COVID-19. Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(6):4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Matias T, Dominski F, Marks D.. Human needs in COVID-19 isolation. J Health Psychol. 2020;25(7):871–882. [DOI] [PubMed] [Google Scholar]
- 76. Tollosa D, Tavener M, Hure A, James E.. Adherence to multiple health behaviours in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2019;13(3):327–343. [DOI] [PubMed] [Google Scholar]
- 77. Meyerhardt J, Giovannucci E, Holmes M, et al. Physical activity and survival after colorectal cancer diagnosis. J Clin Oncol. 2006;24(22):3527–3534. [DOI] [PubMed] [Google Scholar]
- 78. Booth F, Roberts C, Thyfault J, Ruegsegger G, Toedebusch R.. Role of inactivity in chronic diseases: evolutionary insight and pathophysiological mechanisms. Physiol Rev. 2017;97(4):1351–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.World Cancer Research Fund, Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective (Third Report). 2018. https://www.wcrf.org/dietandcancer. Accessed August 21, 2020.
- 80. Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA.. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293(20):2479–2486. [DOI] [PubMed] [Google Scholar]
- 81. Avancini A, Trestini I, Tregnago D, et al. Physical activity for Oncological Patients in COVID-19 era: no time to relax. JNCI Cancer Spectrum. 2020;4(6):pkaa071.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Chen P, Mao L, Nassis G, Harmer P, Ainsworth B, Li F.. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9(2):103–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Schwendinger F, Pocecco E.. Counteracting physical inactivity during the COVID-19 pandemic: evidence-based recommendations for home-based exercise. Int J Environ Res Public Health. 2020;17(11):3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Pinto A, Dunstan D, Owen N, Bonfá E, Gualano B.. Combating physical inactivity during the COVID-19 pandemic. Nat Rev Rheumatol. 2020;16(7):347–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Merchant R, Lurie N.. Social media and emergency preparedness in response to novel coronavirus. JAMA. 2020;323(20):2011–2012. [DOI] [PubMed] [Google Scholar]
- 86. Carrera P, Kantarjian H, Blinder V.. The financial burden and distress of patients with cancer: understanding and stepping‐up action on the financial toxicity of cancer treatment. CA Cancer J Clin. 2018;68(2):153–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Kale H, Carroll N.. Self‐reported financial burden of cancer care and its effect on physical and mental health‐related quality of life among US cancer survivors. Cancer. 2016;122(8):283–289. [DOI] [PubMed] [Google Scholar]
- 88. Zafar S, McNeil R, Thomas C, Lathan C, Ayanian J, Provenzale D.. Population‐based assessment of cancer survivors' financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ramsey S, Bansal A, Fedorenko C, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34(9):980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Selden TM, Berdahl TA.. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff. 2020;39(9):1624–1632. [DOI] [PubMed] [Google Scholar]
- 91. van Egmond M, Duijts S, Loyen A, Vermeulen S, van der Beek A, Anema J.. Barriers and facilitators for return to work in cancer survivors with job loss experience: a focus group study. Eur J Cancer Care. 2017;26(5):e12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. de Boer AG, Torp S, Popa A, et al. Long-term work retention after treatment for cancer: a systematic review and meta-analysis. J Cancer Surviv. 2020;14(2):135–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Curtis J, Kross E, Stapleton R.. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19). JAMA. 2020;323(18):1771–1772. [DOI] [PubMed] [Google Scholar]
- 94. Fried T, Bradley E, Towle V, Allore H.. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–1066. [DOI] [PubMed] [Google Scholar]
- 95. Sudore R, Schillinger D, Katen M, et al. Engaging diverse English- and Spanish-speaking older adults in advance care planning: the PREPARE randomized clinical trial. JAMA Intern Med. 2018;178(12):1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Institute for Healthcare Improvement. The Conversation Project. http://theconversationproject.org. Accessed March 21, 2020.
- 97. Holstead R, Robinson AJOP.. Discussing serious news remotely: navigating difficult conversations during a pandemic. J Clin Oncol Pract. 2020;16(7):363–368. [DOI] [PubMed] [Google Scholar]
- 98.Tides Centre. POLST and COVID-19. 2020. https://polst.org/covid/?pro=1 . Accessed October 2, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.