Abstract
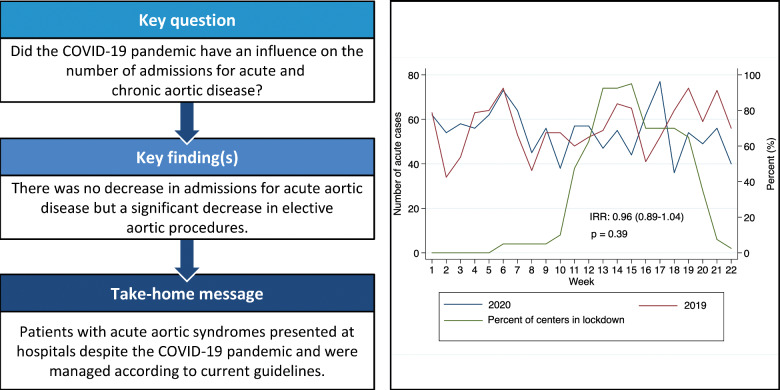
OBJECTIVES
To evaluate the impact of the coronavirus disease 2019 (COVID-19) pandemic on acute and elective thoracic and abdominal aortic procedures.
METHODS
Forty departments shared their data on acute and elective thoracic and abdominal aortic procedures between January and May 2020 and January and May 2019 in Europe, Asia and the USA. Admission rates as well as delay from onset of symptoms to referral were compared.
RESULTS
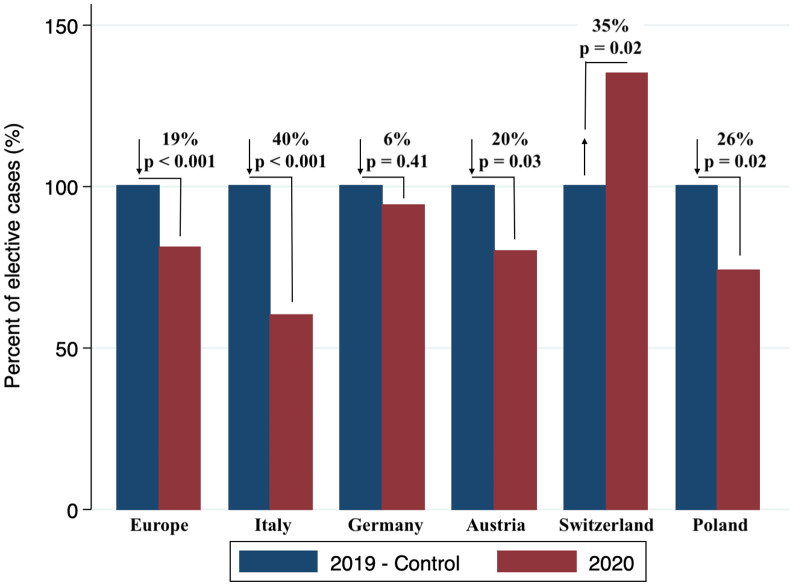
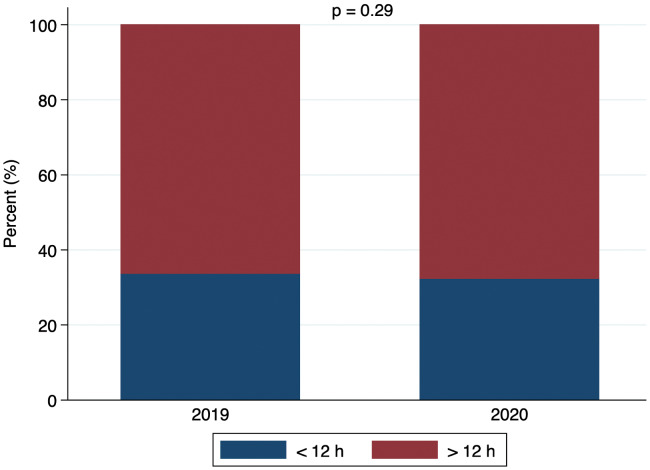
No differences in the number of acute thoracic and abdominal aortic procedures were observed between 2020 and the reference period in 2019 [incidence rates ratio (IRR): 0.96, confidence interval (CI) 0.89–1.04; P = 0.39]. Also, no difference in the time interval from acute onset of symptoms to referral was recorded (<12 h 32% vs > 12 h 68% in 2020, < 12 h 34% vs > 12 h 66% in 2019 P = 0.29). Conversely, a decline of 35% in elective procedures was seen (IRR: 0.81, CI 0.76–0.87; P < 0.001) with substantial differences between countries and the most pronounced decline in Italy (−40%, P < 0.001). Interestingly, in Switzerland, an increase in the number of elective cases was observed (+35%, P = 0.02).
CONCLUSIONS
There was no change in the number of acute thoracic and abdominal aortic cases and procedures during the initial wave of the COVID-19 pandemic, whereas the case load of elective operations and procedures decreased significantly. Patients with acute aortic syndromes presented despite COVID-19 and were managed according to current guidelines. Further analysis is required to prove that deferral of elective cases had no impact on premature mortality.
Keywords: Acute and elective thoracic and abdominal aortic procedures, Coronavirus disease 2019 pandemic
During the initial wave of the coronavirus disease 2019 (COVID-19) pandemic, a substantial decrease in the admission rates of patients with acute coronary syndromes (ACS) and consequently, a sharp decline in the number of emergency coronary procedures performed in Europe and the USA, were observed [1–3].
INTRODUCTION
During the initial wave of the coronavirus disease 2019 (COVID-19) pandemic, a substantial decrease in the admission rates of patients with acute coronary syndromes (ACS) and consequently, a sharp decline in the number of emergency coronary procedures performed in Europe and the USA, were observed [1–3]. In several European countries, the nationwide lockdown severely restricted movement, which might have contributed to this phenomenon on top of the widespread fear of contracting COVID-19 when admitted into a hospital [4]. There is substantial concern that similar trends will be observed in the setting of acute aortic syndrome (aortic dissection) with a substantial death toll, if not managed swiftly.
The aim of this study was to evaluate the impact of the COVID-19 pandemic on acute and elective thoracic and abdominal aortic procedures and to compare the data with the same period in 2019 in participating institutions.
PATIENTS AND METHODS
Patients
The study was registered at the ethics committee—Albert-Ludwigs-University Freiburg under the reference ID: 20-1025. Forty departments from Europe, Asia and the USA that provided services for acute and chronic aortic conditions contributed and shared their data on the number of acute and elective thoracic and abdominal aortic procedures performed between January and May 2020 and between January and May 2019. Only the number of procedures for acute and chronic aortic conditions, further divided into thoracic and abdominal procedures, without any patient-related information was collected. Figure 1 shows the location of the participating departments. Figure 1 was generated with google maps.
Figure 1:
Location of the participating departments (source: google maps).
Definitions
Thoracic aortic pathology comprised any pathology beginning at the proximal thoracic aorta with treatment of the disease is usually limited to the thoracic aorta but also extending down to the abdominal aorta (e.g. type A, type non-A-non-B and type B aortic dissection). Abdominal aortic pathology refers to any pathology below the diaphragm and involving the abdominal aorta with or without the iliac arteries. Acute aortic pathology indicates any pathology requiring urgent or emergency treatment, whereas a chronic aortic pathology was present when treatment could be deferred to an elective setting.
Data collection
A template excel file was sent to all participating aortic centres with the request to share their number of procedures partitioned in calendar weeks [1–22] in 2020 and 2019. In addition, in acute cases, we retrieved the time between onset of symptoms and referral for treatment. Data were systematically retrieved from institutional databases for cardiac and vascular care units.
Statistical methods
The cases are presented as weekly recorded numbers in all centres. Incidence rates ratios (IRRs) were calculated by using Poisson regression analysis. The IRRs are presented with 95% confidence intervals (CIs). Statistical analysis was performed using R version 3.6.1 for macOS (The R Foundation for Statistical Computing, Vienna, Austria) with a level of significance set at P-value <0.05.
RESULTS
Acute and elective aortic cases in Europe, Asia, the USA
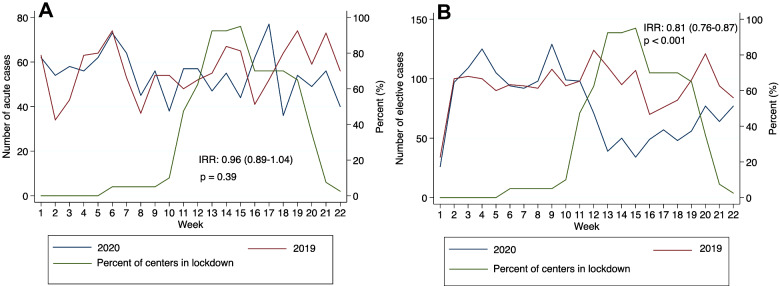
No difference in the number of acute aortic cases could be observed between 2020 and 2019 (IRR: 0.96, CI 0.89–1.04; P = 0.39), Fig. 2A. A significant decrease of 35% in elective cases was seen (IRR: 0.81, CI 0.76–0.87; P < 0.001), Fig. 2B. Table 1 shows the number of acute and elective cases per calendar week in 2020 and stratifies the acute cases in <12 and >12 h between onset of symptoms and referral for treatment. Table 2 shows the number of acute and elective cases per calendar week in 2019 and stratifies the acute cases in <12 and >12 h between onset of symptoms and referral for treatment.
Figure 2:
(A) Acute aortic cases—Europe, Asia, USA. (B) Elective aortic cases—Europe, Asia, USA.
Table 1:
Acute and elective cases per week—2020
| Week | Total cases | Total acute cases | Acute >12 h | Acute <12 h | Total elective cases |
|---|---|---|---|---|---|
| 1 | 88 | 62 | 23 | 39 | 26 |
| 2 | 151 | 54 | 23 | 31 | 97 |
| 3 | 167 | 58 | 21 | 37 | 109 |
| 4 | 181 | 56 | 20 | 36 | 125 |
| 5 | 167 | 62 | 19 | 43 | 105 |
| 6 | 167 | 73 | 17 | 56 | 94 |
| 7 | 156 | 64 | 21 | 43 | 92 |
| 8 | 143 | 45 | 15 | 30 | 98 |
| 9 | 185 | 56 | 17 | 39 | 129 |
| 10 | 137 | 38 | 10 | 28 | 99 |
| 11 | 155 | 57 | 15 | 42 | 98 |
| 12 | 128 | 57 | 20 | 37 | 71 |
| 13 | 86 | 47 | 20 | 27 | 39 |
| 14 | 105 | 55 | 14 | 41 | 50 |
| 15 | 78 | 44 | 16 | 28 | 34 |
| 16 | 111 | 62 | 17 | 45 | 49 |
| 17 | 134 | 77 | 27 | 50 | 57 |
| 18 | 84 | 36 | 9 | 27 | 48 |
| 19 | 110 | 54 | 18 | 36 | 56 |
| 20 | 126 | 49 | 13 | 36 | 77 |
| 21 | 120 | 56 | 19 | 37 | 64 |
| 22 | 117 | 40 | 13 | 27 | 77 |
Table 2:
Acute and elective cases per week—2019
| Week | Total cases | Total acute cases | Acute >12 h | Acute <12 h | Total elective cases |
|---|---|---|---|---|---|
| 1 | 97 | 63 | 26 | 37 | 34 |
| 2 | 134 | 34 | 10 | 24 | 100 |
| 3 | 145 | 43 | 14 | 29 | 102 |
| 4 | 163 | 63 | 20 | 43 | 100 |
| 5 | 154 | 64 | 23 | 41 | 90 |
| 6 | 169 | 74 | 20 | 54 | 95 |
| 7 | 147 | 53 | 23 | 30 | 94 |
| 8 | 129 | 37 | 16 | 21 | 92 |
| 9 | 162 | 54 | 17 | 37 | 108 |
| 10 | 148 | 54 | 15 | 39 | 94 |
| 11 | 146 | 48 | 16 | 32 | 98 |
| 12 | 176 | 52 | 20 | 32 | 124 |
| 13 | 165 | 55 | 19 | 36 | 110 |
| 14 | 162 | 67 | 23 | 44 | 95 |
| 15 | 172 | 65 | 22 | 43 | 107 |
| 16 | 111 | 41 | 13 | 28 | 70 |
| 17 | 128 | 52 | 15 | 37 | 76 |
| 18 | 146 | 64 | 25 | 39 | 82 |
| 19 | 173 | 74 | 19 | 55 | 99 |
| 20 | 180 | 59 | 19 | 40 | 121 |
| 21 | 167 | 73 | 29 | 44 | 94 |
| 22 | 140 | 56 | 14 | 42 | 84 |
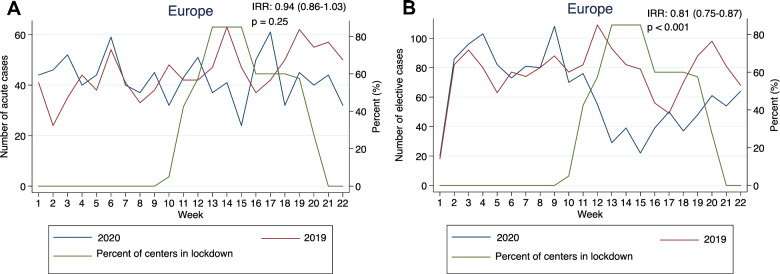
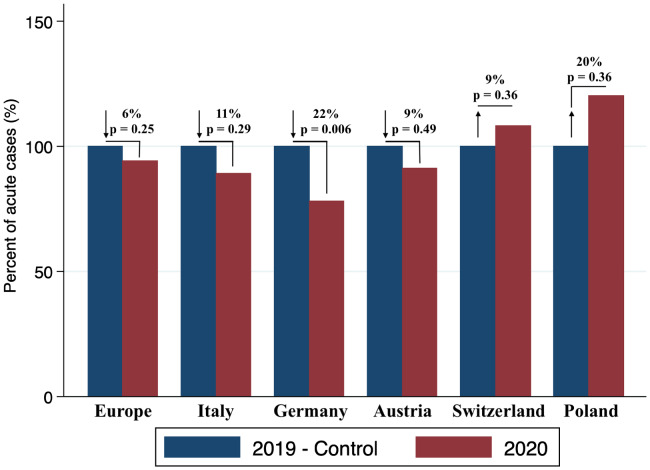
Acute and elective aortic cases—Europe
No difference in the number of acute aortic cases could be observed between 2020 and 2019 (IRR: 0.94, CI 0.86–1.03; P = 0.25), Fig. 3A. A decrease in elective cases was seen (IRR: 0.81, CI 0.75–0.87; P < 0.001) as shown in Fig. 3B. In Figs 2–3, we additionally added the percentage of the centres being affected by the lockdown per week by retrieving these data from https://en.wikipedia.org/wiki/COVID-19_pandemic_lockdowns where the exact time points and durations of lockdowns are documented. Figure 4 shows the changes in acute cases in Europe according to country, where no significant decrease could be observed in Italy (decrease by 11%, P = 0.29) and Austria (decrease by 9%, P = 0.49). In Switzerland (increase by 9%, P = 0.36) and Poland (increase by 20%, P = 0.36), a non-significant increase in acute cases could be observed. Germany was the only country where a significant decrease in acute cases was seen (decrease by 22%, P = 0.006). Figure 5 shows the changes in elective cases in Europe according to country, in which Italy (decrease by 40%, P < 0.001), Austria (decrease by 20%, P = 0.03) and Poland (decrease by 26%, P = 0.02) showed a significant decrease, whereas the decrease was non-significant in Germany (decrease by 6%, P = 0.41). On the other hand, Switzerland showed an increase in elective cases as compared to 2019 (increase by 35%, P = 0.02).
Figure 3:
(A) Acute aortic cases—Europe. (B) Elective aortic cases—Europe.
Figure 4:
Changes in acute cases in Europe according to country.
Figure 5:
Changes in elective cases in Europe according to country.
Time between onset of symptoms and referral
In acute cases, no difference regarding the time interval from acute onset of symptoms to referral was recorded (< 12 h 32% vs > 12 h 68% in 2020, < 12 h 34% vs > 12 h 66% in 2019) P = 0.29 (Fig. 6).
Figure 6:
Time interval from acute onset of symptoms to referral.
DISCUSSION
There was no change in the number of procedures for acute thoracic and abdominal aortic pathologies during the initial phase of the COVID-19 pandemic whereas, due to the provision of intensive care capacity for potential COVID-19 patients, a decrease in elective thoracic and abdominal procedures was observed. The burden of aortic pain seems to outperform the reluctance to seek medical attention which is reflected in a similar time interval between onset of symptoms and referral, when compared with the pre-COVID-19 times.
In comparison to other cardiovascular pathologies, such as ACS, the incidence of acute aortic syndrome and the prevalence of chronic thoracic and abdominal aortic pathologies are low. However, pooling data from 40 institutions affected by the pandemic may enable a robust analysis on a representative cross-section of the current situation in 3 continents. Interestingly, even in 2020 (under pandemic conditions), the overall number of acute cases remained unchanged. This finding might well be attributed to the fact that symptoms from acute aortic syndromes are so striking, that the potential reluctance to seek medical advice, which has been reported in other types of cardiovascular disease such as ACS, is overridden by the urge to seek medical help [5]. This is also backed by a German analysis on admissions for acute myocardial infarction, acute limb ischaemia, aortic rupture, stroke or transient ischaemic attack (TIA) between 1 January 2019 and 31 May 2020 that found a decline in admissions between 9% and 15% for all other conditions but no decline in admissions for aortic rupture [6].
There was a substantial decrease in elective cases in particular between calendar Week 11 and 15 which can be clearly related to nationwide lockdown in most countries and a reduction in elective surgical procedures in order to be able to preserve intensive care capacity for potential COVID-19 patients [7]. As this expected increase in ICU admissions for COVID-19 patients did not occur in many settings, these measures were gradually eased, enabling the resumption of treatment for elective patients.
This exact same pattern could be observed when focusing on various European centres in this report. However, some differences were observed between European countries with regard to both acute and elective procedures. Regarding acute cases, stable conditions could be observed in Italy, Austria, Switzerland and Poland with little fluctuations. Germany was the only country where a significant decrease was observed, in particular between Calendar week 14 and 22. Currently, the reasons remain speculative but reluctance of patients to seek advice or a natural undulation in the incidence might be causative [8]. But in some epicentres of the COVID-19 pandemic a dramatic decrease in patients treated for acute aortic disease could also be seen [9, 10].
The decrease in elective cases in Europe was substantial with 2 exceptions, Germany where conditions were stable, and Switzerland where even an increase in elective cases was observed. The reason here might well represent the fact that one department of vascular surgery was recently newly established—which makes a difference in a small country and referrals were increasing there despite the COVID-19 pandemic. Another reason might well be the adherence to guidelines as well as the newly developed knowledge that even patients with diameters having just crossed the threshold to indication already have a substantial yearly risk of sustaining an acute aortic event, which justifies timely treatment [11]. Finally, the net numbers per country could well explain fluctuations in both directions which refer in particular to smaller countries. This is reasonable, as an acute aortic event on top of a chronic aortic condition will substantially impact immediate as well as long-term outcome [12]. Finally, hospital strategies play a decisive role in this rapidly changing environment. However, as national rules regarding the provision of care for potential COVID-19 patients—at least in the countries participating in this project—have been very similar, we would not expect an effect in this regard on our results.
Interestingly, the time between onset of symptoms and referral in acute cases showed no difference, which is in contrast to a very recent analysis on symptom-to-hospital analysis in ST-elevation myocardial infarction patients in the UK, where a decrease in number of procedures and an increase in the time interval to hospitalization were observed [13]. Here, it seems obvious that typical aortic syndrome is such a devastating clinical event that patients will seek medical advice regardless of circumstances (as long as hospitals provide acute aortic care) and that the need and provision of acute aortic care and emergency operations is independent of any pandemic and should always be an option.
Limitations and strengths
This report lacks nationwide reporting but is the first of its kind to analyse referral pattern in the setting of the COVID-19 pandemic by data sharing of several high-volume cardiovascular referral centres from 3 continents, which provided a unique opportunity to obtain insight into this complex and dynamic topic. It has to be clearly stated that the low number of centres contributing from outside of Europe might therefore not reflect the actual situation in the respective regions or countries. Finally, conservative management of aortic diseases is expected to have increased during the pandemic. This may be related to restrictions on the resources or to a decreased use of health facilities by patients with symptoms, although these data cannot be mirrored by this analysis.
CONCLUSION
In summary, there was no change in the number of procedures in acute thoracic and abdominal aortic pathologies during the initial phase of the COVID-19 pandemic whereas, due to the provision of intensive care capacity for potential COVID-19 patients, a decrease in elective thoracic and abdominal procedures has been observed. The burden of aortic pain seems to exceed the reluctance to seek medical advice which is additionally reflected in an unchanged time interval between onset of symptoms and referral. The need for acute aortic care is unchanged in a pandemic and resources are to be secured.
Conflict of interest: none declared.
Author contributions
Martin Czerny: Conceptualization; Formal analysis; Writing—original draft; Writing—review and editing. Roman Gottardi: Conceptualization; Data curation; Writing—original draft; Writing—review and editing. Paul Puiu: Data curation; Formal analysis; Writing—original draft. Oliver Bernecker: Data curation; Writing—review and editing. Rodolfo Citro: Data curation; Writing—review and editing. Alessandro Della Corte: Data curation; Writing—review and editing. Luca Di Marco: Data curation; Writing—review and editing. Martina Fink: Data curation; Writing—review and editing. Yvonne Gosslau: Data curation; Writing—review and editing. Peter Haldenwang: Data curation; Writing—review and editing. Robin Hejimen: Data curation; Writing—review and editing. Maria Hugas-Mallorqui: Data curation; Writing—review and editing. Severino Iesu: Data curation; Writing—review and editing. Oyvind Jakobsen: Data curation; Writing—review and editing. Arminder S. Jassar: Data curation; Writing—review and editing. Andrzej Juraszek: Data curation; Writing—review and editing. Maciej Kolowca: Data curation; Writing—review and editing. Sandro Lepidi: Data curation; Writing—review and editing. Massimiliano Marrocco-Trischitta: Data curation; Writing—review and editing. Hitoshi Matsuda: Data curation; Writing—review and editing. Katrin Meisenbacher: Data curation; Writing—review and editing. Antonio Micari: Data curation; Writing—review and editing. Kenji Minatoya: Data curation; Writing—review and editing. Kay-Hyun Park: Data curation; Writing—review and editing. Sven Peterss: Data curation; Writing—review and editing. Michael Petrich: Data curation; Writing—review and editing. Gabriele Piffaretti: Data curation; Writing—review and editing. Chris Probst: Data curation; Writing—review and editing. Benedikt Reutersberg: Data curation; Writing—review and editing. Fabrizio Rosati: Data curation; Writing—review and editing. Thomas Schachner. Data curation; Writing—review and editing. Bruno Schachner: Data curation; Writing—review and editing. Vitaly Sorokin: Data curation; Writing—review and editing. Zoltan Szeberin: Writing—review and editing. Eliza Pleban: Data curation; Writing—review and editing. Luigi Di Tommaso: Data curation; Writing—review and editing. Santi Trimarchi: Data curation; Writing—review and editing. Eric Verhoeven: Data curation; Writing—review and editing. Ferdinand Vogt: Data curation; Writing—review and editing. Andreas Voetsch: Data curation; Writing—review and editing. Tim Walter: Data curation; Writing—review and editing. Gabriel Weiss: Data curation; Writing—review and editing. Xun Yuan: Data curation; Writing—review and editing. Antonio De Bellis: Data curation; Writing—review and editing. Mario D'Oria: Conceptualization; Writing—review and editing. Filippo Benedetto: Data curation; Writing—review and editing. Andreas Zierer: Data curation; Writing—review and editing. Chiara Lomazzi: Data curation; Writing—review and editing. Philipp Discher: Data curation; Writing—review and editing. Bartosz Rylski: Writing—original draft; Writing—review and editing. Jos C. Van Den Berg: Writing—original draft; Writing—review and editing. Thomas Wyss: Data curation; Writing—original draft; Writing—review and editing. Eduardo Bossone: Conceptualization; Writing—review and editing. Jürg Schmidli: Conceptualization; Writing—original draft; Writing—review and editing. Christoph Nienaber: Conceptualization; Formal analysis; Writing—original draft; Writing—review and editing.
Reviewer information
European Journal of Cardio-Thoracic Surgery thanks Nikolaos Bonaros and Alexander Janosi and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
Glossary
ABBREVIATIONS
- ACS
Acute coronary syndromes
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- IRR
Incidence rates ratio
- TIA
Transient ischaemic attack
Contributor Information
Martin Czerny, Department for Cardiovascular Surgery, University Heart Center Freiburg-Bad Krozingen, Freiburg, Germany; Faculty of Medicine, Albert-Ludwigs-University Freiburg, Freiburg, Germany.
Roman Gottardi, Department of Cardiovascular and Thoracic Surgery, MediClin Heart Institute Lahr/Baden, Lahr, Germany; Paracelsus Medical University Salzburg, Salzburg, Austria.
Paul Puiu, Department for Cardiovascular Surgery, University Heart Center Freiburg-Bad Krozingen, Freiburg, Germany; Faculty of Medicine, Albert-Ludwigs-University Freiburg, Freiburg, Germany.
Oliver Y Bernecker, Department of Cardiac Surgery, University Hospital St. Poelten, St. Poelten, Austria.
Rodolfo Citro, Cardiology Unit, University Hospital San Giovanni di Dio e Ruggi d´Aragona, Salerno, Italy.
Alessandro Della Corte, Cardiac Surgery Unit, Department of Translational Medical Sciences, University of Campania “L.Vanvitelli”, Monaldi Hospital, Naples, Italy.
Luca di Marco, Department of Cardiac Surgery, Hospital Santa Orsola, University of Bologna, Bologna, Italy.
Martina Fink, Department of Vascular Surgery, HGZ Bad Bevensen, Bad Bevensen, Germany.
Yvonne Gosslau, Department for Vascular and Endovascular Surgery, University Hospital Augsburg, Augsburg, Germany.
Peter Lukas Haldenwang, Department of Cardiothoracic Surgery, University Hospital Bergmannsheil Bochum, Ruhr University of Bochum, Bochum, Germany.
Robin H Heijmen, Department of Cardiothoracic Surgery, St. Antonius Hospital, Nieuwegein, Netherlands.
Maria Hugas-Mallorqui, Department of Cardiovascular Surgery, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Severino Iesu, Cardiac Surgery Unit, University Hospital San Giovanni di Dio e Ruggi d´Aragona, Salerno, Italy.
Oyvind Jacobsen, Department of Cardiothoracic and Vascular Surgery, University Hospital of North Norway, Oslo, Norway.
Arminder S Jassar, Division of Cardiac Surgery, Corrigan Minehan Heart Center, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
Andrzej Juraszek, Department of Cardiac Surgery and Transplantation, The Cardinal Stefan Wyszynski National Institute of Cardiology, Warsaw, Poland.
Maciej Kolowca, Cardiac Surgery Department, University State Hospital No 2, University of Rzesznow, Rzesznow, Poland.
Sandro Lepidi, Division of Vascular and Endovascular Surgery, Cardiovascular Department, University of Trieste Medical School, Trieste, Italy.
Massimiliano M Marrocco-Trischitta, Cardiovascular Department, IRCCS-Policlinico San Donato, Milan, Italy.
Hitoshi Matsuda, Department of Cardiovascular Surgery, National Cerebral and Cardiovascular Center, Osaka, Japan.
Katrin Meisenbacher, Department of Vascular and Endovascular Surgery, University Hospital Heidelberg, Heidelberg, Germany.
Antonio Micari, Cardiology, University of Messina, Messina, Italy.
Kenji Minatoya, Department of Cardiovascular Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan.
Kay-Hyun Park, Department of Thoracic and Cardiovascular Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
Sven Peterss, Department of Cardiac Surgery, LMU University Hospital, Munich, Germany.
Michael Petrich, Department of Vascular and Endovascular Surgery, Hubertus Hospital Berlin, Berlin, Germany.
Gabriele Piffaretti, Vascular Surgery, Department of Medicine and Surgery, University of Insubria, School of Medicine and ASST Settelaghi University Teaching Hospital, Varese, Italy.
Chris Probst, Department of Cardiac Surgery, University of Bonn, Bonn, Germany.
Benedikt Reutersberg, Department for Vascular Surgery, University Hospital Zurich, Zurich, Switzerland.
Fabrizio Rosati, Division of Cardiac Surgery, University of Brescia Medical School, Brescia, Italy.
Bruno Schachner, Department of Cardiothoracic and Vascular Surgery, Kepler University Hospital, Medical Faculty, Johannes Kepler University Linz, Linz, Austria.
Thomas Schachner, Department of Cardiac Surgery, Medical University Innsbruck, Innsbruck, Austria.
Vitali A Sorokin, Department of Cardiac, Thoracic and Vascular Surgery, National University Hospital, National University Health System, Singapore.
Zoltan Szeberin, Department of Vascular and Endovascular Surgery, Semmelweis University, Budapest, Hungary.
Piotr Szopinski, Department of Vascular Surgery, Institute of Hematology and Transfusion Medicine, Warsaw, Poland.
Luigi Di Tommaso, Department of Cardiac Surgery, School of Medicine, University Federico II, Naples, Italy.
Santi Trimarchi, Unita Operativa di Chirurgia Vascolare, Fondazione IRCCS Ca Granda Ospedale Maggiore Policlinico Milan, Milan, Italy; Department of Clinical and Community Sciences, University of Milan, Milan, Italy.
Eric L G Verhoeven, Department of Vascular and Endovascular Surgery, Paracelsus Medical University Nuremberg, Nuremberg, Germany.
Ferdinand Vogt, Department of Cardiac Surgery, Paracelsus Medical University Nuremberg, Nuremberg, Germany.
Andreas Voetsch, Department of Cardiovascular and Endovascular Surgery, Paracelsus Medical University Salzburg, Salzburg, Austria.
Tim Walter, Department for Cardiovascular Surgery, University Heart Center Freiburg-Bad Krozingen, Freiburg, Germany; Faculty of Medicine, Albert-Ludwigs-University Freiburg, Freiburg, Germany.
Gabriel Weiss, Department of Vascular Surgery, Clinic Ottakring.
Xun Yuan, Cardiology and Aortic Centre, The Royal Brompton & Harefield NHS Foundation Trust; National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London, UK.
Filippo Benedetto, Vascular Surgery Unit, University of Messina, Messina, Italy.
Antonio De Bellis, Cardiac Surgery Unit, Heart and Vessels Department, Casa di Cura San Michele, Maddaloni, Italy.
Mario D´ Oria, Division of Vascular and Endovascular Surgery, Cardiovascular Department, University of Trieste Medical School, Trieste, Italy.
Philipp Discher, Department for Cardiovascular Surgery, University Heart Center Freiburg-Bad Krozingen, Freiburg, Germany; Faculty of Medicine, Albert-Ludwigs-University Freiburg, Freiburg, Germany.
Andreas Zierer, Department of Cardiothoracic and Vascular Surgery, Kepler University Hospital, Medical Faculty, Johannes Kepler University Linz, Linz, Austria.
Bartosz Rylski, Department for Cardiovascular Surgery, University Heart Center Freiburg-Bad Krozingen, Freiburg, Germany; Faculty of Medicine, Albert-Ludwigs-University Freiburg, Freiburg, Germany.
Jos C van den Berg, Centro Vasolare Ticino, Ospedale Regionale di Lugano, Lugano, Switzerland; Department of Radiology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Thomas R Wyss, Department of Cardiovascular Surgery, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; Department of Vascular Surgery, Cantonal Hospital Winterthur, Winterthur, Switzerland.
Eduardo Bossone, Division of Cardiology, Cardarelli Hospital, Naples, Italy.
Jürg Schmidli, Department of Cardiovascular Surgery, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Christoph Nienaber, Cardiology and Aortic Centre, The Royal Brompton & Harefield NHS Foundation Trust; National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London, UK.
Giulio Accarino, Cardiac Surgery Unit, University Hospital San Giovanni di Dio e Ruggi d´Aragona, Salerno, Italy.
Francesco Baldascino, Vascular Surgery Unit, University of Messina, Messina, Italy.
Dittmar Böckler, Department of Vascular and Endovascular Surgery, University Hospital Heidelberg, Heidelberg, Germany.
Claudio Corazzari, Department of Cardiac Surgery, Department of Medicine and Surgery, University of Insubria, School of Medicine and ASST Settelaghi University Teaching Hospital, Varese, Italy.
Ilenia D´ Alessio, Unita Operativa di Chirurgia Vascolare, Fondazione IRCCS Ca Granda Ospedale Maggiore Policlinico Milan, Milan, Italy; Department of Clinical and Community Sciences, University of Milan, Milan, Italy.
Hector de Beaufort, Department of Cardiothoracic Surgery, St. Antonius Hospital, Nieuwegein, Netherlands.
Christopher De Troia, Thoracic Aortic Center, Massachusetts General Hospital, Boston, MA, USA.
Julia Dumfarth, Department of Cardiac Surgery, Medical University Innsbruck, Innsbruck, Austria.
Denise Galbiati, Cardiac Surgery Unit, Department of Translational Medical Sciences, University of Campania “L.Vanvitelli”, Monaldi Hospital, Naples, Italy.
Filippo Gorgatti, Division of Vascular and Endovascular Surgery, Cardiovascular Department, University of Trieste Medical School, Trieste, Italy.
Christian Hagl, Department of Cardiac Surgery, LMU University Hospital, Munich, Germany.
Marwan Hamiko, Department of Cardiac Surgery, University of Bonn, Bonn, Germany.
Florian Huber, Department of Cardiothoracic and Vascular Surgery, Kepler University Hospital, Medical Faculty, Johannes Kepler University Linz, Linz, Austria.
Alexander Hyhlik-Duerr, Department for Vascular and Endovascular Surgery, University Hospital Augsburg, Augsburg, Germany.
Gabriele Ianelli, Department of Cardiac Surgery, School of Medicine, University Federico II, Naples, Italy.
Ivana Iesu, Cardiology Unit, University Hospital San Giovanni di Dio e Ruggi d´Aragona, Salerno, Italy.
Joon-Chui Jung, Department of Thoracic and Cardiovascular Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
Frieda-Maria Kainz, Department of Cardiac Surgery, University Hospital St. Poelten, St. Poelten, Austria.
Athanasios Katsargyris, Department of Vascular and Endovascular Surgery, Paracelsus Medical University Nuremberg, Nuremberg, Germany.
Stephan Koter, Department of Cardiovascular and Endovascular Surgery, Paracelsus Medical University Salzburg, Salzburg, Austria.
Mariusz Kusmierczyk, Department of Cardiac Surgery and Transplantation, The Cardinal Stefan Wyszynski National Institute of Cardiology, Warsaw, Poland.
Piotr Kolsut, Department of Cardiac Surgery and Transplantation, The Cardinal Stefan Wyszynski National Institute of Cardiology, Warsaw, Poland.
Balazs Lengyel, Department of Vascular and Endovascular Surgery, Semmelweis University, Budapest, Hungary.
Chiara Lomazzi, Unita Operativa di Chirurgia Vascolare, Fondazione IRCCS Ca Granda Ospedale Maggiore Policlinico Milan, Milan, Italy; Department of Clinical and Community Sciences, University of Milan, Milan, Italy.
Claudio Muneretto, Division of Cardiac Surgery, University of Brescia Medical School, Brescia, Italy.
Giovanni Nava, Cardiovascular Department, IRCCS-Policlinico San Donato, Milan, Italy.
Thomas Nolte, Department of Vascular Surgery, HGZ Bad Bevensen, Bad Bevensen, Germany.
Davide Pacini, Department of Cardiac Surgery, Hospital Santa Orsola, University of Bologna, Bologna, Italy.
Eliza Pleban, Department of Vascular Surgery, Institute of Hematology and Transfusion Medicine, Warsaw, Poland.
Miriam Rychla, Department for Vascular Surgery, University Hospital Zurich, Zurich, Switzerland.
Kazuhisa Sakamoto, Department of Cardiovascular Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan.
Takayuki Shijo, Department of Cardiovascular Surgery, National Cerebral and Cardiovascular Center, Osaka, Japan.
Koki Yokawa, Department of Cardiovascular Surgery, National Cerebral and Cardiovascular Center, Osaka, Japan.
Matthias Siepe, Department for Cardiovascular Surgery, University Heart Center Freiburg-Bad Krozingen, Freiburg, Germany; Faculty of Medicine, Albert-Ludwigs-University Freiburg, Freiburg, Germany.
Joachim Sirch, Department of Cardiac Surgery, Paracelsus Medical University Nuremberg, Nuremberg, Germany.
Justus Strauch, Department of Cardiothoracic Surgery, University Hospital Bergmannsheil Bochum, Ruhr University of Bochum, Bochum, Germany.
Jai Ajitchandra Sule, Department of Cardiac, Thoracic and Vascular Surgery, National University Hospital, National University Health System, Singapore.
Eva-Luca Tobler, Department of Cardiovascular Surgery, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Corinna Walter, Department of Vascular Surgery, Clinic Ottakring.
Ernst Weigang, Department of Vascular and Endovascular Surgery, Hubertus Hospital Berlin, Berlin, Germany.
REFERENCES
- 1. Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020;396:381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH et al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020;383:691–3. [DOI] [PubMed] [Google Scholar]
- 4. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R et al. ; On behalf of the Lombardia CARe researches. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J 2020;41:3045–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Herz N. Why are thousands fewer people being treated for a heart attack? 2020. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/behind-the-headlines/coronavirus/coronavirus-and-reduction-in-heart-attack-treatment (23 April 2020, date last accessed).
- 6. Seiffert M, Brunner FJ, Remmel M, Thomalla G, Marschall U, ĹHoest H et al. Temporal trends in the presentation of cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany: an analysis of health insurance claims. Clin Res Cardiol 2020;4:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leshem E, Klein Y, Haviv Y, Berkenstadt H, Pessach IM. Enhancing intensive care capacity: COVID-19 experience from a tertiary center in Israel. Intensive Care Med 2020;46:1640–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in northern Italy. N Engl J Med 2020;383:88–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zafar MA, Li Y, Rizzo JA, Charilaou P, Saeyeldin A, Velasquez CA, Mansour AM et al. Height alone, rather than body surface area, suffices for risk estimation in ascending aortic aneurysm. J Thorac Cardiovasc Surg 2018;155:1938–50. [DOI] [PubMed] [Google Scholar]
- 10. Valdivia AR, San Norberto E, Moreno R, Salmerón Febres LM, Miralles M, López IM et al. ; RIV “Red de Investigacion Vascular de la SEACV”. Massive drop in elective and urgent aortic procedures during the peak of the COVID-19 outbreak in Spanish multicenter analysis. J Vasc Surg 2020; doi:S0741-5214:31910–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. El-Hamamsy I, Brinster DR, DeRose JJ, Girardi LN, Hisamoto K, Imam MN et al. H. The COVID-19 pandemic and acute aortic dissections in New York: a matter of public health. J Am Coll Cardiol 2020;76:227–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases—document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult—the task force for the diagnosis and treatment of aortic diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2873–926. [DOI] [PubMed] [Google Scholar]
- 13. Kwok CS, Gale CP, Kinnaird T, Curzen N, Ludman P, Kontopantelis E et al. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart 2020;106:1805–7. [DOI] [PubMed] [Google Scholar]