Abstract
Severe respiratory sequelae drive morbidity-associated with coronavirus 2019 (COVID-19) disease. We report a case of COVID-19 pneumonia complicated by cavitary lesions and pneumothorax in a young healthy male. Pneumothorax management with catheter thoracostomy and rapid resolution of the cavitary lesions are described. An extensive work-up for other causes a cavitation was negative and the temporal correlation of the cavities with COVID-19 infection plus their rapid resolution suggest a direct relationship. We propose a mechanism for cavitation secondary to microangiopathy, a cause of cavitation in the vasculitides and a known feature of COVID-19.
Keywords: Coronavirus, Covid-19, Cavitary
CASE REPORT
A 35-year-old male presented to our Emergency Department on 21 April with chest pain and scant haemoptysis. On April 8, he had a positive coronavirus 2019 (COVID-19) nasopharyngeal swab and reverse-transcription polymerase chain reaction of the ORF1ab gene using the Panther Aptima® SARS-CoV-2 assay (Hologic, Marlborough, MA, USA). His initial symptoms of fever, cough and fatigue resolved after several days at home without medications. He was previously healthy and denied family history of pulmonary disease. He endorsed rare alcohol consumption but denied tobacco or illicit drug use. He denied exposures to moulds, tuberculosis or atypical bacterial infections. He was afebrile, with a benign examination. Laboratories were unremarkable (Supplementary Material, Table S1). A chest roentgenogram (CXR) demonstrated bilateral airspace disease (Supplementary Material, Fig. S1a). He was discharged from the Emergency Department. A computed tomography angiography (CTA), obtained the next day due to pain, demonstrated a right-sided pneumothorax as well as right lower lobe (RLL), right upper lobe (RUL) and left lower lobe (LLL) cavities (Supplementary Material, Fig. S1b and Fig. 1a and b). A 14-Fr catheter thoracostomy expanded the lung (Supplementary Material, Fig. S2a). After 48 h of −20 cmH2O suction and 24 h of water seal, the lung remained expanded. The catheter was removed (Supplementary Material, Fig. S2b).
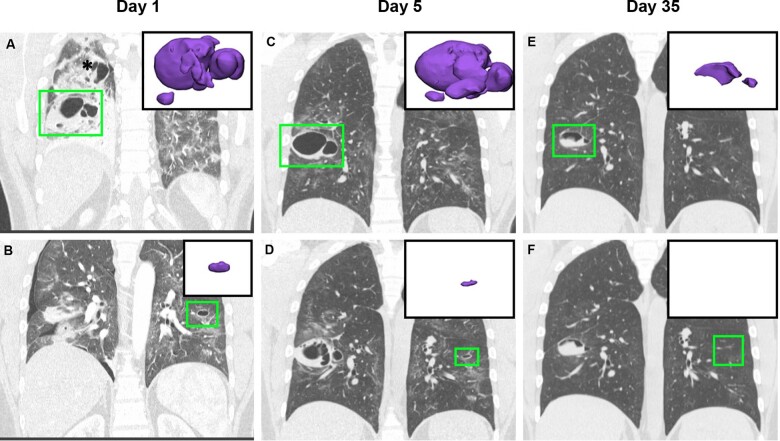
Figure 1:
Cavitary changes. (A) CTA thorax day 1: right lower lobe cavity (green box) and 3D rendering (purple, inset). Asterisk indicates right upper lobe cavity. (B) CTA thorax day 1: left lower lobe cavitary lesion and 3D model. (C) CT thorax day 5: right lower lobe cavity and 3D model in expanded lung. (D) CT thorax day 5: decreased left lower lobe cavity with 3D model. (E) CT thorax day 35: right lower lobe cavity and 3D model. (F) CT thorax day 35: Resolution of left lower lobe cavity. Note: green boxes indicate cavities. 3D models (purple) are scaled for comparison between panels.
Repeat CT imaging on 27 April and analysis with three-dimensional modelling (Mimics, 3-matic; Materialise, Leuven, Belgium) demonstrated cavity volume changes (Fig. 1a–d, Supplementary Material, Fig. S3a and b and Supplementary Material, Table S2). While the pneumothorax confounds comparison of the initial RLL cavity size to the cavity size in the re-expanded lung (Supplementary Material, Table S2), a slight increase was noted. The RUL lesion was more complex but decreased in size (Supplementary Material, Fig. S3a and b and Supplementary Material, Table S2). The LLL cavity clearly decreased (Fig. 1b and d and Supplementary Material, Table S2). After a negative infectious work-up, the patient discharged on 27 April 2020 (Table 1). He underwent CT on 27 May 2020 for mild dyspnoea but required no interventions. The CT revealed a markedly decreased RLL cavity and LLL cavity resolution (Fig. 1e and f and Supplementary Material, Table S2). Scheduled imaging on 15 June 2020 demonstrated continuing RLL cavity resolution and a tiny new RUL cavity (Supplementary Material, Fig. S4a and b and Supplementary Material, Table S2). In addition, he underwent pulmonary function testing on 16 June 2020, which was unremarkable (Supplementary Material, Fig. S5). He is currently doing well and has scheduled follow-up.
Table 1.
Infectious disease work-up
| Test | Outcome |
|---|---|
| COVID-19 nasopharyngeal swab RT-PCR | Positive |
| Blood culture | Coag-negative staphylococcus (20.6 h)a |
| Repeat blood cultures | No growth |
| AFB culture | No growth |
| AFB smear | Negative |
| Quantiferon-Tb Gold | Negative |
| Blastomyces Ag | Negative |
| Histoplasma Ag | Negative |
| Cryptococcal Ag | Negative |
| Coccidioides Ag | Negative |
| Beta-1,3-glucan | Negative |
| Galactomannan | Negative |
| Legionella urinary Ag | Negative |
| Strep pneumoniae Ag | Negative |
| HIV Ab/Ag combo | Negative |
| Repeat COVID-19 nps PCR (17 and 26 days after initial) | Positive |
COVID-19: coronavirus 2019; coag: coagulase; RT-PCR: reverse-transcription polymerase chain reaction.
A single blood culture was positive for coag-negative staphylococcus at 20.6 h and was considered a contaminant by our Infectious Disease colleagues.
DISCUSSION
Cavitary lung disease caused by COVID-19 viral pneumonia has not been described [1, 2]. Cavitary lung disease has many causes, including infectious, neoplastic, vasculitides and congenital. Our rigorous work-up excluded many aetiologies for cavitary disease. There was no evidence for neoplasm and rapid changes are not consistent with congenital aetiologies. No chest imaging exists prior to his presentation in April, making it difficult to exclude pre-existing subclinical pulmonary disease with absolute certainty. The extensive negative work-up, temporal correlation between the cavities and COVID-19 infection and rapid cavity resolution suggest a direct link between cavitation and COVID-19 infection. Our patient had positive repeat COVID-19 nasopharyngeal swab/reverse-transcription polymerase chain reaction tests 17 and 26 days after his initial positive test. Zheng et al. [3] recently reported that more severe pulmonary complications were associated with higher viral loads and a longer duration of COVID-19 infection. Could our patient’s positive repeat COVID-19 tests represent prolonged infection causing pulmonary complications?
If COVID-19 infection directly caused the cavities, what is the mechanism? Ackermann et al. [4] reported microvascular pulmonary endothelialitis in COVID-19 autopsies. Small-vessel vasculitis represents a known aetiology for cavitation [5]. It is tempting to speculate that the microangiopathy known to occur in COVID-19 infection could represent a plausible mechanism for cavitary lesions in our patient.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTSonline.
Conflict of interest: none declared.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Clemens Aigner and René Horsleben Petersen for their contribution to the peer review process of this article.
Supplementary Material
ACKNOWLEDGEMENT
We thank Alejandro Roldan-Alzate for image analysis suggestions.
REFERENCES
- 1. Kanne JP. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology 2020;295:16–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myers L. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and middle east respiratory syndrome. Am J Roentgenol 2020;214:1078–82. [DOI] [PubMed] [Google Scholar]
- 3. Zheng S, Fan J, Yu F, Feng B, Lou B, Zou Q et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January. Retrospective cohort study. BMJ 2020;369:m1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 2020;383:120–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown KK. Pulmonary vasculitis. Proc Am Thorac Soc 2006;3:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.