Abstract
Background
We estimated population-level associations between ethnicity and coronavirus disease 2019 (COVID-19) mortality using a newly linked census-based data set and investigated how ethnicity-specific mortality risk evolved during the pandemic.
Methods
We conducted a retrospective cohort study of respondents to the 2011 Census of England and Wales in private households, linked to death registrations and adjusted for emigration (n = 47 872 412). The outcome of interest was death involving COVID-19 between 2 March 2020 and 15 May 2020. We estimated hazard ratios (HRs) for ethnic-minority groups compared with the White population, controlling for individual, household and area characteristics. HRs were estimated on the full outcome period and separately for pre- and post-lockdown periods.
Results
In age-adjusted models, people from all ethnic-minority groups were at elevated risk of COVID-19 mortality; the HRs for Black males and females were 3.13 (95% confidence interval: 2.93 to 3.34) and 2.40 (2.20 to 2.61), respectively. However, in fully adjusted models for females, the HRs were close to unity for all ethnic groups except Black [1.29 (1.18 to 1.42)]. For males, the mortality risk remained elevated for the Black [1.76 (1.63 to 1.90)], Bangladeshi/Pakistani [1.35 (1.21 to 1.49)] and Indian [1.30 (1.19 to 1.43)] groups. The HRs decreased after lockdown for all ethnic groups, particularly Black and Bangladeshi/Pakistani females.
Conclusion
Differences in COVID-19 mortality between ethnic groups were largely attenuated by geographical and socio-demographic factors, though some residual differences remained. Lockdown was associated with reductions in excess mortality risk in ethnic-minority populations, which has implications for a second wave of infection.
Keywords: COVID-19, coronavirus, ethnicity, BAME, social determinants of health, census, mortality
Introduction
Coronavirus disease 2019 (COVID-19) is a serious infectious disease originally reported in China in December 2019, caused by novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). More than 660 000 deaths attributable to COVID-19 have been reported worldwide and, in the UK alone, >50 000 death registrations have mentioned COVID-191 and >130 000 people have been hospitalized with the disease2 as of 29 July 2020. As the pandemic has evolved, a growing body of evidence has emerged on the clinical risk factors associated with COVID-19 infection, hospitalization and death, including age, sex, obesity and chronic conditions including diabetes, hypertension, lung disease and cardiovascular disease.3–5 However, evidence also suggests that socio-economic factors may be drivers of variations in COVID-19 morbidity and mortality.6 For instance, COVID-19-related mortality in England and Wales is nearly twice the rate in the most deprived areas compared with the least deprived,7 with the highest mortality rates among working-age people observed among those working in elementary occupations or social care.8
Key Messages
Several studies suggest that the risk of adverse outcomes of COVID-19 is elevated for Black, Asian and minority-ethnic groups compared with the White population, but results pertaining to which ethnic groups are at greatest risk are mixed and depend on the data sources used and the covariates adjusted for.
To date, there is no published evidence on the association between lockdown measures and ethnic inequalities in adverse outcomes of COVID-19.
By linking population-level census data for England and Wales to death registrations, we found the elevated risk of COVID-19 mortality for ethnic-minority groups to be largely driven by location, living circumstances, socio-economic factors, occupational exposure and self-reported health status.
Differences in mortality rates between ethnic groups were considerably reduced following the introduction of lockdown measures, with the Black population experiencing the greatest fall in mortality rates.
In the event of a second wave of infection or local spikes in incidence, restricting freedom of movement and activity may reduce the inequality in mortality rates between ethnic groups.
Heterogeneity in health status between ethnic groups has been well documented across multiple countries over the course of a number of decades.9 As the 2009 A(H1N1) influenza pandemic disproportionately affected ethnic-minority groups in England,10 the relationship between ethnicity and COVID-19 outcomes is of substantial interest, particularly in England and Wales, where 14% of the population reported being of non-White ethnicity at the last decennial census in 2011. Existing evidence indicates that the risk of hospitalization and death due to COVID-19 in the UK is elevated for Black, Asian and minority-ethnic (BAME) individuals compared with the White population.3,11,12 However, the magnitude of the association varies depending on the data sources used and the covariates adjusted for,13 and little is known about the mechanisms driving differences in the risk of COVID-19-related death across ethnic groups.
The present study makes three important contributions to the research into ethnic disparities in COVID-19 outcomes. First, we used microdata from the 2011 Census of England and Wales and linked death registrations to investigate, at a population level, the association between ethnicity and COVID-19-related mortality risk. Second, we exploited a broad range of structural factors related to geography, household composition, occupation and socio-economic position available in the 2011 Census, often associated with ethnic inequality in health status, to investigate whether these factors mediate the relationship between ethnicity and COVID-19-mortality risk. Third, we examined how the relative risk of COVID-19 mortality between White and ethnic-minority groups has evolved over the course of the pandemic, focusing on the periods before and after the ‘lockdown’ restrictions on freedom of activity were announced by the UK government.
Methods
Study design and data
In this observational, retrospective cohort study, the study population included all usual residents of England and Wales enumerated in private households (not communal establishments) at the time of the 2011 Census (27 March 2011) who had not died before 2 March 2020. We excluded individuals who entered the UK during the year before the census due to their high propensity for having left the UK prior to the study period and those aged >100 years at the time of the census.
We did not include post-2011 births and immigrants; these groups are not captured in the 2011 Census and therefore have no ethnicity or covariate data recorded. For the same reason, individuals not enumerated in the 2011 Census (estimated to be 6.1% of the population of England and Wales14) were not included in our study population. Our study population therefore consisted of 47 872 412 individuals aged ≥9 years on 2 March 2020 (the youngest possible, given the 9-year lag from enumeration at the 2011 Census).
We linked the 2011 Census to the 2011–2013 NHS Patient Registers to obtain NHS Numbers, with a linkage rate of 94.6% (for further details on Census to Patient Register linkage rates by characteristics of interest, see the Supplementary Appendix, available as Supplementary data at IJE online ). Deaths were then linked to the study data set using NHS Number, achieving linkage rates of 89.9% of deaths between 27 March 2011 and 1 March 2020, and 90.8% of those between 2 March 2020 and 15 May 2020 that were registered by 29 May 2020.
Throughout the analysis, we applied weights reflecting the probability of having remained in the country between March 2011 and March 2020, based on data from the NHS Patient Register and the International Passenger Survey. For further information on the methodology for adjusting for emigration, see the Supplementary Appendix, available as Supplementary data at IJE online. .
Outcome and exposure
Our outcome of interest was death involving COVID-19, between 2 March 2020 and 15 May 2020, registered by 29 May 2020. Deaths involving COVID-19 included those with an underlying cause, or any mention, of ICD-10 codes U07.1 (COVID-19, virus identified) or U07.2 (COVID-19, virus not identified). Time at risk started on 2 March 2020 and ran until 15 May 2020 or date of death.
Our exposure of interest was self-reported ethnic affiliation. Ethnic breakdown was based on the census ethnicity question, with some groups collapsed to ensure that outcome counts were large enough to reliably estimate hazard ratios (HRs) (see Supplementary Table 1, available as Supplementary data at IJE online). The White ethnic group was used as the reference category in all models. Ethnicity was imputed in 3.0% of 2011 Census returns due to item non-response using nearest-neighbour donor imputation, the methodology employed by the Office for National Statistics across all 2011 Census variables.15
Covariates
We controlled for geographical and socio-demographic factors that may be associated with the risk of COVID-19 mortality (Table 1), through either the propensity to become infected or the propensity to die once infected (which could not be distinguished using the data available for this study).
Table 1.
Covariates included in the Cox-regression models
| Variable | Coding |
|---|---|
| Age variables | |
| Single year of age | Second-order polynomial |
| Geographical variables | |
| Local-authority district | Dummy variables representing local-authority districts |
| Population density of Lower Super Output Area (LSOA) | Second-order polynomial, allowing for a different slope beyond the 99th percentile of the distribution to account for extreme values |
| Socio-economic variables | |
| Index of Multiple Deprivation (IMD), Welsh Index of Multiple Deprivation (WIMD)16,17 | Dummy variables representing deciles of deprivation |
| Household deprivation (see table note) | Not deprived, deprived in one dimension, deprived in two dimensions, deprived in three dimensions, deprived in four dimensions |
| Household tenure | Own outright, own with mortgage, social rented, private rented, other |
| National Statistics Socio-Economic Classification (NS-SEC) of household head | Higher managerial, administrative & professional occupations, intermediate occupations, routine & manual occupations, never worked, not applicable (aged ≥75 years) |
| Level of highest qualification | Degree, A-level or equivalent, GCSE or equivalent, no qualification |
| Household variables | |
| Household size | 1 or 2 people, 3 or 4 people, 5 or 6 people, 7+ people |
| Family type | Not a family, couple with children, lone parent |
| Multigenerational household | Three or more generations living together, other |
| Household with children | At least one child aged 18 years or under, other |
| Health-related variables | |
| Self-reported health status | Very good, good, fair, poor, very poor |
| Self-reported disability status | Not disabled, daily activity limited a lot, daily activity limited a little |
| Occupational-exposure variables | |
| Key-worker type | Education & childcare, food & necessity goods, health & social care, public services, national & local government, public safety & national security, transport, utilities & communication, not a key worker |
| Key worker in the household | Yes, no |
| Exposure to disease | Score ranging from 0 (no exposure) to 100 (maximum exposure), derived from O*NET data18 |
| Proximity to others | Score ranging from 0 (no exposure) to 100 (maximum exposure), derived from O*NET data18 |
| Household exposure to disease | Maximum ‘exposure to disease’ score within each household |
| Household proximity to others | Maximum of ‘proximity to others’ score within each household |
Household deprivation is defined according to four dimensions: employment (at least one household member is unemployed or long-term sick, excluding full-time students); education (no household members have at least Level 2 education and no one aged 16–18 years is a full-time student); health and disability (at least one household member reported their health as being ‘bad’/‘very bad’ or has a long-term health problem); and housing (the household’s accommodation is overcrowded, with an occupancy rating of –1 or less, or is in a shared dwelling, or has no central heating). Key-worker type is defined based on the occupation and industry code. ‘Exposure to disease’ and ‘proximity to others’ are derived from the O*NET database, which collects a range of information about individuals’ working conditions and day-to-day tasks of their job. To calculate the proximity and exposure measures, the questions asked were: (i) How physically close to other people are you when you perform your current job? (ii) How often does your current job require that you be exposed to diseases or infection? Scores ranging from 0 (no exposure) to 100 (maximum exposure) were calculated based on these questions using methods previously described by the Office for National Statistics [18].
Statistical analyses
Age-standardized mortality rates
We calculated age-standardized mortality rates (ASMRs) for the different ethnic groups as a measure of differences in absolute risk of COVID-19 mortality, whereby the age-by-sex distribution within each group was standardized to the overall distribution in the study population.
Cox-proportional-hazard models
We used Cox-proportional-hazard models to assess whether differences in the risk of COVID-19-related death across ethnic groups could be accounted for by the factors listed in Table 1. When fitting the Cox models, we included all individuals who died during the analysis period and a weighted 1% random sample of those who did not.
We estimated separate models for males and females, as the risk of death involving COVID19 differs markedly by sex.3 We estimated models that only adjusted for age before adding groups of control variables step by step and assessing how these affected the estimated HRs. First, because exposure to the disease is likely to vary across geographical areas, we adjusted for population density as a covariate and allowed for different baseline hazards for each local-authority district (LAD). Second, we adjusted for a range of measures of socio-economic position, as they may be associated with the risk of infection. Third, we adjusted for household composition, as it is likely to be linked to the risk of infection, especially for the elderly; e.g. living in multigenerational household may increase the risk of exposure to the virus among vulnerable people. Fourth, we adjusted for occupational exposure to capture the differential risks of infection across occupations. Finally, we adjusted for self-reported measures of health, which could affect mortality either through increased exposure to the virus or worsening of the prognosis.
Assessing the proportional-hazards assumption
We used Schoenfeld residuals from the fitted Cox models, smoothed using generalized additive models, to assess whether relative differences in the hazard of COVID-19 mortality between the ethnic groups changed over the course of the pandemic.19
To address potential non-proportionality in hazards between the White and ethnic-minority groups, we allowed for time-dependent ethnicity coefficients in our Cox models by stratifying on pre- and post-lockdown periods. We selected 23 March 2020 (the date on which legally enforceable restrictions to freedom of activity were announced by the UK government) plus 3 weeks (to allow for a lag between lockdown coming into force and its impact on mortality rates) as a landmark date by which to divide individuals’ follow-up time. In sensitivity analysis, we investigated the impact on the estimated HRs of varying the 21-day lag duration by ±7 days.
All statistical analyses were conducted using R version 3.5.20
Results
Characteristics of the study population
In our study population of 47 872 412 usual residents in England and Wales in 2011 who were still alive on 2 March 2020, just over half (51.6%) were female, the mean age was 47 years and 86.4% reported being from a White ethnic background (Table 2). Over the outcome period (2 March 2020 to 15 May 2020), the mean follow-up time was 73.9 days (standard deviation 2.2 days) and 37 956 individuals (0.08%) died of COVID-19.
Table 2.
Distributions of study variables, stratified by White/non-White ethnicity
| Variable | Level | All people | White | Non-White | Cohen’s d |
|---|---|---|---|---|---|
| Age (years) | Mean | 46.5 | 47.8 | 38.1 | 0.45 |
| Sex | Male | 48.4% | 48.5% | 48.4% | 0.00 |
| Female | 51.6% | 51.5% | 51.6% | 0.00 | |
| Ethnicity | White | 86.4% | – | – | – |
| Bangladeshi and Pakistani | 3.0% | – | – | – | |
| Black | 3.2% | – | – | – | |
| Chinese | 0.6% | – | – | – | |
| Indian | 2.6% | – | – | – | |
| Mixed | 2.1% | – | – | – | |
| Other | 2.2% | – | – | – | |
| Population density (people per square kilometre) | Mean | 4424 | 3829 | 8211 | 1.00 |
| National Statistics Socio-Economic Classification (NS-SEC) of household head | Higher managerial, administrative and professional occupations | 30.7% | 31.4% | 26.2% | 0.11 |
| Intermediate occupations | 18.7% | 18.6% | 19.2% | 0.01 | |
| Routine and manual occupations | 25.9% | 26.0% | 25.4% | 0.01 | |
| Never worked, unemployed, Not elsewhere classified | 2.9% | 2.4% | 6.5% | 0.25 | |
| Not applicable | 21.8% | 21.6% | 22.7% | 0.03 | |
| Tenure of household | Owned outright | 24.3% | 25.7% | 15.4% | 0.24 |
| Owned with a mortgage | 42.6% | 43.4% | 37.1% | 0.13 | |
| Shared ownership | 0.7% | 0.7% | 0.8% | 0.02 | |
| Social rented from council | 8.2% | 7.6% | 12.0% | 0.16 | |
| Other social rented | 7.1% | 6.6% | 10.2% | 0.14 | |
| Private rented | 16.2% | 15.1% | 23.0% | 0.21 | |
| Living rent-free | 1.0% | 0.9% | 1.5% | 0.06 | |
| Level of highest qualification | No qualification | 15.4% | 16.0% | 11.9% | 0.11 |
| Level 1: 1–4 GCSE/O-Level | 11.2% | 11.7% | 8.5% | 0.10 | |
| Level 2: 5+ GCSE/O levels | 12.8% | 13.5% | 8.8% | 0.14 | |
| Apprenticeship | 2.9% | 3.2% | 0.7% | 0.15 | |
| Level 3: 2+ A Levels or equivalent | 10.1% | 10.5% | 7.5% | 0.10 | |
| Level 4+: degree or above | 22.9% | 22.8% | 23.9% | 0.03 | |
| Other | 4.4% | 3.7% | 8.8% | 0.24 | |
| Aged 16 years or under/full-time student | 20.2% | 18.6% | 29.9% | 0.28 | |
| Index of Multiple Deprivation (IMD), Welsh Index of Multiple Deprivation (WIMD) | Decile 1 | 9.7% | 8.2% | 19.2% | 0.38 |
| Decile 2 | 9.8% | 8.5% | 18.1% | 0.33 | |
| Decile 3 | 9.9% | 9.2% | 14.8% | 0.19 | |
| Decile 4 | 9.9% | 9.7% | 11.4% | 0.06 | |
| Decile 5 | 10.0% | 10.1% | 9.3% | 0.03 | |
| Decile 6 | 10.1% | 10.5% | 7.3% | 0.11 | |
| Decile 7 | 10.1% | 10.8% | 5.7% | 0.17 | |
| Decile 8 | 10.1% | 10.9% | 5.1% | 0.19 | |
| Decile 9 | 10.2% | 11.1% | 4.6% | 0.21 | |
| Decile 10 | 10.2% | 11.1% | 4.5% | 0.22 | |
| Multigenerational household | Yes | 5.5% | 5.0% | 9.1% | 0.18 |
| No | 94.5% | 95.0% | 90.9% | 0.18 | |
| Child in household | Yes | 49.8% | 47.0% | 67.2% | 0.41 |
| No | 50.2% | 53.0% | 32.8% | 0.41 | |
| Household size | 1 or 2 people | 39.7% | 42.4% | 22.4% | 0.41 |
| 3 or 4 people | 44.2% | 44.4% | 42.5% | 0.04 | |
| 5 or 6 people | 14.1% | 12.0% | 27.2% | 0.44 | |
| 7+ people | 2.1% | 1.1% | 7.9% | 0.48 | |
| Family status | Not in a family | 15.6% | 15.7% | 14.7% | 0.03 |
| In a couple family | 71.0% | 71.7% | 66.5% | 0.11 | |
| In a lone-parent family | 13.5% | 12.6% | 18.8% | 0.18 | |
| Key-worker type | Not key worker | 84.4% | 83.8% | 88.0% | 0.11 |
| Education and childcare | 4.6% | 4.9% | 2.5% | 0.11 | |
| Food and necessary goods | 0.8% | 0.8% | 0.5% | 0.02 | |
| Health and social care | 5.5% | 5.5% | 5.8% | 0.02 | |
| Key public services | 1.2% | 1.2% | 0.8% | 0.02 | |
| National and local government | 0.6% | 0.6% | 0.4% | 0.03 | |
| Public safety and national security | 1.2% | 1.3% | 0.5% | 0.08 | |
| Transport | 0.9% | 0.9% | 0.6% | 0.04 | |
| Utilities and communication | 1.0% | 1.0% | 0.9% | 0.02 | |
| Key worker in household | Yes | 15.9% | 16.5% | 12.3% | 0.06 |
| No | 84.1% | 83.8% | 87.7% | 0.06 | |
| Exposure to disease score (0–100) | Mean (individual) | 14.7 | 15.0 | 12.8 | 0.11 |
| Mean (household) | 28.7 | 28.4 | 30.5 | 0.09 | |
| Proximity to others score (0–100) | Mean (individual) | 45.4 | 46.9 | 35.5 | 0.38 |
| Mean (household) | 67.8 | 67.9 | 67.1 | 0.05 | |
| Self-reported health status | Very good | 49.7% | 49.2% | 53.% | 0.08 |
| Good | 35.0% | 35.2% | 33.6% | 0.03 | |
| Fair | 11.5% | 11.7% | 9.7% | 0.06 | |
| Poor | 3.1% | 3.1% | 2.8% | 0.02 | |
| Very poor | 0.7% | 0.7% | 0.8% | 0.01 | |
| Long-term health problem or disability | Daily activities not limited | 86.1% | 85.6% | 89.4% | 0.11 |
| Daily activities limited a little | 5.6% | 5.8% | 4.6% | 0.05 | |
| Daily activities limited a lot | 8.3% | 8.7% | 5.9% | 0.10 |
Study population consists of usual residents in England and Wales in 2011 who were still alive on 2 March 2020, down weighted to account for emigration over this period. Summary statistics calculated on all individuals who died and a 1% random sample of those who did not die, weighted to represent the full study population. Cohen’s d is a measure of effect size between the White and non-White populations. Values of d = 0.2, d = 0.5 and d = 0.8 are indicative of ‘small’, ‘medium’ and ‘large’ effect sizes, respectively.21
Compared with the White population, individuals in the non-White group: had a lower mean age; tended to reside in more densely populated areas; were more likely to have never worked or be unemployed; were less likely to own their own home and more likely to rent; were more likely to live in a deprived neighbourhood; and were more likely to live in a larger household.
Risk of COVID-19 mortality by ethnicity
For both males and females, the ASMRs of COVID-19 mortality (see Supplementary Table 2, available as Supplementary data at IJE online) were greatest among individuals identifying as Black (250.6 and 116.9 deaths per 100 000 people, respectively) and lowest among those identifying as White (87.3 and 51.8 deaths per 100 000 people, respectively). Levels of absolute risk were greater among all ethnic-minority groups compared with the White population.
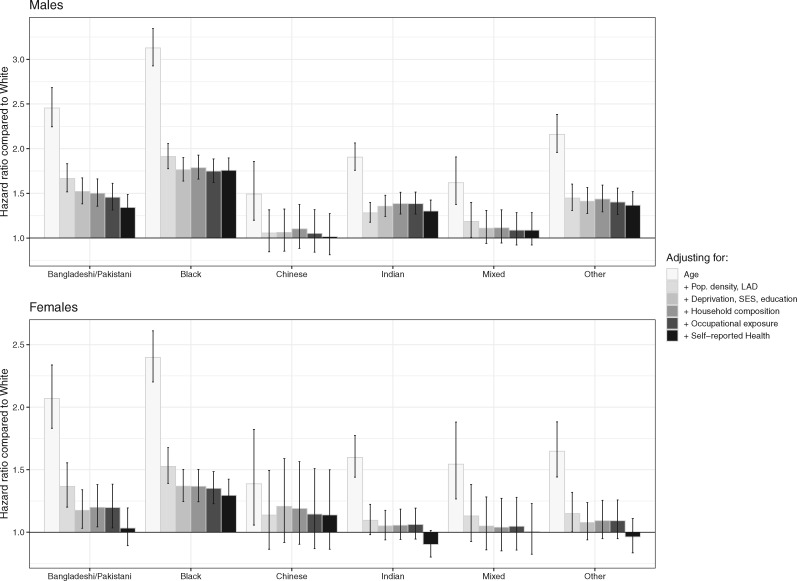
Similarly, age-adjusted HRs indicated that males and females from all ethnic-minority groups (except females of Chinese ethnicity) were at greater risk of death involving COVID-19 compared with those of White ethnicity (Figure 1, Model 1). The rate of death involving COVID-19 was 3.13 (95% confidence interval [CI]: 2.93–3.34) times greater for Black males than for White males, and 2.40 [2.20–2.61] times greater for Black females than White females. People of Bangladeshi/Pakistani, Indian, Mixed and Other ethnic backgrounds also had raised rates of death involving COVID-19 compared with those of White ethnicity.
Figure 1.
Hazard ratios for COVID-19 related death for ethnic-minority groups compared with the White population, stratified by sex. Results obtained from Cox-regression models adjusted for age, population density, area and household deprivation, socio-economic status (SES), household composition, occupational exposure, self-reported health, with baseline hazards specific to local-authority district (LAD). Error bars represent limits of 95% confidence intervals of the hazard ratio. Details of the covariates can be found in Table 1. Numerical results can be found in Supplementary Tables 3 and 4, available as Supplementary data at IJE online.
For females, the characteristics in the fully adjusted model statistically explained the differences in risk compared with the White population for all ethnic-minority groups except those of Black ethnicity, as their hazard ratio remained at 1.29 [1.17–1.42] after adjustment. Adjusting for these characteristics also reduced the estimated HRs for males, but they remained larger than one for all groups other than Chinese and Mixed ethnic backgrounds. Compared with White males, the rate of death involving COVID-19 was 1.77 [1.64–1.91] times greater for Black males, 1.35 [1.22–1.50] times greater for Bangladeshi and Pakistani males, and 1.31 [1.19–1.43] times greater for Indian males.
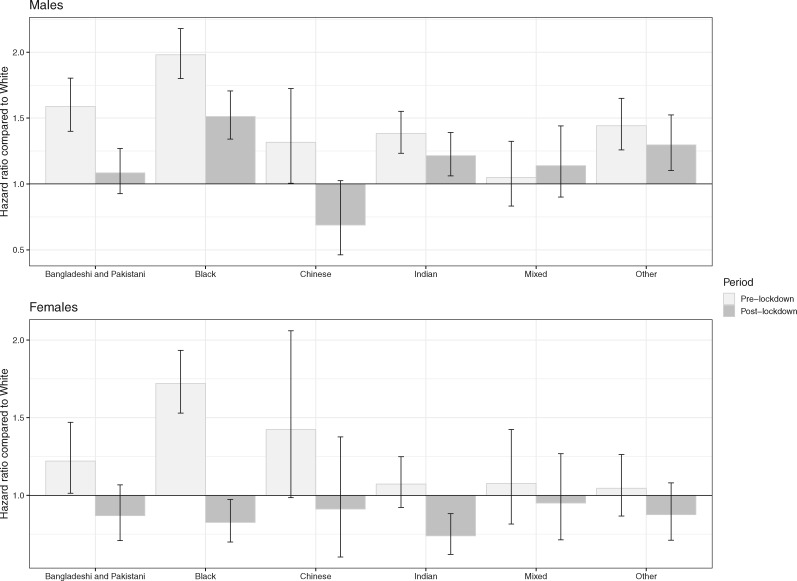
Risk of COVID-19 mortality before and after lockdown
The smoothed Schoenfeld residuals by ethnic group (see Supplementary Figures S1 and S2, available as Supplementary data at IJE online) indicated a non-constant hazard ratio of deaths involving COVID-19 over the course of the pandemic for some groups. For the Bangladeshi/Pakistani and Chinese groups for males and the Black group for females, the log HRs tended to zero midway through the outcome period, indicating diminished differences in risk between these ethnic-minority groups and the White population.
The ASMRs decreased after lockdown for males of all ethnic-minority groups, most notably by 61.8 deaths per 100 000 of the Black population, but increased by 12.1 deaths per 100 000 of the White population (Supplementary Table S5, available as Supplementary data at IJE online). Similar patterns were observed for females, with ASMRs after lockdown decreasing by 42.4 deaths per 100 000 of the Black population but increasing by 13.3 deaths per 100 000 of the White population.
In our time-stratified, fully adjusted Cox models for females (Figure 2), the rate of mortality involving COVID-19 was elevated for the Bangladeshi/Pakistani and Black groups compared with the White population over the pre-lockdown period, with HRs of 1.22 [1.01–1.47] and 1.72 [1.53–1.93] respectively. After the lockdown, the HRs decreased to 0.87 [0.71–1.07] for the Bangladeshi/Pakistani population and 0.83 [0.70–0.97] for the Black population. For males, the Black, Indian and Other ethnic-minority groups continued to experience a greater rate of COVID-19 mortality than the White population, but with reduced HRs.
Figure 2.
Fully adjusted hazard ratios for COVID-19-related death for ethnic-minority groups compared with the White population, before and after lockdown plus 21 days, stratified by sex. Results obtained from a Cox-regression model adjusted for age, population density, deprivation, SES, household composition, occupational exposure, self-reported health, with baseline hazards specific to LAD. Errors bars represent limits of 95% confidence intervals of the hazard ratio. Estimates for each ethnic group are stratified by a time variable indicating pre- and post-lockdown periods.
Results obtained using shorter and longer lag durations for capturing post-lockdown deaths (14 and 28 days instead of 21 days) were similar to those in the main analysis, although less precisely estimated (see Supplementary Figures S3 and S4, available as Supplementary data at IJE online).
Discussion
Principal findings
Firstly, using population-level data we observed a substantially elevated risk of COVID-19 related death among ethnic-minority groups. Secondly, this elevated risk was largely attenuated by location, living circumstances, socio-economic factors, occupational exposure and self-reported health status. Thirdly, differences in COVID-19-mortality rates between ethnic groups were considerably reduced following the introduction of lockdown measures in the UK.
Comparison with related studies
Our finding that ethnic-minority groups were at greater risk of COVID-19 related death compared with the White population is broadly consistent with other UK-based research published to date. An analysis of laboratory confirmed cases of COVID-19 in England found that some, but not all, ethnic-minority groups were at greater risk of death after adjusting for demographics and deprivation, with Black and Asian groups having the greatest mortality rates.12 However, the tested sample is unlikely to be representative of the general population. A retrospective study of electronic primary-care records covering ∼40% of patients in England found elevated COVID-19-mortality risk for Black and South Asian individuals after controlling for deprivation and clinical risk factors.3 Despite its relatively large size and richness of clinical information, the study data set does not include socio-economic covariates other than deprivation.
Studies based on COVID-19-surveillance data suggest that Black and South Asian individuals were more likely than White British people to test positive for COVID-19 after controlling for demographic, socio-economic, behavioural and health-related covariates.22,23 These findings shed some light on our own results, as observed inequality in the risk of dying with COVID-19 may partly be a result of heterogeneity in the risk of infection (but also differences in prognosis). Studies examining differences in outcomes among hospitalized patients found that patients from ethnic-minority groups were more likely to be admitted to critical care11,24 and had higher in-hospital-mortality rates among COVID-19 cases in England.11
Whereas our study data did not allow us to decompose ethnic differences in mortality risk into differences in infection and differences in prognosis, most of the factors we adjusted for in our models were expected to be associated with COVID-19 mortality through infection. We found that a large proportion of the elevated mortality risk among ethnic-minority groups could be explained by these infection-related factors, particularly the geographical ones. This hypothesis is corroborated by results from the national COVID-19 Infection Survey,25 which indicate that ethnic-minority groups are more likely than the White population to test positive for COVID-19 (though the estimates are subject to a high degree of uncertainty).
Beyond the UK, a systematic review of global literature on the association between ethnicity and COVID-19 infection and outcomes concluded that BAME individuals were likely to be at elevated risk.13 However, published evidence available at the time of the review was found to be limited, with much of the emerging data originating from grey literature and preprint articles. Whilst there is evidence that lockdown measures reduced infection,26 little is known on whether these measures affected ethnic groups differently.
Potential mechanisms
We found that area of residence and population density accounted for over half of the excess hazard of COVID-19 mortality across all ethnic-minority groups. These groups are concentrated in large urban areas in the UK, which have been more severely affected by the COVID-19 pandemic in terms of both infection27 and mortality rates.7
The elevated risk of COVID-19 mortality for ethnic-minority groups compared with the White population were also attenuated by including socio-economic variables in our models. The existence of a social gradient in health status and life expectancy is long-established28 and recent official data have shown that White individuals in England are less likely to live in deprived neighbourhoods than non-White individuals.29
The residual differences in COVID-19-mortality risk between ethnic groups may in part be due to unobserved factors, including pre-existing conditions and other clinical risk factors not fully captured by self-reported health status. People from Black and Asian backgrounds tend to have a higher prevalence of obesity and associated conditions of diabetes, hypertension and cardiovascular disease compared with the White population.30 These conditions are known risk factors for adverse COVID-19 outcomes and could mediate the observed differences in mortality rates between ethnic groups; however, they may also be partly attributable to the same socio-economic inequalities already captured in our models.
Socio-economic inequality is a complex, multifaceted, partly ecological concept. The statistical measures of socio-economic status and deprivation included in our models are unlikely to capture fully this conceptual complexity,31 nor the fact that disadvantage accumulated over the life course may be partly responsible for observed health inequalities.32 Given these measurement issues, we cannot rule out the possibility of structural socio-economic factors explaining more of the heterogeneity in outcomes than estimated in our study, rather than the unexplained variation necessarily being attributable to other influences.
On 23 March 2020, the UK government announced a series of lockdown restrictions aimed at reducing the spread of COVID-19, such as requiring people to stay at home, closing all shops selling non-essential goods, and stopping all social events and gatherings. Other measures had also been introduced in the UK prior to this, such as mass homeworking; national school closures; the closure of most cafes, bars and restaurants; the cancellation of sporting and cultural events; and government advice to avoid non-essential international travel. We found the presence of lockdown measures to be associated with a reduction in the differences in COVID-19-mortality rates between ethnic groups. Widespread lockdown restrictions may have levelled infection rates between ethnic groups, by reducing COVID-19 exposure and transmission throughout all parts of society.
Strengths and limitations
The primary strength of our study lies in the use of a unique, newly linked population-level data set based on the 2011 Census, comprising millions of observations and a broad range of demographic, socio-economic, household, occupational and health variables. To our knowledge, our study is the first to demonstrate an association between COVID-19 lockdown measures and ethnicity-specific mortality.
The main limitation of our study data set is the 9-year lag between census day and the start of the pandemic. The covariates included in our models reflect the situations of individuals as they were in 2011, not necessarily those at the start of the COVID-19 pandemic. In addition, the study population did not include people who immigrated or were born between 2011 and 2020, and therefore did not fully represent the population at risk. We found the ethnicity distribution in our study population to be similar to an estimate of that for the current population of England and Wales obtained from the 2019 Annual Population Survey (APS),33 whereas our study population was on average older than that derived from the APS, which is likely to result from not including post-2011 immigrants (who tend to be younger than the population average) in our study; for further details, see Supplementary Table 6 and Supplementary Figure 5, available as Supplementary data at IJE online.
Although we found that differences in COVID-19-mortality rates between ethnic groups were considerably reduced following lockdown, we cannot rule out that this reduction was at least partly attributable to other factors, such as the growing awareness of ethnic disparities in mortality risk causing people in ethnic-minority groups to shield themselves from possible infection. Furthermore, the increase in ASMRs between the pre- and post-lockdown periods that we observed for the White population may be partly due to deaths in care homes peaking later than throughout the rest of the community (see Supplementary Figure 6, available as Supplementary data at IJE online); the White population is older on average than are other ethnic groups and is therefore more likely to live in care settings.
The outcome variable may be subject to measurement error, as not all COVID-19-related deaths may have been captured on death certificates; conversely, not all deaths for which COVID-19 was mentioned on the death certificate may necessarily have involved the disease (in the absence of a test result, medical practitioners were advised to apply clinical judgement to decide whether COVID-19 was suspected to have contributed to the death). Moreover, we cannot rule out the possibility of differential rates of misclassification of COVID-19-related mortality between ethnic groups, e.g. if certain ethnic groups were more or less likely than others to be tested for the presence of the disease prior to death.
Conclusion
Whilst inequality in COVID-19 mortality between ethnic groups was appreciably accounted for by geographical and measured socio-demographic factors, some residual differences in risk remained, particularly for males and during the pre-lockdown period. Further research is urgently needed to understand the causal mechanisms underpinning the observed differences in COVID-19-mortality risk between ethnic groups.
Lockdown measures were associated with substantial reductions in excess mortality risk in ethnic-minority populations, possibly due to behavioural change throughout society and shielding from the virus among the most vulnerable. This finding has major implications in the event of a second wave of infection or local spikes in incidence, namely that placing restrictions on freedom of movement and activity may be seen as a ‘leveller’ in terms of COVID-19-mortality rates between ethnic groups.
Author Contributions
D.A., V.N., C.W., C.G., M.G. and B.H. contributed to the study conceptualization and design. L.B. and N.R. contributed to the preparation of the study data and D.A., V.N., C.W. and C.G. performed the statistical analyses. All authors contributed to interpretation of the results. D.A., V.N., C.W., L.B. and N.R. drafted the manuscript. P.G., A.B., K.K., M.G., B.H. and I.D. contributed to the critical revision of the manuscript. All authors approved the final manuscript. V.N. is the guarantor for the study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
None.
Conflict of interest
Dr Banerjee has received a research grant unrelated to the current work from AstraZeneca and is a Trustee of the South Asian Health Foundation (SAHF). Prof. Khunti is a member of the Independent Scientific Advisory Group for Emergencies (SAGE), a Trustee of the SAHF, Director of the NIHR Applied Research Collaboration (ARC) East Midlands and Director of the Centre for Black and Minority Ethnic (BME) Health. The other authors declare no competing interests.
Supplementary Material
Acknowledgements
The authors would like to thank Karen Tingay and Neil Bannister at the Office for National Statistics, Miqdad Asaria at the London School of Economics and Nazrul Islam at the Nuffield Department of Population Health for their valuable input to the manuscript. The authors also thank Merilynn Pratt, Alexander Cooke, David Tabor and Jessica Walkeden at the Office for National Statistics for their work in preparing the study data. This study was ethically self-assessed against the ethical principles of the National Statistician’s Data Ethics Advisory Committee (NSDEC) using NSDEC’s ethics self-assessment tool. Under the provisions of the Statistics and Registration Service Act 2007, the linked 2011 Census data used in this study are not permitted to be shared.
References
- 1. Office for National Statistics. Deaths registered weekly in England and Wales, provisional: week ending. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deatde/bulletins/deathsregisteredweeklyinenglandandwalesprovisional/weekending17july2020 (11 August 2020, date last accessed).
- 2. Public Health England. Patients admitted to hospital. 2020. https://coronavirus-staging.data.gov.uk/healthcare (11 August 2020, date last accessed).
- 3. Williamson EJ, Walker AJ, Bhaskaran K. et al. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature 2020;584:430–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zheng Z, Peng F, Xu B. et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect 2020;81:16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Singh AK, Gillies CL, Singh R. et al. Prevalence of comorbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab 2020;(online ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Khalatbari-Soltani S, Cumming RG, Delpierre C, Kelly-Irving M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health 2020;74:620–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Office for National Statistics. Deaths involving COVID-19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 31 May 2020. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand31may2020 (11 August 2020, date last accessed).
- 8. Office for National Statistics. Coronavirus (COVID-19) related deaths by occupation, England and Wales: deaths registered between 9 March and 25 May 2020. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregisteredbetween9marchand25may2020 (11 August 2020, date last accessed).
- 9. Nazroo JY, Williams DR. The Social Determination of Ethnic/Racial Inequalities in Health, In: Marmot M, Wilkinson R. (eds). Social Determinants of Health, 2nd edn Oxford: Oxford University Press, 2006. [Google Scholar]
- 10. Zhao H, Harris RJ, Ellis J, Pebody RG. Ethnicity, deprivation and mortality due to 2009 pandemic influenza A(H1N1) in England during the 2009/2010 pandemic and the first post-pandemic season. Epidemiol Infect 2015;143:3375–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aldridge RW, Lewer D, Katikireddi SV. et al. Black, Asian and minority ethnic groups in England are at increased risk of death from COVID-19: indirect standardisation of NHS mortality data. Wellcome Open Res 2020;5:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Public Health England. Disparities in the risk and outcomes of COVID-19. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892085/disparities_review.pdf (11 August 2020, date last accessed).
- 13. Pan D, Sze S, Minhas JS. et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine 2020;23:100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Office for National Statistics. 2011 Census Statistics for England and Wales: March 2011 QMI. 2013. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/methodologies/2011censusstatisticsforenglandandwalesmarch2011qmi#:∼:text=For%202011%2C%20person%20response%20rates, areas%2C%20age%20and%20population%20groups. (11 August 2020, date last accessed).
- 15. Office for National Statistics. Item edit and imputation: evaluation report. 2012. https://www.ons.gov.uk/census/2011census/2011censusdata/2011censususerguide/qualityandmethods (11 August 2020, date last accessed).
- 16. Department for Communities and Local Government. The English Indices of Deprivation 2015. 2015. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (11 August 2020, date last accessed).
- 17. Welsh Government. Welsh Index of Multiple Deprivation (WIMD) 2014. 2014. https://statswales.gov.wales/Catalogue/Community-Safety-and-Social-Inclusion/Welsh-Index-of-Multiple-Deprivation/Archive/WIMD-2014 (11 August 2020, date last accessed).
- 18. Office for National Statistics. Which occupations have the highest potential exposure to the coronavirus (COVID-19)? 2020. https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/articles/whichoccupationshavethehighestpotentialexposuretothecoronaviruscovid19/2020-05-11 (11 August 2020, date last accessed).
- 19. Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika 1982;69:239–41. [Google Scholar]
- 20. R Core Team. R: A language and environment for statistical computing. 2019. https://www.r-project.org (11 August 2020, date last accessed).
- 21. Cohen J. Statistical Power Analysis for the Behavioral Sciences, 2nd edn Hillsdale, NJ: Erlbaum, 1988. [Google Scholar]
- 22. Niedzwiedz CL, O’Donnell CA, Jani BD. et al. Ethnic and socioeconomic differences in SARS-CoV-2 infection: prospective cohort study using UK Biobank. BMC Med 2020;18:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. De Lusignan S, Dorward J, Correa A. et al. Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre primary care network: a cross-sectional study. Lancet Infect Dis 2020;20:1034–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harrison EM, Docherty AB, Barr B. et al. Ethnicity and outcomes from COVID-19: the ISARIC CCP-UK prospective observational cohort study of hospitalised patients. 2020. https://papers.ssrn.com/sol3/papers.cfm? abstract_id=3618215 (11 August 2020, date last accessed).
- 25. Office for National Statistics. Coronavirus (COVID-19) Infection Survey: characteristics of people testing positive for COVID-19 in England, August 2020. 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsinthecommunityinengland/characteristicsofpeopletestingpositiveforcovid19inenglandaugust2020 (8 September 2020, date last accessed).
- 26. Islam N, Sharp SJ, Chowell G. et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ 2020;370:m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hamidi S, Sabouri S, Ewing R. Does density aggravate the COVID-19 pandemic? JAm Planning Assoc 2020;86:495–509. [Google Scholar]
- 28. Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot Review 10 years on. 2020. https://www.health.org.uk/publications/reports/the-marmot-review-10-years-on (11 August 2020, date last accessed).
- 29. Ministry of Housing, Communities and Local Government. People living in deprived neighbourhoods. 2020. https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/people-living-in-deprived-neighbourhoods/latest (11 August 2020, date last accessed).
- 30. Platt L, Warwick R. Are some ethnic groups more vulnerable to COVID-19 than others? 2020. https://www.ifs.org.uk/inequality/chapter/are-some-ethnic-groups-more-vulnerable-to-covid-19-than-others (11 August 2020, date last accessed).
- 31. Nazroo JY. Genetic, cultural or socio‐economic vulnerability? Explaining ethnic inequalities in health. Sociol Health Illness 1998;20:710–30. [Google Scholar]
- 32. Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health 2003;93:277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Office for National Statistics. Annual population survey (APS) QMI. 2020. https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/methodologies/annualpopulationsurveyapsqmi (8 September 2020, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.