Abstract
We are witnessing an unparalleled pandemic caused by the novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) associated with coronavirus disease 2019 (COVID-19). Current data show that SARS-CoV-2 results in mild flu-like symptoms in the majority of healthy and young patients affected. Nevertheless, the severity of COVID-19 respiratory syndrome and the risk of adverse or catastrophic outcomes are increased in patients with pre-existing cardiovascular disease. Patients with adult congenital heart disease (ACHD)—by definition—have underlying cardiovascular disease. Many patients with ACHD are also afflicted with residual haemodynamic lesions such as valve dysfunction, diminished ventricular function, arrhythmias or cyanosis, have extracardiac comorbidities, and face additional challenges regarding pregnancy. Currently, there are emerging data of the effect of COVID-19 on ACHD patients, but many aspects, especially risk stratification and treatment considerations, remain unclear. In this article, we aim to discuss the broad impact of COVID-19 on ACHD patients, focusing specifically on pathophysiology, risk stratification for work, self-isolation, hospitalization, impact on pregnancy, psychosocial health, and longer-term implications for the provision of ACHD care.
Keywords: Adult congenital heart disease, COVID-19, SARS-CoV-2, Corona, Position paper
Introduction
We are witnessing an unparalleled pandemic caused by the novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) associated with coronavirus disease 2019 (COVID-19).
Current data show that SARS-CoV-2 results in mild flu-like symptoms in the majority of healthy and young patients affected.1 Nevertheless, the severity of COVID-19 respiratory syndrome and the risk of adverse or catastrophic outcomes are increased in patients with pre-existing cardiovascular disease.2 Patients with adult congenital heart disease (ACHD)—by definition—have underlying cardiovascular disease. Many patients with ACHD are also afflicted with residual haemodynamic lesions, such as valve dysfunction, diminished ventricular function, arrhythmias, or cyanosis, have extracardiac comorbidities, and face additional challenges regarding pregnancy.3–5 Currently, there are emerging data of the effect of COVID-19 on patients with ACHD, but many aspects, especially risk stratification and treatment considerations, remain unclear. In this article, we aim to discuss the broad impact of COVID-19 on patients with ACHD, focusing specifically on pathophysiology, risk stratification for work, self-isolation, hospitalization, impact on pregnancy, psychosocial health, and longer-term implications for the provision of ACHD care.
Specific clinical, anatomical, and physiological considerations in ACHD cardiovascular cohorts
Theoretically, the SARS-COV-2 virus should cause greatest harm in patients with pre-existing pulmonary or myocardial conditions, due to direct pulmonary and myocardial injury.6,7 Vulnerable patients may include those with pulmonary arterial hypertension (PAH), Eisenmenger syndrome, cyanosis, Fontan palliation, and systemic right ventricles (RVs) from transposition of the great arteries (TGA). Although ‘cardiovascular disease’, broadly defined, is clearly associated with worse outcomes related to respiratory viral infections in general,8–10 not every cardiovascular condition confers equal risk.11 Therefore, it is unknown whether the aforementioned ACHD subgroups fall into this high-risk category or are as vulnerable as they might inherently seem. Plausible arguments of factors conveying risk or protection are herein discussed, although each argument remains speculative due to the paucity of published experiences with COVID-19.
Among the most vulnerable congenital heart patients are likely those with Fontan physiology or various modifications of single ventricle palliation, who are dependent on low pulmonary vascular resistance (PVR) for venous return. As patients with acute respiratory distress syndrome (ARDS) will typically have the mean pulmonary artery pressures of 30 mmHg or greater,12 the effects could be devastating to Fontan patients reliant on passive pulmonary blood flow. Furthermore, Fontan patients are intolerant of ongoing positive pressure ventilation because elevated intrathoracic pressure can adversely affect venous return. Fontan patients are also prone to thromboembolic complications, which have also been described with COVID-19.13 Yet thus far, anecdotal experience assessed via surveys of accredited programmes has not demonstrated a high proportion of Fontan patients succumbing to the virus. In their favour, Fontan patients tend to be younger, and the coronavirus experience thus far suggests favoured outcomes in younger individuals. Furthermore, if exposed, Fontan patients may not necessarily be at greater risk for the virus to precipitate an ARDS-like reaction, without which many of the adverse physiological effects are less worrisome.
PAH is another cohort of patients viewed as high risk. Yet in a similar fashion, anecdotal experience with PAH has not demonstrated high mortality; both infection burden and serious complications have been lower than expected.14 An RV working against chronically increased PVR may be tempered to adverse changes in PVR from acute respiratory infection. For now, however, this remains speculative.
It is easy to postulate that cyanosis including Eisenmenger physiology would confer tremendous vulnerability to a disease that worsens oxygen delivery. These fragile patients endure on delicate homeostatic adaptations that can be fatal when unbalanced. Yet paradoxically, it may be that these same adaptations lessen the impact of acute hypoxaemia from the virus. Generally, RV dysfunction is adversely prognostic in COVID-19,15 and, like PAH, Eisenmenger patients are vulnerable to ventricular dysfunction over time. However, chronically elevated afterload may precondition an RV to better adapt to acute changes in loading. Those with cyanosis from right to left shunting may be vulnerable to thromboembolic phenomena given the association of COVID-19 and thrombosis.13 Despite the perceived risks, anecdotal reports include those with PAH, cyanosis, and Eisenmenger physiology, who, though requiring intubation, notwithstanding survive. Perhaps for some such survivors, youth is in their favour. As above, anecdotes will need to be replaced with population data to verify and understand this more fully.
As biventricular dysfunction is a known complication of COVID-19, those with pre-existing systemic ventricular dysfunction or vulnerability thereto should be considered at risk. Yet the transposition patients have a sub-pulmonic left ventricle, which, in the face of increasing demands such as from ARDS, may pose an advantage. On the other hand, the systemic RV systolic function is often moderate to severely impaired with possible worsening after COVID-19 infection. While published COVID-19 experience describes ventricular failure as a complication from the virus, pre-existing systolic dysfunction it is not highlighted as a risk factor for mortality16 likely because much remains unknown about patient conditions prior to exposure.
Finally, because these cohorts generally require closer follow-up, there may be exposure risk for those without infection who, for ongoing care, visit receive ongoing care in a healthcare facility where the virus may be prevalent. At the opposite extreme there is risk from care avoidance if cardiopulmonary issues are ignored or treatment is delayed due to concerns of such exposure. Examples of both have been experienced.
Ongoing efforts for data collection
The International Society for Adult Congenital Heart Disease endorses a global project initiated by the Adult Congenital Heart Association that is currently collecting COVID-19 data in over 80 centres. The study lasts up to 2 years and aims to document the clinical impact of COVID-19 on patients with congenital heart disease. As of July 2020, the study has collected 90 cases, 48% with moderate and 38% complex congenital heart defects, including 11 Fontan and 8 cyanotic patients. Of these, there have been 29 hospitalizations, 14 with major complications, and 4 COVID-related deaths.17 On a European level, the European Collaboration for Prospective Outcome research in Congenital Heart Disease (EPOCH) launched a project tracking COVID-19 cases in over 20 European tertiary ACHD centres throughout nine countries. Close to 90 COVID-19 cases among patients with ACHD have been reported, including 5 fatalities in patients positive for SARS-CoV-2. A survey of ACHD cardiologists at EPOCH centres indicated that patients with residual pulmonary hypertension, central cyanosis, and the absence of a sub-pulmonary ventricle were considered at the greatest risk of adverse COVID-19 outcomes.
Care recommendations
There are limited data on outcomes in patients with ACHD who develop COVID-19. Current management strategies are largely based on expert opinion and extrapolated from adult patients with acquired cardiovascular disease. Overall, ACHD is a heterogeneous cohort with a broad age range and a wide spectrum of clinical presentations ranging from completely asymptomatic individuals to various degrees of functional limitation, fatigue, and overt heart failure. Some patients also present with cyanosis, reduced oxygen saturations, secondary erythrocytosis, hyperuricaemia, and evidence of other end-organ dysfunction.
Prudence demands that patients with ACHD avoid exposure and infection and thus any risk of unwanted complications but also that unfounded fear is not propagated among patients or providers.10,18
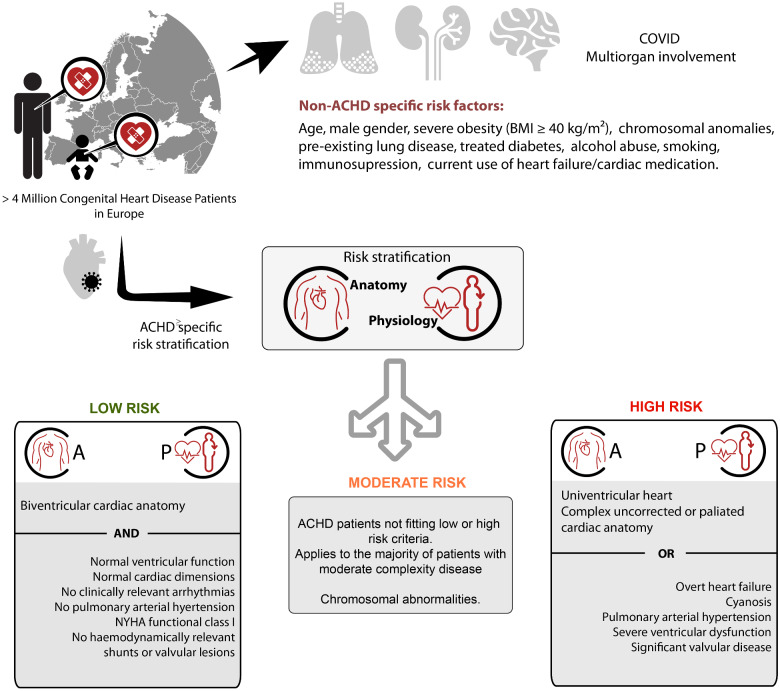
In addition to general recommended measures of disease prevention—including physical distancing, face masks, and meticulous hand hygiene as well as influenza and pneumococcal vaccination—patients with ACHD will likely benefit from additional measures of infection prevention. These measures include avoidance of social or occupational activities involving contact with individuals who might be infected with SARS-CoV-2. The benefit of such measures must be balanced against potential adverse psychosocial and economic implications. In concert with efforts made by employers, many patients should be able to continue active employment in safe environments. Based upon general risk factors as well as ACHD-specific anatomical and physiological considerations, we recommend the risk stratification algorithm outlined in Figure 1. The algorithm adopts and expands on concept and recommendations recently proposed by Radke et al.20 We contend that anatomy is insufficient to inform risk stratification and should be supplemented by physiological aspects and patient status.4,5
Figure 1.
Risk stratification of patients according to anatomical and physiological criteria into low-, moderate-, and high-risk groups. ACHD, adult congenital heart disease; Sars-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2.
Whereas patients with ACHD with complex underlying anatomy post-surgical correction and with pristine haemodynamic status might be regarded low risk, those with simpler anatomical diagnoses yet who are highly symptomatic or have overt heart failure should be considered as higher risk for adverse COVID-19 outcomes.
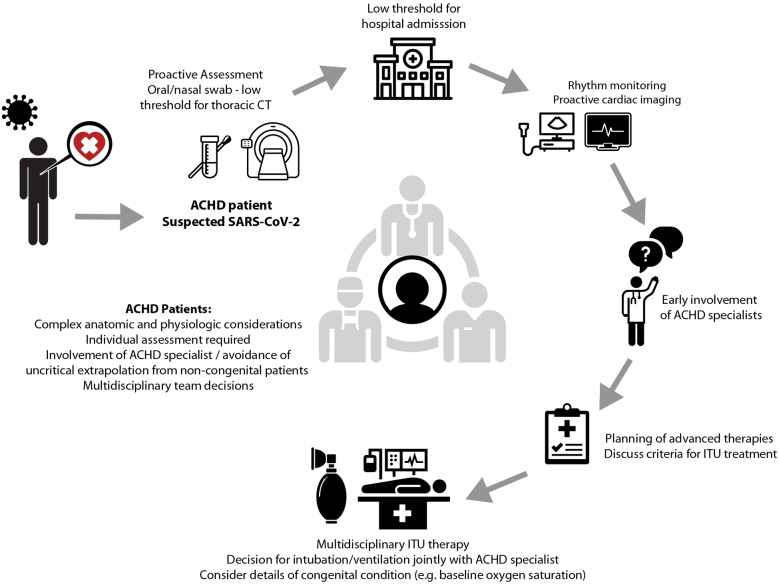
The proposed classification should serve as a starting point for expert assessment that is individualized to each patient and incorporates patients’ personal degree of risk, risk aversion, and lifestyle needs. Particularly vulnerable patients should be offered liberal SARS-CoV-2 testing and should be followed closely including access to tertiary centres if feasible. General considerations regarding professional duties, education, and medical management are outlined in Table 1. Specific therapeutic consideration for selected, potentially particularly vulnerable subgroups of patients with ACHD is presented in Table 2, while Figure 2 illustrates general management principles across the spectrum of congenital heart disease. Additional aspects of intrahospital triage and intensive care treatment of affected patients with ACHD have been outlined elsewhere.19,20
Table 1.
Recommendations for work/education and general medical management according to patient risk category
| General considerations regarding work/education | Therapy in case of SARS-CoV-2 infection: |
|---|---|
|
Low-risk ACHD patients | |
|
Usual protection measures recommended Follow general recommendations (face mask, etc.) No general limitation for work/school |
If clinically stable offer remote home management Contact with ACHD centre advisable Early admission in case of clinical deterioration |
|
Moderate-risk ACHD patients | |
|
Individualized risk assessment. General recommendations: - Reduce non-essential contact with public/clients/students/colleagues - Discuss workplace protective measures (face mask/PPE) |
Consider early admission (even if oligosymptomatic) Discussion with ACHD specialist indispensable Early hospital admission/preferably at ACHD centre in case of clinical deterioration |
|
High-risk ACHD patients | |
|
Meticulous physical distancing Avoidance of direct contact to clients or students whenever possible. Preference for home office work |
Consider early admission (even if asymptomatic) Discussion with ACHD specialist indispensable Early planning of treatment strategy in case of deterioration or intensive care therapy requirement |
ACHD, adult congenital heart disease; Sars-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2.
Table 2.
Specific management considerations and pertinent pathophysiological characteristics of vulnerable adult congenital heart disease sub-cohorts
| ACHD condition | Therapeutic considerations | Pathophysiological characteristics |
|---|---|---|
| Univentricular heart—including Fontan palliation |
ARDS typically leads to mean pulmonary artery pressures of 30 → potentially devastating effect for Fontan patients Positive pressure ventilation poorly tolerated since elevated intrathoracic pressure can adversely affect venous return Prone to thromboembolic complications as described in COVID-19 In patients with desaturation and atrial fenestration potential for paradoxical/air embolism → venous air filters required |
Physiology dependent on low PVR Thrombophilic state Atrial fenestration occasionally present |
| PAH |
In stable PAH patients risk of RV failure unclear but potentially low In patients with RV dysfunction/advanced or unstable disease potential for catastrophic RV failure Potential for thromboembolic complications as described in COVID-19 Dependent on adequate RV preload |
RV preconditioned to chronically increased afterload may be tempered to adverse changes in PVR from acute respiratory infection Thrombophilic state |
| Eisenmenger physiology (shares all aspects with cyanotic conditions) |
Vulnerable to ventricular dysfunction Dependent on adequate RV preload |
RV potentially preconditioned to chronically increased afterload may be tempered to adverse changes in PVR from acute respiratory infection Fragile physiology |
| Cyanotic conditions |
Potential for paradoxical embolism/air embolism (use of air filters on all venous canulae required) Prone to thromboembolic complications as described in COVID-19 Maintenance of adequate haemoglobin concentrations (physiological adaptation to cyanosis) required When considering mechanical ventilation consideration of baseline oxygen saturations (commonly below 90% at rest) required |
Fragile balanced physiology Patients adapted to cyanosis through erythrocytosis Thrombophilic state combined with increased bleeding risk |
| Systemic RV |
In patients with RV dysfunction/advanced or unstable disease potential for catastrophic RV failure Diastolic dysfunction common → dependent on adequate preload |
Subpulmonary LV potentially better suited to withstand acutely increased afterload during ARDS Chronotropic incompetence common |
| Patients with Down syndrome |
Proactive prevention and treatment of infection required General rationing of ITU capacity for Down syndrome patients is opposed |
Increased risk of pulmonary infections or ARDS |
| General recommendation for patients with Down syndrome, univentricular hearts, asplenia, cyanotic congenital heart disease, 22q11 syndrome and other conditions with compromised immune system | Ensure adequate immunization status (influenza/pneumococcal disease) |
ACHD, adult congenital heart disease; ARDS, acute respiratory distress syndrome; COVID-19, coronavirus disease 19; ITU, intensive treatment unit; LV, left ventricle; PAH, pulmonary arterial hypertension; PVR, pulmonary vascular resistance; RV, right ventricle.
Figure 2.
Overview over general management principles recommended for adult congenital heart disease patients. ACHD, adult congenital heart disease; ITU, intensive treatment unit; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2.
Pregnancy and childbirth
Pregnant women are particularly susceptible to respiratory pathogens and severe pneumonia. This is especially true for women with heart disease. It has been reported that viral pneumonia in pregnant women is associated with an increased risk of preterm birth, foetal growth restriction and perinatal mortality.21 The largest study thus far on COVID-19 and pregnancy included 116 pregnant women in China.22 Eight (6.9%) of the 116 pregnant women had severe COVID-19 pneumonia and the clinical characteristics of pregnant COVID-19 patients were found to be similar to those of nonpregnant adult patients presenting with COVID-19 pneumonia. SARS-CoV-2 infection during pregnancy was not associated with an increased risk of spontaneous abortion or spontaneous preterm birth, although many were delivered preterm on maternal indication. There were also no cases of foetal deaths and only 1 (1%) neonatal death. Furthermore, there was no evidence of vertical transmission of SARS-CoV-2 infection from mother to baby and breast milk samples from 12 mothers with COVID-19 tested negative for SARS-CoV. A US-based study of 64 pregnant women hospitalized with COVID-19 reported that 44 (69%) had severe and 20 (31%) critical disease.23 There were no maternal deaths and no cardiomyopathies. Furthermore, no stillbirths, neonatal deaths, or cases of vertical transmission were reported. Despite these largely reassuring results, we advocate that when pregnant women present with any recent onset of cough and anosmia, a high level of suspicion for screening care is warranted. In addition, when COVID-19 is diagnosed in pregnant women, meticulous care should be provided by a multidisciplinary team including obstetricians, intensivists, obstetric anaesthetists, virologists, microbiologists, neonatologists, and infectious-disease specialists.
Psychological considerations
Studies suggest that between one-third and one-half of patients with ACHD meet diagnostic criteria for mood or anxiety disorders at some point during their lives, of whom most will not receive mental health treatment.24–28 The short- and long-term impact of the pandemic on the mental health of patients with ACHD is currently unknown yet warrants great concern. For patients who develop COVID-19, it is difficult to imagine they would not benefit from close psychological support, particularly if they develop advanced disease. Even in the absence of personal COVID-19 diagnoses, we anticipate that the mental health of many patients will be challenged by stressors including social isolation, fear of contracting COVID-19, apprehension when cities re-open, frustration with the actions of others, concern about seeking cardiology care (both routine and urgent), adaptation to telemedicine, thoughts of mortality, and implications for finances, education, and employment. It has been advised that the provision of psychosocial support ‘should be integrated into general pandemic care’.29 Assumptions about emotional well-being at the individual patient level, however, should be avoided. We thus recommend that ACHD providers increase their practice of incorporating discussion about psychological well-being and coping within outpatient clinic visits, whether occurring in clinic or by telemedicine. Providers can normalize and empathize with psychological reactions to COVID-19 and encourage strategies that previously helped patients cope with health anxiety.
Longer-term Implications of the COVID-19 pandemic on ACHD care
In the acute phase of the pandemic, conversion of outpatient appointments to teleclinics and deferment of non-urgent/elective operations to protect patients with ACHD from exposure to COVID-19 was required. However, this may lead to the postponement of essential interventions and expose patients to avoidable ACHD complications, while also increasing the risk of loss to follow-up. Fear of exposure to SARS-CoV-2 may also impact patients’ willingness to seek emergency treatment and/or attend non-urgent outpatient clinic visits and diagnostic testing procedures. Therefore, it is essential to maintain a close link to vulnerable patients with ACHD and ensure appropriate assessment and therapy as soon as the pandemic situation allows. Providers must also prepare for increasing workloads to deal with deferred operations and interventions. At some centres, the COVID-19 situation has served as a natural experiment for the implementation and testing of teleconsultations and technology assisted remote follow-up. This model of care is appealing and will hopefully remain in the long term as it offers patient education and empowerment and technology-based personalized ACHD care, while also minimizing patients’ travel burden.30–32 Technology and artificial intelligence33 may also expedite tertiary work, such as risk stratification, online volumetric analyses of imaging data, and multimodal risk-stratification. Furthermore, lifestyle issues including healthy diet, exercise, avoidance of smoking, contraception, and family planning may be embedded in early interactions with patients to avoid long-term complications, maximize patients’ life potential, and reduce risk when affected by COVID-19. Telehealth certainly cannot achieve all components of ACHD health care. Furthermore, although elective procedures may be delayed, urgent surgical, catheter-based, or electrophysiological interventions should not be postponed due to the COVID-19 pandemic. Given the prolonged nature of the COVID 19 pandemic with recurring restrictions regarding elective procedures, clinicians need to continuously re-evaluate vulnerable patients with ACHD to prevent long-term complications and avoidable morbidity and mortality. Specifically, individualized assessment is required as procedures that may have represented elective interventions/operations during the first wave of the pandemic may since have become urgent and should thus not be postponed further.
Conclusions
Adults with congenital heart disease represent a growing and complex population of patients who requires protection from SARS-CoV-2 and a proactive, tailored treatment in case of COVID-19 infection. Due to anatomical and pathophysiological heterogeneity, however, an individualized approach to risk stratification and management is required. Indeed, although in part afflicted by complex cardiac disease, patients are typically younger and therefore should not be uniformly seen as high risk as many older patients with cardiovascular disease. The mere presence of ACHD in an individual should not be a source of ungrounded fear or isolation. The risk stratification algorithm considers expert opinion and also integrates underlying anatomy, physiology, current symptomatic or functional status, as well as patient age and psychosocial profile into clinical decision-making. We thus discourage collapsing patients with ACHD into the one broad category with adults with acquired cardiovascular disease. Social isolation, psychological distress, and the avoidance of medical care can have devastating impacts, whereas comparatively the risk of COVID-19 infection seems relatively low. The strategy proposed should serve as a basis for decision-making and allow for individualized patient-centred recommendations.
Conflict of interest: none declared.
References
- 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–1242. [DOI] [PubMed] [Google Scholar]
- 2. Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D, Italia L, Zaccone G, Tedino C, Fabbricatore D, Curnis A, Faggiano P, Gorga E, Lombardi CM, Milesi G, Vizzardi E, Volpini M, Nodari S, Specchia C, Maroldi R, Bezzi M, Metra M. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J 2020;41:1821–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gatzoulis MA. COVID-19 and congenital heart disease in perspective. Eur Heart J 2020;41:1871–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller GP, Jung B, Kluin J, Lang IM, Meijboom F, Moons P, Mulder BJM, Oechslin E, Roos-Hesselink J, Schwerzmann M, Sondergaard L, Zeppenfeld K; ESC Scientific Document Group. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J 2020;doi:10.1093/eurheartj/ehaa554. [Google Scholar]
- 5. Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, Crumb SR, Dearani JA, Fuller S, Gurvitz M, Khairy P, Landzberg MJ, Saidi A, Valente AM, Van Hare GF. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;139:e698–e800. [DOI] [PubMed] [Google Scholar]
- 6. Rao S, Sasser W, Diaz F, Sharma N, Alten J. Coronavirus associated fulminant myocarditis successfully treated with intravenous immunoglobulin and extracorporeal membrane oxygenation. Chest 2014;146:336A. [Google Scholar]
- 7. Ukimura A, Satomi H, Ooi Y, Kanzaki Y. Myocarditis associated with influenza A H1N1pdm2009. Influenza Res Treat 2012;2012:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, Walmsley SL, Mazzulli T, Avendano M, Derkach P, Ephtimios IE, Kitai I, Mederski BD, Shadowitz SB, Gold WL, Hawryluck LA, Rea E, Chenkin JS, Cescon DW, Poutanen SM, Detsky AS. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 2003;289:2801–2809. [DOI] [PubMed] [Google Scholar]
- 9. Gilca R, De Serres G, Boulianne N, Ouhoummane N, Papenburg J, Douville-Fradet M, Fortin E, Dionne M, Boivin G, Skowronski DM. Risk factors for hospitalization and severe outcomes of 2009 pandemic H1N1 influenza in Quebec, Canada. Influenza Other Respir Viruses 2011;5:247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tan W, Aboulhosn J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int J Cardiol 2020;309:70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ryan D, Frohlich S, McLoughlin P. Pulmonary vascular dysfunction in ARDS. Ann Intensive Care 2014;4:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quere I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global Covid-19 Thrombosis Collaborative Group. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950–2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Horn EM, Chakinala M, Oudiz R, Joseloff E, Rosenzweig EB. Could pulmonary arterial hypertension patients be at a lower risk from severe COVID-19? Pulm Circ 2020;10. doi:2045894020922799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Argulian E, Sud K, Vogel B, Bohra C, Garg VP, Talebi S, Lerakis S, Narula J. Right ventricular dilation in hospitalized patients with COVID-19 infection. JACC Cardiovasc Imaging 2020;13:2459–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D’Acquisto F, Nicklin SA, Marian AJ, Nosalski R, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020;116:1666–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Association ACH. Medical Leaders of ACHA Initiate Worldwide COVID-19 Study in Adults with CHD. https://www.achaheart.org/about-us/news/2020/medical-leaders-of-acha-initiate-worldwide-covid-19-study-in-adults-with-chd/ (20 May 2020).
- 18. Alsaied T, Aboulhosn JA, Cotts TB, Daniels CJ, Etheridge SP, Feltes TF, Gurvitz MZ, Lewin MB, Oster ME, Saidi A. Coronavirus disease 2019 (COVID-19) pandemic implications in pediatric and adult congenital heart disease. J Am Heart Assoc 2020;9:e017224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lastinger LT, Daniels CJ, Lee M, Sabanayagam A, Bradley EA. Triage and management of the ACHD patient with COVID-19: a single center approach. Int J Cardiol 2020;320:178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Radke RM, Frenzel T, Baumgartner H, Diller GP. Adult congenital heart disease and the COVID-19 pandemic. Heart 2020;106:1302–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, Ng PC, Lam PW, Ho LC, To WW, Lai ST, Yan WW, Tan PY. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol 2004;191:292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, Feng L, Li C, Chen H, Qiao Y, Lei D, Wang C, Xiong G, Xiao F, He W, Pang Q, Hu X, Wang S, Chen D, Zhang Y, Poon LC, Yang H. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol 2020;223:111.e1–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pierce-Williams RAM, Burd J, Felder L, Khoury R, Bernstein PS, Avila K, Penfield CA, Roman AS, DeBolt CA, Stone JL, Bianco A, Kern-Goldberger AR, Hirshberg A, Srinivas SK, Jayakumaran JS, Brandt JS, Anastasio H, Birsner M, O'Brien DS, Sedev HM, Dolin CD, Schnettler WT, Suhag A, Ahluwalia S, Navathe RS, Khalifeh A, Anderson K, Berghella V. Clinical course of severe and critical COVID-19 in hospitalized pregnancies: a US cohort study. Am J Obstet Gynecol 2020;2:100134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bromberg JI, Beasley PJ, D'Angelo EJ, Landzberg M, DeMaso DR. Depression and anxiety in adults with congenital heart disease: a pilot study. Heart and Lung 2003;32:105–110. [DOI] [PubMed] [Google Scholar]
- 25. Horner T, Liberthson R, Jellinek MS. Psychosocial profile of adults with complex congenital heart disease. Mayo Clin Proc 2000;75:31–36. [DOI] [PubMed] [Google Scholar]
- 26. Kovacs AH, Saidi AS, Kuhl EA, Sears SF, Silversides C, Harrison JL, Ong L, Colman J, Oechslin E, Nolan RP. Depression and anxiety in adult congenital heart disease: predictors and prevalence. Int J Cardiol 2009;137:158–164. [DOI] [PubMed] [Google Scholar]
- 27. Kasmi L, Calderon J, Montreuil M, Geronikola N, Lambert V, Belli E, Bonnet D, Kalfa D. Neurocognitive and psychological outcomes in adults with dextro-transposition of the great arteries corrected by the arterial switch operation. Ann Thorac Surg 2018;105:830–836. [DOI] [PubMed] [Google Scholar]
- 28. Westhoff-Bleck M, Briest J, Fraccarollo D, Hilfiker-Kleiner D, Winter L, Maske U, Busch MA, Bleich S, Bauersachs J, Kahl KG. Mental disorders in adults with congenital heart disease: unmet needs and impact on quality of life. J Affect Disord 2016;204:180–186. [DOI] [PubMed] [Google Scholar]
- 29. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020;383:510–512. [DOI] [PubMed] [Google Scholar]
- 30. Brida M, Gatzoulis MA. Adult congenital heart disease: past, present and future. Acta Paediatr 2019;108:1757–1764. [DOI] [PubMed] [Google Scholar]
- 31. Gatzoulis MA. Adult congenital heart disease: education, education, education. Nat Clin Pract Cardiovasc Med 2006;3:2–3. [DOI] [PubMed] [Google Scholar]
- 32. Gatzoulis MA, Chung N, Ferrero P, Chessa M, Giannakoulas G, Tzifa A, Diller GP, Brida M,, Al-Sakini N. Adult congenital heart care in the COVID-19 era, and beyond: a call for action. Int J Cardiol CHD 2020;1:4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Diller GP, Kempny A, Babu-Narayan SV, Henrichs M, Brida M, Uebing A, Lammers AE, Baumgartner H, Li W, Wort SJ, Dimopoulos K, Gatzoulis MA. Machine learning algorithms estimating prognosis and guiding therapy in adult congenital heart disease: data from a single tertiary centre including 10 019 patients. Eur Heart J 2019;40:1069–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]