A 59-year-old man was hospitalized due to worsening dyspnoea during Covid-19 pandemic.
Electrocardiogram (ECG) was unremarkable. Blood laboratory tests showed normal haemoglobin with normal white blood cell count, normal brain natriuretic peptide levels, high sensitivity cardiac troponin I at upper level of normal range, and normal C-reactive protein (PCR) values. Nasopharyngeal swab test was negative for the presence of SARS-CoV-2 genome, while serum SARS-CoV-2 IgG test resulted positive (75 AU/mL), suggesting previous Covid-19 infection.
Chest X-ray excluded pulmonary lesions and pleural effusion (Panel A). Transthoracic echocardiography with strain analysis documented moderate left ventricle (LV) dilatation with mild hypertrophy at septal level, diffuse hypokinesis, more evident at septal and inferior walls, and mildly reduced LV ejection fraction (LVEF 42%) (Panels B and C).
Cardiovascular magnetic resonance (CMR) showed moderate LV dilatation and thickened mid inferior septum (Panel D), with overall moderately reduced LVEF (37%). At tissue characterization, T2-weighted images showed increased signal intensity at basal and mid septum (Panel E), late sequences demonstrated mid-wall enhancement at basal septal and inferolateral levels (Panel F), native T1 mapping demonstrated diffusely increased T1 values, ranging between 1150 and 1300 ms (Panel G), T2 values at septum and basal lateral wall were increased up to 65–70 ms (Panel H), and extracellular volume was shown to be diffusely increased, ranging between 35% and 50% (Panel I). All CMR findings suggested an acute/subacute myocarditis.
Considering the clinical status, invasive assessment was suggested, and endomyocardial biopsy samples were collected at the right side of basal and mid interventricular septum.
At histological analysis, mildly increased cardiomyocyte diameter was found, with some perinuclear halos and dysmetric and dysmorphic nuclei; furthermore, interstitial oedema with lymphocytic aggregates, myocyte necrosis, and focal areas of fibrosis were described (Panels J–M). The final diagnosis of possible chronic active myocarditis was established.
Molecular analysis by reverse transcription polymerase chain reaction demonstrated 2019 Novel Coronavirus (SARS-CoV-2) genome in myocardial specimens. In situ hybridization for SARS-CoV-2 demonstrated the presence of the virus in the endothelial cells (Panel N, red arrow), leading to possible vascular mediated myocardial injury.
This case, which is one of the few reports of SARS-CoV-2-related biopsy-proven myocardial injury, perfectly highlights the role of CMR with advanced tissue characterization sequences in detecting active myocardial injuries in Covid-19 pandemic era, during which possible SARS-CoV-2-related myocardial involvement has been documented.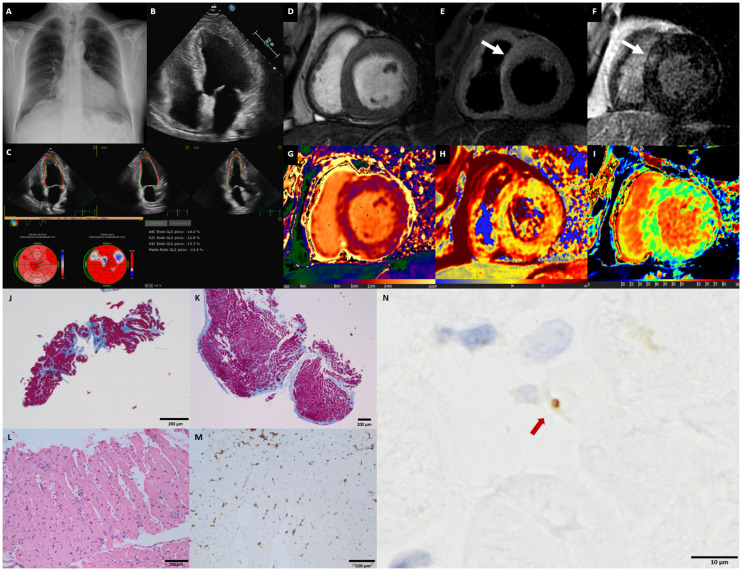
Supplementary Material
Acknowledgements: We thank the following people for their contribution to this work: Giulia Vettor, MD (Centro Cardiologico Monzino IRCCS, Milan, Italy); Mario Babbaro, MD (Dipartimento di Medicina Clinica e Molecolare, Facoltà di Medicina e Psicologia, Università degli studi di Roma ‘Sapienza’—Azienda Ospedaliera Sant’Andrea, Rome, Italy); Rocco Mollace, MD (Department of Cardiology, University of Rome Tor Vergata, Rome, Italy); and Elisa Carturan, BSc, PhD (Department of Cardiac, Thoracic and Vascular Sciences and Public Health, University of Padua, Padua, Italy).
Funding: The authors report no specific funding related to this article.
Conflict of interest: The authors have submitted their declaration which can be found in the article Supplementary Material online.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


