Abstract
The Coronavirus Disease 2019 (COVID-19) epidemic has unprecedently affected many aspects of people’s lives including their health. This study examined the mediating effect of COVID-19 coping strategies on the relationship between COVID-19 anxiety and general health. Participants (70% females) included 4624 adults (Mage = 30.29 ± 10.97 years) collected through an online survey using a convenience sampling approach. Exploratory and confirmatory factor analyses yielded a one-factor structure for the COVID-19 Anxiety Scale (CFI = .98, TLI = .96, SRMR = .02, RMSEA = .09), COVID-19 Coping Scale (CFI = .97, TLI = .97, SRMR = .03, RMSEA = .12), and General Health Scale (CFI = .99, TLI = .97, SRMR = .01, RMSEA = .04) which were developed for the purpose of this study and exhibited satisfactory reliability. Findings showed that COVID-19 anxiety was negatively related with COVID-19 coping and general health. COVID-19 coping had a positive relationship with general health. Hierarchical multiple regression analyses revealed that COVID-19 coping partially mediated the relationship between COVID-19 anxiety and general health. These findings shed more light on the mechanism underlying between COVID-19 anxiety and health. The findings are important for tailoring and implementing coping-based intervention strategies to reduce the impact of COVID-19 anxiety on general health.
Keywords: COVID-19 anxiety, COVID-19 coping, General health, Coronavirus
The COVID-19 pandemic has spread around the world exponentially since it first appeared in China on December 2019. The virus has become a major health concern affecting almost all aspects of individuals’ lives. By 5 October 2020, statistics show that there were more than 35,241,000 confirmed COVID-19 cases and more than 1,038,000 deaths worldwide. In Turkey, the number of confirmed COVID-19 cases and deaths were respectively more than 324,000 and 8400 (Center for Systems Science and Engineering 2020). To prevent and control the COVID-19 pandemic, the Turkish government has taken various measures such as testing, isolation, tracing, and limiting the movement of individuals both within and across the country (Yıldırım and Güler 2020). Undoubtedly, as implementing such measures have been found to be effective to protect physical health of people against COVID-19, the risks of a second or third wave of the pandemic may cause fear, uncertainties, and anxiety among people globally (Yıldırım and Güler 2020).
The COVID-19 pandemic undoubtedly creates a general atmosphere of anxiety, fear, uncertainty, and insecurity (Ahorsu et al. 2020) that needs to be psychologically investigated via well-designed studies in order to better comprehend its negative impacts on individuals’ health. People adopt various personal strategies to cope with such challenging situations to protect their health. As such, this study examined the mediating role of COVID-19 coping strategies on the relationship between COVID-19 anxiety and general health.
By definition, anxiety is the natural waring system of the body representing the likelihood of a potential danger and action used to address it (Hooley et al. 2016). Anxiety frequently occurs in the face of a new and unknow situation. The current COVID-19 pandemic and earlier outbreaks like SARS in 2003 and MERS-CoV in 2014 resulted in a great amount of psychological distress among people in infected areas (de Pablo et al. 2020). Studies demonstrated that negative effects of psychological responses (i.e. anxiety, depression, stress, fear) affect health and well-being of people in times of health crisis (Pappas et al. 2009; Wu et al. 2005).
Due to COVID-19, mental health illnesses including anxiety, depression, stress, and sleep disorder have become prevalent problems across the world. People who are under the high risk of infection, stress, and burnout can develop common mental health problems such as anxiety, depression, and fear (Bao et al. 2020; Tanhan 2020). For example, studies related to COVID-19 conducted in Turkey reported high levels of anxiety, stress, depression and burnout (Yildirim et al. 2020; Tanhan et al. 2020; Yıldırım and Solmaz 2020), and death distress (Yıldırım and Güler 2020). There have also been various studies that have investigated the prevalence of psychological distress among different populations during the pandemic. For instance, in Italy the prevalence rates of mental health problems have been reported as 49.38% for post-traumatic stress disorders, 24.73% for depression, 21.90% for anxiety, and 19.80% for perceived stress among healthcare workers (Rossi et al. 2020). Among general population in China, the prevalence of depressive symptoms, anxiety, and stress ranging from moderate to severe were respectively 16.5%, 28.8%, and 8.1% (Wang et al. 2020). High rates of anxiety, depression, stress, and other negative emotions have also been reported in the UK (The Academy of Medical Sciences 2020).
Recent research has documented various contributing factors to psychosocial and physical health such as demographic, psychological, and behavioural factors during outbreaks (Tanhan et al., 2020; Yıldırım and Arslan 2020). These factors include optimism-pessimism, psychological flexibility, hope, resilience, fear, vulnerability, perceived risk, and preventive behaviours (Arslan et al. 2020; Yıldırım and Arslan 2020; Yıldırım et al. 2020). Stress management strategies have been found to reduce maladaptive coping strategies including avoidance, antagonistic confrontation, and self-blame which have been linked with worse mental health outcomes (Maunder et al. 2006; Sim et al. 2010). Despite these studies on various indices of psychological health, there is a knowledge gap linking to mechanism underlying the relationship between anxiety and psychological health in general population during the COVID-19 pandemic.
Mediating Effect of Coping
Psychological research has largely focused on negative states, their predictive factors, correlates, and consequences of COVID-19 on human health and life. Psychological strengths like coping strategies have been relatively neglected in addressing psychological distress during outbreaks. According to the transactional model, stress occurs when environmental or internal demands are appraised by a person as exceeding or taxing their ability to cope (Folkman, 2008; Lazarus and Folkman 1984). Theoretical approaches of coping emphasized strategies used to reduce distress. Coping has been researched in numerous environments and contexts (Carver et al. 1989; Yıldırım 2019).
During current and past infectious disease outbreak, people have used various coping strategies to deal with challenges stemmed from the diseases (Salopek-Žiha et al. 2020). While those who adopt adaptive coping styles can effectively overcome challenges and obstacles during outbreaks, others may suffer from psychopathological problems. A small number of studies have investigated the role of coping construct in the context of COVID-19. In a systematic review and narrative synthesis of the available evidence on contagious diseases, Chew et al. (2020) reported that people use a wide range of coping strategies (i.e. problem focused-coping, avoidance, seeking social support, and positive appraisal of the situation) to deal with negative psychological outcomes resulted from outbreaks such as fear, anxiety, depression, post-traumatic stress disorders, anger, grief and loss, guilt, and stigmatization. Furthermore, Tanhan (2020) suggests that utilizing an online photovoice approach can be an effective way to deal with biopsychosocial spiritual and economic issues during the COVID-19 pandemic. He argued that such a method can contribute to empowering people and communities to improve their well-being and address biopsychosocial, spiritual, and economic issues via advocacy and collaboration with people, communities, and key individuals and institutions. Studies on Philippine teachers’ and students’ practices to cope with anxiety during the COVID-19 outbreak found that information seeking, preventive behaviours, spending time with family, seeking spiritual guidance, talking with friends online, using social media, playing online games, avoiding media news about COVID-19 fatalities, and other coping mechanisms were among the most common practiced coping strategies to tackle with anxiety during the quarantine period (Baloran 2020; Talidong and Toquero 2020). Similar coping styles have been reported in earlier studies where following strict personal preventive behaviours and avoidance of going to public places to minimize the risk of infectious have been highly practiced (Faye et al. 2015; Khalid et al. 2016).
Within the wider literature, coping strategies have been found to be associated with a wide range of factors. Adaptive coping (i.e. problems-focused and positive reappraisal coping strategies) has been found to be negatively related with depressive symptoms (Erickson & Feldstein 2007), anxiety (Brouzos et al. 2020), and stress (Viana Machado et al. 2020). Maladaptive coping strategies (i.e. emotional and avoidance coping strategies) were negatively associated with psychological well-being and resilience (Mayordomo et al. 2016), humour and adjustment (Erickson and Feldstein 2007), optimism (Scheier et al. 1986), and self-esteem (Brouzos et al. 2020). Accordingly, identifying coping strategies used in response to infectious disease outbreaks is critical to support the general public in tackling with the pandemic.
Present Study
Given the lack of current empirical evidence on the psychological factors affecting general health in the context of COVID-19, this study aims to contribute to the extant literature in general health during the COVID-19 pandemic and incorporates the study of COVID-19 anxiety and coping using a large Turkish sample. Therefore, we investigated whether these potential variables provide explanatory power in the prediction of general health and whether COVID-19 coping explains the underlying mechanism in the relationship between COVID-19 anxiety and general health. This study aimed to examine the associations between COVID-19 anxiety, COVID-19 coping, and general health. Specifically, we hypothesized that (i) COVID-19 anxiety would have a significant direct effect on COVID-19 coping and general health; (ii) COVID-19 coping would have a significant direct effect on general health; and (iii) COVID-19 coping would function as a significant mediator in the relationship between COVID-19 anxiety and general health. The hypothesized structural model is presented in Fig. 1.
Fig. 1.
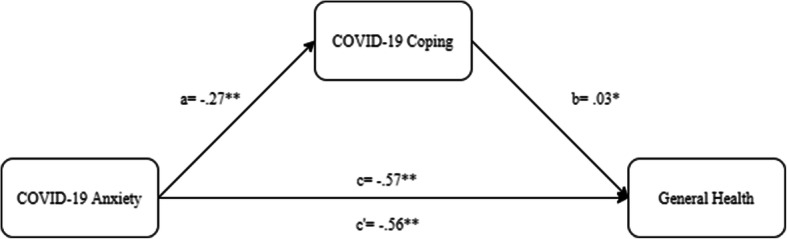
Final schematic diagram in the mediational effects of the COVID-19 coping on the relations between COVID-19 anxiety and general health
Method
Participants
Using a convenience sampling approach, in all, 4624 people were drawn from the general population in Turkey. Participants ranged in age between 18 and 88 years and their mean age was 30.29 (SD = 10.93) years. They were mostly females (70%), single (58%), university students/graduate (63%), and belonging to the medium socio-economic status group (77%). Participants predominantly reported no history of chronic diseases (86%). Participation of this study was voluntary, and participants were not given any incentive for their participation.
Measures
Anxiety
COVID-19 anxiety was measured with five items developed for the purpose of this study. Example item is “I feel anxious about my future due to COVID-19”. Items are scored on a five-point scale ranging from 1 (never) to 5 (always), giving a potential range of 5–25. Higher scores indicate greater anxiety associated with COVID-19. Cronbach’s alpha for the present sample was α = .84.
Coping
For this study, participants were asked to rate four items (“I believe that I have an ability to cope with the COVID-19”) on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), giving a potential range of 4–20. Higher scores show higher levels of COVID-19-related coping strategies. Cronbach’s alpha for the present sample was α = .71.
General Health
In this study, general health was assessed with three questions “During COVID-19, how often have you had trouble with sleep?” answered on a five-point Likert scale ranging from 1 (never) to 5 (always), giving a potential range of 3–15. Lower scores refer to better health status. Cronbach’s alpha for the present sample was α = .58, which is relatively low. However, poor internal consistency reliability can be expected in case of low number of items on a scale (Tavakol and Dennick 2011).
Procedure
There was scarcity of the scales related to the COVID-19 pandemic specific anxiety, coping, and general health at the time of conducting this study. Therefore, all abovementioned scales were developed for the purpose of the current study. They were developed through consensus by the authors of this study and two expert consultants who actively work in the field of psychology. We created the scales by reviewing the relevant studies and previously used measures that assessed anxiety, coping, and general health.
The data for this cross-sectional study came from a larger project on psychological factors affecting psychosocial and physical health of general public in Turkey during the COVID-19 pandemic. We used Google documents as a platform to design the surveys that automatically produced a unique URL. The URL was shared on social networking sites such as Twitter and Facebook. All participants completed online versions of the scales as part of questionnaire batteries being conducted for other studies. A consent was obtained from all participants who have been fully instructed about their rights to withdraw from the study at any time points. Before involvement in the study, participants were required to indicate their agreement with a yes-no question to confirm their willingness to partake in voluntarily. The questionnaires were presented to the participants in the same order. The data were collected between 17 March and 1 April 2020 during the early state of COVID-19 in Turkey.
Data Analysis
Initially, the means, standard deviations, tests of normality (i.e. skewness and kurtosis), and internal consistency reliability coefficients of the items and scales were estimated. Tests of normality assumptions demonstrated that the data were approximately normally distributed. Tests of skewness and kurtosis for individual items and variables fall within the adequate range of ≤ |3| (D’Agostino et al. 1990; Kline 2015). Participants were randomly split into two subsamples; the exploratory factor analysis (EFA) was performed on the first subsample (n = 2.382) and the confirmatory factor analysis (CFA) was carried out on the second subsample (n = 2.242). Correlation analysis was computed to explore the relationships between the measured variables. The regression analysis met the assumptions of normality, independence of errors, and homoscedasticity. Following the recommendations of Baron and Kenny (1986), three regression models were executed to test the mediating effect of the COVID-19 coping on the relationship between the COVID-19 anxiety and general health. Firstly, the regression analysis was conducted to test the predictive effect of COVID-19 anxiety on general health. Secondly, the COVID-19 coping was entered into the model to determine its effect on general health. Thirdly, both COVID-19 anxiety and coping were simultaneously included in the model to predict general health. If the predictive effect of COVID-19 anxiety on general health was no longer significant after controlling for the effect of COVID-19 coping, this would suggest full mediation. However, if the predictive effect of COVID-19 anxiety on general health remained significant after controlling for the impact of the COVID-19 coping, partial mediation would be drawn. Finally, the bootstrap approach with 5000 resamples to estimate the 95% confidence intervals (Hayes 2018; Preacher and Hayes 2008) was conducted to determine if the indirect effects of COVID-19 anxiety through mediating role of COVID-19 coping were statistically significant. Analyses were carried out using SPSS and AMOS v24 for Windows.
Results
Descriptive Analysis
Table 1 presents the means, standard deviations, skewness scores, kurtosis scores, corrected item-total correlations, alpha if the item was deleted, and factor loadings for the three scales. The mean scores for the individual items ranged from 2.69 to 3.81. In all scales, the corrected item-total correlations for individual items were above 0.35, suggesting their appropriateness for scale construction (Tabachnick and Fidell 2007). Except one item (.37), all items had factor loadings above .51, representing “fair” to “excellent” (Comrey and Lee 1992).
Table 1.
Descriptive statistics of the COVID-19 Anxiety Scale, COVID-19 Coping Scale, and General Health Scale
| Item | M | SD | sk | ku | rit | αiid | EFA loading |
|---|---|---|---|---|---|---|---|
| COVID-19 Anxiety Scale | |||||||
| 1. I feel anxious about my future due to the COVID-19. | 3.81 | 0.84 | − 0.17 | − 0.27 | 0.68 | 0.84 | 0.76 |
| 2. I feel anxious about my health because of the COVID-19. | 3.78 | 0.79 | − 0.05 | − 0.29 | 0.74 | 0.82 | 0.83 |
| 3. I feel anxious to contract COVID-19. | 3.72 | 0.78 | − 0.02 | − 0.09 | 0.70 | 0.83 | 0.77 |
| 4. I am preoccupied with anxious thoughts of getting infected to the COVID-19. | 3.61 | 0.79 | 0.04 | 0.10 | 0.68 | 0.84 | 0.73 |
| 5. I am concerned that the COVID-19 will affect all aspects of my life. | 3.70 | 0.83 | − 0.05 | − 0.22 | 0.63 | 0.85 | 0.66 |
| COVID-19 Coping Scale | |||||||
| 1. I believe that I have the ability to cope with the COVID-19. | 3.04 | 0.86 | − 0.09 | 0.39 | 0.35 | 0.72 | 0.34 |
| 2. I am able to enjoy my life despite the COVID-19. | 2.71 | 0.93 | 0.02 | 0.17 | 0.49 | 0.64 | 0.55 |
| 3. I can get through the COVID-19. | 2.69 | 0.81 | − 0.15 | 0.84 | 0.61 | 0.57 | 0.84 |
| 4. I can still focus on the meaning of my life even during the COVID-19. | 2.97 | 0.90 | − 0.02 | 0.36 | 0.52 | 0.62 | 0.74 |
| General Health Scale | |||||||
| 1. During the COVID-19, how often have you had trouble with sleep? | 2.77 | 0.69 | − 0.70 | 2.41 | 0.39 | 0.46 | 0.58 |
| 2. How often have you had difficulty concentrating on your daily routine since the COVID-19 had occurred? | 2.77 | 0.83 | − 0.17 | 0.77 | 0.37 | 0.52 | 0.50 |
| 3. How often have you felt that you are under stress due to the COVID-19? | 2.79 | 0.65 | − 0.74 | 2.72 | 0.41 | 0.45 | 0.59 |
M mean, sk skewness, ku kurtosis, rit corrected item-total correlation, αiid Cronbach’s alpha if item deleted
Exploratory Factor Analysis
EFA using maximum likelihood estimation was performed separately for each of the scale. The factor analysis results yielded Kaiser–Meyer–Olkin (KMO) values of 0.86 for the anxiety (X2 = 5353.43, p < .001), 0.68 (X2 = 2096.27, p < .001) for the coping, and 0.63 (X2 = 625.16, p < .001) for general health scales. The EFA also supported that for all scales, a one-factor solution was the most appropriate, with a first initial factor producing an Eigenvalue of 3.27 explaining 65% of the variance for anxiety, 2.17 explaining 54% of the variance for coping, and 1.62 accounting for 54% of the variance for general health. All items loaded positively on the respective factors.
Confirmatory Factor Analysis
The factor structure of the three scales was verified using CFA. The results were assessed based on data-model fit statistics and their cut-off scores: the root mean square error of approximation (RMSEA) and the standardized root mean squared residual (SRMR) values between .05 and .10 = adequate fit; the comparative fit index (CFI) and the Tucker-Lewis fit index (TLI) > .95 = close fit and values between .90 and .95 = adequate fit (Hooper et al. 2008; Kline 2015). The results of CFA for each of the scales were CFI = .98, TLI = .96, SRMR = .02, and RMSEA [95% CI] = .09 [.08, .11] for anxiety; CFI = .97, TLI = .97, SRMR = .03, and RMSEA [95% CI] = .12 [.09, .14] for coping; and CFI = .99, TLI = .97, SRMR = .01, and RMSEA [95% CI] = .04 [.02, .7] for general health. This indicates satisfactory model-data fit.
Correlation Analysis
Correlation analysis was conducted to explore the relationships between the variables (see Table 2). Results showed that COVID-19 anxiety was negatively significantly correlated with COVID-19 coping (r = − .27, p < .001) and general health (r = − .57, p < .001). COVID-19 coping was significantly positively correlated with general health (r = .18, p < .001). The correlation coefficients ranged from small to large based on a conventional frame where .1 ≤ r < .3 presents a small effect, .3 ≤ r < .5 presents a medium effect, and r ≥ .5 presents a large effect (Cohen 1988).
Table 2.
Descriptive statistics and correlation results
| Variable | Mean | SD | Skewness | Kurtosis | α | 1. | 2. | 3. |
|---|---|---|---|---|---|---|---|---|
| 1. COVID-19 anxiety | 18.62 | 3.24 | 0.03 | 0.15 | .84 | 1 | − .27** | − .57** |
| 2. COVID-19 coping | 11.42 | 2.55 | − 0.25 | 1.22 | .71 | 1 | .18** | |
| 3. General health | 8.32 | 1.61 | − 0.79 | 2.38 | .58 | 1 |
**p < .01
Model Testing
Using regression analysis, a path model was constructed whereby the COVID-19 anxiety was exogenous variable, the COVID-19 coping was the mediating variable, and general health was the dependent variable (see Table 3). In step 1, the direct effect from the COVID-19 anxiety to general health was negative and significant (β = − .57, p < .01). In step 2, the direct effect of the COVID-19 anxiety on COVID-19 coping was negative and significant (β = − .27, p < .01). In step 3, both COVID-19 anxiety and coping were entered into the regression model and the results indicated that both of these variables significantly contributed to the prediction of general health by explaining 32% of total variance. These findings show that COVID-19 coping partially mediated the relationship between COVID-19 anxiety and general health.
Table 3.
Coefficients for the mediating effect
| Step | Outcome | Predictor | B | SE | β | t | p | r2 |
|---|---|---|---|---|---|---|---|---|
| Step 1 (path c) | General health | Anxiety | − 0.28 | 0.01 | − 0.57 | − 46.93 | 0.00 | 0.32 |
| Step 2 (path a) | Coping | Anxiety | − 0.21 | 0.01 | − 0.27 | − 19.30 | 0.00 | 0.08 |
| Step 3 (path c′) | General health | Anxiety | − 0.28 | 0.01 | − 0.56 | − 44.52 | 0.00 | — |
| — | — | Coping | 0.02 | 0.01 | 0.03 | 2.37 | 0.02 | 0.32 |
The bootstrapping method with bias-corrected confidence intervals was computed to test the mediating effect of COVID-19 coping on the association between COVID-19 anxiety and general health. The results of mediation analysis supported our hypothesis about the mediating effect of COVID-19 coping on the COVID-19 anxiety and general health (B = .02; 95% CI = .00 to .04). The structural model is depicted in Fig. 1.
Discussion
While burgeoning research has considerably aimed to determine the prevalence of mental health problems during the COVID-19 pandemic (Liu et al. 2020), relatively little research has focused upon the potential factors that explain the underlying mechanism between pandemic-related stressors and general health. Accordingly, this study aimed to examine the role of COVID-19 coping in the relationship between COVID-19 anxiety and general health in a representative sample of Turkish population. In general, the findings supported the three main hypotheses which are discussed in more details below.
Firstly, COVID-19 anxiety had significant direct effects on COVID-19 coping and general health, which is parallel with findings from earlier research (Baloran 2020; Chew et al. 2020; Talidong and Toquero 2020). This suggests that experience of COVID-19 anxiety negatively affects the ability to cope with stress in the context of COVID-19 and general health.
Secondly, COVID-19 coping had significant direct effects on general health. Past research has also showed that coping is an important factor in contributing psychosocial and physical health of individuals (Yıldırım 2019). Individuals high in adaptive coping strategies experience less depression (Erickson and Feldstein, 2007), anxiety (Brouzos et al. 2020), and stress (Viana Machado et al. 2020) and greater psychological well-being (Mayordomo et al. 2016).
Finally, as expected COVID-19 coping acted as a construct to mediate the relationship between COVID-19 anxiety and general health. This result incorporates with the findings of past research (Cappeliez and Robitaille 2010; Cooper et al. 2008). This implies that when people suffer from COVID-19-related anxiety, it is more likely that they will have an inability to cope with stress which in turn leads them to have poor general health. This indeed provides a mechanism that could partially explain why COVID-19 anxiety diminishes general health, with that involving inability to cope with stress. Accordingly, experience of anxiety is likely to contribute to vulnerability to stress in the forms of low capability to deal with stressors which leads to worsen general health. However, it is important to note that mediation analysis suggests longitudinal causality, which cannot be inferred with cross-sectional data (MacKinnon et al. 2007).
With regard to the psychometric properties of the scales used in the current study, we found that the one-factor structure of the all three scales has been supported and they had acceptable to good internal consistency coefficients. The scales were also related to one another. The aforementioned scales can be used as screening tools to assess COVID-19 anxiety, COVID-19 general coping strategies, and general health.
This study has several theoretical and practical contributions. In terms of theory, the study expands the predictors of general health through demonstrating COVID-19 coping as a significant explanatory factor in the association between COVID-19 anxiety and general health. Past studies have examined the protective roles of coping strategies in protecting mental health following trauma (Park et al. 2015). This study did not only provide direct evidence that the ability of dealing effectively with difficult situations such as COVID-19 can significantly contribute to protect general health but the study also contributed to our understanding on the mechanism of how COVID-19 anxiety influences general health via COVID-19 coping. While coping strategies have been determined as linking with anxiety to influence health (Eisenberg et al. 2012), findings from this research provide implications for future studies to further examine such mechanism beyond Turkish population. Employing different samples is useful, because people use different coping strategies and some people seem to cope with adversity better than others.
In terms of practice, the findings suggest that as COVID-19 anxiety significantly predicts general health through the mediating effect of COVID-19 coping, practitioners are recommended to tailor and implement contextually sensitive interventions and programs that incorporate COVID-19 anxiety as a key element. Implementing such COVID-19-specific interventions has been recommended by previous studies (Tanhan 2020; Tanhan et al. 2020). For instance, using psychological strength–based interventions in the form of minimizing COVID-19 anxiety may be particularly fruitful for people who experience psychological distress, given that it hinders the ability to cope with stress instead of actively engage in solving the problems. Practitioners are also encouraged to focus on psychological treatments that could strengthen the ability of individuals to manage stressful situations. With this capability, these people may accordingly realize the potential of personal strengths which could potentially mitigate their levels of anxiety.
This study used a cross-sectional design, which limits conclusion from cause-and-effect relation to be inferred. Notwithstanding, the present findings present guidance for future investigations on potential causal relations among the study variables. Another limitation of this study is that participants were largely female, single, university students/graduate, and belonging to the medium socio-economic status group. The generalizability of these findings to other samples with different socio-demographic characteristics is limited. Furthermore, future studies can examine the role of other variables including demographic variables that may influence the associations among the measured variables. Finally, the COVID-19 coping and general health scales produced a relatively poor internal consistency reliability. Although scales with low number of items are likely to produce poor reliability, they should be used with caution in future research.
In conclusion, the present study is the first to examine the role of COVID-19 coping in the relationship between COVID-19 anxiety and general health. The results supported the notion that COVID-19 coping reduces the impact of COVID-19 anxiety on general health. Therefore, the results underscore a need for researchers and practitioners to develop and implement coping-based intervention strategies to protect the general health of individuals against stressors emerged in difficult times.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Consent was obtained from all participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction. 2020;1:9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arslan G, Yıldırım M, Tanhan A, Buluş M, Allen KA. Coronavirus stress, optimism-pessimism, psychological inflexibility, and psychological health: testing the psychometrics of the coronavirus stress measure. International Journal of Mental Health and Addiction. 2020;1:17. doi: 10.1007/s11469-020-00337-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baloran ET. Knowledge, attitudes, anxiety, and coping strategies of students during COVID-19 pandemic. Journal of Loss and Trauma. 2020;25:1–8. doi: 10.1080/15325024.2020.1769300. [DOI] [Google Scholar]
- Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. The Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brouzos A, Vassilopoulos SP, Vlachioti A, Baourda V. A coping-oriented group intervention for students waiting to undergo secondary school transition: effects on coping strategies, self-esteem, and social anxiety symptoms. Psychology in the Schools. 2020;57(1):31–43. doi: 10.1002/pits.22319. [DOI] [Google Scholar]
- Cappeliez P, Robitaille A. Coping mediates the relationships between reminiscence and psychological well-being among older adults. Aging & Mental Health. 2010;14(7):807–818. doi: 10.1080/13607861003713307. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Center for Systems Science and Engineering. (2020). Coronavirus COVID-19 global cases at Johns Hopkins University. Available from https://coronavirus.jhu.edu/map.html
- Chew, Q. H., Wei, K. C., Vasoo, S., Chua, H. C., & Sim, K. (2020). Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Medical Journal. Advance online publication. 10.11622/smedj.2020046. [DOI] [PMC free article] [PubMed]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Comrey AL, Lee HB. A first course in factor analysis. Hillsdale, NJ: Erlbaum; 1992. [Google Scholar]
- Cooper C, Katona C, Orrell M, Livingston G. Coping strategies, anxiety and depression in caregivers of people with Alzheimer’s disease. International Journal of Geriatric Psychiatry: A Journal of the Psychiatry of Late Life and Allied Sciences. 2008;23(9):929–936. doi: 10.1002/gps.2007. [DOI] [PubMed] [Google Scholar]
- D’Agostino RB, Belanger A, D’Agostino RB. A suggestion for using powerful and informative tests of normality. The American Statistician. 1990;44(4):316–321. [Google Scholar]
- de Pablo GS, Serrano JV, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. Journal of Affective Disorders. 2020;275:48–57. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg SA, Shen BJ, Schwarz ER, Mallon S. Avoidant coping moderates the association between anxiety and patient-rated physical functioning in heart failure patients. Journal of Behavioral Medicine. 2012;35(3):253–261. doi: 10.1007/s10865-011-9358-0. [DOI] [PubMed] [Google Scholar]
- Erickson SJ, Feldstein SW. Adolescent humor and its relationship to coping, defense strategies, psychological distress, and well-being. Child Psychiatry and Human Development. 2007;37(3):255–271. doi: 10.1007/s10578-006-0034-5. [DOI] [PubMed] [Google Scholar]
- Faye O, Boelle PY, Heleze E, Faye O, Loucoubar C, Magassouba N, Soropogui B, Keita S, Gakou T, Bah el HI, Koivogui L, Sall AA, Cauchemez S. Chains of transmission and control of Ebola virus disease in Conakry, Guinea, in 2014: an observational study. The Lancet. 2015;15(3):320–326. doi: 10.1016/S1473-3099(14)71075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S. The case for positive emotions in the stress process. Anxiety, Stress and Coping. 2008;21(1):3–14. doi: 10.1080/10615800701740457. [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press.
- Hooley JM, Butcher JN, Matthew KN, Mineka S. Abnormal psychology. Boston: Pearson; 2016. [Google Scholar]
- Hooper D, Coughlan J, Mullen MR. Structural equation modelling: guidelines for determining model fit. Electronic Journal of Business Research Methods. 2008;6(1):53–60. [Google Scholar]
- Khalid I, Khalid T, Qabajah M, Barnard A, Qushmaq I. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clinical Medicine & Research. 2016;14(1):7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford; 2015. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, Wu L, Sun Z, Zhou Y, Wang Y, Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Research. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayordomo T, Viguer P, Sales A, Satorres E, Meléndez JC. Resilience and coping as predictors of well-being in adults. The Journal of Psychology. 2016;150(7):809–821. doi: 10.1080/00223980.2016.1203276. [DOI] [PubMed] [Google Scholar]
- Pappas G, Kiriaze IJ, Giannakis P, Falagas ME. Psychosocial consequences of infectious diseases. Clinical Microbiology and Infection. 2009;15(8):743–747. doi: 10.1111/j.1469-0691.2009.02947.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park M, Chang ER, You S. Protective role of coping flexibility in PTSD and depressive symptoms following trauma. Personality and Individual Differences. 2015;82:102–106. doi: 10.1016/j.paid.2015.03.007. [DOI] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open. 2020;3(5):e2010185–e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salopek-Žiha D, Hlavati M, Gvozdanović Z, Gašić M, Placento H, Jakić H, et al. Differences in distress and coping with the COVID-19 stressor in nurses and physicians. Psychiatria Danubina. 2020;32(2):287–293. doi: 10.24869/psyd.2020.287. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Weintraub JK, Carver CS. Coping with stress: divergent strategies of optimists and pessimists. Journal of Personality and Social Psychology. 1986;57(6):1024–1040. doi: 10.1037/0022-3514.57.6.1024. [DOI] [PubMed] [Google Scholar]
- Sim K, Chan YH, Chong PN, Chua HC, Soon SW. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. Journal of Psychosomatic Research. 2010;68(2):195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. New York: Allyn & Bacon; 2007. [Google Scholar]
- Talidong KJB, Toquero CMD. Philippine teachers’ practices to deal with anxiety amid COVID-19. Journal of Loss and Trauma. 2020;25:1–7. doi: 10.1080/15325024.2020.1759225. [DOI] [Google Scholar]
- Tanhan A. COVID-19 Sürecinde Online Seslifoto (OSF) Yöntemiyle Biyopsikososyal Manevi ve Ekonomik Meseleleri ve Genel İyi Oluş Düzeyini Ele Almak: OSF’nin Türkçeye Uyarlanması. Electronic Turkish Studies. 2020;15(4):1029–1086. doi: 10.7827/TurkishStudies.44451. [DOI] [Google Scholar]
- Tanhan A, Yavuz KF, Young JS, Nalbant A, Arslan G, Yıldırım M, Çiçek İ. A proposed framework based on literature review of online contextual mental health services to enhance wellbeing and address psychopathology during COVID-19. Electronic Journal of General Medicine. 2020;17(6):em254. doi: 10.29333/ejgm/8316. [DOI] [Google Scholar]
- Tavakol M, Dennick R. Making sense of Cronbach’s alpha. International Journal of Medical Education. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Academy of Medical Sciences. (2020). Survey results: understanding people’s concerns about the mental health impacts of the COVID-19 pandemic. Available at https://acmedsci.ac.uk/file-download/99436893
- Viana Machado A, Volchan E, Figueira I, Aguiar C, Xavier M, Souza GG, et al. Association between habitual use of coping strategies and posttraumatic stress symptoms in a non-clinical sample of college students: a Bayesian approach. PLoS One. 2020;15(2):e0228661. doi: 10.1371/journal.pone.0228661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yıldırım M. Irrational happiness beliefs: conceptualization, measurement and its relationship with well-being, personality, coping strategies, and arousal. Leicester: University of Leicester; 2019. [Google Scholar]
- Yıldırım, M., & Arslan, G. (2020). Exploring the associations between resilience, dispositional hope, preventive behaviours, subjective well-being, and psychological health among adults during early stage of COVID-19. Current Psychology, 1–11. 10.1007/s12144-020-01177-2. [DOI] [PMC free article] [PubMed]
- Yıldırım M, Güler A. Positivity explains how COVID-19 perceived risk increases death distress and reduces happiness. Personality and Individual Differences. 2020;168:110347. doi: 10.1016/j.paid.2020.110347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yıldırım, M., & Solmaz, F. (2020). COVID-19 burnout, COVID-19 stress and resilience: initial psychometric properties of COVID-19 Burnout Scale. Death Studies, 1–9. 10.1080/07481187.2020.1818885. [DOI] [PubMed]
- Yıldırım, M., Arslan, G. & Özaslan, A. (2020). Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: exploring the mediating effects of resilience and coronavirus fear. International Journal of Mental Health and Addiction, 1–11. 10.1007/s11469-020-00424-8. [DOI] [PMC free article] [PubMed]
- Yıldırım M, Geçer E, Akgül Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Health & Medicine: Psychology; 2020. pp. 1–9. [DOI] [PubMed] [Google Scholar]


