Abstract
We proposed a combined cardiothoracic-MRI (CaTh-MRI) protocol for the comprehensive assessment of cardiovascular structures, lung parenchyma, and pulmonary arterial tree, in COVID-19 patients with progressive worsening of clinical conditions and/or suspicion of acute-onset myocardial inflammation. A 25-minutes fast protocol was also conceived for unstable or uncooperative patients by restricting the number of sequences to those necessary to rule out myocardial and to assess pulmonary involvement. In patients requiring CMR characterization of myocardial damage, the addition of lung and thoracic vessel evaluation is of clinical benefit at a minimal time expense.
Keywords: COVID-19, SARS-CoV-2, cardiovascular magnetic resonance, myocarditis, lung magnetic resonance imaging, pulmonary magnetic resonance angiography
Background
Besides pulmonary manifestations, a high incidence of thrombo-embolic events and cardiac complications has been reported in COVID-19, reflecting the multi-systemic nature of severe acute respiratory syndrome coronavirus 2 infection.1
Myocardial injury, with elevation of troponins, was found in around 17% of hospitalized patients with COVID-19, yielding relevant prognostic implications, with worse clinical course and higher mortality rate.1
The underlying pathological mechanisms have not been fully elucidated yet, likely depending on a combination of direct viral injury and an uncontrolled immune-activation (the so-called ‘cytokine storm’), with subsequent systemic inflammation and the generation of a prothrombotic status.2
Cardiovascular magnetic resonance (CMR) integrates an accurate anatomical and functional assessment of the heart with the characterization of myocardial tissue changes associated with COVID-19. The combined use of conventional pulse sequences with recently developed and purely quantitative T1 and T2 mapping techniques enables to reveal myocardial injury and to discriminate among the different patterns of damage (especially between inflammatory and ischaemic), even in subtle forms and subacute setting.3
Non-invasive recognition of interstitial myocardial oedema, contractile dysfunction, cardiomyocyte necrosis, and ultimately fibrotic replacement by CMR can be supplemented by the assessment of thoracic vascular structures and lung parenchyma. This is particularly relevant in COVID-19 patients due to the high prevalence of pulmonary thrombo-embolic complications, which have been reported to significantly impact patients’ outcome.1
Although computed tomography (CT) angiography remains the primary diagnostic tool to detect pulmonary embolism (PE), pulmonary magnetic resonance angiography (MRA) may also reveal PE as direct visualization of filling defects in the pulmonary artery and/or as parenchymal perfusion defects during the first pass of the contrast agent by dynamic sequences, with high negative predicting value.4
Therefore, in patients performing CMR, the acquisition of an additional pulmonary MRA sequence could help to identify those who would benefit from more aggressive anticoagulation therapy without any disadvantages in terms of exam duration.
Furthermore, as demonstrated by Ates et al.,5 lung MRI may detect both parenchymal and extraparenchymal findings, with nearly complete CT overlap.
Therefore, as an additional strength to be exploited in the complex COVID-19 disease model, MRI could supply a radiation-free evaluation of lung involvement in a patient with known or clinically suspected interstitial pneumonia, in certain cases avoiding unnecessary CT scans.
Embedding lung MRI sequences in a CMR protocol could be a valid example of optimization of imaging resources, helping the assessment of the response to therapy or the progression of the disease with only a minimal time expense.
We propose a combined cardiothoracic-MRI (CaTh-MRI) protocol, that could provide a ‘one stop-shop’ evaluation of cardiovascular structures, lung parenchyma, and pulmonary arterial tree, in COVID-19 patients with progressive worsening of clinical conditions and/or suspicion of acute-onset myocardial inflammation.
Patient selection or clinical indication
Our patient’s population included a cohort of individuals with reverse transcriptase-polymerase chain reaction confirmed diagnosis of active COVID-19 and CT demonstration of pulmonary involvement.
At least one of the following inclusion criteria was additionally required:
High sensitivity troponin T levels > 0.014 ng/mL in absence of ST-elevation or other signs of myocardial infarction;
New-onset left ventricular (LV) systolic dysfunction of uncertain aetiology at fast bed-side echocardiography;
Infarct-like clinical presentation in patients with no obstructive coronary artery disease at invasive coronary angiography;
Exclusion criteria were the following:
Patients with a high pre-test probability of PE according to a preliminary clinical triage (Wells score >4), who were directly addressed to CT angiography.
General contraindications to CMR
Imaging protocol
The CaTh-MRI protocol has been implemented on a 1.5 T MRI unit with a 16-channel phased array surface coil.
Staff members were equipped with contact precautions (filtering facepiece 2 mask, eye shield, gown, and gloves) and reduced in number to the minimum necessary (i.e. one technologist and one radiologist in the control room plus one nurse in the scanning room).
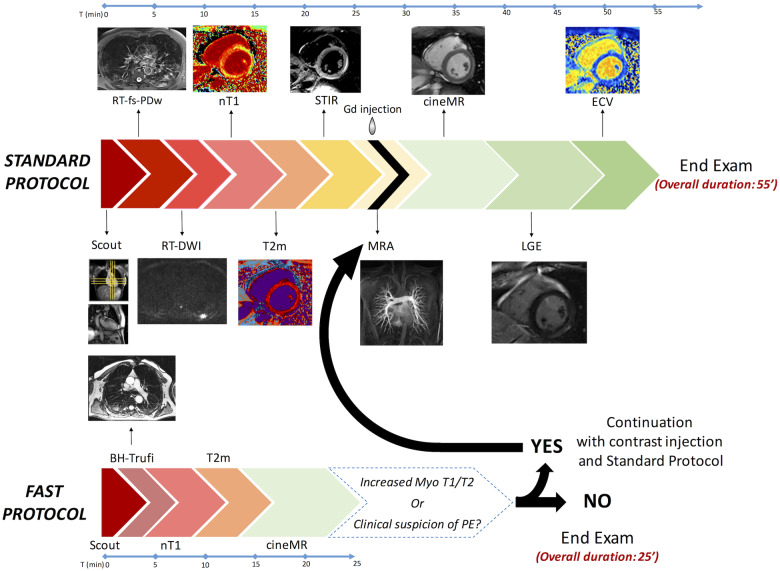
Given the heterogeneity of clinical presentations, ranging from asymptomatic or subclinical forms to critical patients, we designed two specific protocols based on patients’ compliance (Figure 1).
Figure 1:
CaTh-MRI protocols. SP includes RT-fs-PDw and RT-DWI (axial view covering the entire chest) for the detection of lung alterations, MRA double contrast-enhanced acquisition(coronal view on pulmonary arterial and venous phases) for pulmonary embolism, and a comprehensive cardiac evaluation with nT1, T2m and ECV(three slices on SA + HLA), STIR, cineMR and LGE (8–10 SA slices stack + VLA + HLA). For FP, a combined assessment of lung parenchyma and heart is respectively obtained with BH-Trufi in axial and coronal views, and nT1, T2m and cineMR, acquired in the aforementioned cardiac axes. ECV, extracellular volume fraction mapping; Gd, gadolinium; HLA and VLA, horizontal and vertical long axis; MRA, pulmonary magnetic resonance angiography; LGE, late gadolinium-enhanced imaging; BH-Trufi, breath-hold bidimensional true fast imaging with steady-state free-precession; Myo, myocardial; nT1, native T1-mapping; PE, pulmonary embolism; RT-DWI, respiratory-triggered diffusion-weighted (b values 0–500–1000); T2m, T2 mapping; RT-fs-PDw, fast respiratory-triggered fat-saturated proton-density-weighted turbo-spin-echo; SA, short axis; Scout, standard localizer for thorax and cardiac planes; STIR, short-tau inversion-recovery.
For patients in haemodynamically stable conditions and not severely dyspnoic, the standard protocol (SP) included following sequences for a comprehensive cardiothoracic evaluation:
-
Lung MR imaging
Fast respiratory-triggered proton-density weighted fat-saturated turbo spin echo (PD-TSE) sequence acquired on the axial view to detect pulmonary consolidations and ground-glass opacities;
Diffusion weighted imaging (DWI) axial sequence with b values of 0–500–1000 acquired on the axial plane to assess pulmonary inflammation activity;
-
CMR
Black blood Short Tau Inversion-recovery (STIR) T2 weighted sequence: a stack of short-axis images encompassing both entire ventricles to detect areas of myocardial oedema;
Modified Look-Locker inversion-recovery (MOLLI) and T2-prepared True-FISP sequences: acquired on three matched short-axis slices at basal, mid and apical planes to obtain T1 and T2 maps, respectively to identify and characterize diffuse myocardial injury (oedema and fibrosis) which could be missed by conventional sequences; extracellular volume fraction (ECV) maps have been generated by combining MOLLI images acquired before and 15 min after contrast agent injection;
Balanced steady-state free precession cine-MR (SSFP cineMR) images acquired during breath-hold in the standard fashion on multiple-planes oriented on short-axis and long-axis views to evaluate ventricular function;
Contrast-enhanced inversion recovery T1-weighted (IR-CE T1w) sequence acquired from 18 to 20 min after contrast injection to detect late gadolinium-enhanced (LGE) areas.
-
Pulmonary MRA
Fast spoiled Gradient Echo FLASH-3D-sequence acquired in the coronal plane, during first-pass of contrast administration, to identify PE and lung perfusion defects.
For unstable or uncooperative patients, an optimized 25-min fast protocol (FP) was conceived by restricting the number of sequences to those necessary to rule out myocardial and to assess pulmonary involvement.
FP protocol included:
Lung MRI imaging
True Fast Imaging with Steady-State Free Precession acquired during breath-hold on axial and coronal views
CMR
T1 and T2 mapping and SSFP cineMR images acquired during breath-hold in the standard fashion on the aforementioned planes.
As shown in Figure 1, FP scanning protocol was prolonged to the contrast-enhanced branch of the SP, in case of T1/T2 values abnormality or worsening dyspnoea with low- to intermediate pre-test probability of PE.
Preliminary results
During the pandemic first wave in Italy between March and May 2020, 19 patients have been recruited and performed CaTh-MRI exams.
Seven patients (37%), have been addressed to SP whereas twelve patients (63%), intolerant to repeated breath-holding and/or poorly cooperative, were referred to FP. In the FP group, six patients showed signs of active myocardial injury (increased myocardial T2 value) or clinical suspicion of PE and their MRI protocol proceeded with pulmonary MRA, IR-CE T1w and contrast-enhanced MOLLI sequences.
Myocardial oedema was detected in 5/19 patients on T2w images, whereas LGE areas were present in 7/13 patients (six inflammatory vs. one ischemic pattern).
The global myocardial native T1 and T2 values were abnormal respectively in 8/19 and 10/19 patients; 5/13 patients presented increased global ECV.
The final diagnosis of myocarditis was reached in 6/19 patients, pericarditis in 1/19, and myocardial infarction in 1/19.
Pulmonary parenchyma consolidation was detected in 8/19, ground-glass opacity in 16/19, interlobular septal thickening in 6/19 and pleural effusion in 3/19 patients. DWI revealed active lung inflammation in 12/19 patients. No PE was identified at MRA sequence, thus avoiding the CT angiography investigation.
Conclusion
In conclusion, we demonstrated the feasibility of a comprehensive CaTh-MRI protocol as a safe approach for a combined evaluation of the myocardial injury, lung alterations, and pulmonary embolism in COVID-19 patients within a single examination. In patients requiring CMR characterization of myocardial damage, an optimized protocol with the addition of lung and thoracic vessel evaluation is of clinical benefit at a minimal time expense. In our restricted patient’s cohort with low to intermediate pre-test probability of PE, no further investigations were required, exploiting the high negative predictive value of the test.
Conflict of interest: none declared.
References
- 1. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. 2020;141:1648–55. [DOI] [PubMed] [Google Scholar]
- 3. Agricola E, Beneduce A, Esposito A, Ingallina G, Palumbo D, Palmisano A et al. Heart and lung multimodality imaging in COVID-19. JACC: Cardiovasc Imaging 2020;141:1648–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stein PD, Chenevert TL, Fowler SE, Goodman LR, Gottschalk A, Hales CA et al. Gadolinium-enhanced magnetic resonance angiography for pulmonary embolism: a multicenter prospective study (PIOPED III). Ann Intern Med 2010;152:434–W143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ates OF, Taydas O, Dheir H. Thorax magnetic resonance imaging findings in patients with coronavirus disease (COVID-19). Acad Radiol 2020;27:1373–8. [DOI] [PMC free article] [PubMed] [Google Scholar]