Abstract
Background
Investigating antecedents of behaviors, such as wearing face coverings, is critical for developing strategies to prevent SARS-CoV-2 transmission.
Purpose
The purpose of this study was to determine associations between theory-based behavioral predictors of intention to wear a face covering and actual wearing of a face covering in public.
Methods
Data from a cross-sectional panel survey of U.S. adults conducted in May and June 2020 (N = 1,004) were used to test a theory-based behavioral path model. We (a) examined predictors of intention to wear a face covering, (b) reported use of cloth face coverings, and (c) reported use of other face masks (e.g., a surgical mask or N95 respirator) in public.
Results
We found that being female, perceived importance of others wanting the respondent to wear a face covering, confidence to wear a face covering, and perceived importance of personal face covering use was positively associated with intention to wear a face covering in public. Intention to wear a face covering was positively associated with self-reported wearing of a cloth face covering if other people were observed wearing cloth face coverings in public at least “rarely” (aOR = 1.43), with stronger associations if they reported “sometimes” (aOR = 1.83), “often” (aOR = 2.32), or “always” (aOR = 2.96). For other types of face masks, a positive association between intention and behavior was only present when observing others wearing face masks “often” (aOR = 1.25) or “always” (aOR = 1.48).
Conclusions
Intention to wear face coverings and observing other people wearing them are important behavioral predictors of adherence to the CDC recommendation to wear face coverings in public.
Keywords: Face covering, Face mask, Planned behavior, Social norms, Prevention, COVID-19
Introduction
SARS-CoV-2, the virus that causes COVID-19, spreads easily through person-to-person contact [1] by symptomatic and asymptomatic individuals [2, 3]. In the absence of specific therapeutics or vaccines to treat or prevent COVID-19, behavioral mitigation strategies have been implemented [4]. CDC recommendations issued April 2020 promoted the use of cloth face coverings, not including surgical masks or N95 respirators, in public, especially when social distancing is difficult to maintain (since updated to refer more generally to “mask use” in public) [5, 6]. Two recent U.S. national surveys indicate high prevalence estimates (74.1% and 76.4%) of cloth face covering use in public during the COVID-19 pandemic [7, 8], but little is known about predictors of this behavior. Behavioral theories, used extensively in public health [9–12], can help investigate these issues.
This study integrated the Health Belief Model (HBM) and the Theory of Planned Behavior (TPB), two of the most widely used health behavior theories/models in the social and behavioral sciences. As Glanz and Bishop [12] suggest, the strongest interventions may be built from multiple theories and models. By using both HBM (an explanatory model) and the TPB (a change theory) in this research, we were able to explore both the barriers and facilitators to the public’s use of face coverings as well as to identify possible pathways through which the desired behavior (use of face coverings) could be increased among a national sample of the U.S. population.
The HBM includes six key constructs that have been shown to be correlates of health behaviors and predictive of health behavior change [13]. These are perceived susceptibility; perceived severity; perceived threat (the construct formed by combining susceptibility and severity), perceived benefits of taking action; perceived barriers to taking action; cues to action; and self-efficacy [13]. The TPB traditionally includes three primary predictors of behavioral intention, these include attitude toward a behavior, subjective norm, and perceived behavioral control [9]. Behavioral intention serves as a mediator between the predictors (attitude, subject norm, and perceived behavioral control) and engagement in the behavior. Due to the novel nature of wearing face coverings in the United States, people may look to others to determine whether it would be socially appropriate to wear a face covering in public, even if they planned to engage in the behavior [14]. Additionally, due to the potential negative outcomes associated with not wearing a face covering (i.e., contracting COVID-19), the role that explanatory predictors (e.g., perceived susceptibility and severity) were examined in predicting behavioral intention and the behavior (wearing a face covering in public).
The consideration of descriptive norms, or seeing other people engaging in a behavior, has been previously considered as a moderator of the association between intentions and behavior [14] but little is known regarding its role in the public health intervention of face covering use. We were specifically interested in examining the role that descriptive norms played in determining actual face covering use. We hypothesized that the frequency of seeing people wearing face coverings would be an important determinate in one’s decision to wear a face covering.
Consistent with theory, we hypothesized the following associations (a) positive attitudes, positive self-efficacy, higher subjective norms, higher perceived susceptibility, and higher perceived severity would be associated with stronger intentions to wear a cloth face covering; (b) there would be no direct associations between these same behavioral predictors and face covering use after accounting for intention to wear a cloth face covering; and (c) the association between intention to wear a cloth face covering and wearing a face covering would be dependent on the frequency they saw other people wearing face coverings. We explored these associations for both cloth face coverings and other mask use (N95, dust mask, and so on). The latter represented analyses aimed at determining whether there were any differences in associations between intention and behavior for each type of face covering.
Method
To assess cloth face covering use and factors that may influence uptake, in May and June 2020, Porter Novelli Public Services (PN) and ENGINE Insights conducted an opt-in, internet-based survey of 1,004 U.S. adults aged >18 years. PN employs quota sampling and statistical weighting to make the panel representative of the U.S. population by gender, age, region, race/ethnicity, and education. Respondents were asked to take a survey and reminded that they could refuse to answer any question or terminate the survey at any time. No personally identifying information was provided to the CDC.
Survey questions reflected theoretical constructs based on the theory of planned behavior [9] and health belief model [10, 11], which are widely used in public health research and practice [12]. The primary mediator was measured by responses to: I intend to wear a cloth face covering when I go to public spaces, on a 5-point Likert scale from strongly disagree to strongly agree. The outcomes corresponded to items asking: in the past week, when you have gone outside of your home for work, grocery shopping or other activities that involved interacting with other people, how often did you…wear a cloth face covering that covered your nose and mouth? and wear a paper disposable mask, surgical mask, dust mask or other respirator, such as an N95?, with possible responses of never, rarely, sometimes, often, or always. Similar questions were asked to measure descriptive norms, whether they saw other people wearing these same face coverings. The survey items can be found in Supplementary Material File 1.
Respondents who reported not leaving their house in the seven days prior to the survey (n = 119, 12%) were not asked questions regarding wearing face coverings in public. These respondents were more likely than those who left their houses (n = 885) to be aged ≥70 years (27% vs. 8%); live in the Northeast (22% vs. 17%); be retired (36% vs. 20%); and have strong beliefs (“strongly agree”) that: they would become seriously ill with COVID-19 (43% vs. 31%), that wearing a cloth face covering is important (59% vs. 45%), that people important to them want them to wear a cloth face covering (53% vs. 42%), and that they would be able to wear a cloth face covering in public (50% vs. 40%). A richer description of this subsample (n = 119) is found in Supplementary Material File 1.
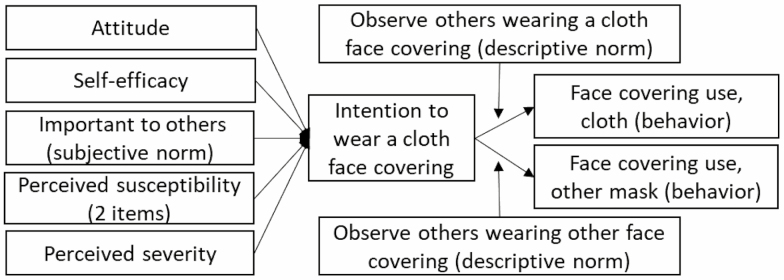
Among those leaving their house in the seven days prior to survey administration (n = 885), a ordinal regression path model was tested utilizing sample weights based on U.S. census characteristics (by gender, age, region, race/ethnicity, and education) and adjusted for clustering by state of residence. The model assessed respondents’ perceptions of theory-based predictors: (a) importance of wearing a cloth face covering in public (attitude); (b) confidence in one’s ability to wear a cloth face covering (self-efficacy); (c) having people important to them wanting them to wear cloth face coverings in public (subjective norm); (d) their likelihood to become ill with COVID-19 and knowing someone hospitalized with COVID-19 (perceived susceptibility, two items); and (e) whether they would become seriously ill if they contracted COVID-19 (perceived severity); (f) if the above were associated with intention to use a cloth face covering (behavioral intention; mediator), (g) if intention to wear a cloth face covering was associated with self-reported cloth face covering use and other face covering use in public (behavior, two items; outcomes), and (h) whether wearing a face covering was dependent on the frequency of seeing other people wearing face coverings (descriptive norms, two items; moderators). The theoretical model is presented in Fig. 1. We tested a path model examining predictors of intention to wear a cloth face covering (hypothesis 1), direct associations of these predictors with face covering use (hypothesis 2), and whether the association between intention and use was dependent upon observing other people wearing cloth face coverings or other face coverings (hypothesis 3).
Fig. 1.
Theoretical model of assessed paths for face covering use in public. Direct paths from all exogenous variables to behavior were estimated but not included for graphical simplicity. The statistical model also included the covariates of age, gender, and urbanicity as predictors of face cover intentions and use.
The covariates of age, gender, and urbanicity were included as predictors of face cover intentions and use. These covariates were included in the model because global perceptions of risk unrelated to face covering use are frequently confounded with gender [15] and age [16], and local health authorities’ recommendations regarding face covering use have often differed based on the population density of the area (urbanicity) [17]. Based on recommendations for correlational research, we only included theoretically driven covariates [18].
Results
Our model included one mediator (intention to use a cloth face covering) and two outcomes (cloth face covering use and other face covering use). When asked how strongly they agreed with the statement “intend to wear a cloth face covering when I go to public spaces,” 47% strongly agreed, 24% somewhat agreed, 15% neither agreed nor disagreed, 7% somewhat disagreed, and 8% strongly disagreed. For actual use of a cloth face covering when entering public spaces, 36% reported “always,” 23% “often,” 21% “sometimes,” 8% “rarely,” and 13% reported “never.” For use of other types of face coverings (e.g., surgical or dust masks or N95s), 27% reported “always,” 24% “often,” 21% “sometimes,” 8% “rarely,” and 21% “never” wearing these types of face coverings in public. Respondents could indicate the use of both cloth and other types of face coverings. Bivariate correlations suggest strong associations between intention to use a face covering and engagement in the behavior (Spearman’s ρ: intention and cloth face covering use = 0.58, p < .001; intention and other face covering use = 0.27, p < .001).
Being female (adjusted OR [aOR] = 1.56; 95% CI, 1.16–2.21), perceived importance of having people important to them wanting them to wear a cloth face covering (aOR = 1.77; 95% CI, 1.46–2.25), confidence to wear a cloth face covering (aOR = 1.90; 95% CI, 1.47–2.58) and perceived importance of personal cloth face covering use (aOR = 4.65; 95% CI, 3.48–6.69) were significantly associated with intention to wear a cloth face covering in public (hypothesis 1). We found no evidence that perceived susceptibility to becoming ill and perceived severity of COVID-19 were associated with intention to use or self-reported use of a face covering, with the exception of a direct association between severity and other face covering use (aOR = 1.13; 95% CI, 1.01–1.29). There was no other evidence of direct associations between the behavioral predictors and face covering use after accounting for intentions (hypothesis 2) despite all bivariate correlations, with the exception of knowing someone who had been hospitalized, between behavioral predictors and face covering use being positive, and statistically significant for both cloth face coverings and other masks use: Spearman’s ρ ranged from 0.54 (subjective norm) to 0.10 (likelihood of infection). Knowing someone who was hospitalized was not correlated with for either cloth face covering (p = .588) or other mask use (p = .644).
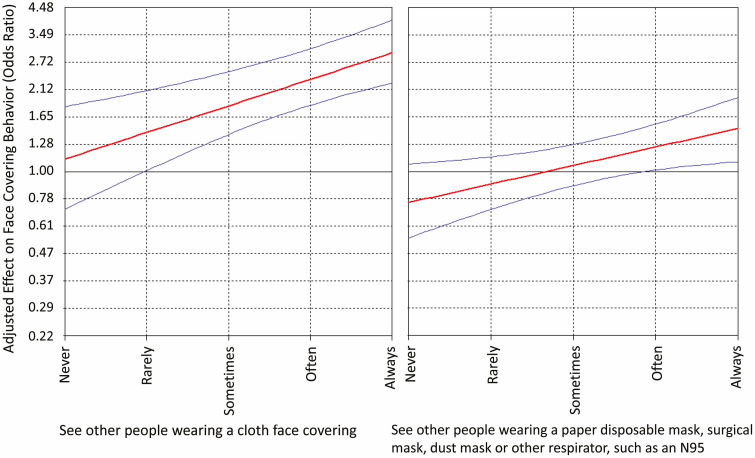
The interaction between face covering use intention and observing others wearing face coverings (descriptive norms) predicted behavior for both cloth face coverings and other types of face coverings (Table 1) (hypothesis 3). The interactions between intention to wear a cloth face covering and observing other people wearing a face covering are shown in Fig. 2. Specifically, the association between intention and behavior was significant when participants reported seeing other people wearing cloth face coverings at least “rarely” (aOR = 1.43; 95% CI, 1.01–2.09), with stronger associations if they reported “sometimes” (aOR = 1.83; 95% CI, 1.40–2.49), “often” (aOR = 2.32; 95% CI, 1.83–3.08) or “always” (aOR = 2.96; 95% CI, 2.24–3.99). For other types of face coverings, a positive and significant association between intention and behavior was only present when participants reported seeing people wearing other face coverings “often” (aOR = 1.25; 95% CI, 1.01–1.54) or “always” (aOR = 1.48; 95% CI, 1.09–1.97). The findings suggest that attitude, self-efficacy and subjective norm are indirectly associated with wearing a face covering via behavioral intention, with the association between behavioral intention and actual face covering use behavior dependent upon the descriptive norm of observing other people wearing a face covering. We found no evidence to support (or not) that any of our hypotheses were dependent upon the covariates included in the model.
Table 1.
Associations among predictors of intention to wear a cloth face covering and reporting wearing a face covering
| Behavioral intention to wear a cloth face covering | Behavior—cloth face covering | Behavior—other face coveringa | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | ORc | b | SE | p | ORc | b | SE | p | ORc | |
| Age in years | 0.00 | 0.00 | 0.979 | 1.00 | 0.00 | 0.00 | 0.449 | 1.00 | 0.00 | 0.01 | 0.520 | 1.00 |
| Female | 0.44 | 0.16 | 0.006 | 1.56 | –0.02 | 0.16 | 0.884 | 0.98 | –0.14 | 0.15 | 0.366 | 0.87 |
| Urban | 0.24 | 0.16 | 0.133 | 1.27 | 0.14 | 0.24 | 0.556 | 1.15 | –0.19 | 0.18 | 0.304 | 0.83 |
| Suburban | Ref. | – | – | – | – | – | – | – | – | – | – | -- |
| Rural | –0.20 | 0.19 | 0.307 | 0.82 | –0.10 | 0.20 | 0.625 | 0.91 | –0.56 | 0.19 | 0.003 | 0.57 |
| Perceived importance (for me) of wearing (Attitude) | 1.54 | 0.17 | <.001 | 4.65 | 0.19 | 0.11 | 0.096 | 1.21 | 0.10 | 0.09 | 0.238 | 1.11 |
| I am confident I can wear (self-efficacy) | 0.64 | 0.14 | <.001 | 1.90 | 0.02 | 0.09 | 0.842 | 1.02 | 0.09 | 0.08 | 0.251 | 1.09 |
| Others feel important I wear (subjective norm) | 0.57 | 0.11 | <.001 | 1.77 | 0.13 | 0.09 | 0.135 | 1.14 | 0.10 | 0.11 | 0.364 | 1.10 |
| Perceived susceptibility (to COVID-19) | –0.01 | 0.09 | 0.933 | 0.99 | 0.05 | 0.05 | 0.337 | 1.05 | 0.03 | 0.05 | 0.550 | 1.03 |
| Perceived susceptibility (know someone hospitalized with COVID-19) | –0.14 | 0.19 | 0.465 | 0.87 | –0.17 | 0.20 | 0.394 | 0.84 | 0.09 | 0.16 | 0.595 | 1.09 |
| Perceived severity (would become seriously ill) | 0.14 | 0.08 | 0.075 | 1.15 | –0.03 | 0.07 | 0.682 | 0.97 | 0.13 | 0.06 | 0.045 | 1.13 |
| Behavioral intention (to wear) | – | – | – | – | 0.11 | 0.24 | 0.637 | 1.12 | –0.29 | 0.17 | 0.098 | 0.75 |
| Observing other people wear (descriptive norms)b | – | – | – | – | –0.19 | 0.17 | 0.246 | 0.83 | 0.32 | 0.21 | 0.129 | 1.38 |
| Behavioral intention X observingb | – | – | – | – | 0.24 | 0.07 | <.001 | 1.28 | 0.17 | 0.07 | 0.009 | 1.19 |
aQuestion referred to other face coverings, include paper disposable mask, surgical mask, dust mask, or other respirator, such as an N95.
bThese constructs are specific and unique for each type of face covering (cloth face covering and other face covering).
cAdusted for all predictors of each outcome.
Fig. 2.
Johnson–Neyman plot. The center lines (red) represent the strength of the association between intention to wear a face covering and face covering use at each value of seeing other people wearing a face covering (cloth face coverings, left; other types of face coverings, right). The outer lines (blue) represent the 95% confidence intervals around these associations. 95% confidence intervals that do not include an odds ratio of one are considered statistically significant.
Discussion
This analysis demonstrates significant associations between theory-based predictors for face covering use with people’s intention to wear cloth face coverings in public. The analysis also revealed that people with intentions of wearing cloth face coverings in public were more likely to report face covering use if they observed other people wearing them. A meta-analysis by Reevis and Sheeran [13] suggests that descriptive norms significantly contribute to the prediction of behavioral intention even after attitude, subjective norm, and perceived behavioral control are taken into account. It is likely that seeing other people wearing a face covering may increase people’s intention to wear a face covering and our findings suggest that intentions are more likely to translate to behaviors when people observe others engaging in the behavior. This phenomenon may be particularly salient for relatively novel behaviors, such as wearing a face covering in the United States during the COVID-19 pandemic. Furthermore, descriptive norms research suggests that observed behaviors in common settings can motivate others by offering cues to action for a particular behavior [14, 19]. While the utility of programs aimed at impacting descriptive norms in the context of face coverings have not been rigorously evaluated, ad campaigns, such as the You Will See Me Campaign, may help normalize the wearing of face coverings to prevent the spread of COVID-19 [20]. We did not find evidence that perceived susceptibility to becoming ill from COVID-19 or perceived severity associated with COVID-19 were associated with intention to use a cloth face covering or self-reported use a face covering (with the exception of a direct association between severity and use of another type of face covering such as a surgical and dust mask or N95). It is possible that messaging strategies that focus susceptibility to and severity of COVID-19 may not be as effective as targeting actions that influence individual intentions and social norms in promoting the use of face coverings while in public. Finally, it is well-documented that theory-based public health interventions are more successful and use of theoretical models improves the ability to identify, define, and influence target outcome variable(s) [12]. Public health campaigns should consider using behavioral models and theories for gaining an understanding of the antecedents of new, mitigation behaviors in the current pandemic, and for designing interventions to enhance positive attitudes and norms around the public’s use of face coverings to prevent the transmission of SARS-CoV-2.
Research limitations include the cross-sectional design, which precludes making causal inferences. Additionally, internet surveys vary in methodology and quality [21], and lower response rates from different socioeconomic and racial/ethnic minority groups are common. Nonetheless, our results are consistent with recent research on cloth face covering use [8]. Finally, our study included a limited set of items that might not fully explain the theoretical constructs and that primarily focus on cloth face coverings. Future research would benefit from larger sample sizes and a longitudinal design that measures outcomes (behavioral intention and actual behavior) at different time points, and a closer examination of sociodemographic and regional differences. A longitudinal design would also enable researchers to best assess and interpret conditional indirect effects of behavioral predictors on engaging in face covering behavior. Additionally, future research on why people use different types of face coverings in different settings would be useful, particularly in light of the association between people who perceived COVID-19 as more severe and wearing a paper disposable/surgical/dust/N95 mask in our study.
Adherence to the CDC recommendation to wear a cloth face covering in public, especially when social distancing is difficult to maintain, is essential to reducing SARS-CoV-2 transmission [5, 22]. Findings from this study demonstrate that intention to wear a face covering, combined with observing other people wearing them, are important behavioral predictors of uptake of the CDC recommendation [5, 6]. Moreover, seeing more people wearing face coverings in public may be a tipping point that translates an individual’s intentions into a behavior. The research highlights the importance of descriptive norms as a key element in proposed behavior change interventions, especially when large scale, sustained behavior change is desired [23]. Public health professionals and clinicians can play a vital role in promoting the importance of wearing face coverings, building people’s confidence in doing so, while conveying social support for this behavior. While state and local requirements for wearing face coverings are important, public health initiatives are also critical to enhancing positive norms around widespread adoption of face covering use during the COVID-19 pandemic.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflict of interest.
Authors’ Contributions Barile was the primary data analyst and drafted the methods, results, and discussion sections. Guerin drafted the introduction and revised all other sections. Fisher, Tian, Okun, Vanden Esschert, and Jeffers provided revisions to initial drafts. Gurbaxani provided statistical expertise and section revisions. Thompson and Prue provided senior leadership and direction for the study.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all individual participants included in the study.
References
- 1. CDC. How COVID-19 Spreads Atlanta, GA: US Department of Health and Human Services, CDC; 2020. Available at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html. Accessed July 11, 2020. [Google Scholar]
- 2. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:411–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. CDC. Coronavirus Disease 2019 (COVID-19): Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community–Based Transmission Atlanta, GA: US Department of Health and Human Services, CDC; 2020. Available at https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html. [Google Scholar]
- 6. CDC. Coronavirus Disease 2019 (COVID-19): Considerations for Events and Gatherings Atlanta, GA: US Department of Health and Human Services, CDC; 2020. Available at https://www.cdc.gov/coronavirus/2019-ncov/community/large-events/considerations-for-events-gatherings.html. Accessed July 11, 2020. [Google Scholar]
- 7. Czeisler MÉ, Tynan MA, Howard ME, et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5–12, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fisher KA, Barile JP, Guerin RJ, et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic—United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:933–937. [DOI] [PubMed] [Google Scholar]
- 9. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 10. Hochbaum GM. Public Participation in Medical Screening Programs: A Sociopsychological Study. Washington, DC: Department of Health, Education, and Welfare; 1958. [Google Scholar]
- 11. Rosenstock IM. The health belief model and preventive health behavior. Health Ed Monograph. 1974;2:354–386. [Google Scholar]
- 12. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399–418. [DOI] [PubMed] [Google Scholar]
- 13. Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education: Theory, Research, and Practice. Philadelphia, PA: John Wiley & Sons; 2008:45–65. [Google Scholar]
- 14. Rivis A, Sheeran P. Descriptive norms as an additional predictor in the theory of planned behaviour: a meta-analysis. Curr Psychol. 2003;22:218–233. [Google Scholar]
- 15. Gustafsod PE. Gender differences in risk perception: theoretical and methodological perspectives. Risk Analysis. 1998;18:805–811. [DOI] [PubMed] [Google Scholar]
- 16. Bonem EM, Ellsworth PC, Gonzalez R. Age differences in risk: perceptions, intentions and domains. J Behav Decis Making. 2015;28:317–330. [Google Scholar]
- 17. Brandtner C, Bettencourt L, Stier A, Berman MG. Creatures of the state? Metropolitan counties compensated for state inaction in initial US response to COVID-19 pandemic. Mansueto Institute for Urban Innovation Research Paper; August 10, 2020. [Google Scholar]
- 18. Becker TE, Atinc G, Breaugh JA, Carlson KD, Edwards JR, Spector PE. Statistical control in correlational studies: 10 essential recommendations for organizational researchers. J Organ Behav. 2016;37:157–167. [Google Scholar]
- 19. Cialdini RB, Demaine LJ, Sagarin BJ, Barrett DW, Rhoads K, Winter PL. Managing social norms for persuasive impact. Soc Influ. 2006;1:3–15. [Google Scholar]
- 20. Sidibe T. You Will See Me Campaign Emphasizes Mask Wearing To Help Black Americans Prevent COVID-19 Spread. CDC Foundation Website August 19, 2020. Accessibility verified August 25, 2020 https://www.cdcfoundation.org/blog/you-will-see-me-campaign-emphasizes-mask-wearing-help-black-americans-prevent-covid-19-spread
- 21. Craig BM, Hays RD, Pickard AS, Cella D, Revicki DA, Reeve BB. Comparison of US panel vendors for online surveys. J Med Internet Res. 2013;15:e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brooks JT, Butler JC, Redfield RR. Universal masking to prevent SARS-CoV-2 transmission—the time is now. JAMA. 2020;324:635–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reynolds KJ, Subašić E, Tindall K. The problem of behaviour change: from social norms to an ingroup focus. Soc Personal Psychol Compass. 2015;9:45–56. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.