Editor
Uncontrolled ‘cytokine storms’ and multiple organ dysfunction syndrome (MODS) are important causes that leading to progression of illness and death in patients with COVID-191,2. The gut is a major organ invaded and damaged by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and plays a vital role in controlling the systemic inflammatory response and preventing MODS. Berberine has a long history in traditional Chinese medicine for the treatment of diarrhoea and gastroenteritis owing to its antimicrobial, antimotility and antisecretory properties. Moreover, a study3 has shown that berberine can protect the intestinal mucosal barrier and suppress the inflammatory response in intestinal epithelium and serum.
We enrolled prospectively 39 patients with severe COVID-19 hospitalized at Wuhan Hospital of Traditional Chinese and Western Medicine, Tongji Hospital and the Second Hospital of Nanjing between January and April 2020. The diagnostic criteria for severe cases were in accordance with the Diagnosis and Treatment Guideline of patients with COVID-19 issued by the National Health Commission of the People’s Republic of China (edition 7)4. Patients were excluded if they were aged below 18 or above 80 years, had inflammatory bowel disease, were unable to take oral or tube feeding, had drug-related contraindications, were considered likely to die within 72 h, were participating in other clinical trials, had other sites of infection at the same time, or were pregnant or lactating women. Eventually, 18 patients were allocated to the berberine group and 17 to the control group. Patients in the berberine group were given berberine plus routine therapy within 14 days of admission, and those in the control group received only routine therapy. Laboratory parameters, including serum interleukin (IL) 6, serum tumour necrosis factor (TNF) α, C-reactive protein (CRP), procalcitonin and white blood cell (WBC) count, were measured on days 1, 3, 7 and 14 after admission. Statistical significance, determined by generalized linear mixed models in GraphPad® Prism 5.0 (GraphPad, La Jolla, CA, USA) was assumed at P < 0.050.
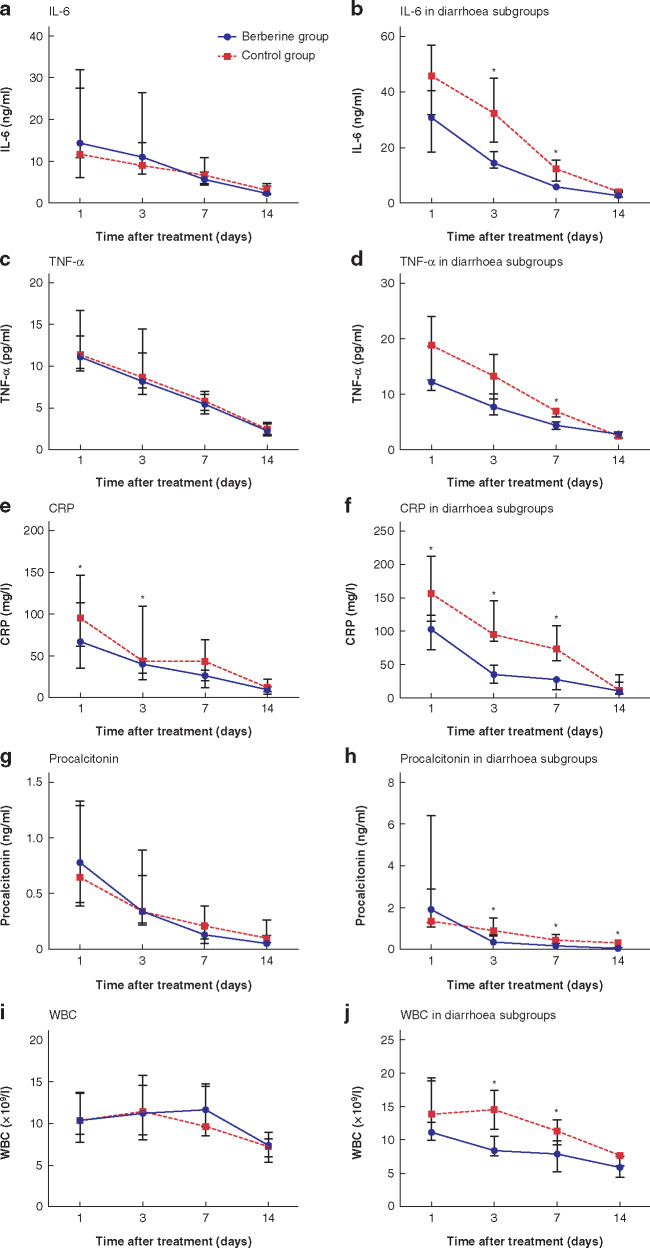
Except for the Acute Physiology and Chronic Health Evaluation (APACHE) II score, other basic clinical characteristics of age, sex, exposure history, co-morbidity, symptoms and the Sequential Organ Failure Assessment (SOFA) score were similar in the two groups. No significant difference was observed between the two groups in the trend of IL-6, TNF-α, CRP, procalcitonin and WBC levels within 14 days (Fig. 1). In subgroup analyses of patients with diarrhoea, berberine significantly improved the changes in IL-6, TNF-α and CRP levels (P < 0.050). Diarrhoea was defined as the passage of loose stools more than three times daily. Only one patient developed a mild rash, which disappeared shortly after the withdrawal of berberine.
Fig. 1.
Blood concentrations of inflammatory mediators in patients with severe COVID-19 in the two treatment groups and the subgroups with diarrhoea
a Interleukin (IL) 6; b IL-6 in subgroups with diarrhoea; c tumour necrosis factor (TNF) α; d TNF-α in subgroups with diarrhoea; e C-reactive protein (CRP); f CRP in subgroups with diarrhoea; g procalcitonin; h procalcitonin in subgroups with diarrhoea; i white blood cell count (WBC); j WBC in subgroups with diarrhoea. Values are median (i.q.r.). There were 18 patients in the berberine group and 17 in the control group, with six and five patients in the respective subgroups with diarrhoea. *P < 0.050, berberine versus control group (generalized linear mixed model).
The maintenance and protection of gastrointestinal function is an important aspect in the treatment of patients with severe COVID-19. Carnevale and colleagues5 reported on a patient with COVID-19 who had diarrhoea and abdominal pain, and underwent endoscopic biopsy sampling of the small bowel. Histopathological findings revealed that mucosal and submucosal tissues had inflammatory infiltrates, prominent multifocal vasculitis, and ischaemic damage. Raised levels of faecal calprotectin, a biomarker of intestinal inflammation, have been observed, and correlated significantly with plasma IL-6 levels in patients with COVID-19 and diarrhoea6. These findings suggest that the gastrointestinal tract is not only the target, but also the source, of inflammatory mediators under SARS-CoV-2 infection. We speculated that berberine may reduce the serum levels of inflammatory mediators through the protection and maintenance of gastrointestinal function, although relevant data were inadequate for evaluating the intestinal mucosal barrier and intestinal microenvironment in our study. In addition, the optimal berberine dose for anti-inflammation related to SARS-CoV-2 remains unclear, although we based our dose of berberine (900 mg daily) on the effective anti-inflammation dose according to other literature. Furthermore, studies7,8 have shown that berberine exhibits direct anti-influenza virus effects in vitro, inhibits lung inflammatory injury, and reduces the release of oxygen radicals in mice suffering from pneumonia associated with influenza virus. As COVID-19 is an emergency global epidemic, it is unclear whether berberine has any antiviral effect on SARS-CoV-2, and further experiments are needed to clarify this.
Disclosure. The authors declare no conflict of interest.
References
- 1. Li X Wang L Yan S, Yang F, Xiang L, Zhu J et al. Clinical characteristics of 25 death cases with COVID-19: a retrospective review of medical records in a single medical center, Wuhan, China. Int J Infect Dis 2020;94:128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhou F Yu T Du R, Fan G, Liu Y, Liu Z et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hou Q Zhu S Zhang C, Huang Y, Guo Y, Li P et al. Berberine improves intestinal epithelial tight junctions by upregulating A20 expression in IBS-D mice. Biomed Pharmacother 2019;118:109206. [DOI] [PubMed] [Google Scholar]
- 4. National Health Commission. Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (Trial Version 7) China, 2020. http://www.nhc.gov.cn/wjw/zcjd/list_6.shtml (accessed 24 July 2020)
- 5. Carnevale S, Beretta P, Morbini P. Direct endothelial damage and vasculitis due to SARS-CoV-2 in small bowel submucosa of COVID-19 patient with diarrhea. J Med Virol 2020; DOI:10.1002/jmv.26119 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Effenberger M Grabherr F Mayr L, Schwaerzler J, Nairz M, Seifert M et al. Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut 2020; 69:1543–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu H You L Wu J, Zhao M, Guo R, Zhang H et al. Berberine suppresses influenza virus-triggered NLRP3 inflammasome activation in macrophages by inducing mitophagy and decreasing mitochondrial ROS. J Leukoc Biol 2020;108:253–266. [DOI] [PubMed] [Google Scholar]
- 8. Wu Y Li JQ Kim YJ, Wu J, Wang Q, Hao Y. In vivo and in vitro antiviral effects of berberine on influenza virus. Chin J Integr Med 2011;17:444–452. [DOI] [PubMed] [Google Scholar]