Since the passage of the Immigration and Nationality Act of 1965, significant growth of the foreign-born population has reshaped the ethnic and racial landscape of the United States (Hamilton, 2019; Portes & Rumbaut, 2014). As of 2018, the 44.8 million immigrants residing in the United States represented ~13.7% of the total population (Krogstad & Gonzalez-Barrera, 2018). As immigrants age, they will account for a greater share of the country’s population in midlife and older ages (Treas & Batalova, 2009). Therefore, understanding the health trajectories of immigrants provides valuable insights into the future health of the entire U.S. population (Treas & Batalova, 2009).
This article examines how aging in the U.S. context differentially impacts the health of U.S. immigrants. We first describe nativity and racial disparities in three chronic conditions—hypertension, diabetes, and obesity—that are life-threatening and prevalent among marginalized U.S.-born populations. We then highlight how immigrants’ health outcomes change as they age in the U.S. context and discuss possible mechanisms for the documented changes in immigrants’ health, including immigration policies that increase the degree of hostility faced by immigrant communities, and restrict access to social services.
Initial Health of Immigrants
Upon arrival in the United States, new immigrants tend to have better health profiles than their native-born counterparts (Antecol & Bedard, 2006). Using data from the 2000–2018 National Health Interview Survey (NHIS) (Blewett et al., 2019), Table 1 documents health disparities between recent immigrants and their native-born same-race/ethnicity counterparts ages 35–45 years, the age range in which most immigrants arrive in the United States. The data show that, regardless of race, new immigrants tend to have more favorable health outcomes than their native-born counterparts. Across all three health outcomes (i.e., hypertension, diabetes, and obesity), the nativity gap is larger among blacks, driven by the uniquely poor health outcomes of black Americans. While Asian immigrants have significantly lower obesity rates than white, black, and Hispanic immigrants, the prevalences of hypertension and diabetes are similar among all new immigrants ages 35–45 years.
Table 1.
Descriptive Statistics for U.S.-Born and Foreign-Born Adults with 0–4 Years of U.S. Residence, Ages 35–45
| All Origin | White | Black | Hispanic | Asian | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | |
| Native | Immigrant | Native | Immigrant | Native | Immigrant | Native | Immigrant | Native | Immigrant | |
| Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | |
| Health outcomes | ||||||||||
| Hypertension | 0.19 | 0.10 | 0.17 | 0.11 | 0.29 | 0.10 | 0.19 | 0.10 | 0.17 | 0.08 |
| Diabetes | 0.04 | 0.02 | 0.04 | 0.02 | 0.07 | 0.03 | 0.06 | 0.02 | 0.04 | 0.03 |
| Obese (BMI 30+) | 0.30 | 0.12 | 0.27 | 0.12 | 0.43 | 0.15 | 0.41 | 0.16 | 0.19 | 0.03 |
| Demographic characteristics | ||||||||||
| Age | 40.07 | 39.10 | 40.14 | 39.24 | 39.93 | 38.70 | 39.65 | 39.11 | 39.55 | 39.14 |
| Female | 0.53 | 0.47 | 0.52 | 0.49 | 0.59 | 0.42 | 0.54 | 0.45 | 0.50 | 0.52 |
| Observations | 84,634 | 2328 | 61,951 | 359 | 14,034 | 244 | 7742 | 1126 | 907 | 599 |
Note. BMI = body mass index; NHIS = National Health Interview Survey. Source: 2000–2018 NHIS. All statistics use NHIS annual weights. Sample sizes are based on hypertension reports because, hypertension has the highest reporting rate.
Selective migration is primarily responsible for immigrants’ initial health advantage (Hamilton, 2015). International immigration is not a random process. People with better health are more likely to emigrate, producing an initial health advantage among immigrants relative to both the native-born population and compatriots in immigrants’ birth places (Akresh & Frank, 2008; Feliciano, 2020). Although not the primary cause of the documented health advantage of immigrants (Hummer et al., 2007), selective return migration—in which sicker immigrants are more likely to return to their home countries—may also artificially improve the mean health profiles of immigrants (Palloni & Arias, 2004).
Health of Immigrants with Greater Tenure of U.S. Residence
Immigrants’ initial health advantage narrows or disappears entirely as immigrants age and spend more time in the United States (Antecol & Bedard, 2006). To illustrate this point, using data from the 2000–2018 waves of the NHIS, Table 2 shows health disparities between immigrants who have been in the United States ≥15 years and natives, both ages 50–60 years. Compared to the estimates in Table 1, those in Table 2 show that the change in the probability of reporting hypertension, diabetes, and obesity is greater for immigrants than natives. For example, U.S.-born blacks in the 50–60 age group are 1.97 times more likely to report hypertension than U.S.-born blacks in the 35–45 age group. By comparison, black immigrants in the 50–60 age group who have been in the United States for at least 15 years are 4.30 times more likely to report hypertension than black immigrants in the 35–45 age group who have been in the United States for five years or less. Similar changes occur for white, Hispanic, and Asian individuals, highlighting the unique effect of aging in the United States for immigrants.
Table 2.
Descriptive Statistics for U.S.-Born and Foreign-Born Adults with 15 or More Years of U.S. Residence, Ages 50–60
| All Origin | White | Black | Hispanic | Asian | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | |
| Native | Immigrant | Native | Immigrant | Native | Immigrant | Native | Immigrant | Native | Immigrant | |
| Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | |
| Health outcomes | ||||||||||
| Hypertension | 0.39 | 0.34 | 0.36 | 0.31 | 0.57 | 0.43 | 0.40 | 0.35 | 0.39 | 0.32 |
| Diabetes | 0.11 | 0.13 | 0.10 | 0.07 | 0.18 | 0.14 | 0.20 | 0.17 | 0.10 | 0.13 |
| Obese (BMI 30+) | 0.33 | 0.24 | 0.31 | 0.23 | 0.44 | 0.30 | 0.40 | 0.32 | 0.21 | 0.08 |
| Demographic characteristics | ||||||||||
| Age | 54.92 | 54.74 | 54.96 | 54.99 | 54.80 | 54.52 | 54.61 | 54.66 | 54.80 | 54.66 |
| Female | 0.54 | 0.52 | 0.53 | 0.52 | 0.58 | 0.52 | 0.55 | 0.52 | 0.49 | 0.53 |
| Observations | 86,413 | 12,062 | 67,118 | 2529 | 13,817 | 1076 | 4701 | 5984 | 777 | 2473 |
Note. BMI = body mass index; NHIS = National Health Interview Survey. Source: 2000–2018 NHIS. All statistics use NHIS annual weights. Sample sizes are based on hypertension reports because, hypertension has the highest reporting rate.
Prior studies highlight the role of structural factors, such as migration stress and poor working conditions (Finch et al., 2001; Gee et al., 2009), in producing the health declines of immigrants, but the dominant explanation for this temporal decline is changes in cultural practices, or acculturation, whereby immigrants adopt the dietary patterns and negative health behaviors (e.g., smoking and alcohol consumption) of the native population as they gain more U.S. experience (Abraido-Lanza et al., 2005; Scribner & Dwyer, 1989).
Few empirical studies, however, have examined whether acculturation is the primary or most important factor for immigrants’ declining health as they age and spend more time in the United States (Gee et al., 2009; Riosmena et al., 2014; Viruell-Fuentes, 2007). This gap in the literature results from the tendency of researchers to document nativity disparities in health among individuals of the same race, often ignoring the extent of racial disparities in initial health and health trajectories among immigrants. Because U.S. immigrants integrate into the same society, the dominant culture should exert a similar effect on all immigrants. Consequently, the relative tempo of health decline among immigrants provides insights into the role of structural factors in shaping the health trajectories of different immigrant populations.
Tables 1 and 2 also show the disparate association between U.S. tenure and aging among immigrants. Racial disparities in health are greater among immigrants who have been in the United States for ≥15 years than among new immigrants ages 35–45 years. For example, among new immigrants, the percentage of individuals reporting hypertension varies by 1 percentage point between white and black immigrants. In contrast, among older immigrants who have been in the United States for ≥15 years, the percentage of individuals reporting hypertension is 12 percentage points higher among blacks than among whites.
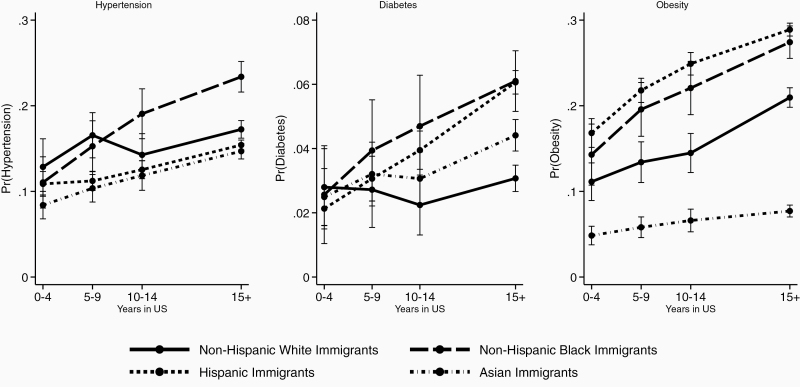
To provide a more refined picture of the disparate impact of U.S. tenure on the health of different immigrant populations, Figure 1 shows predicted probabilities from probit regression models of hypertension, diabetes, and obesity, adjusting for racial differences in demographic, social, and economic factors that are highly correlated with health, including age, sex, marital status, region of current residence, education, employment status, and poverty status.
Figure 1.
Predicted probabilities of health status. Source: 2000–2018 NHIS. All statistics use NHIS annual weights. Predicted probabilities of health status are based on probit regression models that control for age, sex, marital status, region of current residence, education, employment status, poverty status, and survey year. NHIS = National Health Interview Survey.
New immigrants, exhibit modest race-based variation in the predicted probabilities of reporting hypertension and diabetes, however, significant disparities emerge among immigrants as their tenure of U.S. residence increases. For diabetes, after residing in the United States for ≥15 years, a significant gap emerges, separating black and Hispanic immigrants (who have similar probabilities of diabetes) from white and Asian immigrants. Similarly, among immigrants who have been in the United States for ≥15 years, the predicted probability of hypertension is significantly greater for blacks than for whites, Asians, and Hispanics, despite the groups having similar predicted probabilities of hypertension upon arrival in the United States.
In contrast to the results for diabetes and hypertension, Figure 1 shows more variation in the likelihood of being obese among immigrants. Asian immigrants arrive in the United States with the lowest predicted probability of obesity and show modest changes in likelihood over time. Regardless of time spent in the United States, Hispanic and black immigrants have the highest predicted probability of obesity. Moreover, black immigrants experience the largest increase in the predicted probability of obesity as their tenure of U.S. residence increases from 0–4 years to ≥15 years.
Explanations for Immigrants’ Health Decline
The relative tempo of health decline among immigrants provides insights into the role of structural factors in shaping the health trajectories of different immigrant populations, particularly the trajectories of black and Hispanic immigrants, who experience a more pronounced increase in the likelihood of reporting poor health outcomes as they age in the United States. One set of factors is structural and individual-level exposure to racism, discrimination, and xenophobia. The ethno-racial context within which immigrants integrate into American society might produce different patterns of health for immigrants who share a racial status with marginalized U.S.-born minorities (Portes & Rumbaut, 2014; Read & Emerson, 2005). For instance, compared to white Americans, black Americans tend to have poorer health outcomes, including higher rates of hypertension, diabetes, and obesity; these disparities remain even after controlling for sociodemographic characteristics (Goosby et al., 2018; Hummer, 1996). One bio-social mechanism used to explain racial disparities in health is the impact of racism and discrimination faced by racial minorities (Brondolo et al., 2003; Sims et al., 2012; Williams et al., 2019). Indeed, perceived individual-level and structural discrimination are correlated with poor health outcomes for black Americans (Williams et al., 2019).
Policy Context and Immigrants’ Health
Gee and Ford (2011) argue that immigration policies can serve as a form of structural racism that impacts the degree of hostility faced by immigrant populations. In addition to serving as the “most permanent and broad-scale type of segregation by prohibiting groups from entering the country, deporting those already here, and limiting the rights of those deemed to be threats” (Gee & Ford, 2011, p. 122), federal immigration policies also impact the reception faced by different immigrant groups (Portes & Rumbaut, 2014).
For example, beginning in 2017, the Trump administration, initially citing concerns about potential terrorist attacks, instituted bans on immigration from several countries, including the African countries of Somalia, Sudan, Nigeria, and Eritrea. If these policies remain in place, they will dramatically limit immigration from these countries. Further, negative media attention and their new portrayal as arriving from countries with a high probability of sending terrorists to the United States will likely increase the intensity of discrimination and xenophobia faced by these groups in different parts of the country, which could hinder the groups’ health outcomes and prospects of social integration.
Similarly, discussions related to securing the border of the United States have historically been laced with racial overtones such that, the term “illegal aliens” refers to migrants from Mexico and Central America and the word “terrorists” refers to individuals from the Middle East (Gee & Ford, 2011, p. 122). Such rhetoric could increase the intensity of the xenophobia and discrimination faced by highly visible immigrant groups (Viruell-Fuentes, 2007). Asian, black, and Hispanic immigrants are more likely to perceive discrimination as their tenure of U.S. residence increases, and perceived discrimination is correlated with worse health among immigrants (Finch et al., 2001; Gee et al., 2009; Krieger et al., 2011). Consequently, as immigrants become increasingly “American” with each year they spend in the United States, they may experience “othering” and discrimination that negatively impacts their health and erodes their initial health advantage (Viruell-Fuentes, 2007).
Federal policies also determine immigrants’ access to a range of federal programs, which could impact immigrants’ health trajectories. One notable example is the 1996 Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA). Driven by the perception that immigrants migrate to the United States to exploit the country’s social welfare programs, PRWORA introduced restrictions on legal immigrants’ access to cash-transfer programs, food stamps, and health insurance (Fix et al., 2009). In particular, with some exceptions, legal immigrants entering the country after August 22, 1996, were denied federal means-tested public benefits for their first five years in the United States. A range of federal health-care policies, including the 2010 Affordable Care Act, prevent undocumented immigrants from taking advantage of programs designed to boost health-care access. Prior research has found that exclusionary policies such as PRWORA increase the proportion of immigrants without insurance, particularly among less educated, single immigrant women and their children (Kaushal & Kaestner, 2005)
Conclusion
Given the significant and continued growth of the foreign-born U.S. population, immigrants and their descendants will play a significant role in determining the health and welfare of the entire U.S. population in coming decades. Racism and discrimination have long impacted the health of minority populations, particularly black Americans, in the United States. This paper shows that black and Hispanic immigrants arrive the United States with health profiles that are better than those of their native-born counterparts and similar with respect to diabetes and hypertension to those of new white and Asian immigrants. However, time spent in the United States has a more negative impact on the health of black and Hispanic immigrants than on the health of white and Asian immigrants. Although the NHIS data do not allow us to directly measure the impact of structural factors (e.g., racism and xenophobia) on immigrants’ health, the pattern of results is consistent with such exposure having negative consequences (Goosby et al., 2018), which could be driven in part by federal policies that impact the degree of hostility faced by immigrant communities and restrict access to vital social services (Gee & Ford, 2011; Kaushal & Kaestner, 2005). More research is needed to better understand the impacts of federal and state policies on the well-documented health declines of immigrants (Almeida et al., 2016).
More research is needed to better understand the impacts of federal and state policies on the well-documented health declines of immigrants.
Funding
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant number 5R24HD047879).
Conflicts of Interest
None declared.
References
- Abraido-Lanza A. F., Chao M. T., & Florez K. R (2005). Do healthy behaviors decline with greater acculturation?: Implications for the Latino mortality paradox. Social Science & Medicine, 61(6), 1243–1255. doi: 10.1016/j.socscimed.2005.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akresh I. R., & Frank R (2008). Health selection among new immigrants. American Journal of Public Health, 98(11), 2058–2064. doi: 10.2105/AJPH.2006.100974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida J., Biello K. B., Pedraza F., Wintner S., & Viruell-Fuentes E (2016). The association between anti-immigrant policies and perceived discrimination among Latinos in the US: A multilevel analysis. SSM–Population Health, 2, 897–903. doi: 10.1016/j.ssmph.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antecol H., & Bedard K (2006). Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography, 43(2), 337–360. doi: 10.1353/dem.2006.0011 [DOI] [PubMed] [Google Scholar]
- Blewett L. A., Rivera Drew J. A., King M. L., & Williams K. C. W (2019). IPUMS health surveys : National health interview survey, Version 6.4 [data set]. IPUMS. doi: 10.18128/d070.V6.4 [DOI] [Google Scholar]
- Brondolo E., Rieppi R., Kelly K. P., & Gerin W (2003). Perceived racism and blood pressure: A review of the literature and conceptual and methodological critique. Annals of Behavioral Medicine, 25(1), 55–65. doi: 10.1207/S15324796ABM2501_08 [DOI] [PubMed] [Google Scholar]
- Feliciano C. (2020). Immigrant selectivity effects on health, labor market, and educational outcomes. Annual Review of Sociology, 46, 315–334. doi: 10.1146/annurev-soc-121919-054639 [DOI] [Google Scholar]
- Finch B. K., Hummer R. A., Kolody B., & Vega W. A (2001). The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hispanic Journal of Behavioral Sciences, 23(4), 399–429. doi: 10.1177/0739986301234004 [DOI] [Google Scholar]
- Fix M. E., Capps R., & Kaushal N (2009). Immigrants and welfare: Overview. In Fix M. E. (Ed.), Immigrants and welfare: The impact of welfare reform on America’s newcomers (pp. 1–36). Russell Sage Foundation. [Google Scholar]
- Gee G. C., & Ford C. L (2011). Structural racism and health inequities: Old issues, new directions. Du Bois Review: Social Science Research on Race, 1, 115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G. C., Ro A., Shariff-Marco S., & Chae D (2009). Racial discrimination and health among Asian Americans: Evidence, assessment, and directions for future research. Epidemiologic Reviews, 31, 130–151. doi: 10.1093/epirev/mxp009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby B. J., Cheadle J. E., & Mitchell C (2018). Stress-related biosocial mechanisms of discrimination and African American health inequities. Annual Review of Sociology, 44, 319–340. doi: 10.1146/annurev-soc-060116-053403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton T. G. (2015). The healthy immigrant (migrant) effect: In search of a better native-born comparison group. Social Science Research, 54, 353–365. doi: 10.1016/j.ssresearch.2015.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton T. G. (2019). Immigration and the remaking of Black America. Russell Sage Foundation. [Google Scholar]
- Hummer R. A. (1996). Black–White differences in health and mortality: A review and conceptual model. The Sociological Quarterly, 37(1), 105–125. doi: 10.1111/j.1533-8525.1996.tb02333.x [DOI] [Google Scholar]
- Hummer R. A., Powers D. A., Pullum S. G., Gossman G. L., & Frisbie W. P (2007). Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography, 44(3), 441–457. doi: 10.1353/dem.2007.0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushal N., & Kaestner R (2005). Welfare reform and health insurance of immigrants. Health Services Research, 40(3), 697–721. doi: 10.1111/j.1475-6773.2005.00381.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N., Kosheleva A., Waterman P. D., Chen J. T., & Koenen K (2011). Racial discrimination, psychological distress, and self-rated health among US-born and foreign-born Black Americans. American Journal of Public Health, 101(9), 1704–1713. doi: 10.2105/AJPH.2011.300168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krogstad J. M., & Gonzalez-Barrera A (2018). Key facts about US immigration policies and proposed changes. Pew Research Center. [Google Scholar]
- Palloni A., & Arias E (2004). Paradox lost: Explaining the Hispanic adult mortality advantage. Demography, 41(3), 385–415. doi: 10.1353/dem.2004.0024 [DOI] [PubMed] [Google Scholar]
- Portes A., & Rumbaut R (2014). Immigrant America: A portrait (4th ed.). University of California Press. [Google Scholar]
- Read J. G., & Emerson M. O (2005). Racial context, Black immigration and the U.S. Black/White health disparity. Social Forces, 84(1), 181–199. doi: 10.1353/sof.2005.0120 [DOI] [Google Scholar]
- Riosmena F., Everett B. G., Rogers R. G., & Dennis J. A (2014). Negative acculturation and nothing more? Cumulative disadvantage and mortality during the immigrant adaptation process among Latinos in the United States. The International Migration Review, 49(2), 443–478. doi: 10.1111/imre.12102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner R., & Dwyer J. H (1989). Acculturation and low birthweight among Latinos in the Hispanic HANES. American Journal of Public Health, 79(9), 1263–1267. doi: 10.2105/ajph.79.9.1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims M., Diez-Roux A. V., Dudley A., Gebreab S., Wyatt S. B., Bruce M. A., James, S. A., Robinson, J. C., Williams, D. R., & Taylor H. A (2012). Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. American Journal of Public Health, 102(Suppl 2), S258–S265. doi: 10.2105/AJPH.2011.300523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treas J., & Batalova J (2009). Immigrants and aging. In: P. Uhlenberg (Ed.), International handbook of population aging (pp. 365–394). Springer. [Google Scholar]
- Viruell-Fuentes E. A. (2007). Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Social Science & Medicine (1982), 65(7), 1524–1535. doi: 10.1016/j.socscimed.2007.05.010 [DOI] [PubMed] [Google Scholar]
- Williams D. R., Lawrence J. A., & Davis B. A (2019). Racism and health: Evidence and needed research. Annual Review of Public Health, 40, 105–125. doi: 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]