Abstract
Purpose:
This study aimed at describing self-harm and suicidality (SHS) in relation to unobserved heterogeneous groups of college students based on their psychiatric symptoms. SHS of each latent class were examined by race/ethnicity to inform risk factors relevant to subgroups of U.S. college population.
Methods:
The participants (N = 42,779) were drawn from the Spring 2017 American College Health Association-National College Health Assessment II (ACHA-NCHA II) Reference Group. Latent class analysis (LCA) was conducted based on participants’ reports of past-year psychiatric symptoms. The reported SHS were examined by the latent class of students and their race/ethnicity.
Results:
LCA identified two latent classes: The Emotional Exhaustion (EE) class and the Multiple Psychiatric Symptoms (MPS) class. Within the EE class, Black students were at the greatest risk for exhibiting suicide intent and attempted suicide. Within the MPS class, Multiracial students showed the highest odds of self-harm and suicidal intent, and Black students showed the highest odds of attempted suicide, followed by Asians/Pacific Islanders.
Limitations:
The findings were based on a cross-sectional dataset that did not inform the temporal relations of psychiatric symptoms and SHS.
Conclusions:
Utilizing a person-centered latent class analysis, this study revealed that Black students were of the greatest concern for SHS among those who reported only common symptoms of emotional exhaustion. The findings highlight the importance of developing preventive and remedial models that address unique risk factors and mental health needs for various subgroups of U.S. college population.
Keywords: suicide, self-harm, mental health, universities, prevention, race/ethnicity
Self-harm and suicidality (SHS) pose grave concerns for health and well-being among college students (Auerbach et al., 2018; Mortier et al., 2018). Self-harm refers to the act of intentionally causing injury to oneself; while suicide involves the effort of voluntarily causing one’s own death (Nock et al., 2008). Although SHS have been associated with a variety of mental health conditions, such as depression, anxiety disorders, borderline personality disorder, posttraumatic stress disorder, etc. (Garlow et al., 2008; Horowitz, Ballard, & Pao, 2009; Joiner, Buchman-Schmitt, & Chu, 2017; Mortier et al., 2018), many individuals who self-injure or commit suicide do not necessarily meet diagnostic criteria for any mental illness (Britton et al., 2012; Horowitz et al., 2009; Moscicki, 2001; the Centers for Disease Control and Prevention [CDC], 2018, 2019). The difficulty of accurately predicting SHS, including by psychiatric diagnosis, creates challenges for faculty, staff, and peer students to determine whether and how to intervene, particularly among students who only report common college stress experiences (e.g., feeling mentally exhausted and overwhelmed).
In attempting to identify the risk of SHS among college students, a person-centered analytical approach may offer better insight than one that is variable-centered, such as factor analysis or structural equation modeling (Koning et al., 2016; Laursen, & Hoff, 2006; Muthén & Muthén, 2000). Variable-centered approaches often assume homogeneity of a sampled population, ignoring unobserved heterogeneity that may exist within the sample (Collins & Lanza, 2010). However, students with SHS are a heterogeneous group, and certain students are more prone to self-harm/suicidality than others. A person-centered approach that focuses on the relationships of individuals may be better able to identify subgroup phenotypes who share similar characteristics or attributes, particularly when research questions are addressing group differences. Latent class analysis (LCA) is one such person-centered technique that uses the bootstrap ratio likelihood test to describe, first, the likelihood that any random individual belongs to any latent class, and second, the likelihood that an individual from a certain class would endorse certain characteristics. Another advantage of using LCA to classify individuals is that the approach is data-driven and directly derived from modeling; thus, it minimizes the need to arbitrarily determine the cutoff points for underlying dimensions of constructs of interest (Muthén & Muthén, 2000). Altogether, LCA may provide information on meaningful subgroups of college students based on their reported psychiatric symptoms, which may shed light on common risk/protective factors for SHS outcomes unique to each of the subgroups.
For the current study, we first employed LCA to identify unobserved classes of college students based on their endorsement of certain psychiatric symptoms. Given that the extant literature is scant on the subgroups of US college students based on their reported psychiatric symptoms, we did not formulate specific hypotheses regarding the number and nature of latent classes. However, we predicted that these classes would reflect the heterogeneity of this sample of students, with some tending to endorse symptoms typical of common undergraduate stress experiences (e.g., feeling overwhelmed) and others tending to endorse more psychiatric symptoms typical of mood disorders (e.g., feeling so depressed that it was difficult to function) besides common stress experiences.
From there, we examined how self-harm and suicidality of each latent symptom class of students differed by race/ethnicity. There were good reasons to examine how SHS of each symptom class varied by race/ethnicity. Specifically, minority groups face a significant amount of psychological strain and marginalization through racial discrimination and microaggressions (Harris, 2017; Jackson, Yoo, Guevarra, & Harrington, 2012; Walker, Salami, Carter, & Flowers, 2014). However, students from racial/ethnic minority groups may underreport their psychiatric distress due to lack of awareness of psychiatric illnesses, concerns regarding stigma, perceived/real treatment barriers, etc. (Abe, Mertz, Powell, & Hanzlick, 2006; Chen, Stevens, Wong, & Liu, 2019; Mitchell, Watkins, Shires, Chapman, & Burnett, 2017; Walker et al., 2014). Understanding how the link between reported psychiatric symptoms and SHS varies by race/ethnicity is important for developing culturally sensitive suicide prevention and intervention programs.
Methods
Data Source and Sample
Participants (N = 63,497) were drawn from the Spring 2017 American College Health Association-National College Health Assessment II (ACHA-NCHA II) Reference Group. Ninety-two postsecondary institutions across the United States used a random sampling technique to recruit students aged 18 years or older to complete the survey. Three institutions administered paper surveys with an average response rate of 81%, while 92 institutions administered web-based surveys with an average response rate of 19%. The overall average response rate was 21%. The response rates for this data set were on par with typically low response rates by university students. However, Fosnacht et al. (2017) demonstrated in a simulation study that a 20 to 25 percent response rate for a survey study would sufficiently provide simulated means that were very similar to the full sample estimates even with small sample sizes (correlations between the simulated means and the full sample estimates were around .90). All participants were de-identified for secondary data analysis. The current analysis was approved by the Institutional Review Board of the authors’ Institutions.
Here, we focused on degree-seeking undergraduate students in the sample with available data on all measures described in this report. Following previous studies (Ball, Ford, Russell, Williams, & Hockey, 2009; Chen et al., 2019; Liu, Stevens, Wong, Yasui, & Chen, 2019), we eliminated respondents who reported implausible height and weight data (BMI above 65 or below 16; height above 210 cm or below 120 cm; weight above 180 kg or below 35 kg). The final sample used in the analysis included 42,779 degree-seeking undergraduate students.
Measures
Sociodemographic Characteristics
Table 1 shows the sociodemographic characteristics of the sample. Ages of participants were categorized into two groups: “18–24 years” and “25+ years” (Araas & Adams, 2009; Brittain & Dinger, 2015; Lindley, Barnett, Brandt, Hardin, & Burcin, 2008). Year in school of participants was coded as 1, 2, 3, 4, and 5+ years. Both the statuses of transfer and international students were coded as either “yes” or “no.”
Table 1.
Sociodemographic Characteristics of the Sample and Prevalence of Mental Health (MH) Symptoms and Behaviors of Self-Harm and Suicidality (SHS) during the Last 12 Months (N= 42,779)
| Characteristic | Total | White | Asian/Pacific | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | ||||||||||||
| 18–24 | 40,007 | 93.5 | 27,714 | 64.8 | 2,711 | 6.3 | 1,802 | 4.2 | 4,207 | 9.8 | 3,573 | 8.4 |
| > 25 | 2,772 | 6.5 | 1,854 | 4.3 | 229 | 0.5 | 214 | 0.5 | 220 | 0.5 | 255 | 0.6 |
| Gender | ||||||||||||
| Male | 12,654 | 29.6 | 8,820 | 20.6 | 858 | 2.0 | 472 | 1.1 | 1,427 | 3.3 | 1,077 | 2.5 |
| Female | 29,082 | 68.0 | 20,048 | 46.9 | 2,018 | 4.7 | 1,493 | 3.5 | 2,898 | 6.8 | 2,625 | 6.1 |
| Non-Binary | 1,043 | 2.4 | 700 | 1.6 | 64 | 0.1 | 51 | 0.1 | 102 | 0.2 | 126 | 0.3 |
| Sexual Orientation | ||||||||||||
| Heterosexual | 34,273 | 80.1 | 23,960 | 81.0 | 2,303 | 78.3 | 1,648 | 81.7 | 3,466 | 78.3 | 2,896 | 75.7 |
| Gay/Lesbian | 1,344 | 3.1 | 901 | 3.0 | 121 | 4.1 | 48 | 2.4 | 135 | 3.0 | 139 | 3.6 |
| Bisexual | 2,780 | 6.5 | 1,793 | 6.1 | 209 | 7.1 | 121 | 6.0 | 292 | 6.6 | 365 | 9.5 |
| Asexual | 2,178 | 5.1 | 1,526 | 5.2 | 141 | 4.8 | 84 | 4.2 | 305 | 6.9 | 122 | 3.2 |
| Other | 2,204 | 5.2 | 1,388 | 4.7 | 166 | 5.6 | 115 | 5.7 | 229 | 5.2 | 306 | 8.0 |
| Institution | ||||||||||||
| Public | 22,333 | 52.2 | 15,783 | 36.9 | 1,842 | 4.3 | 1,127 | 2.6 | 1,709 | 4.0 | 1,872 | 4.4 |
| Private | 20,446 | 47.8 | 13,785 | 32.2 | 1,098 | 2.6 | 889 | 2.1 | 2,718 | 6.4 | 1,956 | 4.6 |
| Year in school | ||||||||||||
| 1st | 12,275 | 28.7 | 8,146 | 19.0 | 907 | 2.1 | 573 | 1.3 | 1,429 | 3.3 | 1,220 | 2.9 |
| 2nd | 10,130 | 23.7 | 7,016 | 16.4 | 649 | 1.5 | 494 | 1.2 | 1,050 | 2.5 | 921 | 2.2 |
| 3rd | 10,317 | 24.1 | 7,239 | 16.9 | 711 | 1.7 | 463 | 1.1 | 996 | 2.3 | 908 | 2.1 |
| 4th | 8,435 | 19.7 | 6 010 | 14.1 | 562 | 1.3 | 378 | 0.9 | 844 | 2.0 | 641 | 1.5 |
| > 5th | 1,622 | 3.8 | 1,157 | 2.7 | 111 | 0.3 | 108 | 0.3 | 108 | 0.3 | 138 | 0.3 |
| Transfer | ||||||||||||
| No | 37,318 | 87.2 | 25,941 | 60.6 | 2,493 | 5.8 | 1,729 | 4.0 | 3,875 | 9.1 | 3,280 | 7.7 |
| Yes | 5,461 | 12.8 | 3,627 | 8.5 | 447 | 1.0 | 287 | 0.7 | 552 | 1.3 | 548 | 1.3 |
| International | ||||||||||||
| No | 40,589 | 94.9 | 28,947 | 67.7 | 2,755 | 6.4 | 1,869 | 4.4 | 3,372 | 7.9 | 3,646 | 8.5 |
| Yes | 2,190 | 5.1 | 621 | 1.5 | 185 | 0.4 | 147 | 0.3 | 1,055 | 2.5 | 182 | 0.4 |
| MH Symptoms | ||||||||||||
| Hopeless | 22,858 | 53.4 | 15,252 | 51.6 | 1,680 | 57.1 | 1,084 | 53.8 | 2,578 | 58.2 | 2,264 | 59.1 |
| Overwhelmed | 38,119 | 89.1 | 26,616 | 90.0 | 2,619 | 89.1 | 1,689 | 83.8 | 3,740 | 84.5 | 3,455 | 90.3 |
| Exhausted | 36,584 | 85.5 | 25,466 | 86.1 | 2,520 | 85.7 | 1,620 | 80.4 | 3,621 | 81.8 | 3,357 | 87.7 |
| Lonely | 27,765 | 64.9 | 19,044 | 64.4 | 1,846 | 62.8 | 1,224 | 60.7 | 2,970 | 67.1 | 2,681 | 70.0 |
| Sad | 29,705 | 69.4 | 20,410 | 69.0 | 2,037 | 69.3 | 1,333 | 66.1 | 3,070 | 69.3 | 2,855 | 74.6 |
| Depressed | 17,204 | 40.2 | 11,491 | 38.9 | 1,241 | 42.2 | 783 | 38.9 | 1,920 | 43.4 | 1,769 | 46,2 |
| Anxiety | 26,679 | 62.4 | 18,562 | 62.8 | 1,841 | 62.6 | 1,142 | 56.6 | 2,573 | 58.1 | 2,561 | 66.9 |
| Anger | 17,539 | 41.0 | 11,731 | 39.7 | 1,293 | 44.0 | 873 | 43.3 | 1,862 | 42.1 | 1,780 | 46.5 |
| SHS | ||||||||||||
| Self-harm | 3,405 | 8.0 | 2,377 | 8.0 | 209 | 7.1 | 110 | 5.4 | 307 | 6.9 | 402 | 10.5 |
| Suicidal Intent | 4,872 | 11.4 | 3,221 | 10.9 | 339 | 11.5 | 227 | 11.2 | 512 | 11.6 | 573 | 15.0 |
| Attempted Suicide | 705 | 1.6 | 415 | 1.4 | 55 | 1.9 | 53 | 2.6 | 95 | 2.1 | 87 | 2.3 |
Race/ethnicity was coded based on participants’ responses to the item “How do you usually describe yourself? (Mark all that apply)” Multiple options for this item were possible, including “White,” “Black,” “Hispanic or Latino/a,” “Asian or Pacific Islander,” “American Indian, Alaska Native, or Native Hawaiian (AI/AN/NH),” “Biracial or Multiracial,” and “Other.” Mutually exclusive categories of race/ethnicity were created by coding those who selected more than one option and those who selected only “Biracial or Multiracial” as “Multiracial.” Responses with only one option selected were coded as the selected identity. The subsequent analyses did not include the “Other” and “AI/AN/NH” groups due to small sample sizes.
Within the dataset, participants’ gender identity was already recoded as “Male”, “Female”, or “Non-binary” based on student responses to three variables: sex at birth (Female/Male), transgender (Yes/No), and gender identity (Woman, Man, Trans woman, Trans man, Genderqueer, and Another Identity). Participants were coded as “Male” or “Female” when participants selected “No” for transgender item and reported that their sex at birth was in line with their gender identity (e.g., selecting “Female” as sex at birth and “Woman” as gender identity). Participants were coded as “non-binary” when they selected “Yes” for transgender or their sex at birth did not align with their gender identity. If any of the three items was missing, the participant was excluded from the analysis.
For sexual orientation, there were 11 options in the survey. Students’ choices were recoded into five categories of sexual orientation, including “Heterosexual,” “Gay/Lesbian,” “Bisexual,” “Asexual,” and “Other.” The category of “Other” included students selecting “Pansexual,” “Queer,” “Questioning,” “Same Gender Loving,” or “Another identity.”
Mental Health Related Symptoms
Eight self-report items were used to assess participants’ mental health related psychiatric symptoms, including “Felt things were hopeless”; “Felt overwhelmed by all you had to do”; “Felt exhausted (not from physical activity)”; “Felt very lonely”; “Felt very sad”; “Felt so depressed that it was difficult to function”; “Felt overwhelming anxiety”; and “Felt overwhelming anger.”
For each symptom, respondents were asked to select one out of the following options: “No, never”; “No, not in the last 12 months”; “Yes, in the last two weeks”; “Yes, in the last 30 days”; or “Yes, in the last 12 months.” To create categorical indicators for prevalence during the last 12 months, responses to each of the psychiatric symptoms were dichotomously recoded into No (combining “No, not in the past 12 months” and “No, never”) and Yes (combining all three ‘Yes’ responses for the last two weeks, 30 days, and 12 months).
Self-harm and Suicidality
Self-harm behaviors during the past 12 months were measured using one item “(Have you ever) intentionally cut, burned, bruised, or otherwise injured yourself?” Suicidal intention was measured using “(Have you ever) seriously considered suicide?” and attempted suicide was measured using “(Have you ever) attempted suicide?” For each of these items, participants were given the response options of “no, never”, “no, not in the last 12 months”, “yes, in the last 2 weeks”, “yes, in the last 30 days”, and “yes, in the last 12 months.” Similar to the recoding process of psychiatric symptoms, the prevalence of SHS during the last 12 months was indicated by combining “No, not in the past 12 months” and “No, never” into No, and all three ‘Yes’ responses for the last two weeks, 30 days, and 12 months into Yes.
Data Analysis
To identify the unobserved classes of students based on their psychiatric symptoms, latent class analysis (LCA) was implemented. All analyses were performed in the R statistical computing language and environment Version 3.6.0 (R-3.6.0; R Core Team, 2019). LCA was conducted using the poLCA packages (Linzer & Lewis, 2011) for R-3.6.0.
In LCA, models with different numbers of classes are compared to identify the model that provides the best fit to the observed data. Model selection is often determined by simultaneously considering the model fit indices, including Akaike information criteria (AIC), Bayes information criteria (BIC), and entropy (Vermunt & Magidson, 2004). The general rule of thumb for model selection is that the lower the AIC and BIC are, the better the fit of the model to the data, and the closer the value of entropy is to one, the better the class assignment is (i.e. better distinction between classes; Kline, 2005).
A series of logistic regressions were then conducted within each class to reveal the associations of SHS across the five racial/ethnic groups. Specifically, each racial/ethnic group was compared against the others, creating all possible ten pairwise comparisons for each SHS variable within each class. Significance level was adjusted using the conservative Bonferroni correction for each independent set of comparisons; thus, an alpha of .05/10 (= .005) was used to determine significant differences. The sociodemographic characteristics listed in Table 1 were controlled as covariates in the adjusted models because these characteristics have been found to be associated with mental health outcomes. The covariates included participants’ race/ethnicity (Chen et al., 2019), age (Trenz, Ecklund-Flores, & Rapoza, 2015), gender (Eisenberg, Hunt, & Speer, 2013), sexual orientation (Kerr, Santurri, & Peters, 2013), year in school (Bewick, Koutsopoulou, Miles, Slaa, & Barkham, 2010), and transfer and international student status (Beiter et al., 2015).
Results
Prevalence of Psychiatric Symptoms, Self-Harm, and Suicidality
The prevalence of psychiatric symptoms and Self-Harm and Suicidality (SHS) during the past 12 months is shown in the lower half of Table 1. A large proportion of students felt overwhelmed (89.1%) and emotionally exhausted (85.5%), and more than half of the participants felt sad (69.4%), lonely (64.9%), anxious (62.4%), and hopeless (53.4%). Approximately 8% of the students reported past-year self-harm behavior, about 11.4% intention to commit suicide, and close to 1.6% actual suicide attempts.
Latent Class Analysis
To examine unobserved classes of students who shared similar psychiatric symptoms, latent class analyses for two, three, and four latent classes were conducted based on participants’ endorsements of the eight symptoms. A two-class model solution was adopted due to the highest value of entropy (entropy = .87; AIC = 309857.90; BIC = 310005.20; Chi-square (df = 238) = 31472.66, parameters = 17), indicating the best class differentiation. The first class was labeled as Emotional Exhaustion class due to members’ high probabilities of endorsing items of feeling overwhelmed (probability = .75) or exhausted (.67) as opposed to low probabilities of feeling sad (.29), lonely (.27), anxious (.25), or depressed (.02) (Table 2, and as seen in Figure 1). The second class was labeled as Multiple Psychiatric Symptoms class because members not only showed high probabilities of endorsing symptoms of feeling overwhelmed (.99) and exhausted (.99) but also feeling sad (.98), lonely (.92), anxious (.89), hopeless (.84), depressed (.68), or angry (.63). Approximately 40% (n = 17,313) of students fell into the Emotional Exhaustion class and 60% (n = 25,466) the Multiple Psychiatric Symptoms class. The sociodemographic compositions of the two identified latent classes are also shown in Table 2.
Table 2.
Probabilities of Predicted Class Membership, Endorsement for Psychiatric Symptoms, and the Sociodemographic Compositions of the Two Identified Latent Classes
| Class | Emotional Exhaustion Symptoms | Multiple Psychiatric Symptoms |
|---|---|---|
| Predicted class membership | .40 (n = 17,313) | .60 (n = 25,466) |
| Mental Health Symptoms | ||
| Hopeless | .11 | .84 |
| Overwhelmed | .75 | .99 |
| Exhausted | .67 | .99 |
| Lonely | .27 | .92 |
| Sad | .29 | .98 |
| Depressed | .02 | .68 |
| Anxiety | .25 | .89 |
| Anger | .10 | .63 |
| Race | % | % |
| White | 70.4 | 68.3 |
| Hispanic | 6.8 | 6.9 |
| Black | 5.0 | 4.5 |
| Asian/Pacific Islander | 10.1 | 10.5 |
| Multiracial | 7.7 | 9.8 |
| Age | ||
| 18 – 24 | 91.8 | 94.7 |
| > 25 | 8.2 | 5.3 |
| Gender | ||
| Male | 37.4 | 24.3 |
| Female | 61.3 | 72.5 |
| Non-binary | 1.3 | 3.2 |
| Sexual Orientation | ||
| Heterosexual | 86.9 | 75.6 |
| Gay/lesbian | 2.1 | 3.9 |
| Bisexual | 3.2 | 8.8 |
| Asexual | 5.7 | 4.7 |
| Other | 2.2 | 7.2 |
| Year in School | ||
| 1st | 29.2 | 28.3 |
| 2nd | 22.8 | 24.3 |
| 3rd | 23.5 | 24.5 |
| 4th | 20.7 | 19.1 |
| > 5th | 3.7 | 3.8 |
| Transfer | ||
| No | 87.4 | 87.1 |
| Yes | 12.6 | 12.9 |
| International students | ||
| No | 94.5 | 95.1 |
| Yes | 5.5 | 4.9 |
Figure 1.
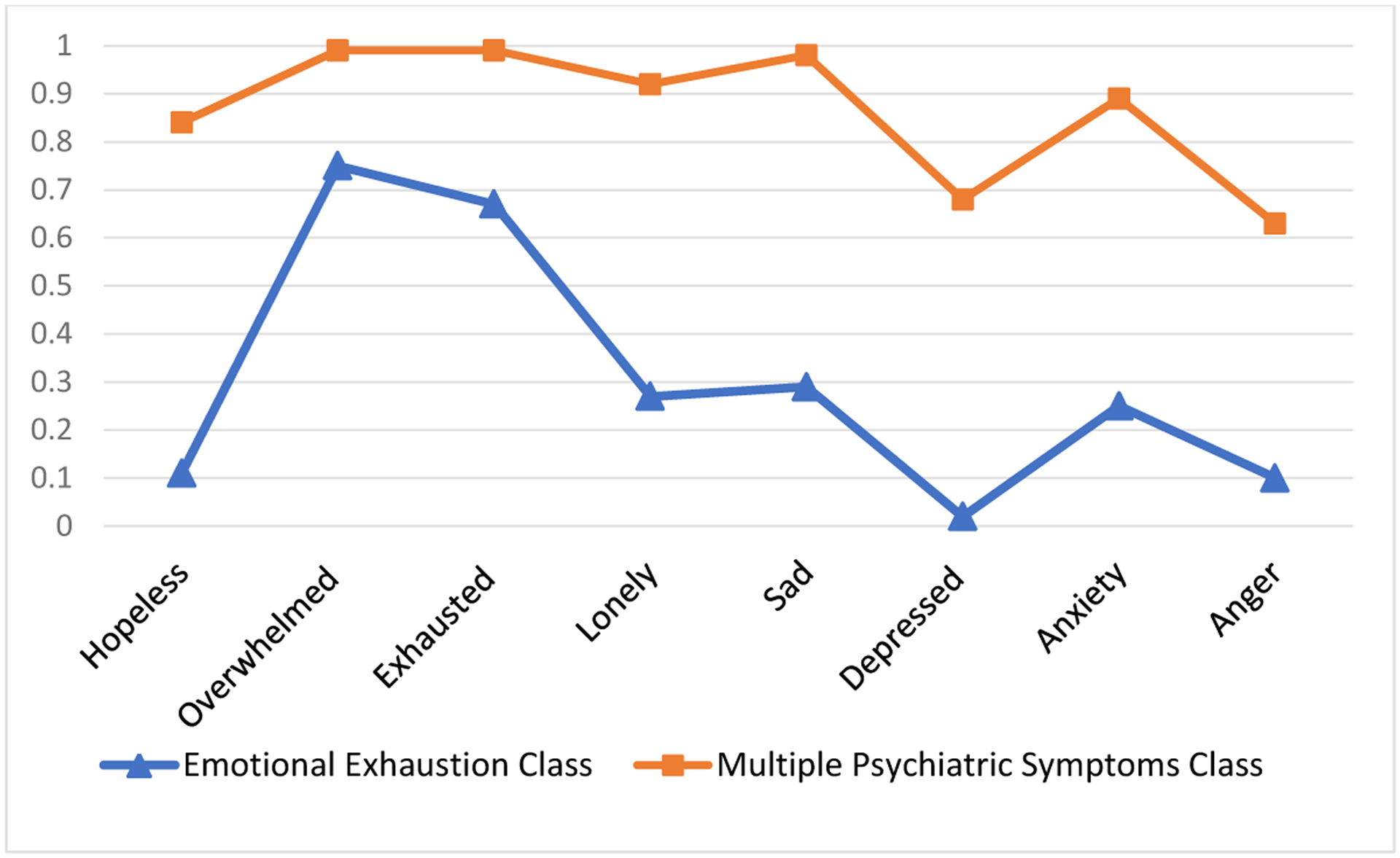
Probabilities of Endorsing Psychiatric Symptoms among Students from the Emotional Exhaustion Class (n = 17,313) and the Multiple Psychiatric Symptoms Class (n = 25,466)
Differences in SHS across Racial/Ethnic Groups
Table 3 and Figure 2 show the percentages of the two class members reporting self-harm, suicidal intent, and attempted suicide by race/ethnicity. Overall, the prevalence of SHS was much higher in the Multiple Psychiatric Symptoms Class (2.3% to 22.5%) than in the Emotional Exhaustion Class (0% to 1.4%). Further information on the prevalence of the three categories of SHS and their combinations is shown in the supplementary data file. Among those who reported at least one category, the largest group included those who reported only suicidal intent (n = 2769, 6.5%), followed by those who reported only self-harm (n = 1473, 3.4%), then both self-harm and suicidal intent (n = 1424, 3.3%), and those who reported all three categories (n = 499, 1.2%).
Table 3.
Percentages of Class Members Reporting Self-harm, Suicidal Intent, Attempted Suicide (SHS) by Race/Ethnicity
| Emotional Exhaustion Symptoms (n =17,313) | ||||||
|---|---|---|---|---|---|---|
| SHS | Across Races | White | Hispanic | Black | Asian/Pacific Islander | Multiracial |
| % | % | % | % | % | ||
| Self-harm | .87 | .85 | .76 | 1.26 | 1.03 | .75 |
| Suicidal intent | .49 | .39 | .34 | 1.38 | .57 | .83 |
| Attempted suicide | .18 | .16 | .17 | .69 | .17 | .00 |
| SHS | Multiple Psychiatric Symptoms (n = 25,466) | |||||
| Across Races | White | Hispanic | Black | Asian/Pacific Islander | Multiracial | |
| % | % | % | % | % | ||
| Self-harm | 12.78 | 13.08 | 11.40 | 8.65 | 10.79 | 15.68 |
| Suicidal intent | 18.80 | 18.25 | 19.09 | 18.79 | 18.74 | 22.48 |
| Attempted suicide | 2.65 | 2.27 | 3.02 | 4.11 | 3.43 | 3.48 |
Figure 2.
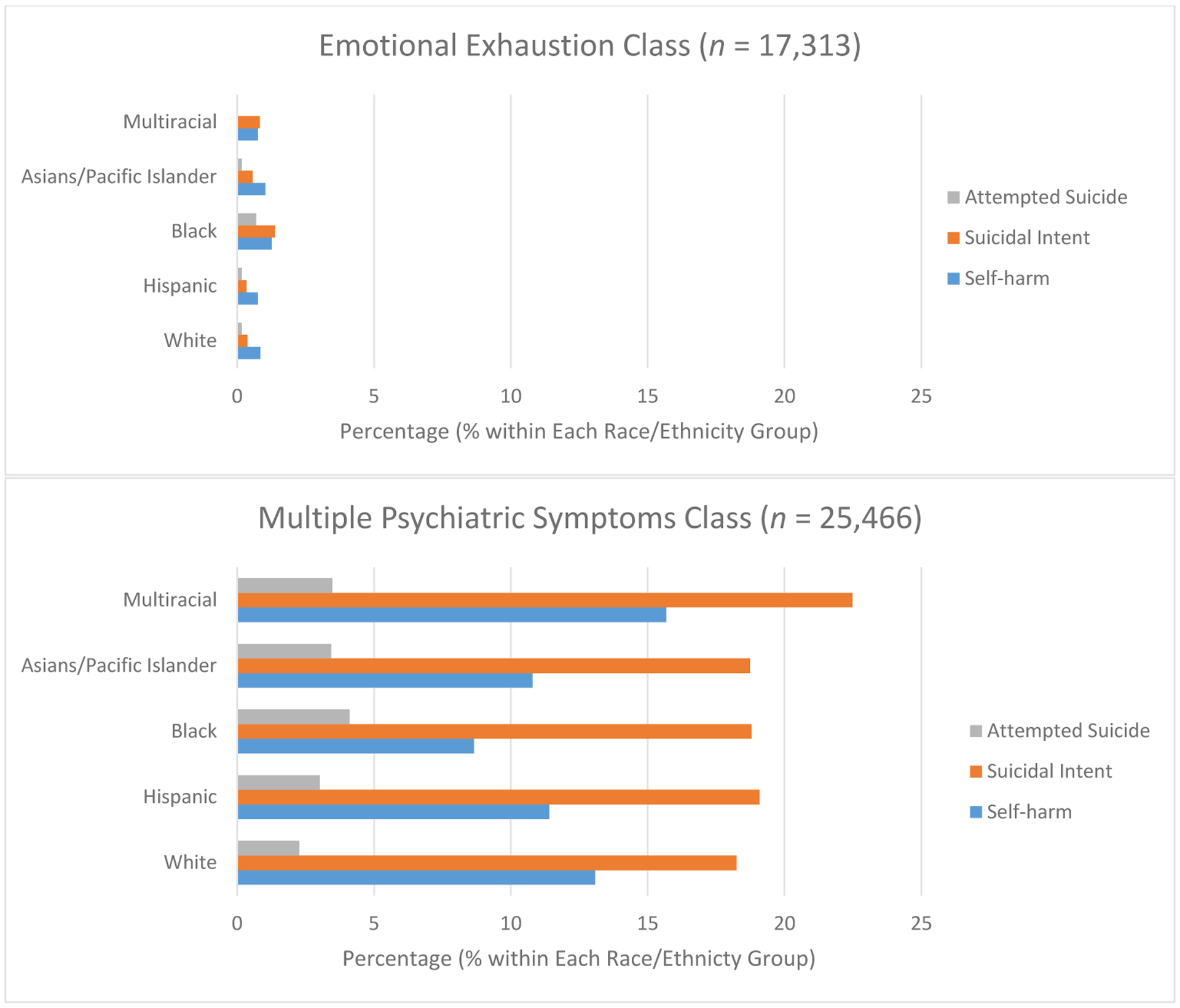
Percentages of Class Members Reporting Self-harm, Suicidal Intent, Attempted Suicide (SHS) by Race/Ethnicity in the Two Identified Latent Classes
The adjusted odds ratios of each of the three SHS outcomes by race/ethnicity among members from the Emotional Exhaustion class are also summarized in the supplementary data file. For self-harm, no significant differences were observed across race/ethnicity groups in this class. However, racial/ethnic differences were observed for the suicidal intent and attempted suicide outcomes. Specifically, Black students showed significantly higher odds for suicidal intent (OR = 3.61, B = 1.28, SE = .33, z = 3.91, p < .0001) and attempted suicide (OR = 4.10, B = 1.41, SE = .47, z = 2.98, p= .003) when compared to White students. The likelihood for any of the three SHS measures for all the other racial/ethnic groups did not significantly differ from White students after Bonferroni correction. Of note, Multiracial students from the Emotional Exhaustion class were not included in the regression models because none of the Multiracial students from the Emotional Exhaustion Class reported instances of attempted suicide in the past 12 months.
The adjusted odds ratios of the three SHS outcomes by race/ethnicity among members from the class of Multiple Psychiatric Symptoms are also summarized in the supplementary data file. None of the minority groups showed higher odds of self-harm than White students. However, the minority groups were generally more likely to endorse suicidal intent and attempted suicide than White students. Specifically, Multiracial students showed higher odds of suicidal intent (OR = 1.20, B = .18, SE = .05, z = 3.45, p < .001) when compared to White students. Similar to the Black students from the Emotion Exhaustion class, Black students from the Multiple Psychiatric Symptoms class also exhibited higher odds for attempted suicide (OR = 1.90, B = .64, SE = .16, z = 4.03, p < .001) when compared to White students. In fact, the odds ratio for attempted suicide reported by Black students in the Multiple Psychiatric Symptoms class were also higher than other minority groups, including Asian/Pacific Islander students and Multiracial students (see supplementary data file). Figure 3 illustrates the adjusted odd rations of SHS by race/ethnicity for both classes.
Figure 3.
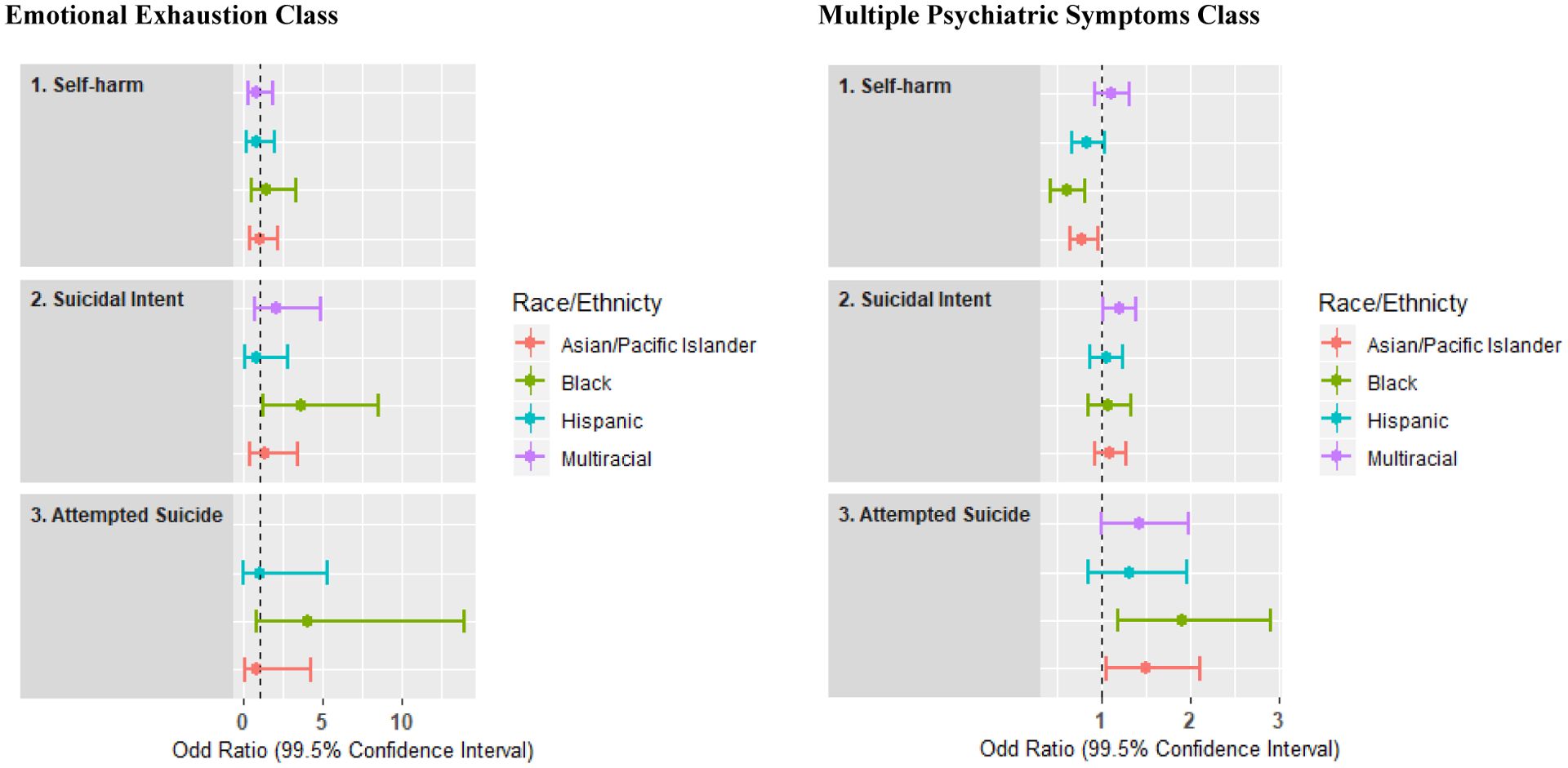
Adjusted Odd Ratios of Self-harm, Suicidal Intent, Attempted Suicide by Race/Ethnicity for Class Members from the Emotional Exhaustion Class (left) and the Multiple Psychiatric Symptoms Class (right).
Note. White students were used as the reference group in both analyses. Odds ratios using other racial/ethnic groups as the comparison groups can be found in the supplementary file.
Discussion
We observed that rates of emotional distress in the current sample were high, with close to 90% of students reporting feeling overwhelmed and emotionally exhausted, and more than half reporting feeling sad, lonely, anxious, and hopeless during the past 12 months. Approximately 8% of the students reported past-year self-harm, 11.4% suicidal intent, and 1.6% attempted suicide; these rates were consistent with previous findings for SHS in other samples (e.g., Barrios, Everett, Simon, & Brener, 2000; Garlow et al., 2008; Nock et al., 2008; Whitlock et al., 2011). The results corroborate previous findings suggesting escalating mental health concerns among US college students and a pressing need to improve early identification and intervention of mental health issues and SHS (Chen et al., 2019; Liu et al., 2019; Xiao et al., 2017).
Using latent class analysis—a person-centered analytical method—we identified two unobserved classes of college students based on their endorsement of psychiatric symptoms during the last 12 months. The two identified classes revealed the heterogeneity of the students in the sample, with one characterized by common undergraduate experiences of emotional overwhelm and exhaustion, and another by multiple psychiatric symptoms typical of mood disorders besides emotional overwhelm and exhaustion. There were 1.5 times more students characterized as belonging to the Multiple Psychiatric Symptoms class relative to those characterized primarily in the Emotional Exhaustion class.
Those students who reported only common symptoms of emotional exhaustion yet ended up engaging in SHS were of the gravest concern. Students who engaged in SHS without clear warning signs pose tremendous challenges for prevention and intervention efforts aimed at reducing SHS in college students. Our findings revealed that Black college students were at greatest risk for exhibiting SHS despite reporting symptoms that predominantly involved no more than experiences of emotional overwhelm and exhaustion. Several factors may help account for the elevated risk for SHS in Black students. Black college students may face social pressures to succeed, and perceived discrimination can worsen their academic strains (Stevens, Liu, & Chen, 2018), which has been found to be a precipitating factor for suicidality (De Luca, Yan, Lytle, & Brownson, 2014). Black college students may also be less likely to report psychiatric symptoms or disclose suicidality relative to other racial/ethnic groups (Abe et al., 2006; Chen et al., 2019; Walker et al., 2014). They may also be concerned with stigmatization associated with mental disorders and thus be reluctant to report their psychiatric symptoms (Walker et al., 2017), making their suicidality less predictable and more difficult to identify. Taylor and Kuo’s (2018) use of the theory of planned behavior (TPB) for demonstrating how a variety of factors contribute to Black American’s low psychological help-seeking, offers an organizing framework for not endorsing warning signs. TPB explains that the collective experiences of perceived negative consequences of seeking help (i.e., academic retaliation, mental illness stigma); intragroup pressure against psychological help-seeking (i.e. endorsing beliefs such as “Black people don’t get mental illness,” “Black people who seek professional help have less faith in God”, and “Black people must be strong”) and reported help-seeking barriers (i.e., cultural mistrust, lack of racially congruent therapeutic relationships, microaggressions in therapy) might perpetuate a reluctance by Black students to endorse more obvious mental health related symptoms such as “overwhelming anxiety”, “overwhelming anger” and feeling “so depressed that it was difficult to function.” Paradoxically, well-documented evidence of the negative psychological and physical impact of race-based trauma among students of color (Carter, 2007; Pieterse, Carter, Evans, & Walter, 2010), may account for an elevated risk of severe outcomes such as SHS. It may be that the juxtaposition of race-based trauma and TPB factors underlies the disconnect between Black students engaging in SHS without endorsing psychiatric symptoms.
Overall, those in the Multiple Psychiatric Symptoms class were more likely to engage in SHS compared to those in the Emotional Exhaustion class. This finding was consistent with documented links between increased number of psychiatric conditions and greater risk for suicidality (Holmstrand, Bogren, Mattisson, & Brådvik, 2015; Brådvik, 2018; Nock, Hwang, Sampson, & Kessler, 2010). Among members of the Multiple Psychiatric Symptoms class, Multiracial students showed the highest odds of self-harm and suicidal intent, and Black students showed the highest odds of attempted suicide, followed by Asians/Pacific Islanders. The findings were consistent with prior reports underscoring the elevated rates of concerning psychiatric symptoms and self-injury and suicidality among racial/ethnic minority groups (Bennett & Joe, 2015; Britton et al., 2012; Chen et al., 2019; Liu et al., 2019). While we do not have data on ethnic identity development, it is possible that the high rates of SHS among the Multiracial students might be partially attributable to challenges that come with having a mixed-race identity. Multiracial students may encounter persistent struggles while having to integrate their multiple racial/ethnic backgrounds to forge a coherent sense of identity (Harris, 2017; Jackson et al., 2012). They may also more frequently experience psychological distress due to perceived racial discrimination (Harris, 2017; Jackson et al., 2012) and a disturbed sense of belonging due to the discrepancy between their self-identification and others’ perception of them as members of certain racial/ethnic groups (Campbell, & Troyer, 2007; Harris, 2017).
Although the prevalence of SHS was much higher in the Multiple Psychiatric Symptoms class, the endorsement of multiple symptoms suggested that members from this class were cognizant of their mental health conditions. While being attuned to psychiatric symptoms does not necessarily relate to constructive help-seeking behavior, awareness and reporting of psychiatric symptoms may facilitate screening and identifying warning signs of SHS and addressing the needs for professional intervention (Britton et al., 2012).
Limitations and Strengths
Several limitations of this study warrant further investigation. First, although the findings revealed the associations between psychiatric symptoms and SHS, the findings were based on a cross-sectional dataset and the analyses were correlational in nature. Thus, it is difficult to determine if SHS were consequences of psychiatric symptoms or vice versa. Future research with longitudinal components may shed light on the temporal relations of psychiatric symptoms and SHS. Second, the racial/ethnic differences in SHS addressed in this research did not provide information on variations across subgroups (such as differences among students from Chinese, Japanese, Korean, Filipino, etc. backgrounds within the larger group of Asians/Pacific Islanders). Future research would benefit from evaluating subgroup differences to target unique issues in each population. Third, this research was conducted entirely based on self-report; without information reported by third parties (e.g., doctors, parents, or friends), it was impossible to verify the reported symptoms and behaviors. Also, the study did not control for mental health diagnoses or services students received during the last 12 months. Therefore, it is difficult to ascertain whether the differential associations of SHS with race/ethnicity by class of symptoms were affected by students’ perception of their mental health diagnoses or outcomes of interventions. In fact, latent classes of psychiatric symptoms, psychiatric diagnoses, and SHS, are all different ways of parsing out students of concern. The range of categories speak to the challenge of our psychiatric nosology and how good symptoms/diagnoses are at describing phenotypes and/or predicting outcomes in subgroups of college students.
Despite the above considerations, the current study presents a novel approach utilizing latent class analysis to revealing unobserved classes of psychiatric symptoms in a large sample of college students. The study also documents the differential associations of the latent classes of symptoms with self-harm and suicidality by race/ethnicity. These findings contribute to refining our understanding of factors conferring risk for SHS and point to the importance of supporting racial/ethnic minority students, particularly Black students, to buffer against dangerous mental health outcomes such as SHS, even when their reported symptoms only reflect common undergraduate experiences such as emotional overwhelm and exhaustion.
Conclusion
Utilizing a person-centered analytical method, this study unveiled two latent classes of college student members based on their endorsement of psychiatric symptoms: one characterized primarily by symptoms of emotional exhaustion, the other by multiple psychiatric symptoms of mood disorders in addition to symptoms of emotional exhaustion. In the Multiple Psychiatric Symptoms class, Multiracial students showed the highest odds of self-harm and suicidal intent, and Black students showed the highest odds of attempted suicide. Notably, among those who reported only common symptoms of emotional overwhelm and exhaustion, Black students were at the greatest risk for engaging in SHS. This study highlights a need to develop models that are sensitive to the differential associations of SHS with racial/ethnic backgrounds in order to improve the effectiveness of screening, prevention, and intervention for self-harm and suicidality in college students.
Supplementary Material
Highlights.
Latent class analysis identified two unobserved classes of US college students (N = 42,779).
One class was characterized by emotional exhaustion, the other multiple psychiatric symptoms.
Black students showed the highest odds for suicidality in the class of emotional exhaustion.
Multiracial students showed the highest odds for suicidality with multiple symptoms.
Clinical models should address unique risk factors for subgroups of college students.
Acknowledgements
The authors with to thank the American College Health Association for providing and approving the use of this this dataset: American College Health Association-National College Health Assessment, Spring 2017. Hanover, MD: American College Health Association [producer and distributor]; (2017-04-17 of distribution). The opinions, findings, and conclusions presented/reported in this article/presentation are those of the author(s), and are in no way meant to represent the corporate opinions, views, or policies of the American College Health Association (ACHA). The ACHA does not warrant nor assume any liability or responsibility for the accuracy, completeness, or usefulness of any information presented in this article/presentation. Support for preparing this manuscript was provided through the Mary A. Tynan Faculty Fellowship and a NIMH K23 MH 107714-01 A1 award (to C.H.L.), the SLEMCO/LEQSF Regents Professorship in Liberal Arts award (to H.C.L.), and a Willamette University Atkinson Research Award (to C.S.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest/Competing interests
There were no commercial associations, current and over the past 5 years, that might pose a conflict of interest on this research. No financial disclosures were reported by the authors of this paper.
Contributor Information
Hung-Chu Lin, University of Louisiana at Lafayette.
Manyu Li, University of Louisiana at Lafayette.
Courtney Stevens, Willamette University.
Stephanie Pinder-Amaker, McLean Hospital, Harvard Medical School.
Justin A. Chen, Massachusetts General Hospital, Harvard Medical School.
Cindy H. Liu, Brigham and Women’s Hospital, Harvard Medical School.
References
- Abe K, Mertz K, Powell K, & Hanzlick R (2006). Characteristics of black and white suicide decedents in Fulton County, Georgia, 1988–2002. American Journal of Public Health, 96, 1794–1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araas TE, & Adams TB (2009). Protective behavioral strategies and negative alcohol-related consequences in college students. Journal of Drug Education, 38(3), 211–224. [DOI] [PubMed] [Google Scholar]
- Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, … WHO WMH-ICS Collaborators. (2018). WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. Journal of Abnormal Psychology, 127(7), 623–638. 10.1037/abn0000362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball J, Ford J, Russell A, Williams L, & Hockey R (2009). Data cleaning for height and weight—Young and mid-aged. Australia: Australian Longitudinal Study on Women’s Health. [Google Scholar]
- Barrios LC, Everett SA, Simon TR, & Brener ND (2000). Suicide ideation among US college students: Associations with other injury risk behaviors. Journal of American College Health, 48(5), 229–233. [DOI] [PubMed] [Google Scholar]
- Bennett MD, & Joe S (2015). Exposure to Community Violence, Suicidality, and Psychological Distress Among African American and Latino Youths: Findings From the CDC Youth Violence Survey. Journal of Human Behavior in the Social Environment, 25(8), 775–789. 10.1080/10911359.2014.922795 [DOI] [Google Scholar]
- Bewick B, Koutsopoulou G, Miles J, Slaa E, & Barkham M (2010). Changes in undergraduate students’ psychological well-being as they progress through university. Studies in Higher Education, 35(6), 633–645. 10.1080/03075070903216643 [DOI] [Google Scholar]
- Brådvik L (2018). Suicide risk and mental disorders. International Journal of Environmental Research and Public Health, 15(9), 2028. doi: 10.3390/ijerph15092028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brittain DR, & Dinger MK (2015). An examination of health inequities among college students by sexual orientation identity and sex. Journal of Public Health Research, 4(1). 10.4081/jphr.2015.414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton PC, Ilgen A, Valenstein M, Knox K, Claassen CA, & Conner KR (2012). Differences Between Veteran Suicides With and Without Psychiatric Symptoms. American Journal of Public Health, 102(S1), S125–S130. 10.2105/AJPH.2011.300415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell ME, & Troyer L (2007). The implications of racial misclassification by observers. American Sociological Review, 72(5), 750–765. 10.1177/000312240707200505 [DOI] [Google Scholar]
- Carter RT (2007). Racism and psychological and emotional injury: Recognizing and assessing race-based traumatic stress. The Counseling Psychologist, 35(13), 13–105. [Google Scholar]
- Centers for Disease Control and Prevention (2018). Suicide rising across the US. Retrieved from https://www.cdc.gov/vitalsigns/suicide/index.html
- Centers for Disease Control and Prevention (2019). Web-based Injury Statistics Query and Reporting System (WISQARS). National center for injury prevention and control, center for disease control and prevention. Retrieved from http://www.cdc.gov/injury/wisqars/index.html [Google Scholar]
- Chen JA, Stevens C, Wong SH, & Liu CH (2019). Psychiatric symptoms and diagnoses among US college students: A comparison by race and ethnicity. Psychiatric Services, 70(6), 442–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2010). Latent class and latent transition analysis with applications in the social, behavioural, and health sciences. Hoboken, NJ: John Wiley & Sons, Inc. [Google Scholar]
- De Luca S, Yan Y, Lytle M, & Brownson C (2014). The associations of race/ethnicity and suicidal ideation among college students: A latent class analysis examining precipitating events and disclosure patterns. Suicide and Life-Threatening Behavior, 44(4), 444–456. 10.1111/sltb.12102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D, Hunt J, & Speer N (2013). Mental health in American colleges and universities: Variation across student subgroups and across campuses. The Journal of Nervous and Mental Disease, 201, 60–67. 10.1097/NMD.0b13e31827ab077 [DOI] [PubMed] [Google Scholar]
- Fosnacht K, Sarraf S, Howe E, & Peck LK (2017). How important are high response rates for college surveys? The Review of Higher Education 40(2), 245–265. 10.1353/rhe.2017.0003 [DOI] [Google Scholar]
- Garlow SJ, Rosenberg J, Moore JD, Haas AP, Koestner B, Hendin H, & Nemeroff CB (2008). Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depression and Anxiety, 25(6), 482–488. 10.1002/da.20321 [DOI] [PubMed] [Google Scholar]
- Harris JC (2017). Multiracial campus professionals’ experiences with multiracial microaggressions. Journal of College Student Development, 58(7), 1055–1073. 10.1080/13613324.2016.1248836 [DOI] [Google Scholar]
- Holmstrand C, Bogren M, Mattisson C, & Brådvik L (2015). Long‐term suicide risk in no, one or more mental disorders: The Lundby Study 1947–1997. Acta Psychiatrica Scandinavica, 132(6), 459–469. 10.1111/acps.12506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM, Ballard ED, & Pao M (2009). Suicide screening in schools, primary care and emergency departments. Current Opinion in Pediatrics, 21(5), 620–627. 10.1097/MOP.0b013e3283307a89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KF, Yoo HC, Guevarra R Jr., & Harrington BA (2012). Role of identity integration on the relationship between perceived racial discrimination and psychological adjustment of multiracial people. Journal of Counseling Psychology, 59(2), 240–250. https://doi/10.1037/a0027639 [DOI] [PubMed] [Google Scholar]
- Joiner TE, Buchman-Schmitt JM, Chu C, & Hom MA (2017). A sociobiological extension of the interpersonal theory of suicide [Editorial]. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 38(2), 69–72. 10.1027/0227-5910/a000463 [DOI] [PubMed] [Google Scholar]
- Kerr DL, Santurri L, & Peters P (2013). A comparison of lesbian, bisexual, and heterosexual college undergraduate women on selected mental health issues. Journal of American College Health, 61(4), 185–194. doi: 10.1080/07448481.2013.787619 [DOI] [PubMed] [Google Scholar]
- Kline RB (2005). Principles and practice of structural equation modeling (2nd ed). New York: Guilford Press. [Google Scholar]
- Koning M, Hoekstra T, Jong E, Visscher TLS, Seidell JC, & Renders CM (2016). Identifying developmental trajectories of body mass index in childhood using latent class growth (mixture) modelling: associations with dietary, sedentary and physical activity behaviors: a longitudinal study. BMC Public Health, 16, 1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen B, & Hoff E (2006). Person-centered and variable-centered approaches to longitudinal data. Merrill-Palmer Quarterly, 52(3), 377–389. 10.1353/mpq.2006.0029 [DOI] [Google Scholar]
- Lindley LL, Barnett CL, Brandt HM, Hardin JW, & Burcin M (2008). STDs among sexually active female college students: Does sexual orientation make a difference? Perspectives on Sexual and Reproductive Health, 40(4), 212–217. [DOI] [PubMed] [Google Scholar]
- Linzer DA, & Lewis JB (2011). PoLCA: An r package for polytomous variable latent class analysis. Journal of Statistical Software, 42(10). https://www.jstatsoft.org/ [Google Scholar]
- Liu CH, Stevens C, Wong SHM, Yasui M, & Chen JA (2019). The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. Depression & Anxiety, 36, 8–17. 10.1002/da.22830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JA, Watkins DC, Shires D, Chapman RA, & Burnett J (2017). Clues to the blues: Predictors of self-reported mental and emotional health among older African American men. American Journal of Men’s Health, 11(5), 1366–1375. doi: 10.1177/1557988315600064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscicki EK (2001). Epidemiology of Completed and Attempted Suicide: Toward a Framework for Prevention. Clinical Neuroscience Research, 1, 310–323. 10.1016/S1566-2772(01)00032-9 [DOI] [Google Scholar]
- Mortier P, Auerbach RP, Alonso J, Bantjes J, Benjet C, Cuipers P, … Kessler RC (2018). Suicidal thoughts and behaviors among firstyear college students: Results from the WMH-ICS project. Journal of the American Academy of Child & Adolescent Psychiatry, 57(4), 263–273. 10.1016/j.jaac.2018.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, & Muthén LK (2000). Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism–Clinical and Experimental Research, 24(6), 882–891. [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso JL, Angermeyer M, Beautrais A, … Williams D (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry, 192(2), 98–105. 10.1192/bjp.bp.107.040113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M, Hwang I, Sampson N, & Kessler RC (2010). Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry, 15, 868–876. 10.1038/mp.2009.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse PL, Carter RT, Evans SA, & Walter RA (2010). An exploratory examinination of the associations among racial and ethnic discrimination, racial climate, and trauma-related symptoms in a college student population. Journal of Counseling Psychology, 57(3), 255–263. [DOI] [PubMed] [Google Scholar]
- R Core Team (2019). R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria: Available online at https://www.R-project.org/. [Google Scholar]
- Stevens C, Liu CH, & Chen JA (2018). Racial/ethnic disparities in US college students’ experience: Discrimination as an impediment to academic performance. Journal of American College Health, 66(7), 665–673. [DOI] [PubMed] [Google Scholar]
- Taylor RE, & Kuo BC (2018). Black American psychological help-seeking intention: an integrated literature review with recommendations for clinical practice. Journal of Psychotherapy Integration. Advance online publication. 10.1037/int0000131 [DOI] [Google Scholar]
- Trenz RC, Ecklund-Flores L, & Rapoza K (2015). A comparison of mental health and alcohol use between traditional and nontraditional students. Journal of American College Health, 63(8), 584–588. 10.1080/07448481.2015.1040409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt JK, & Magidson J (2004). Latent class analysis In The sage encyclopedia of social sciences research methods (2nd ed., pp. 549–553). Sage Publications, Inc. [Google Scholar]
- Walker RL, Salami TK, Carter SE, & Flowers K (2014). Perceived Racism and Suicide Ideation: Mediating Role of Depression but Moderating Role of Religiosity among African American Adults. Suicide and Life-Threatening Behavior, 44(5), 548–559. 10.1111/sltb.12089 [DOI] [PubMed] [Google Scholar]
- Walker R, Francis D, Brody G, Simons R, Cutrona C, & Gibbons F (2017). A Longitudinal Study of Racial Discrimination and Risk for Death Ideation in African American Youth. Suicide and Life-Threatening Behavior, 47(1), 86–102. 10.1111/sltb.12251 [DOI] [PubMed] [Google Scholar]
- Whitlock J, Muehlenkamp J, Purington A, Eckenrode J, Barreira P, Baral Abrams, … Knox K (2011). Nonsuicidal self-injury in a college population: General trends and sex differences. Journal of American College Health, 59(8), 691–698. 10.1080/07448481.2010.529626 [DOI] [PubMed] [Google Scholar]
- Xiao H, Carney DM, Youn SJ, Janis RA, Castonguay LG, Hayes JA, & Locke BD (2017). Are we in crisis? National mental health and treatment trends in college counseling centers. Psychological Services, 14 (4), 407–415. 10.1037/ser0000130 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


