Abstract
Objectives:
Psychosocial challenges associated with perinatally acquired HIV (PHIV) infection are well known, yet many children infected with HIV since birth demonstrate positive outcomes, referred to as resilience. The purpose of this study was to evaluate emotional–behavioral development and identify salient predictors of resilience among long-term survivors of PHIV.
Design:
Prospective investigation of children with PHIV compared with demographically similar perinatally HIV-exposed but uninfected (PHEU) and HIV-unexposed, uninfected (HUU) children, all from Thailand and Cambodia.
Methods:
The Child Behavior Checklist (CBCL; parent version) was administered at baseline and annual follow-up visits (median follow-up of 3 years) to children age 6–14. Resilience was defined as consistent CBCL scores on the Internalizing, Externalizing or Total Problem T scales within normative ranges (T-scores <60) at every time point. Generalized estimating equations examined CBCL scores over time and logistic models examined demographic, socioeconomic, and cultural predictors of resilience.
Results:
Participants included 448 children (236 PHIV, 98 PHEU, 114 HUU), with median (interquartile range) age at first evaluation of 7 (6–9) years. Children with PHIV exhibited similar rates of resilience as PHEU and HUU on the Externalizing and Total Problems scales. Resilience on the Internalizing scale was more likely in PHEU (71%) compared with PHIV (59%) or HUU (56%), P = 0.049. Factors associated with resilience in adjusted models included: HIV-exposed but uninfected status, higher household income, Cambodian nationality, female sex, and caregiver type.
Conclusion:
Despite biopsychosocial risks, resilience is observed among PHIV and PHEU children. Further study is needed to understand mechanisms underlying associated factors and intervention priorities.
Keywords: HIV infection, longitudinal, perinatal, resilience
Introduction
Early studies of children and adolescents with perinatally acquired HIV (PHIV) infection revealed heightened risk for behavioral problems and psychiatric disorders [1-4]. Biological, genetic, and social factors were implicated as pathways of causality, including atypical early brain development, ongoing or intermittent neuroinflammation, HIV treatment toxicities, and effects of living in families affected by illness, poverty and stressful life events [5-7]. With the advent of effective antiretroviral therapy (ART), however, HIV disease morbidity diminished with concomitant improvement in quality of life among many children with PHIV [8]. More recent studies of emotional and behavioral development among children with PHIV in the era of ART reveal mixed results [9-11]. Across investigations, children with PHIV demonstrated higher, similar or sometimes lower rates of emotional and behavioral problems than HIV-exposed but uninfected (HEU) children, HIV unexposed, uninfected (HUU) children, or the general population [12-15]. However, limited longitudinal studies preclude firm conclusions regarding the stability of mental health, particularly during adolescence, when brain and cognitive development is dynamic and social stress and risky behavior escalate.
Recent efforts to understand mental health functioning among children at risk have expanded to include identification of characteristics associated with resilience, that is, positive development and adaptation in the presence of adversity [16-18]. These have been helpful in identifying individual, family, and community characteristics that are likely to promote positive psychosocial development and reduce the likelihood of mental health disorders as children age. For example, key strengths include social and academic competency, adequate self-regulation, problem-solving skills, and adaptive coping at the individual level; parent–child involvement, monitoring, communication, and support at the family level; and school and neighborhood support systems at the community level [19-21].
Resilience has not been widely considered in research with PHIV or HEU youth in the US or other high-resource countries. Relatively few studies have prospectively evaluated and identified positive child, family, or psychosocial characteristics that support the emergence and persistence of emotional and behavioral resilience in HIV-affected children, in part due to limited validated and sensitive measures of protective factors [22]. This is also the case in low and middle-income countries (LMICs) that shoulder more of the global burden of pediatric HIV, with limitations in access to ART, fewer economic and educational assets, and high rates of stress. Stigma and orphanhood may also compromise psychological well being for children affected by HIV, whether PHIV children or HEU children residing in resource-restricted regions [23-25].
Despite additional risk among HIV-affected children in LMICs, resilience may be possible, particularly if family and community resources for positive development are available and accessible during childhood [26]. A recent evidence-informed family-based mental health prevention program evaluated in South Africa (VUKA) and Thailand (CHAMP+ Asia) fosters psychosocial well being via improved family communication and monitoring, development of problem-solving and peer negotiation skills, and support within and between families. This program has shown preliminary efficacy and acceptability in South African and Thai communities and may impact ongoing mental health and the likelihood of resilience among participants during adolescence [27-31].
To identify child, birth family and societal factors that modify risk and support emotional and behavioral resilience in children affected by HIV residing in LMIC settings, we examined longitudinal data on emotional and behavioral functioning in children enrolled in a cohort study conducted in Thailand and Cambodia; each of these countries have approximately 4000 children with PHIV under 15 years of age and many thousands more with in-utero HIV exposure [32,33]. Participants included PHIV children without advanced HIV disease at study entry, perinatally HEU (PHEU) children, and HUU children. Our goals were to examine the emotional–behavioral trajectories of PHIV, PHEU, and HUU children during school-age years; identify the presence and continuity of resilience, that is, emotional and behavioral well being among these groups of children; and determine the role of PHIVand psychosocial and cultural resources in predicting resilience in these populations.
Methods
Data were acquired from participants originally enrolled in the Pediatric Randomized Early versus Deferred Initiation in Cambodia and Thailand (PREDICT) study and a nested neurodevelopmental substudy [14,34]. PREDICT was a randomized open-label trial of early vs. deferred ART initiation, in children ages 1–12 years, with CD4+ percentages between 15 and 24 and no history of AIDS-defining illness or ART use. The neurodevelopmental substudy was conducted at seven hospitals in Thailand and two hospitals in Cambodia, where two age-matched and sex-matched comparison groups were also enrolled: PHEU children, recruited from clinics that provided treatment for the HIV-infected children or HIV-uninfected children born to HIV-infected mothers, and HUU children from general pediatric clinics. Group frequency matching was employed to facilitate age and sex similarity across the PHIV, PHEU, and HUU groups, based on data at the time of enrolment in the PREDICT neurodevelopmental substudy. Children were confirmed as HIV-uninfected by standard immunoassay for HIV Written informed consent was obtained from caregivers and written assent from the children at least 7 years. These studies were approved by local and National Thai and Cambodian Institutional Review Boards and relevant US ethics committees.
Procedures and measures
Emotional–behavioral functioning was assessed with the Child Behavior Checklist (CBCL; parent version) for school-age (6–18 years) children, which has been utilized to study children with chronic illness and children in multiple countries, including Thailand and Cambodia [35-39]. The English version of the CBCL was translated into Thai and Khmer and then back-translated into English to ensure accurate translation, using standard accepted procedures for assessment adaptation [40,41]. Caregivers completed the CBCL questionnaires in their primary language every 6 months (PHIV) or annually (PHEU, HUU). In those cases in which the person completing the questionnaire was not confident to read independently, the caregiver questionnaire was administered by the study nurse as a face-to-face interview.
Standardized scores based on age and sex were calculated from raw scores using US normative data [36,37]. Borderline and clinically significant T-scores are 60–63 and 64 and above, respectively, for each of the three summary scores: Internalizing (e.g., anxious/depressed, withdrawn/depressed, somatic complaints), Externalizing (e.g., aggressive behavior, rule-breaking behavior), and Total Problems (e.g., social problems, thought problems, attention problems). We defined resilience as having CBCL T-scores within the normal range (T-score <60) in Internalizing, Externalizing, or Total Problems at each study visit.
Statistical analyses
Statistical analyses were conducted with Stata 14 (StataCorp, College Station, Texas, USA). For each participant, we examined all available annual CBCL scores. For those with more than one CBCL assessment in the same year, we selected the first administered. Sociodemographic characteristics were compared by exposure group, using Chi-squared or Fisher’s exact tests as appropriate for categorical covariates, and analysis of variance or Kruskal–Wallis tests for normal and nonnormally distributed continuous covariates, respectively. Children living in orphanages at the time of assessment (N = 46; 40 PHIV children and six HEU children) were excluded from the analysis due to frequent changes among staff members who accompanied children and provided CBCL evaluations.
Analysis of emotional–behavioral trajectories
We used generalized estimating equations (GEE) to assess Internalizing, Externalizing, and Total Problem T-scores as children aged. GEE were run using an identity link and an exchangeable correlation matrix with comparisons made between the three HIV status groups; HUU children served as the reference cohort. Adjustments were made for covariates hypothesized to influence emotional–behavioral outcomes, including child age, sex, and nationality, person completing the report (parent, grandparent, or aunt or uncle; herein referred to as caregiver type), and sociodemographic characteristics, including highest caregiver educational achievement, and household income. Dynamic factors (e.g., caregiver type) were modeled as time-updated. We also separately assessed CBCL score changes with age among PHIV children. In these models, we adjusted for the sociodemographic characteristics previously described as well as HIV disease factors, including CD4+ nadir, peak HIV viral load, and time-updated HIV viral load categorized as detectable or undetectable (<50 copies/ml).
Analysis of emotional–behavioral resilience
Logistic models assessed the odds ratio (OR) [95% confidence interval (CI)] of emotional–behavioral resilience (e.g., no borderline or clinical T-scores), separately for Internalizing, Externalizing, and Total T-scores. In these models, we selected the first, last, and middle observation over the entire follow-up period, or first and last observation for children with only two visits. A multivariate model was developed, adjusting for covariates from the analyses described above and consistency of caregiver reporting. As a primary aim was to assess differences in resilience by HIV-exposure group, serostatus was forced into the model regardless of the univariate P value. HIV-specific characteristics modeled included nadir CD4+ cell count and peak HIV viral load during follow-up, and CD4+ cell count at first CBCL assessment.
Results
Participant enrollment and HIV characteristics
A total of 448 children (236 PHIV, 98 PHEU, and 114 HUU) were included in the analyses. The median [interquartile range (IQR)] number of CBCL assessments for participants was 5 (3–6) for PHIV children and 3 (2–3), for both PHEU and HUU participants (Table 1). Fifty-nine percentage of each group were female; approximately 45% were Cambodian. Type of caregivers completing the CBCL at the initial evaluation varied; PHIV children were more likely to have nonbirth parent respondents than PHEU and HUU children (P < 0.001). Caregivers of PHIV and PHEU children had less education than caregivers of HUU children (P < 0.001). An amount of 43, 48, and 59% of the PHIV, PHEU, and HUU households, respectively, had average or above average incomes (P < 0.001). In unadjusted analyses, children with PHIV were younger and had higher (worse) Internalizing, Externalizing, and Total Problem T-scores than PHEU and HUU children (P = 0.001). However, median scores for all groups at their initial CBCL assessment were below the borderline/clinical cutoff scores in Internalizing, Externalizing, and Total Problem Behaviors.
Table 1.
Baseline and follow-up characteristics of perinatally acquired HIV (PHIV), perinatally HIV-exposed but uninfected (PHEU) and HIV-unexposed uninfected (HUU) children.
| Characteristic | PHIV, N = 236 | PHEU, N = 98 | HUU, N = 114 | P |
|---|---|---|---|---|
| Age at PREDICT study entry (years) | 6.3 (4–8.4) | 7.5 (5.9–10) | 7.8 (6.4–10) | <0.001 |
| Age at first CBCL assessment (years) | 7.3 (6.4–9.4) | 7.8 (6.7–10.5) | 8 (7–10.3) | <0.001 |
| Female sex | 140 (59.3) | 57 (58.2) | 68 (59.7) | 0.97 |
| Median (IQR) age at first CBCL assessment | 7 (6–9) | 7 (6–10) | 8 (7–10) | 0.004 |
| Enrolled in school at first CBCL assessment | 190 (80.5) | 98 (100) | 113 (99.1) | <0.001 |
| Caregiver respondent on CBCL at first visit | <0.001 | |||
| Parent | 176 (74.6) | 94 (95.9) | 95 (83.3) | |
| Grandparent | 30 (12.7) | 1 (1) | 7 (6.1) | |
| Others | 30 (12.7) | 3 (3.1) | 12 (10.5) | |
| Consistent respondent | 205 (86.9) | 91 (92.9) | 104 (91.2) | 0.20 |
| Household income (mode) | <0.001 | |||
| ≤Average income | 133 (56.4) | 44 (44.9) | 34 (29.8) | |
| >Average income | 102 (43.2) | 47 (48) | 67 (58.8) | |
| Unknown | 1 (0.4) | 7 (7.1) | 13 (11.4) | |
| Highest educational attainment of primary caregiver | <0.001 | |||
| None/elementary | 140 (59.3) | 56 (57.1) | 34 (29.8) | |
| High school diploma | 92 (39) | 34 (34.7) | 50 (43.9) | |
| College/university | 3 (1.3) | 0 (0) | 5 (4.4) | |
| Unknown | 1 (0.4) | 8 (8.2) | 25 (21.9) | |
| Thai nationality | 126 (53.4) | 53 (54.1) | 63 (55.3) | 0.95 |
| Mean (SD) Internalizing T-score at first assessment | 55 (8.9) | 51.2 (9.1) | 52.1 (9.4) | 0.001 |
| Mean (SD) Externalizing T-score at first assessment | 55.2 (7.4) | 52.4 (7.9) | 51 (8.2) | <0.001 |
| Mean (SD) Total T-score at first assessment | 54.3 (8.1) | 50.6 (9.1) | 49.8 (9.3) | <0.001 |
| Median (IQR) PSI at first CBCL assessment (N = 235) | 81 (68–89) | 90 (81–100) | 94 (84–103) | <0.001 |
| Median (IQR) POI at first CBCL assessment | 80 (66–87) | 87 (80.5–96) | 93.5 (83–104) | <0.001 |
| Years from first to last assessment | 4 (3–5) | 2 (1–3) | 2 (1–3) | <0.001 |
| Median (IQR) number of evaluations in analysis | 5 (3–6) | 3 (2–3) | 3 (2–3) | <0.001 |
| HIV-specific characteristics | ||||
| Study entry | ||||
| N (%) HIV clinical staging | ||||
| CDC category N | 1 (0.4) | |||
| CDC category A | 157 (66.5) | |||
| CDC category B | 78 (33.1) | |||
| Median CD4+% | 20 (17.9–23.7) | |||
| Median CD4+ cell count | 649 (452–899) | |||
| Median log10 viral load (copies/ml) | 4.80 (4.40–5.00) | |||
| During follow-up | ||||
| N (%) who initiate ART | 204 (86.4) | |||
| Median CD4+% at ART initiation | 17 (13.8–21) | |||
| Median CD4+ cell count at ART initiation | 453 (307–697) | |||
| Median viral load at ART initiation | 4.80 (3.60–5.00) | |||
| Median duration of ART (years) | 5.4 (3.0–6.2) | |||
| Median CD4+% at the last visit | 29 (21.4–33.2) | |||
| Median CD4+ cell count at the last visit | 676 (473–915) | |||
| Median (IQR) log10 viral load at the last visit (copies/ml) | 40 (40–50) | |||
| N (%) viral load <50 copies/ml at the last visit | 170 (76) |
Characteristics are N (%) unless otherwise indicated. Values are median (IQR) or number (percentage) unless otherwise indicated. ART, antiretroviral therapy; CBCL, Child Behavior Checklist; CD4+%, CD4+-positive T-lymphocyte percentage; CDC, Centers for Disease Control and Prevention; HUU, HIV unexposed, uninfected; IQR, interquartile range; PHEU, perinatally HIV-exposed but uninfected; PHIV, perinatally acquired HIV; POI, Wechsler Perceptual Organization Index; PREDICT, Pediatric Randomized Early versus Deferred Initiation in Cambodia and Thailand; PSI, Wechsler Processing Speed Index.
Among PHIV children, all were ART-naïve at entry and most were in Centers for Disease Control and Prevention Classification of HIV disease Class A and B, with none in Class C [42]. The median CD4+ cell count was 649 cells/μl and median viral load was 4.8 log10 copies/ml. During the years of follow-up, 204 (86%) initiated ART. At the last visit, the median CD4+ cell count was 676 cells/μl and median viral load was 40 copies/ml, with 76% achieving viral suppression below 50 copies/ml.
Changes in Child Behavior Checklist Internalizing, Externalizing, and Total Problem T-scores by study group
In GEE models, CBCL T-scores were within the normal range at baseline for PHIV, PHEU, and HUU children, with no group differences. Internalizing, Externalizing, and Total Problem T-scores each showed a significant decrease with increased age (Table 2). The Internalizing T-score decreased on average by −0.71 (95% CI −0.89 to −0.54; P < 0.001) units with each year increase in age. In contrast to enrollment data, PHIV children had significantly lower (better) Internalizing T-scores than HUUs during follow-up; the mean difference over follow-up was −2.49 (95% CI −3.92 to −1.06; P < 0.001) units lower.
Table 2.
Coefficients from multivariate generalized estimating equations for change in Child Behavior Checklist Internalizing, Externalizing, and Total problem scores with age, by study group.
| Characteristic | Internalizing T-score |
Externalizing T-score |
Total Problem T-score |
|||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | P | Coefficient (95% CI) | P | Coefficient (95% CI) | P | |
| First CBCL test score | 0.56 (0.51–0.62) | <0.001 | 0.56 (0.5–0.61) | <0.001 | 0.58 (0.51–0.64) | <0.001 |
| Age (per year score increase) | −0.71 (−0.89 to −0.54) | <0.001 | −0.66 (−0.81 to −0.51) | <0.001 | −0.7 (−0.88 to −0.53) | <0.001 |
| Study group | 0.001 | 0.21 | 0.001 | |||
| PHIV | −2.49 (−3.92 to −1.06) | −0.84 (−2.08–0.39) | −2.29 (−3.72 to −0.86) | |||
| HEU | −0.72 (−2.43–0.99) | 0.05 (−1.42–1.52) | −0.15 (−1.85–1.55) | |||
| HUU | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Female vs. male sex | 0.09 (−0.94–1.13) | 0.86 | −0.85 (−1.74–0.05) | 0.06 | −0.36 (−1.38–0.66) | 0.49 |
| Thai vs. Cambodian | 1.72 (0.47–2.97) | 0.007 | −0.03 (−1.09–1.03) | 0.95 | 0.92 (−0.3–2.14) | 0.14 |
| CBCL respondent | 0.002 | 0.09 | 0.04 | |||
| Biological parent | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Grandparent | 2.18 (0.4–3.96) | 0.64 (−0.89–2.16) | 1.8 (0.01–3.58) | |||
| Other relative | 1.73 (0.09–3.37) | 1.57 (0.15–2.99) | 1.79 (0.13–3.46) | |||
| Average income or above vs. <average income | 0.58 (−0.61–1.77) | 0.34 | 0.87 (−0.15–1.89) | 0.1 | 0.7 (−0.47–1.87) | 0.24 |
| Caregiver education | 0.15 | 0.57 | 0.22 | |||
| None/elementary | 1 (ref) | 1 (ref) | 1 (ref) | |||
| High/vocational | 0.64 (−0.5–1.77) | 0.11 (−0.87–1.09) | 0.61 (−0.51–1.73) | |||
| University | −2.19 (−4.79–0.4) | −1.45 (−3.69–0.8) | −1.75 (−4.33–0.84) | |||
| Unknown | −0.21 (−4.3–3.88) | −0.57 (−4.08–2.95) | −1.3 (−5.35–2.76) | |||
CBCL, Child Behavior Checklist; CI, confidence interval; HEU, HIV-exposed but uninfected; HUU, HIV unexposed, uninfected; PHIV, perinatally acquired HIV.
Change in Internalizing T-scores over time did not differ between PHEU and HUU children [−0.72 (95% CI −2.43–0.99; P = 0.41)]. Across groups, children whose CBCL was completed by grandparents or an aunt or uncle had significantly higher Internalizing T-scores than those completed by birth parents [coefficients = 2.18 (95% CI 0.4–3.96; P = 0.02), and 1.73 (95% CI 0.09–3.37; P = 0.04)], respectively. Internalizing T-scores were significantly higher in Thai vs. Cambodian children [coefficient = 1.72 (95% CI 0.47–2.97; P = 0.007)]. There were no significant differences by sex, household income, and caregiver education.
We found no differences in Externalizing T-scores among PHIV HEU, and HUU groups during follow-up. Similar to Internalizing scores, Externalizing T-scores decreased significantly with increasing age [coefficient = −0.66 (95% CI −0.81 to −0.51; P < 0.001)]. There were no significant differences in the Externalizing scores between nationalities or income groups, or based on caregiver education and caregiver type.
The Total Problem T-score decreased on average by −0.70 (−0.88 to −0.53; P < 0.001) units with each year increase in age. Compared with HUU, Total Problem T-scores of PHIV children were 2.29 units (95% CI −3.72 to −0.86) lower (P = 0.001), whereas those of PHEU children were not significantly different. Children whose CBCL questionnaire was completed by grandparents or other relatives had Total Problem T-scores that were significantly higher than those reported by birth parents [coefficient = 1.80 (95% CI 0.01–3.58; P = 0.048) and 1.79 (95% CI 0.13–3.46; P = 0.03)], respectively. There were no significant differences by sex, nationality, household income, or caregiver education.
Perinatally acquired HIV youth only models
In the models incorporating HIV-specific covariates for PHIV children, Internalizing, Externalizing, and Total Problems T-scores decreased significantly with age at approximately the same rate as in the total cohort (Supplemental Table 1, http://links.lww.com/QAD/B454). There were no significant differences in any of the sociodemographic factors or among most HIV-specific covariates including timing of ART initiation, with the exception of undetectable viral load (viral load ≤50 copies/ml) at the time of any CBCL assessment. Among children with undetectable viral load, Internalizing and Total Problem T-scores were significantly lower than those with viral load more than 50 copies/ml.
Logistic models of sustained resilience
The proportion of PHIV PHEU, and HUU children who remained resilient throughout the investigation is shown in Fig. 1. Resilience in Internalizing behaviors was more likely among PHEU children (71%) than among PHIV (59%) and HUU (56%) groups. After adjustment for factors significant in a univariate model, the odds of resilience in PHEU children was 2.0 (95% CI 1.05–3.7; P = 0.03) times higher compared with HUU children with no differences in internalizing resilience between PHIV and HUU children (Table 3). Also associated with resilience in Internalizing scores in a multivariate model was Cambodian nationality; Thai children showed a significantly decreased odds of resilience compared with Cambodian children [OR 0.1 (95% CI 0.08–0.3); P < 0.001]. Among HIV-specific covariates in the PHIV group only, higher CD4+ cell count at first CBCL assessment was associated with higher odds of resilience on the Internalizing scale [OR 1.9 (95% CI 1.04–3.3); P = 0.04].
Fig. 1.
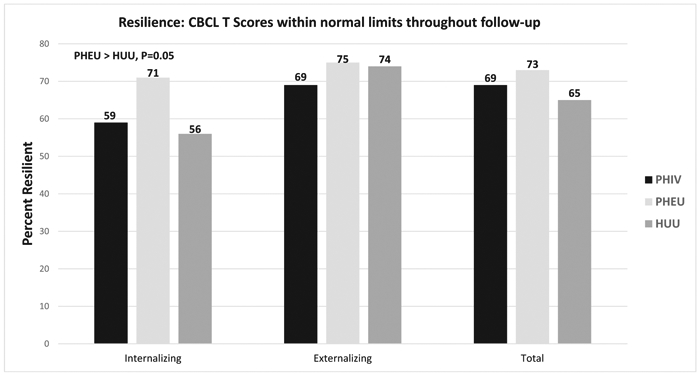
Emotional–behavioral resilience throughout follow-up.
Table 3.
Resilience: characteristics associated with resilience in Internalizing and Externalizing T-scores.
| Internalizing |
Externalizing |
|||||||
|---|---|---|---|---|---|---|---|---|
| Univariate |
Multivariate |
Univariate |
Multivariate |
|||||
| OR (95% CI) | P | aOR (95% CI) | P | OR (95% CI) | P | aOR (95% CI) | P | |
| Group | 0.04 | 0.04 | 0.45 | 0.47 | ||||
| PHIV | 1.1 (0.7–1.8) | 1.0 (0.6–1.7) | 0.8 (0.5–1.3) | 1.3 (0.8–2.3) | ||||
| HEU | 2.0 (1.1–3.5) | 2.0 (1.05–3.7) | 1.0 (0.6–1.9) | 1.3 (0.8–2.1) | ||||
| HUU | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Female | 1.1 (0.7–1.6) | 0.62 | 1.6 (1–2.4) | 0.03 | 1.6 (1.1–2.5) | 0.02 | ||
| Age at first CBCL assessment | 0.003 | 0.1 | 0.51 | 0.06 | ||||
| 6–8 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| 9–11 | 0.5 (0.3–0.7) | 0.7 (0.4–1.2) | 1.2 (0.7–2) | 0.8 (0.5–1.3) | ||||
| 12–14 | 1.1 (0.5–2.5) | 2.0 (0.84–4.8) | 1.5 (0.6–3.6) | 2.5 (1.01–6.3) | ||||
| Years follow-up | 0.9 (0.8–1) | 0.23 | 0.9 (0.8–1) | 0.23 | ||||
| N assessments | 0.08 | 0.47 | 0.12 | 0.47 | ||||
| Two | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Three | 0.7 (0.4–1.1) | 0.8 (0.4–1.3) | 0.7 (0.4–1.1) | 0.8 (0.5–1.3) | ||||
| Caregiver respondent to CBCL | 0.31 | 0.24 | ||||||
| Parent | 1 (ref) | 1 (ref) | ||||||
| Grandparent | 0.8 (0.4–1.6) | 1.5 (0.7–3.4) | ||||||
| Others | 0.6 (0.3–1.2) | 0.7 (0.3–1.2) | ||||||
| Consistent respondent | 1.8 (1–3.3) | 0.05 | 1.1 (0.5–2.4) | 0.97 | 1.7 (0.9–3.2) | 0.08 | 1.4 (0.7–2.7) | 0.32 |
| Household income | 0.03 | 0.97 | 0.3 | 0.04 | ||||
| ≤Average income | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| >Average income | 0.6 (0.4–0.95) | 1.0 (0.3–3.8) | 0.8 (0.5–1.2) | 1.8 (1.04–3.3) | ||||
| Highest educational attainment of primary caregiver | 0.38 | 0.38 | ||||||
| None/elementary | 1 (ref) | 1 (ref) | ||||||
| High school diploma | 0.8 (0.5–1.2) | 0.7 (0.4–1.1) | ||||||
| College/university | 1.6 (0.3–8.3) | 1.0 (0.2–5.2) | ||||||
| Thai (vs. Cambodian) | 0.3 (0.2–0.5) | <0.001 | 0.1 (0.08–0.3) | <0.001 | 0.6 (0.4–0.96) | 0.03 | 0.6 (0.4–1.0) | 0.05 |
| PSI<70 vs. ≥70 | 1.6 (0.8–3.3) | 0.2 | 0.8 (0.4–1.7) | 0.56 | ||||
| POI<70 vs. ≥70 | 1.7 (0.8–3.7) | 0.17 | 1.03 (0.5–2.2) | 0.94 | ||||
| HIV-specific covariates | ||||||||
| Deferred vs. early treatment arm | 0.98 (0.6–1.6) | 0.94 | 1.1 (0.6–1.9) | 0.79 | ||||
| Nadir CD4+ cell count ≥350 vs. <350 cells/μl | 1.08 (0.6–1.8) | 0.75 | 0.8 (0.5–1.3) | 0.32 | ||||
| CD4+ cell count ≥500 cell/μl vs. <500 cells/μl at first test | 1.9 (1.04–3.3) | 0.04 | 0.7 (0.4–1.4) | 0.36 | ||||
| Peak VL < 5 vs. ≥5 log10 copies/ml during follow-up | 1.2 (0.7–2.2) | 0.51 | 1.4 (0.8–2.8) | 0.22 | ||||
aOR, adjusted odds ratio; CBCL, Child Behavior Checklist; CD4+ cell count, CD4+-positive T-lymphocyte count; CD4+%, CD4+-positive T-lymphocyte percentage; CI, confidence interval; HEU, HIV-exposed but uninfected; HUU, HIV unexposed, uninfected; PHIV, perinatally acquired HIV; OR, odds ratio; POI, Wechsler Perceptual Organization Index; PSI, Wechsler Processing Speed Index; VL, viral load.
There were no differences in odds of resilience in Externalizing or Total Problem scores by study group in univariate or multivariate models (Table 3 and Supplemental Table 2, http://links.lww.com/QAD/B454). However, females [OR 1.6 (95% CI 1.1–2.5; P = 0.02)] and children in families with above average incomes [OR 1.8 (95% CI 1.04–3.3; P = 0.04)] had higher odds of resilience on the Externalizing scale; Thai children had significantly decreased odds of resilience on the Externalizing scale compared with Cambodian children [OR 0.6 (95% CI 0.4–1.0; P < 0.05)]. For Total Problem scores, children had higher odds of resilience if grandparents vs. birth-parents responded to the CBCL questionnaire [OR 6.8 (95% CI 2.5–18.5; P < 0.001)]. Thai children were less likely than Cambodian children to exhibit resilience in Total Problem scores [OR 0.2 (95% CI 0.1–0.3; P < 0.001)]. No HIV-specific covariates were associated with resilience in Externalizing or Total Problem scores.
Discussion
Resilience in children is conceptualized in varying ways across studies and populations but typically evokes positive adaptation and sustained well being, even in the presence of disadvantage or adversity [16,43,44]. In this longitudinal investigation, we examined the emotional and behavioral trajectories of PHIV and HEU children and an age-matched and sex-matched HUU group, in Thailand and Cambodia, as reported by children’s caregivers. We also identified the presence and sustainability of resilience among these children, defined as emotional and behavioral functioning that remained within the normal range throughout longitudinal follow-up. Overall, in our longitudinal examination of emotional and behavioral trajectories, we observed limited differences in emotional and behavioral functioning among children affected by HIV, whether PHIV or HEU children, and their HUU peers. We also observed similar rates of resilience in two of three emotional–behavioral domains, despite potential risks associated with intergenerational HIV infection, stigmatized chronic illness, and variable family and sociodemographic characteristics that frequently co-occur with HIV.
In our examination of the presence and continuity of resilience, positive outcomes in Externalizing and Total Problem scales were observed among the majority of children and at similar rates among PHIV, PHEU, and HUU children. However, resilience on the Internalizing scale was more common among PHEU children than among children with PHIV and twice as likely relative to the HUU group. These findings contrast with observations in several earlier US studies and studies in LMIC in which PHEU children display emotional risk, often at similar or even higher rates than children with PHIV [9,12,13,45].
Our findings indicate that potential challenges associated with in-utero HIV-exposure did not modify age-appropriate emotional development among PHEU children; children at risk can vary considerably in their adjustment across multiple domains and may demonstrate adequate coping despite stressful life experiences or emotional distress [46,47]. These children may also have positive resources not fully identified in this investigation that supported emotional well being and protected against development of internalizing symptoms. For example, the extended family network commonly observed in many Asian societies may be protective. Improved access to ART in Thailand and Cambodia and positive health outcomes among caregivers with HIV may support active parental engagement with their children, an important factor associated with reduced mental health difficulties among children [48]. It is also possible that caregivers of PHEU children acknowledge internalizing problems, should they develop, in a different manner or less readily than the CBCL normative group or their caregiver counterparts in this investigation.
Resilience in Externalizing behaviors was more likely endorsed in families with above average incomes. Although it is impossible to determine how distal factors such as family income precisely affected child behavioral functioning in this investigation, adequate family resources are crucial in protecting children from exposure to adverse life events in families affected by HIV, such as discrimination and parental physical and mental health challenges [49]. Prevention/intervention services, such as combinations of cash transfers and family supports that ameliorate financial burdens and increase children’s access to nutrition, school, and cognitive, social, and psychological support may increase the likelihood of children’s mental health resilience, regardless of HIV status [50,51].
Children with PHIV in this investigation, all of whom initiated ART prior to significant immune compromise, obtained higher CBCL scores at their initial evaluation, suggesting more emotional–behavioral problems than their PHEU and HUU peers. Importantly, however, scores of all groups were in the normal range. Of interest, follow-up evaluations revealed a favorable trajectory, that is, improvement in Internalizing and Total Problem T-scores with increasing age among PHIV children relative to the comparison group of HIV-unaffected peers. This observation may be related in part to an effect of ART treatment initiation and reduced symptom burden among PHIV children. In fact, we observed that children with undetectable viral load in our study had lower (better) Internalizing and Total Problem scores than children with detectable viral load as they aged. It is also possible that caregivers’ views of their PHIV children’s emotions and behaviors were tempered over time by children’s stable HIV health status, which could in turn affect children’s emotional–behavioral well being and child-parental adaptation [44]. Ongoing follow-up of our cohort will clarify the impact of compromised or healthy immune function and viral suppression, particularly when risk for nonadherence and associated complications accelerate during adolescence, as is often observed among youth affected by HIV [52-54].
In our analysis of emotional–behavioral trajectories, we also observed a relationship between caregiver type and CBCL ratings of Internalizing and Total behavioral problems during longitudinal follow-up; nonparental caregiver type was associated with higher (worse) ratings of internalizing and total behavioral problems. It is unclear whether these results are related to true differences in children’s emotional development in these contexts or to different expectations or observations of particular affect or behaviors in children as they age among nonparental vs. parental caregivers. Nonparental caregivers, who were more likely among PHIV and PHEU than HUU children, may signal earlier biological parent illness or death and the potential for emotional–behavioral effects, as has been reported in other studies [24,55]. These caregivers may struggle to meet additional and/or unexpected parenting demands and may experience limited financial and other support as they age, as well as psychological distress and stigma [56,57]. Such challenges would be expected to influence emotional well being, attachment relationships with children in their care, and perceptions of children’s emotions and behavior. Going forward, it is important to understand the interaction of caregiver relationship with the child to inform prevention/intervention services to support resilience.
An important limitation of this study was the reliance on parental/caregiver report of children’s emotions and behaviors, without incorporation of corroborating teacher or youth self reports. The higher number of CBCL assessments completed by caregivers of PHIV children during the study period may have attenuated or exaggerated their perceptions of significant symptoms as children aged, relative to the perceptions of caregivers of children who were HEU and HUU. Limited information was available regarding familial and community resources that have been shown to support resilience in earlier studies [27]. The exclusion of children orphaned by AIDS likely improved the overall prevalence rates for resilience in our cohort, as AIDS-orphaned children are known to experience negative mental health outcomes that worsen as they age [23]. In our investigation, Cambodian nationality was associated with higher rates of resilience across all behavioral domains. Although the CBCL measure has been used in earlier studies of emotional and behavioral functioning in both Thailand and Cambodia [58], the scale may perform differently in each setting, requiring further investigation of the psychometric properties in these contexts.
These limitations are balanced by several key strengths of our investigation, including the longitudinal design, inclusion of time-updated risk factors, careful quality assurance process, consideration of HIV biomarkers for PHIV children, inclusion of age and sex-matched comparison groups of Thai and Cambodian children, and a sample without prenatal illegal drug exposure as a major confounder. In US studies, perinatal exposure to substances in older PHIV and PHEU populations, as well as ongoing maternal substance use, are prevalent confounders in studies targeting the emotional and behavioral impact of perinatal HIV [3,9].
Going forward, the longitudinal design of our investigation, along with additional youth, family and social contextual information available in future study visits, will facilitate a more complete understanding of emotional and behavioral trajectories and resilience as youth age [59]. Our investigation thus far suggests moderately high rates of resilience in emotional and behavioral functioning among children affected by HIV in two LMICs who had access to ART. Further study is crucial to determine whether resilience persists or diminishes throughout adolescence and whether factors associated with resilience can be supported via research-informed and context-sensitive prevention services for families affected by HIV in Thailand and Cambodia.
Supplementary Material
Acknowledgements
We thank the children and families who participated in the PREDICT multisite study in Thailand and Cambodia and are grateful to the investigators, clinical centers, and staffs for their contributions.
The research was supported by the US National Institute of Allergy and Infectious Diseases (U19 AI053741) and the US National Institute of Mental Health (R01MH089722 and R01MH102151). Antiretroviral drugs for PREDICT were provided by ViiV Healthcare (AZT, 3TC), Boehringer Ingelheim (NVP), Merck (EFV), Abbott (RTV), and Roche (NFV).
Footnotes
The views expressed are those of the authors and should not be construed to represent the positions of the US Army or the Department of Defense or other institutions listed.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Brouwers P, DeCarli C, Civitello L, Moss H, Wolters P, Pizzo P. Correlations between computed tomographic brain scan abnormalities and neuropsychological function in children with symptomatic human immunodeficiency virus disease. Arch Neurol 1995;52:39–44. [DOI] [PubMed] [Google Scholar]
- 2.Donenberg GR, Pao M. Youths and HIV/AIDS: psychiatry’s role in a changing epidemic. J Am Acad Child Adolesc Psychiatry 2005;44:728–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Havens JF, Mellins CA. Psychiatric aspects of HIV/AIDS in Rutter’s Child and Adolescent Psychiatry, 5th edition. Rutter M, Bishop DVM, Pine DS, Scott S, Stevenson J, Taylor E. Thapar A (Eds.) Oxford: Blackwell; 2008. pp. 945–955. [Google Scholar]
- 4.Mintz M, Sharer L, Civitello J. Clinical and pathological features of HIV-1 encephalopathy in children and adolescents In: Gendelman HE, Everall IP, Fox HS, Grant I, Lipton S, Swindells S,editors. The neurology of AIDS New York: Oxford University Press; 2012. pp. 875–906. [Google Scholar]
- 5.Epstein LG, Gelbard HA. HIV-1 induced neuronal injury in the developing brain. J Leukoc Biol 1999;65:453–457. [DOI] [PubMed] [Google Scholar]
- 6.Crowell CS, Malee KM, Yogev R, Muller WJ. Neurologic disease in HIV-infected children and the impact of combination antiretroviral therapy. Rev Med Virol 2014; 24:316–331 . [DOI] [PubMed] [Google Scholar]
- 7.Kang E, Mellins CA, Dolezal C, Elkington KS, Abrams EJ. Disadvantaged neighborhood influences on depression and anxiety in youth with perinatally acquired human immunodeficiency virus: How life stressors matter. J Community Psychol 2011;39:956–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sohn AH, Hazra R. The changing epidemiology of the global pediatric HIV epidemic: keeping track of perinatally HIV-infected adolescents. J Int AIDS Soc 2013; 16:18555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc 2013;16:18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vreeman RC, Scanlon ML, McHenry MS, Nyandiko WM. The physical and psychological effects of HIV infection and its treatment on perinatally HIV-infected children. J Int AIDS Soc 2015;18 (Suppl 6):20258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith R, Huo Y, Tassiopoulos K, Rutstein R, Kapetanovic S, Mellins CA, et al. Mental health diagnoses, symptoms, and service uptake in US youth with PHIV exposure. AIDS Patient Care STDS 2019;33:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elkington KS, Robbins RN, Bauermeister JA, Abrams EJ, McKay M, Mellins CA. Mental health in youth infected with and affected by HIV: the role of caregiver HIV. J Pediatr Psychol 2011;36:360–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malee KM, Tassiopoulos K, Huo Y, Siberry G, Williams PL, Hazra R, et al. Mental health functioning among children and adolescents with perinatal HIV infection and perinatal HIV exposure. AIDS Care 2011;23:153344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Puthanakit T, Ananworanich J, Vonthanak S, Kosslaraksa P, Hansudewechaukul R, Van der Lugt J, et al. Cognitive function and neurodevelopmental outcomes in children older than 1 year of age randomized to early versus deferred antiretroviral therapy: the PREDICT neurodevelopmental study. Pediatr Infect Dis J 2013;32:501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherr L, Croome N, Parra Castaneda K, Bradshaw K. A systematic review of psychological functioning of children exposed to HIV: using evidence to plan for tomorrow’s HIV needs. AIDS Behav 2014;18:2059–2074. [DOI] [PubMed] [Google Scholar]
- 16.Rutter M Resilience as a dynamic concept. Dev Psychopathol 2012;24:335–344. [DOI] [PubMed] [Google Scholar]
- 17.Hilliard ME, McQuaid EL, Nabors L, Hood KK. Resilience in youth and families living with pediatric health and developmental conditions: introduction to the special issue on resilience. J Pediatr Psychol 2015;40:835–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Schoors M, Caes L, Verhofstadt LL, Goubert L, Alderfer MA. Systemic review: family resilience after pediatric cancer diagnosis. J Pediatr Psychol 2015;40:856–868. [DOI] [PubMed] [Google Scholar]
- 19.Luthar SS, Sawyer JA, Brown PJ. Conceptual issues in studies of resilience: past, present and future research. Ann N Y Acad Sci 2006;1094:105–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Catalano RF, Hawkins JD, Berglund L, Pollar JA, Arthur MS. Prevention science and positive youth development: competitive or cooperative frameworks? J Adolesc Health 2002; 31:230–239. [DOI] [PubMed] [Google Scholar]
- 21.Kia-Keating M, Dowdy E, Morgan ML, Noam GG. Protecting and promoting: an integrative conceptual model for healthy development of adolescents. J Adolesc Health 2011;48:220–228. [DOI] [PubMed] [Google Scholar]
- 22.Betancourt TS, Meyers Ohki SE, Charrow A, Hansen N. Annual research review: mental health and resilience in HIV/AIDS affected children – a review of the literature and recommendations for future research. J Child Psychol Psychatr 2013; 54:423–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. J Child Psychol Psychiatry 2012;53:363–370. [DOI] [PubMed] [Google Scholar]
- 24.Collishaw S, Gardner F, Aber JL, Cluver L. Predictors of mental health resilience in children who have been parentally bereaved by AIDS in Urban South Africa. J Abnorm Child Psychol 2016;44:719–730. [DOI] [PubMed] [Google Scholar]
- 25.Rongkavilit C, Wright K, Chen X, Naar-King S, Chuenyam T, Phanuphak P. HIV stigma, disclosure and psychosocial distress among Thai youth living with HIV. Int J STD AIDS 2010; 21:126–132. [DOI] [PubMed] [Google Scholar]
- 26.Sherr L, Yakubovich AR, Skeen S, Cluver LD, Hensels IS, Macedo A, Tomlinson M. How effective is help on the doorstep? A longitudinal evaluation of coummunit-based organisation support. PLoS One 2016;11:e0151305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhana A, Mellins CA, Small L, Nestadt DF, Leu CK, Petersen I, et al. Resilience in perinatal HIV+ adolescents in South Africa. AIDS Care 2016;52:49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhana A, Mellins CA, Petersen I, Alicea S, Myeza N, Hoist H, et al. The VUKA family program: piloting a family-based psychosocial intervention to promote health and mental health among HIV infected adolescents in South Africa. AIDS Care 2014;26:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mellins CA, Nestadt D, Bhana A, Petersen I, Abrams EJ, Alicea S, et al. Adapting evidence-based interventions to meet the needs of adolescents growing up with HIV in South Africa: the VUKA case example. Glob Soc Welf 2014;1:97–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pardo B, Saisaengjan C, Gopalan P, Ananworanich J, Lakhonpon S, Nestadt D, et al. Cultural adaptation of an evidence-informed psychosocial intervention to address the needs of PHIV+ youth in Thailand. Glob Soc Welf 2017; 4:209–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mellins CA. Strengthening resilience among adolescents/families. Abstract THSY0703. Paper presented in Mental Health & HIV: Supporting Communities and Turning Stress into Resilience. 22nd International AIDS Conference, Amsterdam Netherlands 23–27 July 2018. [Google Scholar]
- 32.UNICEF. The state of the world’s children 2017. 2018, https://data.unicef.org/wpcontent/uploads/2018/03/SOWC-2017-statistical-tables.pdf. [Accessed 4 February 2019].
- 33.UNAIDS. Thailand and Cambodia 2018. 2019, http://www.unaids.org/en/regionscountries/countries/thailand;http://www.unaids.org/en/regionscountries/countries/cambodia [Accessed 4 February 2019].
- 34.Puthanakit T, Saphonn V, Ananworanich J, Kosalaraksa P, Hansudewechakul R, Vibot U, et al. Early versus deferred antiretroviral therapy for children older than 1 year infected with HIV (PREDICT): a multicenter, randomized, open-label trial. Lancet Infect Dis 2012;12:933–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pinquart M, Shen Y. Behavior problems in children and adolescents with chronic physical illness: a meta-analysis. J Pediatr Psychol 2011;36:1003–1116. [DOI] [PubMed] [Google Scholar]
- 36.Achenbach TM. Manual for the Child Behavior Checklist 4–18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry;1991. [Google Scholar]
- 37.Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles. Burlington: University of Vermont Research Center for Children, Youth and Families; 2001. [Google Scholar]
- 38.Achenbach TM, Rescorla LA. Multicultural supplement to the manual for the ASEBA school-age forms & profiles. Burlington: University of Vermont Research Center for Children, Youth and Families; 2007. [Google Scholar]
- 39.Achenbach TM, Becker A, Dopfner M, Heiervang E, Roessner V, Steinhausen HC, et al. Multicultural assessment of child and adolescent psychopathology with ASEBA and SDQ instruments: research findings, applications, and future directions. J Child Psychol Psychiatry 2008; 49:251–275. [DOI] [PubMed] [Google Scholar]
- 40.Cysique LA, Jin H, Franklin DR Jr, Morgan EE, Shi C, Yu X, et al. Neurobehavioral effects of HIV-1 infection in China and the United States: a pilot study. J Int Neuropsychol Soc 2007; 13:781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Preciago J, Henry M. Linguistic barriers in health education and services In: Garcia JG, Zea MC,editors. Psychological interventions and research with Latino populations Boston: Allyn and Bacon;1997. pp. 235–254. [Google Scholar]
- 42.Centers for Disease Control. Revised classification system for human immunodeficiency virus infection in children less than 13 years of age. MMWR Morb Mortal Wkly Rep 1994; 43: 1–10. [Google Scholar]
- 43.Luthar SS, Brown PJ. Maximizing resilience through diverse levels of inquiry: prevailing paradigms, possibilities, and priorities for the future. Dev Psychopathol 2007;19:931–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sameroff AJ. A unified theory of development: a dialectic integration of nature and nurture. Child Dev 2010;81:6–22. [DOI] [PubMed] [Google Scholar]
- 45.Rochat T, Houle B, Stein A, Pearson RM, Bland RM. Prevalence and risk factors for child mental disorders in a population-based cohort of HIV-exposed and unexposed African children aged 7–11 years. Eur Child Adolesc Psychiatry 2018;27:1607–1620. [DOI] [PubMed] [Google Scholar]
- 46.Luthar SS. Annotation: methodological and conceptual issues in research on childhood resilience. J Child Psychol Psychiatry 1993;34:441–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luthar SS, Zigler E. Vulnerability and competence: a review of research on resilience in childhood. Am J Orthopsychiatry 1991;61:6–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. Regional Office for South-East Asia Mental health status of adolescents in South-East Asia: evidence for action. World Health Organization. Regional Office for South-East Asia; 2017, http://www.who.int/iris/handle/10665/254982. [Google Scholar]
- 49.Sherr L, Cluver LD, Betancourt TS, Kellerman SE, Richter LM, Desmond C. Evidence of impact: health, psychological and social effects of adult HIV on children. AIDS 2014;28:S251–S259. [DOI] [PubMed] [Google Scholar]
- 50.Cluver LD, Orkin FM, Meinck F, Boyes ME, Sherr L. Structural drivers and social protection: mechanisms of HIV risk and HIV prevention for South African adolescents. J Int AIDS Soc 2016; 19:20646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ssewamala FM, Bermudez LG, Neilands TB, Mellins CA, McKay MM, Garfinkel I, et al. Suubi4Her: a study protocol to examine the impact and cost associated with a combination intervention to prevent HIV risk behavior and improve mental health functioning among adolescent girls in Uganda. BMC Public Health 2018;18:693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mellins CA, Tassiopoulos K, Malee K, Moscicki AB, Patton D, Smith R, et al. Behavioral health risks in perinatally HIV-exposed youth: co-occurrence of sexual and drug use behavior, mental health problems and nonadherence to antiretroviral treatment. AIDS Patient Care STDS 2011;25:413–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kacanek D, Angelidou K, Williams PL, Chernoff M, Gadow KD, Nachman S. Psychiatric symptoms and antiretroviral nonadherence in US youth with perinatal HIV: a longitudinal study. AIDS 2015;29:1227–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nachman S, Chernoff M, Williams P, Hodge J, Heston J, Gadow KD. Human immunodeficiency virus severity, psychiatric symptoms, and functional outcomes in perinatally infected youth. Arch Pediatr Adolesc Med 2012;166:528–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mellins CA, Brackis-Cott E, Leu CS, Elkington KS, Dolezal C, Wiznia A, et al. Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. J Child Psychol Psychiatry 2009;50:1131–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Knodel J, Saengtienchai C, Im-Em W, Valandingham M. The impact of AIDS on parents and families in Thailand. Res Aging 2001;23:633. [Google Scholar]
- 57.Rotheram-Borus MJ, Swendeman D, Lee SJ, Li L, Amani B, Nartey M. Interventions for families affected by HIV. Transl Behav Med 2011;1:312–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rescorla L, Achenbach T, Ivanova MY, Dumenci L, Almqvist F, Bilenberg N, et al. Behavioral and emotional problems reported by parents of children ages 6–16 in 31 societies. J Emot Behav Disord 2007;15: 130–142. [Google Scholar]
- 59.Sameroff AJ, Rosenblum KL. Psychosocial constraints on the development of resilience. Ann N Y Acad Sci 2006;1094: 116–124. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


