Abstract
Background
Millions of Americans are injured each year, with 75% suffering orthopedic injuries. Those with orthopedic injury often experience post-injury symptoms, such as anxiety, that negatively influence long-term outcomes. The purpose of this systematic review is to evaluate 1) the prevalence of anxiety symptoms chronologically in relation to time of orthopedic injury, 2) the associations of anxiety symptoms with other symptoms in individuals with orthopedic injury, and 3) the associations between anxiety symptoms and functional performance and mental health outcomes in individuals with orthopedic injury.
Methods
The databases CINAHL, OVIDMEDLINE, OVIDPsychINFO, OVIDEmbase, Proquest, and Clinicaltrials.gov, were searched on June 25, 2020. Studies were selected for review if 1) participants were aged 16 years or older, 2) the prevalence of anxiety symptoms was listed, 3) anxiety symptoms were assessed using a validated instrument, 4) the study was published in English, and 5) over 50% of the participants suffered orthopedic injury to the appendicular skeleton or pelvic ring.
Results
Anxiety symptoms were present in 11.5% - 55.9% of individuals up to 10 years after orthopedic injury and often co-occurred with those of depression, pain, and posttraumatic stress disorder to negatively influence functional performance and mental health outcomes.
Conclusions
Anxiety symptoms post-orthopedic injury are highly prevalent and persistent. Anxiety symptoms are associated with other distressing symptoms and influence long-term outcomes. These findings highlight the need to screen for and treat anxiety symptoms following orthopedic injury and may help in designing future self-management interventions.
Keywords: Orthopedic Trauma, Orthopedic Injury, Orthopedics, Anxiety, Symptoms
Each year, millions of Americans are injured as a result of physical trauma, with falls from height motor vehicle collisions, and assaults being the most common mechanisms of injury (National Trauma Data Bank 2016, 2016; Web-Based Injury Statistics Query and Reporting System, 2018). Of those injured, nearly 75% suffer an orthopedic injury marked by damage to the skeleton and associated soft tissues as a result of physical trauma (Armstrong et al., 2016; National Trauma Registry 2012 Report: Hospitalizations for Major Injury in Canada, 2009-2010 Data, 2012). While treating the physical injury is of primary importance, the extra-orthopedic sequelae, including post-injury symptoms, must be addressed to promote recovery of the entire individual—both body and mind (Swann et al., 2017).
Post-orthopedic injury symptoms have received considerable attention of late. A recent review revealed that symptoms of depression and posttraumatic stress disorder (PTSD) were highly prevalent after injury (32.6% and 26.6% respectively) and site of injury and sex contributed (Muscatelli et al., 2017). Additionally, individuals with orthopedic injury report symptoms of anxiety more frequently than the U.S. population and for years after their injuries. Anxiety symptoms after orthopedic injury are associated with reduced functional performance and mental health outcomes, such as decreased rates of returning to work and lower health-related quality of life (Eldin et al., 2012; Giummarra et al., 2017; Statistics, 2018).
Symptoms rarely present in isolation, but often co-occur to exert a synergistic effect on long-term outcomes (Kim et al., 2005; Miaskowski, 2006; Miaskowski et al., 2007). Having symptoms of depression or PTSD after trauma tripled the odds of not returning to work (OR 3.2; 95% CI 2.46-4.16), and having symptoms of both were associated with an almost 6-fold increase in the odds of not returning to work compared to individuals with neither (OR 5.57; 95% CI 2.51-12.37) (Jaquet, 2002; Zatzick et al., 2008). Thus, there is a need to evaluate how anxiety symptoms co-occur with other post-injury symptoms to influence functional performance and mental health outcomes. The purpose of this systematic review is to evaluate 1) the prevalence of anxiety symptoms chronologically in relation to time of orthopedic injury, 2) the associations of anxiety symptoms with other symptoms in individuals with orthopedic injury, and 3) the associations between anxiety symptoms and functional performance and mental health outcomes in individuals with orthopedic injury.
Methods
Review Design and Search Strategy
This systematic review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). The databases CINAHL, OVIDMEDLINE, OVIDPsycINFO, OVIDEmbase, Proquest, and clinicaltrials.gov, were searched on Jun. 25, 2020. The search was completed using the Medical Subject Headings (MeSH) headings “fractures, bone,” “orthopedics,” “multiple trauma,” “anxiety,” and “anxiety disorders,” as well as the keywords “orthopedic trauma,” “anxious,” and various spellings of “orthopedics.” All subheadings of each MeSH term and the auto explode feature were used. Search results were further limited to journal articles published in English that included only adult humans. Reviews and qualitative studies were also removed from the search. The journal article limitation was not applied to the search of OVIDEmbase to capture conference proceedings. Finally, the reference lists of the included articles were searched for any potential articles. Table 1 provides the search strategy used for MEDLINE as an example.
Table 1.
Search Strategy for OVIDMEDLINE on 6/25/20
| Search Number | Searches | Results |
|---|---|---|
| 1 | Exp Fractures, Bone/ or exp orthopedics/ or orthopaedic trauma.mp. or orthopedic.mp. or orthopaedic.mp. or orthopedics.mp. or orthopaedics.mp. | 288925 |
| 2 | Exp Multiple Trauma/ | 12819 |
| 3 | 1 or 2 | 298125 |
| 4 | Exp Anxiety/ or Anxiety.mp. or exp Anxiety Disorders/ | 270144 |
| 5 | Anxious.mp. | 16555 |
| 6 | 4 or 5 | 274919 |
| 7 | 3 and 6 | 1042 |
| 8 | (3 and 6) not (exp animals/ not humans.sh.) | 1030 |
| 9 | Limit 8 to (English language and “all adult (19 plus years)” and journal article | 595 |
| 10 | Limit 9 to “reviews (best balance of sensitivity and specificity)” | 21 |
| 11 | 9 not 10 | 574 |
| 12 | Limit 11 to “qualitative (best balance of sensitivity and specificity)” | 136 |
| 13 | 11 not 12 | 438 |
Eligibility Criteria
The inclusion and exclusion criteria are shown in Digital Content 1. Articles were included if 1) participants were aged 16 years or older, 2) the prevalence of anxiety symptoms in the study population was listed, 3) the researchers used a validated instrument to assess for anxiety symptoms, 4) the study was published in English, and 5) the majority (over 50%), of participants, suffered an orthopedic injury to the appendicular skeleton or pelvic ring. Randomized controlled trials were excluded from the analysis. Studies with heterogenous orthopedic populations (i.e., arthroplasty, tumor, injury, etc.) were included if over half of the sample reported orthopedic injuries. Orthopedic injury was limited to fractures of the appendicular skeleton and pelvic ring because fractures beyond this (e.g., spine, skull, jaw) have distinctly different treatment and recovery.
Selection Process
Records were compiled and deduplicated from all databases using EndNote version X8.2. Two authors independently screened all titles and abstracts to identify potentially relevant studies. Two authors completed the full-text screening to determine the final studies selected for this review. Disagreements were resolved via discussion until consensus was reached, with a third author available for additional discussion as needed.
Quality Evaluation
The National Heart, Lung, and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used to assess the quality of the included studies (Study Quality Assessment Tools, 2019). Two authors independently assessed each article for quality. Disagreements were resolved with discussion until consensus was reached. The domains related to sample size calculation and blinding of personnel to exposure status were not considered in the assessment because of the prospective nature of cohort studies and because exposure status as a criterion for inclusion in this review.
Data Extraction
Two authors independently extracted the data with a standardized extraction form created using Excel version 2002. Author(s), publication title, year of publication, study design, care setting, location, the timeframe of assessment from orthopedic injury, inclusion and exclusion criteria, sample demographics, injury characteristics in the sample, the comparison group if applicable, the assessment tool and cutoff used, the prevalence of anxiety symptoms, the associations of anxiety symptoms with other symptoms, the associations of anxiety symptoms with functional performance and mental health outcomes, and general comments for each study were extracted. Disagreements in the extracted data were reconciled by checking the original reports and by discussion between the authors until consensus was reached.
Data Synthesis
Narrative synthesis of the data was conducted by initially grouping records according to the time of assessment of anxiety symptoms around the injury. Studies that included a time range for the assessment of anxiety symptoms in the study protocol were grouped by the earliest time of data collection. Once grouped, studies were compared regarding participant demographic and clinical characteristics, the assessment tool used, the assessment tool cutoff score, the overall prevalence rates of anxiety symptoms, the associations of anxiety symptoms with other symptoms, and the associations between anxiety symptoms and functional performance and mental health outcomes. The mean prevalence of anxiety symptoms at timepoints was computed using the total number of individuals with clinically significant anxiety symptoms as defined in each study at a given timepoint as the numerator and the total sample size at that timepoint as the denominator.
Results
The search resulted in 1,944 unique records. After screening titles and abstracts, the full text of 116 records were screened. One hundred four records were excluded in full-text screening, resulting in a final sample of 12 studies. Figure 1 illustrates the flow diagram of the selection process.
Figure 1.
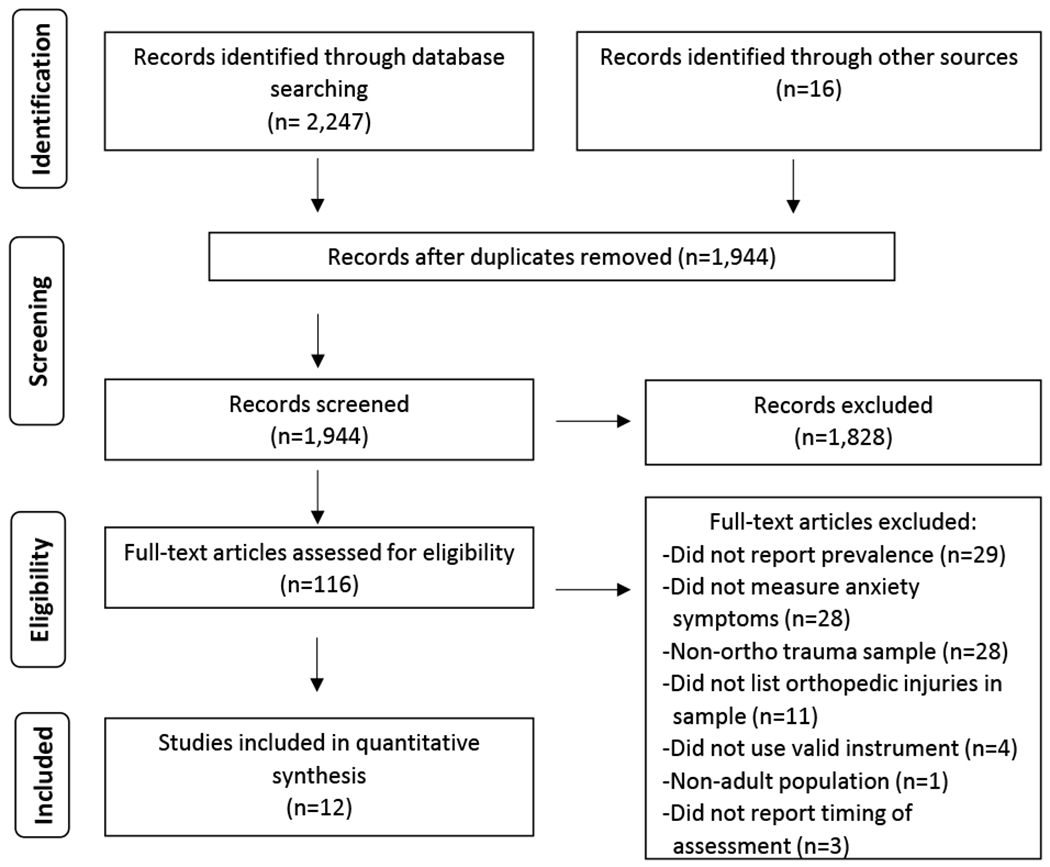
Flow Diagram of the Selection of the Included Studies in this Review
Study Populations
Two thousand ninety-two participants were included in all studies. The average or median age in each study ranged from 31-50.6 years (McCrabb et al., 2019; Snekkevik et al., 2003), and males represented between 52.8- 90.1% of each sample (Brouwers et al., 2018; Eldin et al., 2012). The included studies consisted of participants from 8 countries: Australia, Brazil, Egypt, Germany, Netherlands, Sweden, the United Kingdom, and the United States. Researchers from eight studies included participants with injury to upper or lower extremities; three examined only those with pelvic fractures (Brouwers et al., 2018; Gerbershagen et al., 2010; Harvey-Kelly et al., 2014), and one examined individuals with grade III open tibial shaft fractures who were treated with circular frames (Dickson et al., 2015). Anxiety symptoms were assessed using four different validated instruments: the 5-item European Quality of Life instrument (EQ-5D) (Niles et al., 2018), the 2-item questionnaire for Generalized Anxiety Disorder (GAD-2) (Kroenke et al., 2007), the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983), and the state subscale of the State-Trait Anxiety Inventory (STAI-S) (Julian, 2011). Collectively, anxiety symptoms were measured from pre-injury to over ten years after injury. Researchers in eight studies included cross-sectional data, while those in 4 used longitudinal data. Table 2 presents a summary of the included studies.
Table 2.
Summary of Included Records
| Author (Year), Record Number | Year | Country | Design | Sample Size | Male (%) | Mean Age (SD) |
|---|---|---|---|---|---|---|
| Brouwers, et al. (2018) | 2018 | NL | CS | 195 | 52.8 | 56.7 (-) |
| Dahm and Ponsford (2015) | 2015 | AU | CS | 96 | 53 | 43.9 (17.1) |
| de Moraes, et al. (2010) | 2010 | BRL | CS | 100 | 64 | 46.06 (19.66) |
| Dickson, et al. (2015) | 2015 | UK | Case Series | 22 | 86.4 | 35.5 (-) |
| Eldin, et al. (2012) | 2012 | EG | CS | 131 | 90.1 | 40.1 (11.6) |
| Gerbershagen, et al. (2010) | 2010 | GER | CS | 69 | 71 | 45.4 (17.7) |
| Giummarra, et al. (2017) | 2017 | AU | CS | 354 | 77.7 | 42.97 (13.19) |
| Harvey-Kelly, et al. (2014) | 2014 | UK | Cohort | 80 | 60 | 44.1 (12.9) |
| McCrabb, et al. (2019) | 2019 | AU | CS | 805 | 59.7 | 50.6 (17.7) |
| Ponsford, et al. (2008) | 2008 | AU | Cohort | 113 | 55.5 | 45.15 (18.8) |
| Snekkevik, et al. (2003) | 2003 | SE | Cohort | 26 | 69.2 | 31* |
| Vincent, et al. (2018) | 2018 | USA | Cohort | 101 | 59.4 | 43.5 (16.4) |
Note. AU = Australia; BRL = Brazil; EG = Egypt; GER = Germany; NL = The Netherlands; SE = Sweden; UK = United Kingdom; USA = United States of America; CS= Cross-sectional;
= median age reported;
(−) = not reported.
Study Quality
Nine records were determined to be of good quality and 3 of fair quality. The most common limitations were enrolling fewer than 50% of eligible patients (Dahm & Ponsford, 2015; Vincent et al., 2018), losing more than 20% of the sample to follow-up (Ponsford et al., 2008; Vincent et al., 2018), and not controlling for confounders (Dickson et al., 2015; Snekkevik et al., 2003). Table 3 presents the full details of the quality assessment.
Table 3.
Quality Assessment of Included Records Using the National Heart, Lung, and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies
| Author (Year), Record Number | Was the research question or objective clearly stated? | Was the study population clearly specified and defined? | Was the participation rate of eligible persons at least 50%? | Were all subjects selected from similar populations? | Was sample size justified? | Were exposures measured prior to outcomes? | Was timeframe sufficient between exposure and outcome? | Did study examine various levels of exposure related to outcome? |
|---|---|---|---|---|---|---|---|---|
| Brouwers, et al. (2018) | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Dahm and Ponsford (2015) | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| de Moraes, et al. (2010) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Dickson, et al. (2015) | Yes | Yes | Yes | Yes | No | Yes | Yes | No |
| Eldin, et al. (2012) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Gerbershagen, et al. (2010) | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Giummarra, et al. (2017) | Yes | Yes | Yes | Yes | No | Yes | Yes | No |
| Harvey-Kelly, et al. (2014) | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| McCrabb, et al. (2019) | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Ponsford, et al. (2008) | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Snekkevik, et al. (2003) | Yes | Yes | Yes | Yes | No | Yes | Yes | No |
| Vincent, et al. (2018) | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Author (Year), Record Number | Were exposure measures clearly defined, valid, and reliable? | Was exposure measured more than once? | Were outcomes clearly defined, valid, reliable? | Were assessors blinded to exposure status of patient? | Was loss to follow up less than 20%? | Were confounders measured and controlled for? | Quality Rating (Good, fair, poor) |
|---|---|---|---|---|---|---|---|
| Brouwers, et al. (2018) | Yes | No | Yes | No | Yes | Yes | Good |
| Dahm and Ponsford (2015) | Yes | No | Yes | No | NA | Yes | Good |
| de Moraes, et al. (2010) | Yes | No | Yes | No | NA | Yes | Good |
| Dickson, et al. (2015) | Yes | No | Yes | No | Yes | No | Fair |
| Eldin, et al. (2012) | Yes | No | Yes | No | NA | Yes | Good |
| Gerbershagen, et al. (2010) | Yes | No | Yes | No | NA | Yes | Good |
| Giummarra, et al. (2017) | Yes | No | Yes | No | NA | Yes | Good |
| Harvey-Kelly, et al. (2014) | Yes | No | Yes | No | NA | Yes | Good |
| McCrabb, et al. (2019) | Yes | No | Yes | No | NA | Yes | Good |
| Ponsford, et al. (2008) | Yes | No | Yes | No | No | Yes | Good |
| Snekkevik, et al. (2003) | Yes | No | Yes | No | Yes | No | Fair |
| Vincent, et al. (2018) | Yes | No | Yes | No | No | Yes | Fair |
Note. NA = not applicable, studies were cross-sectional.
Prevalence of Anxiety Symptoms Over Time
Researchers in one study assessed the pre-injury prevalence of anxiety symptoms. Participants who were one year removed from injury retrospectively completed the assessment tool, with 6.25% reporting moderate to severe anxiety symptoms before injury (Harvey-Kelly et al., 2014).
Researchers in four studies examined anxiety symptoms immediately following injury, finding that 11.5% - 55.7% of participants had clinically significant anxiety symptoms during their inpatient admissions with a mean prevalence of 19.7% (Snekkevik et al., 2003; Vincent et al., 2018). The prevalence of anxiety symptoms measured in a single sample at 2, 6, and 12 weeks post-injury was 55.9%, 31.2%, and 35.3%, respectively (Vincent et al., 2018). At six months, post-injury clinically significant anxiety symptoms ranged from 35.4% - 38.9%, with a mean prevalence of 36.8% (Brouwers et al., 2018; Eldin et al., 2012).
Researchers in five studies found that 13.6% - 40% of participants reported clinically significant anxiety symptoms one year after injury with a mean prevalence of 22% (Dickson et al., 2015; Giummarra et al., 2017; Harvey-Kelly et al., 2014; Ponsford et al., 2008). The study reporting the highest rate (40%) of anxiety symptoms one-year post-injury is also the study that reported a 6.25% prevalence of pre-injury anxiety symptoms (Harvey-Kelly et al., 2014).
Research with extended follow-up performed 19 months to ten years after injury found that 20% - 39% of participants had clinically significant anxiety symptoms (Dahm & Ponsford, 2015; Gerbershagen et al., 2010; Ponsford et al., 2008). The 39% prevalence of clinically significant anxiety symptoms 2 years after injury is an increase from the 35.5% found in the same sample one year after injury (Ponsford et al., 2008). The prevalence of anxiety symptoms over time is presented in Table 4.
Table 4.
Summary of Findings of Anxiety Symptoms by Timing of Assessment
| Author (Year), Record Number | Timing | Instrument | Cutoff | Prevalence (%) | Associations with Other Symptoms (correlation coefficient) | Associations with Functional and Mental Health Outcomes |
|---|---|---|---|---|---|---|
| Harvey-Kelly, et al. (2014) | Pre-injury | EQ-5D | 3L | 6.25 | NR | NR |
| de Moraes, et al. (2010) | Inpatient | HADS | ≥9 | 44 | NR | NR |
| McCrabb, et al. (2019) | Inpatient | GAD-2 | ≥3 | 12.4 | Depression (NR) | NR |
| Snekkevik, et al. (2003) | Inpatient | HADS | ≥11 | 11.5 | NR | Not associated with life satisfaction 1 year after OI |
| Vincent, et al. (2018) | Inpatient 2 weeks 6 weeks 12 weeks |
STAI-S | ≥40 | 55.7 55.9 31.2 35.3 |
Depression (NR) | Not associated with physical function |
| Brouwers, et al. (2018) | 6 months | EQ-5D | 3L | 35.4 | NR | NR |
| Eldin, et al. (2012) | 6 months | EQ-5D | 3L | 38.9 | NR | Negatively associated with health-related quality of life |
| Dickson, et al. (2015) | 1 year | EQ-5D | 3L | 13.6 | NR | NR |
| Harvey-Kelly , et al. (2014) | 1 year | EQ-5D | 3L | 40 | NR | NR |
| Giummarra, et al. (2017) | 1 year | HADS | ≥11 | 14.4 | Depression (r = 0.7, p < 0.00001) PTSD (r = 0.78, p < 0.00001)) |
Increased odds of not returning to work after OI (OR 4.77, 95% CI 2.46-9.23) |
| Ponsford, et al. (2008) | 1 year | HADS | NR | 35.5 | NR | NR |
| Snekkevik, et al. (2003) | 1 year | HADS | ≥11 | 19.2 | NR | NR |
| Gerbershagen , et al. (2010) | 19 months. | HADS | ≥11 | 21.7 | Chronic Pain (r = 0.51, p < 0.001) | NR |
| Ponsford, et al. (2008) | 2 years | HADS | NR | 39 | NR | Anxiety symptoms immediately after OI positively associated with physical function 2 years after OI Anxiety symptoms 2 years after OI negatively associated with overall mental health 2 years after OI Anxiety symptoms either immediately after OI or 2 years after OI unassociated with return to work |
| Dahm and Ponsford (2015) | 10 years | HADS | NR | 20 | NR | NR |
Note. EQ-5d = 5-item European Quality of Life instrument; GAD-2 = 2-item questionnaire for Generalized Anxiety Disorder; HADS = the Hospital Anxiety and Depression Scale; STAI = State-Trait Anxiety Inventory; 3L = 3 level assessment; (NR) = not reported.
Associations of Anxiety Symptoms with Other Symptoms
The severity of anxiety symptoms positively correlated with the severity of those of depression (r = 0.7, p < 0.00001), posttraumatic stress disorder (r = 0.78, p < 0.00001), and chronic pain (r = 0.51, p < 0.001) more than one year after injury (Gerbershagen et al., 2010; Giummarra et al., 2017). Further, 6.3% had clinically significant depressive and anxiety symptoms during their post-injury hospitalizations, while 83.4% of patients who had clinically significant depressive symptoms also had clinically significant anxiety symptoms 12 weeks after injury (McCrabb et al., 2019; Vincent et al., 2018). The associations of anxiety symptoms with other symptoms are presented in Table 4.
Associations of Anxiety Symptoms with Functional Performance and Mental Health Outcomes
Studies of the associations between anxiety symptoms and various outcomes after orthopedic injury produced mixed results. The severity of anxiety symptoms immediately after injury predicted physical function, measured with the 36-item Short-Form Health Survey (SF-36) administered two years post-injury (Ponsford et al., 2008). However, anxiety symptoms were not associated with physical function 12 weeks after injury as measured by the Patient-Reported Outcomes Information System (PROMIS) Physical Function instrument (Vincent et al., 2018).
The associations of anxiety symptoms on return to work were also mixed. In univariate analysis, moderate to severe anxiety symptoms one year after injury were associated with increased odds of not returning to work (4.77 OR, 95% CI 2.46-9.23) (Giummarra et al., 2017). However, the relationship was no longer significant when placed in a hierarchical logistic regression model that controlled for pain, depression, and PTSD (Giummarra et al., 2017). Anxiety symptoms two years after injury were not significantly associated with return to work (Ponsford et al., 2008).
Lastly, the severity of anxiety symptoms two years after injury was negatively associated with mental health as measured by the SF-36 (Ponsford et al., 2008). Anxiety symptom severity was also negatively associated with health-related quality of life (Eldin et al., 2012). The severity of an individual’s anxiety symptoms 6 months post-injury was associated with lower scores on the visual analog scale of the EQ-5D, a line marked 0-100 upon which a person indicates their total perceived health-related quality of life (Eldin et al., 2012; EQ-5D-3L, 2018). However, the severity of anxiety symptoms during the peri-traumatic period was not associated with life satisfaction one year after injury measured by the LiSat Checklist (Snekkevik et al., 2003). The association of anxiety symptoms with outcomes are presented in Table 4.
Discussion
Following orthopedic injury, anxiety symptoms are prevalent and can persist up to 10 years. The prevalence of anxiety after injury (11.5% - 55.9%) stands in stark contrast to the reported pre-injury prevalence of anxiety symptoms (6.25%), a rate that mirrors that of the general population (5.7%) (Harvey-Kelly et al., 2014; Statistics, 2018; Vincent et al., 2018). While the prevalence of anxiety symptoms is highest immediately after injury, 20% of individuals still experience anxiety symptoms up to 10 years later, which highlights how anxiety symptoms continue to present long after physical injuries heal (Dahm & Ponsford, 2015; Vincent et al., 2018). Anxiety symptoms are also long-lasting, as demonstrated by the three longitudinal studies in which 35.3% - 40% of participants continued to experience anxiety symptoms 3 months to 2 years after injury (Harvey-Kelly et al., 2014; Ponsford et al., 2008; Vincent et al., 2018).
In addition to being highly prevalent after injury, anxiety symptoms are negatively associated with long-term outcomes like physical and mental health, return to work, and overall health-related quality of life (Eldin et al., 2012; Giummarra et al., 2017; Ponsford et al., 2008). These quantitative findings reflect previous qualitative research in which injured individuals identified restoring physical function and emotional stability, as well as returning to work, as key to recovery (Aitken et al., 2016; Tutton et al., 2018). These findings suggest that anxiety symptoms that emerge soon after injury are not transient and should be assessed for and treated early in the post-injury period to minimize their effects on long-term outcomes and recovery.
The association of anxiety symptoms with those of depression, pain, and PTSD found in this review provide evidence for a symptom cluster following orthopedic injury. Symptom clusters are defined as two or more symptoms that occur together with a high degree of predictability (Kim et al., 2005). Support for clustered symptoms after injury is also seen in the findings of Giummarra et al. (2017), where univariate analysis revealed that symptoms of anxiety, depression, pain, and PTSD significantly increased the odds of not returning to work after orthopedic injury. However, when added to a hierarchical model that controlled for pain, the associations of symptoms of anxiety, depression, and PTSD with a return to work were no longer significant (Giummarra et al., 2017). The correlation of anxiety, depression, pain, and PTSD in this review may have created collinearity in the regression, which, because of the order in which the symptoms were entered into the model, only found pain to be significantly associated with the odds of failing to return to work.
The identification of symptom clusters post-injury may help improve outcomes because treating clustered symptoms with a single intervention may be more effective than treating each symptom separately (Kim et al., 2005; Miaskowski, 2006; Sidani, 2015). Symptoms do not occur in isolation and are likely to affect long-term outcomes synergistically. Assessing for clustered symptoms is recommended to ensure that post-injury experiences are assessed and managed in total (Miaskowski et al., 2007).
This review reveals directions for future research. More longitudinal studies are needed to assess the prevalence of anxiety symptoms over time. Studies are also needed to evaluate individual and clustered symptoms to identify those at highest risk for adverse long-term outcomes. These recommendations will aid in the design of comprehensive, precision health interventions that aim to improve outcomes beyond those targeted at individual symptoms.
Limitations
The main limitation of this review is the inability to perform a meta-analysis. Researchers in the included studies used four different validated instruments to assess for anxiety symptoms and used multiple cutoff scores or failed to report the cutoff score utilized when administering the HADS. The use of multiple instruments and multiple cutoff scores within a single instrument preclude comparison of findings across studies and limit the generalizability of findings (Redeker et al., 2015). The use of multiple instruments and cutoff scores complicating symptom research is not isolated to the orthopedic trauma population (Redeker et al., 2015). The use of common data elements in symptom research is recommended, with PROMIS instruments recommended in particular (Moore et al., 2016).
Several timepoints examined in this review are represented by single studies with relatively small sample sizes. This limited representation makes it difficult to evaluate the nature of anxiety symptoms at certain timepoints fully and limits the strength of the conclusions. Finally, while the GAD-2, HADS, and STAI-S are reliable and valid at detecting anxiety symptoms, the EQ-5D is flawed. The EQ-5D asks the participant if they have problems with anxiety or depression simultaneously (Brooks, 1996). Differentiating symptoms of anxiety from depression using the EQ-5D is impossible. Anxiety was not separately assessed in the included studies in which the EQ-5D was used.
Conclusion
Anxiety symptoms are highly prevalent and chronic following orthopedic injury and may present comorbidly with other symptoms to affect long-term outcomes after injury. Clinicians should assess for and treat the symptom cluster of anxiety, depression, pain, and PTSD following orthopedic injury.
Supplementary Material
Key Points.
Anxiety symptoms are prevalent following orthopedic injury and can persist up to 10 years post-injury.
The association of anxiety with depression, pain, and PTSD is evidence of a symptom cluster that can follow orthopedic injury.
Treating clustered symptoms with a single intervention may be more effective than treating each symptom separately.
Acknowledgments
Sources of Support
Mr. Breazeale’s enrollment in the PhD program at Yale Graduate School of Arts and Sciences and Yale School of Nursing is funded in part by the Robert Wood Johnson Foundation Future of Nursing Scholars Program.
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number F31NR018996. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This publication was made possible by CTSA Grant Number TL1TR001864 from the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Footnotes
List of Supplemental Digital Content
Table, Supplemental Digital Content 1, Inclusion and Exclusion Criteria for Review of Full-Text Reports.
Contributor Information
Stephen Breazeale, Yale University.
Samantha Conley, Yale University.
Edward Gaiser, Yale New Haven Hospital.
Nancy S. Redeker, Yale University.
References
- Aitken LM, Chaboyer W, Jeffrey C, Martin B, Whitty JA, Schuetz M, & Richmond TS (2016). Indicators of injury recovery identified by patients, family members and clinicians. Injury, 47(12), 2655–2663. 10.1016/j.injury.2016.10.006 [DOI] [PubMed] [Google Scholar]
- Armstrong AD, Hubbard MC, American Academy of Orthopaedic Surgeons, & American Academy of Pediatrics (2016). Essentials of Musculoskeletal Care (5th ed.) American Academy of Orthopaedic Surgeons. [Google Scholar]
- Brooks R (1996). EuroQol: the current state of play. Health Policy, 37(1), 53–72. https://www.ncbi.nlm.nih.gov/pubmed/10158943 [DOI] [PubMed] [Google Scholar]
- Brouwers L, Lansink KWW, & de Jongh MAC (2018). Quality of life after pelvic ring fractures: A cross-sectional study. Injury, 49(4), 812–818. 10.1016/j.injury.2018.03.012 [DOI] [PubMed] [Google Scholar]
- Dahm J, & Ponsford J (2015). Comparison of long-term outcomes following traumatic injury: What is the unique experience for those with brain injury compared with orthopaedic injury? Injury, 46(1), 142–149. [DOI] [PubMed] [Google Scholar]
- Dickson DR, Moulder E, Hadland Y, Giannoudis PV, & Sharma HK (2015). Grade 3 open tibial shaft fractures treated with a circular frame, functional outcome and systematic review of literature. Injury, 46(4), 751–758. 10.1016/j.injury.2015.01.025 [DOI] [PubMed] [Google Scholar]
- Eldin WS, Hirshon JM, Smith GS, Mohamad Kamal AA, Abou-El-Fetouh A, & El-Setouhy M (2012). Health-related quality of life after serious occupational injury in Egyptian workers: A cross-sectional study. BMJ Open, 2 (6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- EQ-5D-3L. (2018). Retrieved December 4 from https://euroqol.org/wp-content/uploads/2016/10/Sample_UK_English_EQ-5D-3L_Paper_Self_complete_v1.0_ID_23963.pdf
- Gerbershagen HJ, Dagtekin O, Isenberg J, Martens N, Ozgur E, Krep H, Sabatowski R, & Petzke F (2010). Chronic pain and disability after pelvic and acetabular fractures-assessment with the mainz pain staging system. Journal of Trauma - Injury, Infection and Critical Care, 69(1), 128–136. [DOI] [PubMed] [Google Scholar]
- Giummarra MJ, Cameron PA, Ponsford J, Ioannou L, Gibson SJ, Jennings PA, & Georgiou-Karistianis N (2017). Return to work after traumatic injury: Increased work-related disability in injured persons receiving financial compensation is mediated by perceived injustice. Journal of Occupational Rehabilitation, 27(2), 173–185. [DOI] [PubMed] [Google Scholar]
- Harvey-Kelly KF, Kanakaris NK, Obakponovwe O, West RM, & Giannoudis PV (2014). Quality of life and sexual function after traumatic pelvic fracture. Journal of Orthopaedic Trauma, 28(1), 28–35. [DOI] [PubMed] [Google Scholar]
- Jaquet JB (2002). Early psychological stress after forearm nerve injuries: A predictor for long-term functional outcome and return to productivity. Annals of Plastic Surgery, 49(1), 82–90. 10.1097/00000637-200207000-00013 [DOI] [PubMed] [Google Scholar]
- Julian LJ (2011, 2011). Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care & Research (2010), 63(s11), S467–S472. 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, McGuire DB, Tulman L, & Barsevick AM (2005). Symptom clusters: Concept analysis and clinical implications for cancer nursing. Cancer Nursing, 28(4), 270–284. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, Williams J, Monahan P, & Lowe B (2007). The 2-item Generalized Anxiety Disorder scale had high sensitivity and specificity for detecting GAD in primary care. Evidence-Based Medicine, 12(5), 149 10.1136/ebm.12.5.149 [DOI] [PubMed] [Google Scholar]
- McCrabb S, Baker AL, Attia J, Balogh ZJ, Lott N, Palazzi K, Naylor J, Harris IA, Doran CM, George J, Wolfenden L, Skelton E, & Bonevski B (2019). Comorbid tobacco and other substance use and symptoms of anxiety and depression among hospitalised orthopaedic trauma patients [Article]. BMC Psychiatry, 19(1), Article 28. 10.1186/s12888-019-2021-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miaskowski C (2006). Symptom clusters: Establishing the link between clinical practice and symptom management research. Supportive Care in Cancer, 14(8), 792–794. 10.1007/s00520-006-0038-5 [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Aouizerat BE, Dodd M, & Cooper B (2007). Conceptual issues in symptom clusters research and their implications for quality-of-life assessment in patients with cancer. Journal of the National Cancer Institute. Monographs(37), 39–46. 10.1093/jncimonographs/lgm003 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology, 62(10), 1006–1012. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Moore SM, Schiffman R, Waldrop-Valverde D, Redeker NS, McCloskey DJ, Kim MT, Heitkemper MM, Guthrie BJ, Dorsey SG, Docherty SL, Barton D, Bailey DE Jr., Austin JK, & Grady P (2016). Recommendations of common data elements to advance the science of self-management of chronic conditions. Journal of Nursing Scholarship, 48(5), 437–447. 10.1111/jnu.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscatelli S, Spurr H, O’Hara NN, O’Hara LM, Sprague SA, & Slobogean GP (2017). Prevalence of depression and posttraumatic stress disorder after acute orthopaedic trauma: A systematic review and meta-analysis. Journal of Orthopaedic Trauma, 31(1), 47–55. 10.1097/BOT.0000000000000664 [DOI] [PubMed] [Google Scholar]
- National Trauma Data Bank 2016. (2016). https://www.facs.org/-/media/files/quality-programs/trauma/ntdb/ntdb-annual-report-2016.ashx?la=en
- National Trauma Registry 2012 Report: Hospitalizations for Major Injury in Canada, 2009-2010 Data. (2012). C. I. f. H. Information; https://secure.cihi.ca/estore/productSeries.htm?pc=PCC46 [Google Scholar]
- Niles AN, Smirnova M, Lin J, & O’Donovan A (2018). Gender differences in longitudinal relationships between depression and anxiety symptoms and inflammation in the health and retirement study. Psychoneuroendocrinology, 95, 149–157. 10.1016/j.psyneuen.2018.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponsford J, Hill B, Karamitsios M, & Bahar-Fuchs A (2008). Factors influencing outcome after orthopedic trauma. Journal of Trauma-Injury Infection & Critical Care, 64(4), 1001–1009. 10.1097/TA.0b013e31809fec16 [DOI] [PubMed] [Google Scholar]
- Redeker NS, Anderson R, Bakken S, Corwin E, Docherty S, Dorsey SG, Heitkemper M, McCloskey DJ, Moore S, Pullen C, Rapkin B, Schiffman R, Waldrop-Valverde D, & Grady P. (2015). Advancing symptom science through use of common data elements. Journal of Nursing Scholarship, 47(5), 379–388. 10.1111/jnu.12155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidani S (2015). Health intervention research: Understanding research design & methods. SAGE Publications Ltd. [Google Scholar]
- Snekkevik H, Anke AGW, Stanghelle JK, & Fugl-Meyer AR (2003). Is sense of coherence stable after multiple trauma? Clinical Rehabilitation, 17(4), 443–453. 10.1191/0269215503cr630oa [DOI] [PubMed] [Google Scholar]
- Statistics. (2018). National Institute of Mental Health. https://www.nimh.nih.gov/health/statistics/index.shtml
- Study Quality Assessment Tools. (2019). National Heart, Lung, and Blood Institute; Retrieved August, 28 from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Google Scholar]
- Swann MC, Batty M, Hu G, Mitchell T, Box H, & Starr A (2017). Sleep disturbance in orthopaedic trauma patients. Journal of Orthopaedic Trauma, 32(10), 500–504. [DOI] [PubMed] [Google Scholar]
- Tutton E, Achten J, Lamb SE, Willett K, & Costa ML (2018). A qualitative study of patient experience of an open fracture of the lower limb during acute care. The Bone and Joint Journal, 100-B(4), 522–526. 10.1302/0301-620X.100B4.BJJ-2017-0891.R1 [DOI] [PubMed] [Google Scholar]
- Vincent HK, Hagen JE, Zdziarski-Horodyski LA, Patrick M, Sadasivan KK, Guenther R, Vasilopoulos T, Sharififar S, & Horodyski M (2018). Patient-reported outcomes measurement information system outcome measures and mental health in orthopaedic trauma patients during early recovery. Journal of Orthopaedic Trauma, 32(9), 467–473. [DOI] [PubMed] [Google Scholar]
- Web-Based Injury Statistics Query and Reporting System. (2018). Centers for Disease Control and Prevention; Retrieved Nov. 20 from https://www.cdc.gov/injury/wisqars/index.html [Google Scholar]
- Zatzick D, Jurkovich GJ, Rivara FP, Wang J, Fan MY, Joesch J, & Mackenzie E (2008). A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Annals of Surgery, 248(3), 429–437. 10.1097/SLA.0b013e318185a6b8 [DOI] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


