Abstract
Background
Although the direct toll of COVID-19 in the United States has been substantial, concerns have also arisen about the indirect effects of the pandemic. Hospitalizations for acute cardiovascular conditions have declined, raising concern that patients may be avoiding hospitals because of fear of contracting severe acute respiratory syndrome- coronavirus-2 (SARS-CoV-2). Other factors, including strain on health care systems, may also have had an indirect toll.
Objectives
This investigation aimed to evaluate whether population-level deaths due to cardiovascular causes increased during the COVID-19 pandemic.
Methods
The authors conducted an observational cohort study using data from the National Center for Health Statistics to evaluate the rate of deaths due to cardiovascular causes after the onset of the pandemic in the United States, from March 18, 2020, to June 2, 2020, relative to the period immediately preceding the pandemic (January 1, 2020 to March 17, 2020). Changes in deaths were compared with the same periods in the previous year.
Results
There were 397,042 cardiovascular deaths from January 1, 2020, to June 2, 2020. Deaths caused by ischemic heart disease increased nationally after the onset of the pandemic in 2020, compared with changes over the same period in 2019 (ratio of the relative change in deaths per 100,000 in 2020 vs. 2019: 1.11, 95% confidence interval: 1.04 to 1.18). An increase was also observed for deaths caused by hypertensive disease (1.17, 95% confidence interval: 1.09 to 1.26), but not for heart failure, cerebrovascular disease, or other diseases of the circulatory system. New York City experienced a large relative increase in deaths caused by ischemic heart disease (2.39, 95% confidence interval: 1.39 to 4.09) and hypertensive diseases (2.64, 95% confidence interval: 1.52 to 4.56) during the pandemic. More modest increases in deaths caused by these conditions occurred in the remainder of New York State, New Jersey, Michigan, and Illinois but not in Massachusetts or Louisiana.
Conclusions
There was an increase in deaths caused by ischemic heart disease and hypertensive diseases in some regions of the United States during the initial phase of the COVID-19 pandemic. These findings suggest that the pandemic may have had an indirect toll on patients with cardiovascular disease.
Key Words: cardiovascular disease, coronavirus disease 2019, COVID-19 pandemic, mortality
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2
Central Illustration
Although the direct toll of the novel coronavirus disease 2019 (COVID-19) in the United States has been substantial (1), concerns have also arisen about the indirect effects of the pandemic on higher-risk patients with chronic medical conditions such as cardiovascular disease. Recent reports suggest large increases in mortality during the pandemic that cannot be explained by COVID-19 deaths alone (2, 3, 4). At the same time, hospitalizations for acute cardiovascular conditions, including myocardial infarction, heart failure, and stroke, have declined precipitously (5, 6, 7). These patterns have raised concern that patients may be avoiding hospitals because of fear of contracting severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) and that some may have died of cardiovascular conditions without seeking medical care (8,9). Other factors, including the deferral of outpatient cardiovascular visits, diagnostic testing, and semi-elective procedures, as well as greater strain on health care systems, may also have unintended effects on higher-risk patients.
Evaluating if population-level deaths due to cardiovascular causes have increased over this period could provide important insights on whether the pandemic has had an indirect toll and may also inform public health responses and policy efforts in states that are currently experiencing a surge in COVID-19 cases. Therefore, in this study, we aimed to answer 2 questions: First, did population-level deaths due to cardiovascular causes (ischemic heart disease, heart failure, hypertensive diseases, cerebrovascular disease, other diseases of circulatory system) change in the United States after the onset of the COVID-19 pandemic relative to the same period in the year before? Second, were changes more pronounced in states that experienced the initial surge of COVID-19 cases in the United States?
Methods
Data
Weekly death data were obtained from the National Center for Health Statistics (Centers for Disease Control and Prevention) for January through June 2020, as well as for the same weeks during the preceding year (2019) (10). International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes were then used to identify underlying causes of death caused by ischemic heart disease (I20–I25), heart failure (I50), hypertensive diseases (I10–I15), cerebrovascular disease (I60–I69), and other disease of the circulatory system (I00–I09, I26–I49, I51, I52, I70–I99) (11). As we sought to examine the potential indirect effect of the pandemic, deaths with an underlying cause of COVID-19 were excluded from the analysis (10). Data on state populations from the 2018 American Community Survey files were used to calculate mortality rates.
Statistical analysis
Our initial analysis included all states (and District of Columbia) in the United States. We then focused on areas that experienced early surges in COVID-19 cases: New York (excluding New York City), New York City, New Jersey, Massachusetts, Louisiana, Michigan, and Illinois. We considered the “pre-pandemic” period to be the first 11 weeks in 2020 (January 1 to March 17), and the “pandemic” period to be the subsequent 11 weeks of 2020 (March 18 to June 2). The start of the pandemic period was determined based on when states began to experience rapid rises in reported cases of COVID-19 and issued stay-at-home orders (over the third and fourth weeks of March). We constructed corresponding periods of an identical duration from January to June in 2019 to serve as a historical control.
For each state/city, we calculated weekly death rates (per 100,000 population) for each cardiovascular cause of death for January through June 2020 (pandemic year), as well as for the corresponding weeks in 2019 (nonpandemic “control” year). Next, we fit a Poisson regression model to compare death rates during the 11-week pandemic period to the 11-week pre-pandemic period in 2020. We used a similar approach to compare mortality rates during the same 11-week periods in 2019. We then calculated the ratio of the relative change in death rates in 2020 versus the relative change in death rates 2019. This approach allowed us to estimate the increase in deaths due to cardiovascular causes that were attributable to the pandemic, compared with a historical baseline, while accounting for seasonal variation in deaths. The 95% confidence interval (CI) for all values was constructed with the dispersion parameter estimated by deviance.
Statistical analyses were performed using SAS 9.4 (SAS Inc., Cary, North Carolina) and figures were created using R version 4.0.2 (R Foundation, Vienna, Austria). Institutional review board approval from Beth Israel Deaconess Medical Center was not sought because of the use of publicly available deidentified data, per usual institutional policy.
Results
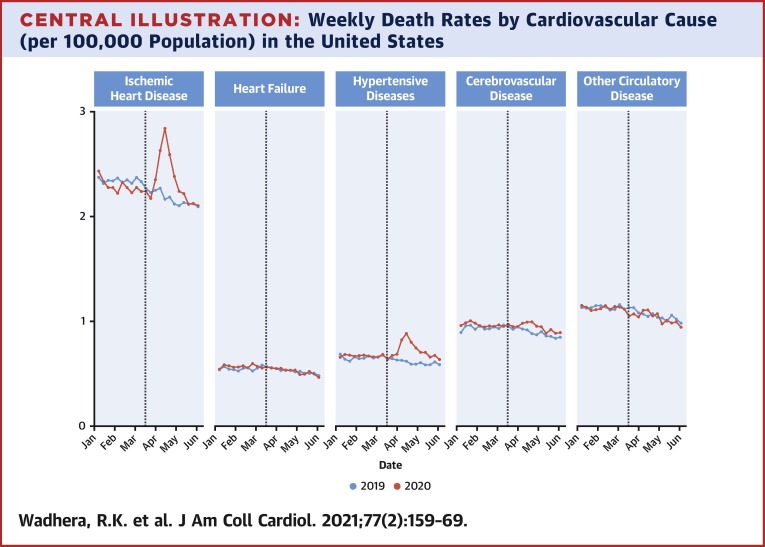
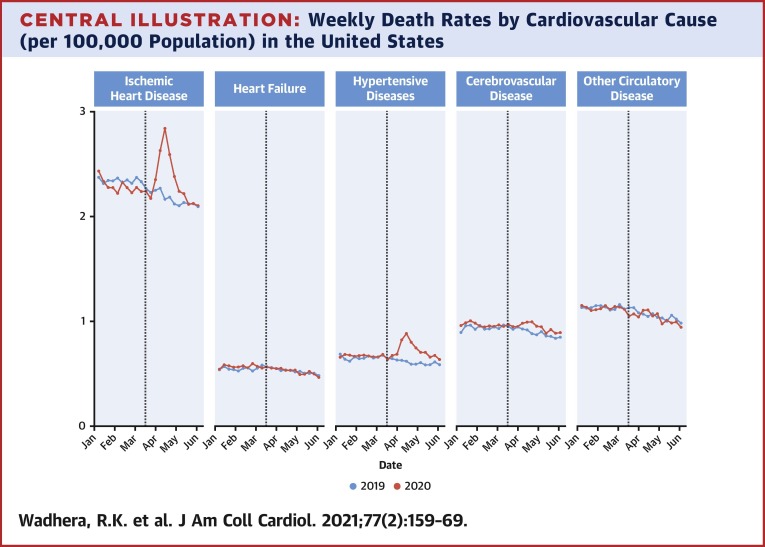
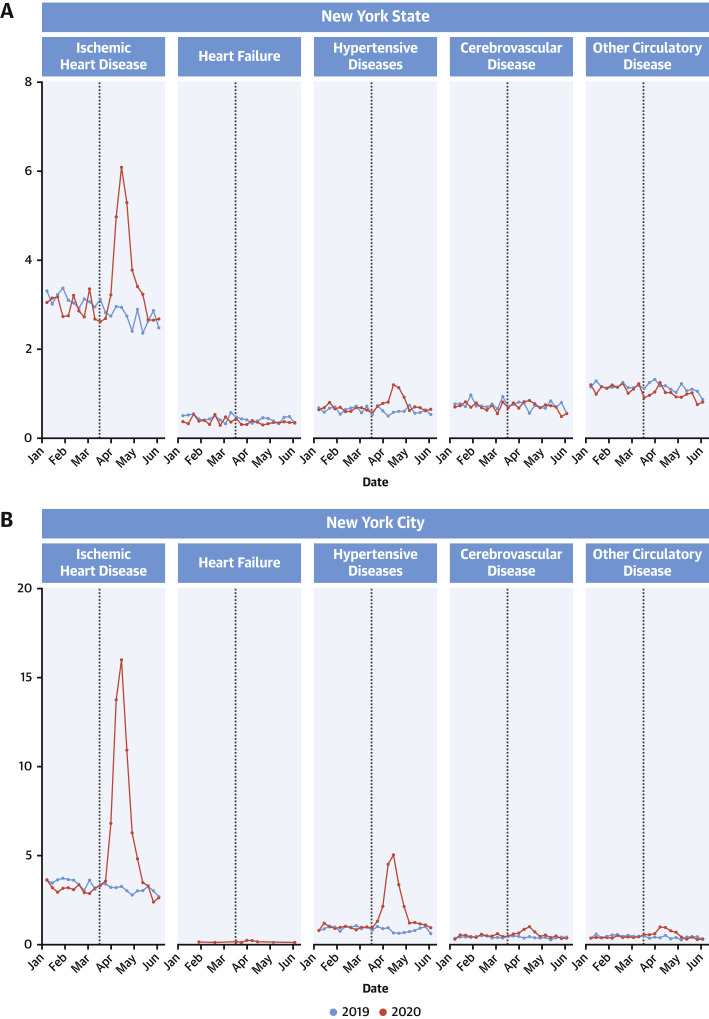
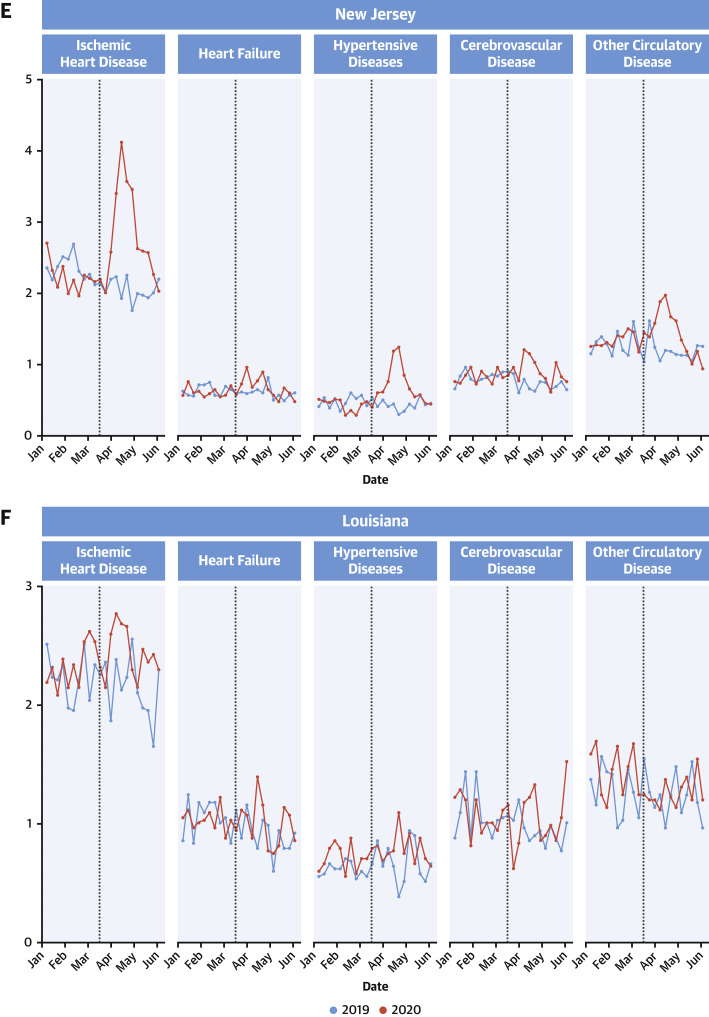
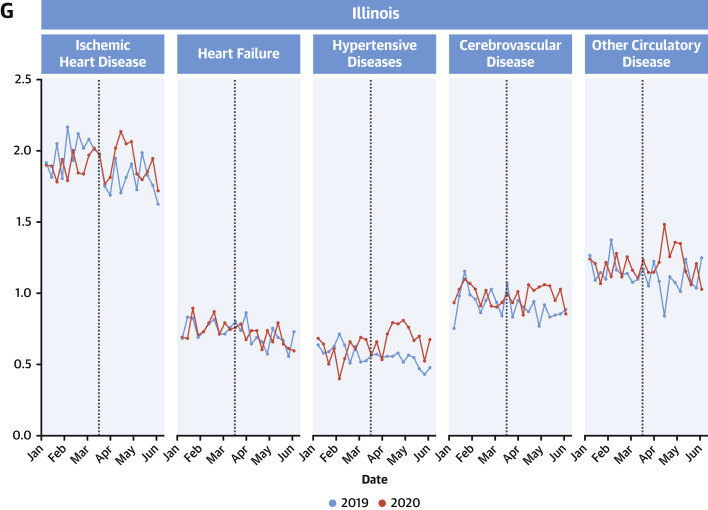
In the United States, there was a total of 397,042 deaths caused by ischemic heart disease, heart failure, hypertensive disease, cerebrovascular disease, and other diseases of the circulatory system through June 2, 2020. Of these, 199,311 occurred during the pre-pandemic period (January 1, 2020, to March 17, 2020), and 197,731 occurred during the pandemic period (March 18, 2020, to June 2, 2020). Across the 6 most affected states, there was a total of 85,262 deaths, 39,053 of which occurred during the pre-pandemic period and 46,209 of which occurred during the pandemic period. Weekly mortality rates (per 100,000 population) by cause of death in the United States in 2020, compared with the same period in 2019, are shown in the Central Illustration and Supplemental Table 1. Weekly mortality rates by cause of death for each of the seven jurisdictions are shown in Figure 1 and Supplemental Table 2.
Central Illustration.
Weekly Death Rates by Cardiovascular Cause (per 100,000 Population) in the United States
Weekly death rates (per 100,000 population) by underlying cause (ischemic heart disease, heart failure, hypertensive diseases, cerebrovascular disease, and other circulatory diseases) are shown in red for January to June 2020, and in blue for the same period in 2019. Conditions considered “other diseases of the circulatory system” include pulmonary embolism, pericarditis, myocarditis, and cardiac arrest. The vertical dashed line represents the onset of the US pandemic (third week of March 2020), when states began experiencing rapid increases in reported COVID-19 cases and implementing stay-at-home orders. Overall, there was an increase in deaths caused by ischemic heart disease and hypertensive disease after the onset of the pandemic.
Figure 1.
Weekly Death Rates (per 100,000 Population) by State (and New York City)
There was a nationwide increase in deaths caused by ischemic heart disease after the onset of the pandemic in 2020, compared with changes over the same period in 2019 (ratio of the relative change in deaths per 100,000 in 2020 vs. the relative change in 2019: 1.11; 95% CI: 1.04 to 1.18) (Table 1 ). A similar increase was observed for deaths caused by hypertensive disease (1.17; 95% CI: 1.09 to 1.26) but not for heart failure (0.97; 95% CI: 0.92 to 1.01), cerebrovascular disease (1.03; 95% CI: 0.99 to 1.07), or other diseases of the circulatory system (0.99; 95% CI: 0.95 to 1.04).
Table 1.
Change in Death Rates Associated With the COVID-19 Pandemic in the United States
| Relative Change in Death Rate in 2019∗ (3/19–6/3 vs. 1/1–3/18) (95% CI) | Relative Change in Death Rate in 2020† (3/18–6/2 vs. 1/1–3/17) (95% CI) | Ratio of Relative Change in Death Rates in 2020 versus 2019‡ (95% CI) | |
|---|---|---|---|
| Ischemic heart disease | 0.93 (0.88–0.97) | 1.03 (0.98–1.07) | 1.11 (1.04–1.18) |
| Heart failure | 0.95 (0.92–0.98) | 0.92 (0.89–0.95) | 0.97 (0.92–1.01) |
| Hypertensive diseases | 0.93 (0.88–0.98) | 1.09 (1.03–1.14) | 1.17 (1.09–1.26) |
| Cerebrovascular disease | 0.94 (0.92–0.97) | 0.97 (0.95–1) | 1.03 (0.99–1.07) |
| Other diseases of the circulatory system§ | 0.93 (0.9–0.95) | 0.92 (0.89–0.95) | 1.99 (0.95–1.04) |
Ratio of the average weekly mortality rate (per 100,000 population) from March 19 to June 3, 2019 versus January 1 to March 18, 2019.
Ratio of the average weekly mortality rate (per 100,000 population) from March 18 to June 2, 2020 (pandemic period) versus January 1 to March 17, 2020 (pre-pandemic period). March 18, 2020 was chosen as the start of the pandemic period, as states began experiencing rapid increases in reported COVID-19 cases and implementing stay-at-home orders during the third week of March 2020.
Ratio of the change in the average weekly mortality rate in 2020 (March 18 to June 2 vs. January 1 to March 17) compared with the change in the average weekly mortality rate during the same periods in 2019 (March 19 to June 3 vs. January 1 to March 18). This ratio reflects the relative change in mortality rates attributable to the pandemic in 2020, compared with a historical control (2019).
Conditions considered “other diseases of the circulatory system” include pulmonary embolism, pericarditis, myocarditis, and cardiac arrest.
New York City experienced the largest relative increase in deaths caused by ischemic heart disease (ratio of the relative change in deaths per 100,000 in 2020 vs. the relative change in 2019: 2.39; 95% CI: 1.39 to 4.09) during the pandemic, compared with baseline changes in 2019 (Table 2 ). A more modest increase in deaths caused by ischemic heart disease was seen in the remainder of New York State (1.44; 95% CI: 1.16 to 1.79), New Jersey (1.45; 95% CI: 1.22 to 1.73), Michigan (1.23; 95% CI: 1.07 to 1.41), and Illinois (1.11; 95% CI: 1.04 to 1.19) but not in Massachusetts or Louisiana. There were also relative increases in deaths caused by hypertensive diseases after the onset of the pandemic in New York City (2.64; 95% CI: 1.52 to 4.56), the remainder of New York State (1.28; 95% CI: 1.06 to 1.55), New Jersey (1.88; 95% CI: 1.38 to 2.57), Michigan (1.16; 95% CI: 1.00 to 1.35), and Illinois (1.30; 95% CI: 1.12 to 1.51). New Jersey was the only state that experienced a rise in deaths caused by cerebrovascular disease (1.28; 95% CI: 1.09 to 1.51), and New York City was the only jurisdiction where there was a rise in deaths caused by other diseases of the circulatory system (1.65; 95% CI: 1.20 to 2.27). In contrast, deaths caused by heart failure did not increase in any state.
Table 2.
Change in Death Rates Associated with the COVID-19 Pandemic by State (and New York City)
| Relative Change in Death Rate in 2019∗ (3/19–6/3 vs. 1/1–3/18) (95% CI) | Relative Change in Death Rate in 2020† (3/18–6/2 vs. 1/1–3/17) (95% CI) | Ratio of Relative Change in Death Rates (2020 vs. 2019)‡ (95% CI) | |
|---|---|---|---|
| New York (excluding NYC) | |||
| Ischemic heart disease | 0.87 (0.74–1.02) | 1.26 (1.08–1.46) | 1.44 (1.16–1.79) |
| Heart failure | 0.88 (0.77–0.99) | 0.85 (0.74–0.98) | 0.97 (0.81–1.17) |
| Hypertensive diseases | 0.95 (0.82–1.09) | 1.22 (1.07–1.38) | 1.28 (1.06–1.55) |
| Cerebrovascular disease | 0.94 (0.84–1.04) | 1.00 (0.89–1.11) | 1.07 (0.91–1.25) |
| Other diseases of the circulatory system§ | 0.96 (0.89–1.05) | 0.87 (0.8–0.95) | 0.91 (0.81–1.02) |
| New York City|| | |||
| Ischemic heart disease | 0.89 (0.59–1.33) | 2.12 (1.49–3.01) | 2.39 (1.39–4.09) |
| Hypertensive diseases | 0.87 (0.57–1.33) | 2.28 (1.62–3.23) | 2.64 (1.52–4.56) |
| Cerebrovascular disease | 0.94 (0.77–1.15) | 1.20 (1.00–1.44) | 1.28 (0.97–1.68) |
| Other diseases of the circulatory system§ | 0.82 (0.65–1.03) | 1.35 (1.08–1.68) | 1.65 (1.2–2.27) |
| New Jersey | |||
| Ischemic heart disease | 0.88 (0.77–1.00) | 1.28 (1.13–1.44) | 1.45 (1.22–1.73) |
| Heart failure | 0.95 (0.83–1.08) | 1.11 (0.98–1.26) | 1.17 (0.98–1.41) |
| Hypertensive diseases | 0.89 (0.71–1.12) | 1.67 (1.35–2.06) | 1.88 (1.38–2.57) |
| Cerebrovascular disease | 0.86 (0.76–0.97) | 1.10 (0.98–1.23) | 1.28 (1.09–1.51) |
| Other diseases of the circulatory system§ | 0.95 (0.83–1.09) | 1.07 (0.94–1.22) | 1.12 (0.93–1.35) |
| Massachusetts | |||
| Ischemic heart disease | 0.92 (0.82–1.03) | 1.02 (0.9–1.15) | 1.11 (0.94–1.31) |
| Heart failure | 0.84 (0.73–0.96) | 0.89 (0.78–1.02) | 1.06 (0.88–1.29) |
| Hypertensive diseases | 0.97 (0.82–1.14) | 1.02 (0.88–1.19) | 1.06 (0.85–1.32) |
| Cerebrovascular disease | 0.88 (0.79–0.99) | 1.01 (0.9–1.14) | 1.14 (0.97–1.35) |
| Other diseases of the circulatory system§ | 0.86 (0.76–0.96) | 0.96 (0.86–1.08) | 1.12 (0.95–1.32) |
| Louisiana | |||
| Ischemic heart disease | 0.96 (0.88–1.04) | 1.05 (0.97–1.13) | 1.10 (0.98–1.23) |
| Heart failure | 0.85 (0.75–0.97) | 0.98 (0.86–1.11) | 1.15 (0.96–1.38) |
| Hypertensive diseases | 1.09 (0.94–1.28) | 1.09 (0.95–1.27) | 1.00 (0.81–1.24) |
| Cerebrovascular disease | 0.88 (0.75–1.02) | 0.96 (0.82–1.11) | 1.09 (0.88–1.35) |
| Other diseases of the circulatory system§ | 0.94 (0.83–1.06) | 0.89 (0.79–1.00) | 0.95 (0.8–1.12) |
| Michigan | |||
| Ischemic heart disease | 0.89 (0.81–0.98) | 1.09 (0.99–1.2) | 1.23 (1.07–1.41) |
| Heart failure | 0.94 (0.83–1.08) | 1.06 (0.93–1.22) | 1.13 (0.93–1.36) |
| Hypertensive diseases | 0.99 (0.89–1.11) | 1.16 (1.05–1.28) | 1.16 (1.00–1.35) |
| Cerebrovascular disease | 0.97 (0.88–1.06) | 1.03 (0.94–1.13) | 1.07 (0.93–1.22) |
| Other diseases of the circulatory system§ | 0.95 (0.87–1.04) | 0.96 (0.89–1.05) | 1.02 (0.90–1.15) |
| Illinois | |||
| Ischemic heart disease | 0.90 (0.86–0.95) | 1.00 (0.95–1.05) | 1.11 (1.04, 1.19) |
| Heart failure | 0.91 (0.83–0.98) | 0.90 (0.83–0.98) | 1.00 (0.89–1.12) |
| Hypertensive diseases | 0.89 (0.80–1.00) | 1.16 (1.05–1.28) | 1.30 (1.12–1.51) |
| Cerebrovascular disease | 0.91 (0.85–0.98) | 1.00 (0.94–1.08) | 1.10 (0.99–1.21) |
| Other diseases of the circulatory system§ | 0.94 (0.87–1.02) | 1.03 (0.96–1.11) | 1.10 (0.98–1.22) |
Ratio of the average weekly mortality rate (per 100,000 population) from March 19 to June 3, 2019 versus January 1 to March 18, 2019.
Ratio of the average weekly mortality rate (per 100,000 population) from March 18 to June 2, 2020 (pandemic period) versus January 1 to March 17, 2020 (pre-pandemic period). March 18, 2020 was chosen as the start of the pandemic period, as states began experiencing a rapid increase in reported COVID-19 cases and implementing stay-at-home orders during the third week of March 2020.
Ratio of the change in the average weekly mortality rate in 2020 (March 18 to June 2 vs. January 1 to March 17) compared with the change in the average weekly mortality rate during the same periods in 2019 (March 19 to June 3 vs. January 1 to March 18). This ratio reflects the relative change in mortality rates attributable to the pandemic in 2020, compared with a historical control (2019).
Conditions considered “other diseases of the circulatory system” include pulmonary embolism, pericarditis, myocarditis, and cardiac arrest.
Relative change in heart failure deaths for New York City (NYC) are not shown, owing to a high number of missing values for 2019.
Discussion
In the United States, there have been marked increases in deaths caused by ischemic heart disease and hypertensive heart disease since the onset of the COVID-19 pandemic. In contrast, deaths caused by heart failure and cerebrovascular disease have not increased. Among the areas initially most affected by COVID-19, New York City experienced the largest relative rise in deaths from ischemic heart disease (139%) and hypertensive disease (164%) compared with a historical baseline. More modest increases in deaths due to these causes also occurred in the remainder of New York State, Michigan, and New Jersey, with the latter also experiencing a rise in deaths caused by cerebrovascular disease.
The large increase in population-level deaths caused by ischemic heart disease suggests that the pandemic may have had important indirect effects on cardiovascular outcomes. Although hospitalizations for acute myocardial infarction, and cardiac catheterization laboratory activations for ST-segment elevation myocardial infarction (12), have declined substantially during the pandemic (5, 6, 7), it is unlikely that these changes reflect a true reduction in the incidence of cardiovascular events. Instead, our findings suggest that patients with acute coronary syndromes who require emergent treatment may be avoiding medical care and dying at home, possibly because of concerns about contracting the virus in a hospital setting, and consistent with reports that deaths at home have risen dramatically in areas of the United States hardest hit by COVID-19 (3,4,13,14). In addition, the incidence out-of-hospital cardiac arrests has increased during the pandemic and cannot be entirely explained by COVID-19 (8,15). Recent evidence indicate that delays in emergency medical service response times and a reduction in bystander cardiopulmonary resuscitation rates have likely contributed to reduced survival after cardiac arrest (16). In contrast, we observed no increase in deaths caused by other cardiovascular conditions, such as heart failure, possibly because they often do not require emergent hospitalization for potentially life-saving treatment. Overall, our data highlight the urgent need to improve public health messaging, communication, and education to ensure that patients with emergent conditions seek and receive medical care, particularly in regions that are currently experiencing surges or resurgences of COVID-19 cases.
Health care-system factors may also explain the rise in cardiovascular deaths during the pandemic. The cancellation of outpatient cardiovascular visits has likely delayed access to medication prescriptions/refills and important diagnostic testing (17). In addition, the delay of semi-elective cardiovascular procedures (e.g., transcatheter aortic valve replacement) may have adversely affected higher-risk patients with cardiovascular disease. Health care systems in some regions were also pushed to adapt and reallocate resources rapidly to care for the surge of patients with COVID-19. The burden imposed on some hospitals may have led to delays in access to care or the delivery of suboptimal inpatient and procedural care for non–COVID-19 patients (18). One recent study, for example, found markedly higher in-hospital mortality rates for patients with ST-segment elevation myocardial infarction during the pandemic (19). This might explain why Massachusetts, which had time to plan for a surge of COVID-19 cases and expand hospital capacity and staffing effectively, did not experience an increase in cardiovascular deaths. Beyond health care-system factors, greater psychosocial, community, and environmental stress amid the pandemic also may have played important roles.
Although our analysis excluded deaths with underlying causes of COVID-19, it is possible that some COVID-19 deaths were misclassified as cardiovascular deaths or that a portion of cardiovascular deaths were related to COVID-19. Preliminary reports suggest cardiac complications among patients with COVID-19, including myocardial injury (20), myocarditis (21), ventricular arrhythmias, and shock (22), which are associated with higher risk of mortality (23). A recent autopsy series of deaths during the pandemic, however, found that reduced access to health care systems (for conditions such as myocardial infarction) was more far likely to be identified as a contributory factor to death than undiagnosed COVID-19 (9). Further, our findings are consistent with analyses from other nations, such as England and Wales, which have also experienced an increase in acute cardiovascular deaths, most of which were unrelated to COVID-19 (24).
Study limitations
First, our analysis was based on provisional data from the Centers for Disease control and Prevention (CDC), which may be incomplete in recent weeks owing to reporting delays. We only analyzed data through June 2, to minimize the effect of reporting delays. Second, our analysis only included underlying causes of death caused by cardiovascular diseases, but it is possible that COVID-19 may have been a contributing cause of death. However, the CDC reports that for the majority of deaths (95%) for which COVID-19 is reported on the death certificate, COVID-19 is selected as an underlying cause (11); these deaths were excluded from our analysis. Third, we lacked a contemporaneous control group, but used data during corresponding weeks of the most recent year (2019) as a historical control to quantify increases in deaths attributable to the onset of the pandemic in the United States. Fourth, individual-level demographic data for cardiovascular deaths were not made publicly available by the CDC and require further study, particularly given evidence of significant racial/ethnic and socioeconomic disparities in deaths during the pandemic (25, 26, 27).
Conclusions
Deaths caused by ischemic heart disease and hypertensive diseases increased during the COVID-19 pandemic, particularly in areas that experienced the initial surge of cases in the United States. Our findings suggest that the pandemic may have had an indirect toll on patients with cardiovascular disease, possibly owing to the avoidance of hospitals because of concerns about exposure to the virus, increased strain on health care systems, and deferred outpatient and procedural care. These patterns may also, in part, reflect the cardiovascular sequelae of undiagnosed COVID-19. Further study is needed to clarify the relative extent to which these different mechanisms have contributed to the rise in cardiovascular deaths. As COVID-19 cases surge in different regions of the United States, public health officials and policymakers should improve public health messaging to encourage patients with acute conditions to seek medical care and expand health care system resources to mitigate the indirect effects of the pandemic.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: During the COVID-19 pandemic in the United States, there has been a marked increase in deaths caused by ischemic heart disease and hypertensive diseases.
TRANSLATIONAL OUTLOOK: Further study is needed to clarify the extent to which avoidance of hospital-based treatment because of concern about exposure to the virus, deferred outpatient and procedural care, strain imposed on health care systems, and the cardiovascular sequelae of undiagnosed COVID-19 contributed to the rise in cardiovascular deaths.
Author Disclosures
Dr. Wadhera has received research support from the National Heart, Lung, and Blood Institute (grant K23HL148525-1) at the National Institutes of Health; and has previously served as a consultant for Regeneron, outside the submitted work. Dr. Yeh has received research support from the National Heart, Lung, and Blood Institute (R01HL136708) and the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology; has received personal fees from Biosense Webster; and has received grants and personal fees from Abbott Vascular, AstraZeneca, Boston Scientific, and Medtronic, outside the submitted work. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables, please see the online version of this paper.
Appendix
References
- 1.Coronavirus Resource Center . Johns Hopkins University & Medicine; Baltimore, MD: 2020. COVID-19: United States Cases by County. [Google Scholar]
- 2.Weinberger D.M., Chen J., Cohen T. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324:510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L., Taylor D.D.H. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhatt A.S., Moscone A., McElrath E.E. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76:280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baum A., Schwartz M.D. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324:96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solomon M.D., McNulty E.J., Rana J.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 8.Lai P.H., Lancet E.A., Weiden M.D. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5:1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pell R., Fryer E., Manek S., Winter L., Roberts I.S.D. Coronial autopsies identify the indirect effects of COVID-19. Lancet Public Health. 2020;5:e474. doi: 10.1016/S2468-2667(20)30180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics . Centers for Disease Control and Prevention; Atlanta, GA: 2020. Weekly counts of death by jurisdiction and cause of death. [Google Scholar]
- 11.National Center for Health Statistics . Centers for Disease Control and Prevention; Atlanta, GA: 2020. Excess Deaths Associated with COVID-19. [Google Scholar]
- 12.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hogan G. NPR; New York, NY: 2020. After deaths at home spike in NYC, officials plan to count many as COVID-19. [Google Scholar]
- 14.Gillum J., Song L., Kao J. ProPublica; Washington, DC: 2020. There’s been a spike in people dying at home in several cities; that suggests coronavirus deaths are higher than reported. [Google Scholar]
- 15.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uy-Evanado A., Chugh H.S., Sargsyan A. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. J Am Coll Cardiol EP. 2020 Aug 14 doi: 10.1016/j.jacep.2020.08.010. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehrotra A., Chernew M., Linetsky D., Hatch H., Cutler D., Schneider E.C. The Commonwealth Fund; New York, NY: 2020. The impact of the COVID-19 pandemic on outpatient visits: changing patterns of care in the newest COVID-19 hot spots. [Google Scholar]
- 18.Rosenbaum L. Facing Covid-19 in Italy: ethics, logistics, and therapeutics on the epidemic's front line. N Engl J Med. 2020;382:1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 19.Gluckman T.J., Wilson M.A., Chiu S.T. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1–8. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inciardi R.M., Lupi L., Zaccone G. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:819–824. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goyal P., Choi J.J., Pinheiro L.C. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonow R.O., Fonarow G.C., O'Gara P.T., Yancy C.W. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5:751–753. doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 24.Wu J., Mamas M.A., Mohamed M.O. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2020 Sept 28 doi: 10.1136/heartjnl-2020-317912. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Wadhera R.K., Wadhera P., Gaba P. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Figueroa J.F., Wadhera R.K., Lee D., Yeh R.W., Sommers B.D. Community-level factors associated with racial and ethnic disparities in COVID-19 rates In Massachusetts. Health Aff (Millwood) 2020;39:1984–1992. doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.